transport in mammals
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
21 Terms
describe a double circulatory system
birds and most mammals
blood passes through the heart twice per circuit
one circuit of vessels carries blood away from heart to lungs for gas exchange: pulmonary circulation
second circuit carries blood from heart to the rest of the body: systemic circulation
structure & function of arteries
smooth muscle layer → constriction and dilation to control volume of blood
elastic layer → maintains blood pressure, walls stretch and recoil in response to heartbeat
collagen layer → provides structural support
wall thickness → prevents vessels from bursting due to high pressure
no valves
structure & function of arterioles
smooth muscle layer → restrict flow into capillaries
elastic layer → thinner than arteries as pressure is lower
collagen layer → thinner
wall thickness → thinner as pressure is slightly lower
no valves
structure & function of capillaries
no smooth muscular layer
no elastic layer
no collagen layer
walls one cell thick to provide a short diffusion distance for exchanging materials between blood and cells
no valves
structure & function of veins
smooth muscle layer → relatively thin so cannot control blood flow
elastic layer → relatively thinner as pressure is much lower
collagen layer → lots of collagen
wall thickness → thin as low pressure so low risk of vessel bursting, thinness means vessels are easily flattened, helps flow of blood to heart
valves are present
structure & function of venues
smooth muscle layer → thin layer
elastic layer → none
collagen layer → none
wall thickness → very thin, several venues join to form a vein
valves present
identifying RBCs, monocytes, neutrophils, and lymphocytes
RBCs: biconcave shaped cell with no nucleus
monocyte: non-granular cytoplasm and nucleus looks like a kidney bean
neutrophil: granular looking cytoplasm and nucleus is lobed, looking like a string of beads
lymphocyte: non-granular cytoplasm with a large, spherical nucleus
how is tissue fluid formed
blood enters capillaries from arterioles → smaller diameter results in high hydrostatic pressure
pressure forces water, glucose, amino acids, fatty acids, ions, and oxygen out of capillaries
this tissue fluid bathes cells in substances they need
hydrostatic pressure
pressure exerted by liquid
oncotic pressure
tendency of water to move into blood by osmosis
how does liquid move out of the capillaries
hydrostatic pressure is higher than oncotic pressure at arterial end of capillaries
net movement of liquid is out of capillaries
what happens to remaining liquid
absorbed into lymphatic system
eventually drains back into bloodstream near the heart
once in lymphatic system it is called lymph
how does the affinity of haemoglobin for oxygen change
as each molecule binds the shape of haemoglobin changes, making the binding of further oxygen molecules easier
areas with high partial pressure of oxygen (high concentration) the affinity for heamoglobin fro oxygen is high
in humans, alveoli have a high partial pressure of oxygen
what is the Bohr effect
A high partial pressure of carbon dioxide results in haemoglobin having a reduced affinity for oxygen.
Haemoglobin will more readily unload oxygen.
reduced affinity is caused by change in shape of haemoglobin
3 ways carbon dioxide is transported
dissolved in blood plasma
as haemoglobonic acid → CO2 reacts reversibly with amino acids in haemoglobin to form haemoglobin acid
in cytoplasm of RBCs in the form of hydrogen carbonate ions
What is the chloride shift
carbonic acid leaves RBCs by diffusion
in exchange chloride ions diffuse into RBCs
both ions are negative, so this exchange maintains the electrical balance of RBCs
structure of the heart
coronary arteries supply cardiac muscle with ATP
left ventricle has thickest muscular wall
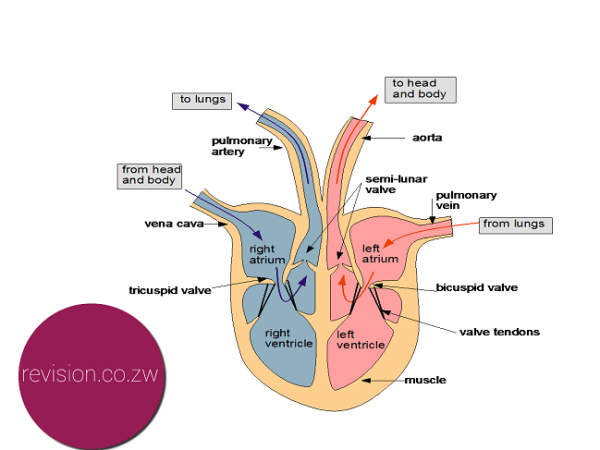
cardiac cycle
atrial systole is when atria contract: increases pressure in atria, opening atrioventricular valves and forcing blood to flow into ventricles
ventricular systole is when ventricles contract and aura relax: increases pressure in ventricles, causing atrioventricular valves to shut and semilunar valves to open, therefore blood flows out of ventricles and into the pulmonary artery and aorta
formula for cardiac output
stroke volume x heart rate
what is the rate of heart contraction controlled by
waves of electrical activity
process of heart contractions controlled by electrical activity
sinoatrial node(SAN) is in right atrium: releases a wave of depolarisation across the atria, causing the cardiac muscle to contract
atrioventricular node (AVN) is located near the border of right and left ventricles within the atria: releases another wave of depolarisation once first wave has reached it
non-conductive layer between atria and ventricles prevents wave of depolarisation from travelling down to the ventricles
bundle of His in septum conducts wave of depolarisation down septum and Purkyne fibres
muscles in Apex contract first, then walls of ventricles