mod 3
1/273
Earn XP
Description and Tags
Chap 36, 37, 38, 39, 40, 41, 42 and 56.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
274 Terms
Antihistamines, Decongestants, Antitussives, and Expectorants- chap 36
Major disease that affects the lower respiratory disease is
COPD: emphysema, chronic bronchitis (obstruction of airflow in the airway)
Understanding the Common Cold
•Most caused by viral infection (rhinovirus or influenza virus)
•Virus invades tissues (mucosa) of upper respiratory tract, causing upper respiratory infection (URI)
Treatment of the Common Cold
•Involves combined use of antihistamines, nasal decongestants, antitussives, and expectorants
•Treatment is symptomatic only, not curative
•Symptomatic treatment does not eliminate the causative pathogen.
FDA recommendation
on 2008 FDA stated that OTC cough medication should not be given to children under the age of 2 due to recurrent oversedation, tachycardia, and death- parent are asked to consult pediatrician before giving the medication.
The common cold is treated with empiric therapy, which means
A.the medications cure the cold.
B.the medications only treat the symptoms.
C.herbal medications are useful to eliminate symptoms.
D. it is prevented with careful use of medications
OTC can only relieve the symptom of URI, They can do nothing to eliminate the causative pathogen
Antihistamines
§Drugs that directly compete with histamine for specific receptor sites
§MOA: it is involve in nerve impulse transmission in the CNS, dilation of capillaries, contraction of smooth muscles, stimulation of gastric secretion and acceleration of the heart
§Two histamine receptors
§H1 (histamine 1)- mediates smooth muscles and dilates the capillaries
§H2 (histamine 2)- mediates the acceleration of the heart and gastric acid secretion.
Antihistamine directly compete with histamine for specific receptor site- called histamine antagonist
AE- drowsiness that affects people
Anaphylaxis: Severe Allergic Reactions
•Release of excessive amounts of histamine can lead to:
•Constriction of smooth muscle, especially in the stomach and lungs
•Increase in body secretions
•Vasodilatation and increased capillary permeability- cause a drop in BP and edema.
•Major inflammatory mediator in many allergic disorders
•Allergic rhinitis (e.g., hay fever and mold, dust allergies)
•Anaphylaxis
•Angioedema
Antihistamines and Histamine Antagonists
•H1 antagonists (also called H1 blockers)-treatment for nasal allergies e.g hay fever.
•Examples: chlorpheniramine, fexofenadine (Allegra), loratadine (Claritin), cetirizine (Zyrtec), diphenhydramine (Benadryl)
•H2 blockers or H2 antagonists-used to reduce gastric acid in peptic ulcer disease.
•Examples: cimetidine (Tagamet), ranitidine (Zantac), famotidine (Pepcid), nizatidine (Axid)
Histamine vs. Antihistamine Effects
§Cardiovascular (small blood vessels)
§Histamine effect dilates the blood vessel, increase blood vessel permeability.
§Antihistamine effects- reduce the dilation of the blood vessel and increase permeability.
§Smooth muscle (on exocrine glands)
§Histamine effects causes extravascular smooth muscle in the bronchial tree. it stimilates salivary, gastric lacrimal and bronchial secretion
§Antihistamine effects: causes the bronchial tree to relax. reduces salivary , gastric, lacrimal and bronchial secretion.
§Immune system (release of substances commonly associated with allergic reactions)
§Histamine effects- release form mast cell with several other substance causes pruritus by stimulating the nerve endings ,
§Antihistamine effects prevent or alleviates itching, it does not stabilize mast cell.
Antihistamines: Indications
Management of
•Nasal allergies
•Seasonal or perennial allergic rhinitis (hay fever)
•Allergic reactions
motion sickness
parkinson disease - due to it anticholinergic effects
vertigo
Antihistamines: Contraindications
known drug allergy
narrow angle glaucoma
cardiac disease,
hypertension
bronchial asthma,
COPD
kidney disease
seizure disorders
BPH
pregnancy
Fexofenadine is not recommended for people with renal impairment
Loratidine is not recommended for chidren under 2 years.
Caution of antihistamine
use with caution on patients with impaired liver function and renal insufficiency as well with lactating mothers.
Amtihistamine Adverse effects
Anticholinergic (drying) effect most common
Drowsiness
change in vision
urinary retention
constipation
hypotension
palpitation
syncope
muscular weakness
paradoxical excitement
restlessness
seizures and nervousness
N/V/D
tinnitus
headache
In asthmatic attack
Do not use antihistamine as a sole drug during an acute asthmatic attack- use a rapid acting bronchodillator such as albuterol or in extreme cases epinephrine is urgently needed.
Before administering an antihistamine to a patient, it is most important for the nurse to assess the patient for a history of which condition?
A.Chronic urticaria
B.Motion sickness
C.Urinary retention
D.Insomnia
Antihistamines (2 types)
Traditional:•brompheniramine, chlorpheniramine, dimenhydrinate, diphenhydramine, meclizine, and promethazine
work peripherally and centrally
have anticholinergic effects
more effective than the nonsedative histamine
can be use alone or with others to relieve disorders ranging from insomnia to motion sickness.
Nonsedating:•loratadine, cetirizine, and fexofenadine
nonsedative histamine were develop to eliminate the unwanted effects of sedation of the older histamine. they do not cross the blood brain barrier.
they have longer duration of action
Loratidine(Claritin)
Class: H1 antihistamine
a nonsedative antihistamine taken once daily.
it does not redily distributes to the CNS, which readily diminish the sedative effects but if given in higher dose it might cause sedative effect.
they relieve symptoms of seasonal allergic rhinitis e.g hay fever, urticaria.
Contraindications:- drug allergies
Interaction:-ketocanazole, cimetidine, erythromycin- it inhibits its metabolism and increases the loratidine level.
Diphennhydamine(Benadryl)
Traditional antihistamine, it works pheripherally and centrally
have anticholinergic effect
more effective to the nonsedative antihistamine.
used as an hypnotic drug because of its sedative effect
its used to relief or prevent histamine mediated allergies, motion sickness, treats parkinson’s, promotes sleep
can be used in conjuction with epinephrine to manage anaphylaxis and treatment of acute dystonic reaction.
Contraindications
hypersensitivity
caution with elderly patients sinces it increases potential for falls.
caution with nursing mothers, neonates, and patients with lower respiratory tract symptoms
Antihistamines:Nursing Implications
§Instruct patients to report- advise patient to report any SOB, palpitation, or unusual adverse effects.
instruct patient to take medication with caution and report and fever, chest tightness, change of sputum from clear to colored, dyspnea or noisy breathing, activitities intolerance or weakness.
§Instruct patients to avoid driving or operating heavy machinery
§Instruct patients not to take these medications with other prescribed or OTC
§GI upset, how do you take- adise patient to take medication with snack or meal to minimize the GI upset.
§What do you do for dry mouth- encourage chewing gum, and fluids.
Nasal Congestion
•Excessive nasal secretions
•Inflamed and swollen nasal mucosa
•Primary causes
•Allergies
•URIs (common cold)
Decongestants: Types
§Three main types are used:
§Adrenergics(Sympathomimetics)Largest group,
§Anticholinergics(Parasympatholytics)Less commonly used
§Corticosteroids-Topical, intranasal steroids
Nasal Decongestants:
•MOA-Site of action: blood vessels surrounding nasal sinuses
•Adrenergics- constrict the small arterioles that supply the structure of the upper respiratory tract- blood vessel surronding the nasal sinus
•Nasal steroids- most commonly used for their effect to shrink engorged nasal mucous membranes and relieve nasal stiffness.
•Effects-aim at the inflammatory response elicited by by invading organism: virus, bacteria and other antigen.
•Indications-reduce nasal congestionassociated with acute and chronic rhinitis and hay fever or other allergies.
it reduces swelling on the nasal pasage and visualization of the nasal and pharyneal membrane.
•Contrainindications-
known drug allergy
narrow angle glaucoma
uncontrolled cardiovascular disease
hypertension
hyperthriodism
DM
Contraindication for decongestion include pt who are unable to control their eyes due to CVA or hx of CVA or TIA, long lasting asthma,BPH, or diabetes
Interaction- systemic sympathomimetic drugs and sympathomimetic nasal decongestant are likely to cause drug toxicity.
MOAI rise Bp when given with sympathomimetic nasal decongestants.
Nasal Decongestants: Adverse Effects
Adrenergics
Nervousness
Insomnia
Palpitations
Tremors
(Systemic effects caused by adrenergic stimulation)
excessive dosage can cause system effect elsewhere e.g Cardiovascular effects such as hypertension and palpitation, CNS effect such as headache, nervousness, and dizziness
Steroids
Local mucosal dryness and irritation
*Teaching
take medication as ordered
long term or excessive use may lead to rebound congestion
report any excessive dizziness, heart palpitation, weakness, sedation or irritability
Before administering an adrenergic decongestant, it is most important for the nurse to asses the patient for a history of
A.cataracts.
B.gastric ulcer.
C.diabetes mellitus.
D.hypothyroidism.
Adrenergic drugs are contraindicated in narrow angle glaucoma, uncontrolled cardiovascular disease, HTN, DM and hyperthyroidism
Antitussives
§Drugs used to stop or reduce coughing
§Opioid and nonopioid
§May be used in cases when coughing is harmful surgical procedure such as hernia repair and non productive cough
Antitussives: Mechanism of Action
Opioids: •Suppress the cough reflex by direct action on the cough center in the medulla
•Analgesia and drying the effect on the mucosa if the respiratory tract
helps reduce symptoms of runny nose and post nasal drip
Nonopiods:•Dextromethorphan: works in the same way by supressing the the cough reflex through a direct action on the cough center
•No CNS depression
no analgesic effect
Antitussives:
§Indications
§Used to stop the cough reflex when the cough is nonproductive or harmful
§Contraindications
known drug allergy
opiod dependency
high risk for respiratory depression
§Adverse effects
Benzonate- dizziness, headaches, sedation, nausea, constipation, pruirits and nasal congestion.
Codeine and hydrocodone: sedation, nausea, vomiting, lightheadedness, and constipation
Dextromethorphan: dizziness, drowsiness, and nausea
Diphenhydramine: sedation, dry mouth, and other anticholinergic effects
Antitussives:Nursing Implications
§Report any of the following symptoms to the caregiver:
§Cough that lasts more than 1 week
§Persistent headache
§Fever
§Rash
§Antitussive drugs are for nonproductive coughs.
Drowsiness or dizziness may occur with the use of antitussives; therefore caution patients against driving a car
§Monitor for intended therapeutic effects.
Dextromethorpahn
nonopioid antitussive
it is safe, nonaddicting, and does not cause respiratory or CNS depression.
Its use is contraindicated in cases of known drug allergy, asthma or emphysema, or persistent headache.
Benzonate
is a nonopioid antitussive drug
work by anesthetizing or numbing the cough receptors
Its use is contraindicated in patients with a known hypersensitivity to it
A 94-year-old patient has a severe dry cough. He has coughed so hard that the muscles in his chest are hurting. He is unsteady on his feet and slightly confused. Which drug would be the best choice for this patient’s cough
A. Benzonate (tessalon perles)
B. Dextromethorphan (Robitussin-DM) oral solution
C. Codeine cough syrup
D. Guaifenesin(Mucinex)
Bezonaates supresses the cough reflex by anesthetizing the stretch receptor cell in the respiratory tract, which prevents reflex stimulation of the medullary cough center.
Expectorants
§Drugs that aid in the expectoration (removal) of mucus
§Reduce the viscosity of secretions
§Disintegrate and thin secretions
§Example: guaifenesin
Indication: used to relief productive cough commonly associated with common cold, bronchitis, larynitis, pharyngitis, pertussis, influenza and measles.
Guaifenesin
MOA: act by increasing the hydration of the respiratory tract
maintaining the sol layer which is needed for ciliary clearance reducing the viscosity of mucus
facilitates mucus removal.
§Indication: Relief of productive cough commonly associated with the common cold, bronchitis, laryngitis, pharyngitis, pertussis, influenza, and measles.
used for suppression of coughs caused by chronic paranasal sinusitis.
Contraindication: known drug allergy
AE- may cause nausea, vomiting, and gastric irritation.
Expectorants:Nursing Implications
•Expectorants should be used with caution in older adults and patients with asthma or respiratory insufficiency.
•Patients taking expectorants should receive more fluids, if permitted, to help loosen and liquefy secretions.
•Report a fever, cough, or other symptoms lasting longer than 1 week.
•Monitor for intended therapeutic effects.
A patient with a tracheostomy developed pneumonia. It is very difficult for the patient to cough up the thick, dry secretions he has developed. The nurse identifies which drug as being most effective in helping this patient
A.Benzonatate (Tessalon Perles) capsules
B.Dextromethorphan (Robitussin-DM) oral solution
C.Codeine cough syrup
D.Guaifenesin (Mucinex)
Guanifesin is beneficial in treatment of productive cough because it thins mucus in the respiratory tract that is unable to cough up.
When assessing a patient who is to receive a decongestant, the nurse will recognize that a potential contraindication to this drug would be which condition? Select all that apply.
A. Glaucoma
b. Fever
c. Hypertension
d. Peptic ulcer disease
e. Allergic rhinitis
•Contrainindications-known drug allergy, narrow angle glaucoma, uncontrolled cardiovascular disease, hypertension, hyperthriodism, DM
When giving decongestants, the nurse must remember that these drugs have alpha-adrenergic–stimulating effects that may result in which effect?
a. Fever
b. Bradycardia
c. Hypertension
d. CNS depression
The nurse is reviewing a patient's medication orders for prn (as necessary) medications that can be given to a patient who has bronchitis with a productive cough. Which drug will the nurse choose?
a. An antitussive
b. An expectorant
c. An antihistamine
d. A decongestant
Drugs that aid in the expectoration (removal) of mucus.Expectorants are used for the relief of productive cough commonly associated with the common cold, bronchitis, laryngitis, pharyngitis, pertussis, influenza, and measles.
The nurse knows that an antitussive cough medication would be the best choice for which patient?
A patient with a productive cough
b. A patient with chronic paranasal sinusitis
c. A patient who has had recent abdominal surgery
d. A patient who has influenza
antiussive may be used in cases when coughing is harmful surgical procedure such as hernia repair and non productive cough
A patient is taking a decongestant to help reduce symptoms of a cold. The nurse will instruct the patient to observe for which possible symptom, which may indicate an adverse effect of this drug?
a. Increased cough
b. Dry mouth
c. Slower heart rate
d. Heart palpitations
possible adverse effect of this drug is nervousness, insomnia, palpitation, and tremor.
The nurse is giving an antihistamine and will observe the patient for which side effects? (Select all that apply.)
a. Hypertension
b. Dizziness
c. “Hangover” effect
d. Drowsiness
e. Tachycardia
f. Dry mouth
Drowsiness is usually the chief complaint.
The order for patient reads: “Give guaifenesin, 300 mg per enteral feeding tube every 4 hours as needed for cough.” The medication comes in a bottle that has 100 mg/5 mL. How many milliliters will the nurse give per dose?
15ml
The nurse notes in a patient's medication history that the patient is taking benzonatate (Tessalon Perles) as needed. Based on this finding, the nurse interprets that the patient has which problem?
a. Cough
b. Seasonal allergies
c. Chronic rhinitis
d. Motion sickness
Benzonatate (Tessalon Perles) is a nonopioid antitussive drug that is thought to work by anesthetizing or numbing the cough receptors.
Respiratory Drugs chap 37
Diseases of the Lower Respiratory Tract
-Chronic obstructive pulmonary disease (COPD): obstruct airflow to the airway.
–Asthma (persistent and present most of the time despite treatment)
–Emphysema
–Chronic bronchitis
other LRT syndrome include
Cystic fibrosis
infant respiratory distress syndrome
Asthma
Recurrent and reversible shortness of breath.
Asthma occurs when the airways of the lung (bronchi and bronchioles) become narrow as a result of bronchospasm, inflammation, and edema of the bronchial mucosa, and the production of viscous (sticky) mucus.
Four categories
–Intrinsic: occur in patients with no history of allergies
cause of intrinsic, or idiopathic, asthma is unknown.
It is not mediated by IgE
There is often no family history of allergies
–Extrinsic: occur in patients exposed to a known allergen due to hypersensivity
E.g include pollen, mold, dust, animal dander, and cigarette smoke, from either smoking or exposure to secondhand smoke.
–Exercise induced
–Drug induced
■Status asthmaticus- asthma attack that may be prolonged and may not respond to typical drug therapy.
Asthma attack
Wheezing and difficulty breathing.
When an episode has a sudden and dramatic onset.
The antibody involved with asthma
IgE
Chronic Bronchitis
•Continuous inflammation and low-grade infection of the bronchi
•Excessive secretion of mucus and certain pathologic changes in the bronchial structure
Inflammation in the associated bronchioles (smaller bronchi) is responsible for most of the airflow obstruction
•Often occurs as a result of prolonged exposure to bronchial irritants most common is cigarette
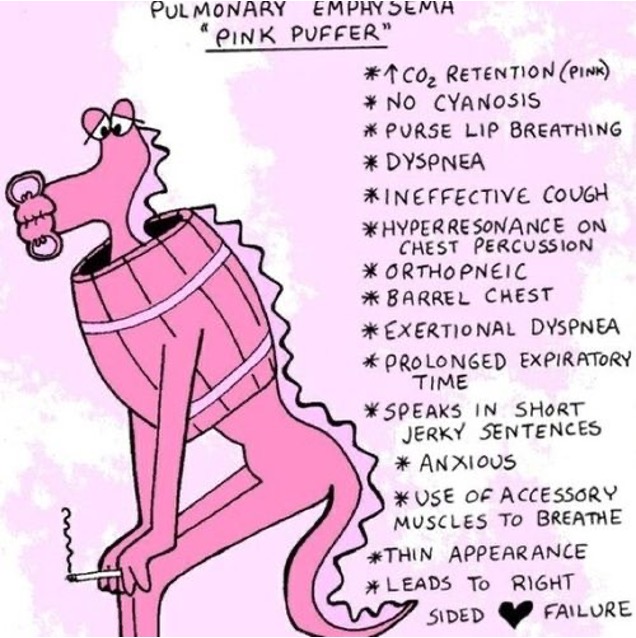
Emphysema
•Air spaces enlarge as a result of the destruction of alveolar walls.
•Caused by the effect of proteolytic enzymes released from leukocytes in response to alveolar inflammation
Alveolar walls are partially destroyed
There is also an associated genetic deficiency of the enzyme alpha1-antitrypsin.
Bronchodilator
–These drugs relax bronchial smooth muscle, which causes dilation of the bronchi and bronchioles that are narrowed as a result of the disease process.
–Three classes: beta-adrenergic agonists, anticholinergics, and xanthine derivatives
Bronchodilators: Beta-Adrenergic Agonists
•Commonly used during the acute phase of an asthmatic attack to quickly reduce airway constriction and restore airflow
Beta agonists imitate the effects of norepinephrine on beta receptors, they are also called sympathomimetic bronchodilators
Short-acting beta agonist (SABA) inhalers
•albuterol (Ventolin)
•levalbuterol (Xopenex)
•pirbuterol (Maxair)
•terbutaline (Brethine)
•metaproterenol (Alupent)
•Long-acting beta agonist (LABA) inhalers
•arformoterol (Brovana)
•formoterol (Foradil, Perforomist)
•salmeterol (Serevent)
•Used during acute phase of asthmatic attacks
•Quickly reduce airway constriction and restore normal airflow
•Agonists, or stimulators, of the adrenergic receptors in the sympathetic nervous system
•Sympathomimetics
Bronchodilators: Beta-Adrenergic Agonists
•Nonselective adrenergics agonist drugs
•Stimulate alpha, beta1 (cardiac), and beta2 (respiratory) receptors
•Example: epinephrine (EpiPen)
•Nonselective beta-adrenergics
•Stimulate both beta1 and beta2 receptors
•Example: metaproterenol
•Selective beta2 drugs
•Stimulate only beta2 receptors
•Example: albuterol,levalbuterol
Beta-Adrenergic Agonists:
•MOA-
•Begins at the specific receptor stimulated
•Ends with dilation of the airways
The action of beta agonist bronchodilators begins at the specific receptor stimulated and ends with the relaxation and dilation of the airways.
When a beta2-adrenergic receptor is stimulated by a beta agonist, adenylate cyclase is activated and produces cyclic adenosine monophosphate (cAMP).
Adenylate cyclase is an enzyme needed to make cAMP. The increased levels of cAMP cause bronchial smooth muscles to relax, which results in bronchial dilation and increased airflow into and out of the lungs.
•Indications: prevention or relief of bronchospasm related to bronchial asthma, bronchitis, and other pulmonary diseases.
they have the ability to stimulate both beta1- and alpha-adrenergic receptors, they may be used to treat hypotension and shock
•Contraindications known drug allergy, uncontrolled hypertension or cardiac dysrhythmias, and high risk for stroke
Beta-Adrenergic Agonists: Adverse Effects
•Alpha and beta- mixed (epinephrine)
•Hyperglycemia
•Tremor
•Cardiac stimulation
insomnia
restlesness
anorexia
•Beta1 and beta2 (metaproterenol)
•Cardiac stimulation
•Tremor
•Hypotension
vascular headache
anginal pain
•Beta2 (albuterol)
•Hypotension or hypertension
•Vascular headache
•Tremor
Antidote of beta2 drugs
administration of a beta blocker while the patient is under close observation due to the risk for bronchospasm. Because the half-life of most adrenergic agonists is relatively short, the patient may just be observed while the body eliminates the medication.
Beta-Adrenergic Agonists: Interactions
•Diminished bronchodilation when nonselective beta blockers are used with the beta agonist bronchodilators
•Monoamine oxidase inhibitors- enhance risk of hypertension
•Sympathomimetics
•Monitor patients with diabetes; an increase in blood glucose levels can occur
Beta-Adrenergic Agonists: Albuterol (Proventil)
■Short-acting, beta2-specific bronchodilating beta agonist-(SABA)
■Most commonly used drug in this class
■Must not be used too frequently
If albuterol is used too frequently, dose-related adverse effects may be seen, because albuterol loses its beta2-specific actions, especially at larger dosages. As a consequence, the beta1 receptors are stimulated, which causes nausea, increased anxiety, palpitations, tremors, and an increased heart rate.
■Oral and inhalational use
Beta-Adrenergic Agonists: Salmeterol (Serevent)
■Long-acting beta2 agonist bronchodilator (LABA)
■Never to be used for acute treatment
■Used for the maintenance treatment of asthma and COPD and is used in conjunction with an inhaled corticosteroid
Black box warning: increase in asthma related death when added in usual asthma therapy- risk in African American
AE- immediate hypersensitivity reactions, headache, hypertension, and neuromuscular and skeletal pain.
Do not give this medication twice, nor should the maximum dose be exceeded. one puff twice daily.
Anticholinergics: Mechanism of Action- LAMAs
•Acetylcholine (ACh) causes bronchial constriction and narrowing of the airways.
Long acting muscarinic antagonist.
•Anticholinergics bind to the ACh receptors, preventing ACh from binding.
•Result: bronchoconstriction is prevented, airways dilate
•Ipratropium (Atrovent), tiotropium (Spiriva), and aclidinium (Tudorza)
•Indirectly cause airway relaxation and dilation
•Help reduce secretions in COPD patients
•Indications:
•prevention of the bronchospasm associated with COPD and not for the
management of acute symptoms.
Contrainidications-
use of bronchial anticholinergic drugs is known drug allergy, including allergy to atropine.
Caution is necessary in patients with acute narrow-angle glaucoma and prostate enlargement.
Anticholinergics: Adverse Effects
•Dry mouth or throat
•Nasal congestion
•Heart palpitations
•Gastrointestinal (GI) distress
•Headache
•Coughing
•Anxiety
urinary retention
increase intraocular pressure
Anticholinergics: Ipratropium (Atrovent)
■Oldest and most commonly used anticholinergic bronchodilator
■Available both as a liquid aerosol for inhalation and as a multidose inhaler
■Usually dosed twice daily
Xanthine Derivatives
■Plant alkaloids: caffeine, theobromine, and theophylline
■Only theophylline is used as a bronchodilator
■Synthetic xanthines: aminophylline and dyphilline
■MOA- Xanthines cause bronchodilation by increasing the levels of the energy-producing substance cAMP. They do this by competitively inhibiting phosphodiesterase, the enzyme responsible for breaking down cAMP.
■Indications- used in mild to moderate cases of acute asthma and as an adjunct drug in the management of COPD.
Contraindication: known drug allergy, uncontrolled cardiac dysrhythmias, seizure disorders, hyperthyroidism, and peptic ulcers
Adverse effects- nausea, vomiting, and anorexia. Cardiac adverse effects include sinus tachycardia, extrasystole, palpitations, and ventricular dysrhythmias. Transient increased urination and hyperglycemia
In patients with COPD
cAMP plays an integral role in the maintenance of open airways.
Higher intracellular levels of cAMP contribute to smooth muscle relaxation inhibit IgE-induced release of the chemical mediators that drive allergic reactions
Xanthine Derivatives: Caffeine
■Used without prescription as a CNS stimulant or analeptic to promote alertness( long duration, driving and studying
■Cardiac stimulant in infants with bradycardia
■Enhancement of respiratory drive in infants
Xanthine Derivatives: Theophylline
■Most commonly used xanthine derivative
■Oral, rectal, injectable (as aminophylline), and topical dosage forms
■Aminophylline: intravenous (IV) treatment of patients with status asthmaticus
prodrug if theophylline
■Therapeutic range for theophylline blood level is 10-20 mcg/ml however most prescriber now recommend 5-15mcg/ml
beneficial effects of theophylline can be maximized by maintaining blood levels within a certain target range.
Theophylline is metabolized to caffeine in the body
Theophylline and other xanthines stimulate the CNS, but to a lesser degree than caffeine
In large doses, theophylline may stimulate the cardiovascular system, which results in both an increased force of contraction (positive inotropy) and an increased heart rate (positive chronotropy).
The increased force of contraction raises cardiac output and hence blood flow to the kidneys. which causes xanthines to dilate blood vessels in and around the kidney, increasing the GFR and produces a diuretic effect.
Nonbronchodilating Respiratory drugs
•Leukotriene receptor antagonists (montelukast, zafirlukast, and zileuton)
•Corticosteroids (beclomethasone, budesonide, dexamethasone, flunisolide, fluticasone, ciclesonide, and triamcinolone)
•Mast cell stabilizers: rarely used cromolyn and nedocromil
they work by stabilizing the cell membranes of mast cells to prevent the release of inflammatory mediators such as histamine.
When a chain reaction triggers allergen.
Leukotrienes is produced. In people with asthma, leukotrienes cause inflammation, bronchoconstriction, and mucus production. This in turn leads to coughing, wheezing, and shortness of breath.
Leukotriene Receptor Antagonists (LTRAs)
The first subclass of LTRAs acts by an indirect mechanism and inhibits the enzyme 5-lipoxygenase, which is necessary for leukotriene synthesis.
Example: Zileuton (Zyflo)
Drugs in the second subclass of LTRAs act more directly by binding to the D4 leukotriene receptor subtype in respiratory tract tissues and organs.
Example: montelukast (Singulair) and zafirlukast (Accolate).
LTRA are primarily limited to the lungs
•MOA
LTRAs prevent leukotrienes from attaching to receptors located on circulating immune cells (e.g., lymphocytes in the blood) as well as local immune cells within the lungs (e.g., alveolar macrophages).
They prevent smooth muscle contraction of the bronchial airways, decrease mucus secretion
reduce vascular permeability (which reduces edema) through their reduction of leukotriene synthesis.
prevention of the mobilization and migration of such cells as neutrophils and lymphocytes into the lungs. This also serves to reduce airway inflammation.
•Indications- The LTRAs montelukast, zafirlukast, and zileuton are used for the prophylaxis and long-term treatment and prevention of asthma.
improvement is seen in 1 wk.
•Contindications- KDA
Allergy to povidone
lactose
titanium dioxide or cellulose derivatives
•Adverse effects- The most commonly reported adverse effects of zileuton include headache, nausea, dizziness, and insomnia.
he most common adverse effects of montelukast and zafirlukast include headache, nausea, and diarrhea.
Montelukast (singulair)
LTRA
works by blocking leukotrine D4 receptors to augment the inflammatory response.
Corticosteroids (Glucocorticoids)
•Antiinflammatory properties
•Used for chronic asthma
•Do not relieve symptoms of acute asthma attacks
•Oral or inhaled forms
•May take several weeks before full
effects are seen
•MOA- it is thought that they have the dual effect of both reducing inflammation and enhancing the activity of beta agonists.
prevent various nonspecific inflammatory processes.
stabilize the membranes of cells that normally release bronchoconstricting substances.
White Blood cells with costicosteriod effects
Neutrophils (65%): Contain powerful lysosomes; release chemicals that destroy invading organisms and also attack other WBCs ——-Stabilize cell membranes so that inflammation-causing substances are not released
Eosinophils (2%–5%): Function mainly in allergic reactions and protect against parasitic infections; ingest inflammatory chemicals and antigen-antibody complexes—-Little effect, if any
Basophils (0.5%–1%): Contain histamine, an inflammation-causing substance, and heparin, an anticoagulant———Stabilize cell membranes so that histamine is not released
Agranulocytes
Lymphocytes (25%):Two types: T lymphocytes and B lymphocytes; T cells attack infecting microbial or cancerous cells; B cells produce antibodies against specific antigens——Decrease activity of the lymphocytes
Monocytes (3%–5%)": Produce macrophages, which can migrate out of the bloodstream to such places as mucous membranes, where they are capable of engulfing large bacteria or virus-infected cells____Inhibit macrophage accumulation in already inflamed areas, thus preventing more inflammation
Inhaled Corticosteroids
•beclomethasone dipropionate (Beclovent), budesonide (Pulmicort Turbuhaler), dexamethasone sodium phosphate (Decadron Phosphate Respihaler), fluticasone (Flovent)
•Indications: Used for the primary treatment of bronchospastic disorders to control the inflammatory responses that are believed to be the cause of these disorders; they are indicated for persistent asthma
In respiratory illnesses, systemic corticosteroids are generally used only to treat acute exacerbations, or severe asthma.
When a rapid, pronounced antiinflammatory effect is needed, as in an acute exacerbation of asthma or other COPD, intravenous corticosteroids (e.g., methylprednisolone) are often used.
•Contraindications: contraindicated in patients who are hypersensitive to glucocorticoids,
in patients whose sputum tests positive for Candida organisms,
in patients with systemic fungal infection, as the corticosteroids can suppress the immune system.
•Adverse effects
pharyngeal irritation
coughing
dry mouth
oral fungal infections.
Instruct patients to rinse their mouths after use of an inhaled corticosteroid.
Systemic drug effects:
adrenocortical insufficiency
increased susceptibility to infection
fluid and electrolyte disturbances
endocrine effects
CNS effects (insomnia, nervousness, seizures)
dermatologic and connective tissue effects, including brittle skin, bone loss, osteoporosis, and Cushing's syndrome
Nursing teaching on costicosteriod
Taper medication slowly to avoid Addisonian crisis
The patient who is dependent on systemic corticosteroids may need up to 1 year of recovery time after discontinuation of systemic therapy.
There is evidence that bone growth is suppressed in children and adolescents taking corticosteroids
Drug to Drug interaction of Corticosteroid
increase glucose level- adjustments in dosages of antidiabetic drugs is needed.
The antifungal drug itraconazole may reduce clearance of the steroids
phenytoin, phenobarbital, and rifampin may enhance clearance.
There is greater risk for hypokalemia with concurrent use of potassium-depleting diuretics such as hydrochlorothiazide and furosemide.
Nursing Implications
–Avoid exposure to conditions that precipitate bronchospasm (allergens, smoking, stress, air pollutants).
–Adequate fluid intake
–Compliance with medical treatment
–Avoid excessive fatigue, heat, extremes in temperature, and caffeine.
■Perform a thorough assessment before beginning therapy, including:
Which medication will the nurse teach a patient with asthma to use when experiencing an acute asthma attack?
A.albuterol (Ventolin)
B.salmeterol (Serevent)
C.theophylline (Theo-Dur)
D.montelukast (Singulair)
Albuterols is a SABA and IV systemic corticosteroids are used to provide quick relief of asthma.
A patient with chronic bronchitis calls the office for a refill of his albuterol inhaler. He just had the prescription filled 2 weeks ago, but he says it is empty. When asked, he tells the nurse, “I use it whenever I need it, but now when I use it, I feel so sick. I’ve been needing to use it more often.” What is the most appropriate action by the nurse?
A.The nurse should confirm the pharmacy location for the needed refill.
B.The nurse should ask the patient to come to the office for an evaluation of his respiratory status.
C.The nurse should tell the patient not to use this drug too often.
D.The nurse should consult the prescriber for a different inhaler prescription.
If albuterol is used too frequently, dose-related adverse effects may be seen, because albuterol loses its beta2-specific actions, especially at larger dosages. As a consequence, the beta1 receptors are stimulated, which causes nausea, increased anxiety, palpitations, tremors, and an increased heart rate.
Inhalers: Patient education
■For any inhaler prescribed, ensure that the patient is able to self-administer the medication.
–Provide demonstration and return demonstration.
–Ensure that the patient knows the correct time intervals for inhalers.
–Provide a spacer if the patient has difficulty coordinating breathing with inhaler activation.
–Ensure that the patient knows how to keep track of the number of doses in the inhaler device.
A patient is prescribed two different types of inhaled medications for treatment of COPD. After administering the first medication, how long should the nurse wait to administer the second medication?
A.1 minute
B.5 minutes
C.10 minutes
D.15 minutes
If a second puff of the same drug is ordered, instruct the patient to wait 1 to 2 minutes between puffs. If a second type of inhaled drug is ordered, instruct the patient to wait 2 to 5 minutes between the medication
The nurse is providing teaching to a group of individuals with COPD at a community center. Which statement by one of the attendees indicates that further teaching is needed?
A.“If I develop a puffy face, I will stop taking methylprednisolone (Medrol) immediately.”
B.“I will inform my prescriber of any weight gain of 2 lb or more in 24 hours or 5 lb or more in 1 week.”
C.“I use omalizumab (Xolair) to control my asthma but not for an acute asthma attack.”
D.“When taking theophylline (Theo-Dur), I will advise my prescriber if I experience epigastric pain.”
Advise the patient to take the medication as ordered every day, regardless of whether or not he or she is feeling better
One of the attendees expresses concern regarding her granddaughter’s asthma. The attendee tells the nurse that she is afraid that she will not know which of her granddaughter's medications to give first in case of an asthma attack. Which medication should the nurse inform the attendee to administer first for an acute asthma attack?
A. ipratropium (Atrovent)
B. albuterol (Proventil)
C. budesonide (Pulmicort Turbuhaler)
D. montelukast (Singulair)
1. A patient who has a history of asthma is experiencing an acute episode of shortness of breath and needs to take a medication for immediate relief. The nurse will choose which medication that is appropriate for this situation?
A beta agonist, such as albuterol
b. A leukotriene receptor antagonist, such as montelukast
c. A corticosteroid, such as fluticasone
d. An anticholinergic, such as ipratropium
2. After a nebulizer treatment with the beta agonist albuterol, the patient complains of
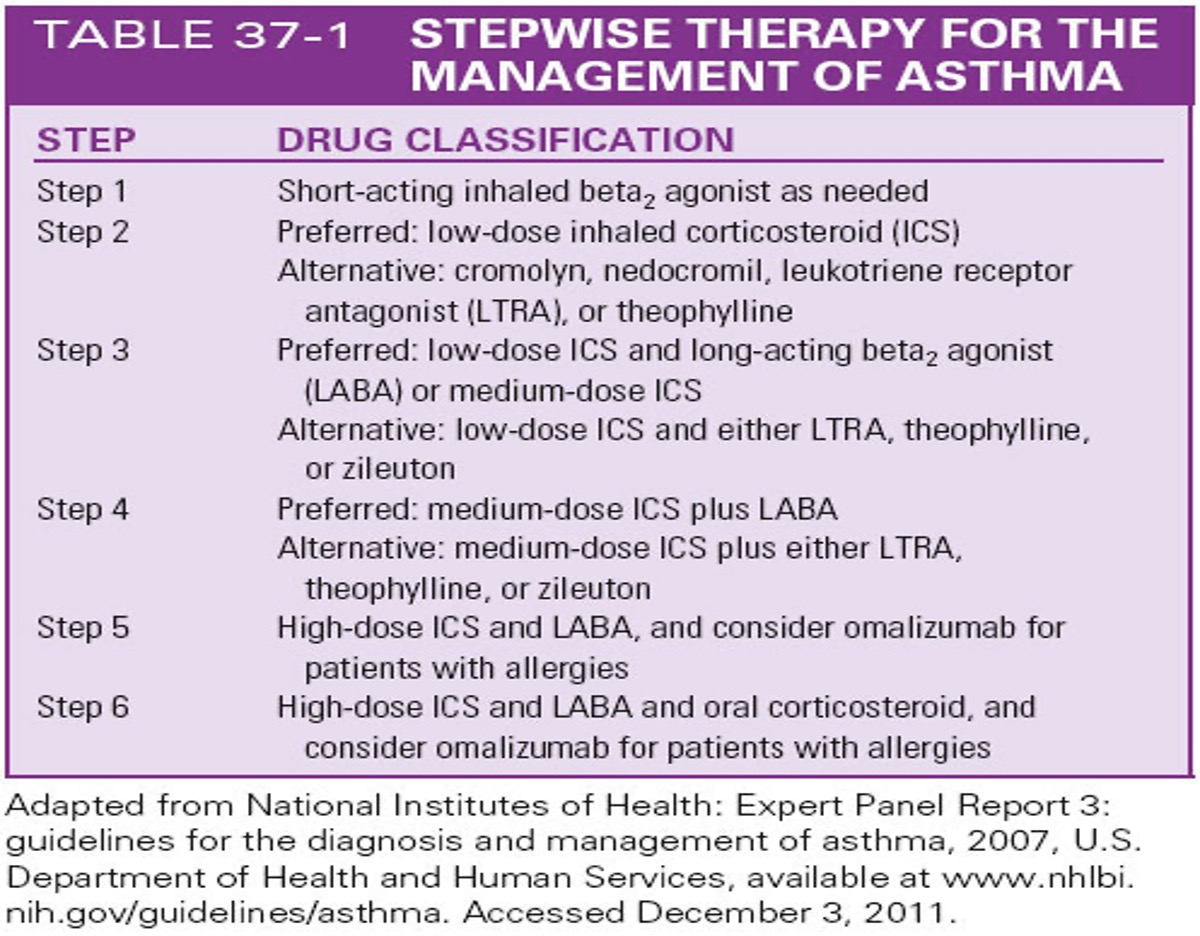
One of the attendees tells the nurse that he has asthma and is being treated with a short-acting inhaled beta2 agonist. The nurse identifies this treatment as which step of the stepwise therapy for the treatment of asthma?
A.Step 1
B.Step 2
C.Step 3
D.Step 4
After a nebulizer treatment with the beta agonist albuterol, the patient complains of feeling a little “shaky,” with slight tremors of the hands. The patient's heart rate is 98 beats/min, increased from the pretreatment rate of 88 beats/min. The nurse knows that this reaction is which of these?
a. An expected adverse effect of the medication.
b. An allergic reaction to the medication.
c. An indication that he has received an overdose of the medication.
d. An idiosyncratic reaction to the medication.
The beta2 drugs can cause both hypertension and hypotension, vascular headaches, and tremor
A patient is receiving ipratropium via an inhaler. The nurse will assess the patient for which of these adverse effects? (Select all that apply.)
a. CNS depression
b. Dry mouth or throat
c. Increased appetite
d. Nasal congestion
e. Headache
Adverse effects of inhaled anticholinergics are related to their pharmacology and include dry mouth or throat, nasal congestion, heart palpitations, gastrointestinal (GI) distress, urinary retention, increased intraocular pressure, headache, coughing, and anxiety.
During a teaching session for a patient who will be receiving a new prescription for the LTRA montelukast (Singulair), the nurse will tell the patient that the drug has which therapeutic effect?
a. Improves the respiratory drive
b. Loosens and removes thickened secretions
c. Reduces inflammation in the airway
d. Stimulates immediate bronchodilator
Montelukast work by blocking leukotriene D4 receptors to augment the inflammatory response. They block the inflammatory process in asthma
After the patient takes a dose of an inhaled corticosteroid, such as fluticasone (Flovent), what is the most important action the patient needs to do next?
a. Hold the breath for 60 seconds.
b. Rinse out the mouth with water.
c. Follow the corticosteroid with a bronchodilator inhaler, if ordered.
d. Repeat the dose in 15 minutes if the patient feels short of breath.
Rinsing the mouth with water is appropriate and necessary to prevent oral fungal infections. Instruct the patient about keeping the inhaler clean.
The nurse is teaching a patient about the inhaler Advair (fluticasone/salmeterol). Which statements by the patient indicate a correct understanding of this medication? (Select all that apply.)
a. “I will rinse my mouth with water after each dose.”
b. “I need to use this inhaler whenever I feel short of breath, but not less than 4 hours between doses.”
c. “This medication is taken twice a day, every 12 hours.”
d. “I can take this inhaler if I get short of breath while exercising.”
e. “I will call my doctor if I notice white patches inside my mouth.”
A patient who is taking a xanthine derivative for COPD asks the nurse, “I miss my morning coffee. I can't wait to go home and have some.” What is the nurse's best response?
a. “I know how you feel. I'd miss my coffee too.”
b. “I can get some coffee for you. I’ll be right back.”
c. “It's important not to take coffee or other caffeinated products with this medicine, as it may cause an increased heart rate as well as other problems.”
d. “You’ve been on this medicine for a few days. I can call your prescriber to ask
Instruct patients about food and beverage items that contain caffeine (e.g., chocolate, coffee, cola, cocoa, tea), because their consumption can exacerbate CNS stimulation.
The nurse is preparing to administer the elixir form of theophylline to a patient who has a PEG tube. The dose is 240 mg daily, and the medication is available in a concentration of 80 mg/15 mL. How many milliliters of medication will the nurse give per dose?
45ml
if bronchodilator and cortecosteriod inhaler is ordered for a patient
always administer the bronchodilator first before the cortecoidsteriod to help provide the bronchial with relaxation and dilation before administering antiinflammatory drug.
Antitubellar Drugs chap 42
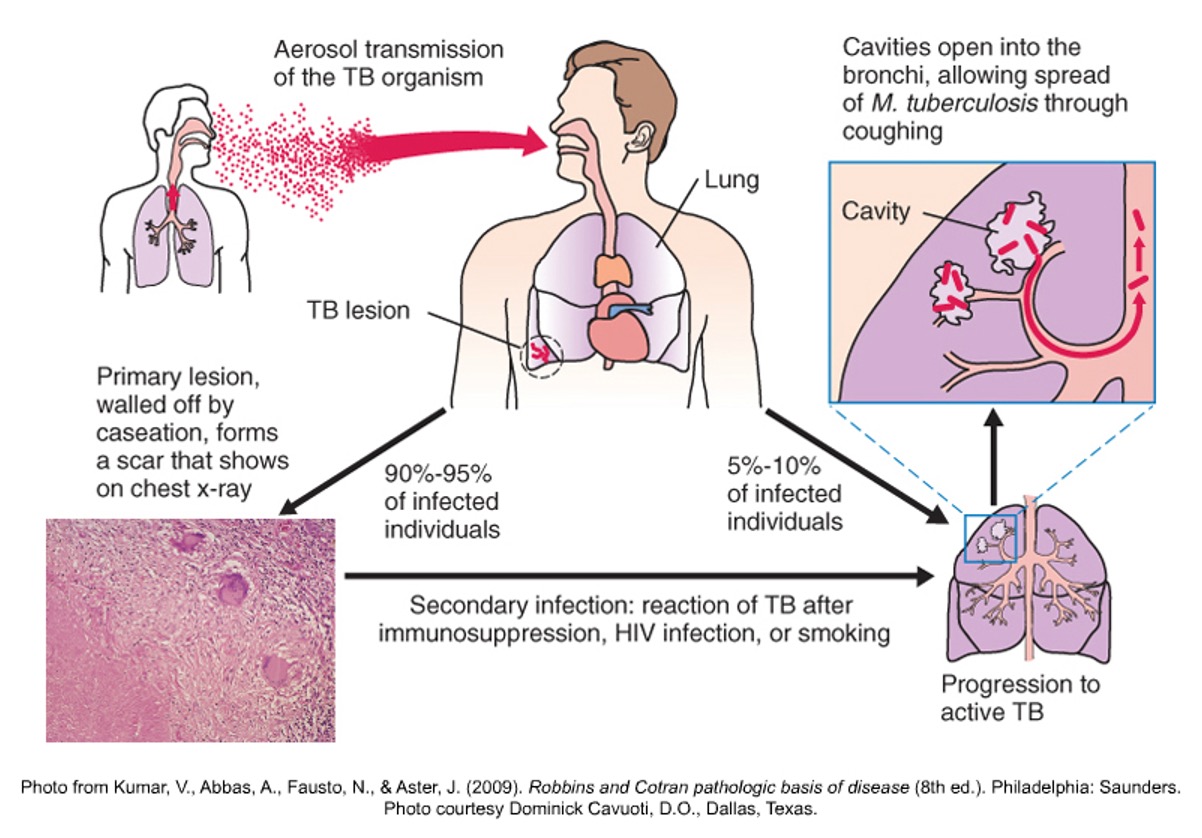
TB infection
•Lesions may progress by entering bloodstream
•Usually affects only the lungs
•May take years for symptoms to develop
•Secondary TB: Reactivation of the disease in a previously infected person whose primary lesions never completely resolved
Types of drugs of tuberculosis
■First line antitubercular drugs- primary
ethambutol
isoniazid (INH)
pyrazinamide (PZA)
rifabutin
rifampin
rifapentine
streptomycin
–Risk of transmission is reduced after 2-3 weeks of therapy
–Combination drug therapy is needed
Before the results of the susceptibility tests are known, the patient is started on a four-drug regimen consisting of isoniazid, rifampin, pyrazinamide (PZA), and ethambutol or streptomycin, which together are 95% effective in
–Therapy continues until infection is under control
–Current first-line therapy for TB uses isoniazid, rifampin, pyrazinamide, and ethambutol in different combinations and schedules
How these drugs work
■Bactericidal versus bacteriostatic
The major effects of drug therapy include reduction of cough and, therefore, reduction of the infectiousness of the patient
Successful treatment usually involves taking several antibiotic drugs for at least 6 months and sometimes for as long as 12 months.
–Isoniazid works by inhibiting several enzymes important to mycobacteria metabolism and reproduction
–Rifampin prevents reproduction of the TB organism by binding to the enzyme that allows RNA to be transcribed
–Pyrazinamide reduces the pH of the intracellular fluid of WBCs in which the TB bacillus resides
Intended Responses and Side Effects
•Cough is reduced and sputum production reduced
•Fatigue is reduced and weight is gained
•Sputum culture is negative
•Side effects
•Diarrhea and vomiting
•Difficulty sleeping
•Breast tenderness or enlargement
•Loss of appetite and sore throat
Adverse effects
•Liver toxicity
•Potential to interact with other drugs
•Isoniazid can cause peripheral neuropathy with loss of sensation
•Rifampin often causes anemia
•Ethambutol at high doses can cause optic neuritis vision changes
What to do
•Before
•Make sure patient has no liver problems
•Ask males if they have enlarged prostate
•Ask all patients about urine retention
•Before starting rifampin, check for anemia
•Before giving pyrazinamide or ethambutol, ask about gout