Health Assessment EXAM 2 REVIEW
1/142
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
143 Terms
what is cranial nerve II?
optic nerve
what is cranial nerve I?
-olfactory
-smell
what is cranial nerve V(5)?
-trigeminal
-chewing
what is cranial nerve VII(7)?
-facial
-facial sensation and facial movement and taste on the tip of the tongue
what is cranial nerve VIII(8)?
-vestibulocochlear
-hearing and balance
what is cranial nerve IX(9)?
-glossopharyngeal
-gag reflex, swallowing, and taste in the back of the tongue
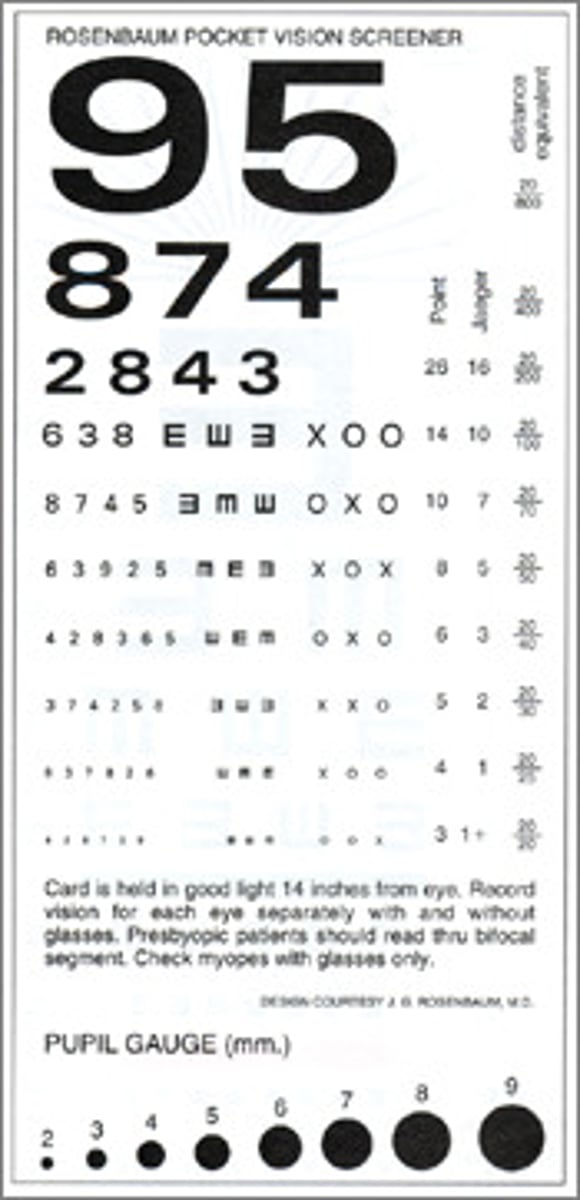
which chart measures near vision?
rosenbaum chart
which chart measures distance vision?
snellen chart
what is the normal vision count?
20/20
what is the legally blind vision count?
20/200
what does the numerator represent in a vision count?
-the distance the patient is away from the chart
-always 20!
-20 feet away
what does the denominator represent in a vision count?
-the distance at which a person with normal vision can clearly read the same line on the eye chart
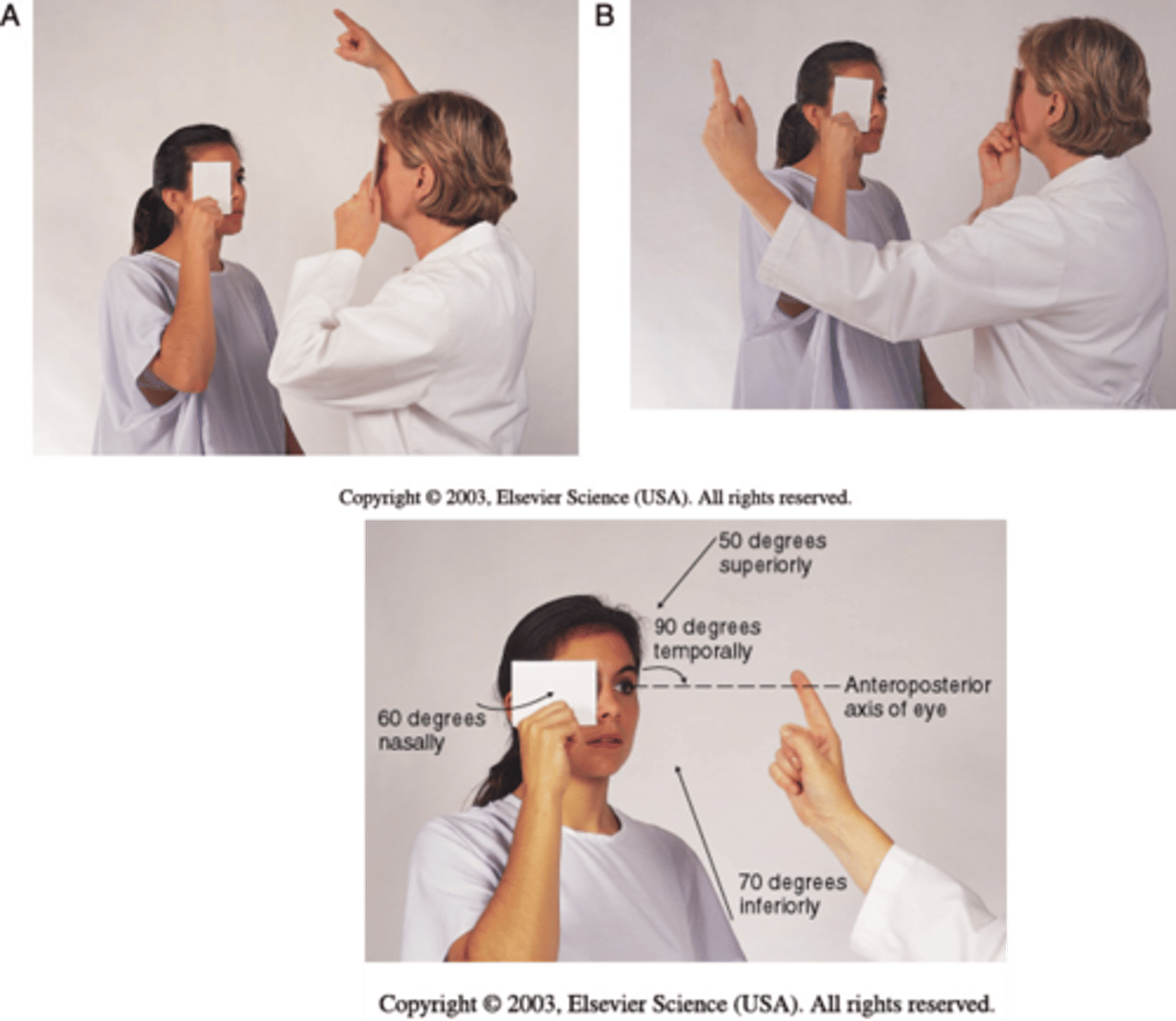
what does confrontation measure visually?
-measures peripheral vision
-fingers will go around a patients head and have them state when they see them
how do we test visual acuity?
-in a well lit area
-pt is 20 feet away from the chart
-use an opaque card (prevent peaking through fingers)
-test only one eye at a time
-leave corrective eyewear on unless it is reading glasses
-encourage the smallest line first
which cranial nerve is associated with visual acuity?
-cranial nerve II this is the optic nerve
-carries sensory visual information from the retina of the eye to the brain
-this includes visual acuity (sharpness and clarity of vision), visual fields, and light perception
which cranial nerves are associated with eye movement?
-cranial nerve III (occulomotor)
-cranial nerve IV (trochlear)
-cranial nerve VI (abducens)
*3, 4, 6 make the eyes do tricks
what is the occulomotor nerve?
-controls the direct light reflex (pupil constricts when lights shone on it)
-controls consensual light reflex (pupil constricts in eye without light)
-controls accommodation (switch from focusing on close object to far away object)
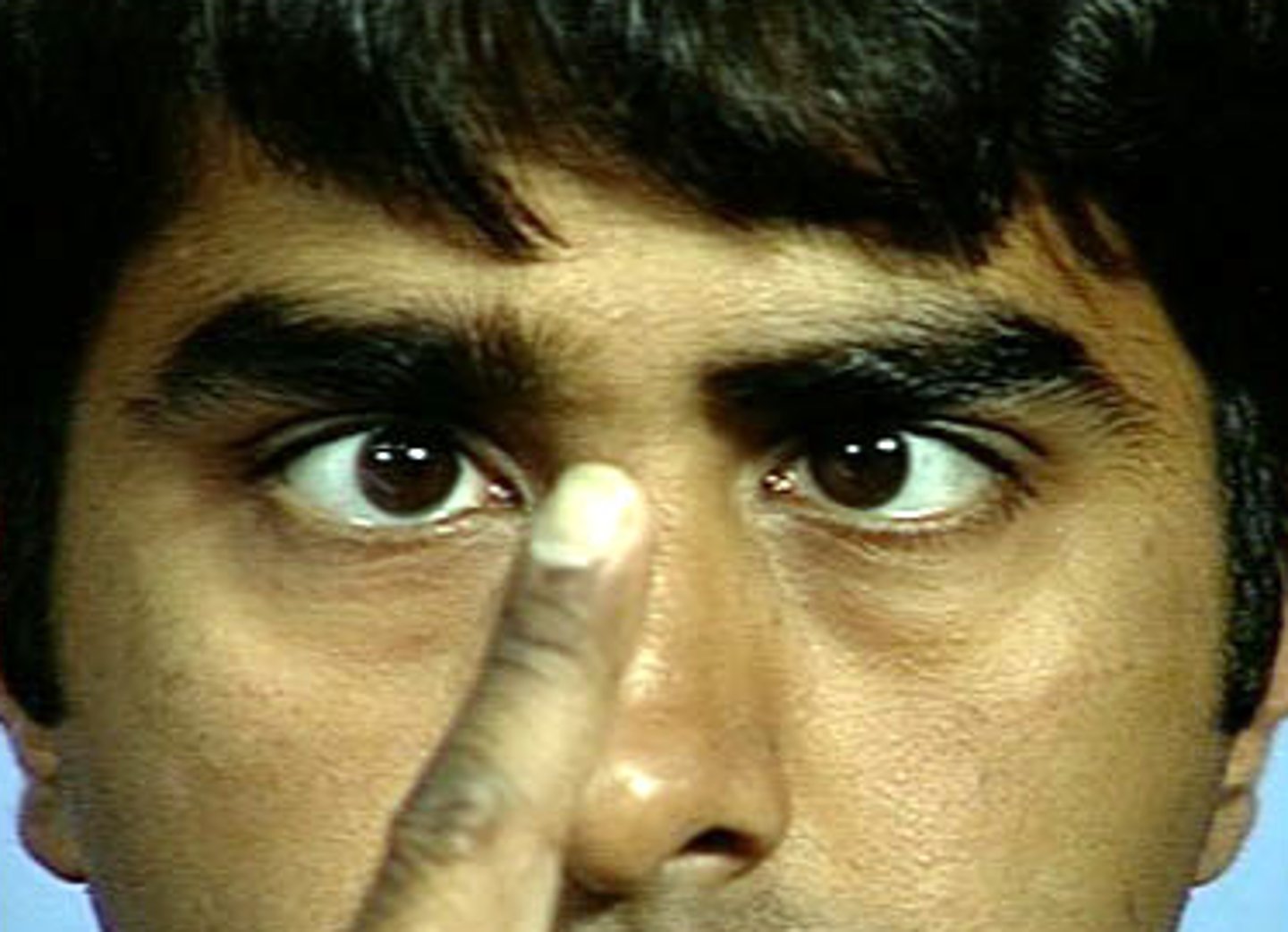
-controls convergence (move finger towards nose and eyes turn inward)
what is accommodation?
the eye's ability to change the shape of the lens to focus on objects at different distances — allowing you to see clearly up close and far away
-looking at different objects from different distances
what is convergence?
medial rotation of the eyeballs toward the object being viewed
-going cross eyes
what does the trochlear nerve control?
-movement of superior oblique muscles
-it helps your eye look down and in (like when you're reading a book or walking downstairs).

what does the abducens nerve control?
-movement of the lateral rectus muscles
-it makes your eye move outward (abduct) away from the nose
-moves the eye to the side
what does PERRLA stand for?
pupils are equal, round, and reactive to light and accommodation
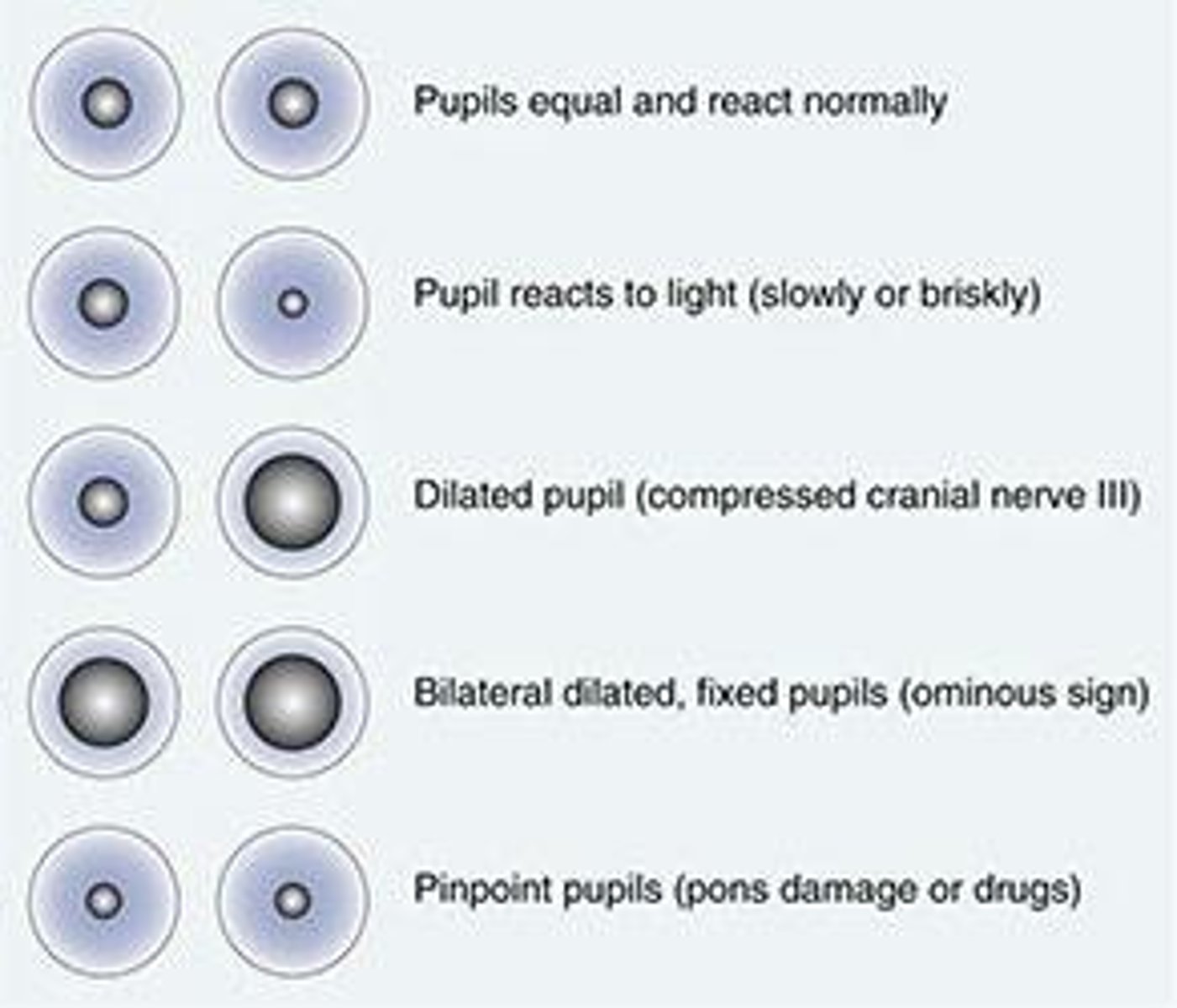
what are the components of PERRLA?
Pupils: Both pupils are present and visible.
Equal: Both pupils are the same size (usually 3–5 mm in normal light).
Round: Pupils are round in shape, not irregular.
Reactive to Light: Pupils constrict when exposed to light and dilate in darkness — this checks cranial nerves II (optic) and III (oculomotor).
Accommodation: Pupils constrict and eyes converge when focusing on something close, then dilate when shifting focus far away.
what is direct vs consensual?
-direct: the pupil constricts when light is shined directly into it
-consensual: pupil constricts when light shined in opposite eye
what is cranial nerve XI(11)?
-spinal accessory
-measures movement of the trapezius and sternomastoid muscles
-should be equal and bilateral in movement
-ask pt to rotate head with resistance and shrug shoulders
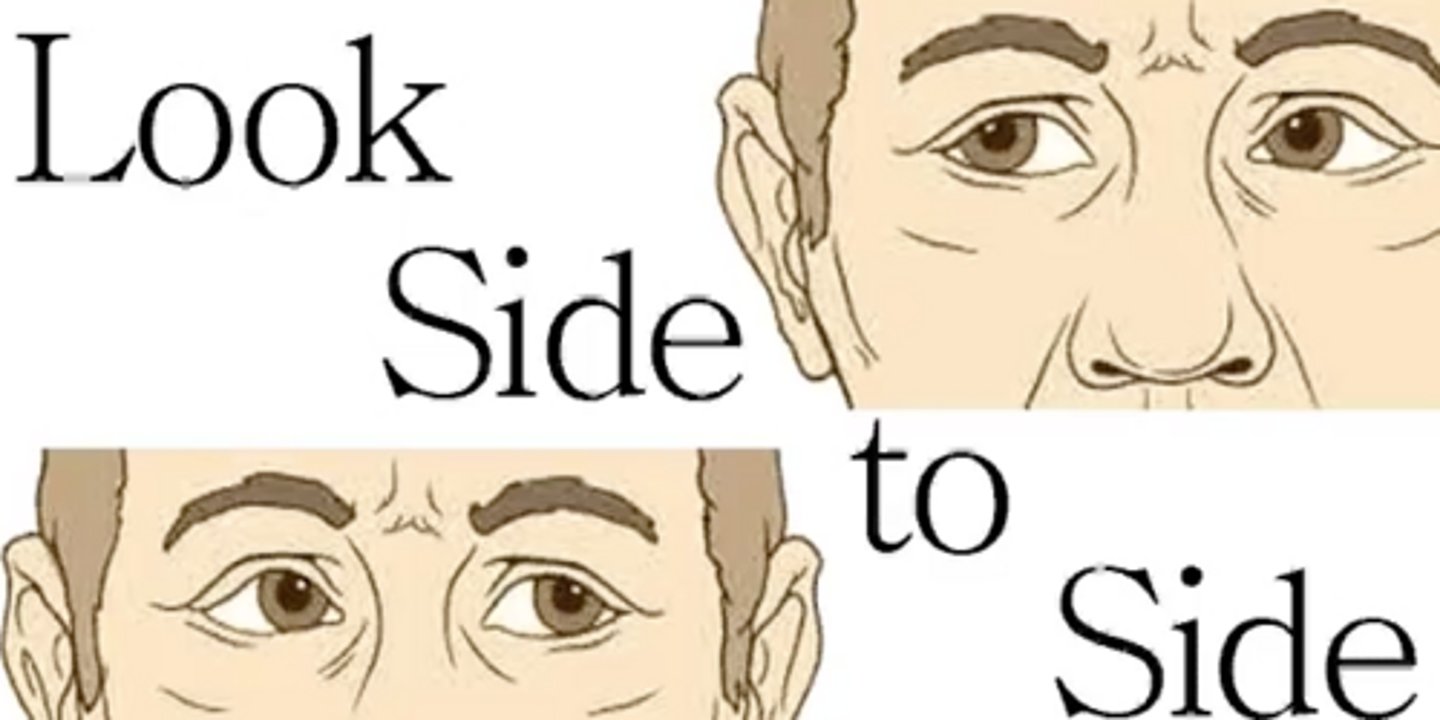
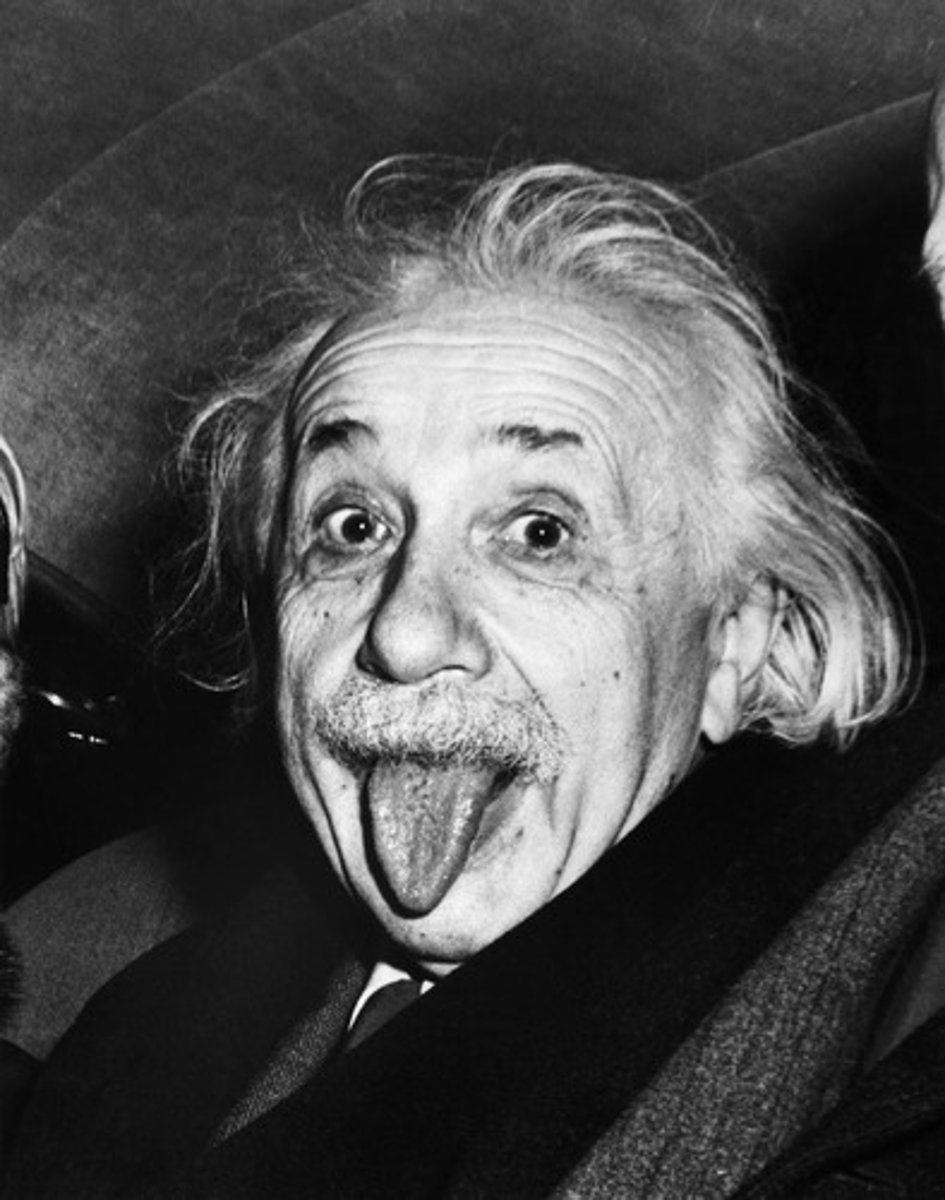
what is cranial nerve XII?
-hypoglossal nerve
-measures tongue movements
-have pt stick out tongue and move side to side assessing for strength or deviation
how do we palpate lymph nodes?
-gentle pressure in a circular motion
what are normal findings in lymph nodes?
-soft
-mobile (you can move them)
-non-tender
-discrete (not connected together)
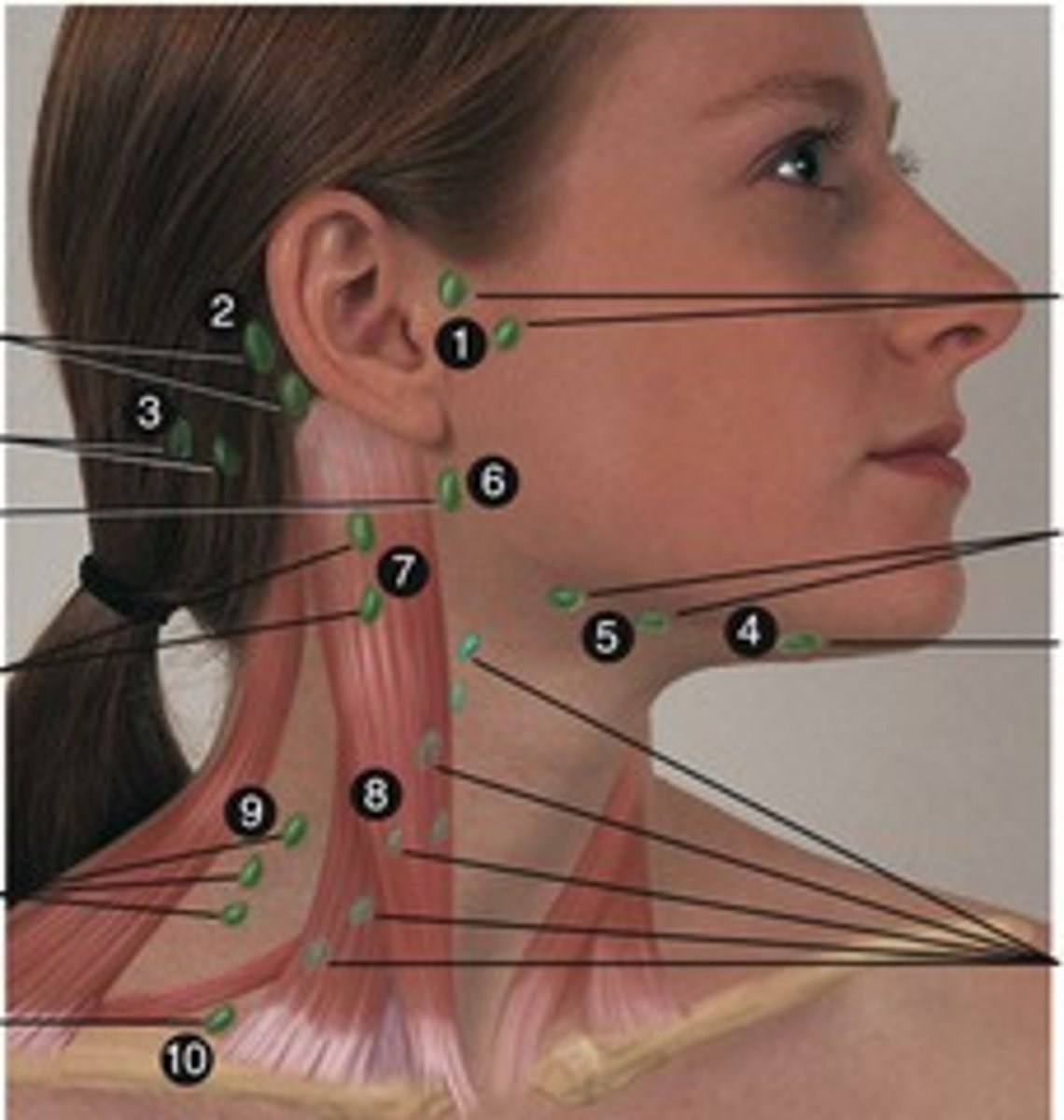
what are abnormal findings in lymph nodes?
- size larger than 1cm
- swelling longer after 3 weeks
- asymmetry
- erythema (redness)
- hardness/tenderness
- fixed/attached to the skin (immobile = bad)
- pain
what can cause abnormal findings in lymph nodes?
-acute infection
-chronic inflammation
-neoplasms
-lymphoma
what is lymphadenopathy?
-enlarged lymph nodes
-GREATER than 1cm in size
-caused by infection, allergy, or neoplasm
what is a neoplasm?
-a new and abnormal growth of tissue in some part of the body
-especially as a characteristic of cancer
-a tumor
what does rate mean in the cardiac cycle?
-number of times the heart beats per minute
-normal: 60-100bpm
-bradycardia: LESS than 60
-tachycardia: GREATER than 100
what does rhythm mean in the cardiac cycle?
-how regular the heartbeats are whether the heart is beating in a steady pattern or not
-regular or irregular
-are the heartbeats even and steady or uneven and unpredictable
what does amplitude mean in the cardiac cycle?
-the strength or force of the heartbeat basically how strong the pulse feels when the heart pumps blood
what is the scale for determining amplitude?
0: no pulse
1+: weak and thready
2+: normal
3+: bounding
what is the blood flow of the cardiac cycle?
right atrium TO tricuspid valve TO right ventricle TO pulmonic valve TO pulmonary artery TO lungs TO pulmonary veins TO left atrium TO mitral valve TO left ventricle TO aortic valve TO aorta TO organs and tissues
what are the AV valves?
tricuspid and mitral (bicuspid)
what are the SL valves?
pulmonary and aortic
what is the s1 sound?
-the FIRST sound heard
-the closure of the AV valves
-the BEGINNING of systole (when the atrium is filling up with blood)
-louder at the apex (the bottom of the heart)
what is the s2 sound?
-the SECOND sound heard
-the closure of the SL valves
-the END of systole
-louder at the base (the top of the heart)
what is the s3 sound?
-heard AFTER s2
-AV valves open and arterial blood flows into ventricles
-KEN-TU-CKY
what can an s3 sound be a sign of in older adults?
-MV (mitral valve) or TV (tricuspid valve) regurgitation
-cardiomyopathy
-heart failure
what can an s3 sound be a sign of in pregnant women, children, and athletes?
-this is NORMAL TO HEAR in these groups of people
what is the s4 sound?
-heard BEFORE s1
-ventricle is resistant to filling with blood
-the END of diastole
-TEN-NE-SSEE
-ALWAYS PATHOLOGICAL!
-indicates diastolic failure
what are some causes of an s4 sound?
-left ventricle hypertrophy
-cardiac ischemia
-uncontrolled hypertension
-hypertrophic restrictive cardiomyopathy
what is a heart murmur?
-abnormal heart sound is typically due to a leaky valve
-blowing or swooshing sound from turbulent blood flow
-abnormal EXCEPT for innocent murmurs
how do we inspect the carotid arteries?
-don't want to see any pulsations!
-they should not be visibly prominent
-visible or bounding pulses can signal abnormal pressure or vascular problems
how do we palpate the carotid arteries?
-ONE AT A TIME (can cause a syncope episode and have someone pass out if do both at the same time)
-feel contour (shape and smoothness of the pulse) and amplitude
-feel for thrills
-should feel the same BILATERALLY
what are thrills?
-turbulent blood flow
-abnormal vibration (feels like a cat purring underneath the skin)
-ABNORMAL
how do we auscultate the carotid arteries?
-use the BELL side of stethoscope to hear for BRUITS (these are low pitched sounds)
-one side at a time
-have the pt hold their breath as a bruit can be confused with lung sounds

what are bruits?
-abnormal blowing or swishing sounds indicating turbulent blood flow
-you HEAR it
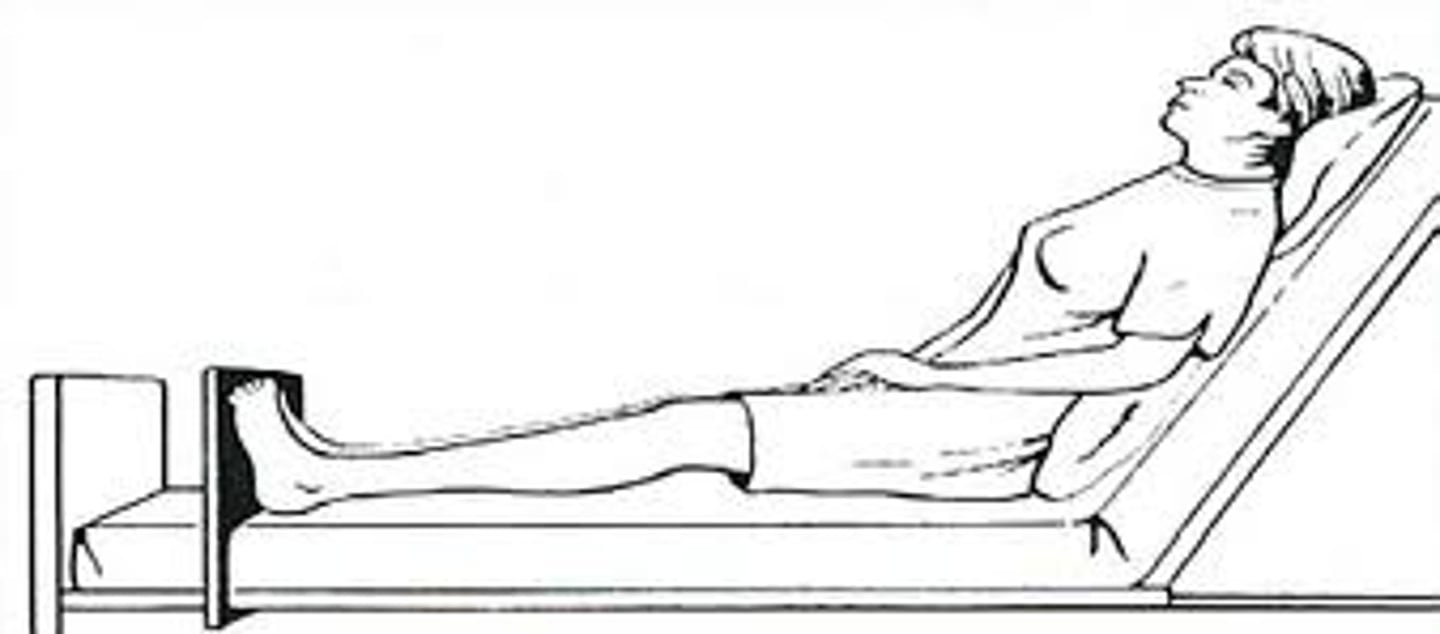
how do we assess the jugular venous pulse?
-patient must be in supine (laying down)
-the HOB must be in semi-fowlers (30-45 degrees)
-remove any pillows and turn the head
-normal: external jugular should flatten and disappear at 45 degrees
-abnormal: external jugular is STILL present meaning JVD!
how do we inspect the anterior chest?
-look at the apical pulse (which is the pulsation against the left ventricle against chest wall)
-visible at 4th or 5th intercostal space
-easier to see in children or patients with a thin chest wall
-look for lifts or heaves

what are lifts or heaves?
-sustained or forceful thrusting of ventricle during systole
-shows increased workload
-rv: seen at sternal board
-lv: seen at apex
how do we palpate the point of maximal input?
-have pt sit up and displace breast tissue and turn to the left side
-have pt exhale and hold breath
-located at the 4th and 5th intercostal space
-feel for lifts and heaves as well
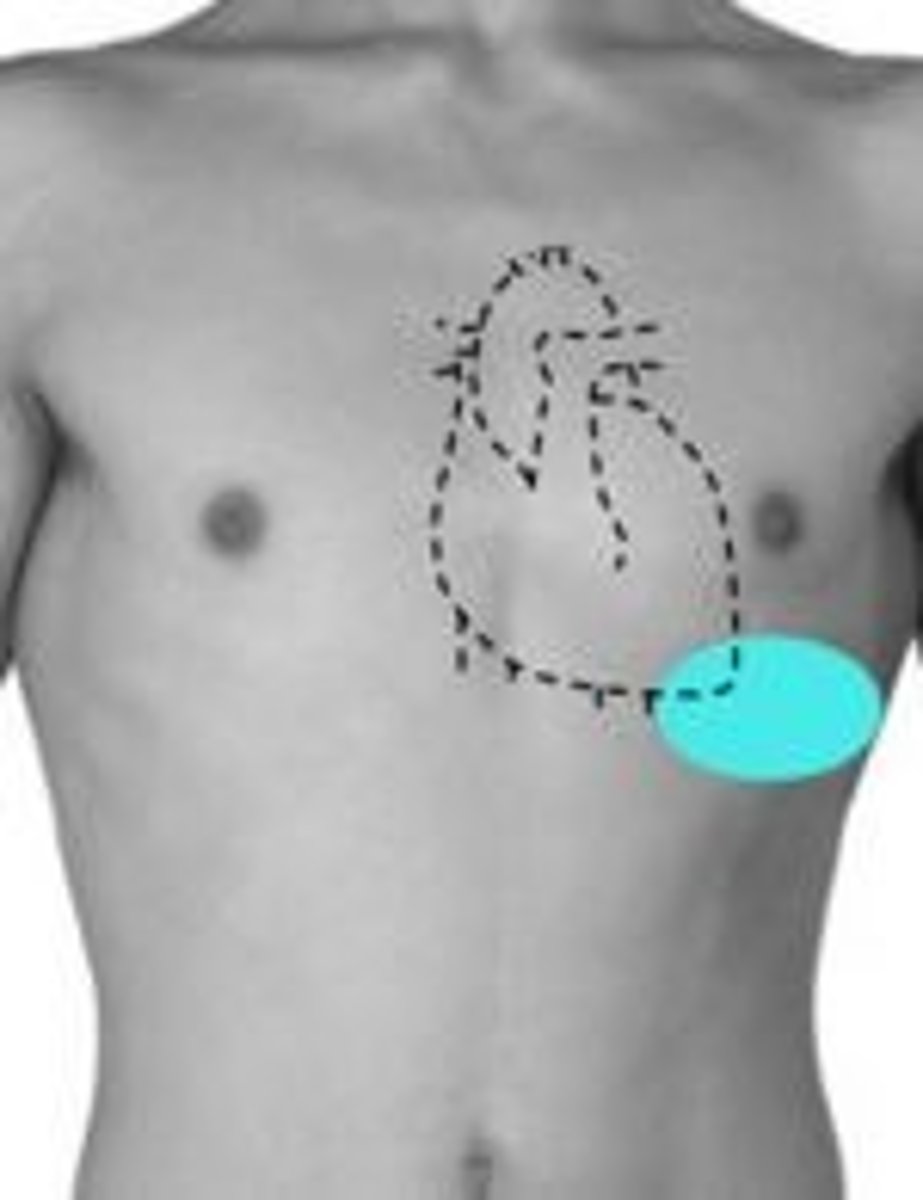
what is the point of maximal input?
-the spot on the chest where you can feel the heart beating the strongest
-at the 5th intercostal space, left midclavicular line, and it represents the apex of the heart hitting the chest wall during contraction
how do we auscultate the anterior chest?
-start with the diaphragm of the stethoscope FIRST!
-note the rate and the rhythm
-listen for s1 and s2 sounds
-also listen for s3 and s4 sounds and murmurs
-end with listening with the bell of the stethoscope LAST!
how do we palpate the percordium?
-palm fingers on the chest
-gently feel for thrills
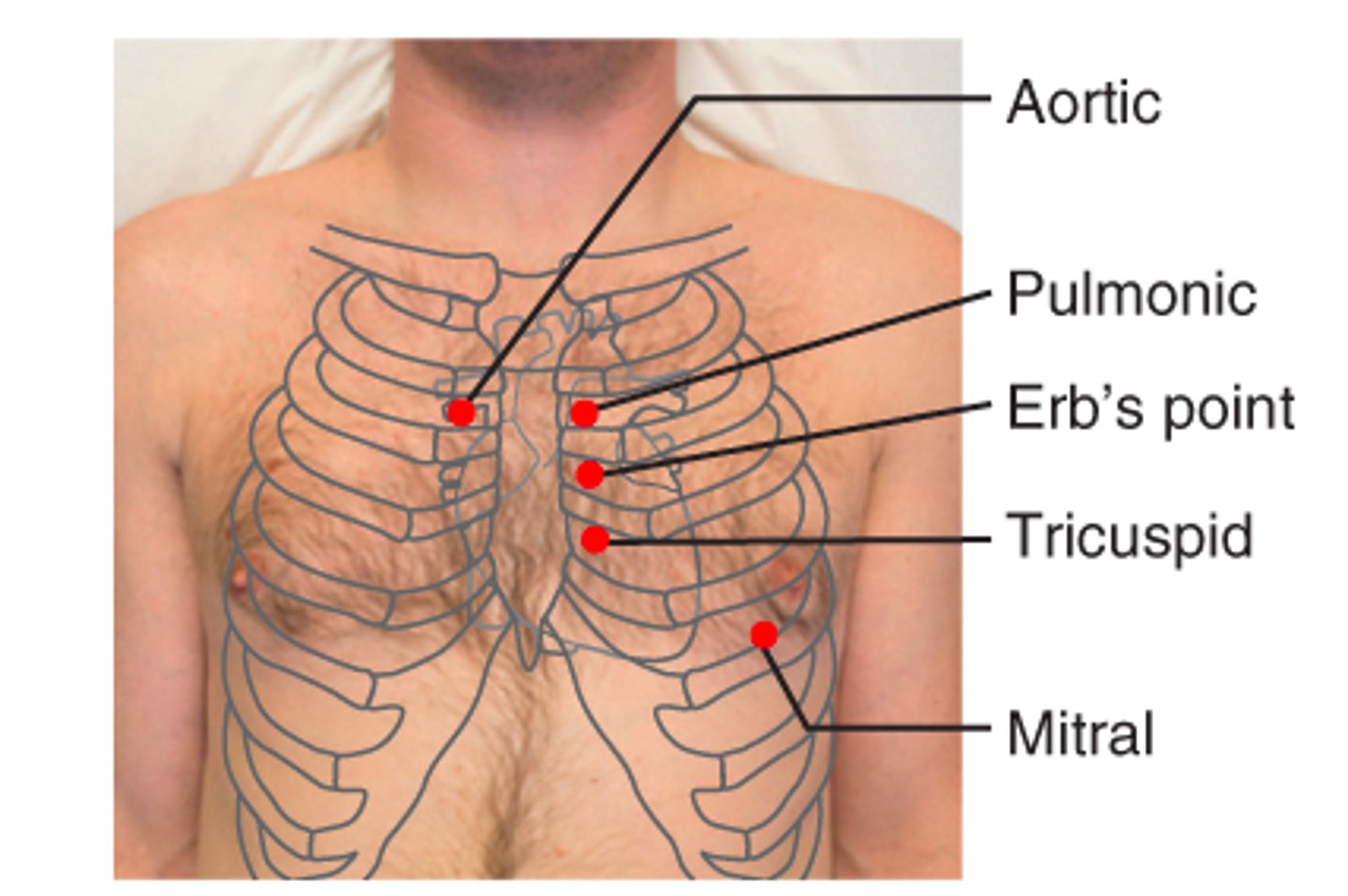
what is the order of the valves?
aortic: 2nd intercostal; right sternal border
pulmonic: 2nd intercostal; left sternal border
erb's point: 3rd intercostal; left sternal border
tricuspid: 4th intercostal; left sternal border
mitral: 5th intercostal; midclavicular line
*A PET Monkey
what is the z pattern in cardiac auscultation?
-the path you move your stethoscope in a "Z" shape across the chest to listen to all four heart valves — aortic, pulmonic, tricuspid, and mitral — in order during auscultation
-TO LISTEN TO HEART SOUNDS
what is the lymphatic system?
-retrieves excess fluid and plasma proteins from interstitial spaces and puts them back into the bloodstream
-protects the body from infection
-detects and eliminates foreign substances, filter lymph, and engulf pathogens
what are cervical nodes?
drain the head and neck
what are the axillary nodes?
drain the breast and upper arm
what are the inguinal nodes?
drains the lower extremities, external genitalia, and anterior abdominal wall
where are the different pulse sites?
1. temporal
2. carotid*
3. apical* (PMI)
4. brachial*
5. radial*
6. femoral
7. popliteal (behind the knee)
8. posterior tibial (by your ankle)
9. dorsalis pedis (on top of the foot)
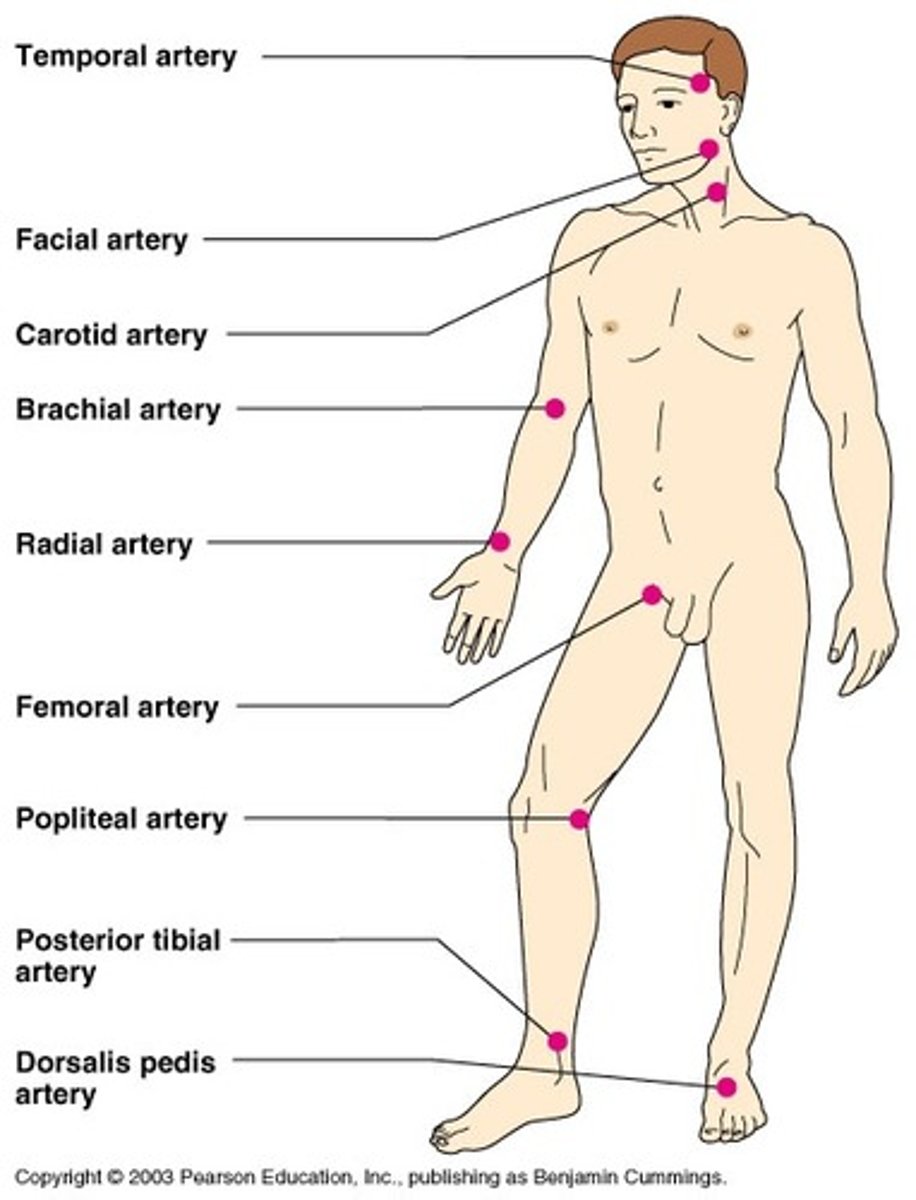
how do palpate for pules?
-palpate for 30 seconds and then multiply by 2 if normal OR palpate for a full minute if abnormal
-palpate both radial pulses for rate, rhythm, elasticity, and force and grade the amplitude (ex: 2+)
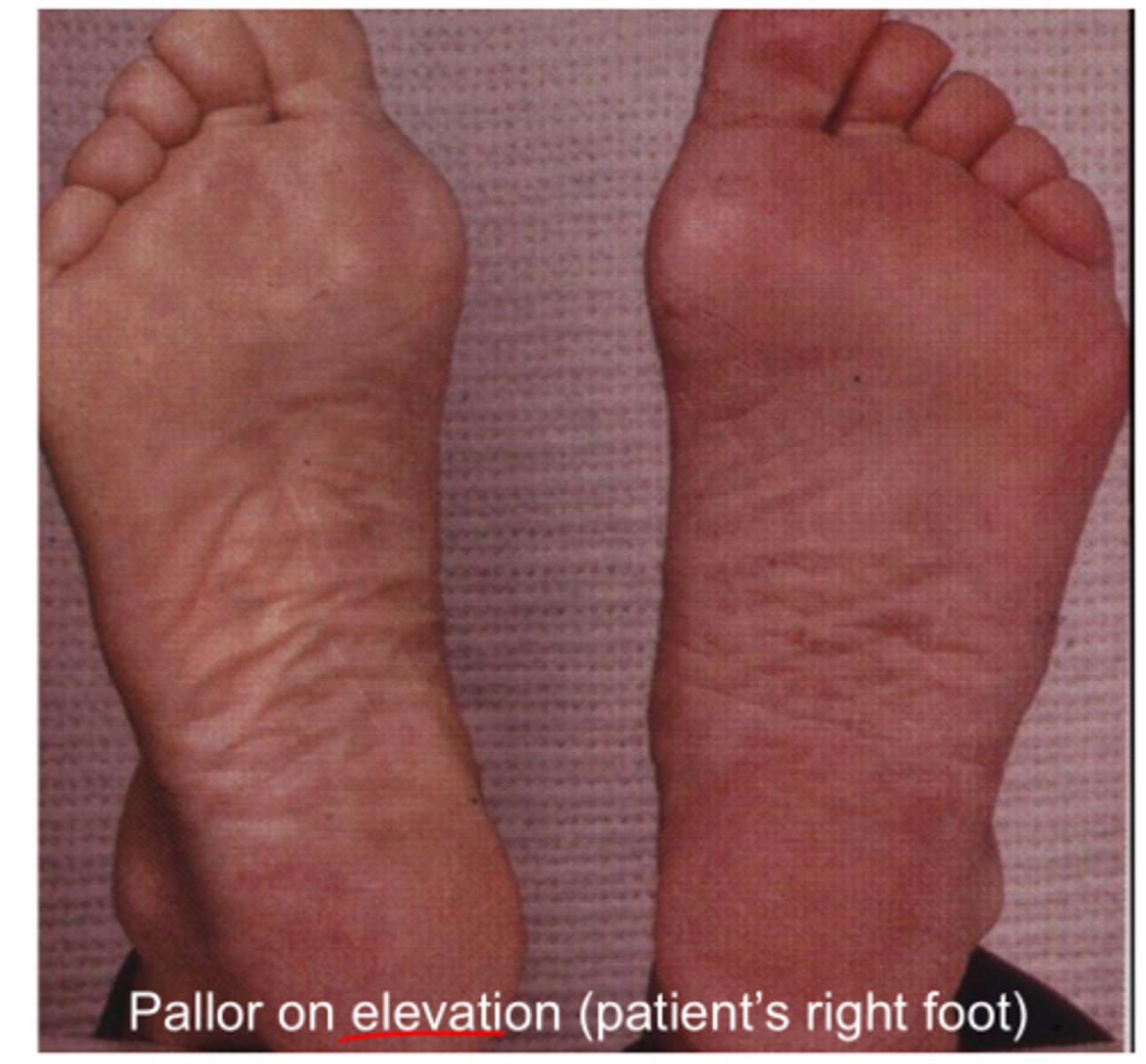
what is PAD (peripheral artery disease)?
-arteries in the legs (or other limbs) become narrowed or blocked by plaque, reducing blood flow
-blood cannot be pumped to peripheral extremities
-LIMITED BLOOD FLOW
what signs and symptoms do we see in PAD?
-hairless
-cold/pale extremities
-slow healing ulcers
-pallor on elevation and cyanosis on nail bed
-thin shiny skin
-intermittent claudification relieved with rest
-weak/absent pulses
-paresthesia (tingling sensation)
what are the risk factors asscociated with PAD?
-diabetes
-arterial insufficiency
-slow healing wounds
-pressure ulcers
-necrosis
what is PVD (peripheral venous disease)?
-veins in the legs are damaged or not working properly, making it hard for blood to flow back up to the heart
-blood pools in lower extremities as it CANNOT return to the heart
what are the signs and symptoms of PVD?
-bilateral pitting edema
-brownish discoloration to the skin of the lower leg
-warm/erythema
-pain relieved by walking and worsens when sitting down/at the end of the day
what are DVT's?
-deep vein thrombosis
-formation of a blood clot (thrombosis) due to inactivity
-NEVER massage DVT's can cause a pulmonary embolism
what are the signs and symptoms of DVT's?
-unilateral edema
-warmth
-redness (erythema)
-tenderness
how do we prevent DVT's?
-scd's
-have patient walk/ambulate
what are superficial varicose veins?
-dilated leg veins from increased venous pressure from obesity, pregnancy, and prolonged standing
what are vascular occlusions?
-calcification of vessel wall and thrombus formation
-caused by atherosclerosis
what are risk factors associated with vascular occlusions?
-obesity
-diabetes mellitus
-hypertension
-hyperlipidemia
what makes up the sternum?
manubrium, sternal body, xiphoid process
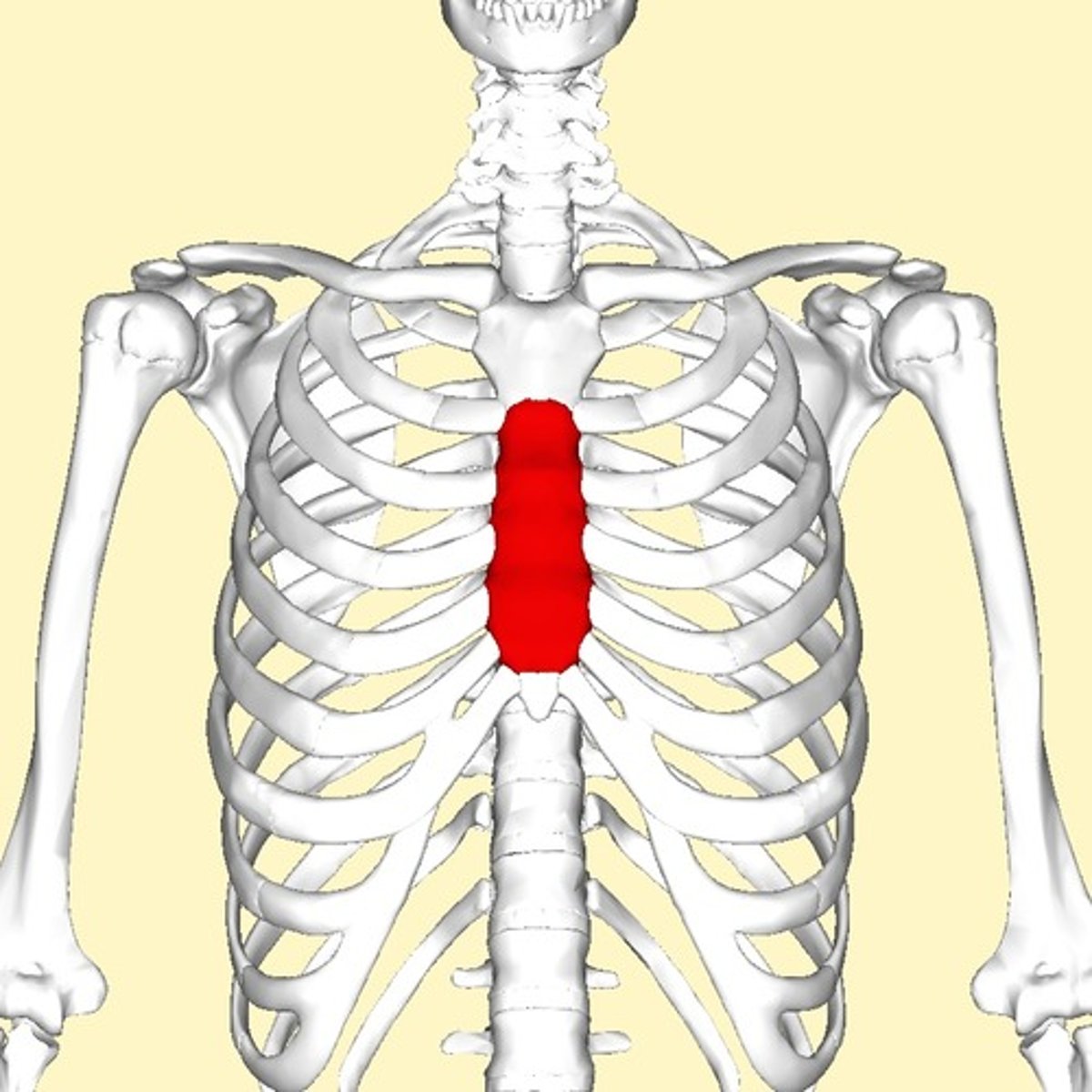
what is the angle of louis?
-sternal angle
-landmark to count the ribs
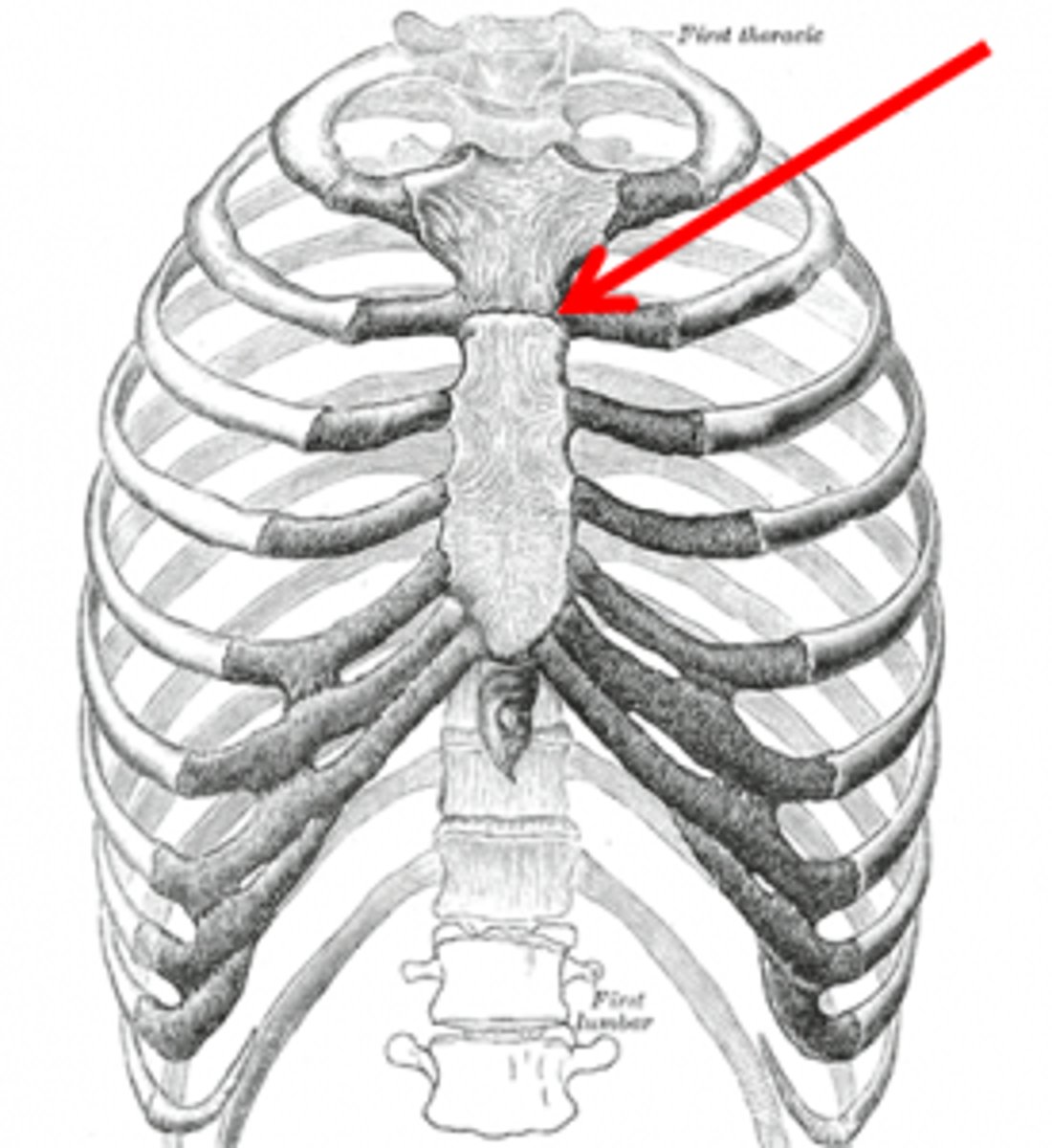
what is the costal angle?
-the angle formed where the right and left costal (rib) margins meet at the bottom of the sternum
-normally about 90° or less
-if it's wider than 90°, it can mean conditions like chronic lung overinflation (ex: COPD)
what is the vertebra prominens?
-the most prominent bone you can feel when you bend your head forward, and it's often used as a landmark for counting vertebrae or ribs during assessments
-C7

what is your spinous processes?
-the bony bumps you feel down the middle of your back they're the parts of your vertebrae that stick out to the back
-one spinous process for EACH rib
-they angle downwards
what is the inferior border of the scapula?
-the bottom tip of the scapula, and when your arms are at your sides, it's usually at the level of the 7th or 8th rib
-they are symmetrical with each hemithorax (aka each side of your chest) IF NOT something is abnormal
what are normal inspection findings for the lungs and thorax?
-chest is elliptically shaped
-upright and relaxed
-AP diameter of 1:2
what are abnormal inspection findings for the lungs and thorax?
-retractions
-use of accessory muscles
-tripod positioning
-chest is barrel shaped
-AP diameter of 1:1
-pectus excavatum
-pectus carinatum
what is pectus excavatum?
-sunken sternum
-occurs at birth
*think excavate=dig a hole

what is pectus carinatum?
-protrusion of the sternum
-happens during puberty
-benign

what is an anterior lag in expansion a sign of when palpating the lungs and thorax?
-pneumonia because of all the fluid buildup
what is a posterior unequal expansion a sign of when palpating the lungs and thorax?
-atelectasis
-pneumothorax
what is the greek key pattern?
-greek key pattern means you move your stethoscope in a side-to-side, step-down pattern, comparing one spot on the right lung to the same level on the left lung all the way down
-compare both sides!
-use the diaphragm
-TO HEAR LUNG SOUNDS
what are abnormal findings in auscultation for lungs and thorax?
-crackles (rales)
-rhonchi
-wheezing
-stridor
what are crackles (rales)?
-straw and empty cup sound
-indicator of fluid in the airways
-heard on inspiration and CANNOT be cleared with a cough
-associated with pneumonia and atelectasis
what are rhonci?
-a low pitch snoring sound
-indicator of thick secretions but can be cleared by a cough
-mucous is present!
-associated with bronchitis, COPD, pneumonia
what is wheezing?
-difficult breathing with a high-pitched whistling or sighing sound during expiration
-louder on expiration
-associated with asthma and COPD
what is stridor?
-inspiratory wheezing
-indicates upper airway obstruction
-MEDICAL EMERGENCY
-common sx of epiglotitis
what is tactile fremitus?
-palpable vibration on the chest wall
-strongest over the trachea
-have patient say "99"
-use palmar or dorsal surface of hand
when do we feel an increase in tactile fremitus?
-with INCREASED consolidation aka with increased fluid in the lungs
-highly associated with pneumonia
*air is a poor conductor of sound and vibration
when do we feel a decrease in tactile fremitus?
-with DECREASE consolidation aka with an increase of plueral effusion
-pleural effusion is when there is fluid in the space BETWEEN the lungs and chest wall
-emphysema, pneumothorax, and pleural effusion
what is consolidation?
-means that the normal air-filled spaces in the lungs (alveoli) are filled with something else like fluid, pus, blood, or cells
-makes the lung tissue solid instead of spongy
-common in pneumonia