Sodium Disorders I
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
36 Terms
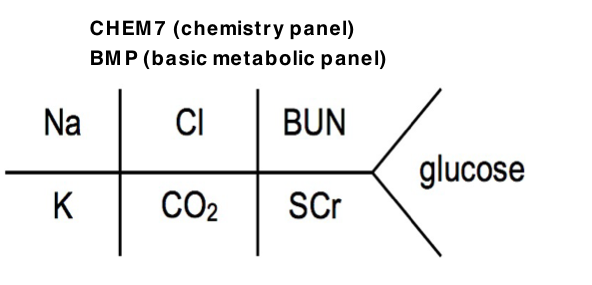
Serum Na (135–145 mEq/L)
Lab Values
Normal range serum Na: 135–145 mEq/L
Hyponatremia = Na <135 mEq/L
<130 mEq/L – clinically significant
Hypernatremia = Na >145 mEq/L
>150 mEq/L – clinically significant
Hyponatremia (<135 mEq/L)
Sodium
Accounts for 90% of osmotic activity in the ECF
Plasma sodium concentration reflects water balance
Most common electrolyte disorder
Common in both inpatient and ambulatory settings
1–6% of hospitalized patients
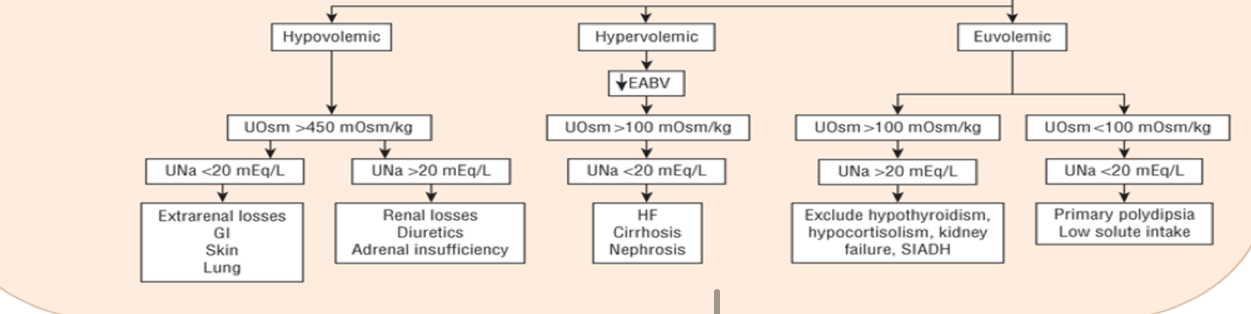
Diagnostic Algorithm for Hyponatremia
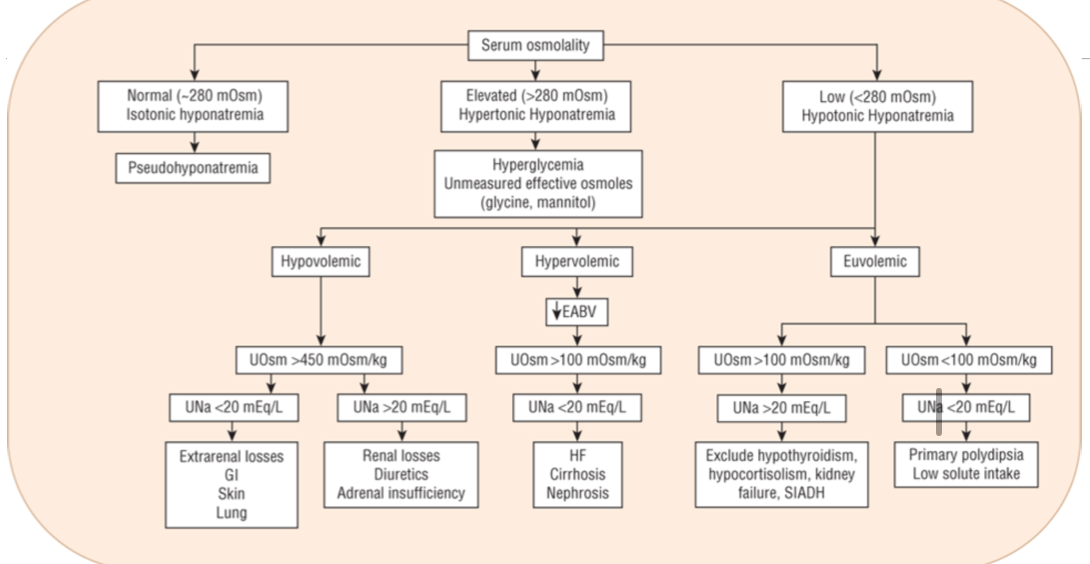
Step 1: Assess Serum Osmolality
Low (<280 mOsm/kg)
→ Hypotonic hyponatremiaNormal (280–285 mOsm/kg)
→ Isotonic hyponatremia (pseudohyponatremia)Elevated (>285 mOsm/kg)
→ Hypertonic hyponatremia
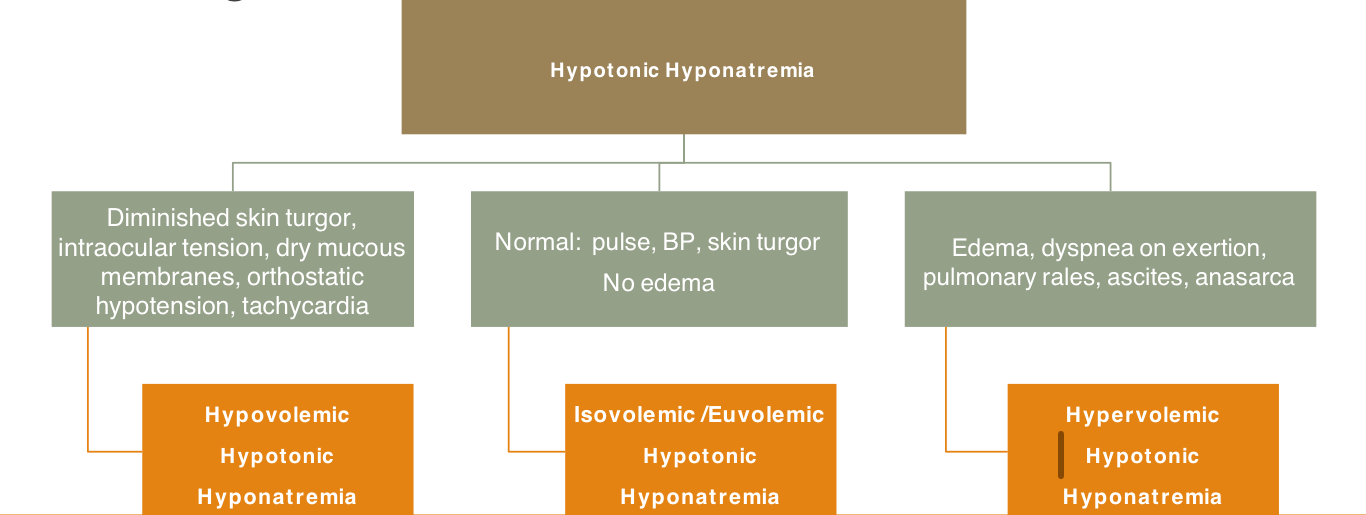
Step 1: Assess Volume Status
After identifying hypotonic hyponatremia, assess clinical volume status:
Hypovolemic Hypotonic Hyponatremia
Diminished skin turgor
Decreased intraocular tension
Dry mucous membranes
Orthostatic hypotension
Tachycardia
Isovolemic (Euvolemic) Hypotonic Hyponatremia
Normal pulse
Normal blood pressure
Normal skin turgor
No edema
Hypervolemic Hypotonic Hyponatremia
Edema
Dyspnea on exertion
Pulmonary rales
Ascites
Anasarca
Clinical Manifestations
Primary system affected: Central nervous system (CNS)
General
Many patients are asymptomatic when Na⁺ > 120 mEq/L
Symptoms are more pronounced with:
Large decreases in sodium
Rapid decreases in sodium
Symptoms
Mild
Nausea
Malaise
Moderate
Disorientation
Headache
Restlessness
Lethargy
Severe
Seizures
Coma
Respiratory arrest
Permanent brain damage
Brainstem herniation
Death
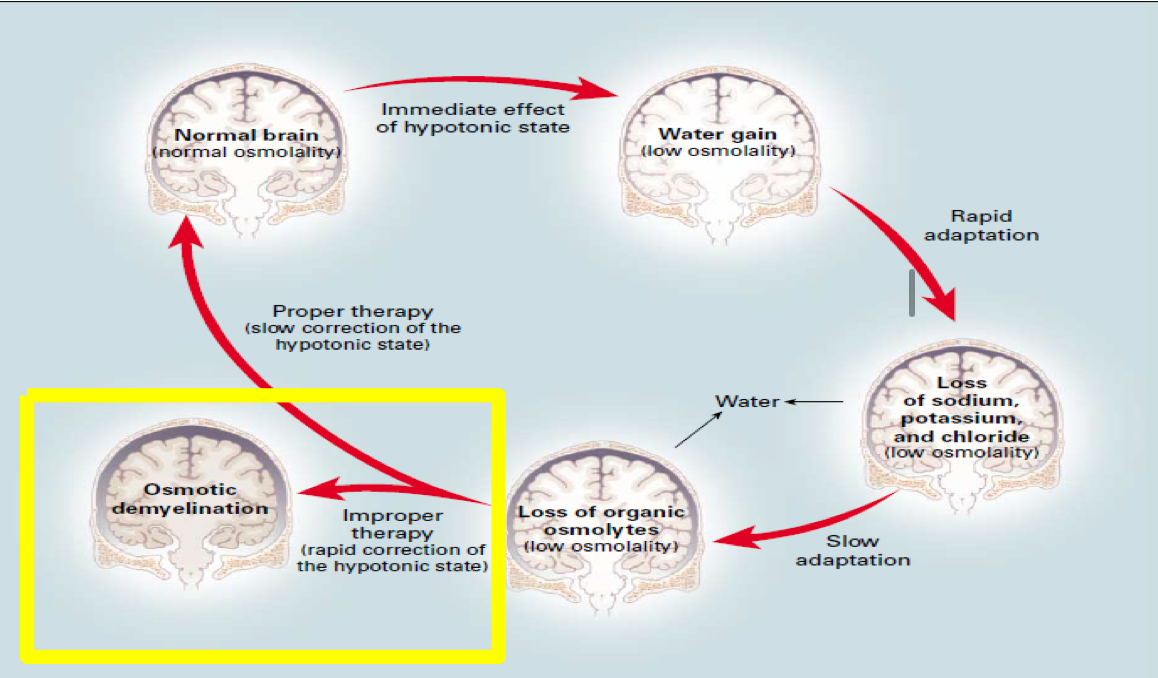
Pathophysiology
Initial effect
Hypotonic state → water moves into brain cells
Results in brain swelling (low osmolality)
Brain adaptation
Rapid adaptation
Loss of sodium, potassium, and chloride
Slow adaptation
Loss of organic osmolytes
Correction Considerations
Proper correction
Slow correction of hypotonic state
Allows restoration of normal brain osmolality
Improper correction
Rapid correction of hypotonic hyponatremia
Leads to osmotic demyelination
Non-Hypotonic Hyponatremia
Isotonic Hyponatremia
Serum osmolality
Normal (~280 mOsm)
Description
Normal plasma osmolality
Low serum sodium
Associated condition
Pseudohyponatremia
Hypertonic Hyponatremia
Serum osmolality
Elevated (>280 mOsm)
Causes
Hyperglycemia
Unmeasured effective osmoles
Glycine
Mannitol
Isotonic Hyponatremia
Plasma findings
Normal plasma osmolality
Low serum sodium
Pseudohyponatremia
Mechanism
Sodium is displaced in the extracellular fluid (ECF)
Causes
Hypertriglyceridemia
Hyperproteinemia
Multiple myeloma
Treatment
None
Correct underlying problem
Hypertonic Hyponatremia
Definition
Increase in plasma osmolality
Decrease in sodium (Na⁺) levels
Mechanism
Caused by a shift of water from the ICF → ECF
Causes
Mannitol administration / infusions
Hyperglycemia
↓ Na⁺ by 1.6 mEq/L for each 100 mg/dL increase in blood glucose over 100 mg/dL
Corrected sodium formula
Corrected Na⁺ = measured Na⁺ + [0.016 × (serum glucose − 100)]
Treatment
Manage underlying cause (e.g., Diabetic Ketoacidosis)
Example:
Hyperglycemia → give insulin
Calculation: Hyperglycemic Hyponatremia
Patient
45-year-old male
70 kg, 5’10”
Type 1 diabetes mellitus (T1DM)
Presents with lethargy, nausea/vomiting, increased thirst
Insulin pump malfunctioned 2 days ago
Labs
Glucose: 528 mg/dL
Na⁺: 124 mEq/L
K⁺: 5.4 mEq/L
Beta-hydroxybutyrate: 4.5
Diagnosis
Diabetic ketoacidosis (DKA)
Corrected Serum Sodium Calculation
124 + [0.016 × (528 − 100)] = 131 mEq/L
Management
Fluid to start
0.9% NaCl
Treatment for underlying problem
Insulin infusion
Hypotonic Hyponatremia
Overview
Most common cause of hyponatremia
“True” hyponatremia
Approach
Differentiate by volume status
Urine Chemistries
Urine Osmolality
< 100 mOsm/kg
Normal water excretion
Intake problem:
Polydipsia
Low solute intake
> 100 mOsm/kg
Impaired water excretion
Rule out:
Hypothyroid
Adrenal insufficiency
Evaluate urine sodium
Urine Sodium
> 20 mEq/L
Renal losses
Diuretics
Adrenal insufficiency
SIADH
< 20 mEq/L
Extrarenal losses:
GI
Skin
Lung
Heart failure
Cirrhosis
Nephrosis
Polydipsia
Low solute intake
“Tea & toast”
“Beer potomania”
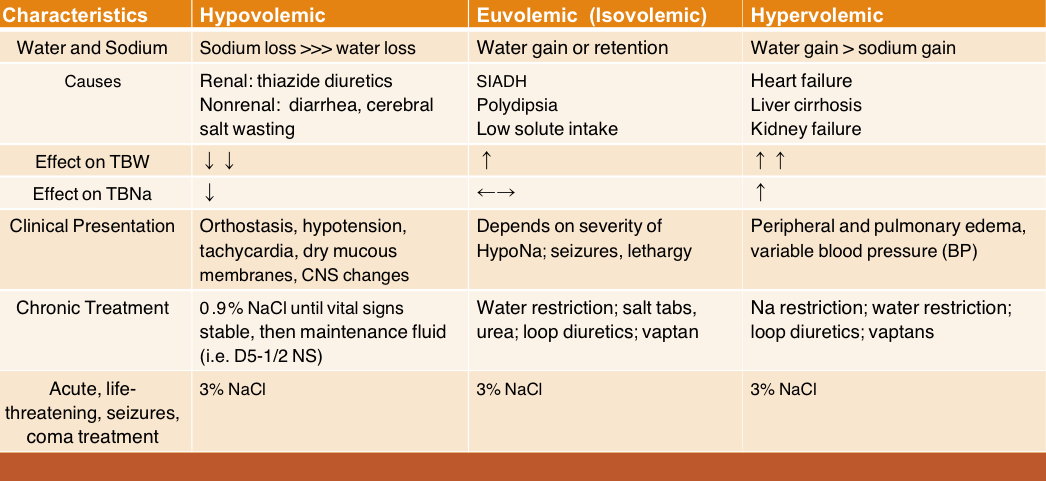
Hypovolemic Hypotonic Hyponatremia
Loss of Water and Sodium
GI salt loss
Diarrhea
Vomiting
NG suction
Fluid sequestration
Bowel obstruction
Peritonitis
Pancreatitis
Skin losses
Excessive sweating (marathon runners)
Burns
Renal losses
Renal disease
Mineralocorticoid deficiency
Cerebral salt wasting syndrome
Diuretics
Characteristics
Water and Sodium
Sodium loss >>> water loss
Causes
Renal: thiazide diuretics
Nonrenal: diarrhea, vomiting
Effect on Total Body Water (TBW)
↓ ↓
Effect on Total Body Sodium (TBNa)
↓
Laboratory Findings
Renal: urine osmolality high, urine sodium high
Nonrenal: urine osmolality high, urine sodium low
Clinical Presentation
Orthostasis
Hypotension
Tachycardia
Dry mucous membranes
CNS changes
Chronic Treatment
0.9% NaCl until vital signs stable
Then maintenance fluid (e.g., D5–½
Diuretic-Induced Hypovolemic Hypotonic Hyponatremia
Overview
Very common
Most cases of severe hyponatremia are due to a thiazide-type diuretic
Risk Factors
Elderly
Low body mass
Low potassium
Thiazide Mechanism
Interferes with sodium reabsorption in the distal convoluted tubule (DCT)
Blocks Na⁺ reabsorption at the Na⁺/Cl⁻ cotransporter in the DCT
Produces volume depletion → stimulates ADH release
Enhanced water reabsorption
Medullary concentration gradient unaffected (unlike loop diuretics)
Hypovolemic Hypotonic Hyponatremia – Treatment
Goals
Reverse hypotonicity without causing osmotic demyelination
Assess Acuity and Symptoms
Acute: < 48 hours
Chronic: > 48 hours
Chronic cases have higher risk of osmotic demyelination
Symptomatic?
Severe or moderate symptoms
Treatment (Chronic Cases)
0.9% NaCl
Correct at a maximum rate of 10–12 mEq/L/day
Slower rate for more severe cases
Monitor sodium every 4 hours
Treat Underlying Cause
Permanently discontinue thiazide diuretics
Treat vomiting, diarrhea, etc.
Hypovolemic Hypotonic Hyponatremia – Acute or Life-Threatening
Indications
Seizures or coma
Treatment
3% NaCl
Risk of cerebral edema or brain herniation outweighs risk of correcting sodium too rapidly
Monitor Na every 2 hours
Severe Symptoms (Seizures or Coma)
Hypertonic saline (3% NaCl) bolus 100 mL over 10 minutes
May repeat up to 3 times as needed
Moderate Symptoms (Confusion or Lethargy)
Hypertonic saline (3% NaCl) continuous infusion
0.5–2 mL/kg/hr
Euvolemic Hypotonic Hyponatremia
Overview
Water retention
Causes
Primary polydipsia
“Tea & toast” or “beer potomania”
Hypothyroidism
Hypocortisolism
SIADH
Characteristics
Water and Sodium
Water gain or retention
Causes
SIADH
Polydipsia
Effect on Total Body Water (TBW)
↑ ↑ ↑
Effect on Total Body Sodium (TBNa)
↔
Laboratory Findings
SIADH: urine osmolality high, urine sodium high
Polydipsia / low solute intake: urine osmolality low, urine sodium low
Clinical Presentation
Depends on severity of hyponatremia
Seizures
Lethargy
Chronic Treatment
Water restriction
Salt tablets
Urea
Loop diuretics
Vaptans
Euvolemic Hypotonic Hyponatremia
SIADH – Syndrome of Inappropriate Antidiuretic Hormone Secretion
Most common cause
Elevated levels of ADH that are inappropriate based on osmotic and volume stimuli
Induces reabsorption of water from the collecting duct, which further increases hyponatremia
Leads to a reduction in aldosterone secretion
Induces urinary sodium excretion (high urine Na)
Component of increased water intake also involved
SIAD (SIADH): Drug-Induced Causes — MOA
Mechanisms
Stimulate ADH release (Central)
Serotonin may stimulate ADH release
5HT₂C, 5HT₄, & 5HT₇ implicated in DI-SIADH
Antidepressants (SSRIs), antipsychotics, cyclophosphamide, vinca alkaloids, carbamazepine, & MDMA
Potentiate the action of ADH (Renal)
Chlorpropamide, carbamazepine, oxcarbazepine, & cyclophosphamide
SIAD (SIADH): Drug-Induced Causes — Drug classes with strongest association
Antidepressants
SSRIs (Celexa, Prozac, Zoloft, Lexapro, Paxil)
Tricyclics
Venlafaxine
Chemotherapy
Vincristine/Vinblastine, Cisplatin, & Cyclophosphamide
Anticonvulsants
Carbamazepine & Oxcarbazepine
Euvolemic Hypotonic Hyponatremia – Treatment
⭐ Fluid Restriction
Less than 1 liter per day
Life-threatening SIADH (coma/seizures) or Acute (<48 hrs)
3% saline plus IV furosemide
Treat until any one of the following occur:
Asymptomatic
Serum Na level >120 is achieved
Monitor serum Na levels every 2 hours
Euvolemic Hypotonic Hyponatremia – Treatment
Chronic SIADH with mild to moderate symptoms
Stop causative agent or treat underlying cause
Fluid restriction: less than 1 liter per day
Patients who do not respond to fluid restriction
(about 1 to 2 weeks) may need chronic medication treatment
Correct at a maximum rate of 10–12 mEq/L/day
Monitor sodium every 4 hours
Medications
Urea
Salt tablets
Demeclocycline
May take 1 to 2 weeks for peak effects
Vasopressin receptor antagonists (vaptans)
Conivaptan – IV formulation
Risk of osmotic demyelination
Tolvaptan – PO formulation
Hepatoxic, excessive thirst, $$
Don’t use more than 30 days
Hypervolemic Hypotonic Hyponatremia
Increase in water and sodium
Mechanism
Angiotensin II
Aldosterone
Norepinephrine
ADH
Characteristics – Hypervolemic
Water and Sodium
Water gain >>> sodium gain
Causes
Heart failure
Liver cirrhosis
Kidney failure
Effect on TBW
↑ ↑ ↑
Effect on TBNa
↑ ↑
Laboratory
UOsm high
UNa high
Clinical Presentation
Peripheral and pulmonary edema
Variable blood pressure (BP)
Chronic Treatment
Na restriction
Water restriction
Loop diuretics
Vaptans
Hypervolemic Hypotonic Hyponatremia: Treatment
Treatment in Heart Failure
Fluid restriction
Sodium restriction
Less than 2 grams/day
Loop diuretics
Treat heart failure – Cardiology section of Therapeutics I
Treatment in Cirrhosis
Fluid restriction
Sodium restriction
Less than 2 grams/day
Diuretics (loop + mineralocorticoid receptor antagonist)
Treat ascites – GI section of Therapeutics I
Summary of Hypotonic Hyponatremia
A 21-year-old male with type 1 diabetes mellitus presents to the emergency department with:
Nausea
Vomiting
Confusion
He ran out of insulin 3 days ago.
Laboratory Results
Na: 122
K: 3.9
Cl: 101
CO₂: 13
BUN: 32
Cr: 0.9
Glucose: 600
Ketones: 4.7
Question
Which of the following most likely describes this type of hyponatremia?
Answer choices:
A. Isotonic hyponatremia
B. Hypertonic hyponatremia
C. Hypotonic hyponatremia
B. Hypertonic hyponatremia
A 57-year-old female with:
Stage IV breast cancer
Depression
Trigeminal neuralgia
presents to the emergency department after a new-onset witnessed seizure at home.
Recent Chemotherapy
Vincristine
Cyclophosphamide
Home Medications
Zoloft 200 mg daily
Carbamazepine 900 mg TID
Laboratory Results
Na: 108
K: 3.7
Cl: 87
CO₂: 20
BUN: 65
SCr: 2.3
Glucose: 105
Urine osmolality (UOsm): 248
Urine sodium (UNa): 62
Question
What is the most likely underlying cause(s) of hyponatremia?
(Select all that apply.)
Answer choices:
A. Vincristine
B. Cyclophosphamide
C. Zoloft
D. Carbamazepine
All of the above.
A 57-year-old female with:
Stage IV breast cancer
Depression
Trigeminal neuralgia
presents to the emergency department after a new-onset witnessed seizure at home.
Recent Chemotherapy
Vincristine
Cyclophosphamide
Home Medications
Zoloft 200 mg daily
Carbamazepine 900 mg TID
Laboratory Results
Na: 108
K: 3.7
Cl: 87
CO₂: 20
BUN: 65
SCr: 2.3
Glucose: 105
Urine osmolality (UOsm): 248
Urine sodium (UNa): 62
Question
Interpret the urine chemistries.
A. UOSm is high. UNa is high.
B. UOSm is high. UNa is low.
C. UOSm is low. UNa is high.
D. UOSm is low. UNa is low.
A. UOSm is high. UNa is high.
A 57-year-old female with:
Stage IV breast cancer
Depression
Trigeminal neuralgia
presents to the emergency department after a new-onset witnessed seizure at home.
Recent Chemotherapy
Vincristine
Cyclophosphamide
Home Medications
Zoloft 200 mg daily
Carbamazepine 900 mg TID
Laboratory Results
Na: 108
K: 3.7
Cl: 87
CO₂: 20
BUN: 65
SCr: 2.3
Glucose: 105
Urine osmolality (UOsm): 248
Urine sodium (UNa): 62
Question
After holding home medications, what is the first-line treatment option, and what frequency of laboratory monitoring should be ordered?
Answer choices:
A. Give 0.45% NaCl, monitor every 4–6 hours
B. Fluid restriction, give 3% NaCl, monitor every 2–4 hours
C. Give 0.9% NaCl, monitor once daily
D. Fluid restriction, give tolvaptan, monitor every 8–12 hours
B. Fluid restriction, give 3% NaCl, monitor every 2–4 hours
An 85-year-old female with hypertension presents to the emergency department with:
Nausea and vomiting
Orthostatic hypotension
Confusion for 3 days
Family reports she may have caught a “stomach bug.”
She has not been able to keep liquids down.
She continued taking hydrochlorothiazide (HCTZ) 25 mg daily as prescribed.
Her mucous membranes are dry.
Laboratory Results
Na: 119
K: 3.7
Cl: 96
CO₂: 24
BUN: 65
SCr: 2.3
Glucose: 87
Urine osmolality (UOsm): 532
Urine sodium (UNa): 46
Question
What is the most likely type of hyponatremia, and what is the most likely underlying cause?
Answer choices:
A. Euvolemic; SIADH
B. Hypervolemic; stomach bug
C. Hypovolemic; HCTZ
D. SIADH; HCTZ
C. Hypovolemic; HCTZ
An 85-year-old female with hypertension presents to the emergency department with:
Nausea and vomiting
Orthostatic hypotension
Confusion for 3 days
Family reports she may have caught a “stomach bug.”
She has not been able to keep liquids down.
She continued taking hydrochlorothiazide (HCTZ) 25 mg daily as prescribed.
Her mucous membranes are dry.
Laboratory Results
Na: 119
K: 3.7
Cl: 96
CO₂: 24
BUN: 65
SCr: 2.3
Glucose: 87
Urine osmolality (UOsm): 532
Urine sodium (UNa): 46
Question
How should the urine chemistries be interpreted?
Answer choices:
A. UOsm is high; UNa is high
B. UOsm is high; UNa is low
C. UOsm is low; UNa is high
D. UOsm is low; UNa is low
A. UOsm is high; UNa is high
An 85-year-old female with hypertension presents to the emergency department with:
Nausea and vomiting
Orthostatic hypotension
Confusion for 3 days
Family reports she may have caught a “stomach bug.”
She has not been able to keep liquids down.
She continued taking hydrochlorothiazide (HCTZ) 25 mg daily as prescribed.
Her mucous membranes are dry.
Laboratory Results
Na: 119
K: 3.7
Cl: 96
CO₂: 24
BUN: 65
SCr: 2.3
Glucose: 87
Urine osmolality (UOsm): 532
Urine sodium (UNa): 46
Question
What is the best treatment option, and what is the maximum correction rate?
Answer choices:
A. Fluid restriction, 10–12 mEq/L/day
B. Stop HCTZ, give 3% NaCl, 15–20 mEq/L/day
C. Stop HCTZ, give salt tablets, 4–6 mEq/L/day
D. Stop HCTZ, give 0.9% NaCl, 10–12 mEq/L/day
D. Stop HCTZ, give 0.9% NaCl, 10–12 mEq/L/day
A 32-year-old previously healthy female collapses at the finish line of a marathon with a new-onset, witnessed seizure.
In the emergency department:
Na: 117 mEq/L
Vital signs are stable
Yesterday, her Na was 137 mEq/L on a routine lab draw.
Question
What is the most appropriate treatment and monitoring?
Answer choices:
A. Lactated Ringer’s, check electrolytes in 4 hours
B. 0.9% NaCl, check electrolytes in 24 hours
C. D5W, check electrolytes in 12 hours
D. 3% NaCl, check electrolytes in 4 hours
D. 3% NaCl, check electrolytes in 4 hours
A 48-year-old male with a 30-year history of alcohol use presents to the emergency department with:
Shortness of breath
Abdominal ascites
He reports a 20-pound weight gain over the last 3 weeks and is diagnosed with new-onset cirrhosis.
Laboratory Results
Na: 118
K: 3.4
Cl: 104
CO₂: 22
BUN: 20
SCr: 1.2
Glucose: 193
Urine osmolality (UOsm): 170
Urine sodium (UNa): 16
Question
What is the most likely type of hyponatremia and underlying cause?
Answer choices:
A. Hypovolemic; SIADH
B. Euvolemic; hyperglycemia
C. Hypervolemic; cirrhosis
D. Pseudohyponatremia; “beer potomania”
C. Hypervolemic; cirrhosis
A 48-year-old male with a 30-year history of alcohol use presents to the emergency department with:
Shortness of breath
Abdominal ascites
He reports a 20-pound weight gain over the last 3 weeks and is diagnosed with new-onset cirrhosis.
Laboratory Results
Na: 118
K: 3.4
Cl: 104
CO₂: 22
BUN: 20
SCr: 1.2
Glucose: 193
Urine osmolality (UOsm): 170
Urine sodium (UNa): 16
Question
What are the best treatment options? (Select all that apply)
A. Fluid restriction
B. Salt restriction
C. Start Bumex
D. Start Aldactone
All of the above.