Principles of Screening
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
16 Terms
What is screening and its importance
To identify people in an apparently healthy population who are at an increased risk of a health problem or condition
→allows for early intervention to reduce mortality and new cases
→no screening is 100%, but does allow for the individual make an informed choice
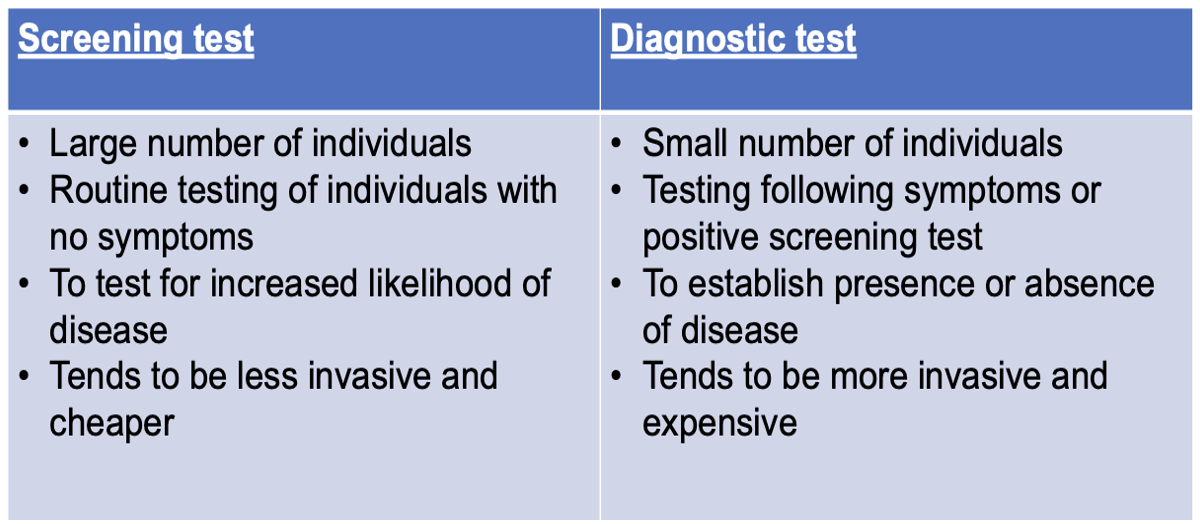
Give the differences between screening and diagnostic tests
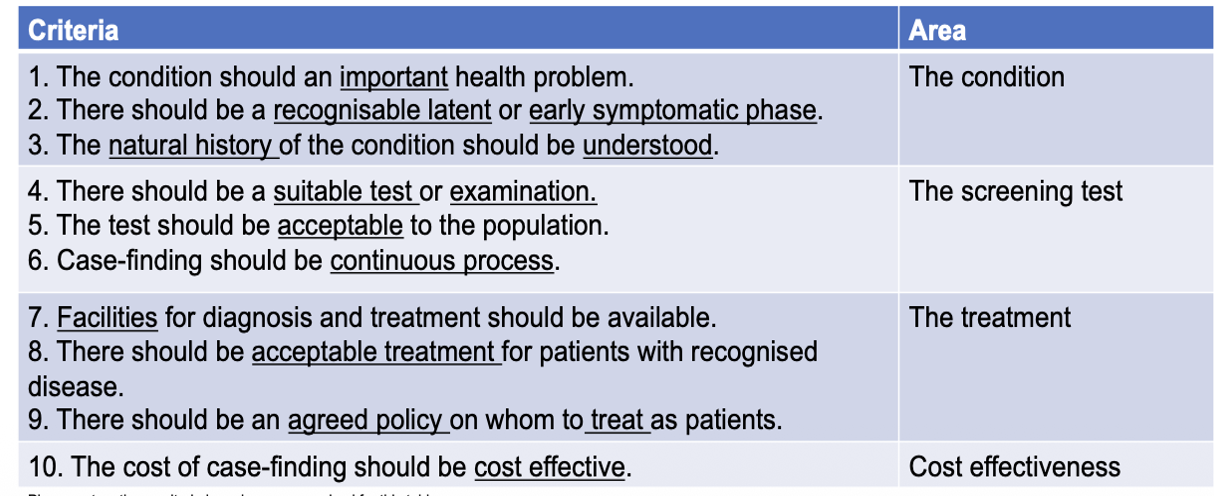
What is the Wilson and Junger screening process
Criteria that shows the importance and screening and how to make it econmically balanced
List 4 benefits of screening
Early intervention of condition allows for early treatment and improve prognosis e.g. neonatal blood spots can detect congenital hypothyroidism
Reduce number of new cases e.g. cervical cancer via screening
Increases choice of individuals by identifying factors early e.g. breast cancer scans
More information to allow for an informed decision about treatment e.g. antenatal screening e.g. Down’s or Patau’s syndrome
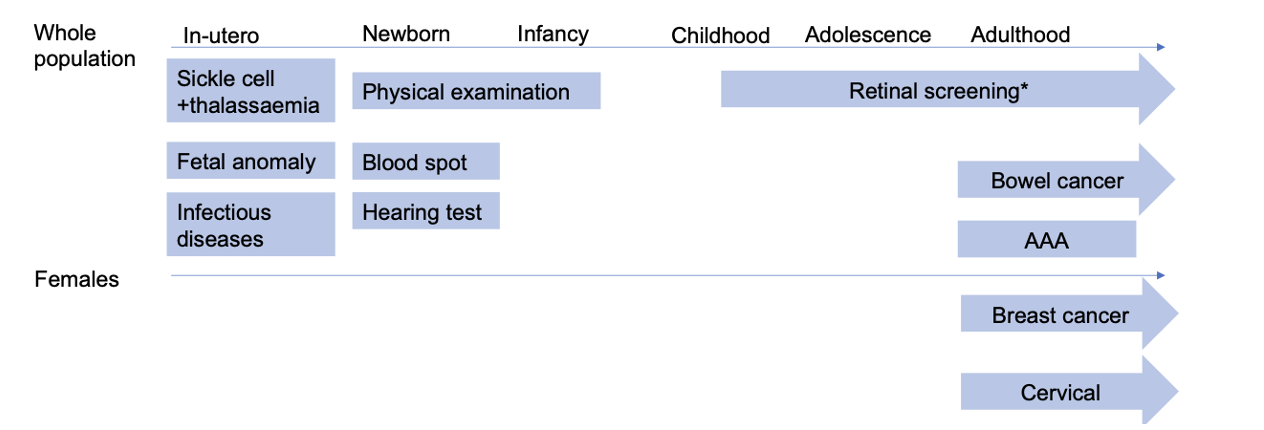
Fill in the gaps on the screening programmes across a life course
State the role with screening with ovarian cancer
6th most in females
earlier diagnosis is associated with higher survival -over 90%- of stage 1 patients are alive 5yrs after diagnosis vs 4% of stage IV
UKCTOCS is used for this screening
Define Lead time bias
Where screening looks like a good thing to do but does not change the outcome as makes survial longer as diagnosis brought forward
List the negatives of screening
Risk of false positives but also false negatives
Can lead to difficult decisions on test e.g. amniocentesis can have risk of miscarriage, stress of outcome
Over-diagnosis in detecting conditions that would never become clinically apparent e.g. small AAA
Beneficial use of limited resources
Exacerbate health inequalities based on uptake
What is PKU used for in screening
HEEL PRICK!!!
inherited metabolic condition caused by defect in enzyme phenylalanine hydroxylase = can lead to learning difficulties
= is asymptomatic at birth
→treatment: dietary manipulation to avoid high protein, regular blood tests = screening cost-effective here
State the screening stages in pregancy
6–9 weeks: Pregnancy confirmation.
11–14 weeks: Dating scan to estimate due date and nuchal translucency (NT) scan (assesses risk of chromosomal conditions).
18–21 weeks: Foetal anomaly scan (checks for 11 major physical conditions).
24–42 weeks: Growth and development monitoring if low amniotic fluid or first pregnancy
What are the optional scans in pregancy
Optional:
3D/4D scans (26–30 weeks).
Non-invasive prenatal testing (NIPT): Maternal blood test to estimate risk of chromosomal syndromes.
What are the newborn screening processes
Physical examination: Checks heart, eyes, hips, testes.
Hearing test: Detects early hearing loss.
Blood spot (“heel prick”) test:
Done at around 5 days old.
Tests for 9 rare but serious conditions, such as cystic fibrosis and sickle cell disease.
What are the screening for women commonly used
Cervical (HPV) screening:
Ages 25–49: every 3 years.
Ages 50–64: every 5 years.
Detects high-risk HPV types that can cause cervical cancer.
Breast screening:
Ages 50–53 (first invite), then every 3 years up to age 71 (can opt to continue).
Uses mammogram to detect early breast cancer.
Bowel cancer screening:
Ages 60–74: home test kit every 2 years.
Over 75s can request to continue screening.
What are the common screening scans for males
Bowel cancer screening: same as above.
Abdominal Aortic Aneurysm (AAA): offered at 65 years.
What is diabetic eye screening
Offered to all individuals with diabetes (type 1 or 2) from age 12 onwards.
Checks for diabetic retinopathy.
Conducted every 1–2 years alongside regular eye checks.
Applies to both sexes.
What is the committee that oversees screening
UK National Screening Committee (UK NSC)
key in making sure that the benefits outweigh the harm