Sleep Apnea and OHS - MedPath
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
What does this refer to
_________ is a sleep disorder characterized by pauses in breathing or periods of shallow breathing during sleep.
Main types:
Obstructive sleep apnea (osa)
Central sleep apnea (csa)
Complex sleep apnea syndrome.
Sleep apnea
What does this refer to
OSA affects 2-4% of the adult population.
More common in males, older adults, and obese individuals.
CSA is less common, often associated with heart failure or stroke.
Epidemiology of Sleep Apnea
What does this refer to
Sleep divided into REM and non-rem stages.
Muscle tone decreases during rem sleep.
Normal airway patency is maintained by pharyngeal dilator muscles.
Normal Sleep Physiology
What does this refer to
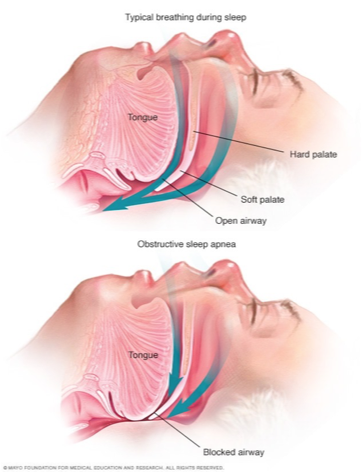
Recurrent upper airway collapse during sleep due to pharyngeal muscle relaxation.
This begins a cascade of effects:
Apnea or hypopnea due to this mechanical obstruction
Which leads to hypoxia, hypercapnia
This in turn leads to sleep fragmentation
The brain senses the falling pO2 and rising pCO2. which results in sympathetic nervous system activation.
That activation briefly arouses the patient to resume respirations.
The patient may not even be aware of these awakenings.
The cycle may occur repeatedly throughout the night.
Pathophysiology of obstructive sleep apnea
What does this refer to
Obstructive Sleep Apnea
What does this refer to
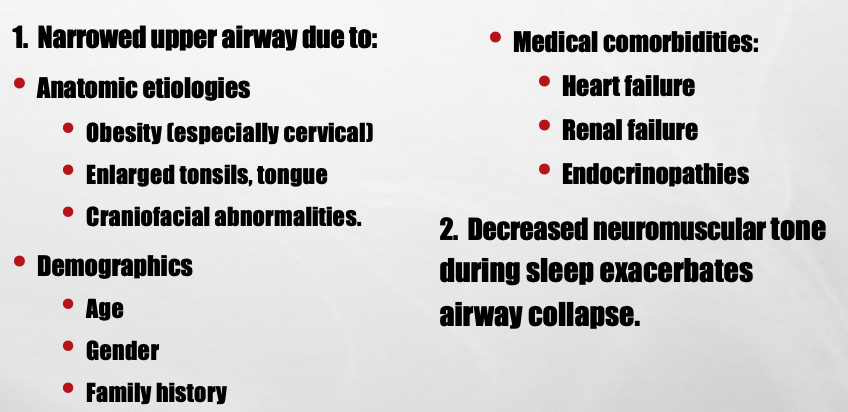
Anatomical Factors in OSA
What does this refer to
Functional Factors in OSA
What does this refer to
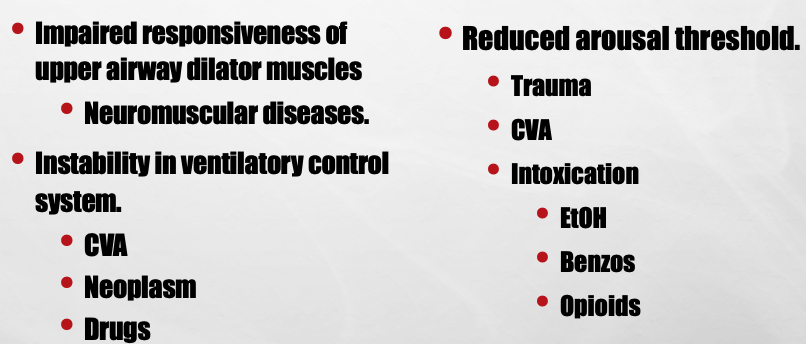
Reduced respiratory drive from the brainstem.
Characterized by lack of respiratory effort during apnea episodes.
Common in patients with heart failure, stroke, or opioid use.
Pathophysiology of central sleep apnea
What does this refer to
Pattern of crescendo-decrescendo breathing with central apneas.
Often seen in csa associated with heart failure.
Cheyne-Stokes Respiration
What does this refer to
CompSAS – AKA Treatment-Emergent Sleep Apnea
Occurs when a patient with OSA on CPAP develops CSA, often after starting CPAP treatment
Etiology unclear. Possibly due to elimination of airway obstruction causing overreaction and dysregulated breathing
Pathophysiology of complex sleep apnea
What does this refer to
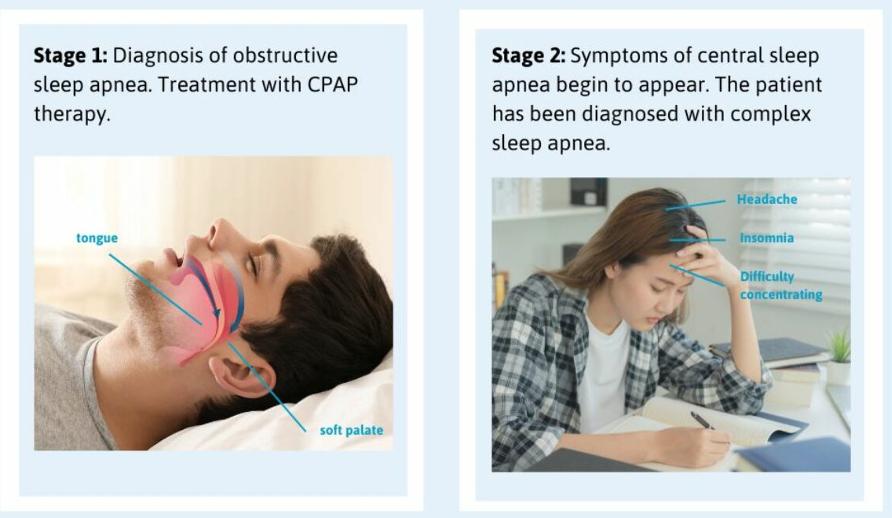
Complex Sleep Apnea (combo of OSA and CSA)
What does this refer to
Intermittent hypoxia and sleep fragmentation.
Increased sympathetic activity.
Inflammatory and metabolic dysregulation.
Consequences of Sleep Apnea
What does this refer to
Hypertension
Arrhythmias
Coronary artery disease.
Increased risk of stroke and heart failure.
Nocturnal surges in blood pressure.
Cardiovascular Complications
What does this refer to
Daytime sleepiness and fatigue.
Impaired attention, memory, concentration and executive function.
Mood disturbances and increased risk of depression.
Increased risks of accidents, i.e. MVCs
Neurocognitive Effects
What does this refer to
Insulin resistance and type 2 diabetes.
Altered leptin and ghrelin levels.
Obesity exacerbates osa and vice versa.
Metabolic and Endocrine Effects
What does this refer to
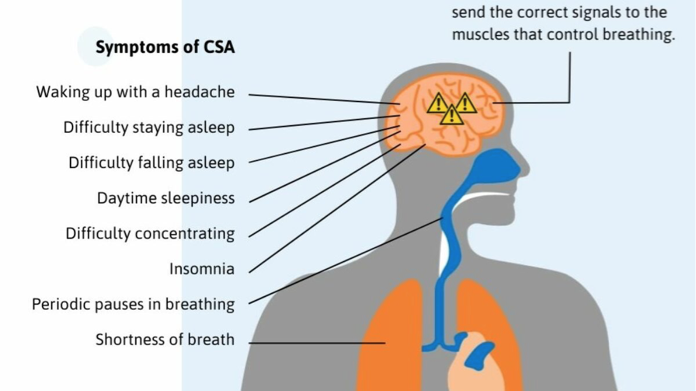
At night:
Loud snoring
witnessed apneas
Gasping, choking during sleep.
Daytime:
sleepiness
morning headaches
poor concentration.
Use of screening tools like STOP-BANG questionnaire.
Clinical features for Diagnosis of CSA
What does this refer to
Gold standard diagnostic test.
Measures respiratory events, oxygen levels, sleep stages.
Apnea-hypopnea index (ahi) used to determine severity.
Polysomnography (for diagnosis)
What does this refer to
Weight loss, exercise, avoiding alcohol and sedatives.
Positional therapy to prevent supine sleep.
Smoking cessation.
Lifestyle modifications treatment
What does this refer to
CPAP: continuous positive airway pressure.
Most effective treatment for moderate to severe osa.
Improves daytime alertness and cardiovascular outcomes.
Positive Airway Pressure (treatment)
What does this refer to
Oral appliances to reposition jaw and tongue.
Surgical interventions: uvulopalatopharyngoplasty, maxillomandibular advancement.
Hypoglossal nerve stimulation.
Other treatment options
What does this refer to
Optimize treatment of underlying condition (e.g., Heart failure).
Adaptive servo-ventilation (asv) for select patients.
Avoidance of opioids and sedatives.
Treatment of CSA
What does this refer to
Adaptive servo-ventilation
A type of continuous positive pressure ventilation which adjusts automatically to breathing patterns
Other PAPs
BiPAP
Treatment of CompSAS
What does this refer to
Good prognosis with adherence to treatment.
Long-term monitoring needed for cardiovascular and metabolic risks.
Patient education and support are crucial.
Prognosis and Follow-Up of CSA
What does this refer to
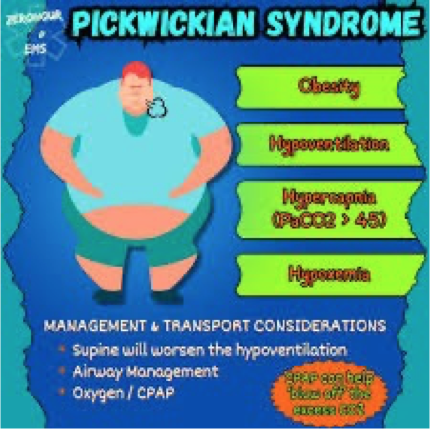
__________ is defined as obesity (BMI ≥30 kg/m²), daytime hypercapnia (paco₂ >45 mmhg), and absence of other causes of hypoventilation.
Also known as pickwickian syndrome.
Obesity hypoventilation syndrome (OHS)
What does this refer to
Prevalence: ~10-20% of obese individuals with obstructive sleep apnea (OSA).
Risk factors:
Male sex
Severe obesity
Postmenopausal status
Coexisting osa.
Epidemiology and Risk Factors of Obesity Hypoventilation Syndrome
What does this refer to
Ventilation regulated by central and peripheral chemoreceptors.
Diaphragmatic and intercostal muscle function crucial for ventilation.
Obesity increases workload of breathing and reduces chest wall compliance.
Normal Respiratory Physiology (Obesity Hypoventilation Syndrome)
What does this refer to
Excess body weight impairs lung mechanics and respiratory muscle function.
Blunted ventilatory response to hypercapnia and hypoxia.
Leptin resistance may reduce respiratory drive.
Pathophysiology of Hypoventilation
What does this refer to
Majority of OHS patients have coexisting OSA.
Recurrent apneas and hypopneas worsen daytime hypercapnia.
Sleep fragmentation and hypoxemia increase sympathetic drive.
Sleep-Related Breathing Disorders
What does this refer to
Hypoventilation leads to chronic hypercapnia and hypoxemia.
V/Q mismatch due to atelectasis and reduced alveolar ventilation.
Polycythemia may develop as a compensatory response.
Gas Exchange Abnormalities
What does this refer to
Daytime sleepiness and fatigue: Due to poor oxygenation and high carbon dioxide levels.
Shortness of breath: Especially during exertion.
Loud snoring and pauses in breathing during sleep: Often associated with sleep apnea.
Headaches: Particularly in the morning.
Swelling in the legs or feet: Due to fluid retention.
Bluish tint to the skin, lips, or fingertips (cyanosis): Caused by low oxygen levels.
Irritability and depression: Can be related to sleep disturbances and poor oxygenation.
Signs and symptoms of Obesity Hypoventilation Syndrome
What does this refer to
Pulmonary hypertension and cor pulmonale common.
Increased risk of heart failure, arrhythmias, and metabolic syndrome.
Insulin resistance and systemic inflammation are often present.
Cardiovascular and Metabolic Consequences of OHS
What does this refer to
Clinical suspicion in obese patients with hypersomnolence and elevated pCO₂.
Confirmed by arterial blood gases, overnight oximetry or polysomnography.
Rule out other causes of hypoventilation like neuromuscular disease.
Diagnosis of OHS
What does this refer to
Mainstay: positive airway pressure (CPAP or bipap).
Weight loss critical for long-term management.
Supplemental oxygen and pharmacologic therapy used selectively.
Treatment strategies of OHS
What does this refer to
Untreated OHS associated with high morbidity and mortality.
Adherence to noninvasive ventilation improves survival.
Regular monitoring of blood gases, weight, and sleep-disordered breathing needed.
Prognosis and Follow-Up of OSA