week 5: The Biopsychosocial Model Patient (DONE) -centered care
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
18 Terms
life can be altered by what a patient:
“HAS” – diseases
such a bipolar disorder, and major depressive disorder
“IS” –dimensions -
intelligence and personality traits: openness, conscientiousness, extrovert/introvert, agreeable, worries.
“DOES” – behaviors --- such as excessive use of alcohol or drugs.
“ENCOUNTERS” - life-story --- such as grief due to the death of a loved one, fear after a rape, or demoralization after loss of a job.
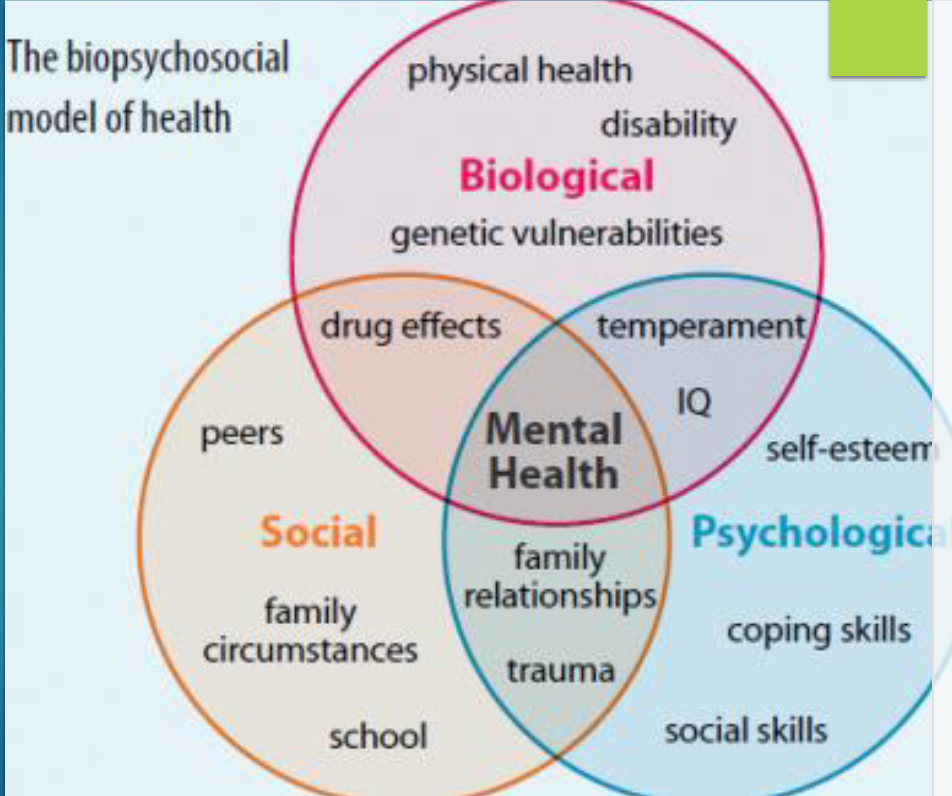
Health and illness can be understood most fully by considering
interactions of biological, psychological, and social factors
The most effective intervention to promote health for the patient will…
address any relevant psychological or social factors in addition to treating the biological illness
What are biological factors?
The pathophysiology of disease, or the disordered physical response to disease.
caused by things such as:
- Viruses
- Bacteria
- Genetic predisposition to illness
- Immunity
What are psychological factors?
Things that are internal to the patient that impact illness and treatment
such as:
Self-Esteem
Emotions, such as stress, fear, or discomfort
Mood disorders (depression, anxiety, bipolar)
Thought disorders (schizophrenia, psychosis)
What are social factors?
Things that are external to the patient.
such as:
Social network and support (or lack thereof)
Insurance status
Employment
Socioeconomic status
Cultural traditions
Religious beliefs
Experiences of discrimination and harassment
Abuse/neglect
Trauma history
substance abuse
Psychosocial Factors
It can be challenging to clearly separate psychological and social factors, so we often think of them together
Psychological (internal to patient) + Social (external to patient) = PSYCHOSOCIAL
Psychosocial considerations for dental care
Impact of medical illness or disability on oral and treatment plan
Need for emotional support related to new diagnosis or treatment plan
Language barriers, including low health literacy
Difficulty with primary medical care access
Transportation barriers
Cultural considerations
Lack of insurance coverage
Concern about affording medications or treatment
Lack of access to basic needs such as food, housing, clothing, etc.
Substance abuse
Mental health, such as dental anxiety or unmanaged depression
Suspicions of abuse or neglect of a child or vulnerable adult
How can Providers address psychosocial Considerations?
Care coordination between providers
Referrals to appropriate community resources and state/federal assistance programs
Self-reflection regarding privilege and assumptions
Preparation to serve a diverse population of patients (cultural competence)
Building communication skills
Awareness of social determinants of health, such as poverty and
discrimination
Commitment to person/patient-centered care
Person/patient-Centered Care
Treating the people accessing health care as “equal partners in planning, developing, and monitoring care.”
“A person who has a tooth attached, as opposed to a tooth that may or may not be attached to a person.
Principles of person-centered care: 1. Respect and cultural
competence
Cultural sensitivity towards patient and family
including, but not limited to, socioeconomic status, race, religion, ethnicity
Considering patient/family needs and preferences to make treatment decisions
Principles of person-centered care: 2. Integration and coordination of care
Care provided by multi-disciplinary teams: families, health care providers, case managers, educators, insurers, community support systems, etc.
Improving collaboration between care teams to improve access to
care: where is care received?
Principles of person-centered care: 3. Communication and information sharing
Open communication between the health care team members and between the team, patient and family to ensure transparency and continuity of care
Enhancing communication skills of providers
Enhancing health literary so patients can understand treatment plans and options
Principles of person-centered care: 4. Quality of care
Providing evidence-based care that is high quality: the best care is not always the most expensive, or the most elaborate!
Receiving feedback from patients and collecting data to improve the delivery of health care
Principles of person-centered care: 5. Whole-Person and comprehensive Care
Attending to the overall health of the person, not just the presenting oral health problem
Emphasizing health promotion to reduce risk and increase quality of life
Common PCC myths
We are practicing PCC if we:
Implement an electronic health record
Have a patient on our committee to redesign the office
Send text reminders to patients
Receive high patient satisfaction scores
What could this look like in dentistry?
Integration of primary and dental care
Mid-level providers to increase access to preventive dental care
Including patients in office decisions such as preferred office hours, design/language of forms, appointment reminder systems
Getting to know patients as individuals, and responding to their particular needs and concerns, aka, the Platinum Rule
Addressing psychosocial considerations for treatment