IMED1001 - ANS 2 (Wk 12)
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
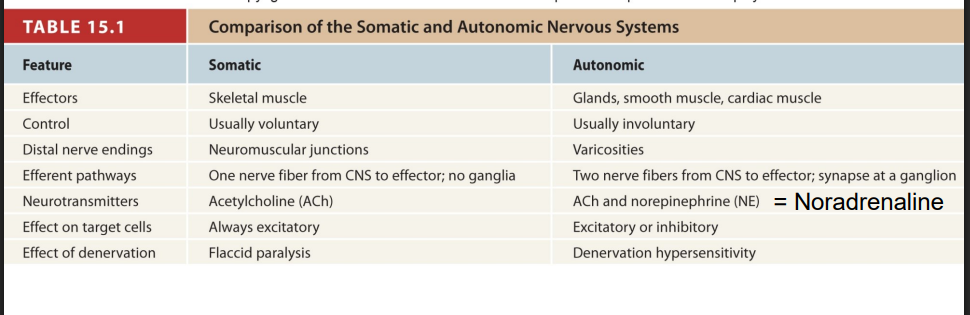
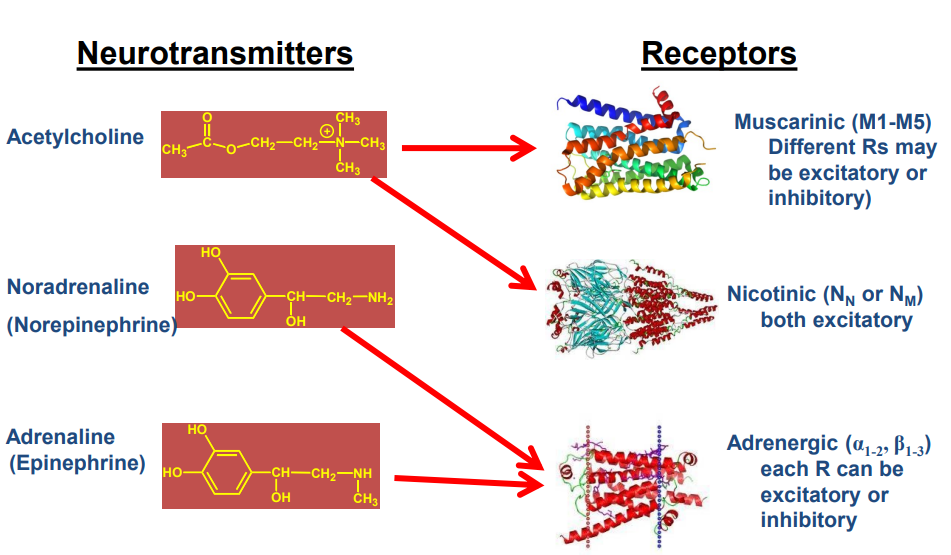
Mediators of Autonomic Response
Noradrenaline/Adrenaline (NA/A) and acetylcholine (ACh)
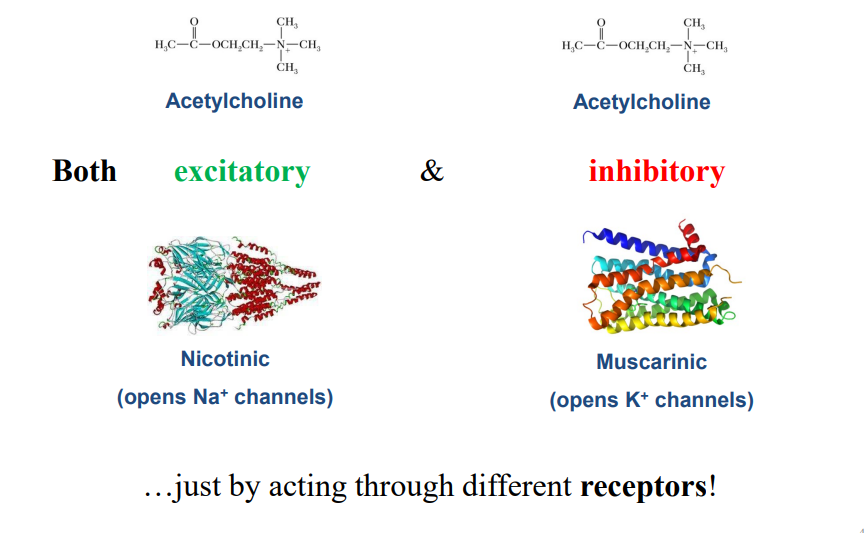
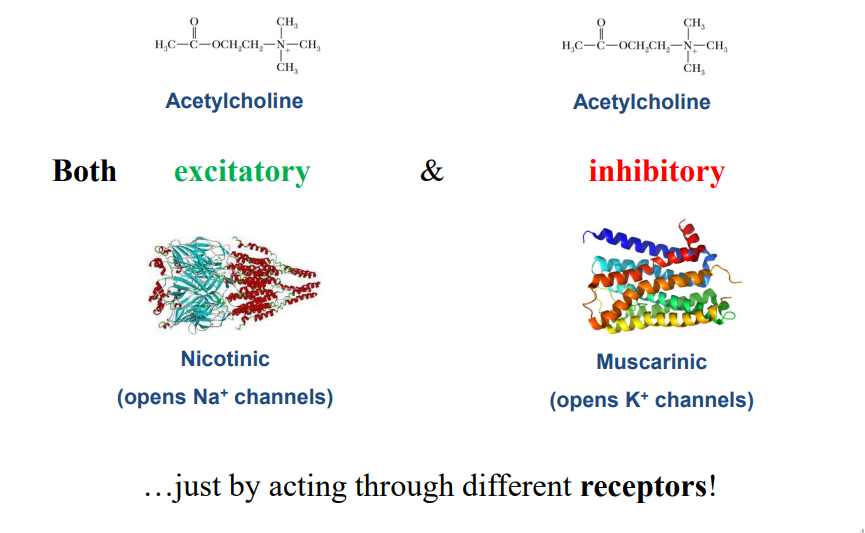
The same neurotransmitter can be
fast (ionotropic), or slow (metabotropic)
- can be excitatory or inhibitory depending on the receptor
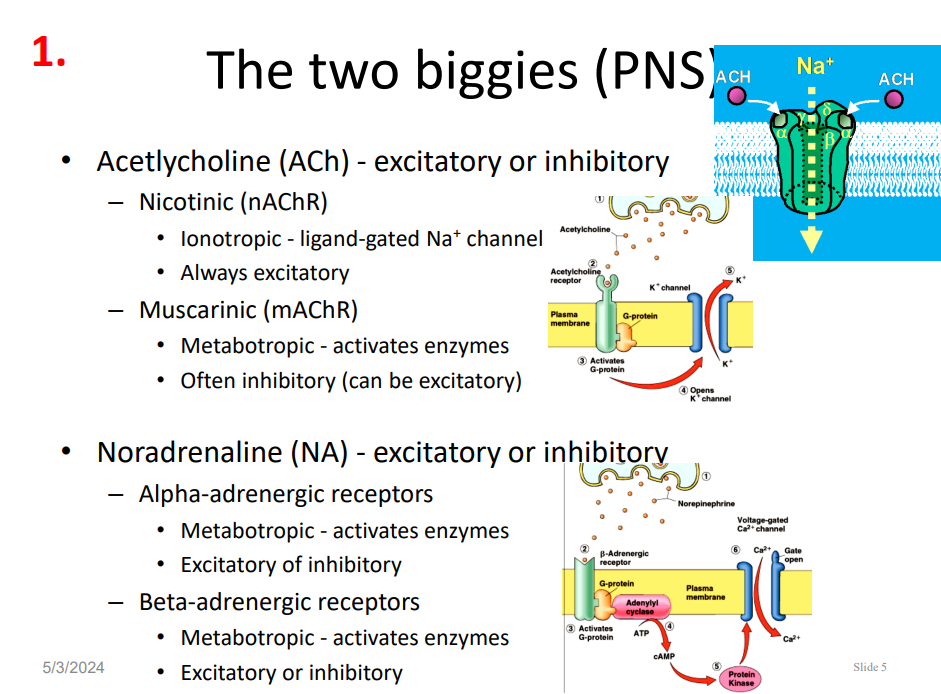
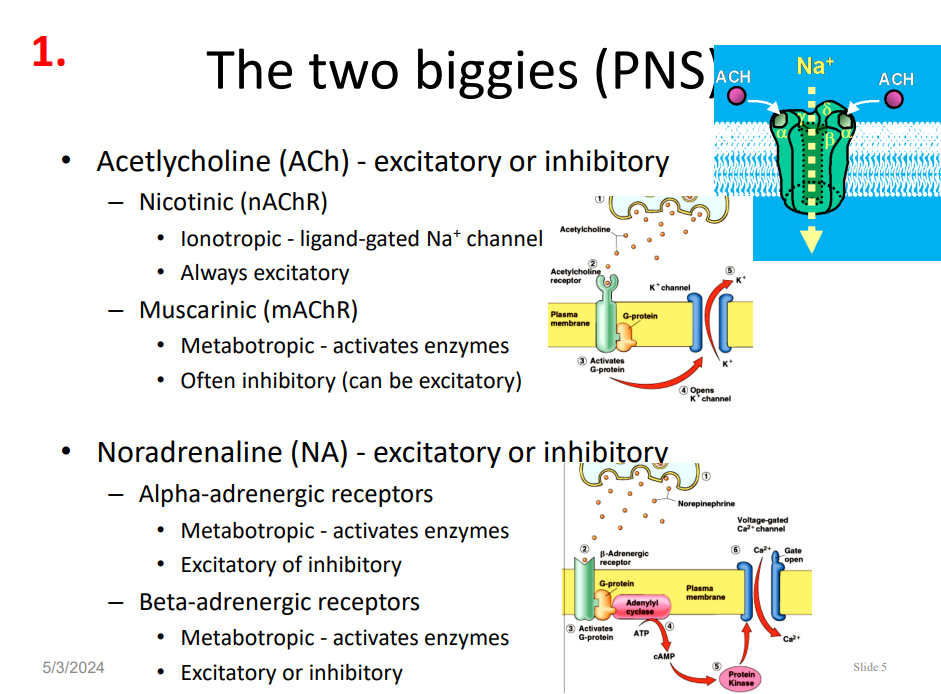
PNS Neurotransmitters
ACETYLCHOLINE (ACh) - excitatory or inhibitory
- Nicotinic: (nAChR): ionotropic - ligand-gated Na+ channel, always excitatory
- Muscarinic (mAChR): metabotropic - activates enzymes (often inhibitory, can be excitatory)
NORADRENALINE (NA): excitatory or inhibitory
- Alpha-adrenergic receptors: metabotropic - activates enzymes and can be excitatory or inhibitory
- Beta-adrenergic receptors: metabotropic - activates enzymes, can be excitatory or inhibitory
Nervous System we use to control skeletal muscle
is as quick as it can possibly be, quick means fewest number of synapses
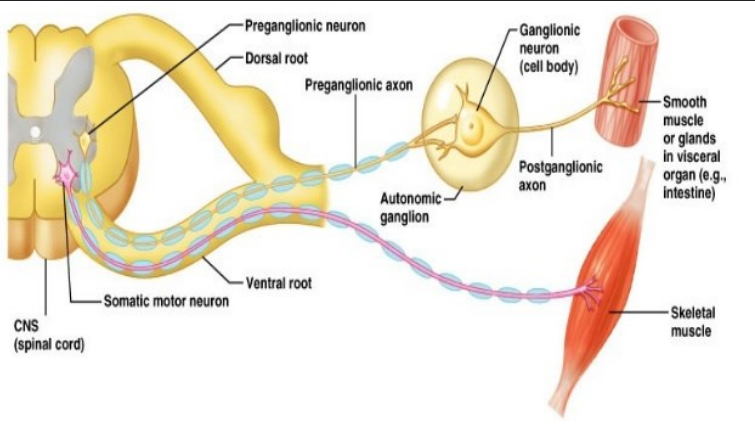
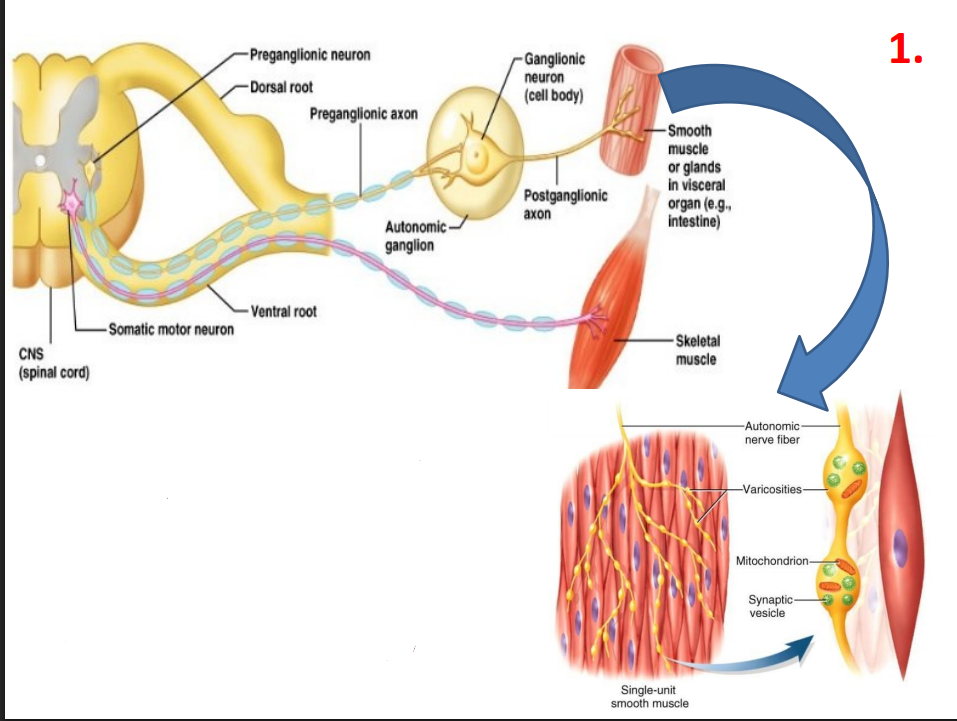
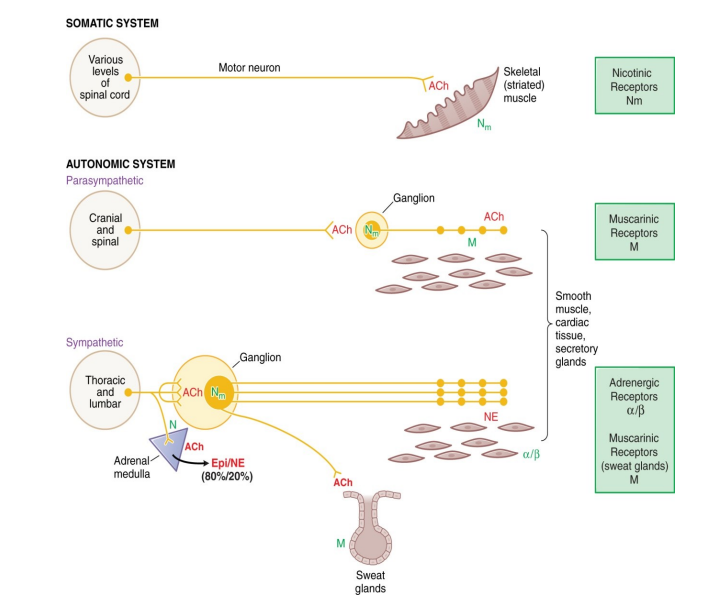
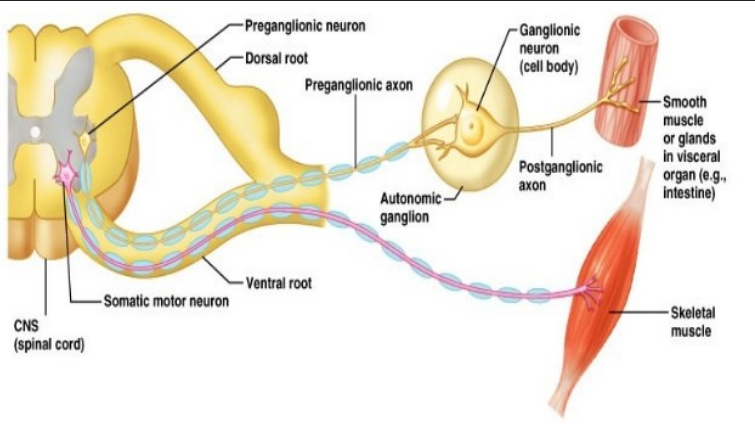
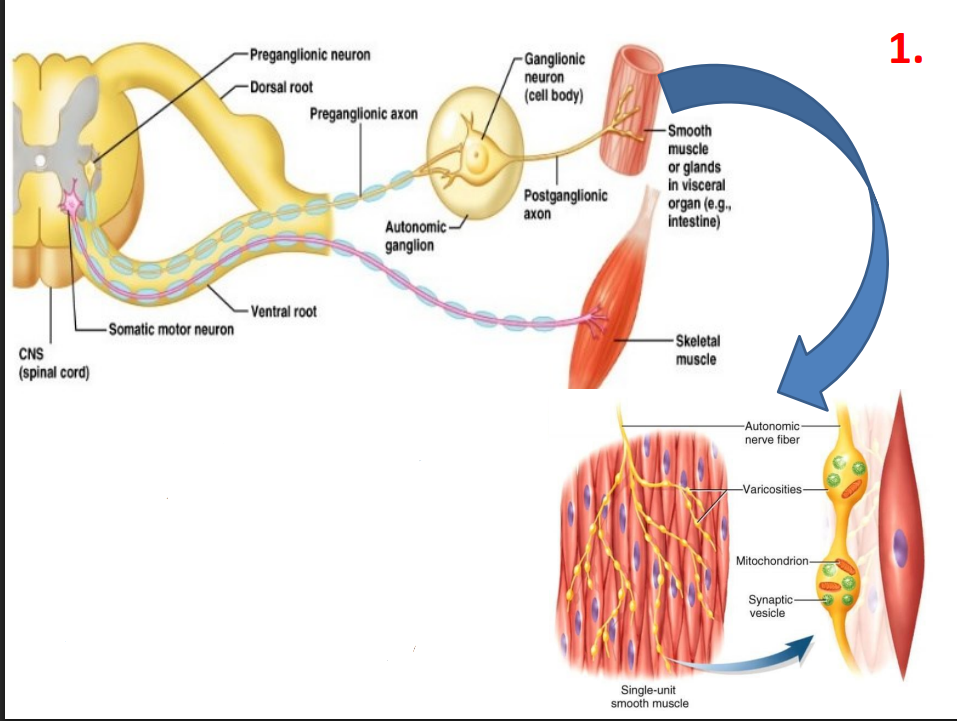
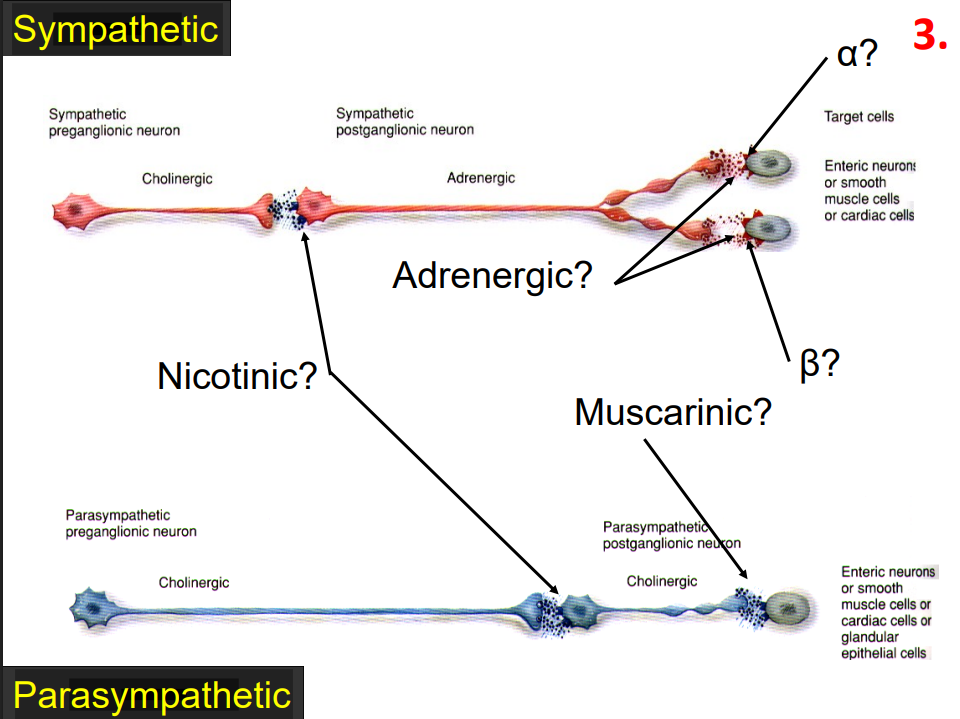
ANS Path
- doesn't need to be that fast, actually needs more coordination
- two neurons from CNS to effector
- "Ganglion" = a collection of nerve cell bodies outside the CNS
- Preganglionic neuron cell body is in CNS
- Postganglionic neuron cell body is in a ganglion
- Preganglionic neuron is myelinated (= fast)
- Postganglionic neuron is unmyelinated (=slow)
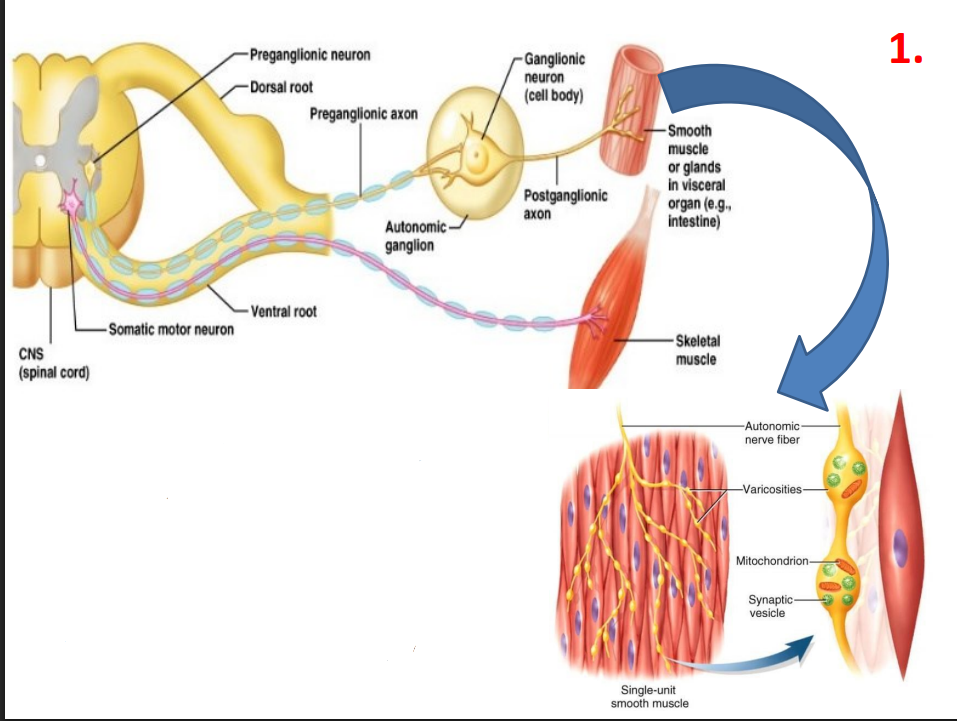
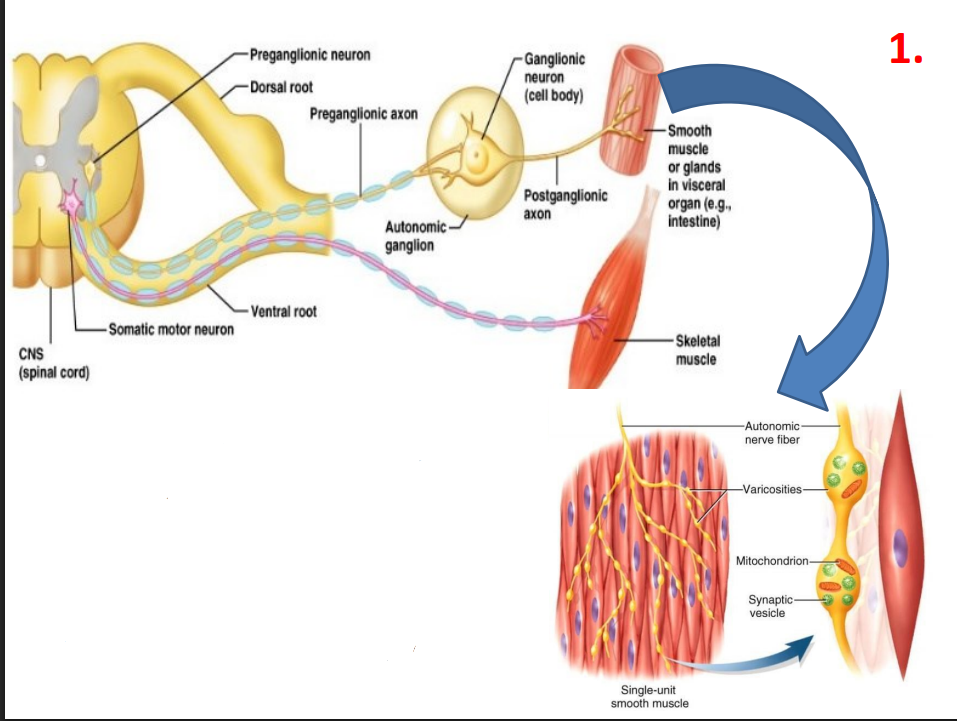
Postganglionic ANS nerves releases effector NTs via varicosities
- not discrete like NMJs, spread more NT around, prolonged + subtle response (NTs diffuse to other cells)
- basically what hes saying is that cardiac muscle does not have a NMJ meaning it instead gets decorated by acetylcholine or noradrenaline from ANS
- basically what happens is the ends of the neurons become like sprinkler systems where the ends of the nerves sprinkle out neurotransmitters to the muscle. the ends of these nerves are called variscosities
- allows us to cut down on the number of nerves we need to innervate
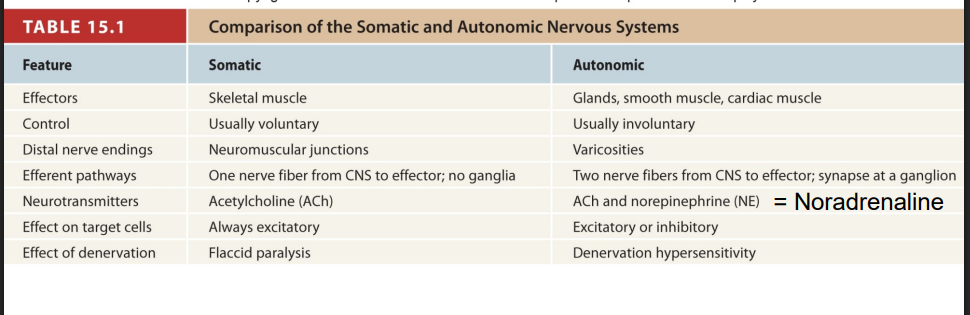
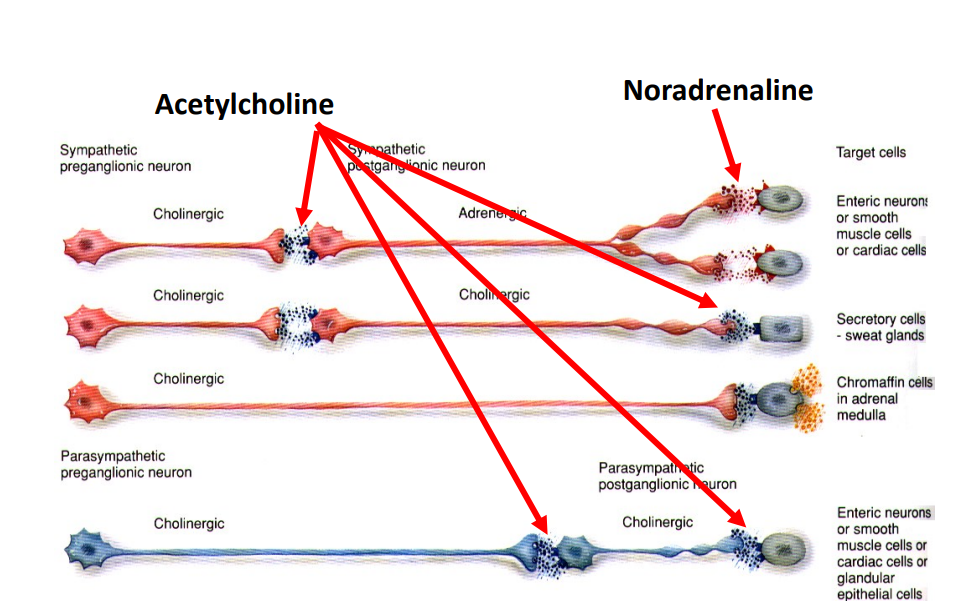
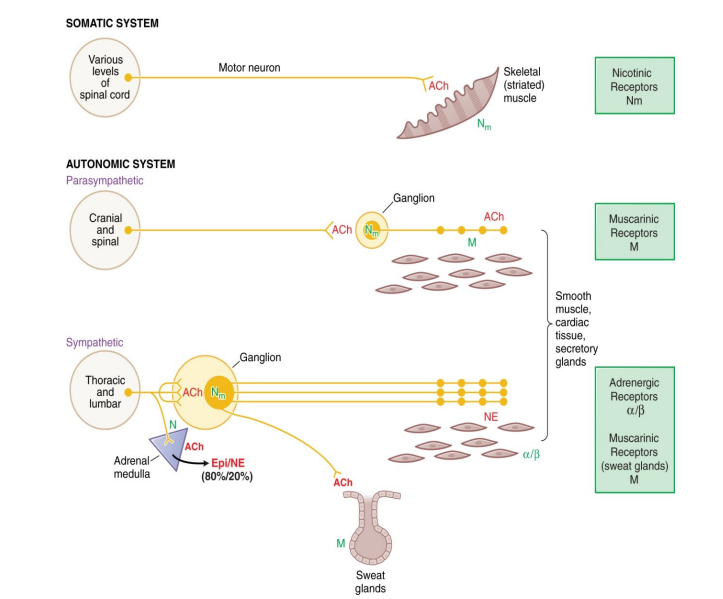
Autonomic Output Pathways
should know everything except last line
Characteristic Differences between sympathetic and parasympathetic divisions (NAMING ONLY)
Different Effector (BIG ONE), Leave SC at different sites, sympathetic controls endocrine system
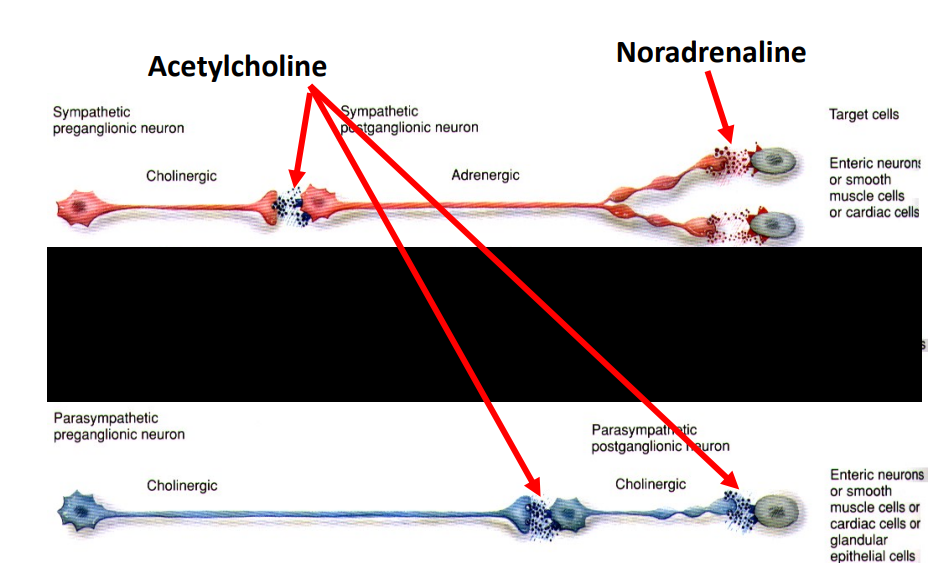
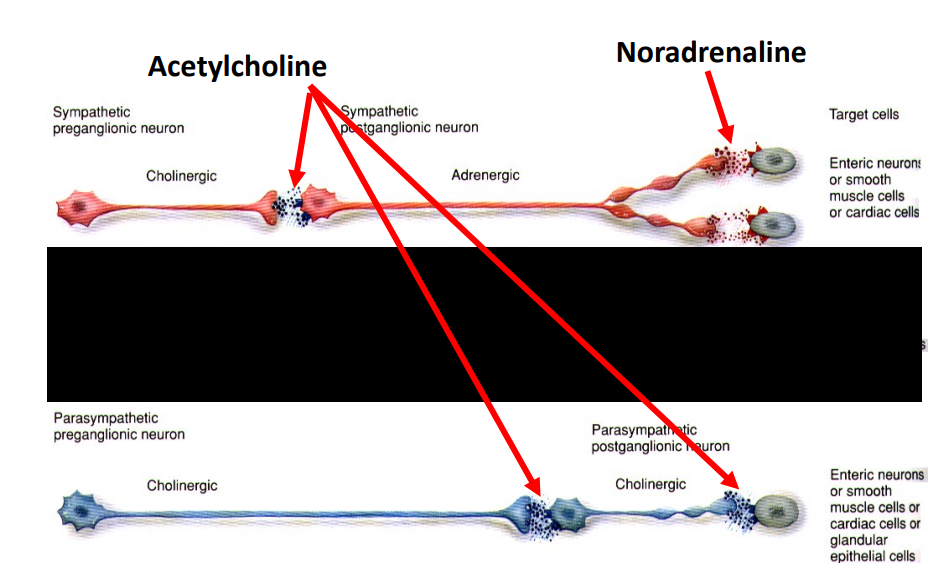
1st Difference: Different Effector (Postganglionic) NTs
- Sympathetic: NA/A (aka catecholamines)
- Parasympathetic: ACh
- both of them use acetylcholine as the neurotransmitter at their ganglionic synapse
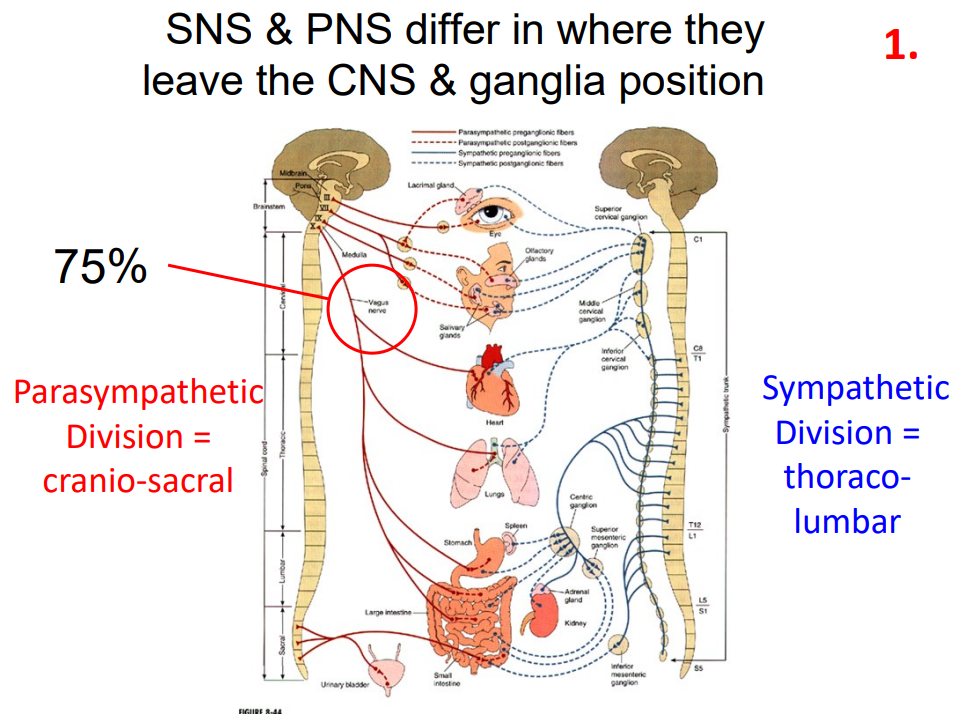
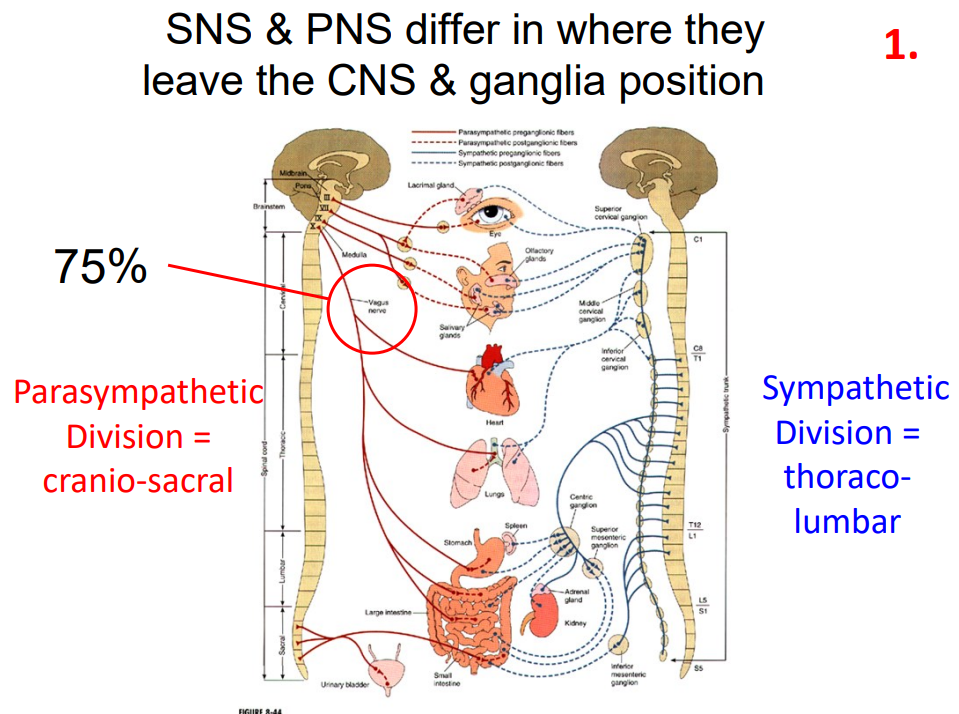
2nd Difference: Anatomical Differences (Leave SC at different sites, different locations of ganglia)
- Parasympathetic: cranio-sacral, ganglia near organs
- Sympathetic: thoraco-lumbar, ganglia near Spinal cord (SC)
- thoraco-lumbar means near thoracic and lumbar region
- cranio-sacral means near cranial and sacral (pelvis) regions
- one thing to notice: preganglionic neuron is very short in sympathetic and postganglionic neuron is very long. Opposite in parasympathetic, as shown by diagram
- ganglionic neuron is found on organ on paraympathetic path
3rd Difference: Sympathetic Division also controls endocrine system
ADRENAL MEDULLA:
- Composed of modified sympathetic neurons called Chromaffin cells
- secrete adrenaline (80%) and noradrenaline (20%)
- secreted directly into the bloodstream - a hormone
- slow to act (secretion - travel)
- prolonged response (half life around 2 min, [synapses are cleared within milliseconds]
- activated by preganglionic neurons that come and synapse to chromaffin cells (post-ganglionic)
- this is why you still feel high heart rate. etc. when sympathetic division has stopped acting, because the effects are longer term
![<p>ADRENAL MEDULLA:</p><p>- Composed of modified sympathetic neurons called Chromaffin cells</p><p>- secrete adrenaline (80%) and noradrenaline (20%)</p><p>- secreted directly into the bloodstream - a hormone</p><p>- slow to act (secretion - travel)</p><p>- prolonged response (half life around 2 min, [synapses are cleared within milliseconds]</p><p></p><p>- activated by preganglionic neurons that come and synapse to chromaffin cells (post-ganglionic)</p><p>- this is why you still feel high heart rate. etc. when sympathetic division has stopped acting, because the effects are longer term</p>](https://knowt-user-attachments.s3.amazonaws.com/d5230096-0c02-4da8-bb82-231804bd1e2b.png)
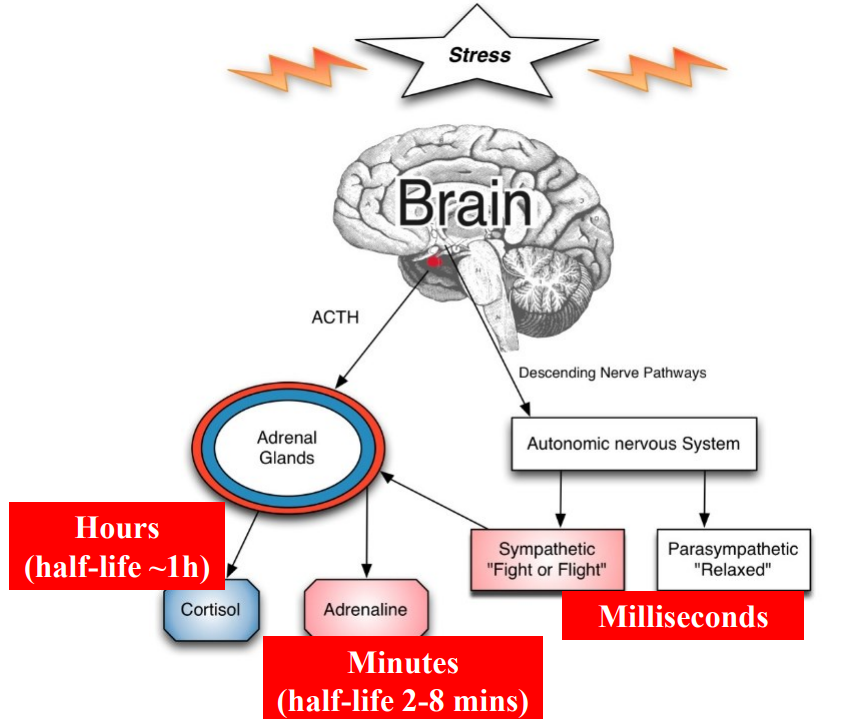
Stress Response Loop
DIAGRAM ON SLIDE 16
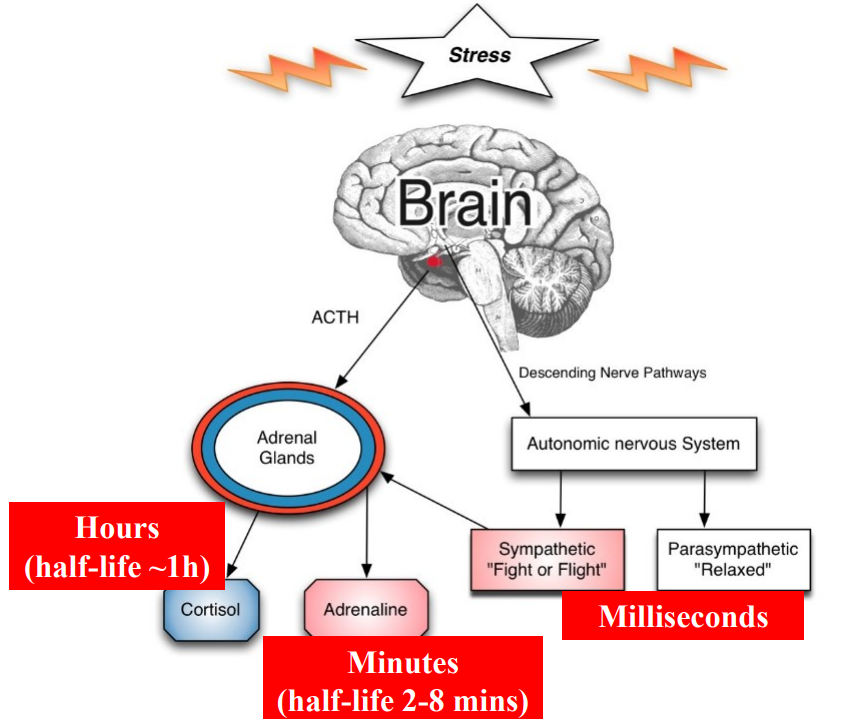
Why do steroid hormones have long term effects
- backbone made from cholesterol
- e.g cortisol lasts for a long time
- cortisol keeps blood nice and full of fats and sugars
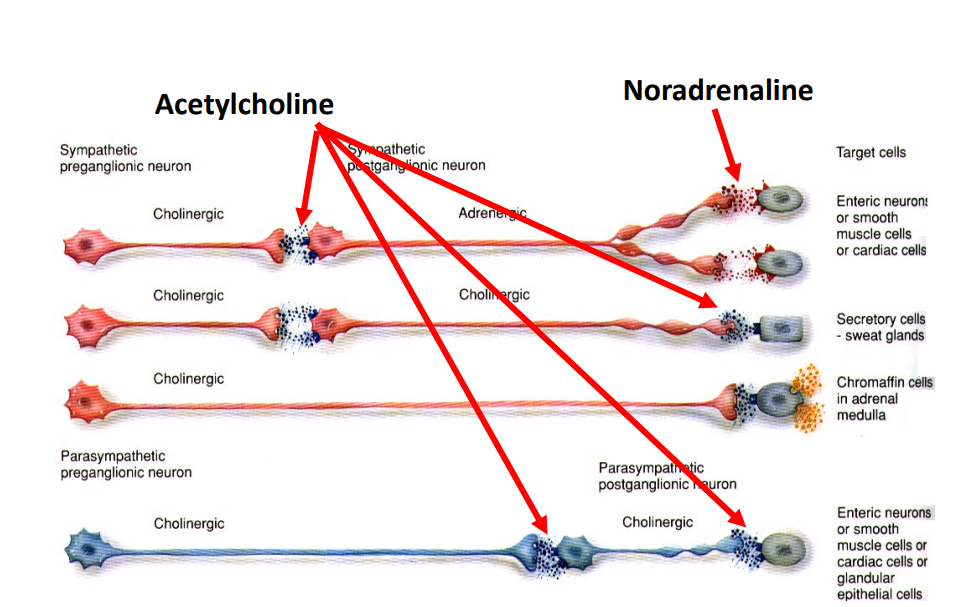
Exceptions
- sweat glands produce acetylcholine at the end as well as start, only exception
- nerve to adrenal medulla is long

Noradrenaline
- Causes constriction in most vascular smooth muscle (as well as vasodilation)
- Causes relaxation of vascular smooth muscle in skeletal muscles
- Causes relaxation of bronchial smooth muscle
- different receptors

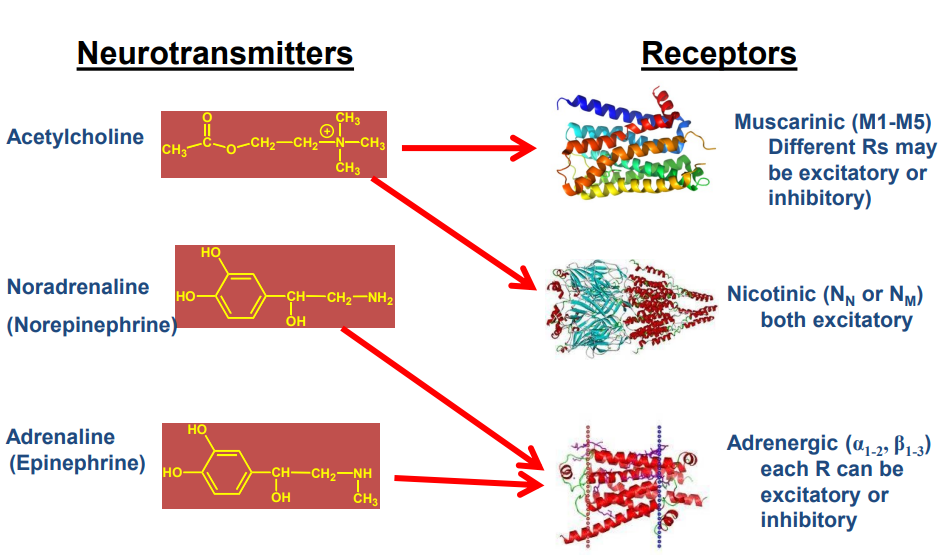
ANS Transmitters and Receivers
- Acetylcholine has Muscarinic (M1-M5) (Different Rs may be excitatory or inhibitory)
- Noradrenaline (Norepinephrine) has Nicotinic (both excitatory)
- Adrenaline (Epinephrine) has Adrenergic each R can be excitatory or inhibitory
Similarities between Parasympathetic and Sympathetic
- all ganglionic syanpses use:
- ACh which binds to nicotinic AChR (ionotropic = always excitatory)
Differences between Parasympathetic and Sympathetic
- Postganglionic syanpses use different Receptors
Parasympathetic:
- all cholinergic, but muscarinic (M1-M5, but we really only care about M2 + M3) (cholinergic means all acetylcholine)
Sympathetic:
- all adrenergic but alpha adrenergic (alpha 1-2) and beta-adrenergic (beta 1-3)
all of these receptors are metabotropic = various effects = generates cell-specific diversity
Postganglionic AChRs
All muscarinic receptors:
- M1, M4, M5 receptors: CNS (not ANS... probably)
- M2 receptors: cardiac = cardiac muscle cells. Inhibitory (IPSP) -> decreases heart rate
- M3 receptors: glands and smooth muscle cells almost always excitatory (via Ca2+) but can also cause smooth muscle relaxation (via NO)
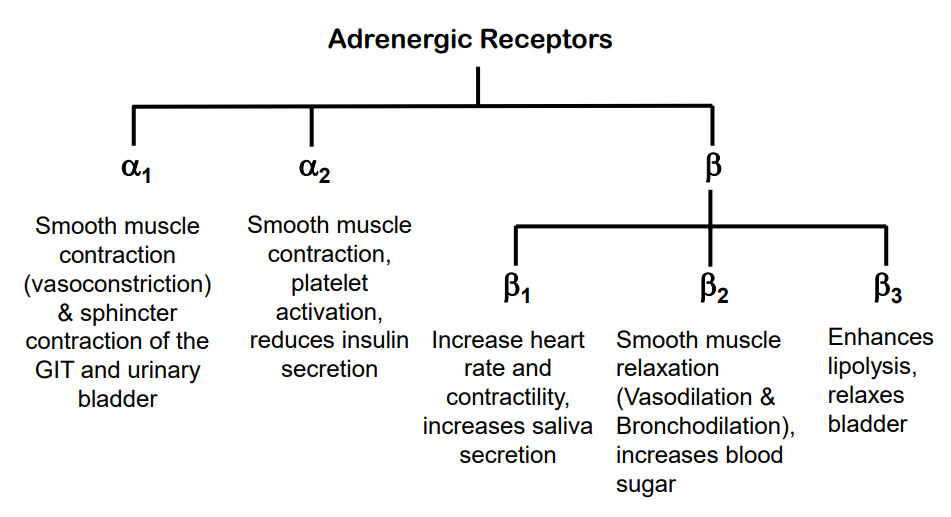
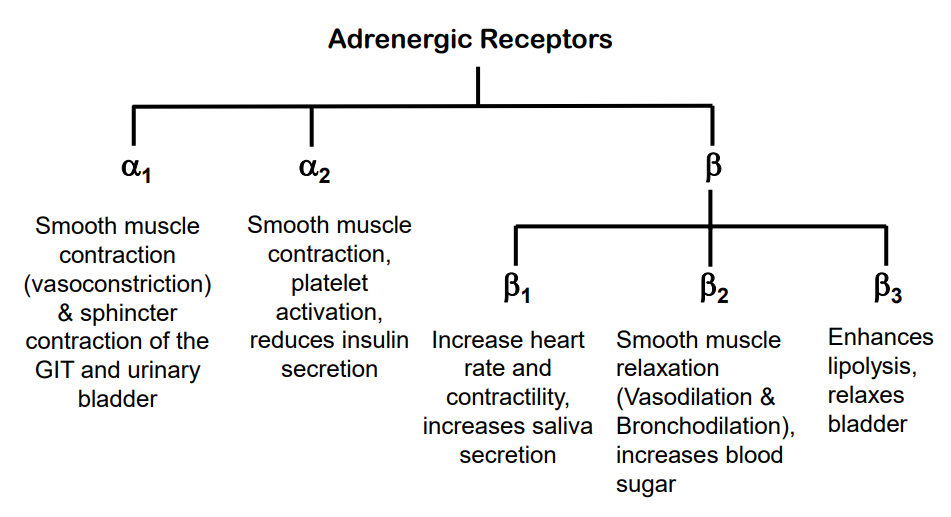
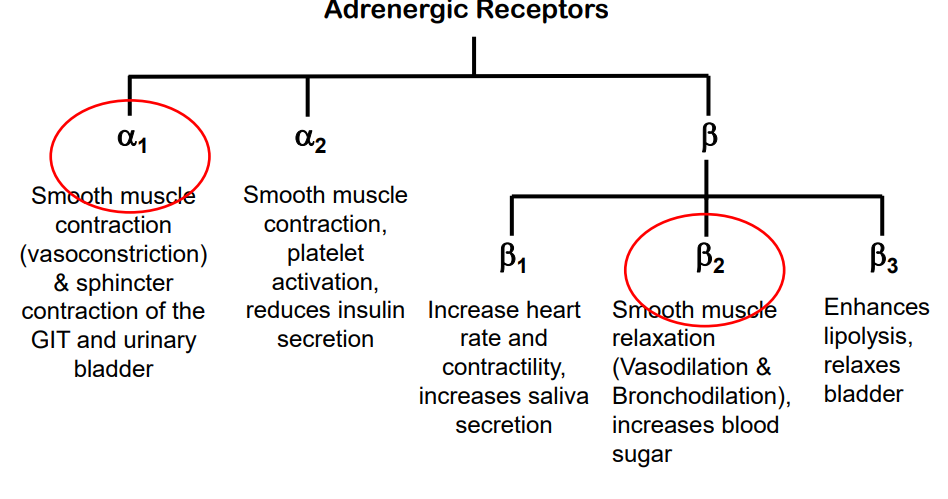
Adrenergic Receptors in ANS
- Adrenergic Receptors:
- alpha 1 and alpha 2
- beta 1, beta 2, beta 3
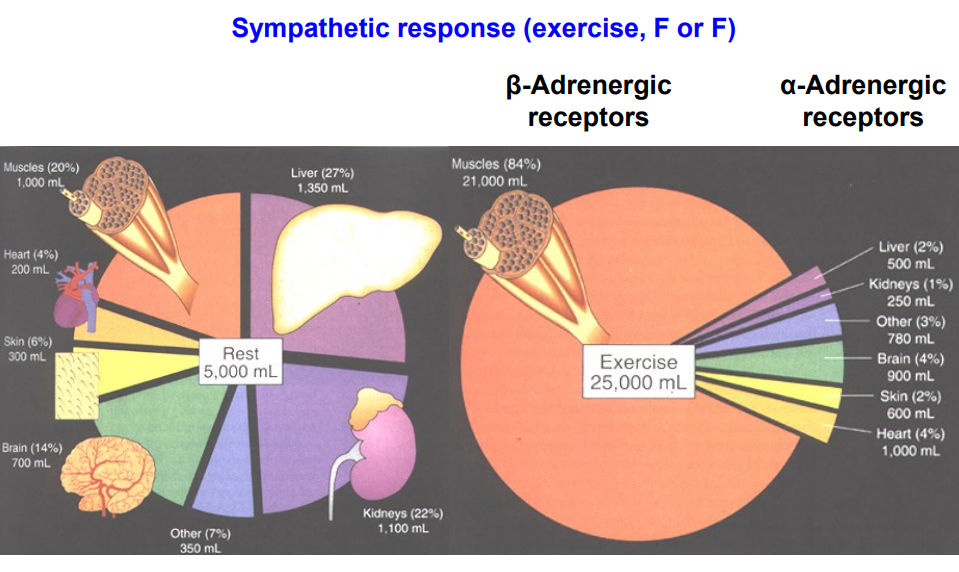
Regulating Blood Distribution
- sympathetic response (exercise, Fight or Flight)
- noradrenaline is binding to alpha adrenergic receptors and those alpha adrenegic receptors are causing vasoconstriction to the areas on diagram where the percentage has gone down
- the only way we can concurrently increase blood flow to other areas is to not have alpha receptors on them. if we dont get alpha receptors on skeletal muscle we dont get vasoconstriction
- we can increase blood flow to skeletal muscle through beta receptors
- whats gonna happen is if you inject someone with adrenaline you'll get vasoconstriction in areas with alpha receptors and vasodilation in areas with beta receptors
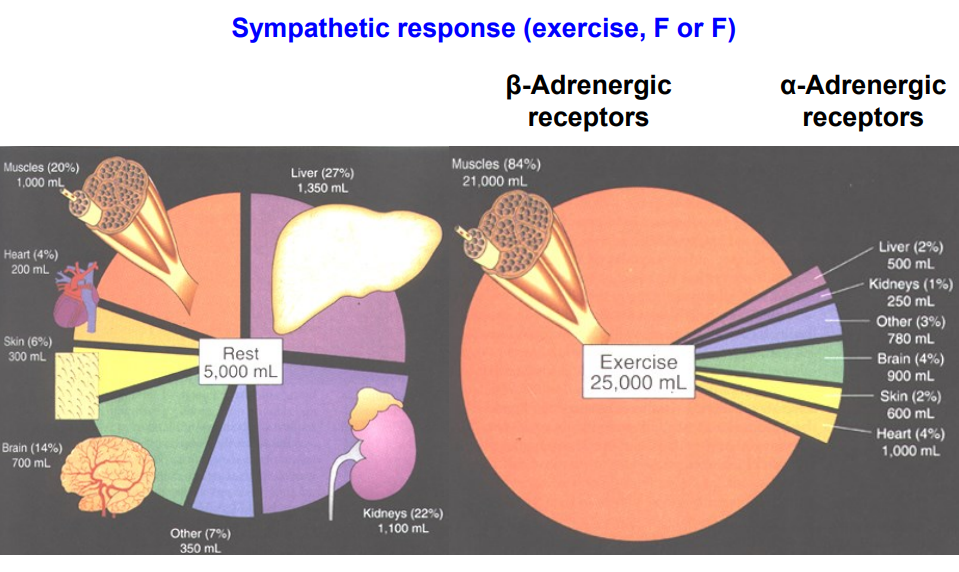
Adrenaline and Noradrenaline bind differently to receptors
- NA is more potent on alpha 1 receptors (instantaneous FF response to increase BP (baroreceptor reflex)
- Adrenaline is more potent on beta 2 receptors (slow but prolonged muscle bed vasodilation and bronchodilation (to fuel and refuel muscles)
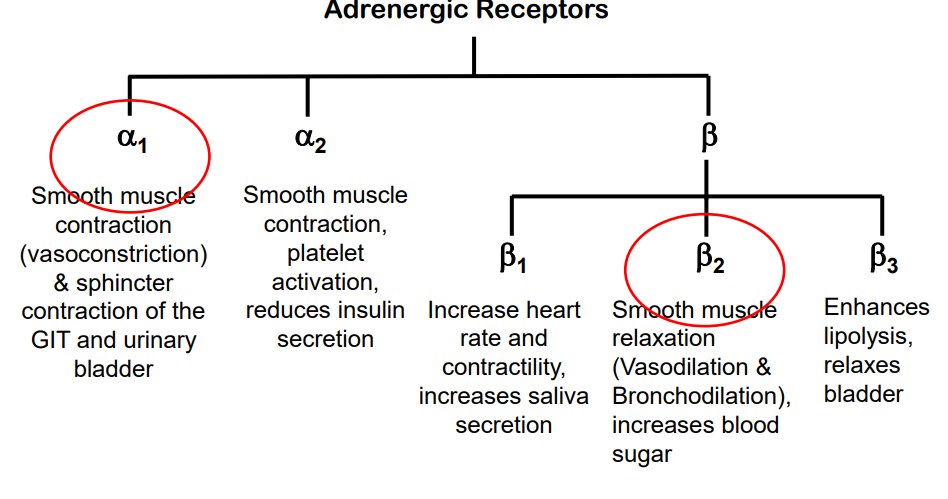
Alpha 1 Receptors
- cause smooth muscle contraction (vasoconstriction) and sphincter contraction of the GIT and urinary bladder
Beta 2 receptors
smooth muscle relaxation (vasodilation and bronchodilation), increases blood sugar
Drugs that Influence the ANS
- mimic or block the effects of the two primary neurotransmitters, Acetylcholine and Noradrenaline/Adrenaline
- drugs that mimic neurotransmitters are referred to as "receptor agonists": these drugs activate receptors
- drugs that block neurotransmitters are referred to as "receptor antagonists": these drugs block receptors
- if we administer acetylcholine it can work where we have acetylcholine receptors
- if we have nicotinic receptors its only going to work on these relay synapses
- if we have drugs that work at muscarinic receptors, they will work there
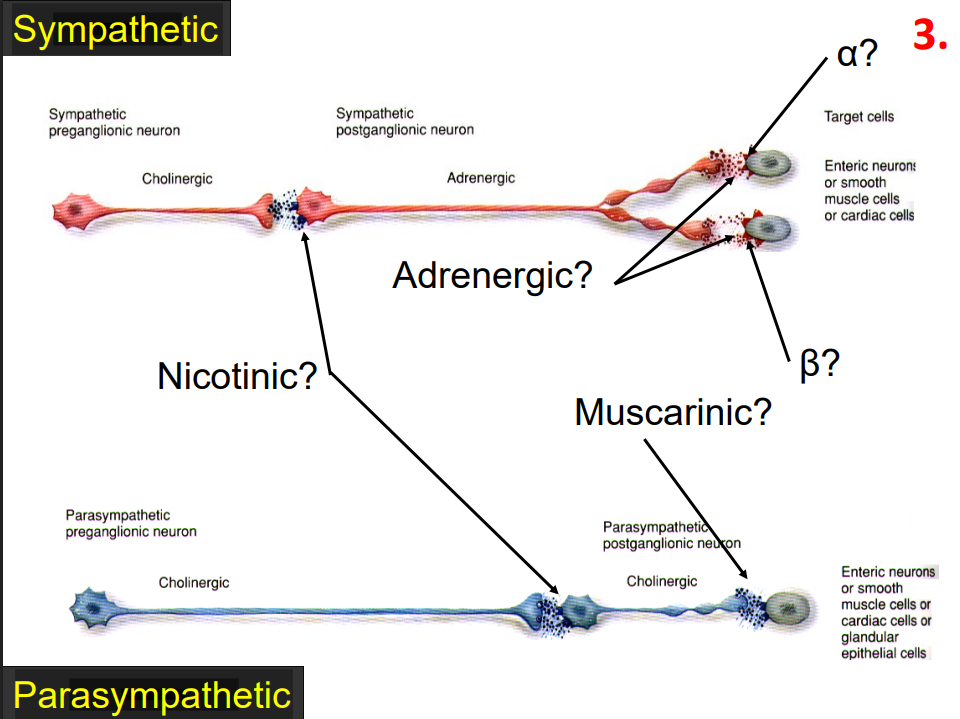
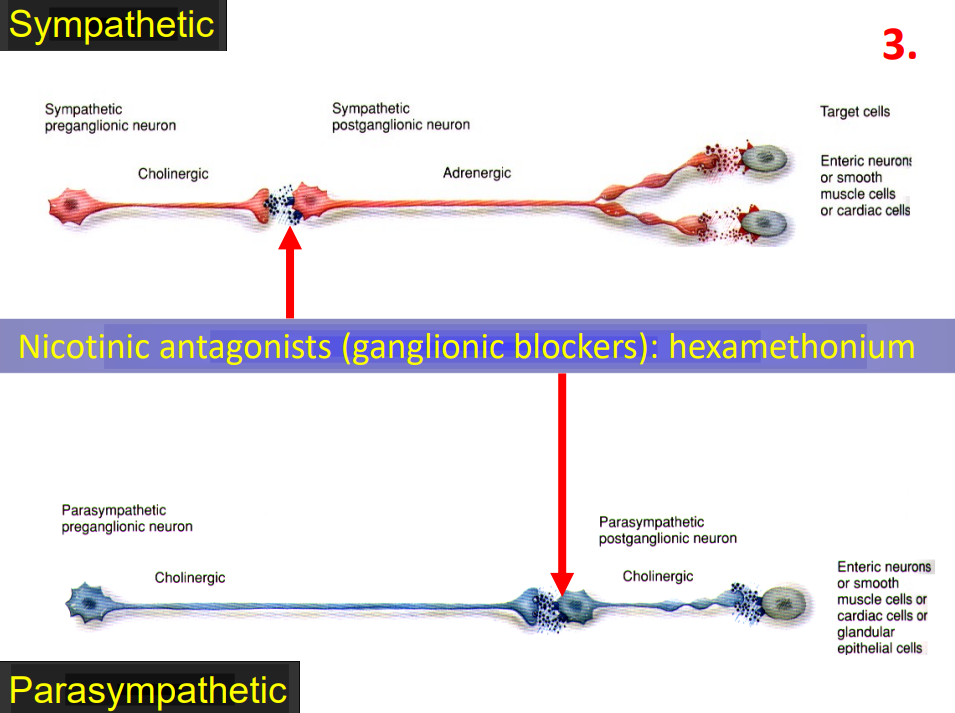
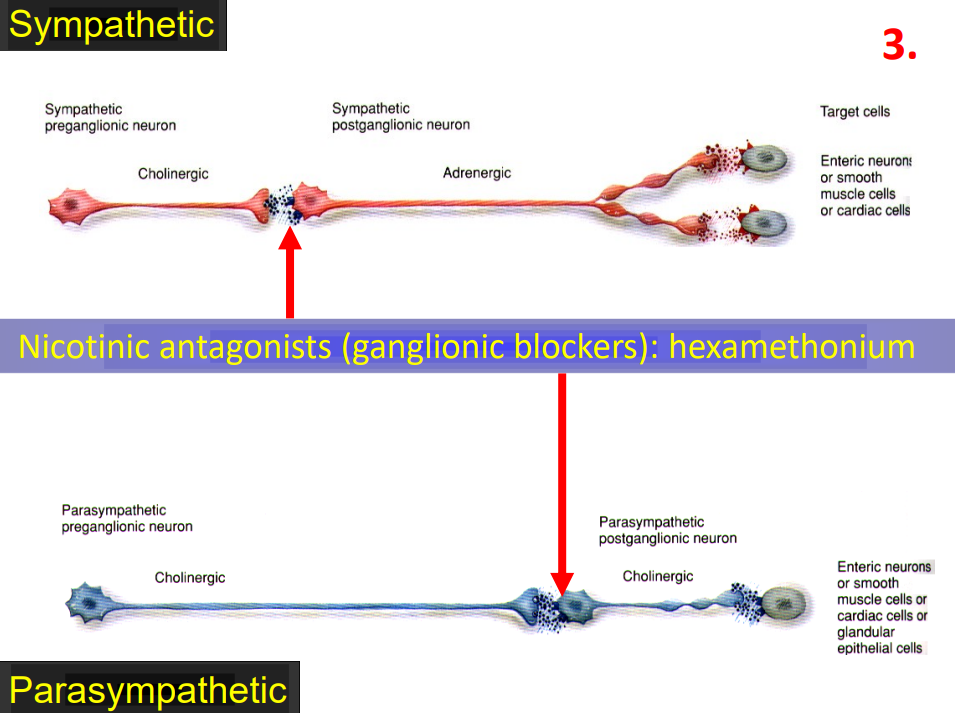
Nicotinic Antagonist
- need to know which synapses are involved, what receptors are being bound, what effect its having
- ganglionic blockers
- if you wanted to poison someone and shut down their ANS, this is the drug of choice
- these bind to nicotinic receptors and they will not allow neurotransmission through these synapses.
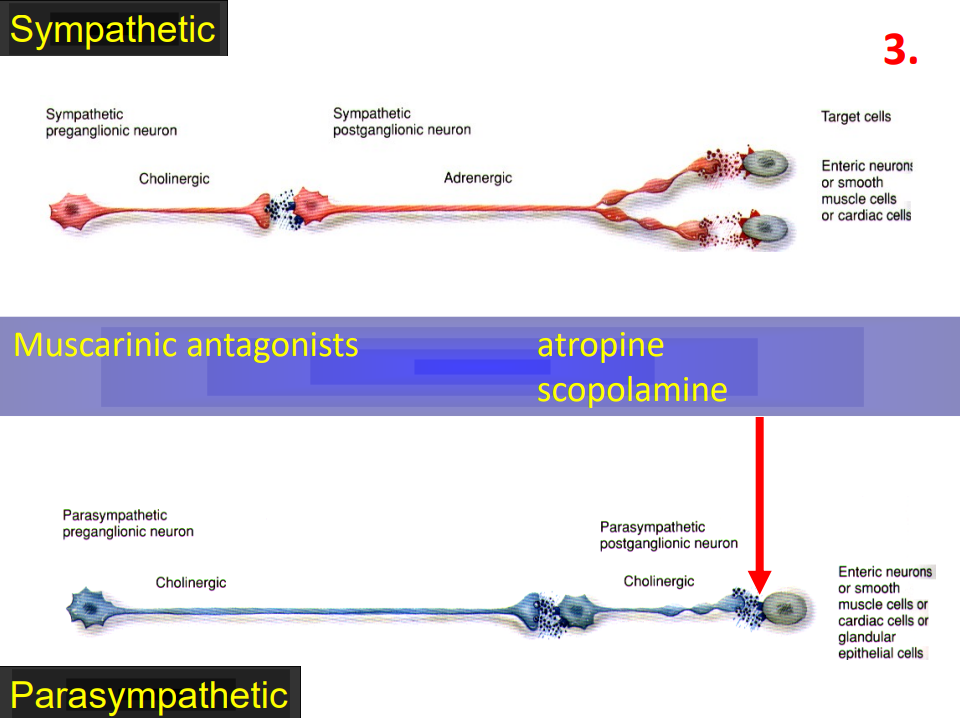
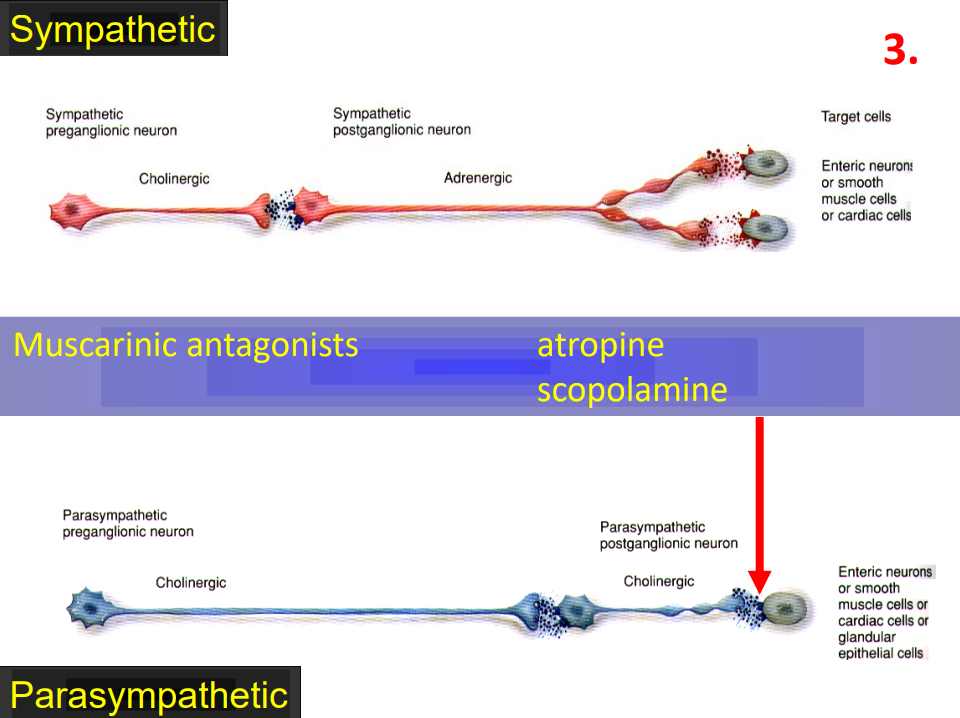
Muscarinic Antagonist
- can have antagonists for different types of acetylcholine receptors
- act by blocking muscarinic receptors on end organ itself
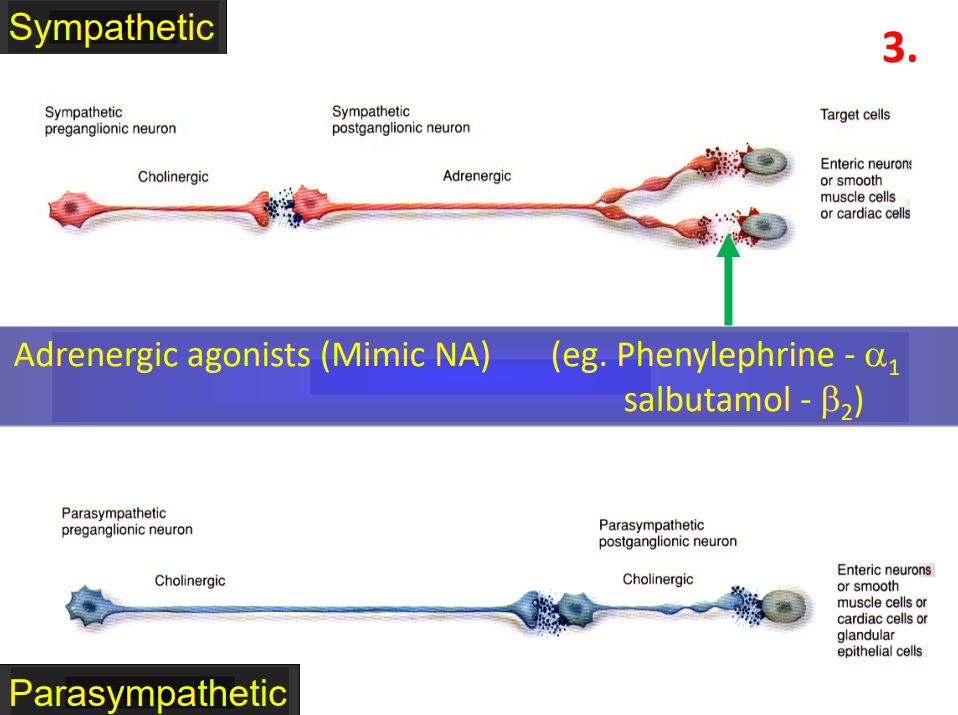
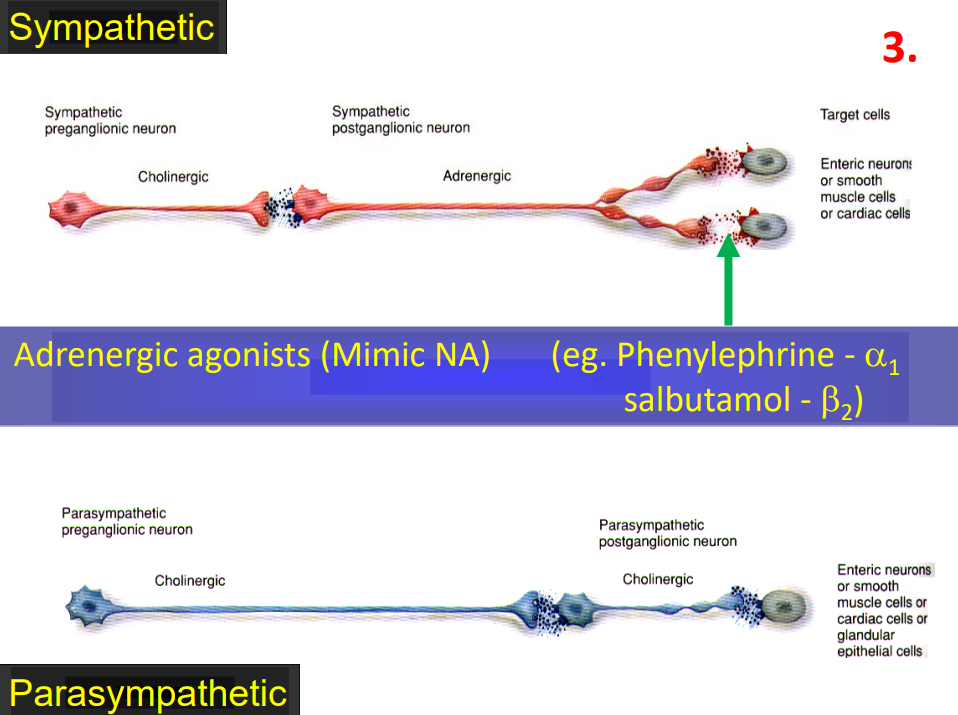
Adrenergic Agonists
- mimic noradrenaline
- e.g asthma drugs. they bind to beta 2 receptors and open up the airways in lungs
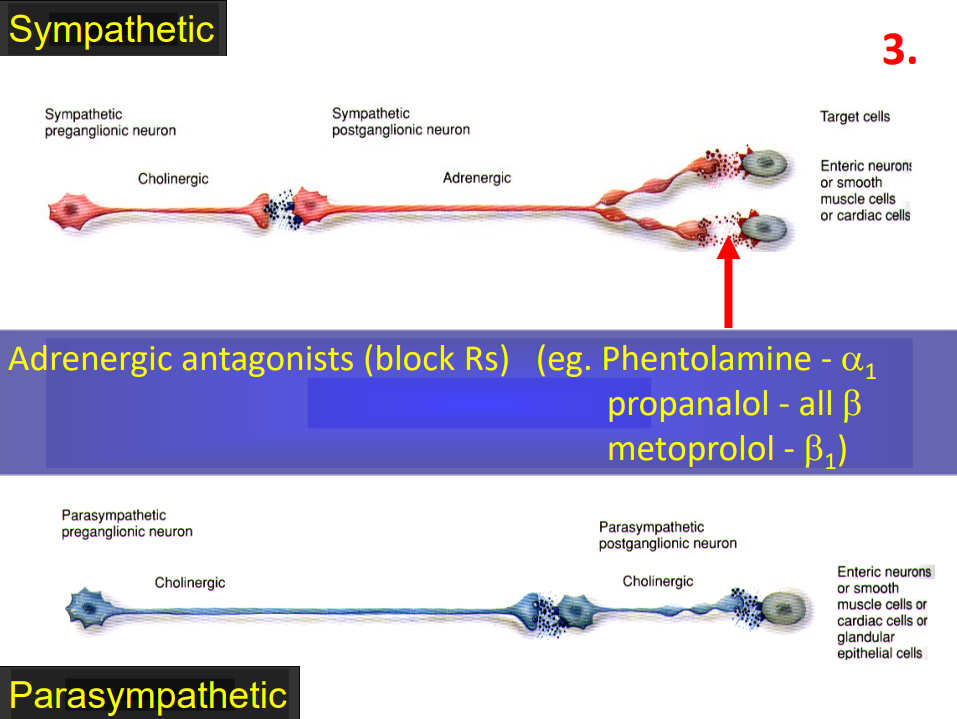
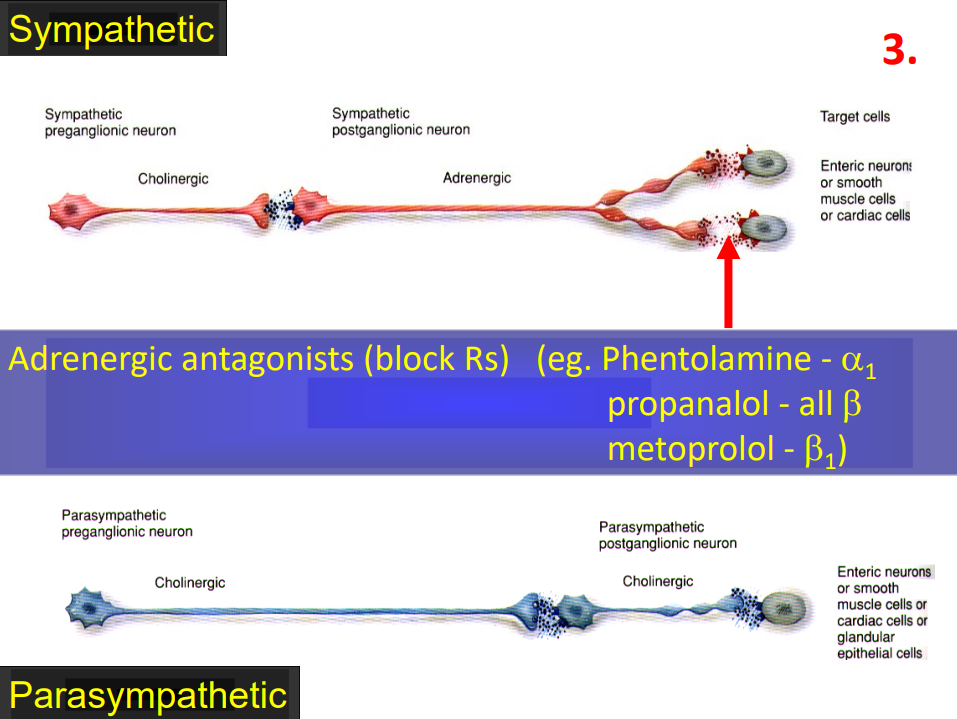
Adrenergic Antagonists
- if you have high BP and you want to slow down your heart rate an adrenergic antagonist will help
- these block the receptors and prevent message from getting through
SUMMARY
DIAGRAM ON SLIDE 33