PIE- Reproductive Pathology in the Male
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
What are the main types of disorders of the Testis and Epididymis? (4)
- Developmental anomalies
- Degeneration
- Inflammation
- Neoplasia
OR
class them as an increase in size or decrease in size
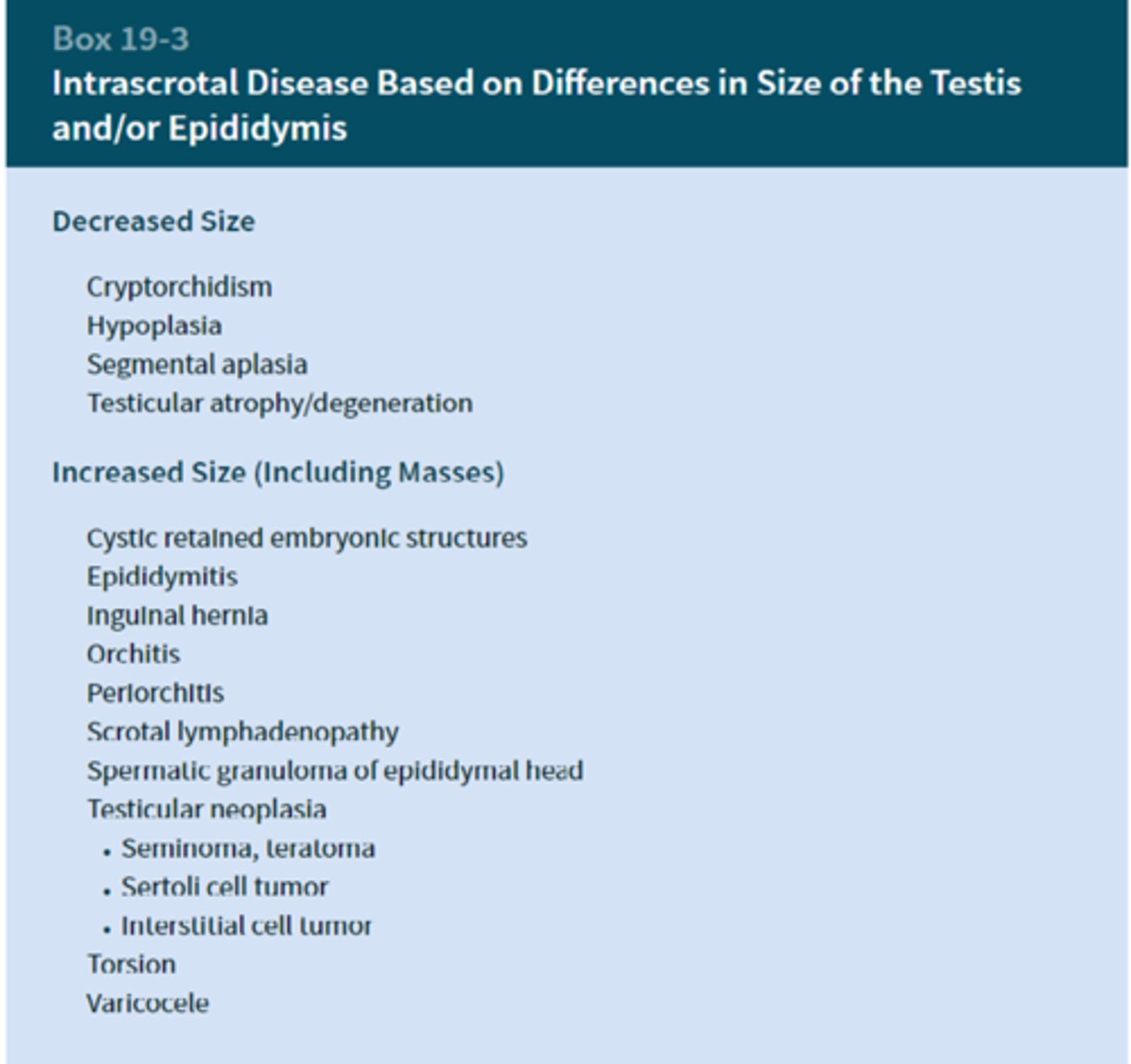
what conditions cause a decrease in testis size
cryptorchidism
hypoplasia
segmental aplasia
testicular atrophy
what conditions cause a increase in testis size
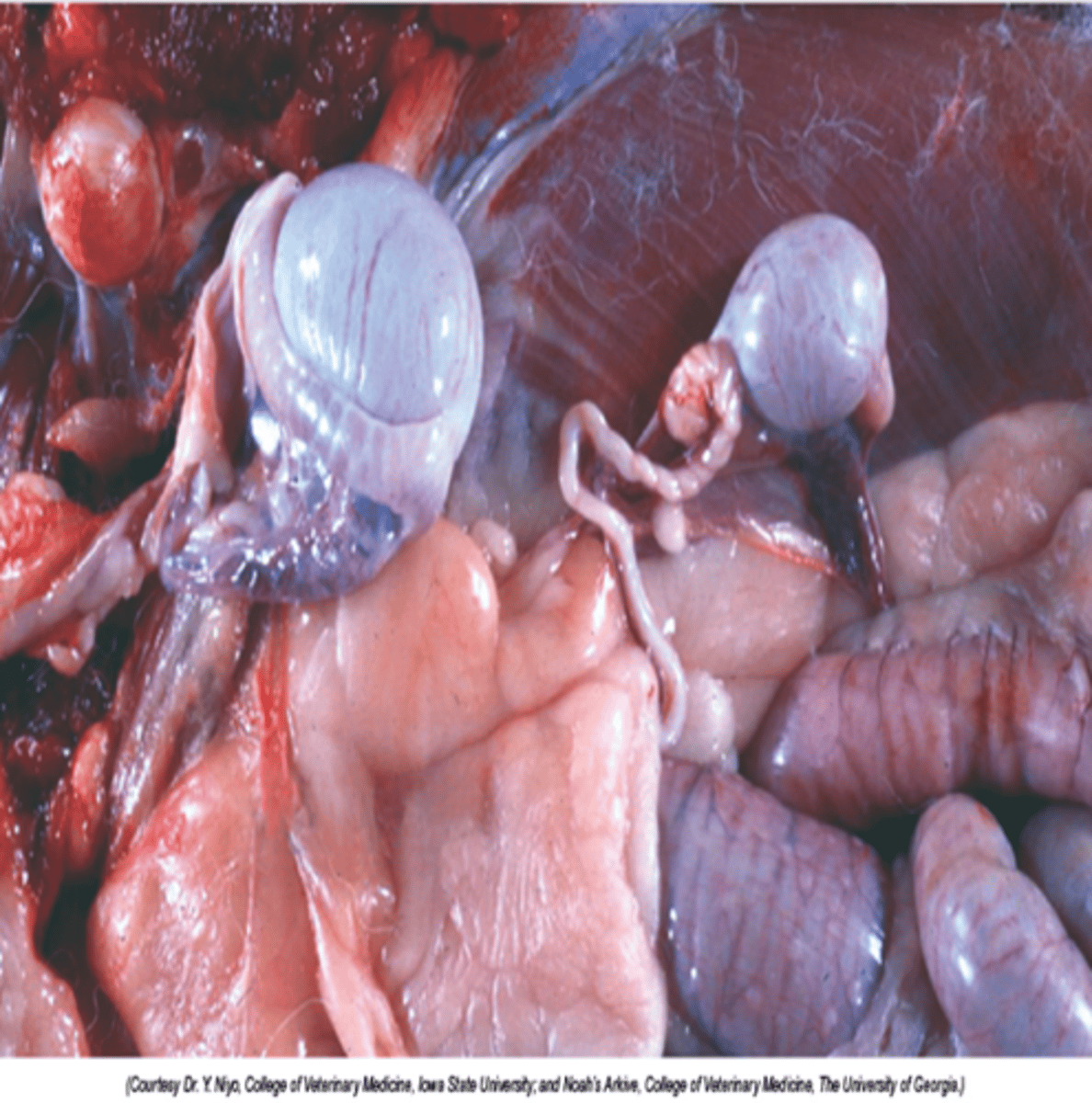
What is cryptorchidism?
Incomplete descent of the testis, they're retained between kidney, inguinal canal → in abd cavity
- Likely polygenetic basis, multiple gene mutations involved.
- Often hypoplastic (small testes due to arrested development)
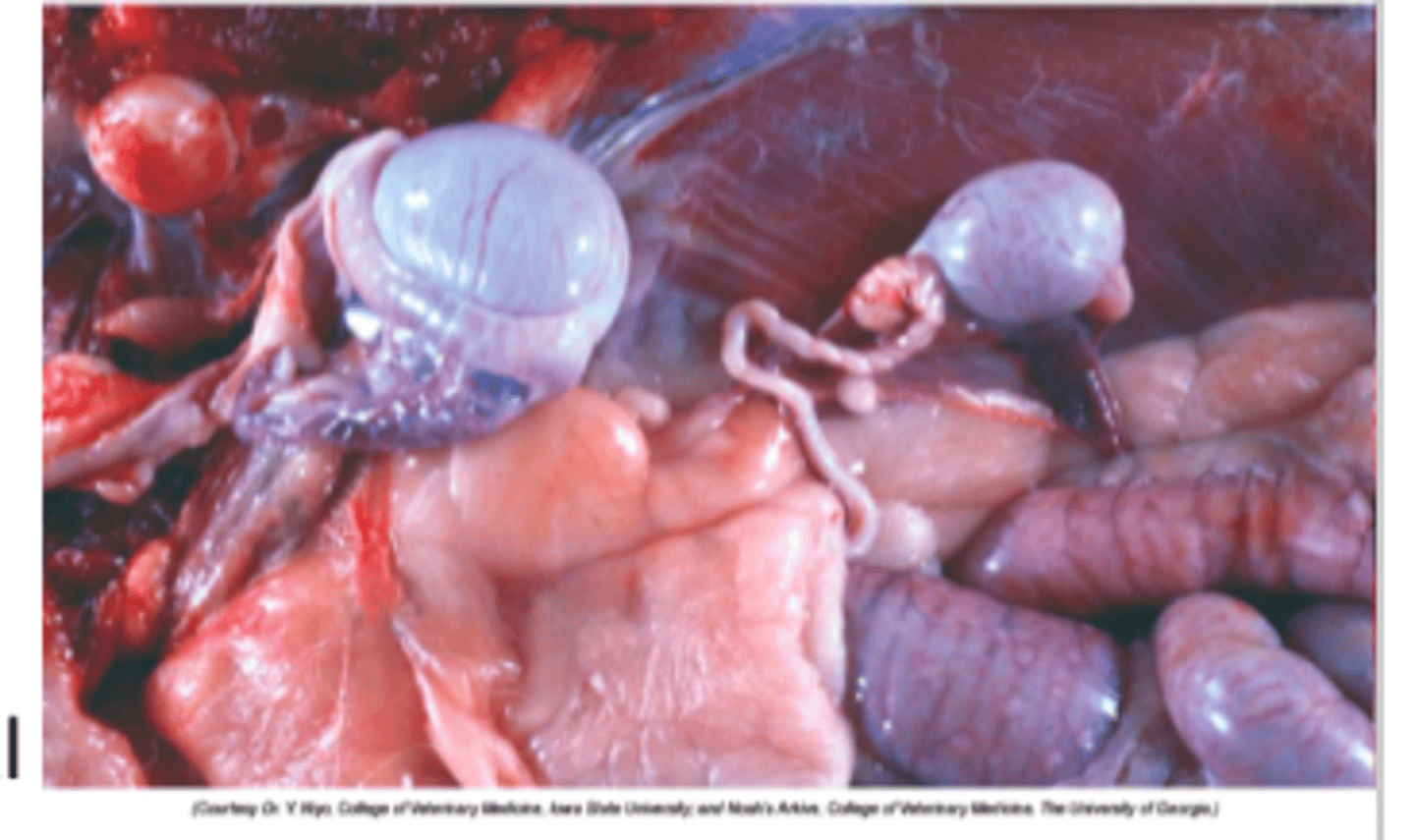
What is the main concern with cryptorchidism?
Increased risk of tumour formation
Is cryptorchidism more likely to be uni or bilateral?
Unilateral
What is testicular hypoplasia?
Hypoplastic (organ/tissue has underdeveloped or has had incomplete development)- so still has normal consistency for a testes.
But testes appear smaller than normal for age and animal.
When does testicular hypoplasia occur?
Congenital or pre-puberty but often isn't observed until after puberty. → so cant diagnose until here
Is testicular hypoplasia more likely to be uni or bilateral?
Both!
What are some causes of testicular hypoplasia?
- Nutrition (Zn def.)
- Genetic
- Endocrine abnormalities
What species are most commonly affected by testicular hypoplasia?
Mostly cattle, sheep, and goats.
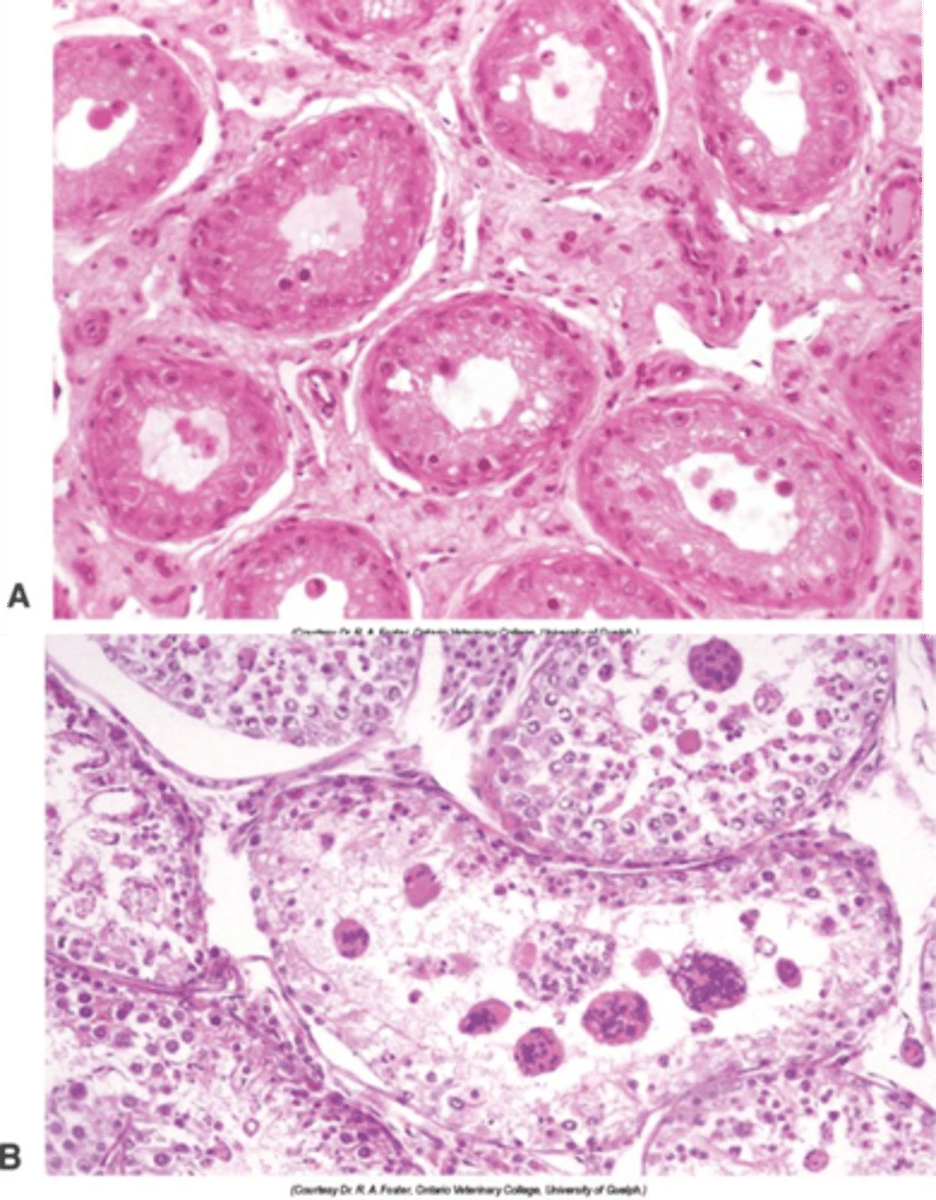
Describe the histological appearance of testicular hypoplasia
Absent/ incomplete spermatogenesis with hypoplastic and normal tubules often intermingled
what is a common cause of male infertility?
Testicular atrophy/degeneration
define Atrophy
Atrophy is a cellular adaptation that causes cells, tissues, or organs to shrink in size.
What is testicular atrophy/degeneration?
One or both testicles shrink in size,
often accompanied by reduced testicular function, which can lead to decreased sperm production and lower testosterone levels due to a loss of germ cells and Leydig cells within the testes; essentially, the tissue within the testicles is Wdegenerating and shrinking the organ itself.
When does Testicular Atrophy/Degeneration occur?
After puberty
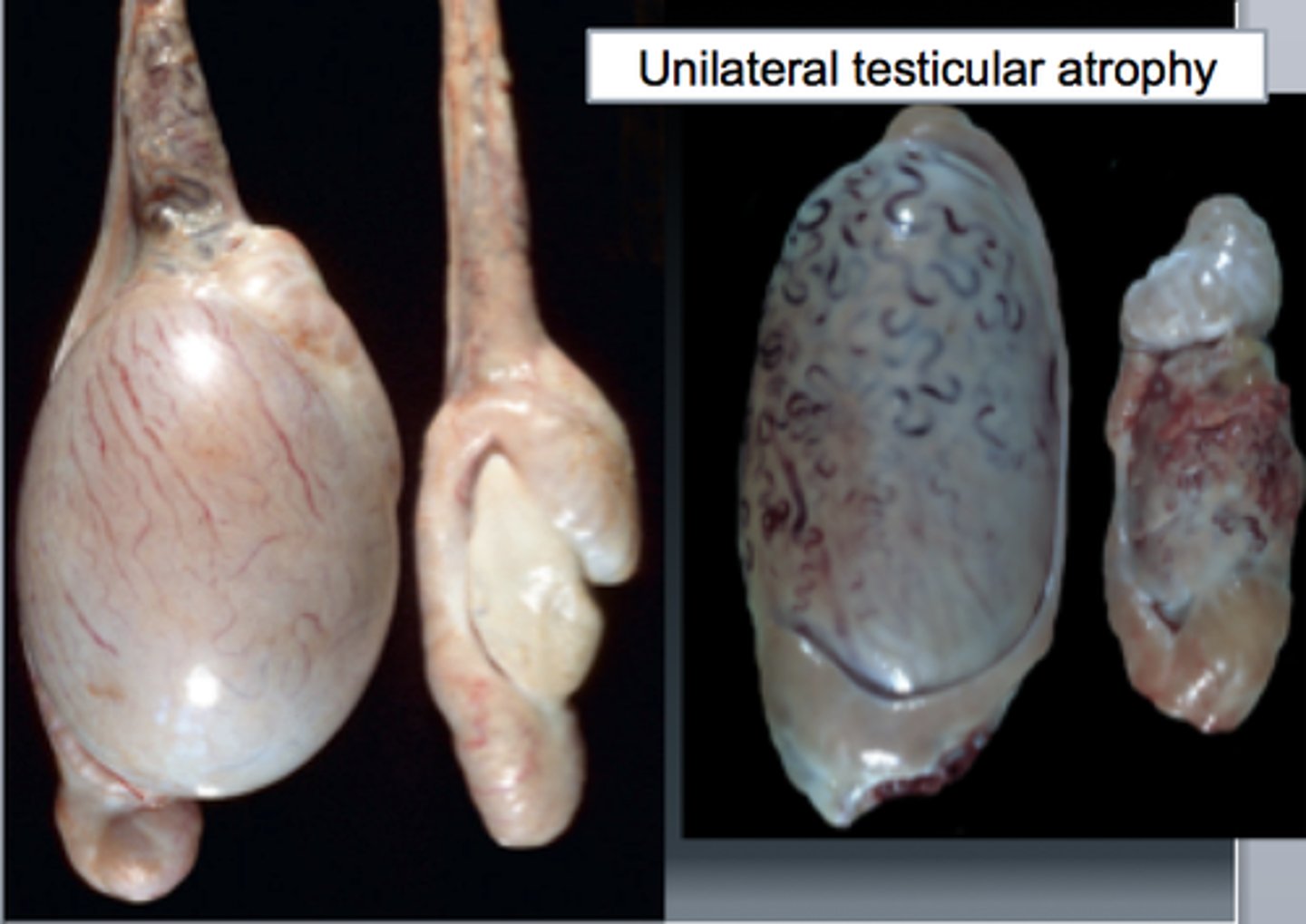
Is testicular atrophy/degeneration more likely to be uni or bilateral?
both!
What is the consistency of tests affected by testicular atrophy/degeneration?
Small - firm consistency (chronic)
Fibrosis gives a firmer texture
the fibrosis that is deposited expands the interstitial space
Causes of Testicular Atrophy/Degeneration (8)
- Infections
- Increased scrotal temperature
- Decreased testicular blood supply
- Vitamin A/Zn deficiency
- Drug reactions
- Radiation damage
- Obstruction
- Hyperoestrogenism
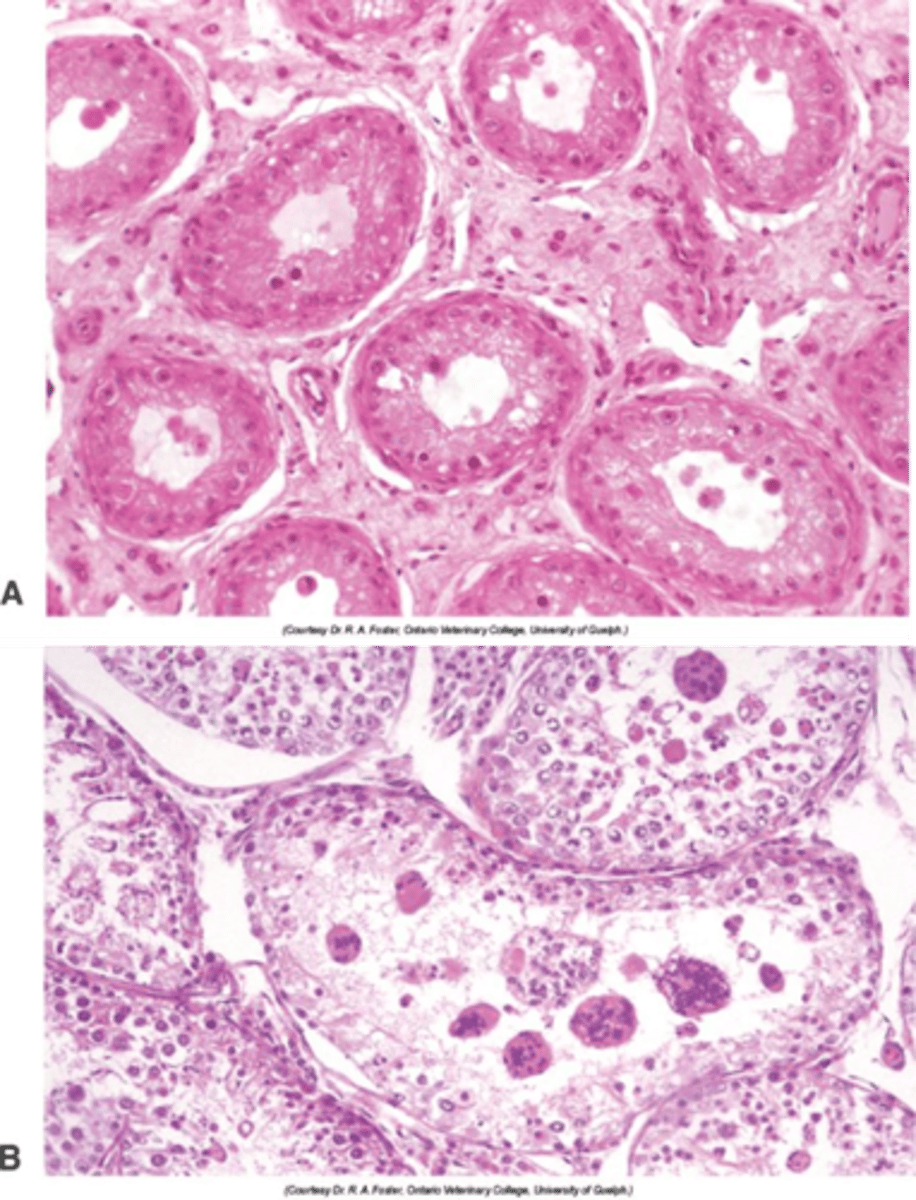
Describe the histological appearance of testicular atrophy/degeneration
Similar to hypoplasia (incomplete/underdevelopment of organ/tissue): +/- fibrosis, multinucleated spermatids
Degeneration of seminiferous tubules
absence of spermatogenesis
What is epididymitis?
inflammation of epididymis
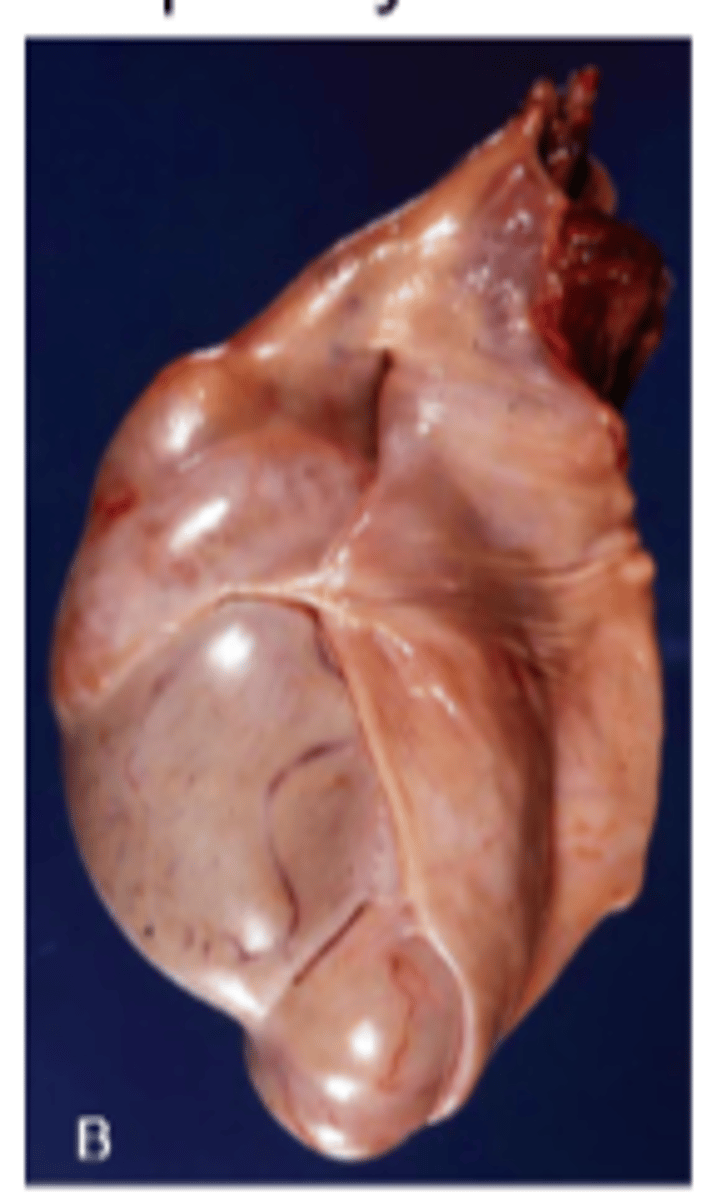
What is orchitis?
inflammation of a testicle
Epididymitis
Inflammation of the epididymis
- Almost always affects the tail of the epididymis (different from spermatic granuloma of the epididymal head)
What is more common epididymitis or orchitis?
epididymitis
What two species are affected most by epididymitis?
Rams and dogs
What is a common cause of epididymitis in rams?
Brucella ovis - notifiable
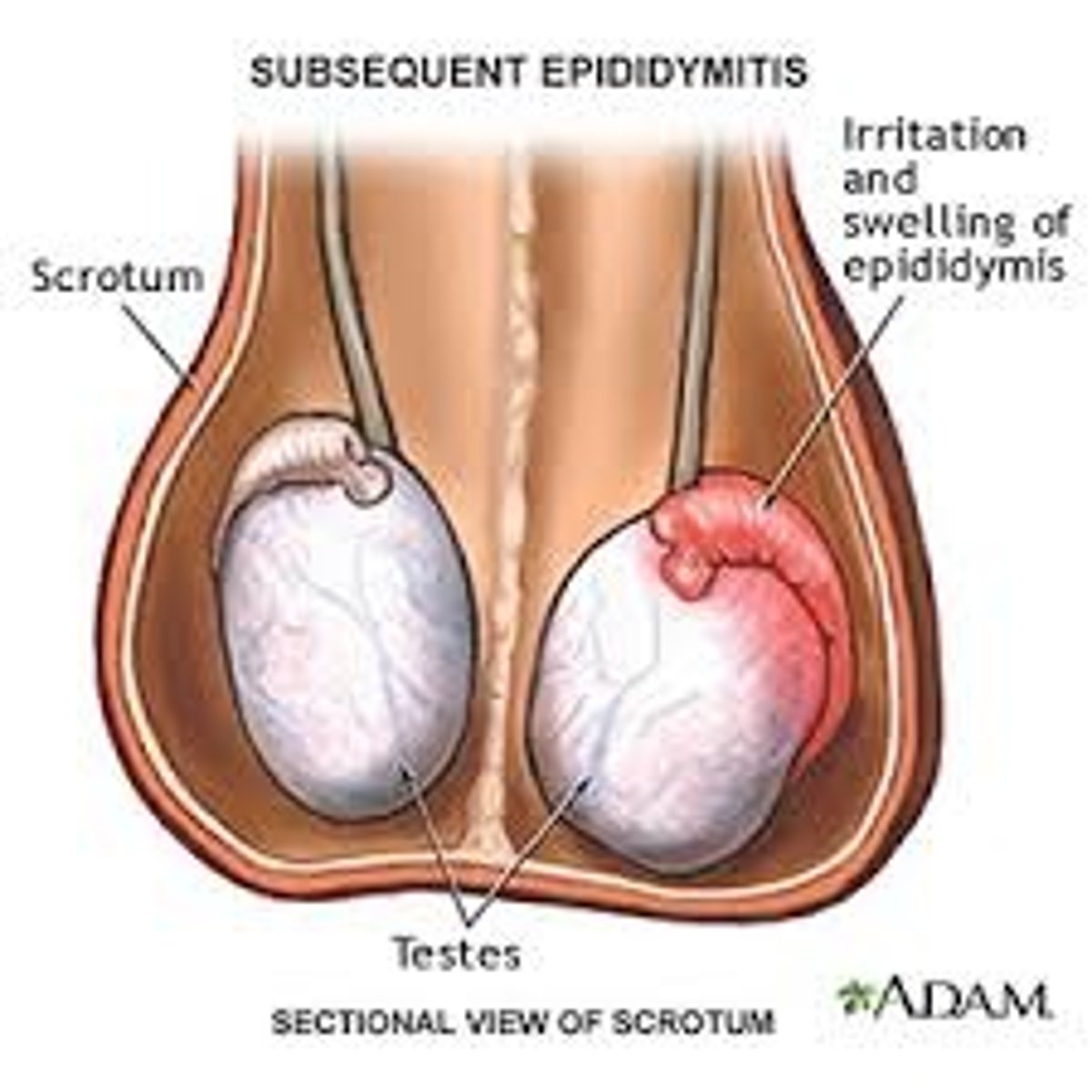
What is epididymitis most commonly caused by?
- Mostly ascending infection (accessory glands, urinary tract) → ecoli common
- Rarer haematogenous (e.g. Brucella spp) or trauma
What can occur secondary to epididymitis?
Secondary testicular degeneration/atrophy
By compression due to inflam or pyrexia
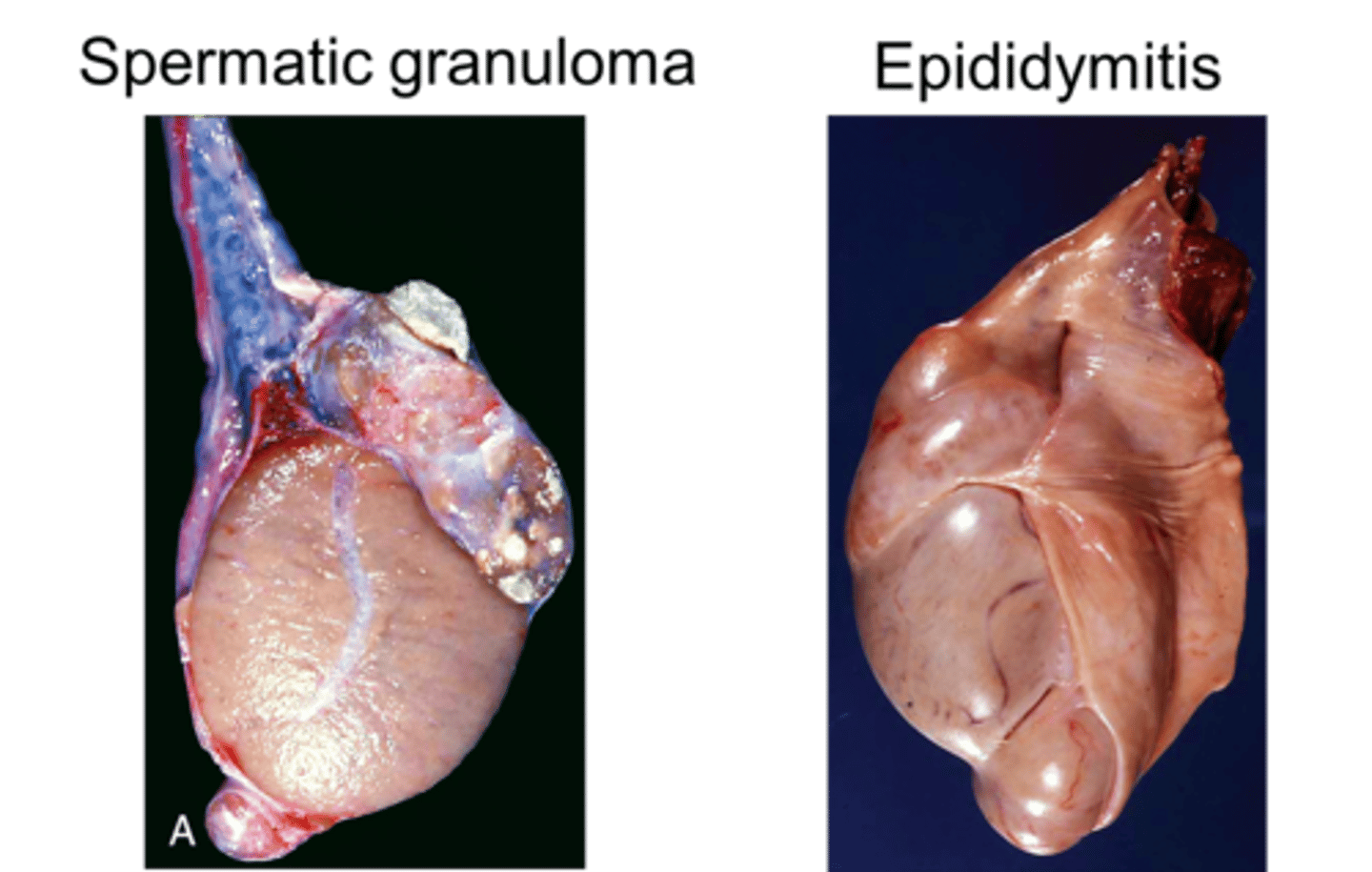
What is spermatic granuloma?
- Spermatic granuloma is an inflammatory condition not caused by infection, but as response to extravasated spermatozoa (like from vasectomy/trauma/obstruction)
- The inflammation predominantly involves the efferent ducts (which are part of the spermatic duct system) and can spread to the head of the epididymis as well.
-get incrs in size of head of epididymis
in epididymitis what incrs in size
the whole of the epididymis
Describe testicular neoplasia
- More common in older dogs (>> horses)
- Almost always benign
- Three primary types that may also occur in combination
Primary types of testicular neoplasia (3)
1. Seminoma (germ cell tumour, also teratoma) (spermatozoa)
2. Interstitial (Leydig) cell tumour
3. Sertoli cell tumour
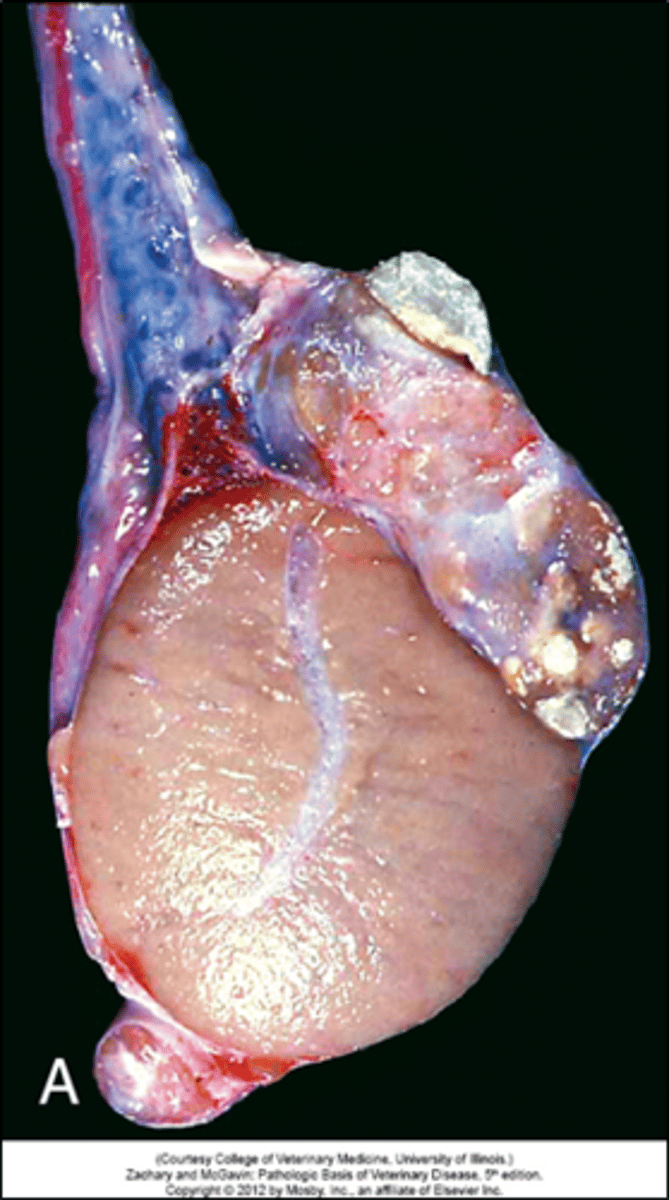
Describe seminoma
Derived from spermatogonia (germ cell tumour, homogenous)
2nd most common dog; most common in aged stallions
Causes swelling and pain
More prevalent in retained testes
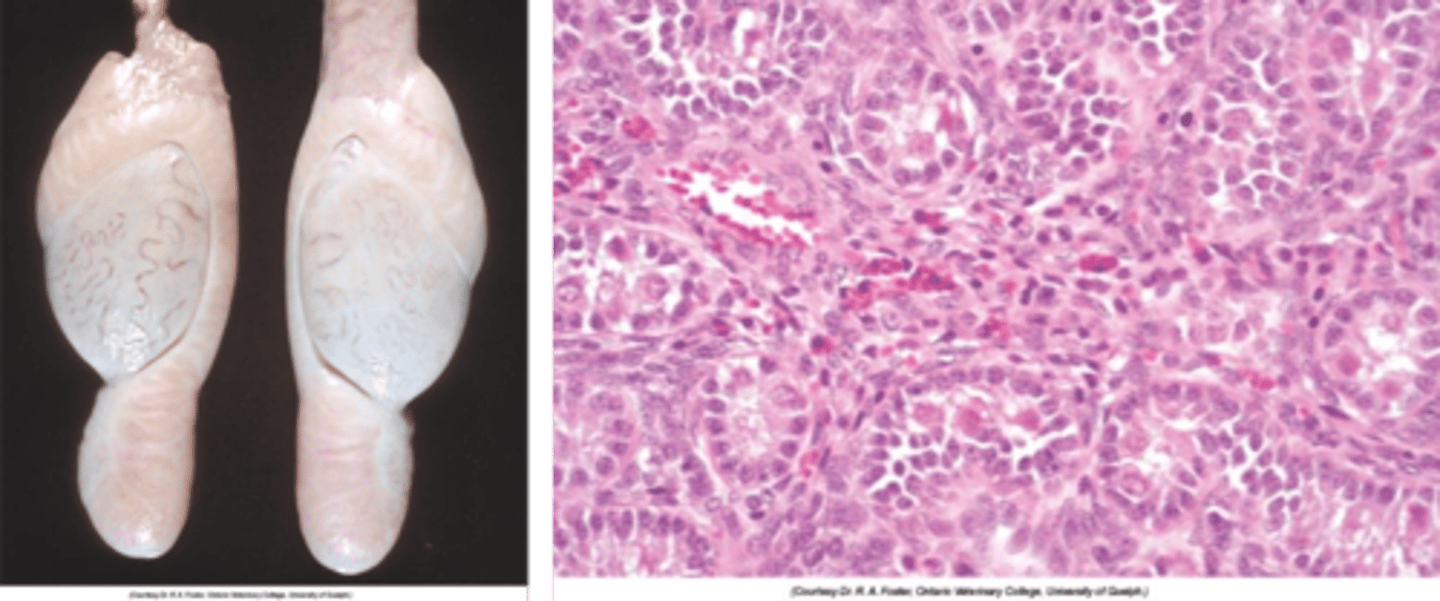
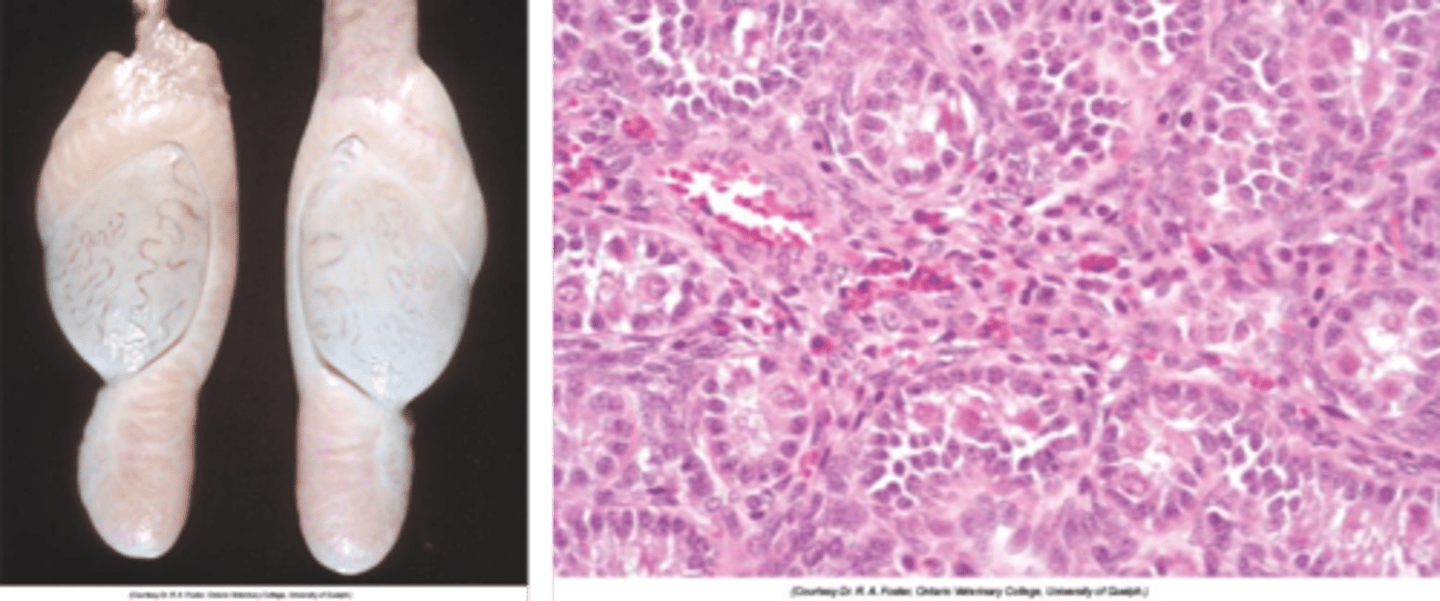
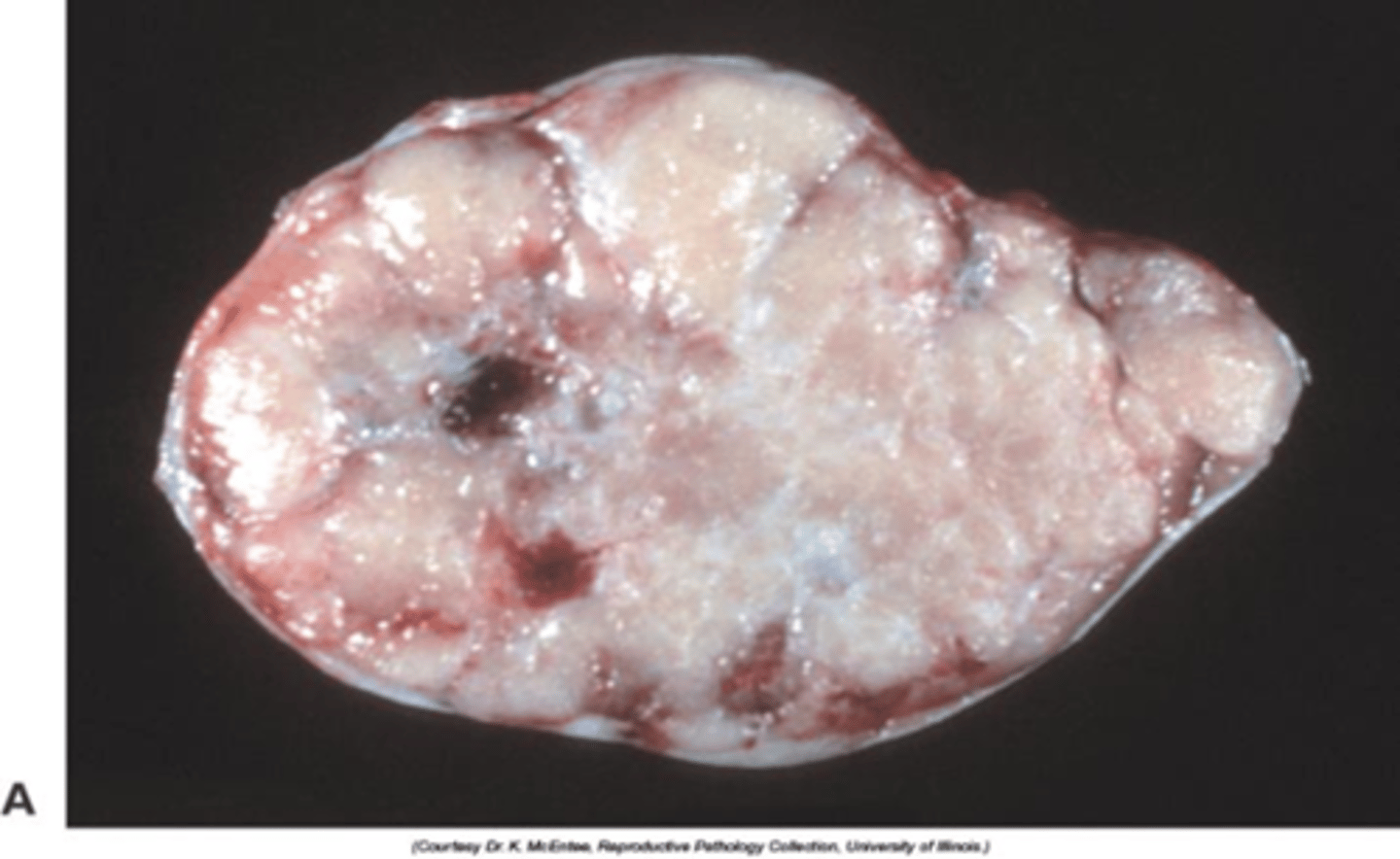
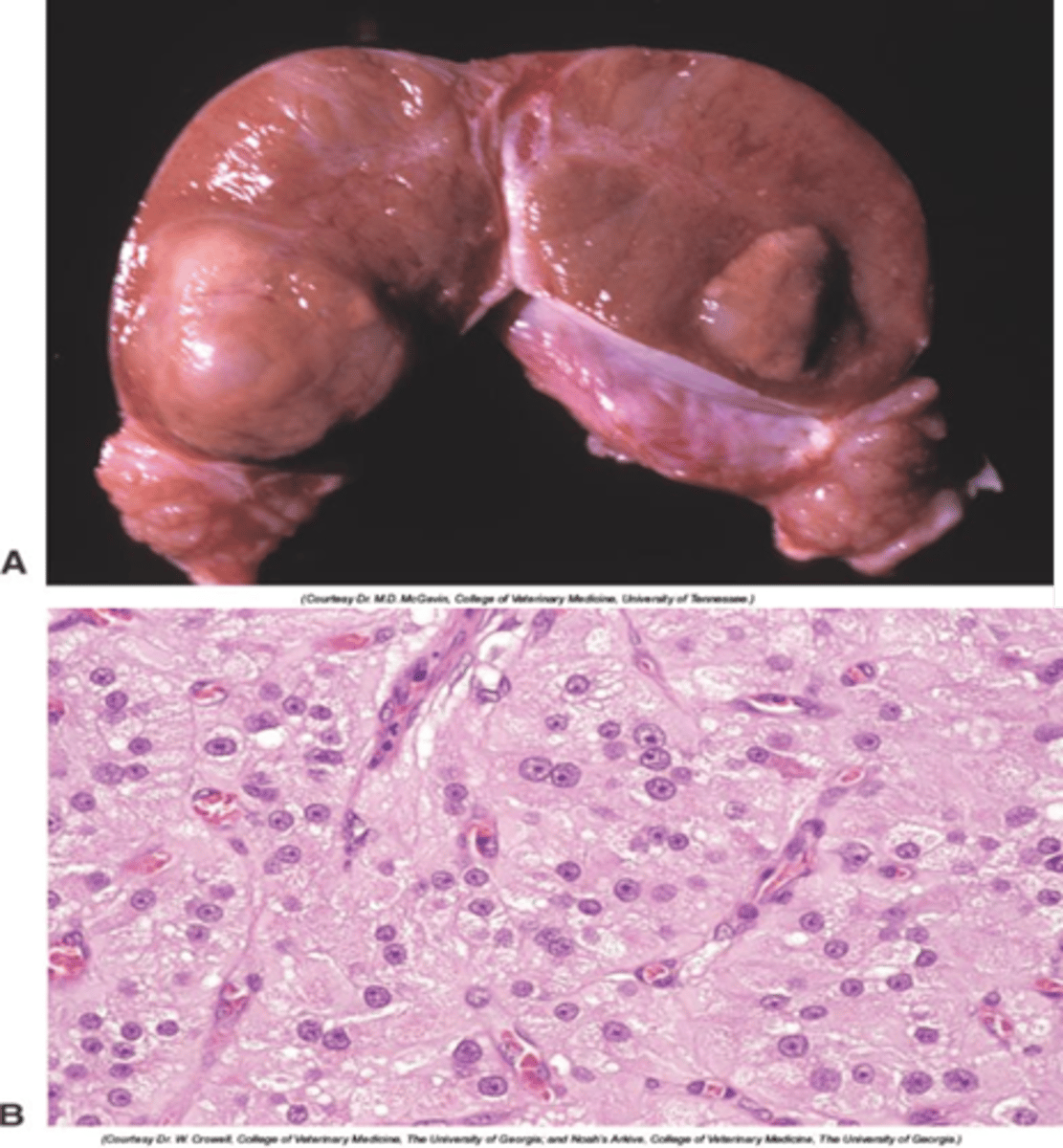
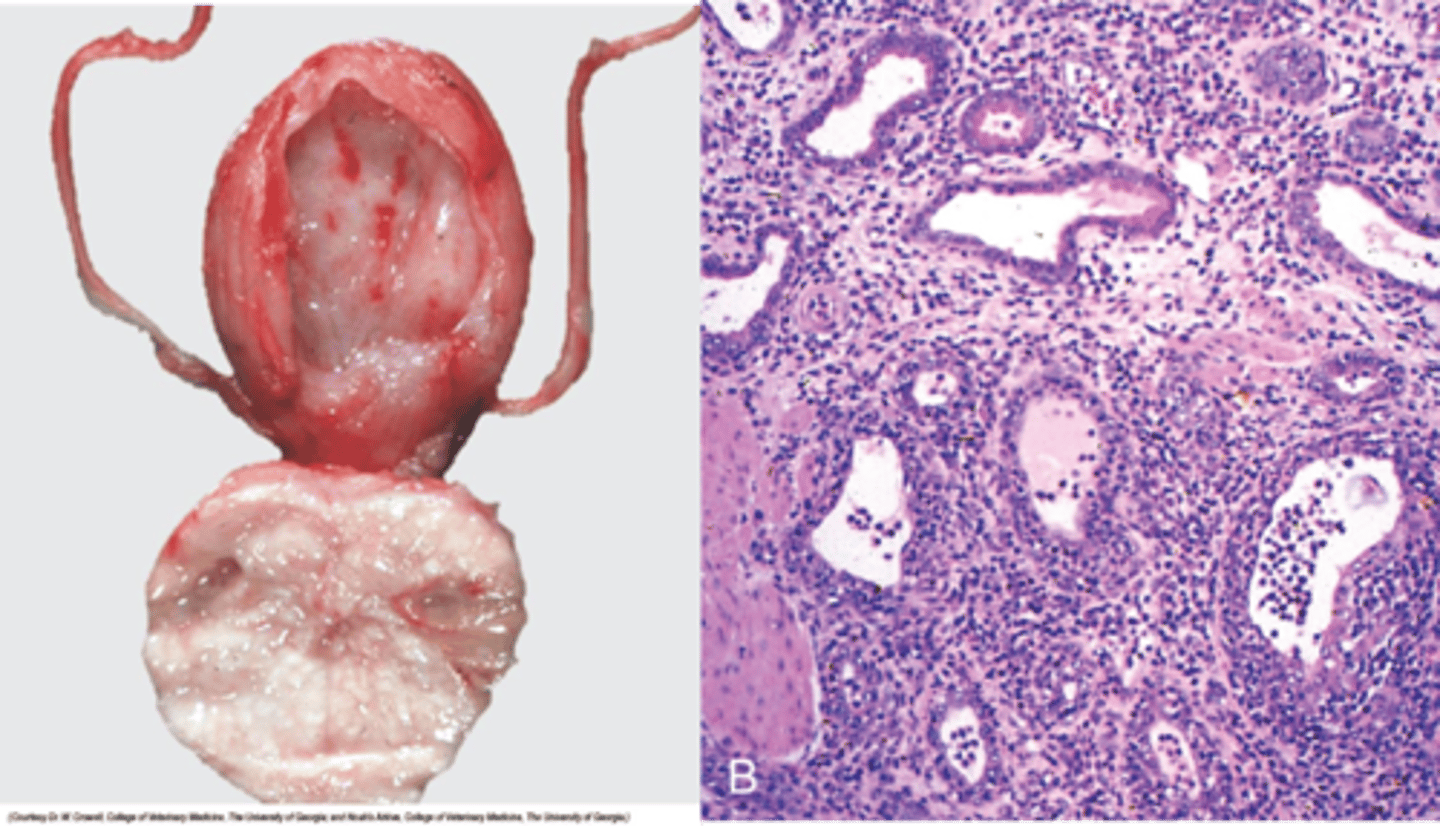
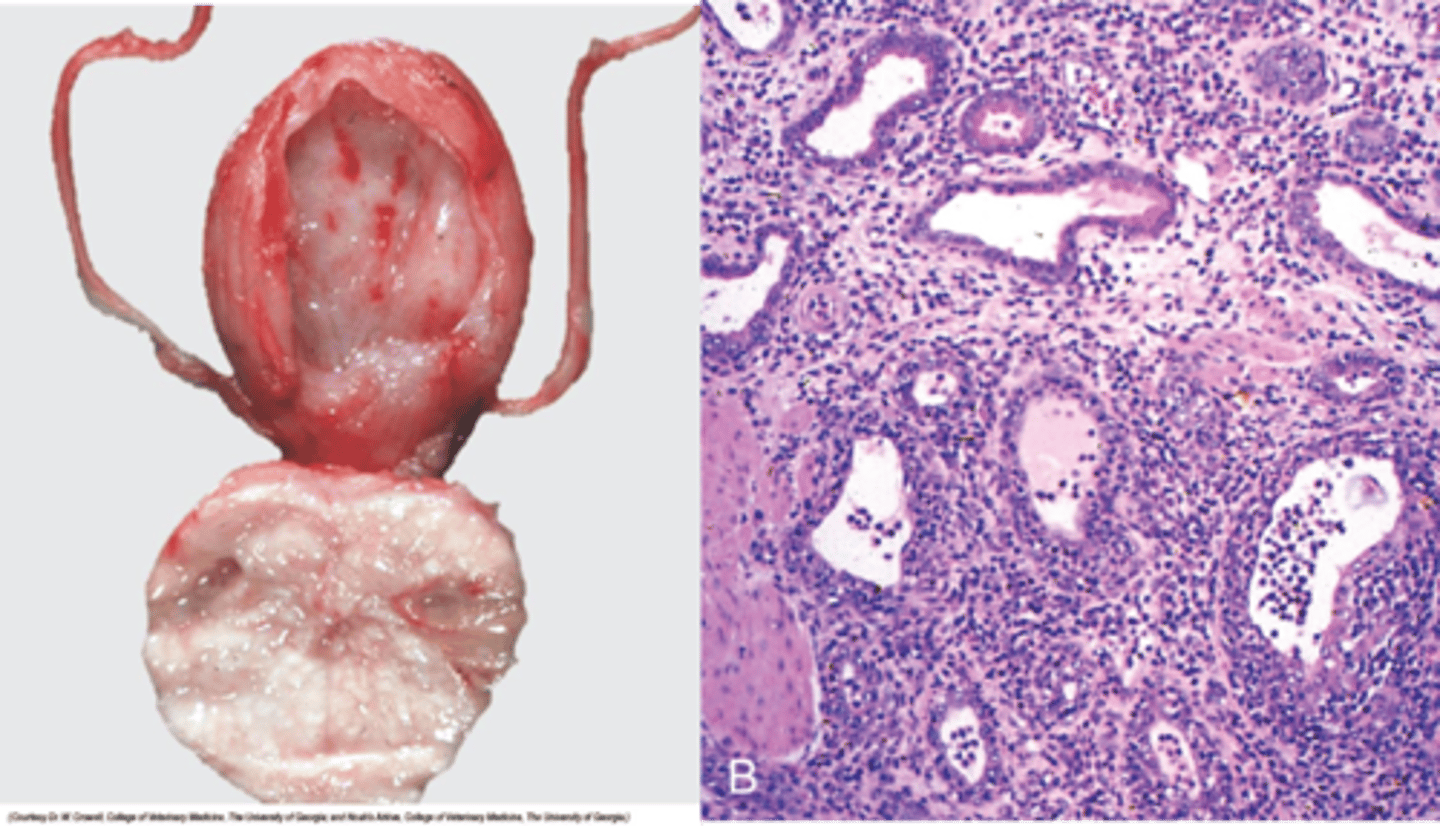
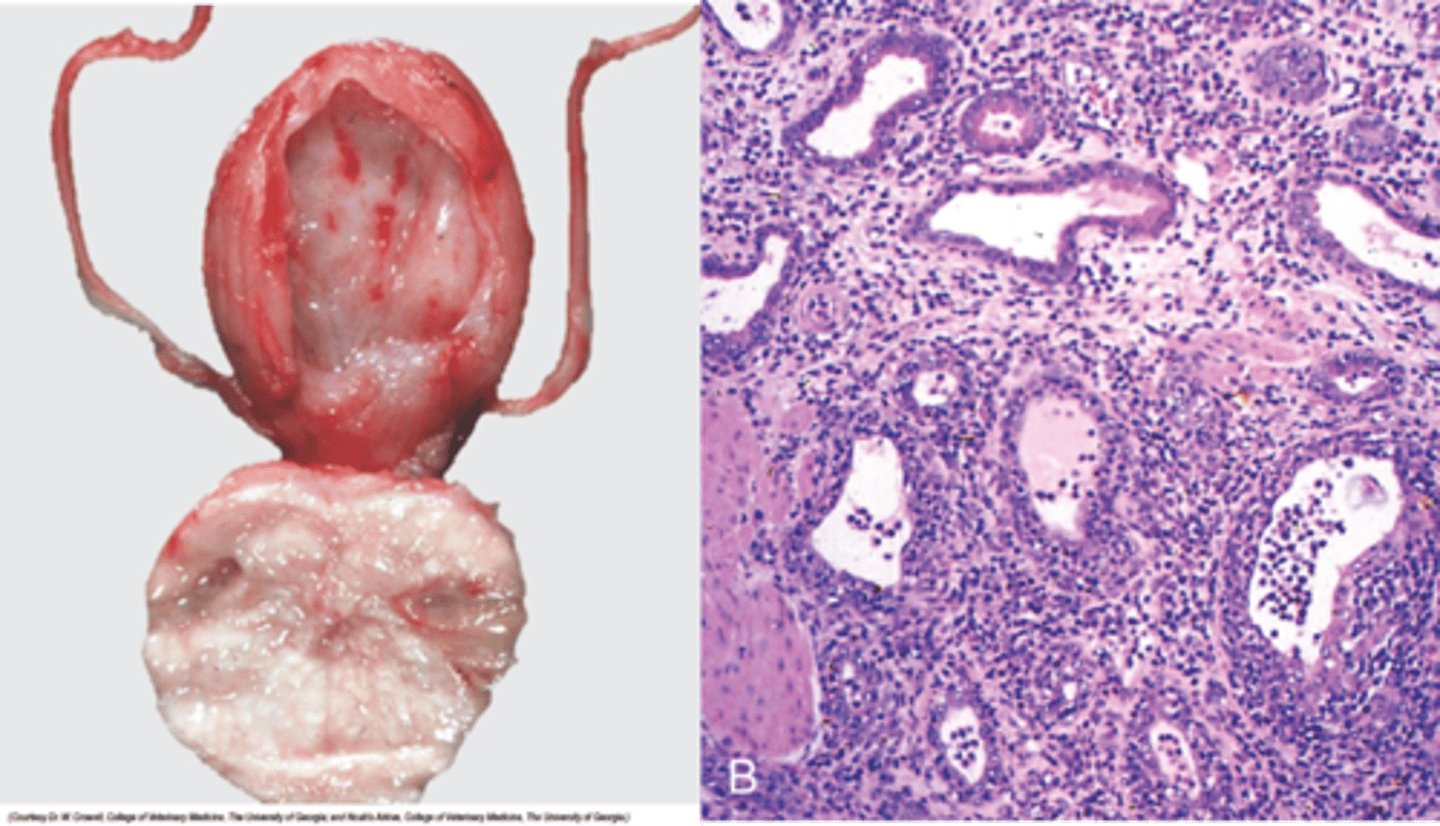
Gross anatomy of Seminoma
Cream bulging mass
increase in size of testes, likely unilateral
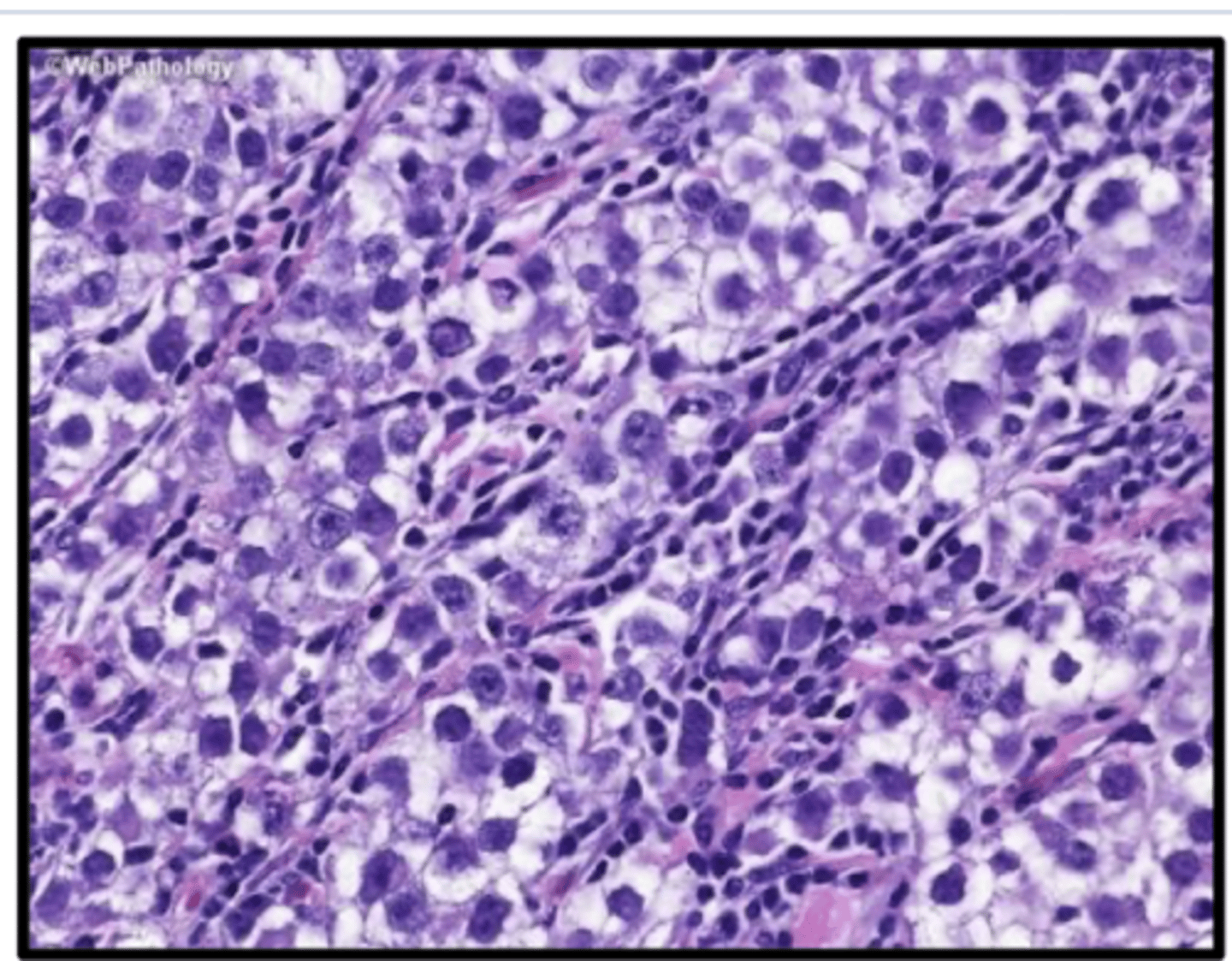
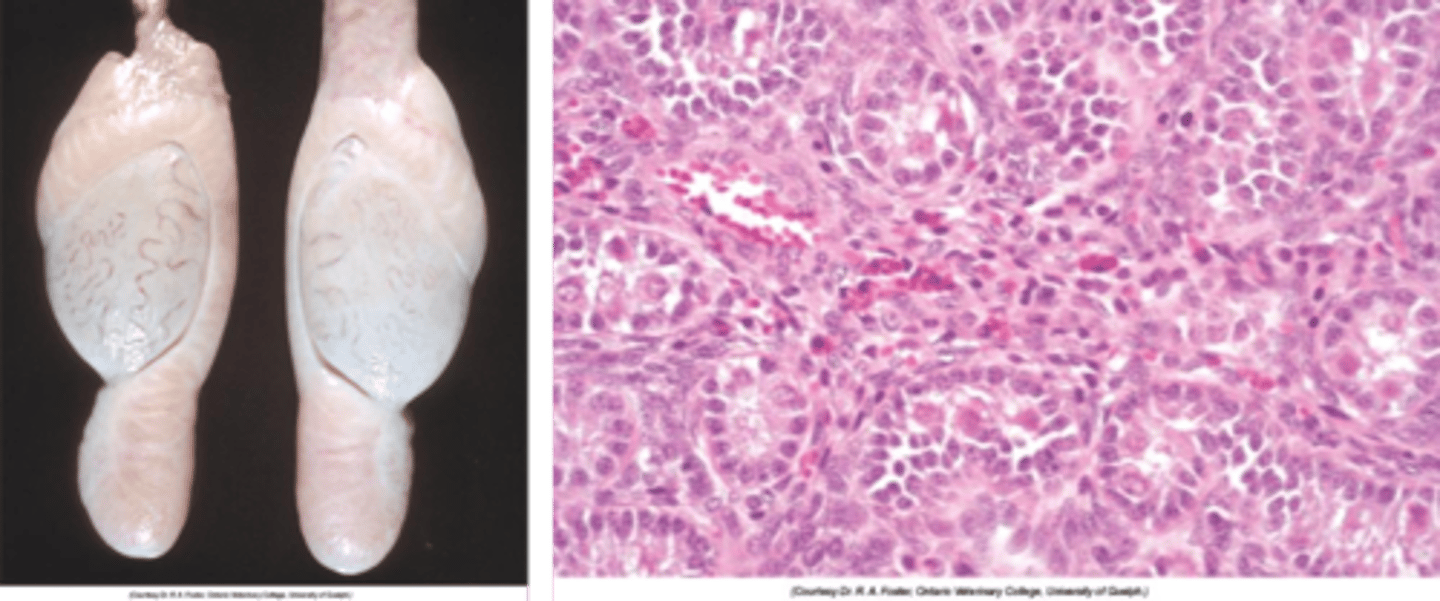
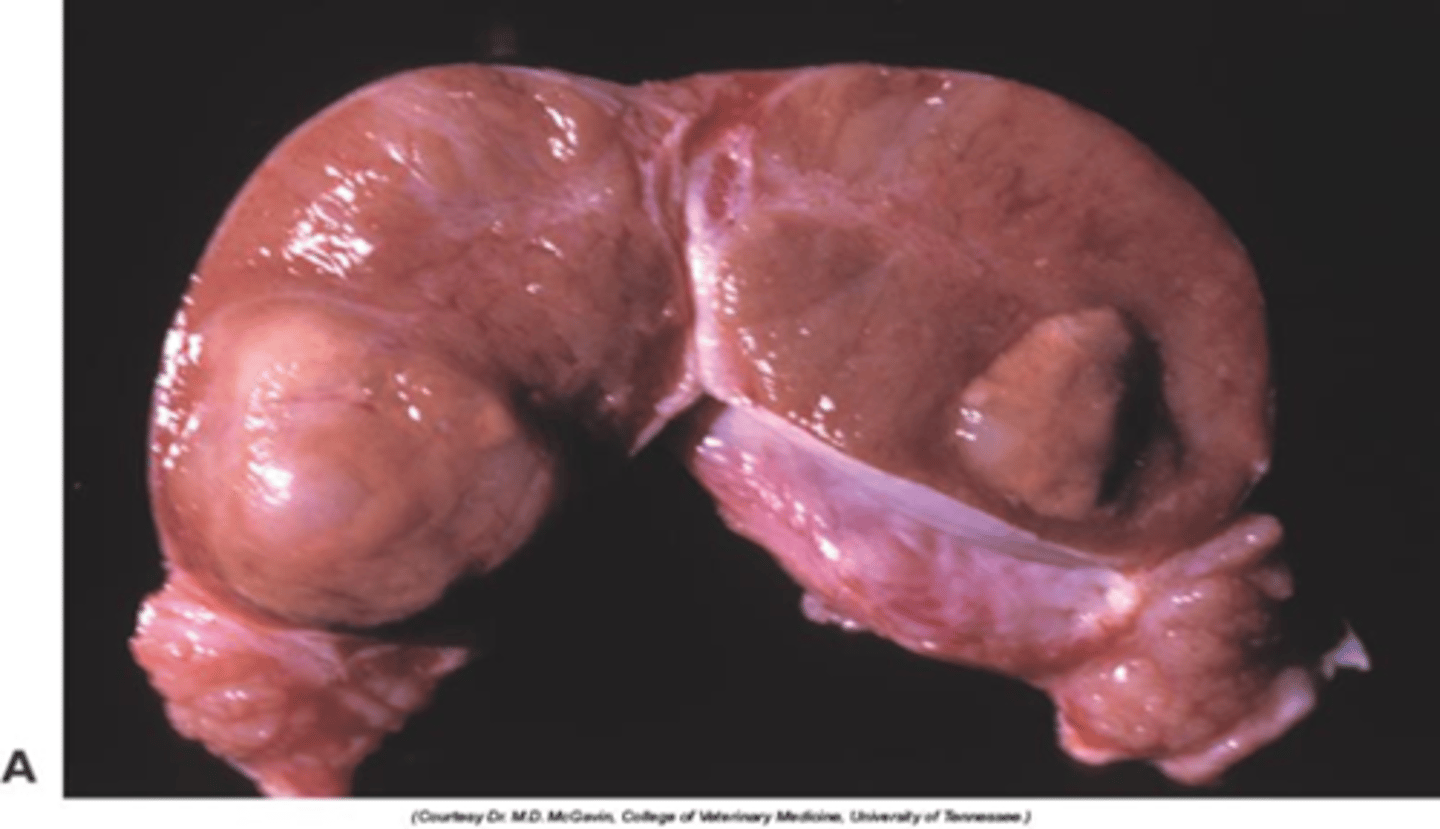
What is the histological appearance of seminoma?
Polyhedral cells, large nucleus, thin rim of cytoplasm, mitoses are frequent
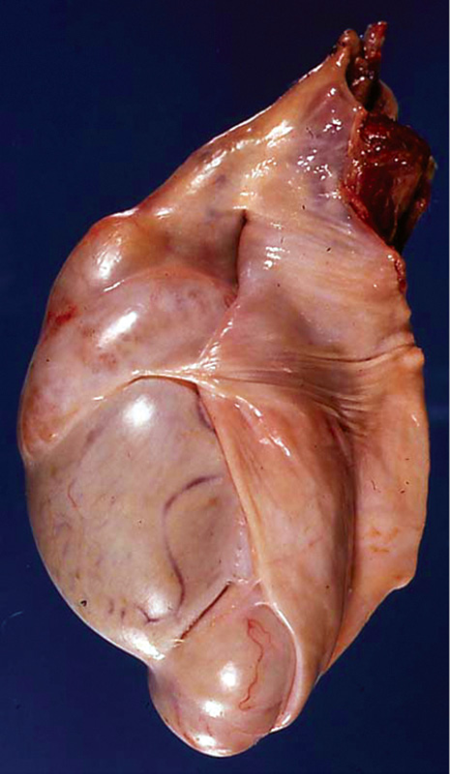
Describe a sertoli cell tumour
3rd most common
50% occur in retained testes
Around 1/3 secrete oestrogen (and/or inhibin) -> cause feminisation
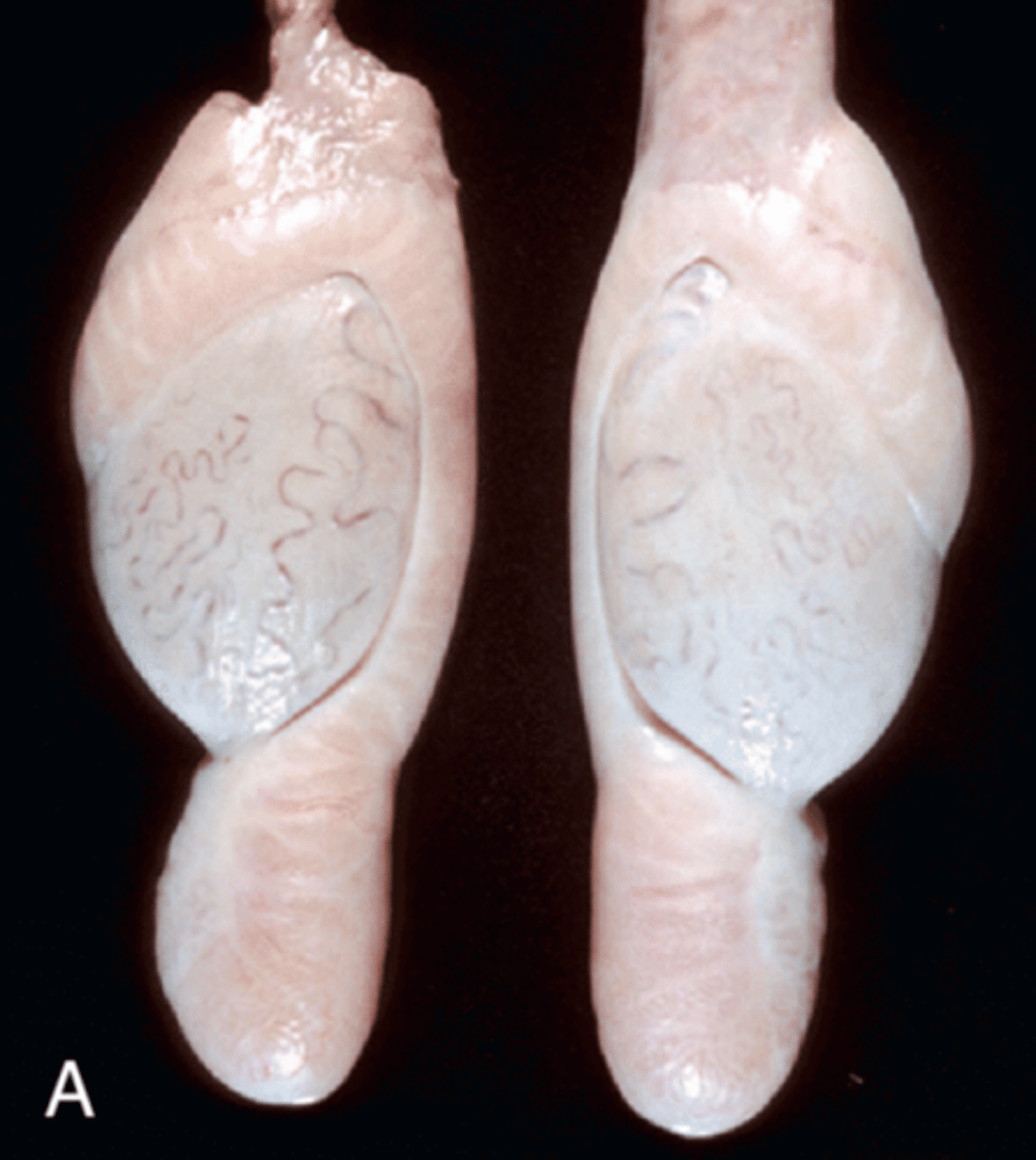
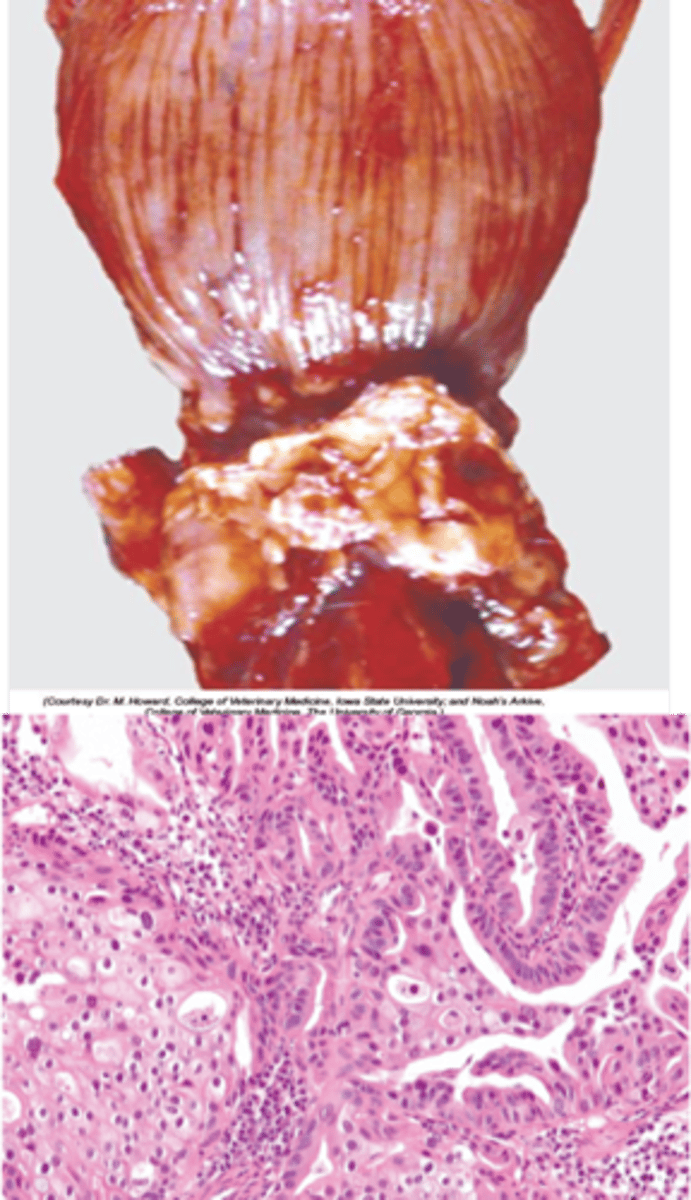
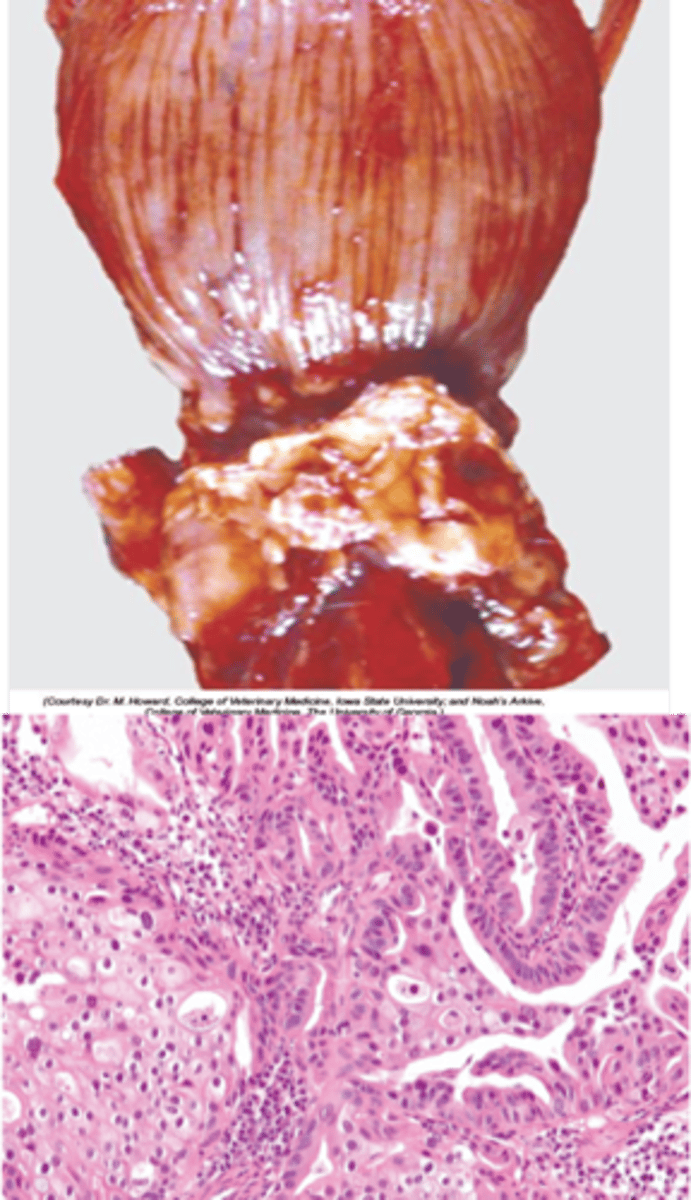
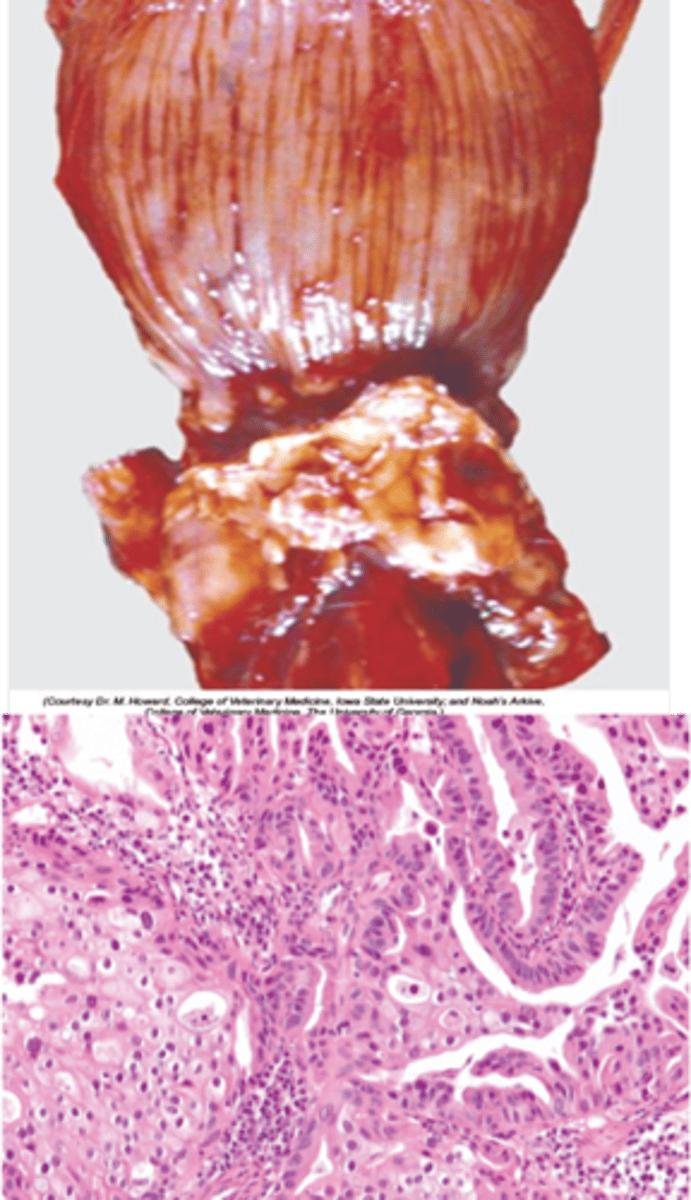
Gross appearance of a Sertoli cell tumour
- Firm white to brown lobulated mass
- Fibrous
- Cysts
- Testicular enlargement
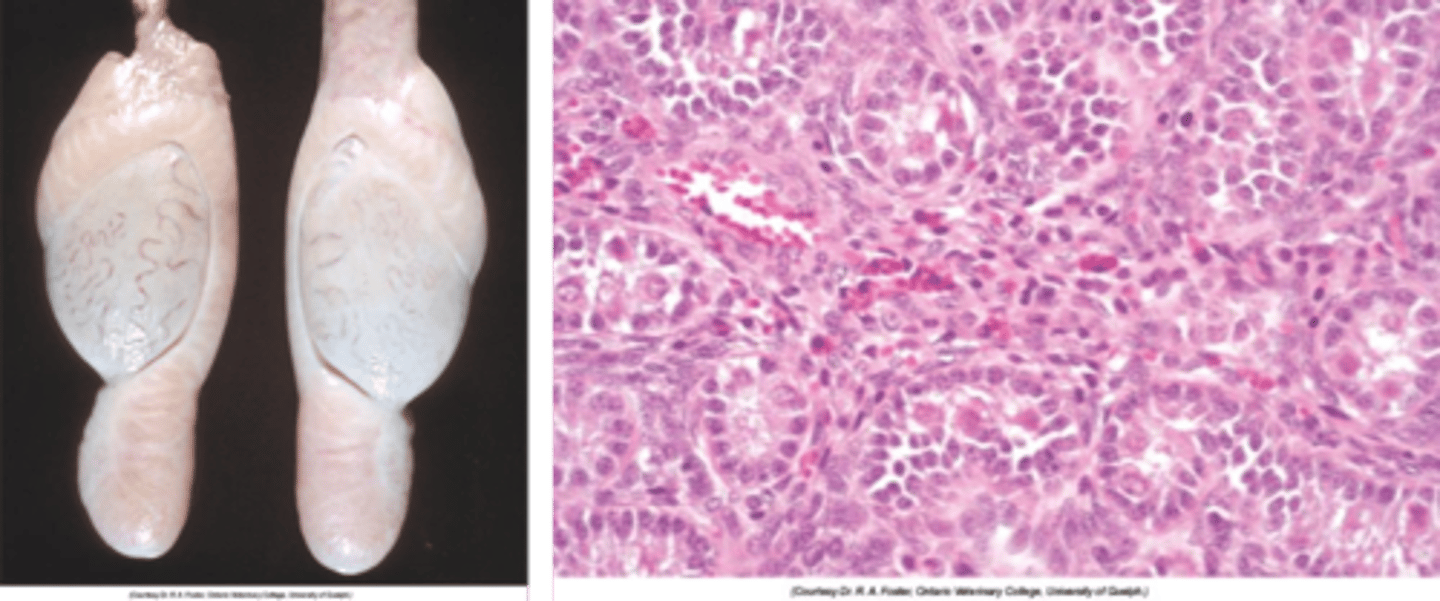
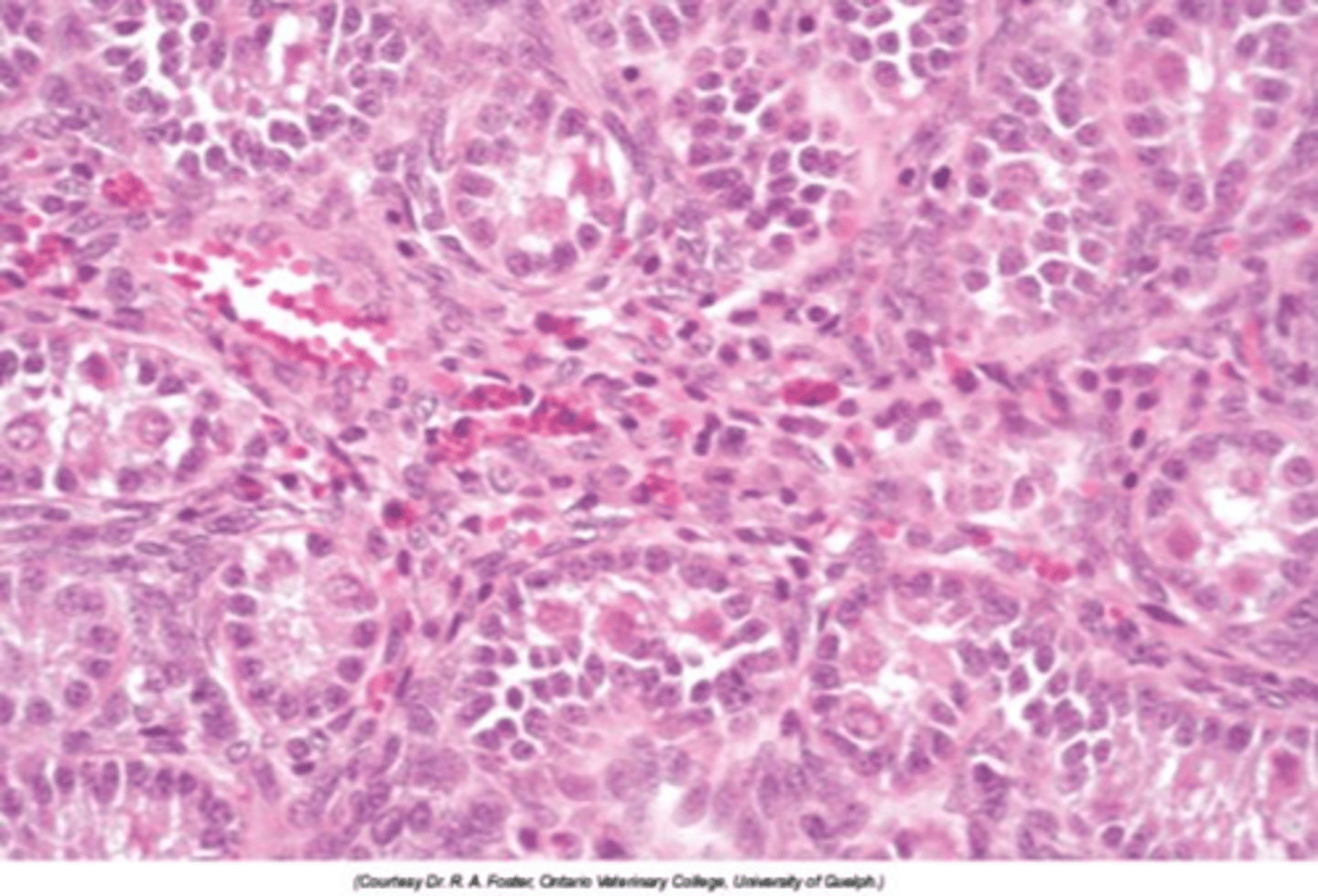
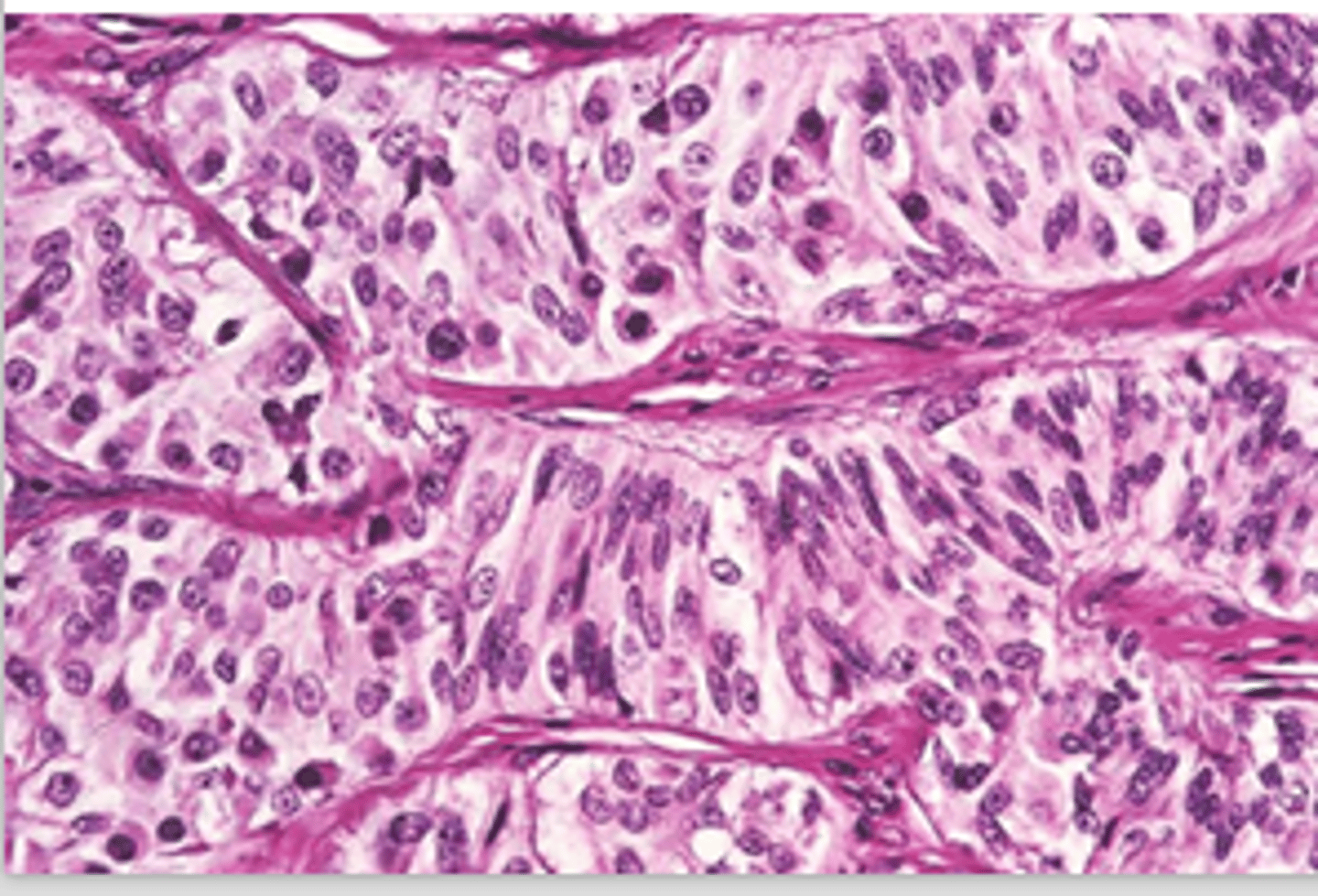
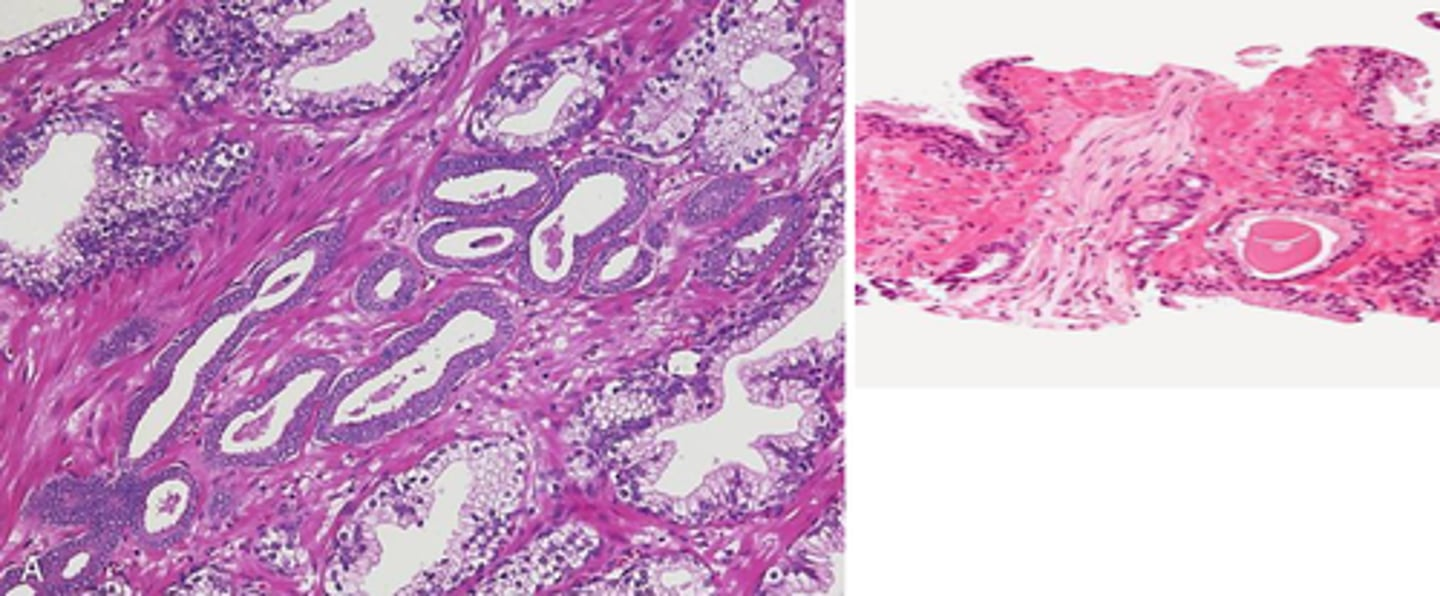
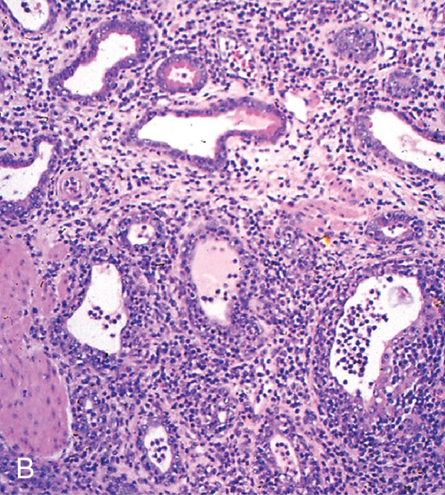
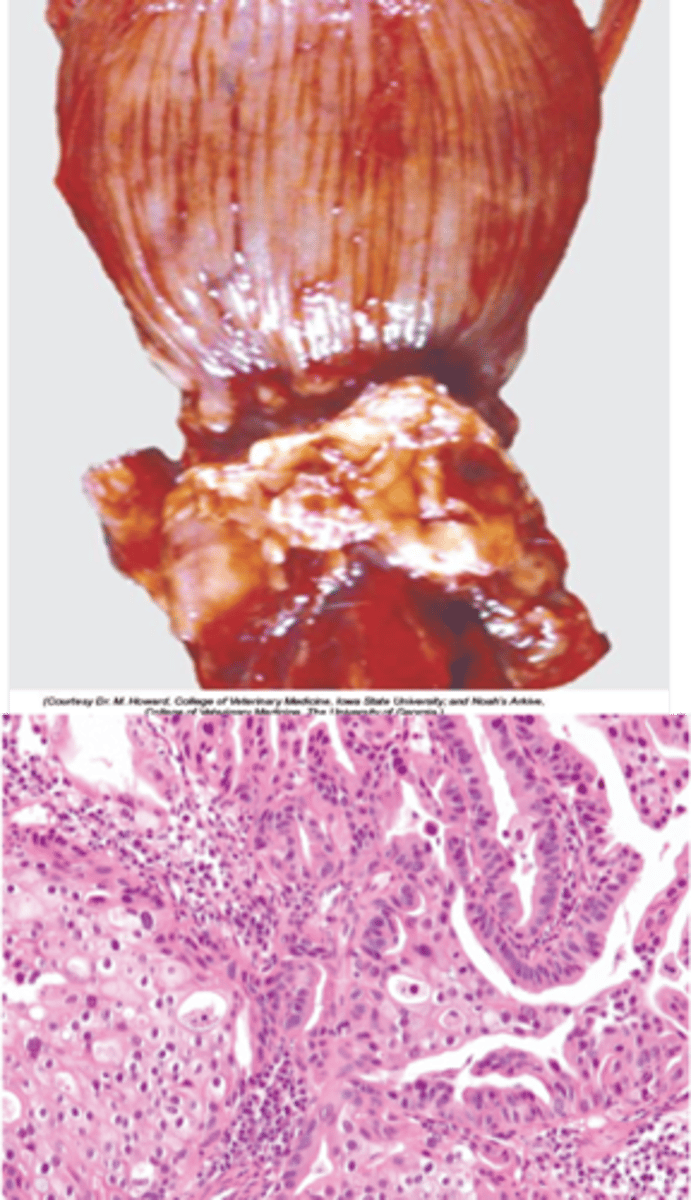
Describe the histological appearance of a Sertoli cell tumour
Sertoli cells multi-layered in tubules or invading interstitial tissue
Abundant fibrous tissue
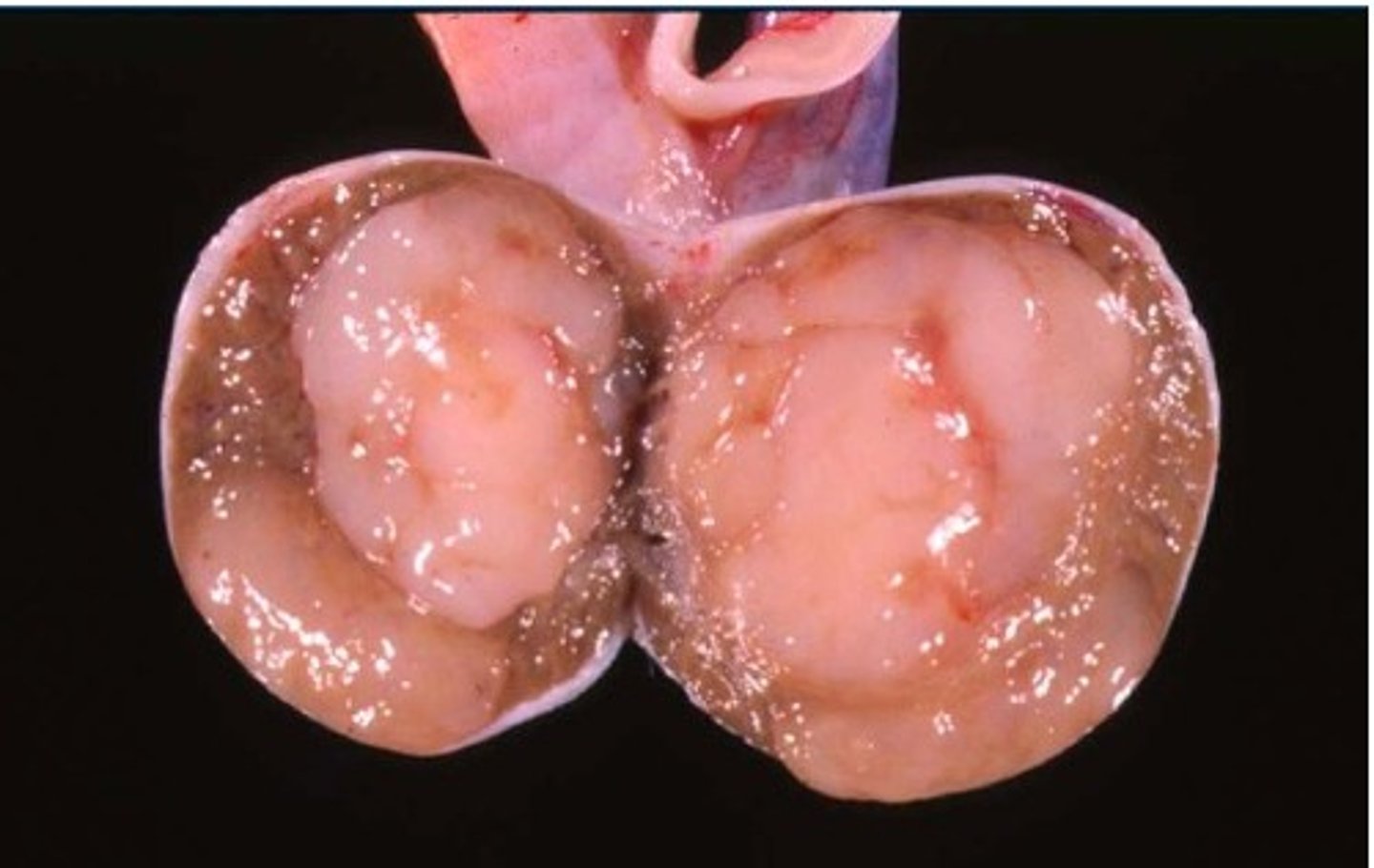
What is the most common testicular neoplasia in dogs, cats and bulls?
Interstitial (Leydig) cell tumour
True or false- All interstitial (Leydig) cell tumours produce hormones?
False- only some produce hormones
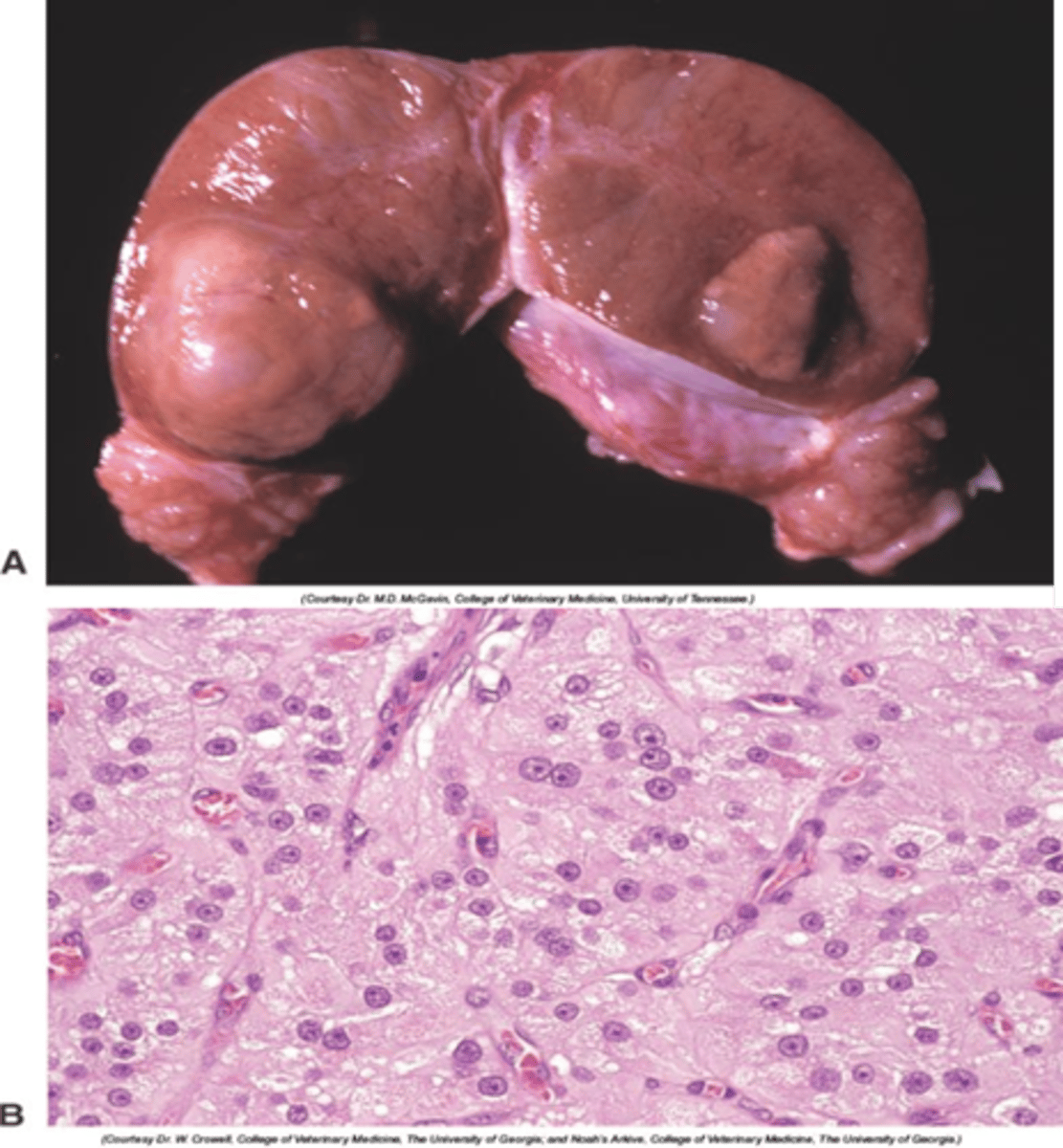
Gross appearance of a interstitial (Leydig) cell tumour
- Single or multiple spherical
- Tan to orange or haemorrhagic (bulging on cut surface)
-No enlargement of testis
Describe the histological appearance of a interstitial (Leydig) cell tumour
Polyhedral cells packed in small groups by fine fibrous stroma
What species is most affected by prostatic disease?
Dogs
Describe the incidence of different prostatic diseases in dogs from most to least common
Hyperplasia > inflammation > neoplasia
Other: Cysts, squamous metaplasia
define Hyperplasia
The enlargement of an organ or tissue because of an abnormal increase in the number of cells in the tissues
Describe prostatic hyperplasia
Enlargement of the prostate due to increased number of prostatic cells:
- Testosterone, converted to DHT in the prostate plays a significant role in the enlargement of the prostate in intact male dogs.
- Oestrogen can contribute to prostatic changes, as it acts synergistically with androgens to potentiate hyperplasia of the epithelium. This occurs especially in neutered male dogs (and also intact older male dogs as testosterone decreases with age). When testosterone levels decrease, and oestrogen can have a more significant impact because of a decrease in the inhibitory effects of testosterone on oestrogen receptors in the prostate.
- Most common in old entire dogs
- Causes constipation and/or urinary stasis

What is the main way to cause atrophy of hyperplastic prostate?
Castration
What is the gross anatomy of Prostatic Hyperplasia?
Bilaterally, symmetrically larger prostate

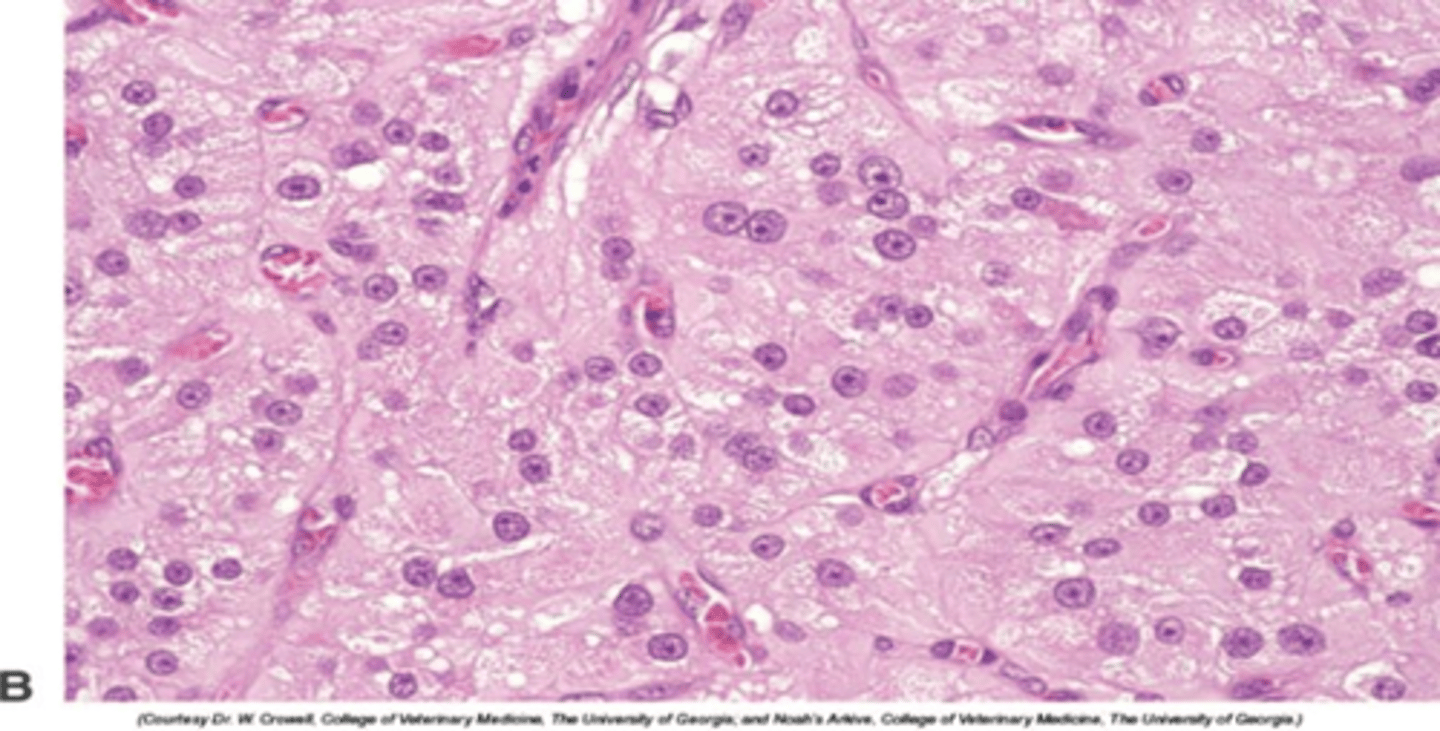
Describe the histological appearance of prostatic hyperplasia
- Hyperplasia and papillary proliferation of the glandular tissue
- Stromal hyperplasia
without infiltration of surrounding tissues
What is commonly found in older dogs, often alongside prostatic hyperplasia?
Prostatitis
What is the main cause of prostatitis?
Ascending bacterial infection
What is the gross anatomy of prostatisis?
Asymmetrical enlargement; may contain abscesses (untreated cases can develop into peritonitis or septicaemia/toxaemia).
- But chronic cases may be subclinical.
What is a common age group for dogs affected by prostatic carcinoma?
Older dogs
describe the histological appearance of prostatitis
Glands dilated
Necrotic neutrophils and sloughed epithelial cells
Does castration prevent or treat prostatic carcinoma?
Neither prevention nor treatment
What is a gross characteristic of prostatic carcinoma?
Asymmetrical mild enlargement

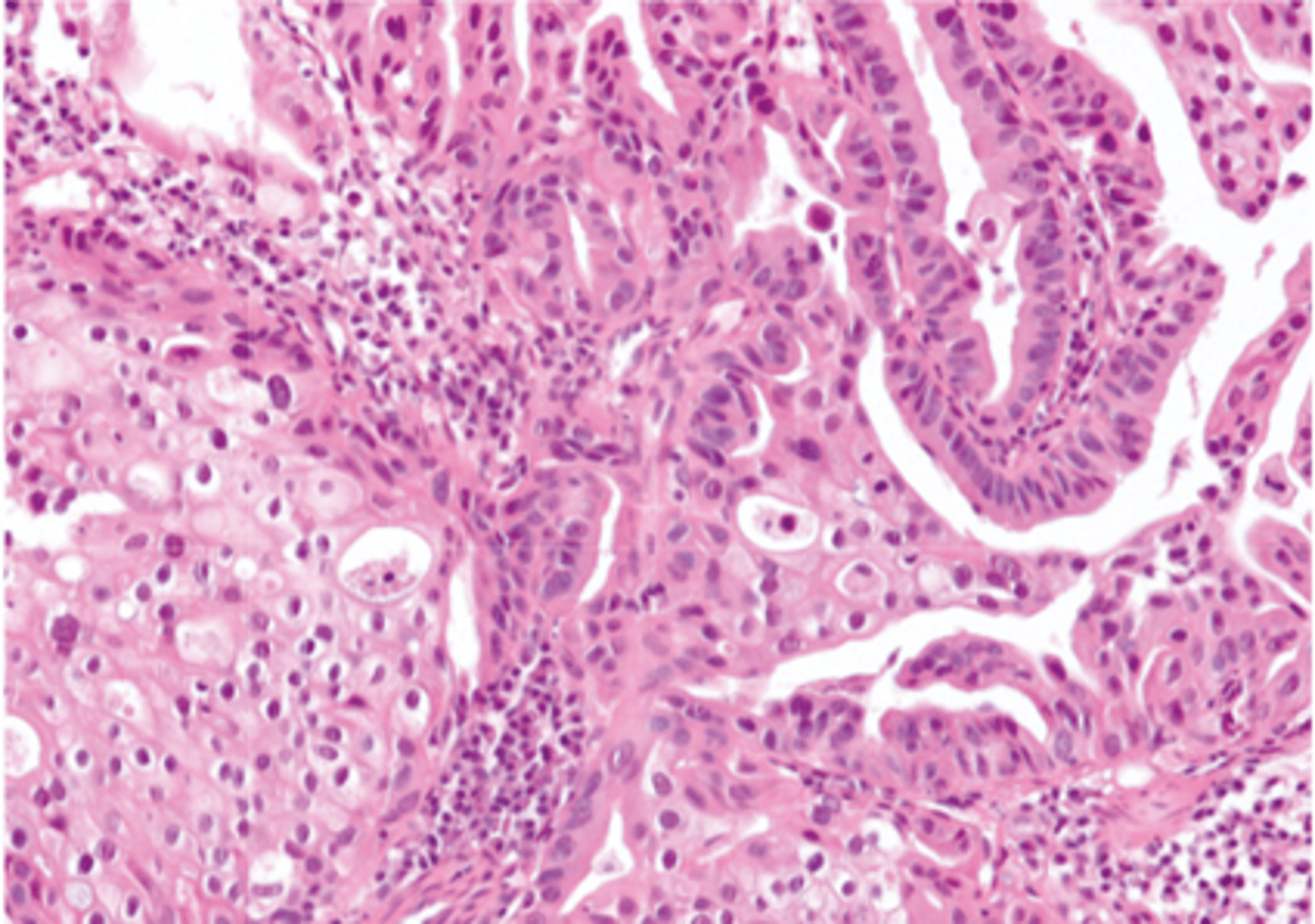
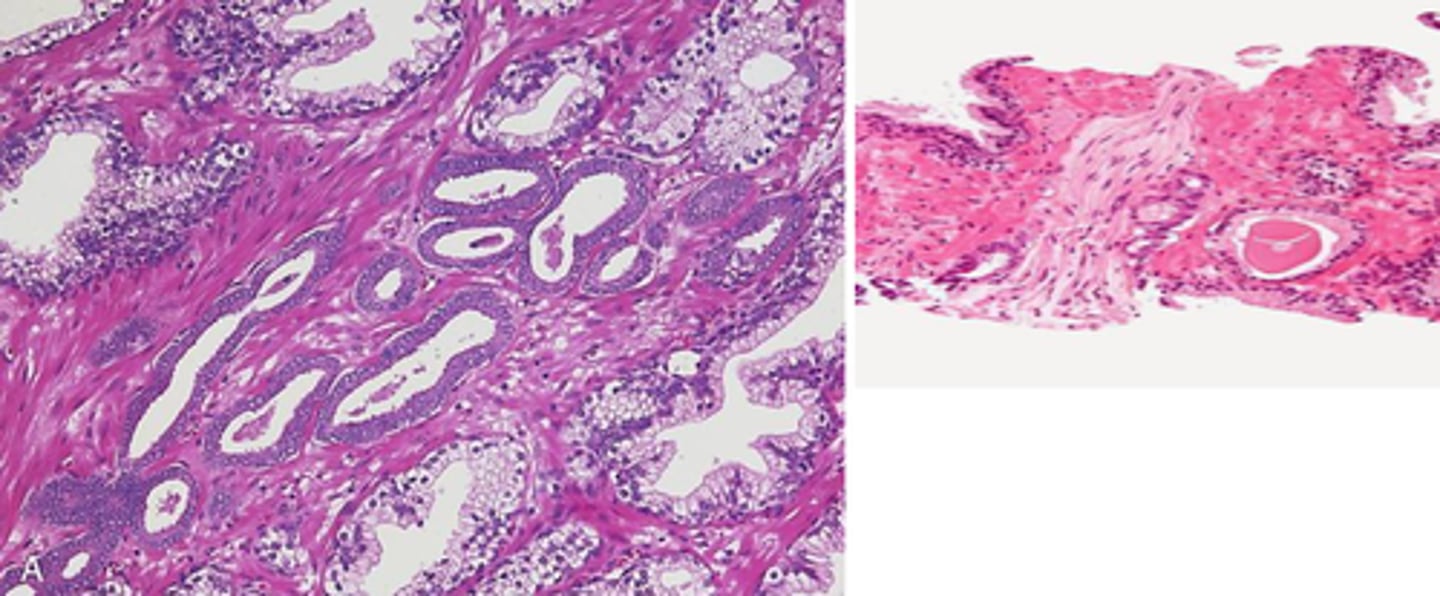
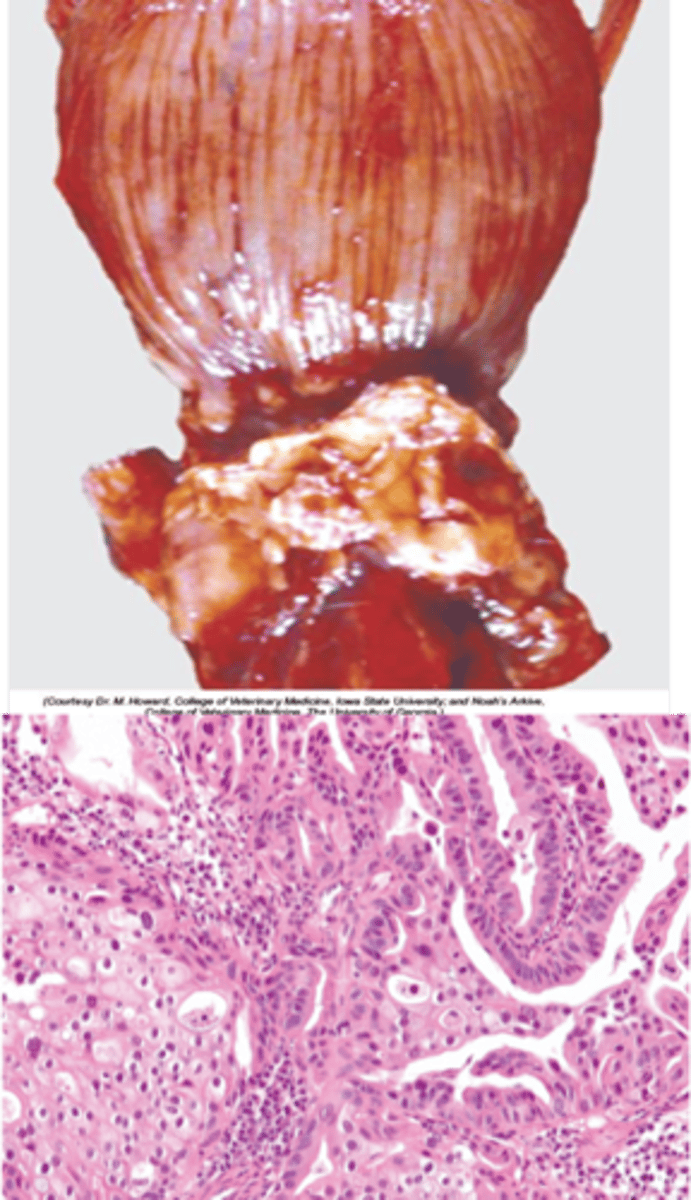
What is observed microscopically in prostatic carcinoma?
Haphazardly arranged glandular cells invading interstitium and marked fibrosis
Potential infiltration of surrounding tissues
Where is metastasis common in prostatic carcinoma?
Lymph node, lung, bone
What is the prognosis for prostatic carcinoma?
Guarded
What are some clinical signs of prostatic carcinoma?
Constipation, urinary stasis, cachexia, and locomotor abnormalities
The cachexia can be considered a paraneoplastic syndrome
What is the common misconception with a prostatic carcinoma?
That castration is prevention or treatment but it isn't
What's the gross anatomy of a prostatic carcinoma?
Asymmetrical mild enlargement