Cases test 1 revision
1/48
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
49 Terms
CT features of epidural haematoma
Biconvex collection of blood which does not cross suture lines
Hyperdense
Bubbles at fracture site (bone window)
Usually in pteryion temporal region
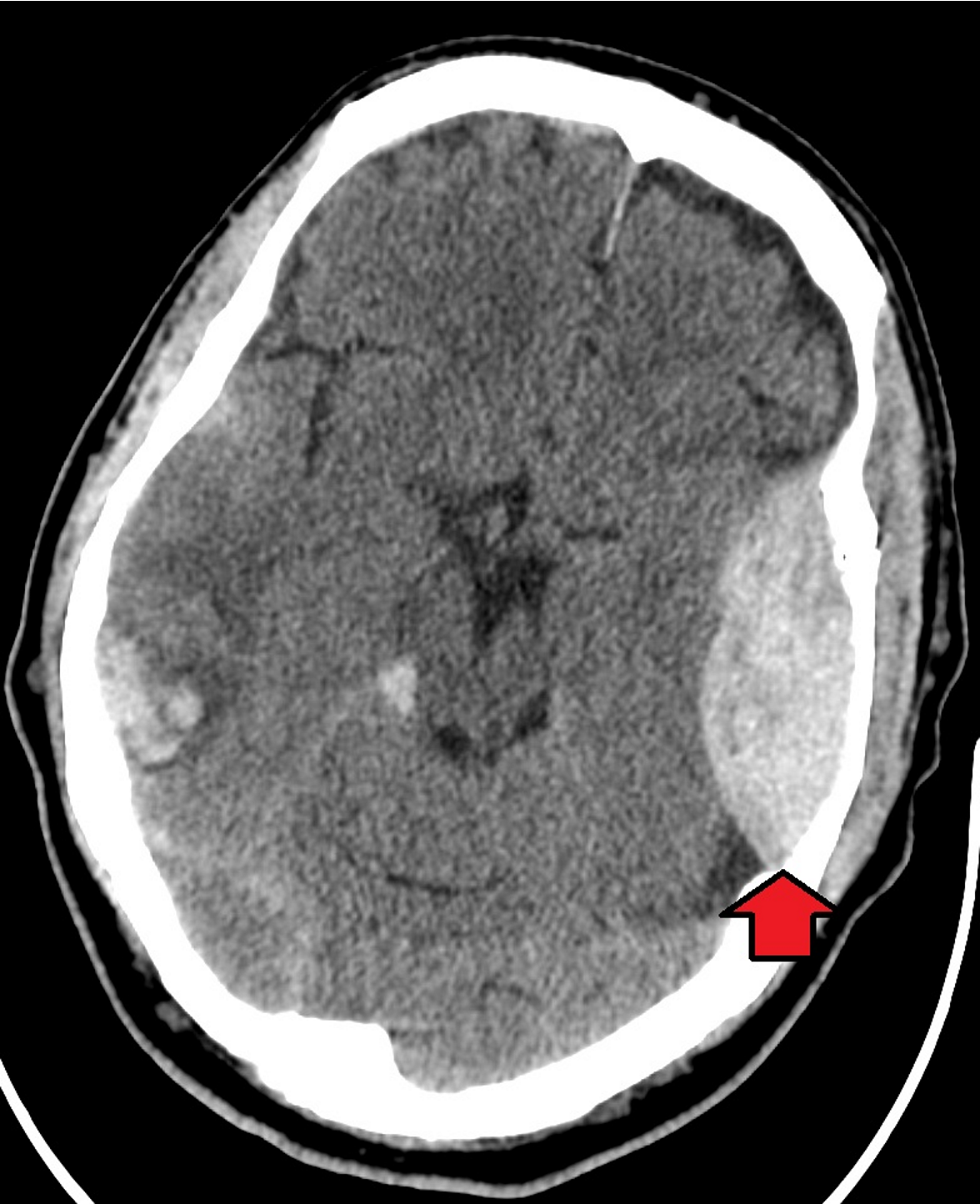
CT features of subdural haematoma
Crescent shaped, usually over convexity
Crosses suture lines
Hyperdense (acute) ir hypodense (chronic)
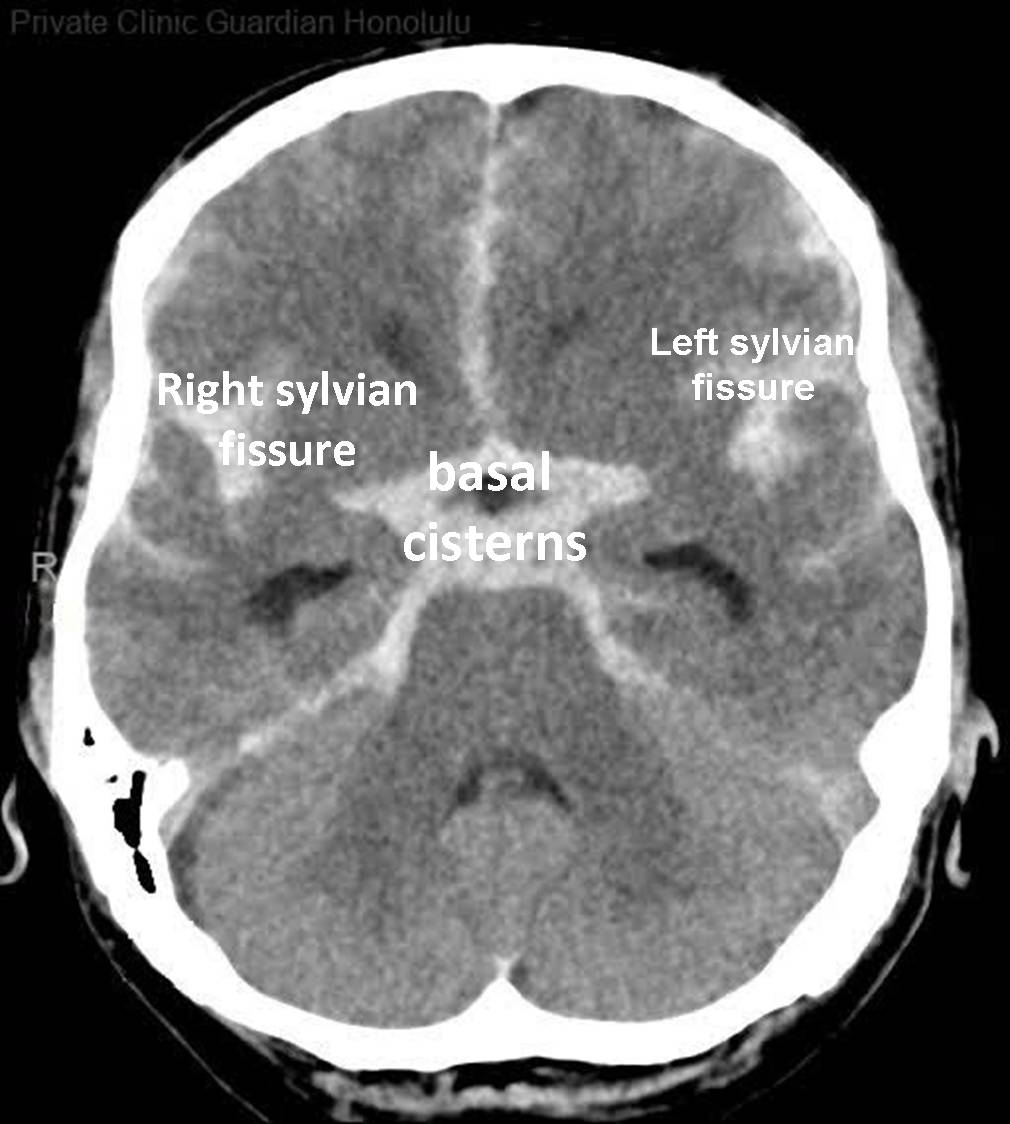
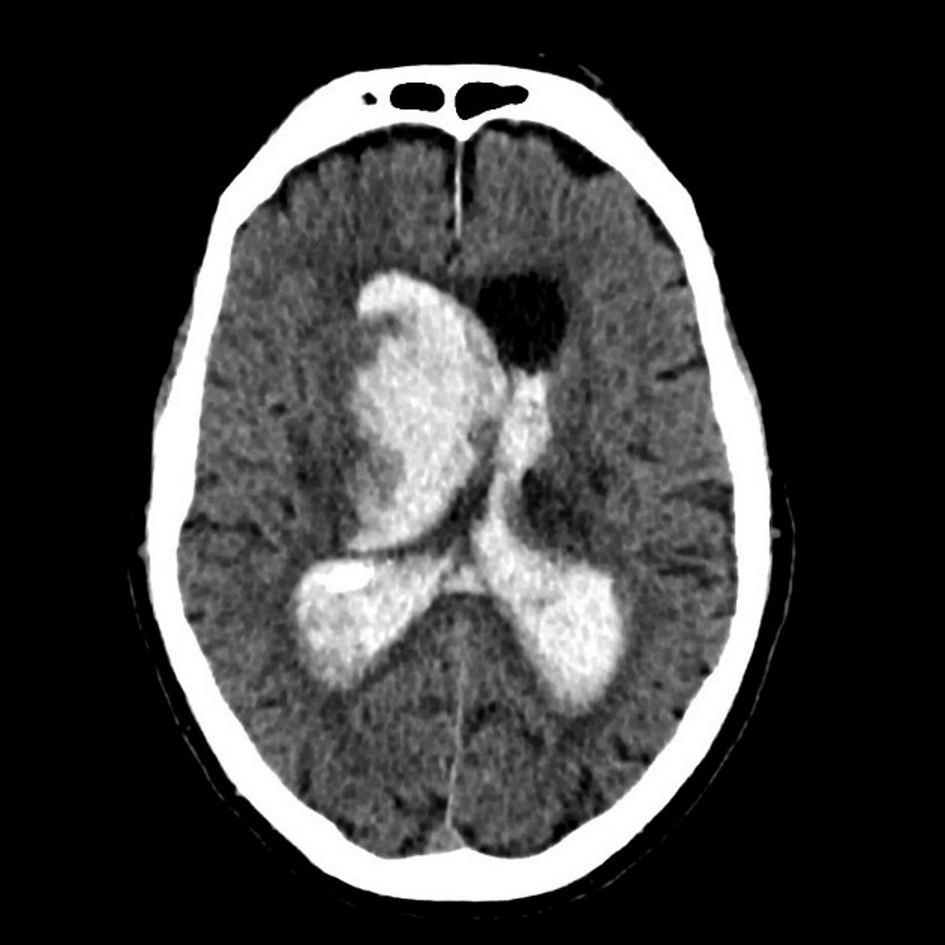
CT features of SAH
‘Dancing man’ around circle of willis
Hyperdense in basal cistern, lateral fissues, L and R sylvian cistern
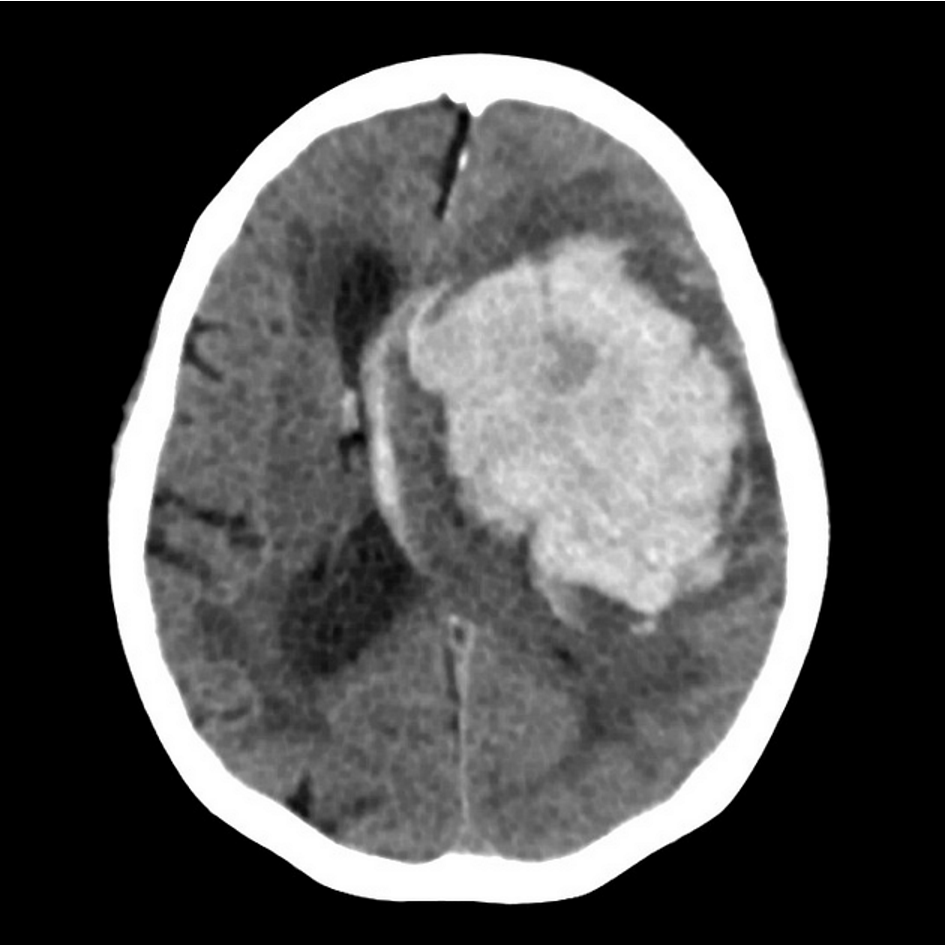
CT features of intracerebral haemorrhage
Blood within cerebral hemispheres
Hyperdense (acute)
CT of intraventricular haemorrhage
Assessment of head trauma
ABC’s (airway, breathing, circulation)
GCS
Head-to-toe examination
Neurological exam: CN’s, motor and sensory function, reflexes
Blood tests: including INR and PT
Monitor overnight
Eye response score in GCS
4: open spontaneously
3: response to sound
2: response to pressure
1: no response
Verbal response in GCS
5: oriented
4: confused
3: words
2: incomprehensible sounds
1: no response
Motor response in GCS
6: obeys commands
5: localised response
4: normal flexion
3: abnormal flexion (decorticate)
2: extension (decerebrate)
1: no movement
AVINDICATED-PI
Anoxic
Vascular
Infection/ inflammation
Neoplastic
Degenerative
Intoxication
Congenital
Autoimmune/ allergy
Trauma
Endocrine
Dietary
Psychiatric
Iatrogenic
Phenytoin (drug class + MOA + indications + ADR’s + caution)
Drug class: anti-epileptic
MOA: blocks vg Na+ channels and stabilises excitatory neuronal membranes. This suppresses repetitive neuronal discharges which generate seizures. Speficially, inhibits the positive feedback loop that results in neural propagation of high frequency action potentials.
Indications: focal and generalised seizures in epilepsy, status epilepticus
ADR’s: vertigo, ataxia, nystagmus
Caution: narrow TI- monitor dosage, hypoalbuminemia, Stocks-Adams syndrome
Valproate (drug class + MOA + indications + ADR’s + caution)
Drug class: anti-epileptic
MOA: increases number of vg Na+ channels in inactivated state, as well as increasing brain concentrations of GABA (an inhibitory nurotransmitter). This suppresses neuronal discharges which generate seizures
(specifically increases GABA by inhibiting succinic semialdehyde dehydrogenase, which thus increases succinic semialdehyde which then reduces GABA metabolism)
Indications: epilepsy, BPD, migraine prophylaxis
ADR’s: stomach ache, diarrhoea, weight gain
Cuations: avoid in pregnancy
Diazepam (drug class + MOA + indications + ADR’s)
Drug class: benzodiazepine
MOA: act as positive allosteric modulator to increase the effect of GABA on GABA-A receptors. These are inhibitory neurotransmitters which suppress electrical activity in the brain which generate seizures. Specifically, binds allosterically between gamma and alpha subunits on GABA-A receptor Cl- ion channels, thus increasing frequency of Cl- channels opening and causing hypopolarisation and reduced excitation of the cell
Indications: insomnia, status epilepticus (first choice)
ADR’s: dorwsiness, decreased alertness, ataxia, agitation in elderly
Monro-Kellie hypothesis
The sum of the volumes of the brain (brain + blood + CSF) is constant, thus an increase to any 1 component results in raised ICP
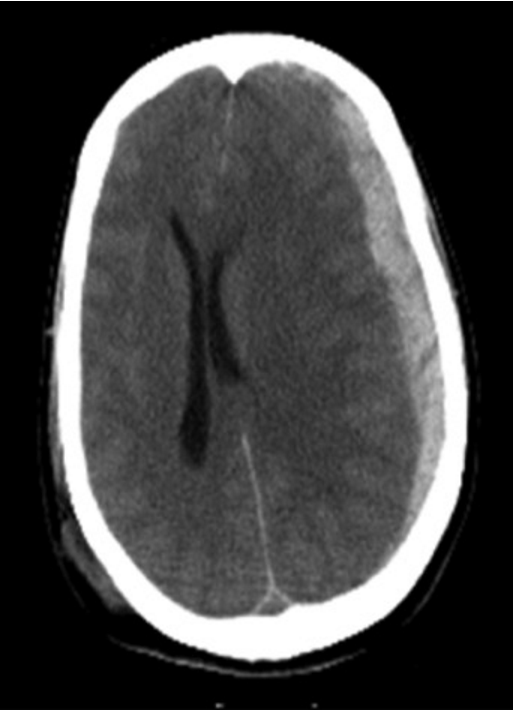
CT feautres of raised ICP
MIdline shift
Venitrcular compression
Narrow sulci and wider gyri
Signs + symptoms of raised ICP
Headache
Confusion
papilledema
nausea
Symptoms of herniation
Signs of meningeal irritation (neck stiffness, photophobia, +ve Kernig’s or Brudzinski sign)
Abnormla posturing (Decroticate or decerebrate)
Valsalva manoeuvre + effect on ICP
Method used to slow HR and clear ears
close mouth and block nose, and forcefully exhale against closed airway for 10s
temporarily increases ICP by raising intrathoracic pressure, reducing venous circulation and cerebral perfusion (and causing venius congestion)
Risk of unacceptable badness (RUB)
The likelihood of a patient surviving a severe head injury but being left severely disabled, a condition which they would find unacceptable
Substantial benefit
An outcome that now or in the future the patient would consider worthwhile
ROSIER scale
Used to assess the possibility of stroke
>0: stroke possible
0 or less: stroke unlikely
ABCD2 score
Used to assess the risk of stroke after TIA
0-3: low risk
4-5: moderate risk
6-7: high risk
Signs of stroke
Fluent/ non-fluent aphasia
Dysarthria (slurred speech)
Hemiparesis
Signs of UMN lesion
Loss of sensation one one side
Facial droop
CT features of ischaemic stroke
Infarct appears hypodense on side of lesion

Pathophysiology of ischaemic stroke
Occlusion of a cerebral artery (ACA, PCA, MCA) caused by thrombosis of embolism
Treatment of ischaemic stroke
Stabilisation: maintain airways (venilator, endo-tracheal tube), oxygen if needed, monitor glucose, BP hydration
If <8 hours: alteplase + mechanical thrombectomy
Aspirin/ clopdogrel after 24hrs of alteplase administration
Management of cormorbidities (e.g. AF, MI, HTN, diabetes)
Phsyiotherapy, OT, speech therapy
CT features of haemorrhagic stroke
Hyperdense at site of haemorrhage
Hypodense around site
Mass effect (e.g. midline shift, herniation)

Pathophysiology of haemorrhagic stroke
Hypertensive cerebrovascular disease causing hylaine arteriosclerosis and occlusion/ rupture of BV
rupture of saccular aneurysm causing SAH
Treatment of haemorrhagic stroke
Stabilisation: airways (venilator or endo-tracheal tube if needed), oxygen if needed, monitor BP, glucose, hydration
Surgical evacuation: clip or coil aneurysm
Reverse anticoagulant medications if taken
Aspirin (drug class + MOA + indications + contraindications)
Drug class: antiplatelet
MOA: non-selective COX inhibitor which reduces TXA2 production in the lifetime of platelets. This inhibits platelet aggregation and thrombus formation
Indications: prevention of thrombo-embolic events in CVD
Contraindications: Reye’s syndrome, haemorrhage, gastric ulceration
Clopdigrel (drug class + MOA + indications + ADR’s)
Drug class: antiplatelet
MOA: non-competitvely blocks ADP P2Y receptors, preventing ADP from binding and activating GPIIb/IIIa, thus reducing platelet aggregation
Indications: prevention of thrombo-embolic events in CVD
ADR’s: haemorrhage, abdominal pain, headache, dizziness, paraesthesia
Diltiazem (drug class + MOA + indications + ADR’s)
Drug class: calcium channel blocker
MOA: inhibits Ca2+ during membrane depolarisation of primarily cardiac vascualr smooth muscle
Indications: anti-arrhythmic in AF, angina, reverse coronary vasospasm
ADRs: bradycardia, AV block, palpitation, dizziness, hypotension
Warfarin (drug class + MOA + indications + contraindications)
Drug class: anticoagulant
MOA: competitively blocks heparin vitaminK epoxide reductase in liver to prevent vitamin K recycling and synthesis. This prevents activation of clotting factors X, IX, VII, II (and protein C and S) to prevent thrombus formation
Indications:stroke prevention in CVD, prosthetic heart valves
Contraindications: haemorrhage, pregnancy
Dabigatran (drug class + MOA + indications + contraindications + emergency reversal)
Drug class: DOAC
MOA: directly inhibits thrombin, thus preventing thrombus formation
Indications: stroke prevention in CVD
Contraindications: haemorrhage, prosthetic heart valves
Emergency reversal: idarucizumab
CHA2DS2VASc score
Used to assess risk of stroke in AF and management
Congestive heart failure: 1
Hypertension: 1
Age (75+): 2
Diabetes mellitus: 1
Stroke, TIA previously: 2
Vascular disease: 1
Age (65-74): 1
Sex category (female): 1
Consider offering anticoagulants if 1+ in males and 2+ in females
Effect of pre-eclampsia on ICP
Causes rapid hypertension during pregnancy which can cause brain oedemad thus raised ICP. This can lead to cerebral or CN damage
Cushing’s triad
Late stage raised ICP after head injury
Hypertension
Bradycardia
Irregular respiration
Severity of TBI according to GCS
Mild TBI: 13-15
Moderate TBI: 9-12
Severe TBI: ≤8
Legal documents protecting workers rights
Accident compensation corporation 1972
Health and safety at work act 2015
Health and Safety in employment act 1992
Pathophysiology of epidural haematoma
Tearing of a middle meningeal artery following a fracture in the temporal bone forming a rapidly expanding haematoma
Pathophysiology of sbdural haematoma
Milder repeated trauma puts pressure on bridging veins leading to eventual tearing, more common in elderly patients with cerebral atrophy (as greater space and thus traction on veins)
Criteria for determingin brain death
GCS 3
No brainstem reflexes (e.g. pupil constriction, VOR)
No venilatory effort
2 sets of tests at least 2 hours apart (4 tests total) by 2 different physicians
How does SAH cause hydrocephalus?
Blood and inflammation block CSF drainage into arachnoid granulations
CSF cannot flow into next chamber and accumulates in ventricles
Raised ICP - monro-kelli hypothesis causing displacement of brain tissue in response
PERRLA
Pupils equally round, reactive to light and accomodation
Why should morphine not be administered in stroke?
Causes hypotension and sedation - can mask the effects of decrease in LoC
CNS depressant causing respiratory depression: can cause hypercapnia which reduces CBF and thus raised ICP
Culminative effects of morphine with other treatment medications
Types of radiological imaging
CT
MRI
Diffusion-weighted imaging (DWT)
angiography
perfusion scan
PET scan
What causes hypodense appearance on CT?
Water-like densities of tissue resulting in reflection of x-rays
Causes of hypercoagualability
Oral contraceptive pill (contains estrogen)
prolonged immbolisation (e.g. long haul flight) promoting decreased venous return and stasis
Low fluid intake (decreases circulatory volume)
Most common cause of trauamtic SAH?
Rupture of vertebral artery via blunt force trauma to the neck
Process of examining CT scan (Blood Can Be Very Bad)
Blood
Cisterns
Brain
Ventricles
Bone