HAD 381 - Quiz 8 - Intracellular Organisms & Viruses
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
120 Terms
RNA viruses: general characteristics:
Can be ss (single-stranded) or dsRNA (double-stranded)
Most are ssRNA
Include the medically important viruses
Hepatotropic viruses
Influenza viruses
Retrovirus
HIV
Filoviruses
Ebola and Marberg
Hepatotropic Viruses: general characteristics:
Causes hepatitis
Inflammatory condition of the liver
Hepatotropic Viruses: signs & symptoms
fatigue, fever, joint and abdominal pain, vomiting, anorexia, dark urine, hepatomegaly, elevated liver enzymes and jaundice
Hepatototrophic liver function tests for diagnosis:
Six types identified:
Hepatitis A virus (HAV), Hepatitis B virus (HBV), Hepatitis C virus (HCV), Hepatitis D virus (HDV), Hepatitis E virus (HEV), Hepatitis G virus (HGV)
Other viruses such as EBV, CMV, and HSV can also cause hepatitis
Specifically infect liver cells
Hepatitis A Virus (HAV): general characteristics:
Enterovirus belonging to the family Picornaviridae
Mode of transmission: fecal–oral route by ingestion of
food/water contaminated with feces
Occasionally parenteral transmission
Called infectious hepatitis because can occur in outbreaks
often affects large numbers of people
Hepatitis A Virus (HAV): Symptoms:
Acute, chronic, or asymptomatic infections
Asymptomatic
No clinical symptoms but liver enzymes are elevated
Incubation period of 2-6 weeks
Flu-like illness and pain in area of liver
Viral shedding for up to 30 days after onset of symptoms
Resolution in 6 months
HAV infection:
Anti-HAV antibodies emerge at about 10 days
IgM antibodies peak at 30 days and are undetectable at about 6 months
IgG antibodies emerge after 14 days and peak at 30 days
Can remain detectable for more than 10 years
HAV diagnosis & treatment:
Diagnosed by demonstration of a significant rise in titers between acute and convalescent sera using RIA or EIA
No specific treatment
rest is recommended during acute stage of illness
Immunity conferred by the production of neutralizing antibodies directed against HAV
HAV vaccine can be administered to prevent infection in uninfected individuals exposed to virus
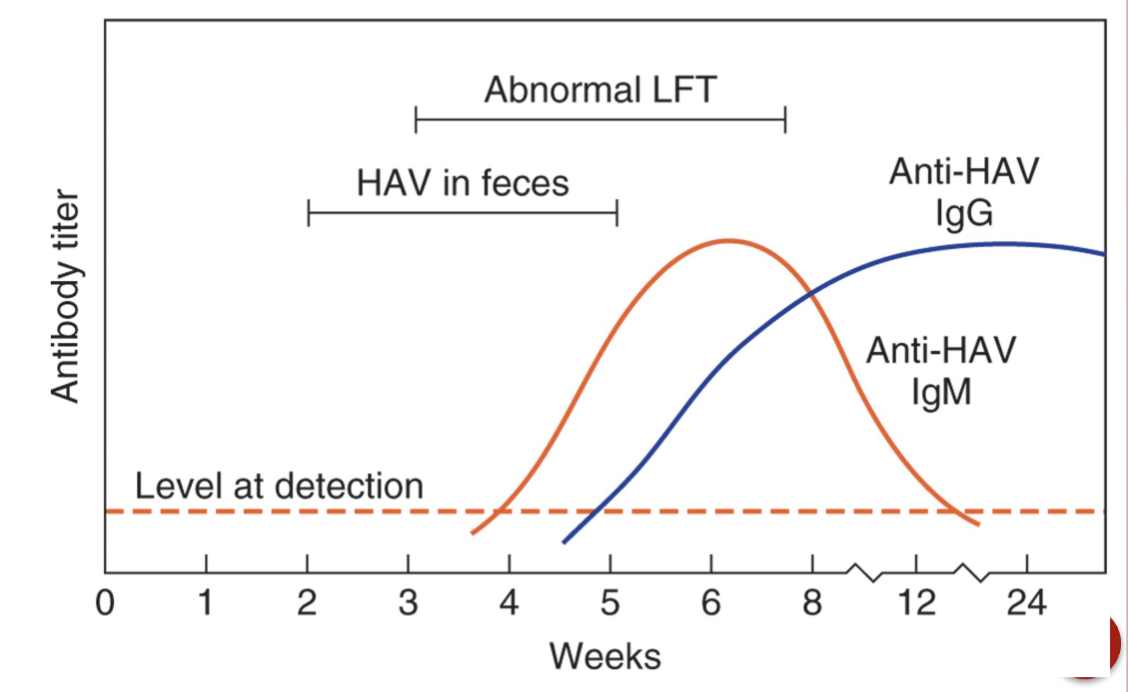
A serological profile of detectable antibodies to HAV infection. LFT, liver function tests.
Hepatitis C Virus (HCV): general characteristics:
Belongs to the family Flaviviridae
Formerly known as non-A, non-B hepatitis
Mode of transmission is primarily parenteral
bloodborne
perinatal and sexual transmission is possible
20% of cases are acute and 80% can result in chronic infection
Causes cirrhosis and liver cancer
Leading cause of liver transplants
Parenteral transmission:
The introduction of pathogens into the body through a route other than the gastrointestinal tract, such as through injections, cuts, or bites, bypassing the digestive system
HCV diagnosis & treatment:
Diagnosis previously based on:
demonstration of elevated liver enzymes such as ALT
exclusion of known viral etiologic agents
EIA procedure to screen donor blood for anti-HCV antibodies
Treatment
Antiviral drugs such as ribaviron
Immunodulatory drugs such as interferon-alpha
Hepatitis D Virus (HDV): general characteristics:
A defective virus because its genome lacks essential genes
Probably a subviral agent because it requires a helper virus, HBV
HDV infection can only occur in individuals with HBV infection
must be transmitted simultaneously with HBV or as a superinfection of HBV infected individuals
Transmission is parenteral like HBV
Infection increases risk of cirrhosis and cancer
HDV: diagnosis:
IgM antibodies appear first 6-7 weeks after infection then decline after the acute phase
IgG antibodies appear during the acute phase and decline within a few months
Both IgM and IgG are elevated in cases of chronic infection
Diagnosis depends upon the detection of antibodies to the HDV (delta) antigen
Hepatitis E Virus (HEV): general characteristics:
Family Hepeviridae
Mode of transmission is fecal–oral route
Causes an acute self-limiting illness with no chronic phase
Symptoms similar to those of HAV except in pregnant women where mortality rate is high
No vaccine available
Diagnosis through demonstration of IgM antibodies during acute phase
Hepatitis G Virus (HGV): general characteristics:
Family Flaviviridae
Discovered in 1995
Associated with acute and chronic cases of hepatitis
Transmitted by parenteral route
Blood transfusions and intravenous drug use
Diagnosis through use of EIA, PCR, and Western blot techniques
Picornaviridae: general characteritics:
Includes the following medically important genera:
Enteroviruses, which includes the coxsackie and polio viruses
Rhinoviruses which are a major cause of the common cold
Heptovirus including hepatitis A virus
Are very hardy and resistant to many disinfectants
Members of this family cause a variety of diseases from asymptomatic to symptomatic
Aseptic meningitis, a disease seen in infants less than a year old, may be fatal
Enteroviruses: Includes 5 groups
Polioviruses types 1-3
Coxsackie A viruses types 1-24
Coxsackie B viruses types 1-6
Echoviruses types 1-34
Enteroviruses serotypes 68-71
Enteroviruses: general characteristics:
Second most common viral infectious agents in humans
Cause febrile illnesses, respiratory illnesses, rashes, aseptic meningitis, and paralysis
Children tend to be affected during summer, fall and winter months
Resistant to most commonly used disinfectants
Detergents
70% alcohol
Phenolic compounds
Halides (iodine and chlorine solutions) can inactivate enteroviruses and are effective
CSF is specimen of choice in cases of aseptic meningitis
Nucleic acid assays faster than cell culture
Enteroviruses: transmission:
primarily fecal–oral route but also respiratory aerosols
Poliomyelitis viruses: general characteristics:
ssRNA
Etiologic agents of polio especially in children
Transmitted thru oral-fecal route via ingestion of contaminated food and water
Multiplies in gastrointestinal tract then invades blood and finally CNS causing irreversible paralysis
95% of cases are asymptomatic
Vaccine has eradicated it in developed countries but still significant threat in 3rd world countries
Two types of polio vaccines:
Salk inctivated poliovirus vaccine (IPV) 1955
Sabin oral live poliovirus vaccine (OPV) weakened poliovirus 1961
Vaccine-associated parlytic poliomyelitis 3/million
Cost in the developing world is about US $0.25 per dose
Coxsackie viruses: general characteristics;
Human pathogens include coxsackie A and B
They are both implicated in aseptic meningitis
Coxsackie viruses: Coxsackie A 16
Cause of hand, foot, and mouth disease in children
Fever, mouth blisters, and rash
Aseptic meningitis
Human foot and mouth disease (HFMD) (Cattle)-Plum Island
Coxsackie viruses: Coxsackie A 24:
hemorrhagic conjunctivitis
Coxsackie viruses: Coxsackie B:
infectious pericarditis, myocarditis, Bornholm disease
(pleurodynia)
Coxsackie viruses: Coxsackie B 24:
Type 1 diabetes
Rhinoviruses: general characteristics:
Major cause of common cold primarily during fall and spring
Rare cause of bronchitis and pneumonia
Very hardy, heat stable and resistant to effects of desiccation
Rhinoviruses: factors associated with transmission:
Close proximity of individuals in cold weather
Viral shedding in nasal secretions before symptoms
Shedding persists for several days after recovery
1/2 of cases are asymptomatic but still shed virus
Hands of infected individuals transfer nasal secretions to inanimate objects
Self inoculation of uninfected persons by rubbing eyes or nose
Rhinoviruses: diagnosis & prevention:
Laboratory diagnosis rarely attempted because of mild nature of infection
Control thru hand washing and avoiding contact between eyes, nose, and hands
Vaccine not likely due to number of serotypes
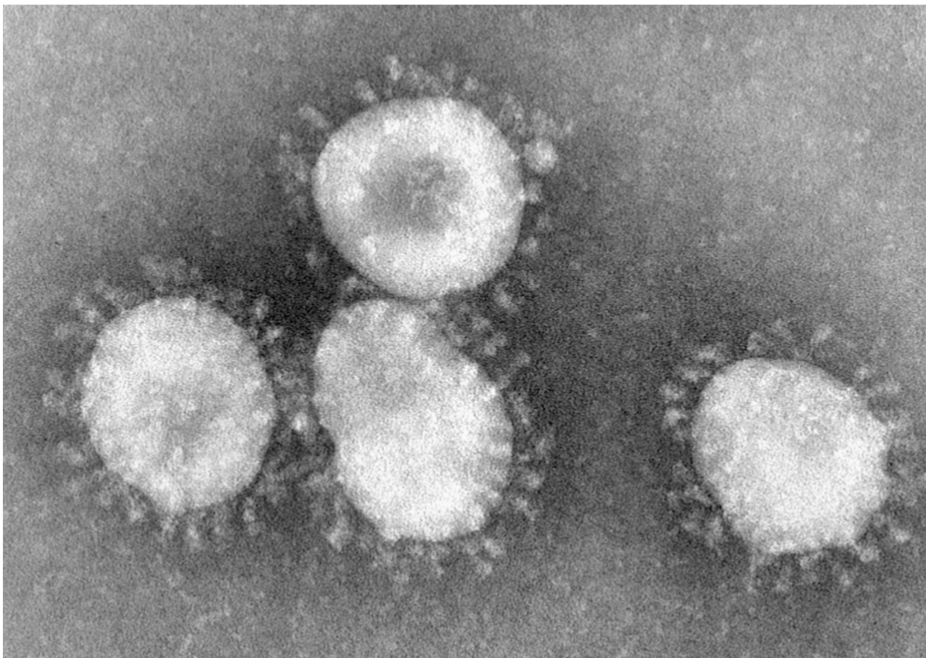
Coronaviruses: general characteristics
Enveloped, ssRNA
Cause of pharyngitis and most colds occurring during the winter months
Transmission via respiratory secretions
Word “Coronavirus” is derived from Latin corona, meaning crown or halo.
Under EM each virion appears corona or halo. This is due to the presence of viral spikes peplomers emanating from each proteinaeous envelope.
Common human corona viruses
Alphacoronaviruses: HcoV-229E, HCoV-NL63
Beta coronaviruses: HCoV-oc43, HCoV-HKU1
Effects upper respiratory and gastrointestinal tract of mammals and bird.
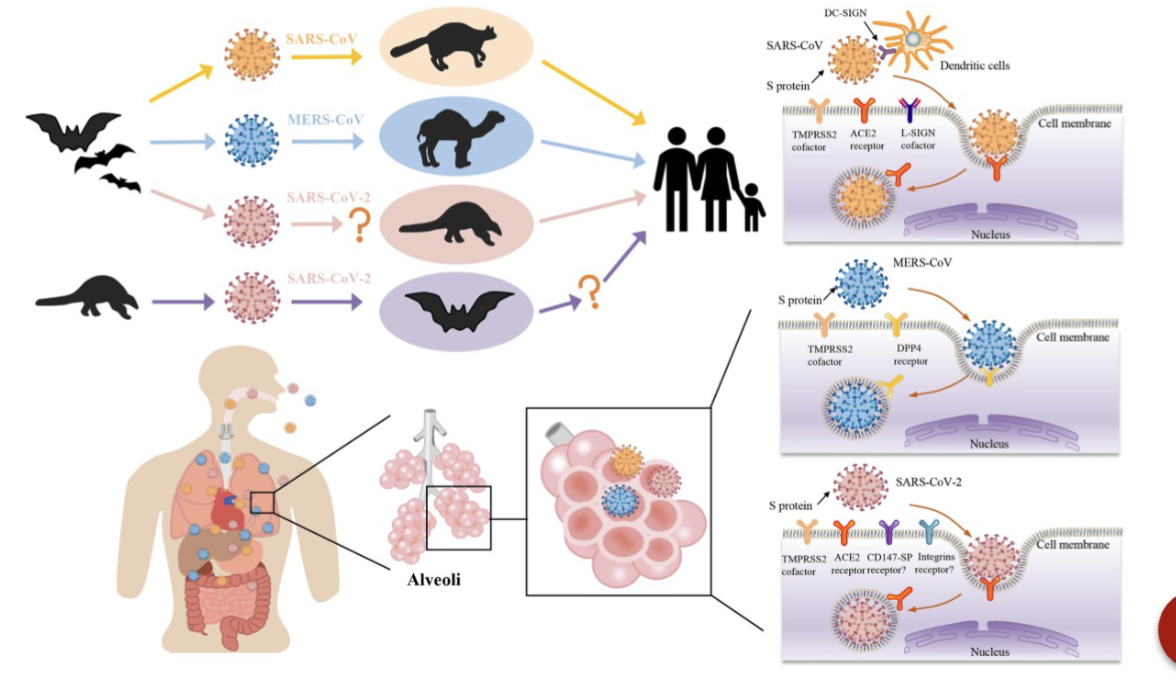
SARS-CoV-1
Mers-Cov
SARS-CoV-2
Severe acute respiratory syndrome (SARS):
China earliest case in healthcare worker.
8422 cases reported in August 2003 from 30 countries
Cause of severe acute respiratory syndrome (SARS) that emerged in 2003
Bat natural reservoir
Chills, fever, myalgia, headache, pharyngitis, rhinorrhea and diarrhea
Cough, shortness of breath and difficulty breathing, Acute respiratory distress syndrome (ARDS)
SARS diagnosis:
History of travel to Far East (China, Taiwan, Hong Kong, etc.)
Exposure to known cases of SARS
Symptomology
Radiographic evidence
Specimens: nasopharyngeal, oropharyngeal, bronchial aveolar lavage and lung tissue
Tests: immunofluorescence, nucleic acid assays, serology
Difficult to grow in culture
SARS diagnostic tests:
Conventional reverse transcriptase PCR (RT- PCR) and real time reverse transcriptase PCR( real-time RT-PCR) assay detecting RNA virus:
2 type of specimens- nasopharyngeal and stool specimen
OR
The same specimen collected on 2 or more occasions during the course of the illness.
SARS prevention:
Early recognition of infected patients
Hospitalization when necessary
Contact and airborne infection isolation precautions
Cough etiquette
SARS treatment:
None available at this time
Possible vaccine being investigated
Middle East Respiratory Syndrome (MERS): general characteristics:
April 2012, new virus that has not been seen in humans before. After that 26 countries reported the cases.
Middle East Respiratory Syndrome Corona Virus (MERS- CoV).
3-4 out of every 10 died with MERS (36% case fatality rate), can affect anyone.
Fever, cough, and shortness of breath, and can also include diarrhea, nausea, or vomiting
Complications- pneumonia, respiratory failure, septic shock
Zoonotic virus
Originated in bats and was transmitted to dromedary camels.
Most of the human cases do not have a history of direct contact with camels. Then the transmission may be indirect.
MERS clinical manifestation:
Acute respiratory illness, cough shortness of breath.
Gastrointestinal symptoms
More sever complications such as pneumonia and kidney failure.
Pre-existing conditions like diabetes, cancer, heart and lung disease or weakened immune system had severe cases.
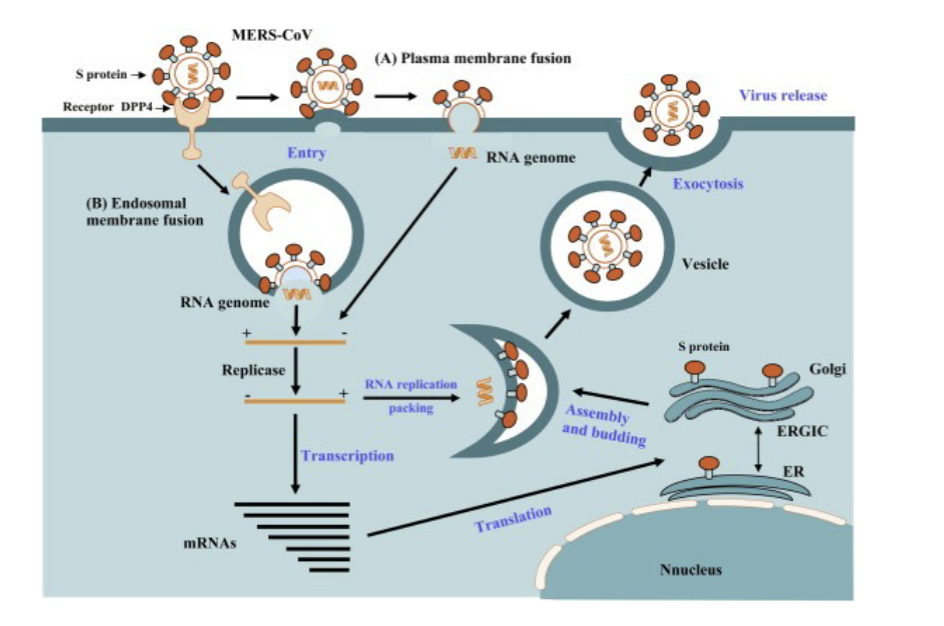
Life cycle of MERS
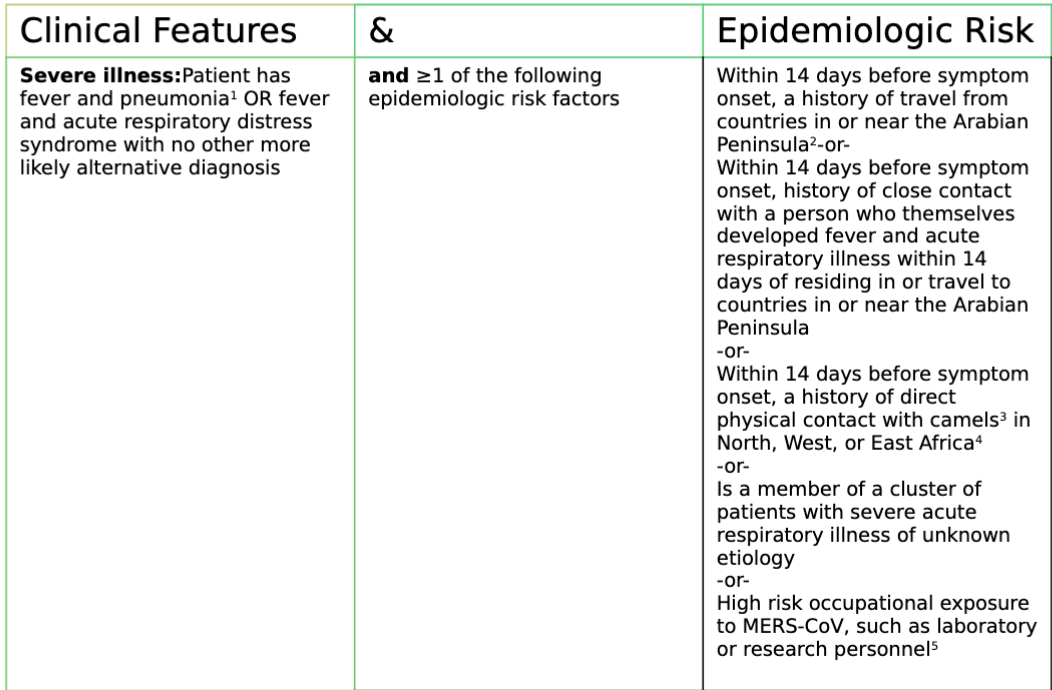
Criteria serving as guidance for who should be tested for MERS-CoV infection in the United States
MERS treatment:
Currently no medicine is available to cure.Treatment for is done to help support your body while it fights the disease. This is known as supportive care. Supportive care may include:
Pain medicines. These include acetaminophen and ibuprofen. They are used to help ease pain and reduce fever.
Bed rest. This helps your body fight the illness. Care during severe illness may include:
IV fluids. These are given through a vein to help keep your body hydrated.
Oxygen. Supplemental oxygen or assisted ventilation may be given. This is done to keep enough oxygen in your body.
Vasopressor medicine. These help to raise blood pressure that is too low from shock.
No antiviral drug
Care and support of vital organ.
Corticosteroids
Interferon
Convalescent serum
Intravenous immunoglobulin
Nitazoxanide
Ribavirin
Interferon plus ribavirin
MERS prevention:
Distancing, washing hand, cover your mouth, clean and disinfect frequently.
Coronavirus Disease (COVID-19) pandemic: general characteristics:
an infectious disease caused by the SARS-CoV-2 virus.
Nucleocapsid surrounded by envelope.
Envelope is lipoprotein in which proteins are embedded
Spike protein (S)
Membrane glycoprotein (M)
Envelope protein (E)
Non structural protein
Include enzyme which help in replication such as RNA dependent RNA polymerase, helicase, etc.
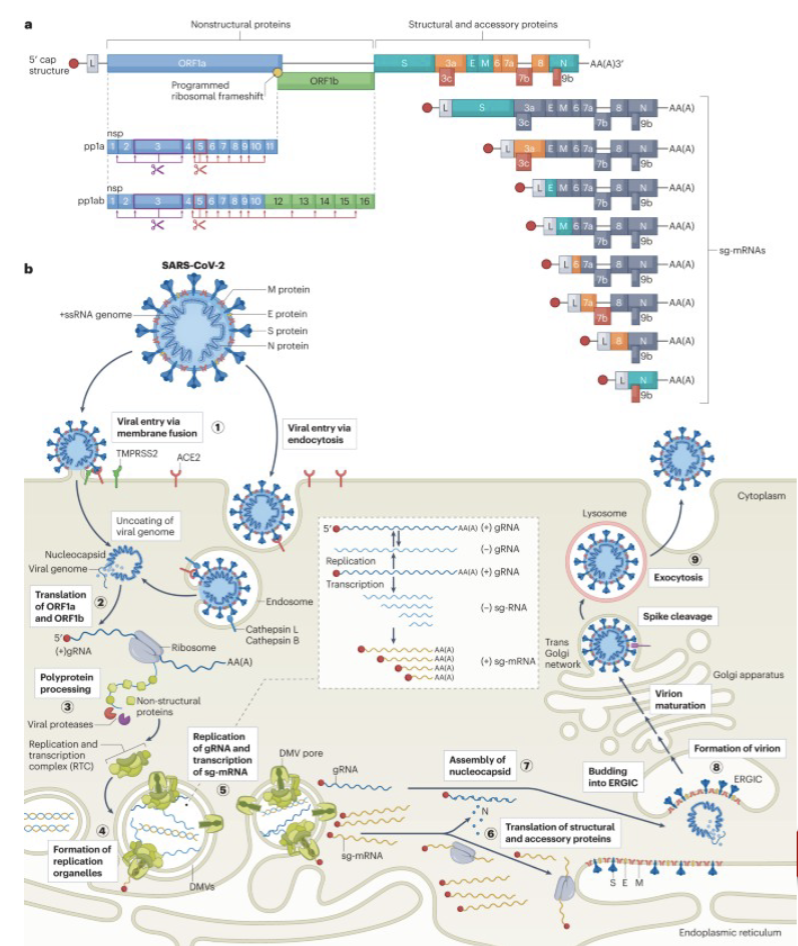
Life cycle of COVID-19
COVID-19 diagnostic tests:
Nucleic Acid Amplification Tests (NAATs).
Nucleic acid amplification tests (NAATs), including PCR tests, are more likely to detect the virus than antigen tests. NAATs tests are the “gold standard”
Antigen Tests: Antigen tests* are rapid tests that usually produce results in 15-30 minutes. Positive results are accurate and reliable. However, in general, antigen tests are less likely to detect the virus than NAAT tests, especially when symptoms are not present. Therefore, a single negative antigen test cannot rule out infection.
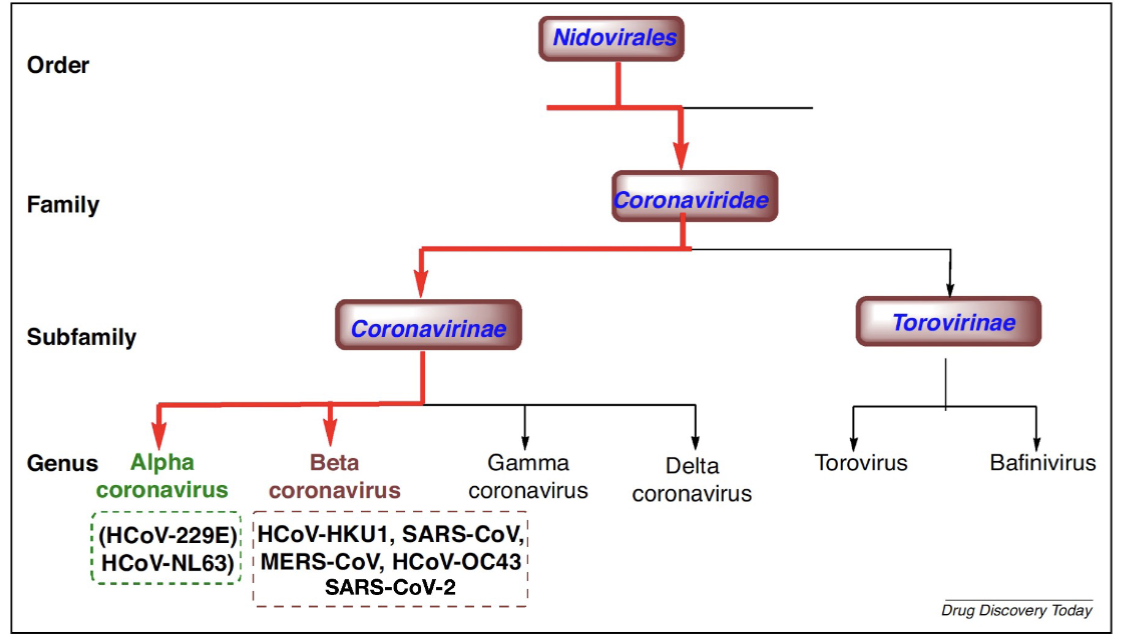
Flow chart of different viral families
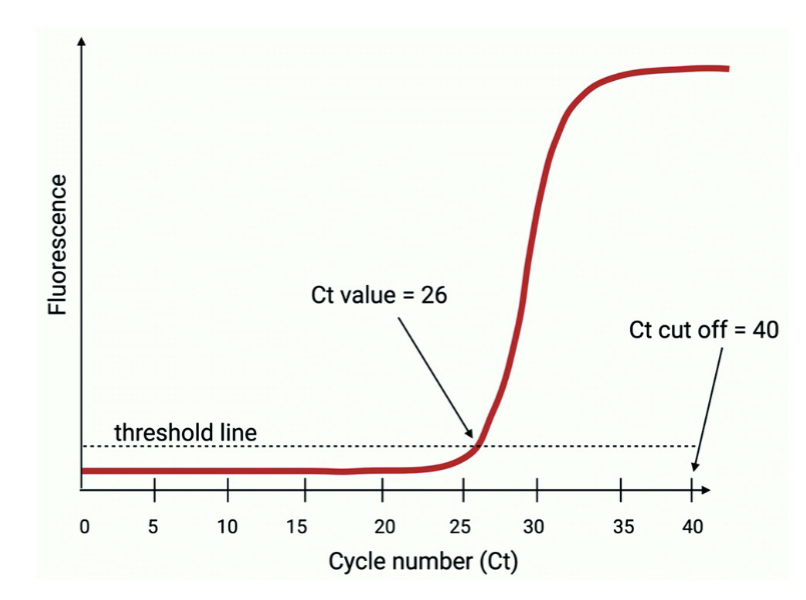
Cycle threshold (Ct) value:
The number of reaction cycles it takes to reach that threshold
CORONAVIRUS
COVID-19 treatment options:
FDA has authorized or approved several antiviral medications used to treat mild to moderate disease in people who are more likely to get very sick.
Paxlovid- Orally
Remdesivir – IV – for 3 days
Lagevrio- Orally
SARS-CoV-2 shares approximately 79.5% genomic homology with SARS-CoV while only about 50% similarity with MERS-CoV, indicating that SARS-CoV is closer to SARS-CoV2.
Orthomyxoviridae, orthos, “straight”; myxa “mucus”: Influenza Viruses:
Enveloped, single-stranded negative-sense RNA
a positive-sense RNA must be produced by an RNA- dependent RNA polymerase (RdRp) prior to translation
Influenza Viruses: general characteristics:
Enveloped, single-stranded, segmented, negative-sense RNA
Projections resembling spikes embedded in lipoprotein viral envelope
Hemagglutinin A (H)
Major glycoprotein of influenza virus
Responsible for attachment to host cells
Neuraminidase (N)
Glycoprotein enzyme on surface of virus
Responsible for release of viral progeny from cell
Combinations of 19 hemagglutinins and 9 neuramidases determine subtype such as H1N1, H5,N1, etc.
Influenza strains can show species specificity due to variation in hemagglutinin genes
Mutations enable the viral proteins to bind to receptors on host cells
passing from animals to humans can lead to a pandemic
Lack polymerases with proofreading activity (cannot find and fix errors during replication)
a characteristic of many RNA viruses
Lead to a high mutation rate
Mutations in hemagglutinin genes can allow the virus to easily pass from animals to humans leading to a pandemic
Have a high mutation rate they lack DNA polymerases which find and fix DNA
a characteristic of many RNA viruses
Are able to escape host defenses through antigenic variation
Influenza A most implicated in pandemics
Spanish flu (1918-1919, H1N1), Asian flu (1957-1958, H2N2), Hong Kong flu (1968-1969, H3N2), Avian flu (2003, H5N1), Novel swine flu (2009-????, H1N1)
Types A and B cause life-threatening infections in humans
Most cases of the flu are self-limiting
Complications, such as bronchitis and pneumonia, can be very serious in infants, elderly, and chronically ill patients
Appear in November to December and linger through March or April
Transmission is through respiratory aerosols
Antigenic Drift:
refers to the gradual accumulation of point mutations in the genes encoding the surface proteins hemagglutinin (HA) and neuraminidase (NA) due to the virus’s error-prone RNA polymerase.
If a mutation alters the structure of HA or NA in a way that helps the virus escape pre-existing immune recognition, it can give the virus a selective advantage.
Effects of antigenic drift:
Causes seasonal flu epidemics, requiring frequent updates to flu vaccines.
Results in milder but recurrent outbreaks since population immunity is only partially effective.
Antigenic shift:
a rapid and dramatic genetic change that occurs when two
different influenza A viruses infect the same host and undergo reassortment, leading to a new viral strain with a completely different HA or NA subtype.
This reassortment can generate a completely new influenza A virus with a novel HA and/or NA protein, against which humans have little to no immunity.
Antigenic effects:
Causes pandemics because the new strain can spread rapidly in a population with no pre-existing immunity.
Influenza type A infections:
Found to infect swine, horses, birds, and other animals
Asian flu and Hong Kong flu caused by strains resulting from reassortment of human and avian viruses
Wild birds are the only animals having all subtypes of influenza A
H5N1 is the etiologic agent of the avian or bird flu
2003 strain of H5N1 responsible for outbreak in southeast Asia
H5N1 strains able to merge genes with strains found in hosts such as humans and birds
Outbreak continues to this day and is a major cause of concern because of increased virulence in humans
Infection acquired by close contact with fowls
No cases of human-to-human transfer documented at this point
Influenza type A clinical manifestations:
Often asymptomatic or mild
Symptoms: fever, chills, myalgia, sore throat, and cough
Fatalities associated with viral pneumonia or secondary bacterial infection
Influenza type A preventation:
Vaccination is most effective method
Live attenuated vaccine (weakened virus)
Individuals with allergies to chicken eggs should not be vaccinated because the virus is propagated in chicken eggs
Influenza type A specimens of choice:
Nasal washings or aspirates are best
Throat swabs can be used but contain less virus
Influenza type A screening:
Rapid immunoassay
Monoclonal antibody assay detects either influenza A or B or both
sensitivity about 80% depending on specimen quality
Influenza type A more sensitive assays:
direct immunofluorescence
cell culture
Primary monkey kidney and A-549 (human lung carcinoma)
Cytopathic effect (CPE) in 3-5 days
Cell rounding
Vacuoles in cell lawn
Hemabsorption
Influenza virus-infected cells absorb guinea pig RBCs
Hemagglutinin binds to sialic receptor on blood cells
RT-PCR:
Detect viral RNA
Influenza type B: general characteristics
Causes a milder upper respiratory disease in younger children
Complications such as pneumonia are rare
Reye’s syndrome with use of salicylates (aspirin) to reduce fever in children
Influenza type C: general characterisitcs:
Associated with a common mild illness in early childhood
Influenza Vaccination:
Those at risk for complications and healthcare workers should be vaccinated
New vaccine reformulated each year because each epidemic is antigenically different.
Vaccine confers immunity to specific strains or subtypes
2 types
Killed: TIV trivalent (3 strains; usually A/H1N1, A/H3N2, and B) inactivated vaccine
Live: LAIV nasal spray (mist) of live attenuated influenza vaccine.
Individuals with allergies to chicken eggs should not be vaccinated because the virus is propagated in chicken eggs
Changes in virus (surface antigens) occur so immunity to one strain does not prevent susceptibility to another strain
Orthomyxoviridae: Treatment:
Oseltamivir (Tamiflu) effective in children and pregnant women
Zanamivir, a neuraminidase inhibitor, used in prophylaxis and treatment of influenza A and B- inhaled medication not recommended for patients with respiratory illness.
Baloxavir Marboxil (Xofluza)- effective in older- single dose.
Amantadine and rimantadine effective against influenza A but not influenza B
Differentiation is very important
Peramivir (Rapivab)- Intravenous antiviral for hospitalized patients or those unable to take oral medication.
Paramyxovirus family: categorization:
Enveloped, helical RNA
Respirovirus genus
Parainfluenza virus
Pneumovirus genus
Respiratory syncytial virus (RSV)
Metapneumonia virus
Morbillivirus genus
Measles virus
Canine distemper virus
Rubulavirus genus
Mumps virus
Parainfluenza viruses: general characteristics:
Acute respiratory illnesses in children
Croup, an upper respiratory infection, causing laryngitis and associated with characteristic hoarse cough like the bark of a seal
Pneumonia and bronchitis in infants
Transmission via inhalation of droplets or person to person contact
Parainfluenza viruses: diagnosis & prevention:
Specimen
throat swabs or nasopharyngeal washings
Direct fluorescent antibody to demonstrate virus in respiratory secretions
Cell culture: primary monkey kidney, human neonatal kidney, or human lung cancer
CPE can take up to 14 days
Round, granular cells and syncytia
Immunofluorescence or hemadsorption on cells exhibiting CPE
Parainfluenza viruses: treatment:
No vaccine or effective treatment; hand hygiene is best prevention
PCR is more popular test
Respiratory Syncytial Virus (RSV): general characteristics:
Named for characteristic CPE
Syncytia are created when cells merge to form large, multinucleated cells
Major cause of upper respiratory diseases in infants
Range from mild disease, to bronchiolitis and pneumonia, to severe respiratory distress and death
Increased risk of RSV pneumonia in premature infants or those with congenital heart defects or chronic lung disease
Pneumonia increases risk of asthma later in life
Most infections in late winter and early spring
Peak in February and March
Nursery outbreaks associated with high infection rates and some fatalities
Transmission via direct contact with respiratory secretions
Respiratory Syncytial Virus: infection in adults:
Acute, febrile, upper respiratory infection
may be chronic and severe in elderly
Can lead to bronchiolitis and pneumonia
RSV diagnosis:
Specimen: nasal washing or aspirates
Procedure: direct fluorescent antibody technique
Rapid antigen tests or more sensitive molecular tests like RT-PCR (real-time reverse transcription-polymerase chain reaction) to detect the virus
Direct immunoassays
enzyme immunoassays (EIA) used in most labs
sensitivity & specificity > 80%
Direct fluorescent antibody or viral cultures should be used to confirm negative direct immunoassay tests
Cell culture: HEp-2 (human larynx cancer) and H292 and A-549 (human lung cancers) for demonstration of syncytia in 3-5 days
RSV prevention & treatment:
No vaccine is available
hand washing is important control measure
Ribavirin is an effective antiviral drug
Measles virus: general characteristics:
Enveloped, ssRNA
Also known as rubeola virus
Highly infectious disease spread by respiratory
aerosols
Measles clinical manifestation:
Incubation period of 10 days
Symptoms: fever, cough, coryza (runny nose), conjunctivitis, and generalized erythematous rash
Koplik’s spots: bright red spots with white centers on the oral mucosa are diagnostic and, if apparent, no laboratory diagnosis required
Skin rash and Koplik’s spots are diagnostic and laboratory diagnosis is not needed
Measles diagnosis:
Laboratory diagnosis when required
Specimen: NP swab or urine
Cell culture: human kidney cells showing distinctive multinucleated cells
Serologic tests to demonstrate IgM antibodies
acute phase of infection
EIA or serum neutralization assays used to obtain antibody titers
Measles vaccination:
Best means of protection
Prior to vaccine, as much as 95% of population infected at sometime during life
Vaccine given at the age of 18 months as a part of the measles, mumps, rubella (MMR) vaccine
Booster administered before 5th birthday
In 2019 there were 1282 cases reported in 31 states in unvaccinated children
Mumps virus: general characteristics:
Enveloped, ssRNA
Cause of mumps or epidemic parotitis, a self- limiting systemic viral disease
Transmission via droplets of infected saliva
Symptoms: painful swelling of parotid glands, fever, headache, and sore throat
Pancreas, ovaries and testes can be infected
Orchitis can lead to infertility
Photo shows mumps due to infection of the parotid or salivary glands by the virus. The resulting neck swelling is easily recognized.

Mumps virus: laboratory diagnosis:
Specimen: saliva or urine
Direct detection through immunofluorescence
Diagnosis most commonly made through serologic testing using EIA to measure IgG and IgM
4-fold rise in titer is diagnostic
Other serologic tests include hemagglutination inhibition and complement fixation
Mumps virus prevention:
Immunization with MMR vaccine
Togaviridae: Rubella virus: general characteristics:
Enveloped, ssRNA
Causative agent of rubella or German measles
also called 3-day measles or epidemic roseola
Transmission via inhalation of respiratory droplets
In young children, rubella is mild and in most cases,
asymptomatic
In adults, infection is more severe
Symptomatic infection: fever, rash on face, trunk, or limbs, red papules on the soft palate, conjunctivitis, and lymphadenopathy
Rubella: Congenital infection:
Transmission from infected mother to fetus
With primary infection, there is no protective antibody to cross placenta and protect fetus
Infection during 1st trimester can result in severe developmental defects
cataracts, glaucoma, deafness, congenital heart disease, mental retardation, spontaneous abortion, premature birth, and fetal death
Rubella virus: Postnatal infection:
transmission through breast milk but usually a mild disease
Rubella diagnosis:
Specimens: saliva, nasopharyngeal secretions, and urine
Can be cultured on African green monkey kidney cells but does not produce CPE
Rarely used
PCR or immunofluorescence to confirm presence of virus
Serologic tests
Passive hemagglutination
red cells or latex particles coated with viral antigen
EIA for IgM or IgG antibodies
IgM indicates acute illness and used to diagnose congenital infection in newborn
IgG indicates current immune status
Rubella prevention:
Attenuated vaccine for children around 1 year old
Part of MMR vaccine
Booster given again before child starts school
Arbovirus infections: general characteristics:
Name derived from arthropod-born viruses
Often cause severe or fatal infections
Humans are not native hosts and have no inherent resistance
Insect vector is most often the female mosquito
Monkeys, horses, birds, reptiles, and amphibians serve as sources of infection
Infections most prevalent during late spring, summer, and early fall when mosquitoes and ticks are most active
Encephalitis viruses symptoms
fever, nausea, headaches, stiff neck and back, photosensitivity and confusion
in severe cases, coma and death
Even in nonfatal cases neurological sequelae include mental deficiencies, deafness, blindness, and paralysis
Arboviruses: Alphaviruses: general characteristics:
Eastern equine encephalitis virus (EEE) (2019- 29 cases in US)
Western equine encephalitis virus (WEE)
Venezuelan equine encephalitis virus (VEE) of North, Central and South America
Arboviruses: Flaviviruses:
St. Louis encephalitis virus (SLE)
West Nile virus
Originated in Africa
Appeared in U.S. in 1999
LI- elderly
Yellow fever virus
Africa and South America
Causes degeneration of liver
causing jaundice, so the name yellow fever, kidneys, and heart
Dengue fever virus
Worldwide
Associated with internal bleeding, loss of plasma, and shock
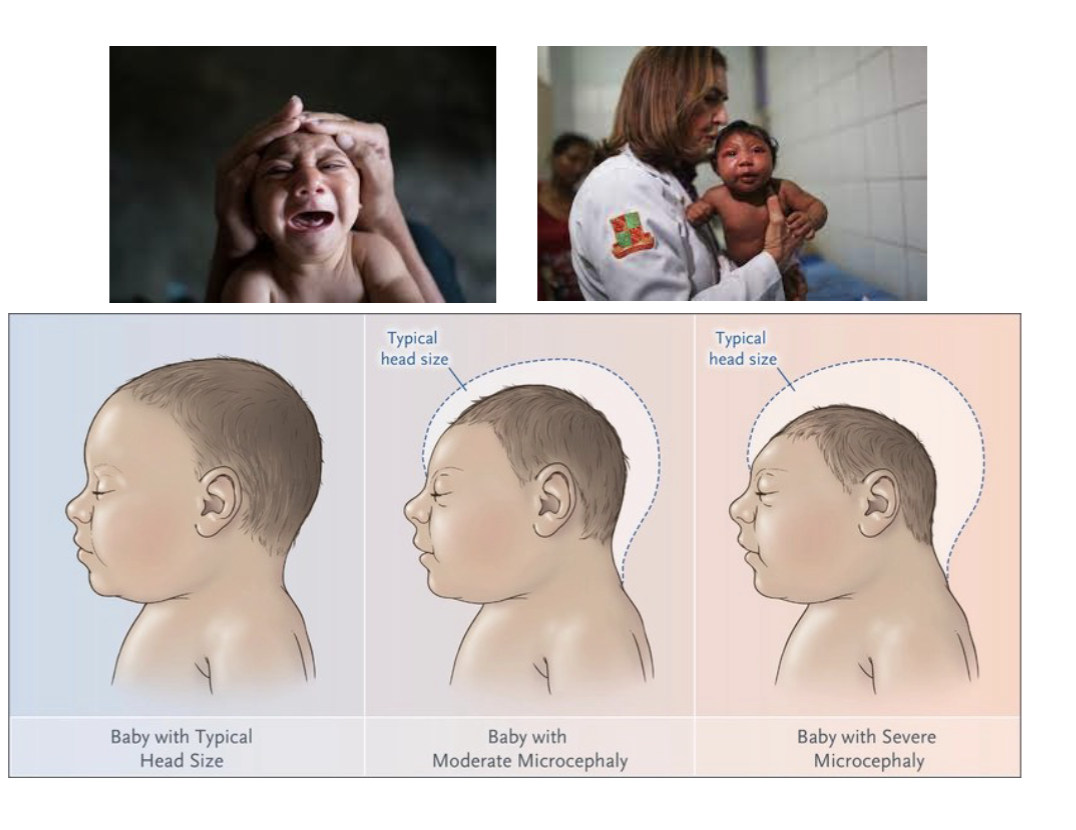
Zika virus:
Started in Brazil in 2015. Spread by mosquitos. Can cause mild disease also Guillain-Barre (transient paralysis)
Virus can be passed to fetus. Causes birth defect (microcephaly)
Gastroenteritis Viruses: general characteristics:
Noroviruses, rotaviruses, and adenoviruses (already discussed)
Cause illnesses associated with vomiting, diarrhea or both
Often referred to as “stomach flu”
Spread via fecal-oral route
Noroviruses: general characteristics:
Nonenveloped, ssRNA
Very hardy and not inactivated by pH or heat
Symptoms: low-grade fever, abdominal pain, vomiting, and diarrhea
Complete recovery after 1-5 days
Nearly 50% of all foodborne outbreaks of gastroenteritis caused by noroviruses
Can be serious or fatal in older adults
Can be one of the causative agents of traveler’s diarrhea
Isolated during outbreak in Norwalk, Ohio in 1968 (Norwalk virus)
Symptoms: “Winter vomiting bug”
Complete recovery after 1-5 days
Outbreaks occur in closed or semiclosed communities, such as long- term care facilities, dormitories, and cruise ships
Noroviruses; diagnosis:
Specimen of choice is feces but vomitus acceptable
Molecular techniques such as real-time PCR
Electron microscopy can identify the small round virus but is not practical for most laboratories
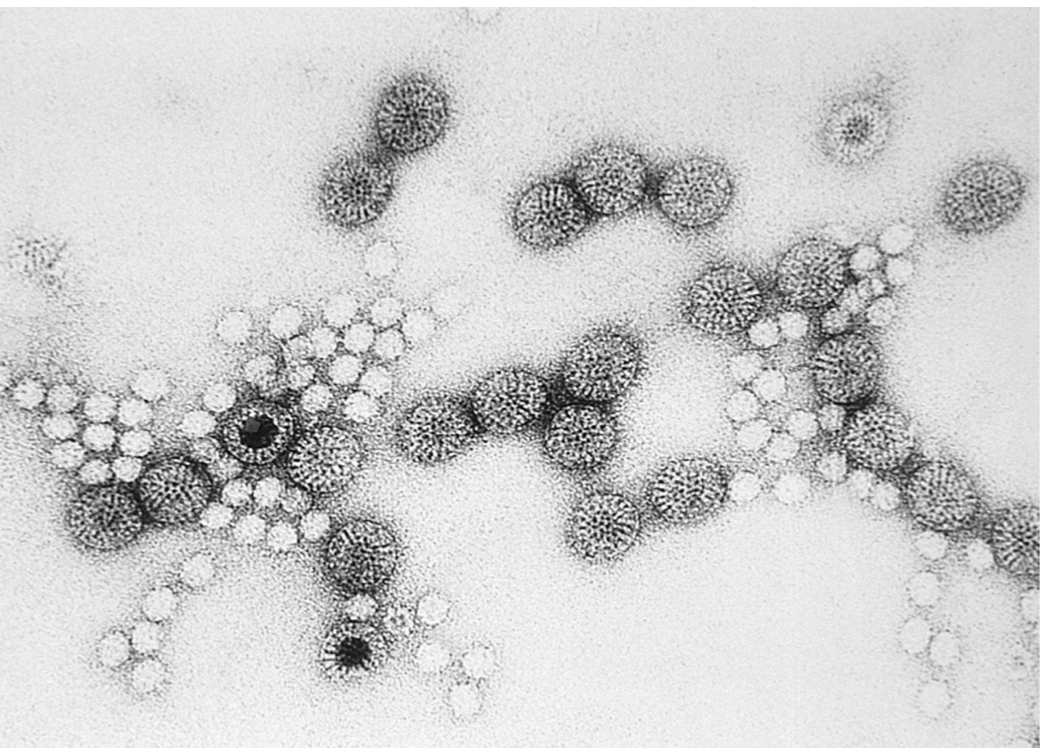
Rotoviruses: general characteristics:
Small, nonenveloped, dsRNA
“Rota” is Latin word for “wheel” and describes morphology of the virus
Double capsid seen with electron microscope resembles wheel with wide hub and short spokes radiating from hub to rim of the wheel
Transmission via fecal-oral route
Transmission is often via contaminated water and foods such as oysters, clams, and raw shellfish
Infection may be asymptomatic, mild, or severe dehydrating diarrheal illness
Symptoms: fever, vomiting, diarrhea, and dehydration due to water loss
Most cases in infants 16-24 months of age
Most common cause of severe diarrhea
Leading cause of mortality
In developing countries, many children succumb to complications of infection
Rabies Virus: general characteristics:
Family Rhabdoviridae; ssRNA
Transmission via bite of infected animals
possibly transplant surgery
Virus shed in saliva of infected animals
dogs, cats, foxes, raccoons, and bats
Rabies always fatal once symptoms appear
Virus enters peripheral nerves and travels to central nervous
system
Causes encephalitis and myelitis
Symptoms
May take months to show
Pain at the bite site
Flu-like symptoms
CNS invasion associated with:
Insomnia, anxiety, confusion, hallucinations, and hydrophobia
Eventually host succumbs to coma and death
Rabies Virus: diagnosis & prevention:
Biopsy of brain demonstrating presence of Negri bodies
Seen in 70-80% of cases
Negri bodies are eosinophilic inclusions in cytoplasm of neurons
EIA testing to detect antibodies
Rapid fluorescent-focus inhibition test (RFFIT) for antibodies
Flow cytometry could be used to detect rabies virus antigen in infected cells
Prevention: vaccination in humans and animals
Rabies treatment:
Virus must travel from bite site to brain and spinal cord to cause serious damage but is extremely slow
Postexposure treatment consists of vigorous cleansing of wound site
Administration of vaccine and immunoglobulin is extremely effective in providing protection from lethal effects
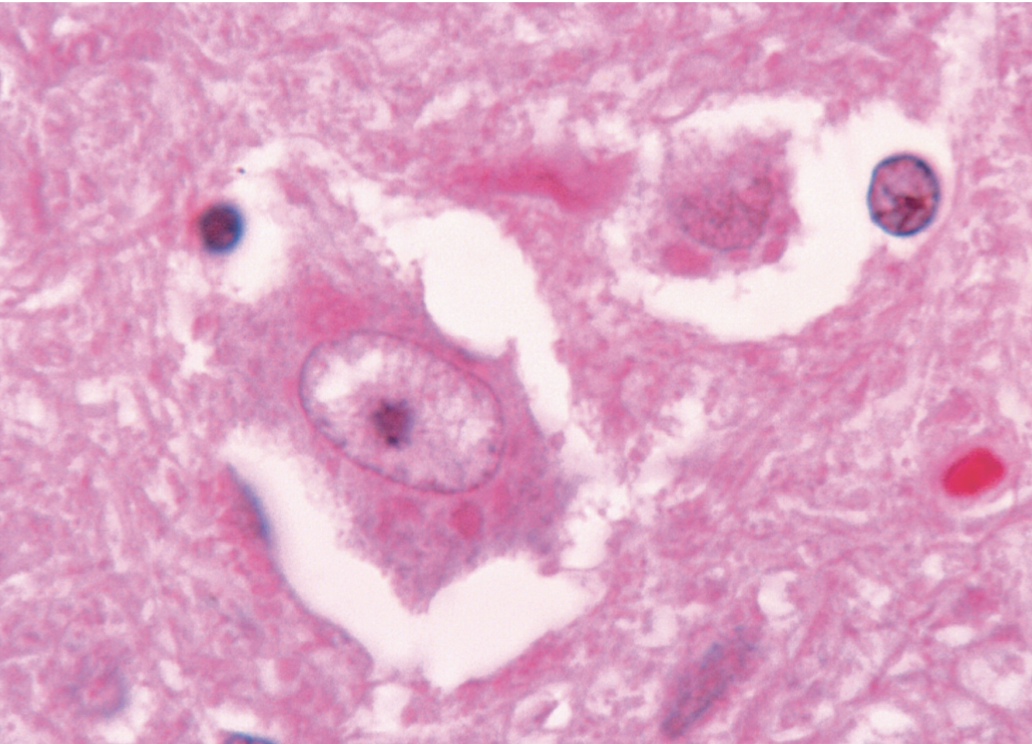
Negri bodies, as seen in the neural cell in the center, is characterisitc for rabies
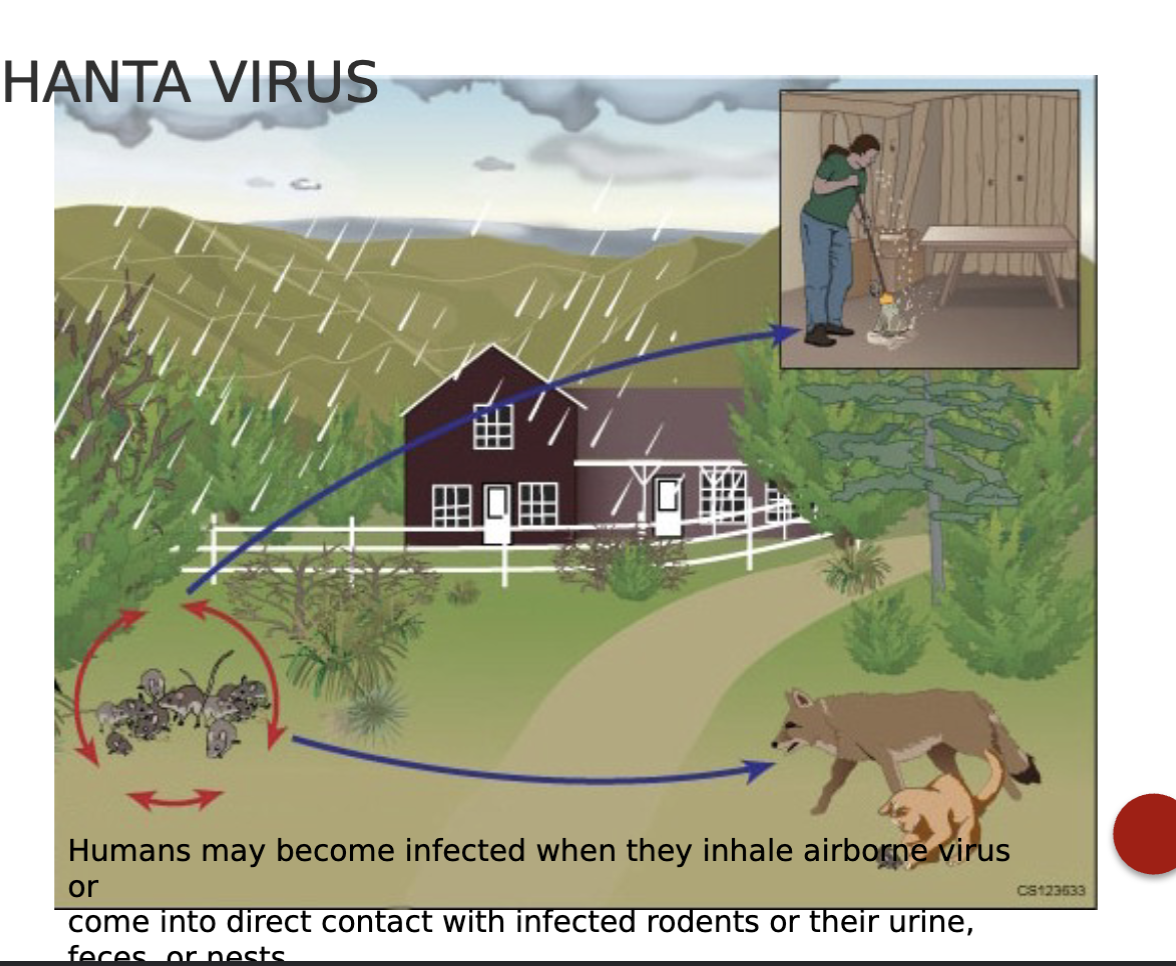
Emerging Viruses: Hantavirus: general characteristics:
RNA virus in the family Bunyaviridae
Produces 2 distinct diseases
Hemorrhagic fever with renal syndrome (HFRS)
Hanta virus pulmonary syndrome (HPS)
Pulmonary syndrome fills the lungs with fluid so patient literally drowns
Transmission: aerosolized urine and feces of rodents
Appeared in 1993 in four corners area of the U.S. (Arizona, Colorado, Utah, and New Mexico)
Has the potential a bioterrorism agent
Humans may become infected when they inhale airborne virus or come into direct contact with infected rodents or their urine, feces, or pests
Emerging viruses: Rift valley fever virus: general characteristics:
Family Bunyaviridae
Primarily found in cattle in Africa
Transmission via mosquitoes or contact with animals
Causes ocular infections, meningoencephalitis, or hemorrhagic fever
Primarily found in cattle