childhood and adolescent psychological problems (Davey - chapter 16) | Quizlet
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
externalizing disorders
- disorders based on outward-directed behaviour problems
- aggressiveness, hyperactivity, non-compliance or impulsiveness
(also internalizing disorders more inward-looking and withdrawn behaviours like - depression, anxiety, and active attempts to socially withdraw)
identification and diagnosis
- What is normal for a particular age? (e.g. bed wetting above 5 is not)
- children often don't have the abilities to express themselves properly
- lack of self-knowledge, communication skills, preciseness
- cultural norms
- changes occur rapidly -> can escalate quickly and dramatically
childhood psychopathology as the precursor of adult psychopathology
- preschool behaviour problems predict psychopathology in alter life
- developmental psychopathology:
-> research concerned with mapping how early childhood experiences may act as a risk factor for later diagnosable psychological disorders
-> attempts to describe the pathways by which early experiences may generate adult psychological problems
- childhood experiences may contribute in several ways:
-> e.g. anxiety: persists to anxiety later in life
-> adverse effect on subsequent development and indirectly lead to different forms of maladjustment
-> precursor for more severe disorder (phobia - panic disorder)
-> e.g., maltreatment influences indirect: heightened reactivity to stressors etc.
-> may change completely or disappear
developmental psychopathology
- An area of research concerned with mapping how early childhood experiences may act as risk factors for later diagnosable psychological disorders.
-It also attempts to describe the pathways by which early experiences may generate adult psychological problems.
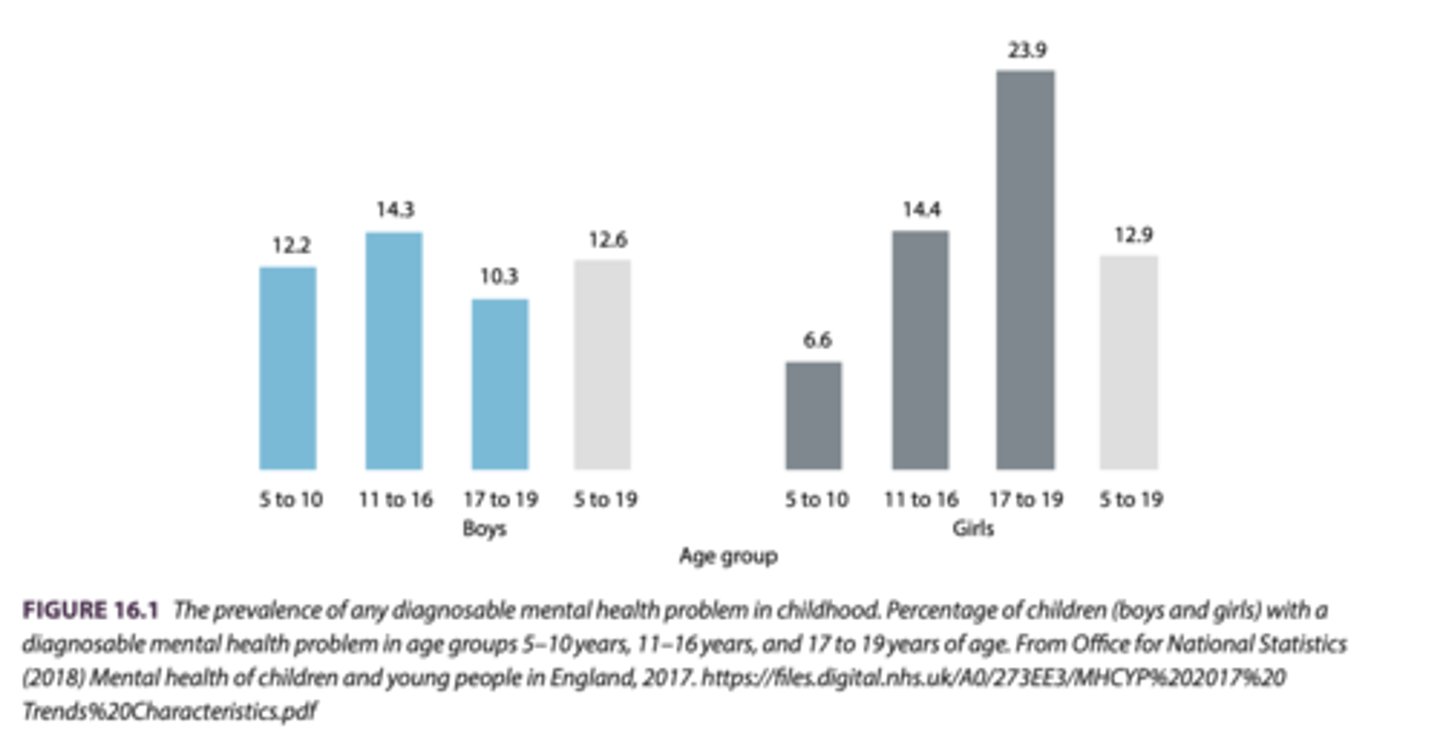
prevalence of childhood and adolescent psychological disorders
- 10-20% of children and adolescents have a diagnosable disorder
-> boys often conduct disorders
-> girls emotional disorders
- co-morbidity common (2% more than one disorder)
- risk factors include:
-> lone parents, parental psychopathology, repeated early separation from parents, harsh or inadequate parenting, exposure to abuse or neglect, and adverse peer group influences
2 disruptive behaviour problems in DSM-5
attention deficit hyperactivity disorder (ADHD) and
conduct disorder
- are characterised by impulsive, disruptive, and poorly controlled behaviour.
attention deficit hyperactivity disorder (ADHD)
- manifest itself as lack of attention, hyperactivity, or impulsivity.
- ADHD significantly affects educational achievement and social integration.
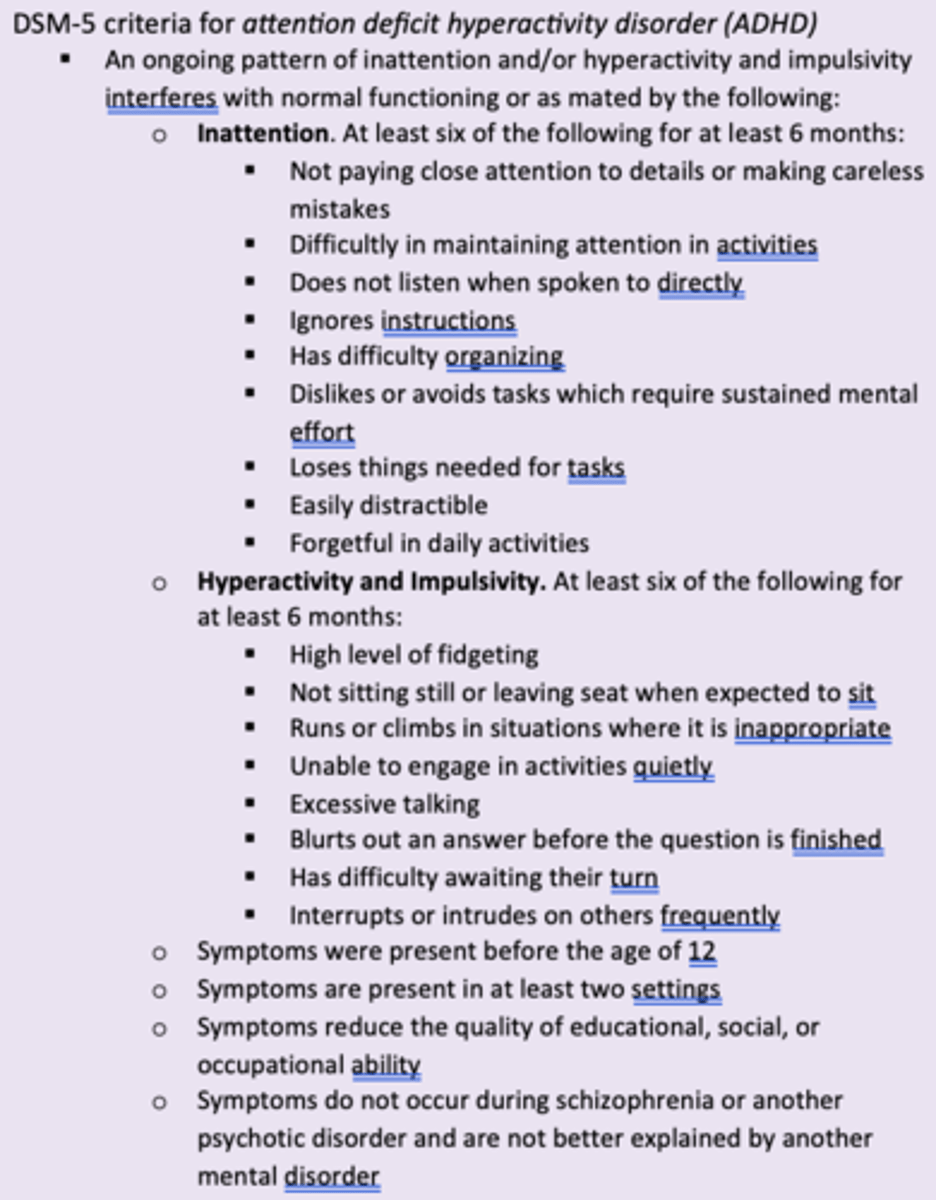
2 ADHD subtypes
-> ADHD, predominantly inattentive presentation (just enough symptoms for inattention)
-> ADHD, predominantly hyperactive/impulsive presentation (just enough for H./I.)
=> if both elements are present it is called combined presentation
- 50% of combined presentation diagnosis will also be diagnosed with ODD or CD
- violations of social norms and basic rights
- usually first recognized by parents after begin school
prevalence of ADHD
- 5% of school children and 2.5% of adults diagnosed
- half of those diagnosed as children will carry the diagnosis into adulthood
-> more common in boys
Aetiology of ADHD
- biological
(genetics, neuroscience, prenatal factors,envrionmental toxins)
- psychological factors
(parent-child interaction, TOM deficits,)
biological factors of ADHD
- particularly important -> vulnerability in specific environmental situations
genetics:
- one of the most heritable psychiatric disorders (76%)
- abnormalities with dopamine, norepinephrine and serotonin
neuroscience:
- smaller brain and develop more slowly
-> main areas affected being the frontal, parietal, temporal, and occipital lobes, frontal cortex, basal ganglia, cerebellum
=> e.g. impaired executive functioning
prenatal factors:
- smoking and drinking
- birth complications
environmental toxins:
- food colorings…
- exposure to nicotine
psychological factors
Parent-child interactions:
- appears to run in families
- parents with ADHD may reinforce any symptoms, or they may be less effective parents
- Dysfunctional parent–child interactions may contribute (no evidence that these are sole cause).
Theory of mind deficits:
- some suggest ADHD sufferers have theory of mind (TOM) deficits -> studies are inconsistent
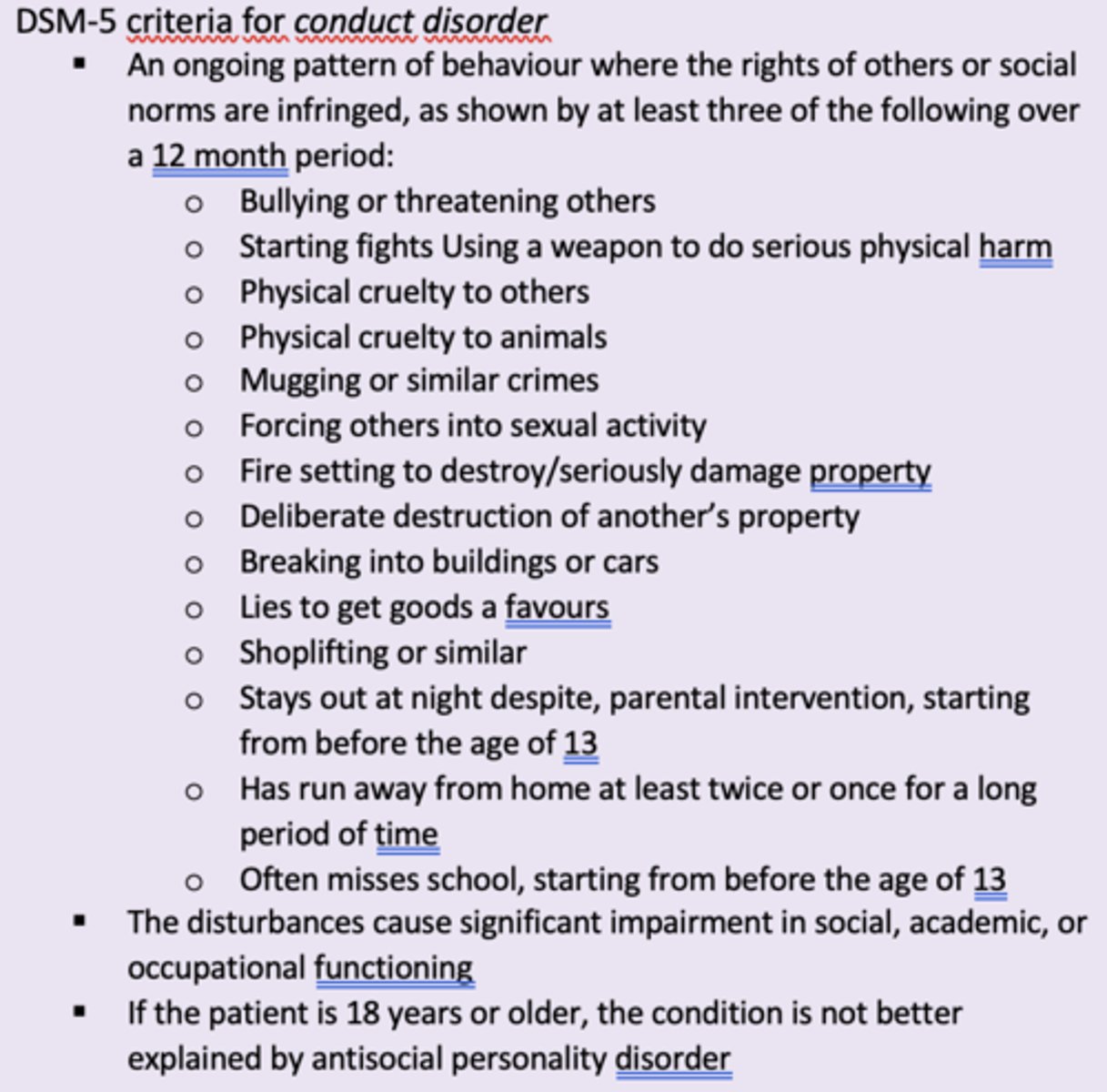
conduct disorder (CD)
- behaviour that is aggressive, causes vandalism, property loss or damage, deceitful- ness and lying, and serious violation of accepted rules
- regularly co-morbid with impulse disorders
- more common in males
- lack of inhibition to control impulses
- two main subtypes of conduct disorder:
1. childhood-onset conduct disorder:
- onset of at least on criterion characteristic prior to 10 years of age
2. adolescent-onset conduct disorder:
- symptoms only after the age of 10 years
- less physical aggression
- better peer relationships
two main subtypes of conduct disorder
1. childhood-onset conduct disorder:
- onset of at least on criterion characteristic prior to 10 years of age
2. adolescent-onset conduct disorder:
- symptoms only after the age of 10 years
- less physical aggression
- better peer relationships
oppositional defiant disorder (ODD)
A mild form of disruptive behaviour disorders reserved for children who do not meet the full criteria for conduct disorder.
prevalence of CD
- lifetime prevalence 9.5%, median age of onset is 11.6 years
- 4-16% in boys (mostly violent behaviour)
- 1.2-9% in girls (lying, running away, theft, prostitution, ...)
biological factors of CD
Genetic factors:
- genetic component with heritability ca. 45-67%
- serotonin and monoamine neurotransmitter abnormality
-> socio-emotional information processing in prefrontal cortex
Neuropsychological deficits:
- associated with neuropsychological deficits in cognitive functioning
-> executive functioning, verbal IQ, and memory
-> reduced activity in amygdala, ventral stratium and prefrontal cortex (emotion and reward)
Parental factors:
- maternal smoking and drinking during pregnancy
- prenatal (and postnatal) malnutrition, especially deficits in proteins, iron, and zinc
issues related to CD diagnosis
- under 18 years of age
- social context has to be taken into account (e.g. stealing bc of poverty?)
- might sometimes be oppositional defiant disorder (ODD)
-> mild form: do not meet the full criteria for conduct disorder
-> might be a precursor
psychological factors of CD
family environment and parent-child relationship:
- unemployment, parents with antisocial personality disorder, many conflicts, poverty, social deprivation…
- nature of parent-child interactions during childhood
-> abuse, disrupted care, maltreatment, harsh parenting, inconsistency in discipline
Media and peer influences:
- mimic the violent activities that they see around them in the media or by their peers
- media violence has its effect primarily on children who are already emotionally and psychiatrically disturbed
-> vicious cycle of associating with aggressive peers - more exposure violence
-> being rejected by peers has been shown to cause increased aggressiveness
cognitive factors:
- fail to acquire a moral awareness - achieve goals by e.g., using violence
socioeconomic factors:
-poverty, low socioeconomic class, unemployment, urban living, poor educational achievement
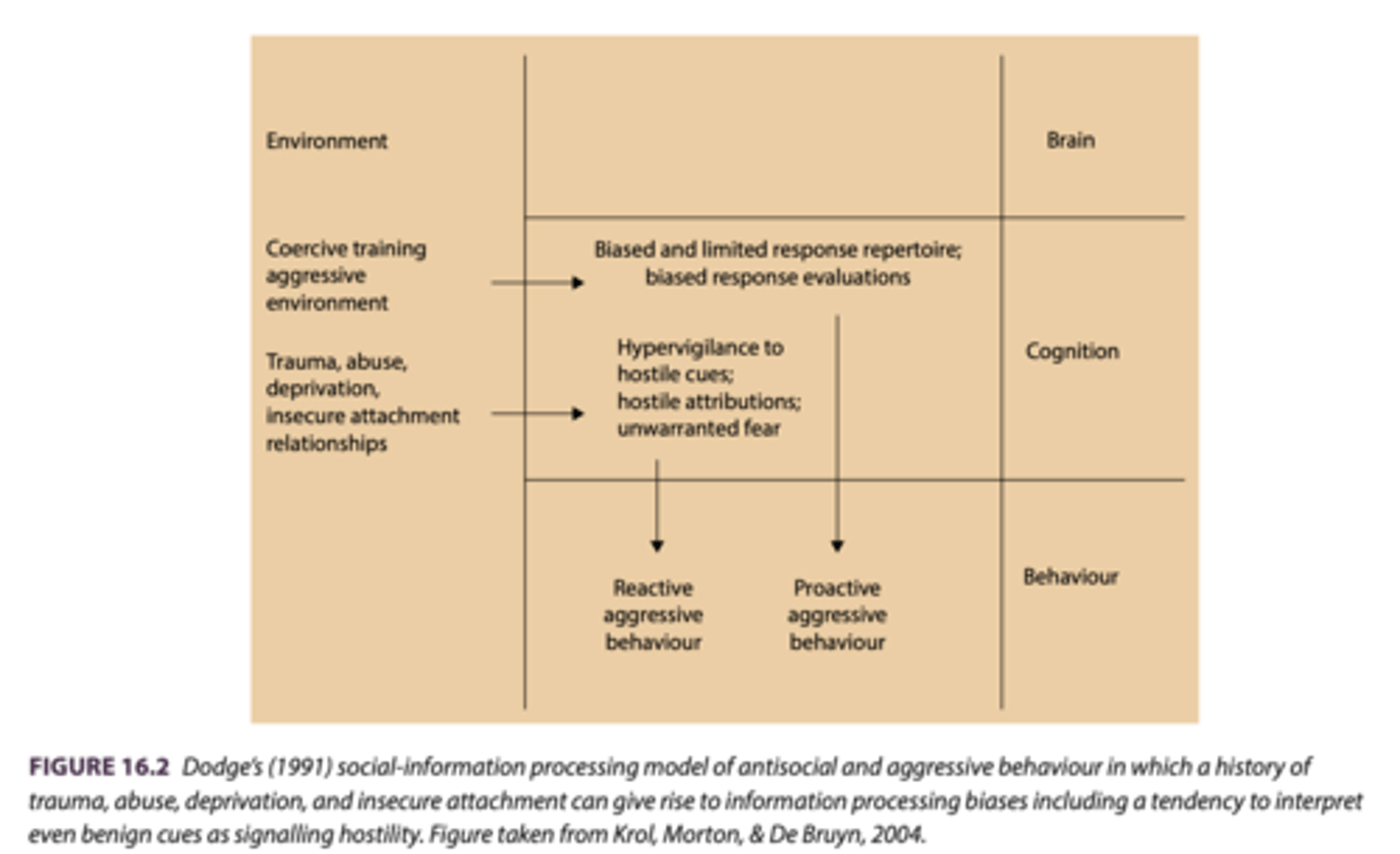
cognitive factors of CD
- fail to acquire a moral awareness - achieve goals by e.g., using violence
-> high interpretation/information bias (e.g. more interpreting others behaviour as violent)
- social-information processing model of antisocial an aggressive behaviour:
-> hostile attributional bias:
=> interpret not only ambiguous cues as signalling hostility, but also many cues that are generated with benign intentions
socioeconomic factors of CD
- associated with poverty, low socioeconomic class, unemployment, urban living, poor educational achievement
- these things may even be a cause rather than a consequence
childhood anxiety
- anxiety is primarily manifested as with drawn behaviour (internalising).
- child avoids activities where they may have to socialise with others
- will be clinging and demanding of parents and carers they will express a desire to want to stay at home
- Many childhood anxiety disorders do tend to be recognisable as those also found in adulthood
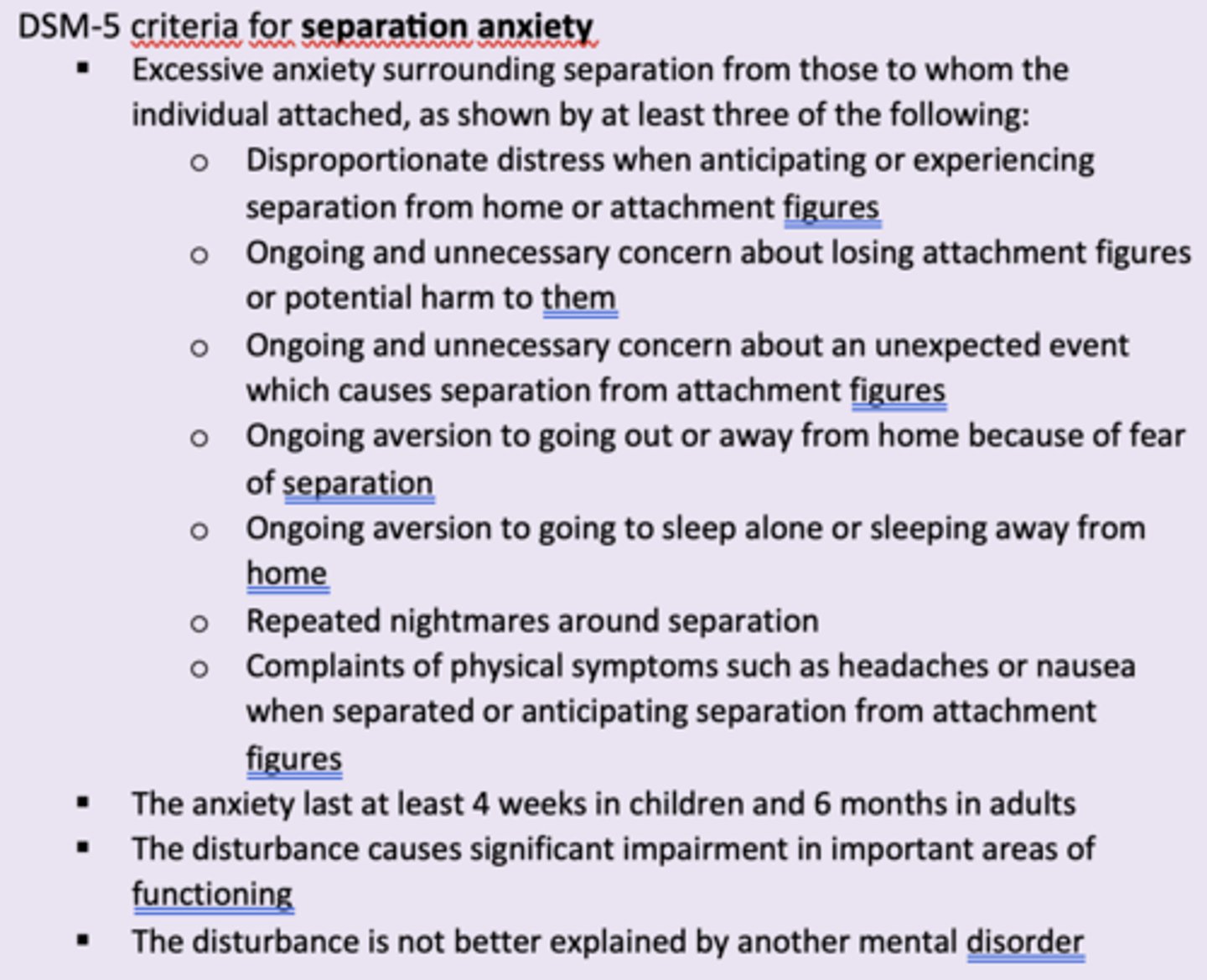
seperation anxiety (DSM-5)
- intense fear of being separated from parents or carers.
- commonly found in many children at the end of the first year of life but usually gradually subsides
-> may cause social anxiety in school age
- can be triggered by specific life stressors
- prevalence approximately 4% in children between 6 and 12 years of age
obsessive compulsive disorder (OCD)
- very similar to adult OCD
- intrusive, repetitive thoughts, obsessions and compulsions
-> fear of contaminations and aggression main fears
-> compulsions (e.g. behavioural ritulas) without obsessions (e.g. intrusive thoughts) can be quite common in children
- boys have an earlier age and more likely to have sexual obsessions
- girls exhibit more hoarding compulsions
- age of onset can be as early as 3-4 years but mean age of onset is more likely to be around 10 years
- co-morbid with tic disorders or Tourette's syndrome, anxiety and eating disorders
tic disorders
Uncontrollable physical movements such as facial twitches, rapid blinking or twitches of the mouth.
Tourette's syndrome
A disorder in which motor and vocal tics occur frequently throughout the day for at least 1 year.
internalizing disorders
- disorder represented by more inward-looking and withdrawn behaviours
- depression, anxiety, and active attempts to socially withdraw
- Childhood anxiety and depression
- Diagnosable forms of childhood anxiety include separation anxiety, OCD, GAD, specific phobias, and social phobia.
generalized anxiety disorder (GAD)
- anticipatory anxiety: pathological worrying
-> perseverative worrying that an individual finds uncontrollable
- caused by negative info processing bias, attentional bias, interpretation bias and lack of executive functioning
- what a child worries about tends to be determined by their age
- 4–7-year-olds: personal harm, separation from parents, imaginary creatures
- 11–13-year-olds: social threats and being punished
pathological worrying
perseverative worrying that an individual finds uncontrollable
specific phobias
- normally children go through phases of 'phobia' but here they don't disappear
- e.g., social phobia often being in childhood as a fear of strangers
- prevalence of specific phobia in 8-9-year-olds is 7% for boys and 10% for girls
aetiology of childhood anxiety
genetic factors:
- heritability averaging 54%
- Genetic factors play a relatively nonspecific role in childhood anxiety by determining general levels of temperament probably transmitted through many gene variants.
trauma and stress:
- trauma and stress and exposure to threat-relevant info increases anxious responding (abuse, extreme experiences, illness, accidents)
modelling and exposure to information:
- modelling and exposure to info from different sources
-> peers, authoritative people, media
- e.g parenting style:
- dysfunctional forms of parenting
-> detached, rejecting, over-controlling, overprotective, demanding…
-> reactions to temperament
-> psychological and adjustment problems during childhood
childhood and adolescent depression
- In early childhood, depression will manifest as clingy behaviour, school refusal, and exaggerated fears and also somatic complaints
- nearly same diagnostics as adult depression
-> children: more somatic complaints, social withdrawal…
- adolscence: retarded thinking, hypersomnia, suicidal, self-harm…
- prevalence
-> less than 1% in pre-schoolers
-> 2 and 3% for school-age children
-> ~ 5% in 17-19
--> between 11 and 28% of adolescents aged up to 19 years of age will have a diagnosed episode of major depression
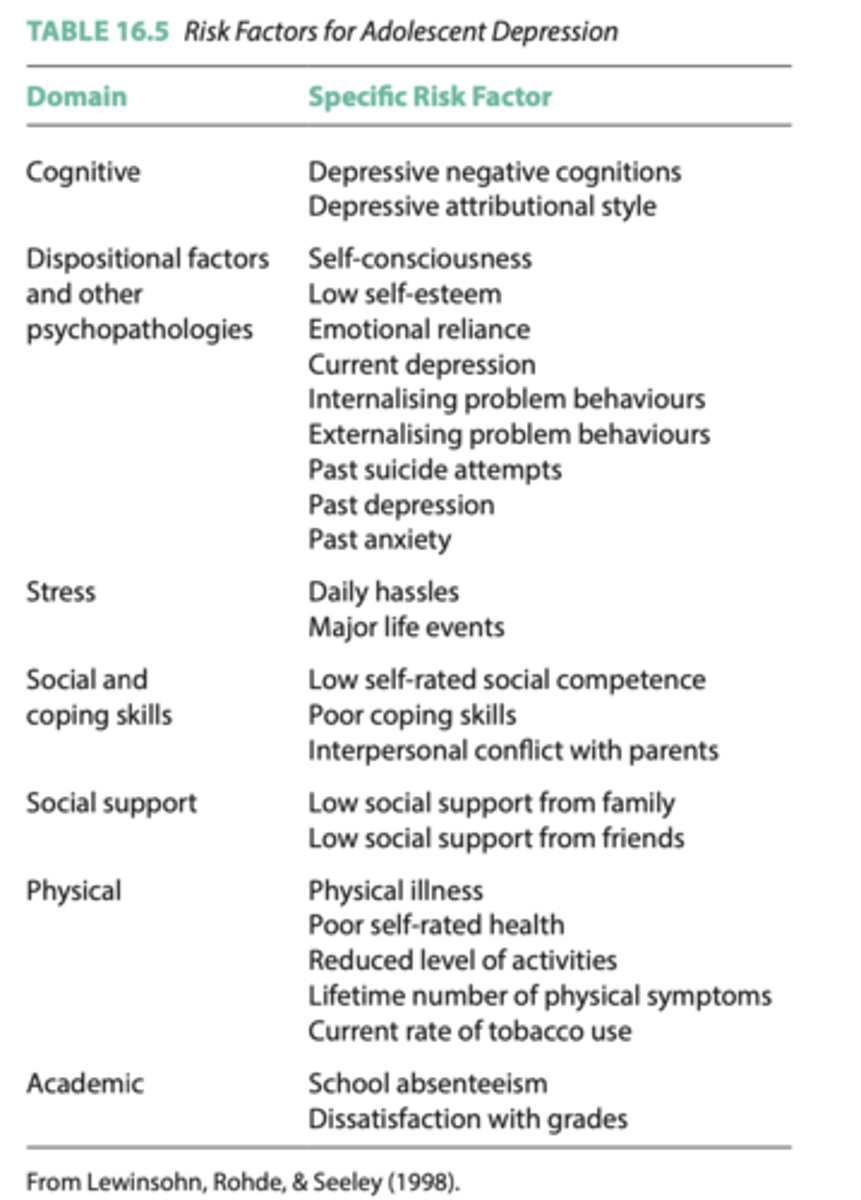
aetiology of childhood and adolescent depression
genetic:
- only a modest genetic component
risk factors:
- risk factors (see pic): the greater the number, the greater the possibility
- childhood abuse or neglect, younger than 5 years of age include parental marital partner changes, mother’s health problems in pregnancy, child’s health....
psychological:
(a) the role of parent‐child interaction and
(b) the development of dysfunctional cognitions that shape and support depressive thinking in childhood.
=> Studies suggest a modest genetic component to childhood depression and a substantial environmental component.
childhood depression is comorbid with...
.. other psychological problems and can have detrimental effects on educational and social functioning.
pessimistic inferential styles
- attribution of negative events to stable, global causes
- more likely to experience increases in self‐ reported -depressive symptoms following negative events than children who do not possesses this inferential style
-> reared by a depressed parent may contribute to childhood depression, and as the child grows older it may develop a this inferential style.
influence of parents on childhood and adolescent depression
- interaction
-> transmit their negative mood to their children
-> children may model the behavioural symptoms of depression exhibited by their parents
-> parents may not be able to properly respond to their children's emotional experiences
- dysfunctional cognitions
-> pessimistic inferential style: attribution to stable, global causes
-> catastrophising
-> infer negative characteristics
treatment of childhood and adolescent psychological problems
- requires a coordinated provision of services that extends across educational, health, and social services.
- often require a multifaceted approach:
-> specific symptoms
-> general emotional states and cognitions
-> behavioural problems
-> intrafamily relationships
drug treatment
- are used for childhood anxiety and depression, and ADHD
- should be cautious about recommending the use of drugs
- rarely a complete elimination of symptoms
- undesirable side effects
- doubts about the safety and efficacy
- ritalin is a stimulant used for ADHD treatment, may act on neurotransmitters norepinephrine and dopamine
Ritalin (methylphenidate)
A stimulant medication that is used to treat ADHD in around half of those diagnosed with the disorder.
behaviour therapy
- systematic desensitization
-> for anxiety problmes
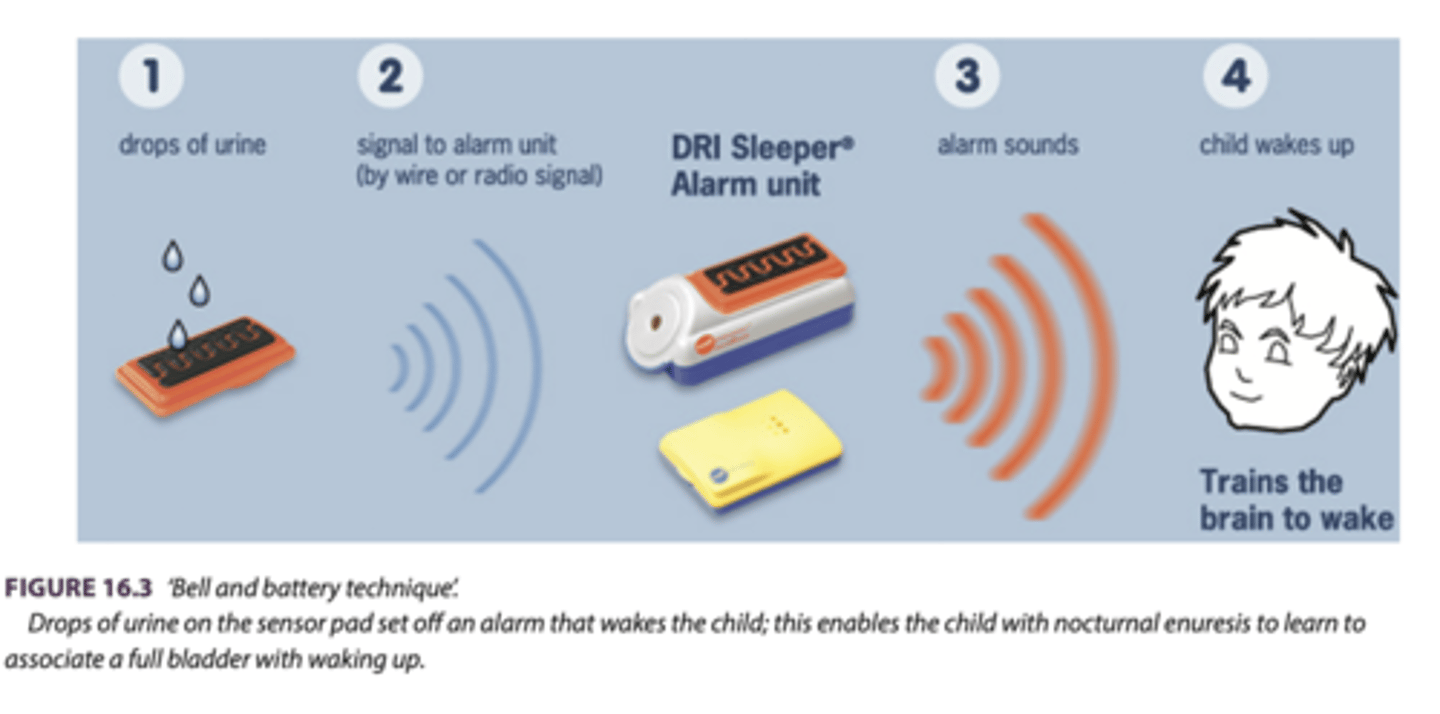
- bell-and-battery technique
-> pair alarm with urine: conditioning
- selective Reinforcement (ADHD):
time-out (TO)
- reducing disruptive behavioursby removing the child from the situation
- e.g. time-out chair for periods between 5 and 15 minutes
-> disruptive behaviour is positively reinforced by the attention it receives from peers and adults
behaviour management techniques:
- even taught to parents as an aid to controlling and responding to their children in the home
-> e.g., identify and reward positive behaviours etc.
family interventions
systemic family therapy:
- inappropriate family structure and organization
- boundaries between parents and children, and the ways in which they communicate
parent management training:
- acceptable rather than antisocial behaviours are reinforced
- conduct disorders
functional family therapy (FFT):
- strengthening relationships in the family by opening up communication between parents and children
systematic desensitization
A type of exposure therapy that associates a pleasant relaxed state with gradually increasing anxiety-triggering stimuli. Commonly used to treat phobias.
time-out (TO)
- reducing disruptive behaviours by removing the child from the situation
- directing them, for example, to sit in a specific time-out chair for periods between 5 and 15 minutes
-> disruptive behaviour is positively reinforced by the attention it receives from peers and adults -> therefore the time out helps giving no attention to negative behaviour
behaviour management techniques
- can be used in a range of environments
- can even be taught to parents as an aid to controlling and responding to their children in the home
-> e.g., teaching parents to identify and reward positive behaviour also helps to prevent parents from focussing on the negative and disruptive behaviours (children with ADHD and CS)
bell‐and‐battery technique
A widely used classical conditioning method for treating nocturnal enuresis (bett nässen).
cognitive behaviour therapy (CBT)
- helps depressed individuals become aware of pessimistic and negative thoughts, depressive beliefs and causal attributions
- has been successfully adapted to treat childhood and adolescent depression and anxiety, as well as a number of other childhood psychological problems.
- increase social interactions
- improve problem-solving skills
- goal setting and attainment
- involve parents
- for anxious children, a typical treatment programme involves:
-> recognition of anxious feelings and somatic reactions
-> understanding the role of cognitions and self-talk in anxious situations
-> learning the use of problem solving and coping skills to manage anxiety
-> using self-evaluation and self-reinforcement strategies to facilitate the maintenance of coping
-> implementing a plan of what to do in order to cope in an anxious situation
- less effective for children under 4 years of age
systemic family therapy
- view that childhood problems result from inappropriate family structure and organization
- boundaries between parents and children, and the ways in which they communicate
parent management training
- teach parents to modify their responses to their children so that acceptable rather than antisocial behaviours are reinforced
- used especially with the families of children diagnosed with conduct disorders
functional family therapy (FFT)
- strengthening relationships in the family by opening up communication between parents and children
- elements of systematic family therapy and CBT
play therapy
- a range of play-based therapeutical and assessment techniques
- used with younger children who are less able to communicate and express feelings
- play itself can be curing with anxiety and depression
- helps to express, learn coping and manage behaviour
- develop positive relationship with therapist
prevention strategies
- school‐based prevention programmes
- especially to help children to develop strategies for managing common mental health problems such as depression and anxiety.