GI and Retroperitoneal Viscera
1/142
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
143 Terms
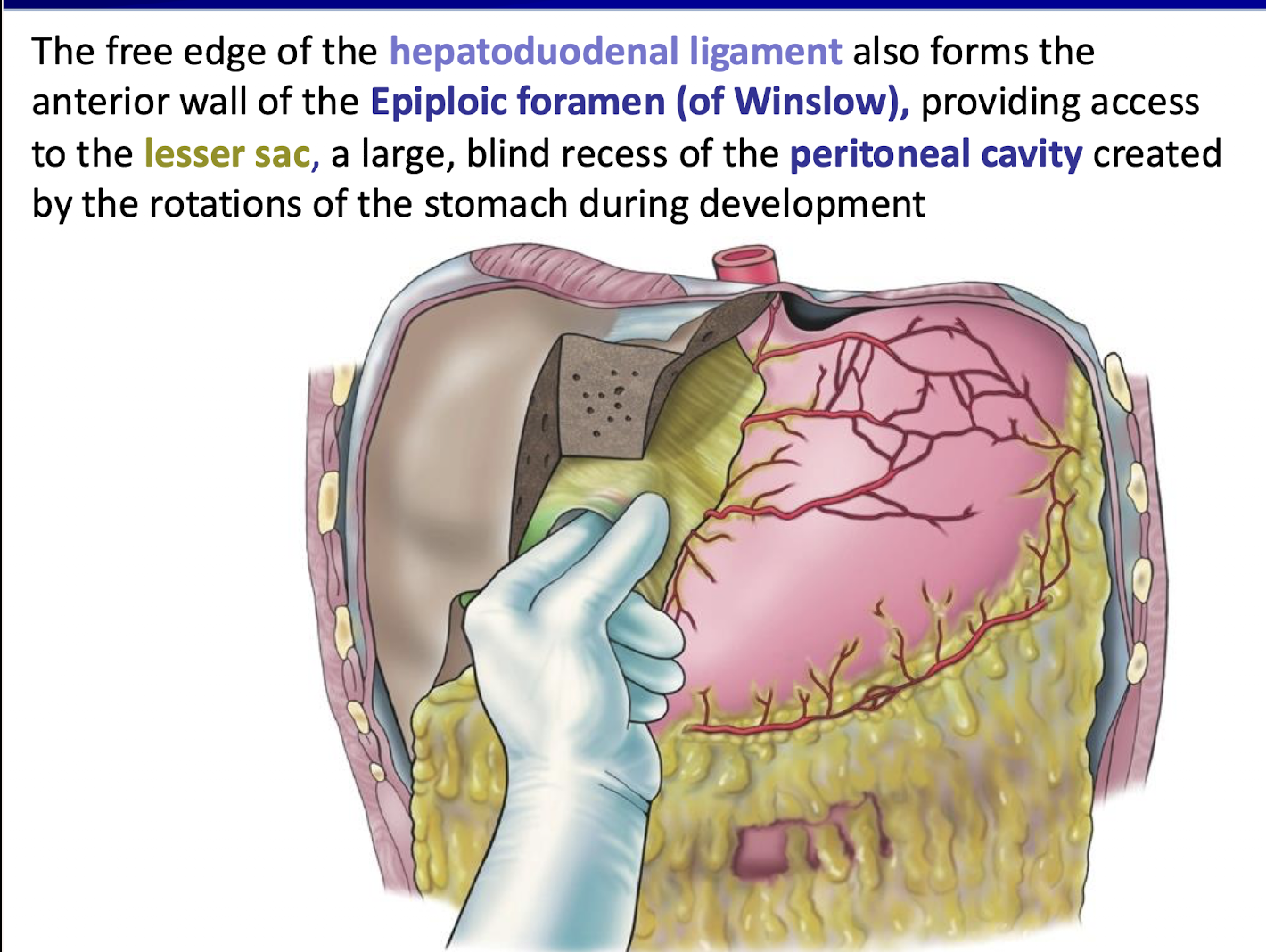
What forms the anterior wall of the Epiploic foramen (of Winslow)
The free edge of the hepatoduodenal ligament.
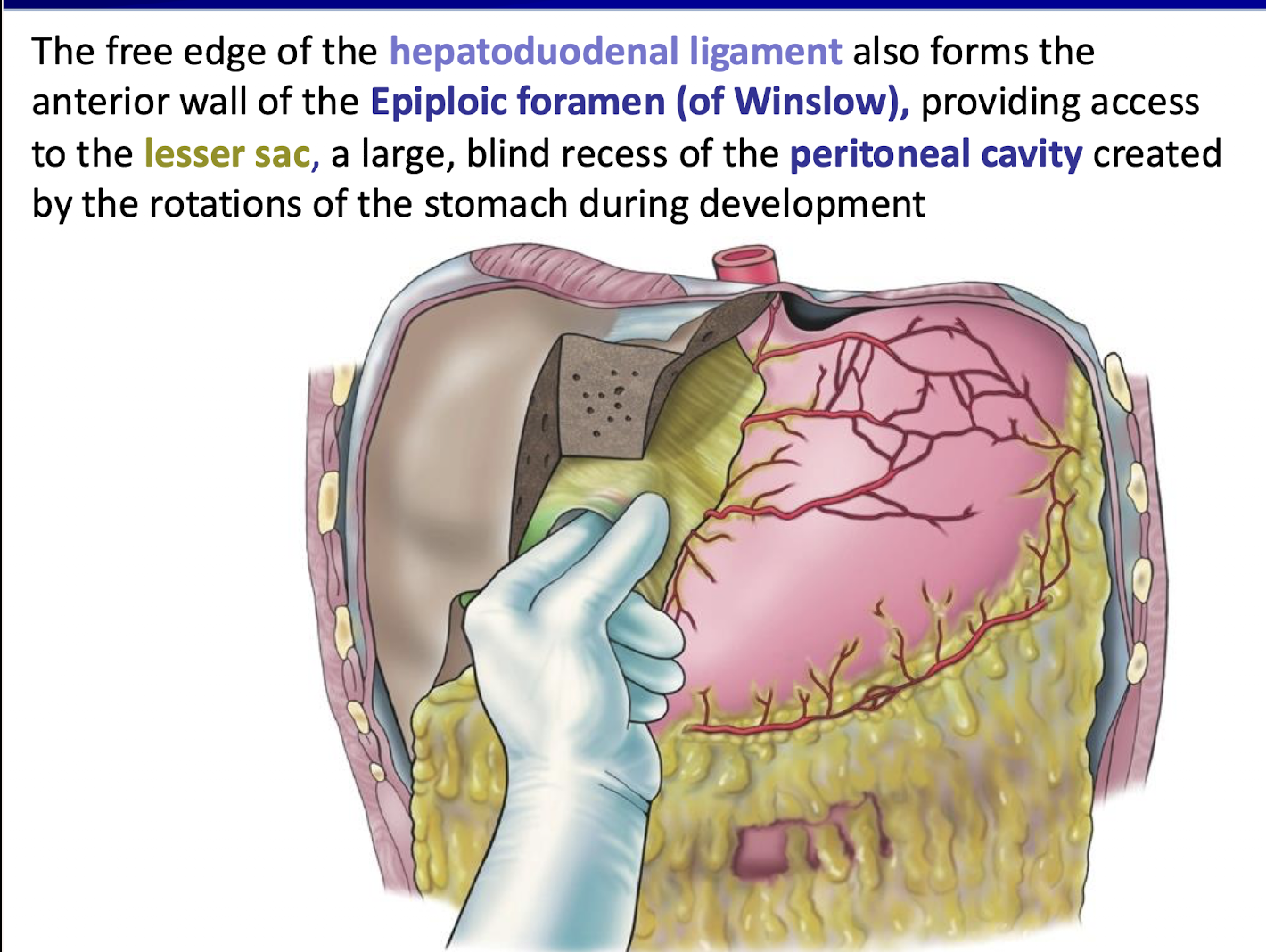
What is the significance of the Epiploic foramen (of Winslow)
It provides access to the lesser sac.
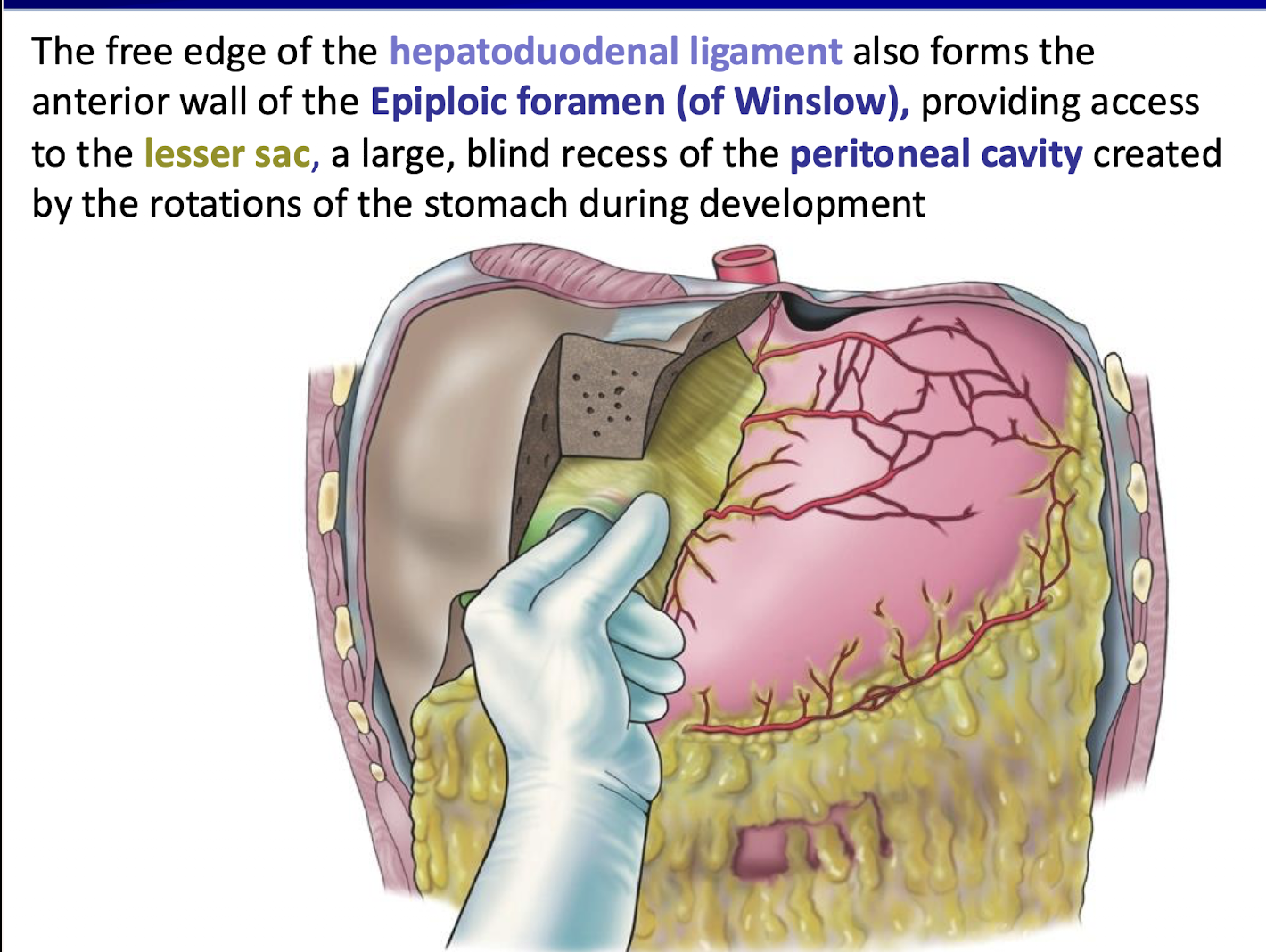
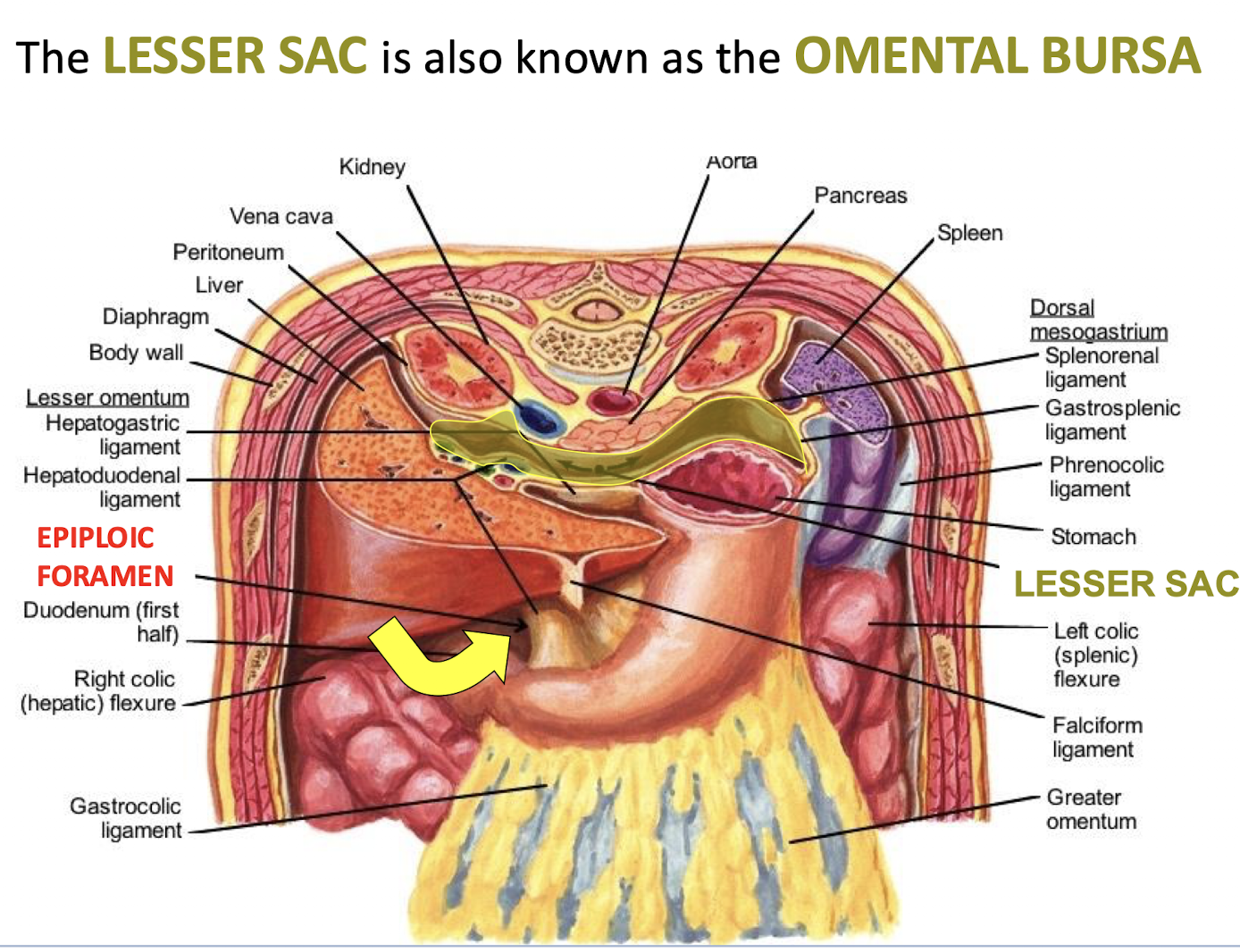
What is the anatomical nature of the lesser sac
A large, blind recess of the peritoneal cavity created by the rotations of the stomach during development.
What is the alternative name for the LESSER SAC
OMENTAL BURSA.
What is a bursa and why is it important
A bursa is a sac filled with synovial fluid that lies between muscle and bone.
Reduces friction during movement.
Without a bursa, the muscle would become inflamed and abraded.
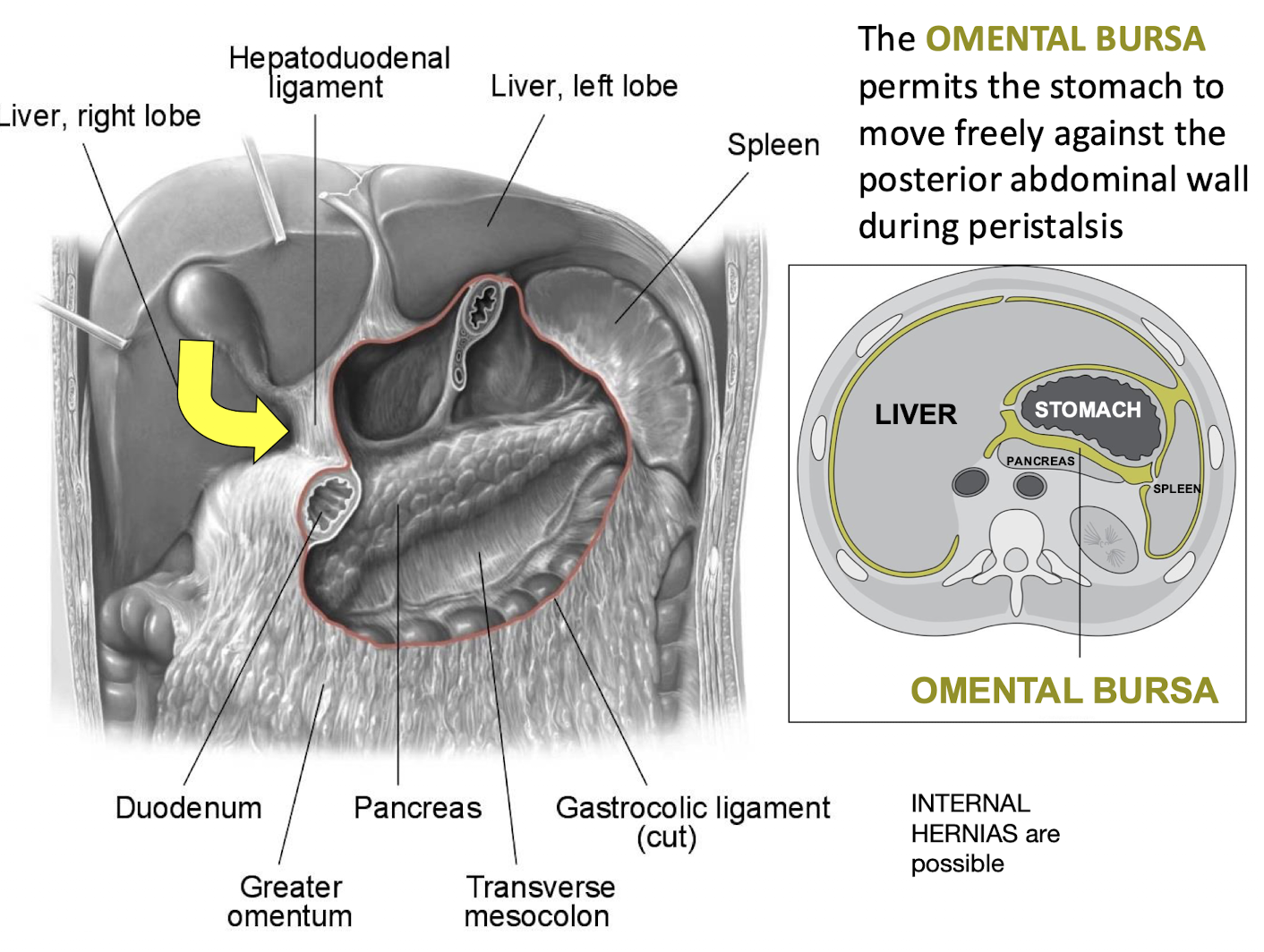
What function does the OMENTAL BURSA permit? How is it related to internal hernias?
It permits the stomach to move freely against the posterior abdominal wall during peristalsis.
Internal hernias are possible through the omental bursa
Herniation can occur via the epiploic foramen (foramen of Winslow)
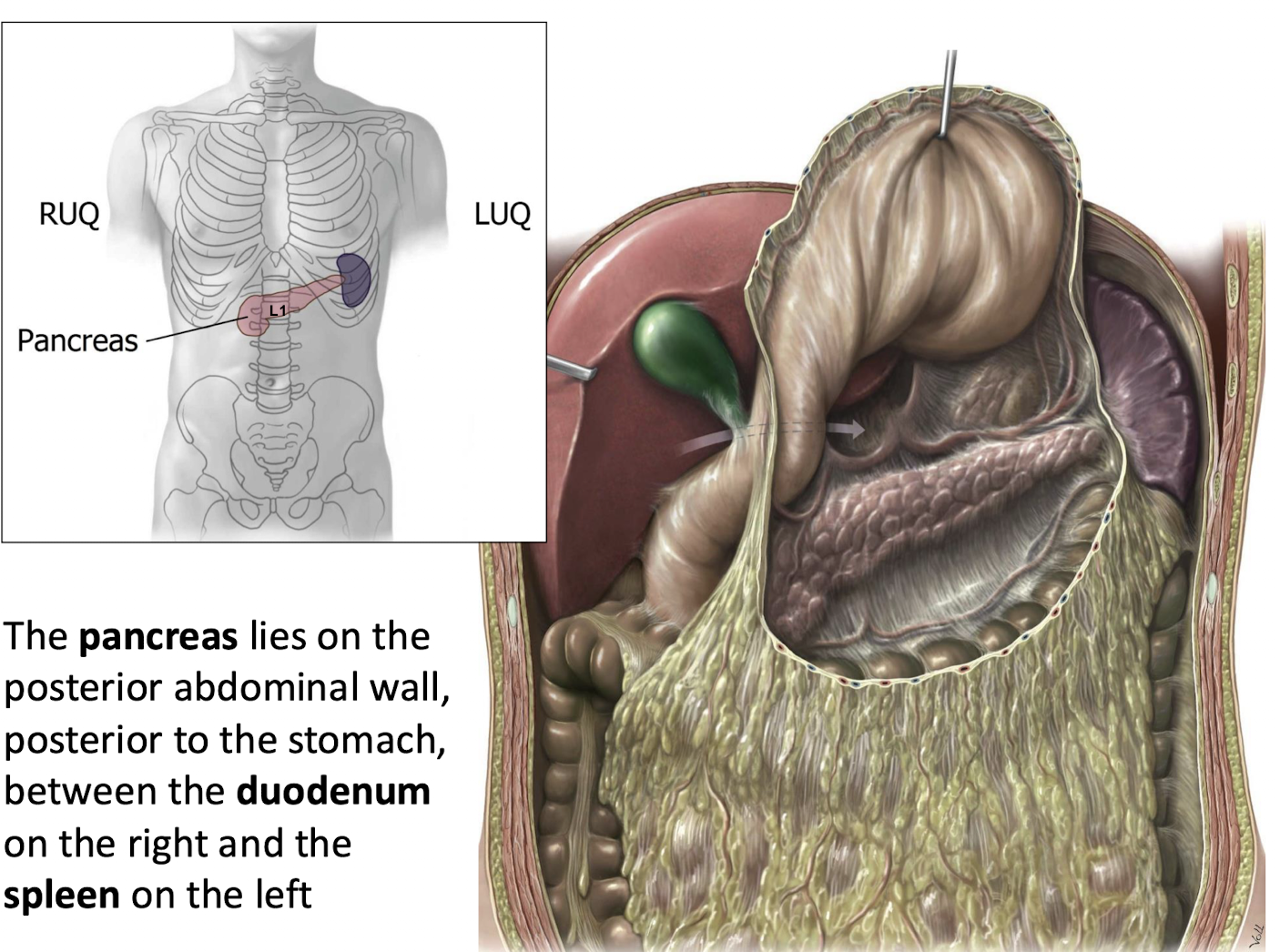
Where is the pancreas located anatomically?
It lies on the posterior abdominal wall; posterior to the stomach; between the duodenum on the right and the spleen on the left.
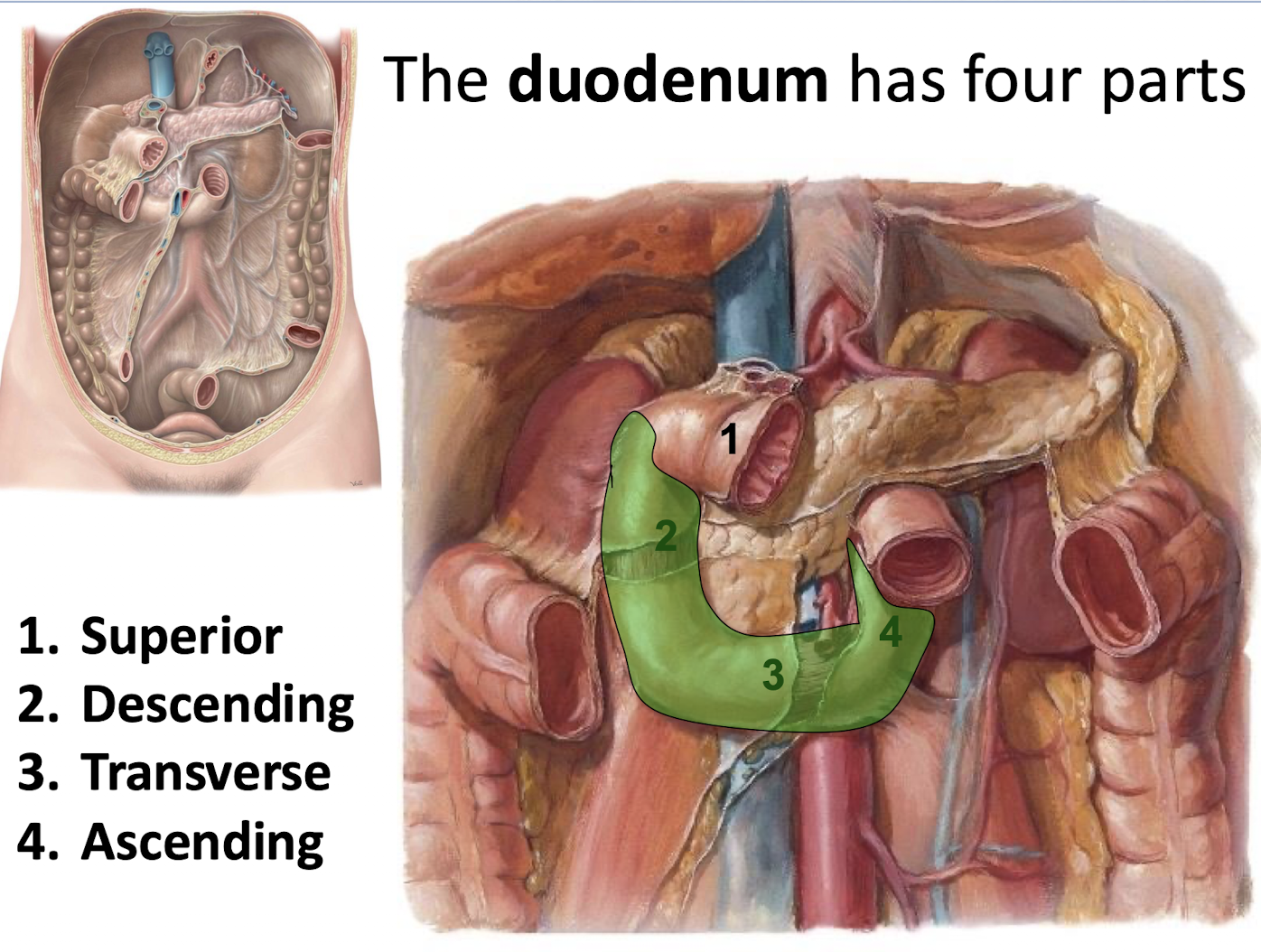
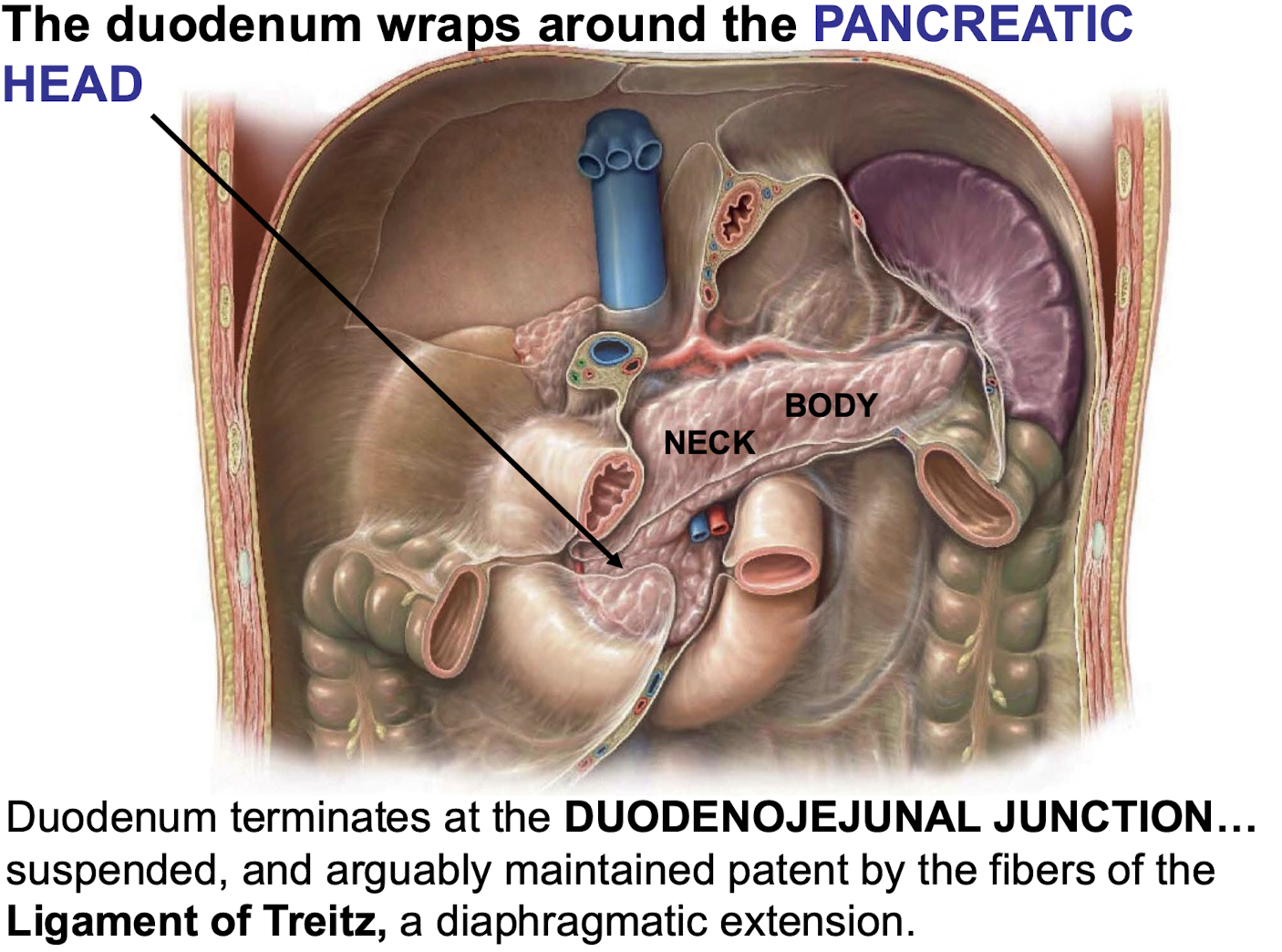
How many parts does the duodenum have? What are they? What is unique about parts 2-4?
Four parts; specifically Superior; Descending; Transverse; and Ascending.
Parts 2–4 are fused to the posterior abdominal wall and become secondarily retroperitoneal structures.
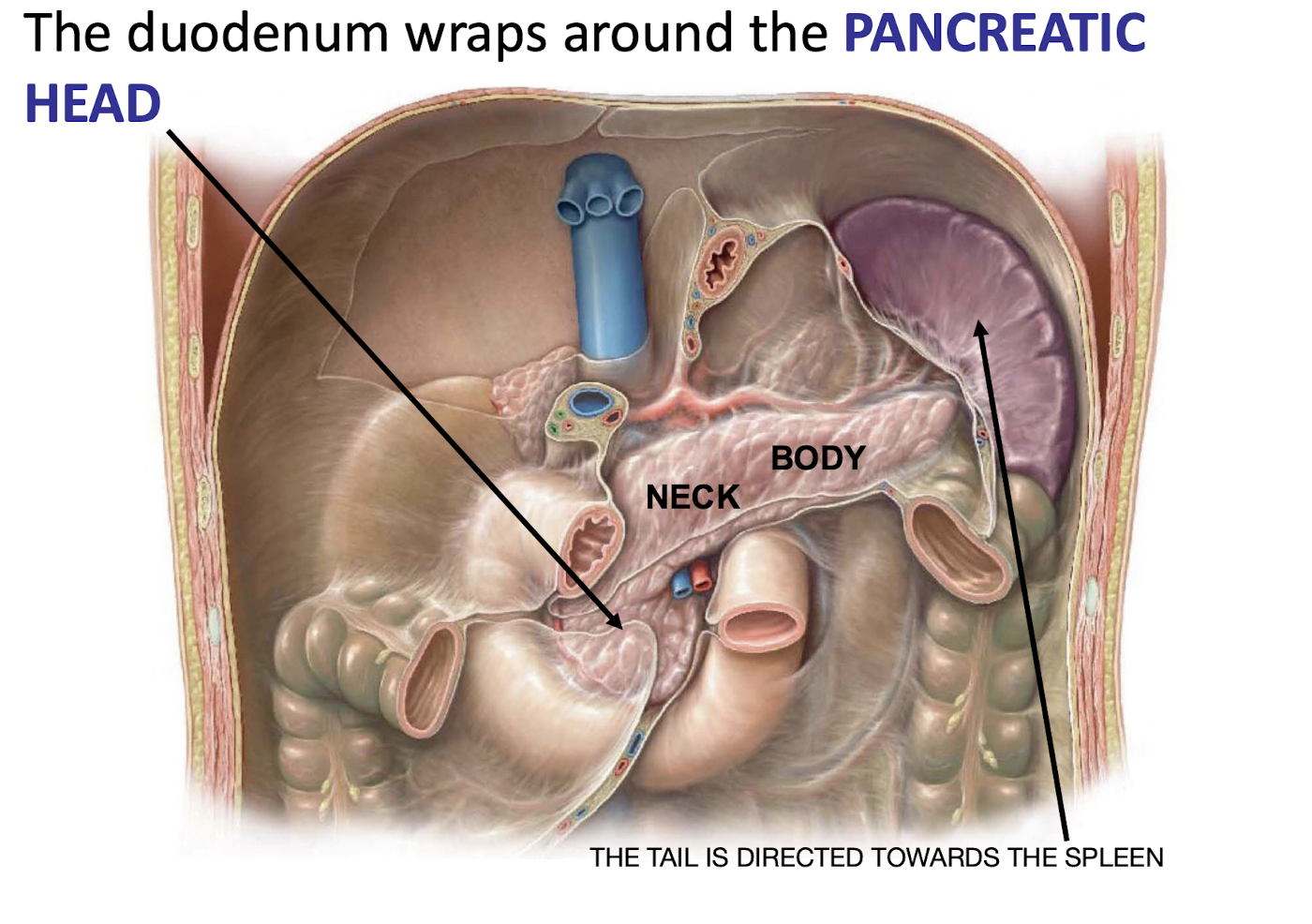
What part of the pancreas does the duodenum wrap around? Where is the pancreatic tail directed?
The PANCREATIC HEAD.
THE TAIL IS DIRECTED TOWARDS THE SPLEEN
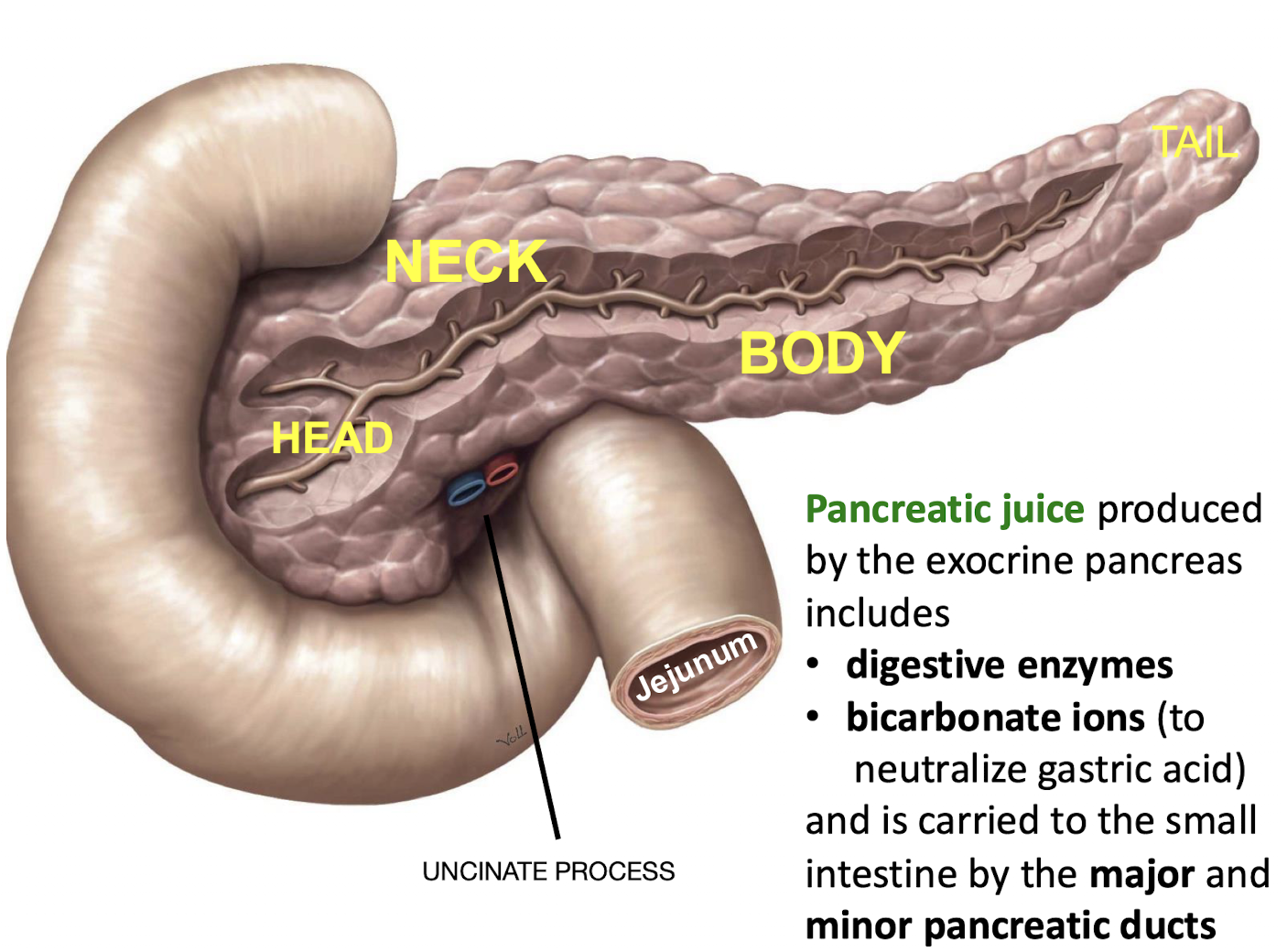
What components are included in pancreatic juice produced by the exocrine pancreas? Where is the pancreatic juice carried to and how?
Digestive enzymes; and bicarbonate ions (to neutralize gastric acid).
Carried to the small intestine by the major and minor pancreatic duct
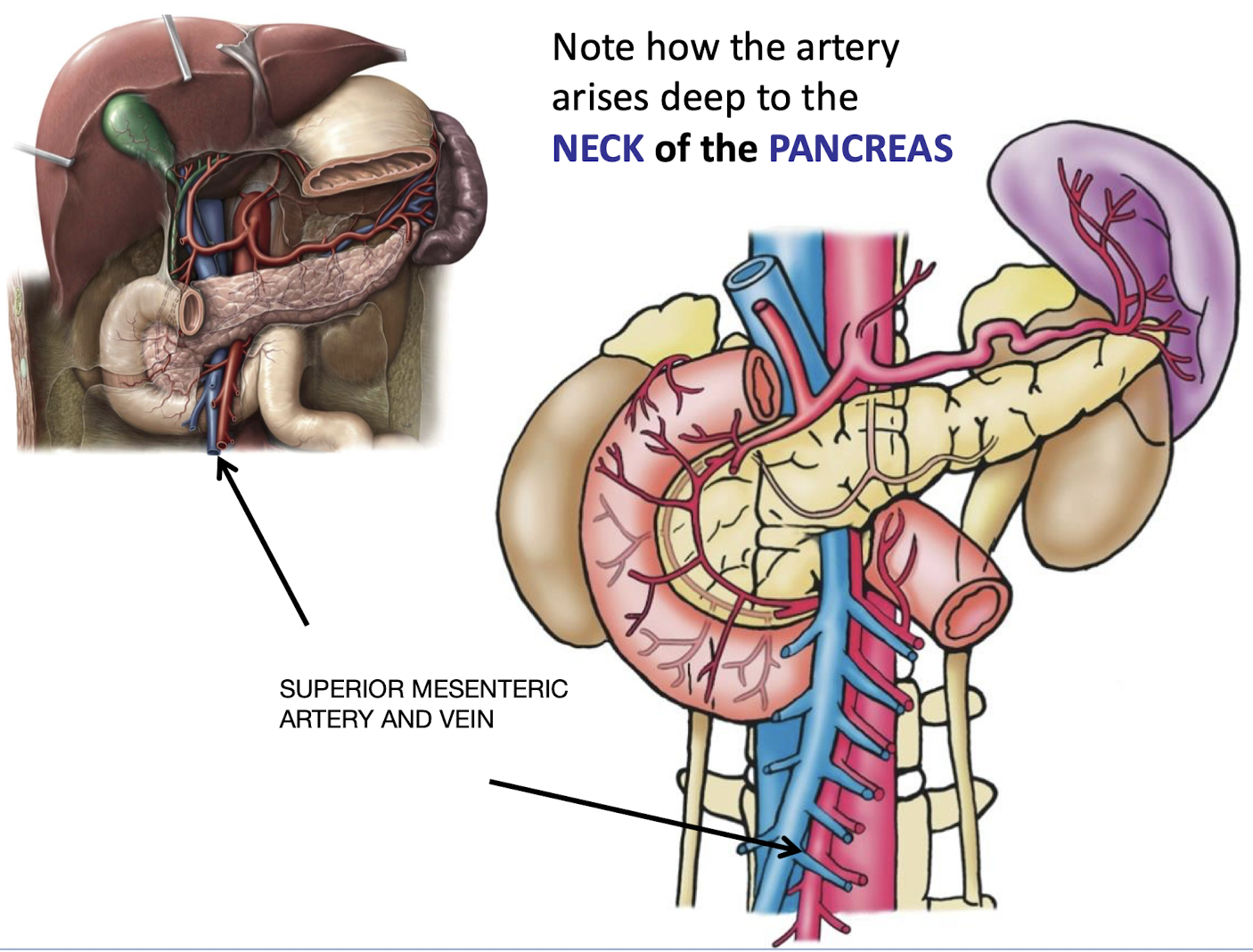
What significant structure arises deep to the _____of the PANCREAS
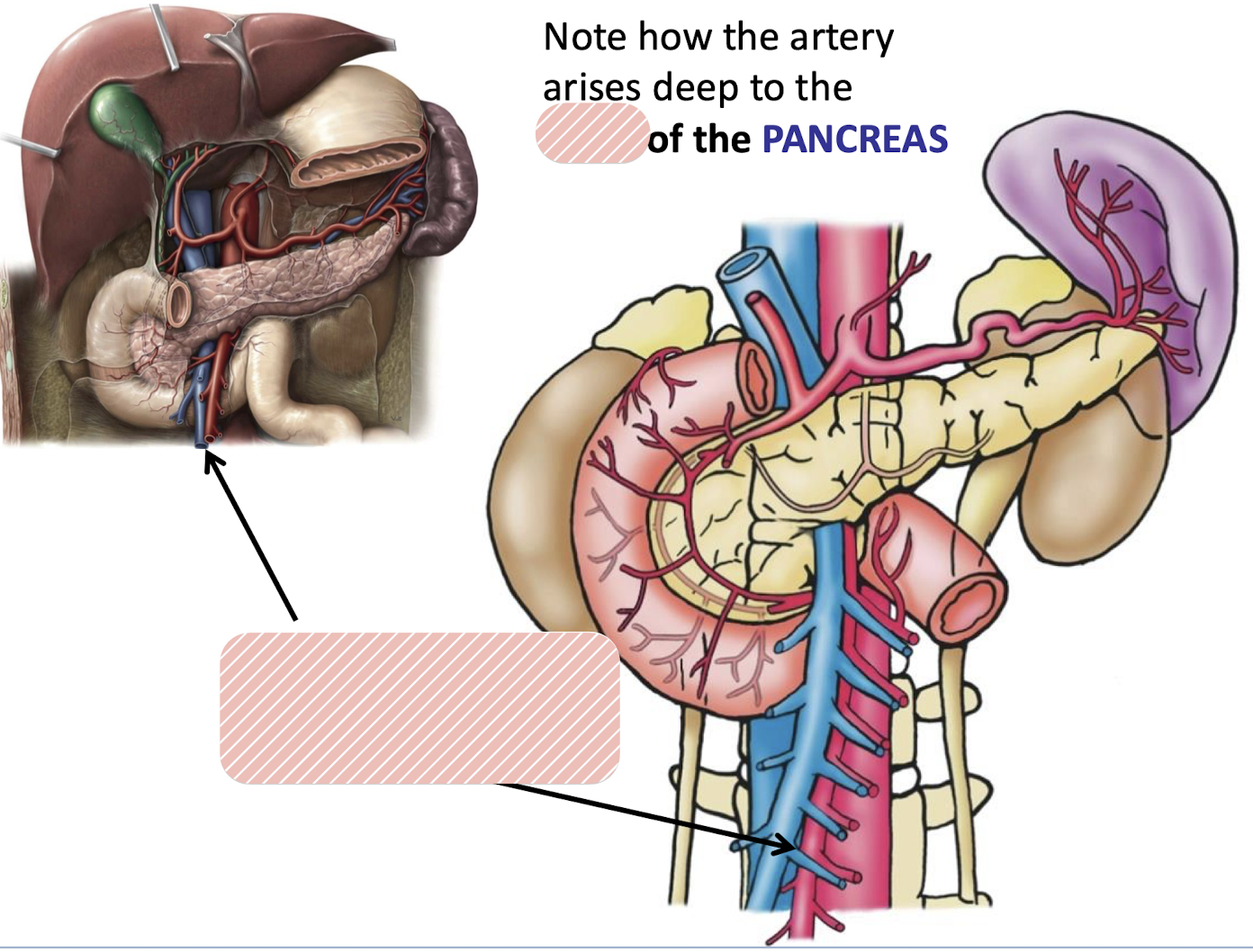
The superior mesenteric artery and vein arise deep to the NECK of the pancreas
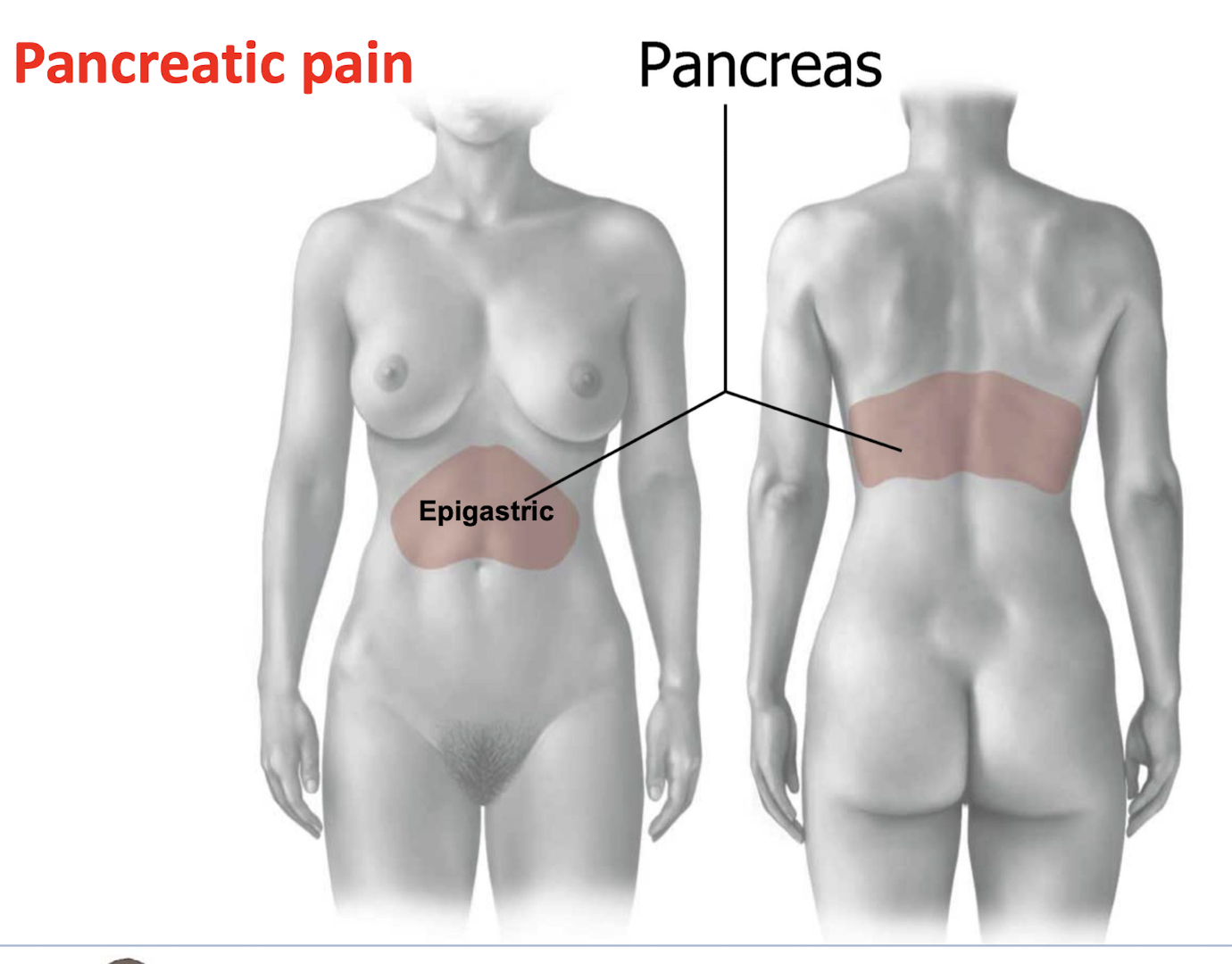
Where is pancreatic pain located
Epigastic region anteriorly and posteriorly
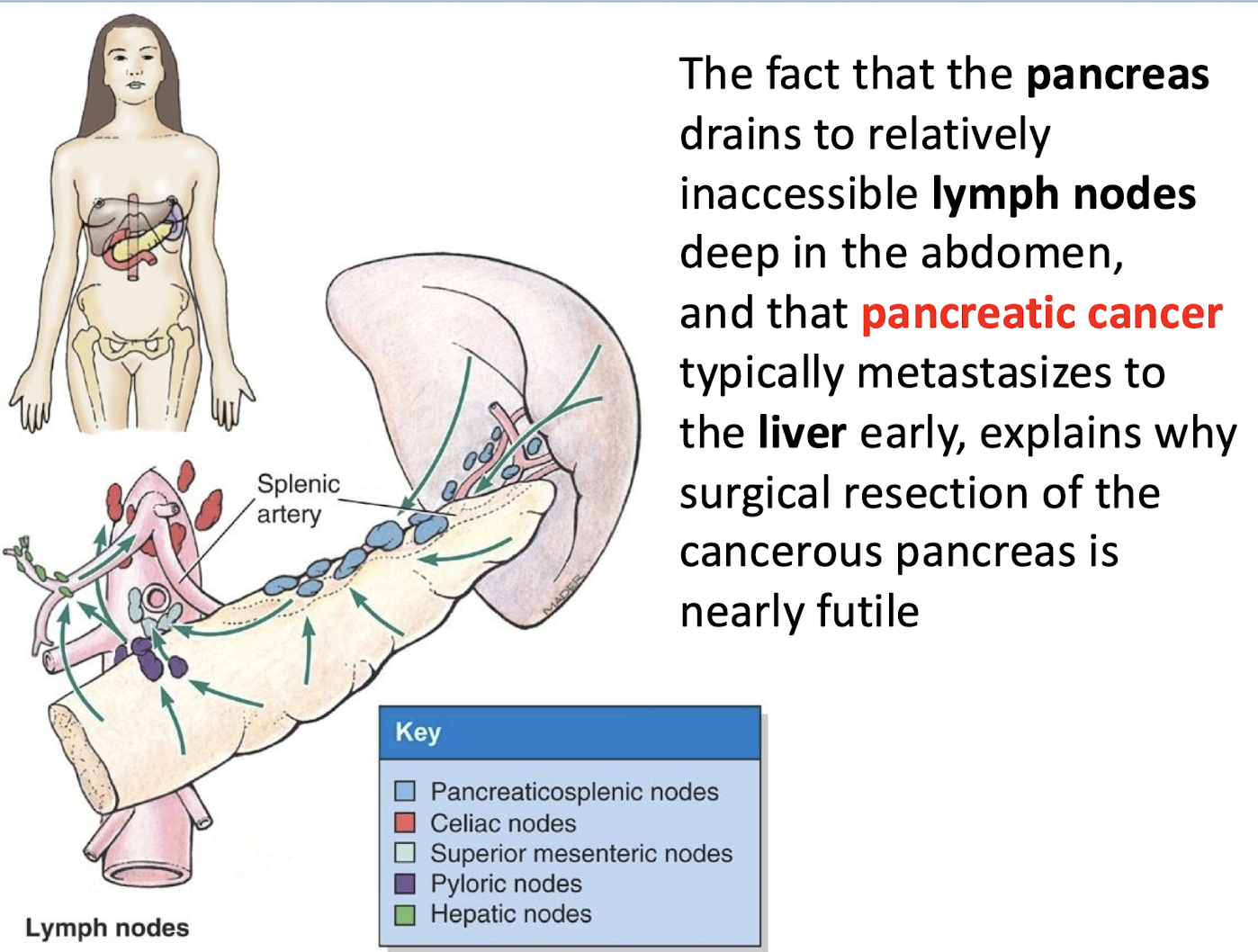
Why is surgical resection of cancerous pancreas nearly futile
The pancreas drains to relatively inaccessible lymph nodes deep in the abdomen; and pancreatic cancer typically metastasizes to the liver early.
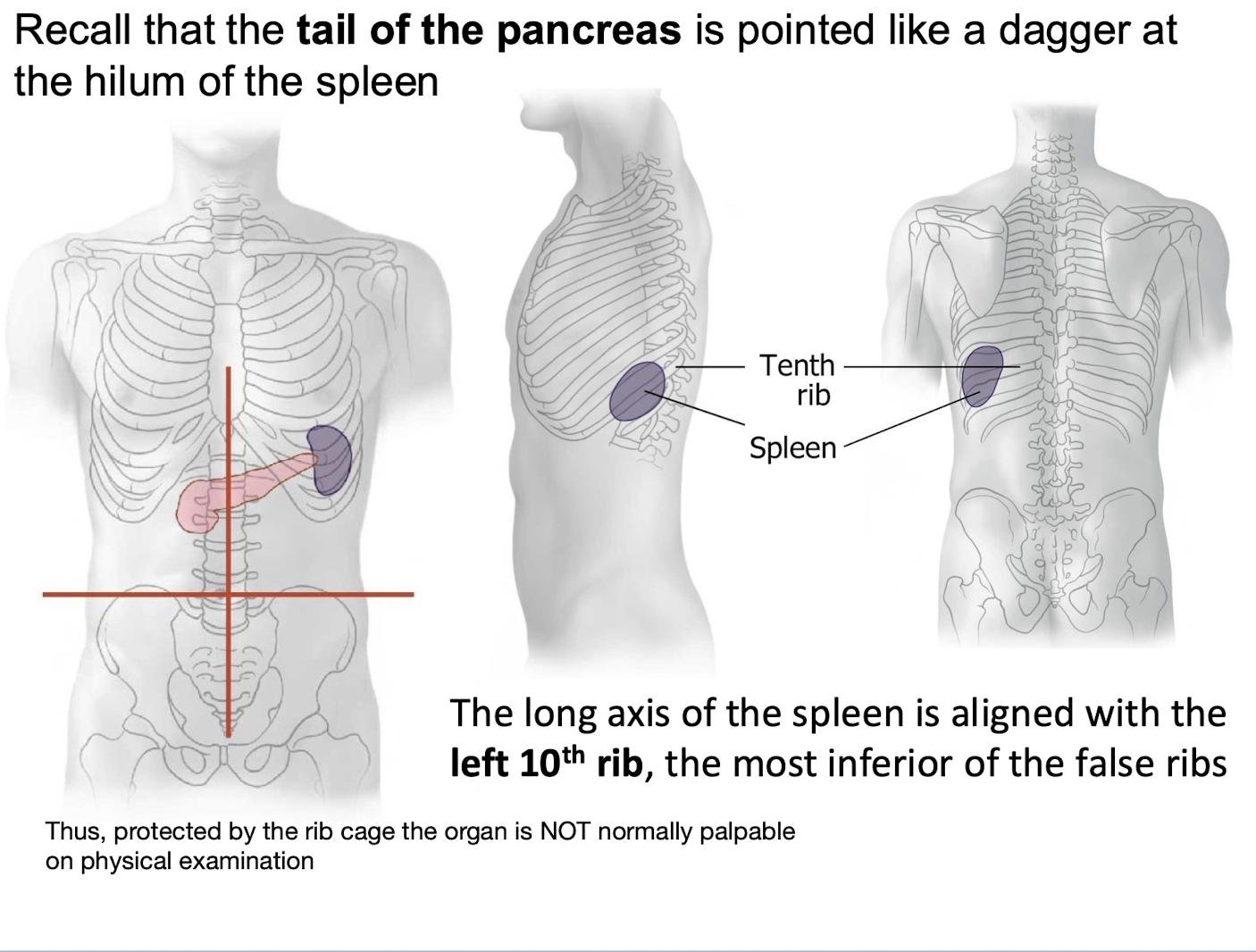
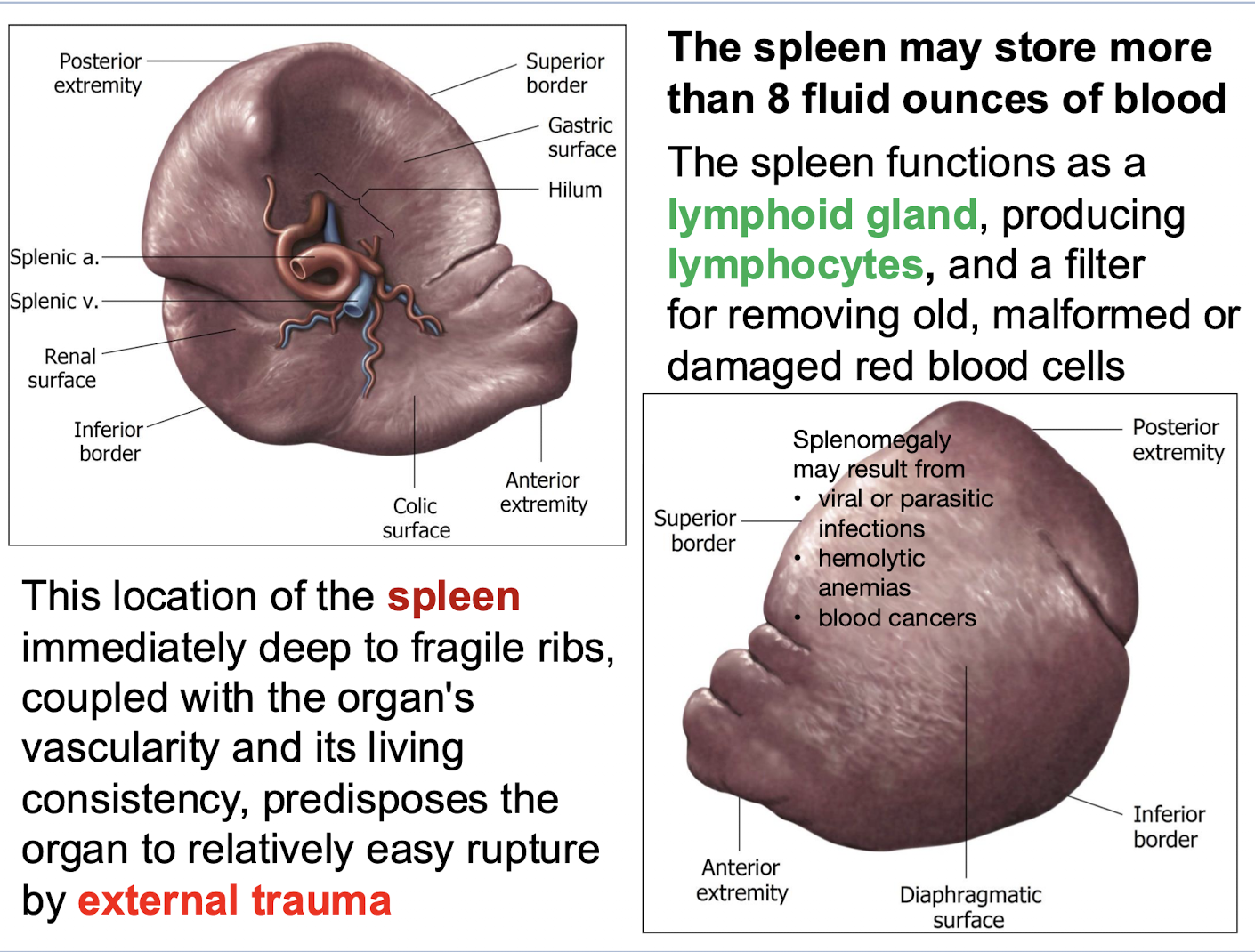
With which rib is the long axis of the spleen aligned? What is the result for physical exam?
The left 10th rib; the most inferior of the false ribs.
Thus, protected by the rib cage the organ is NOT normally palpable on physical examination
What is the peritoneal status of the spleen
It is a fully peritonealized organ.
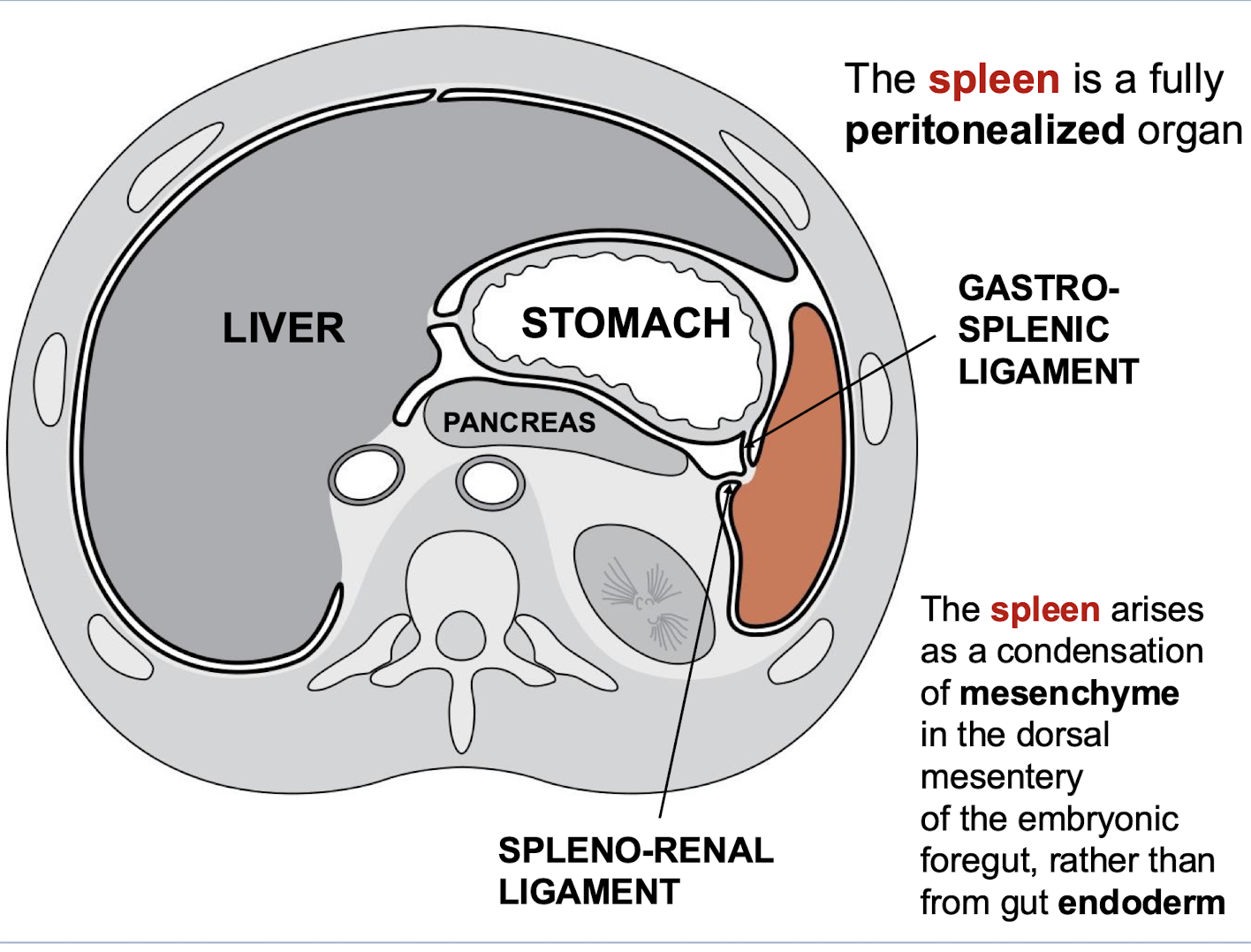
What two ligaments are associated with the spleen's peritoneal attachments
GASTRO-SPLENIC LIGAMENT; SPLENO-RENAL ligament.
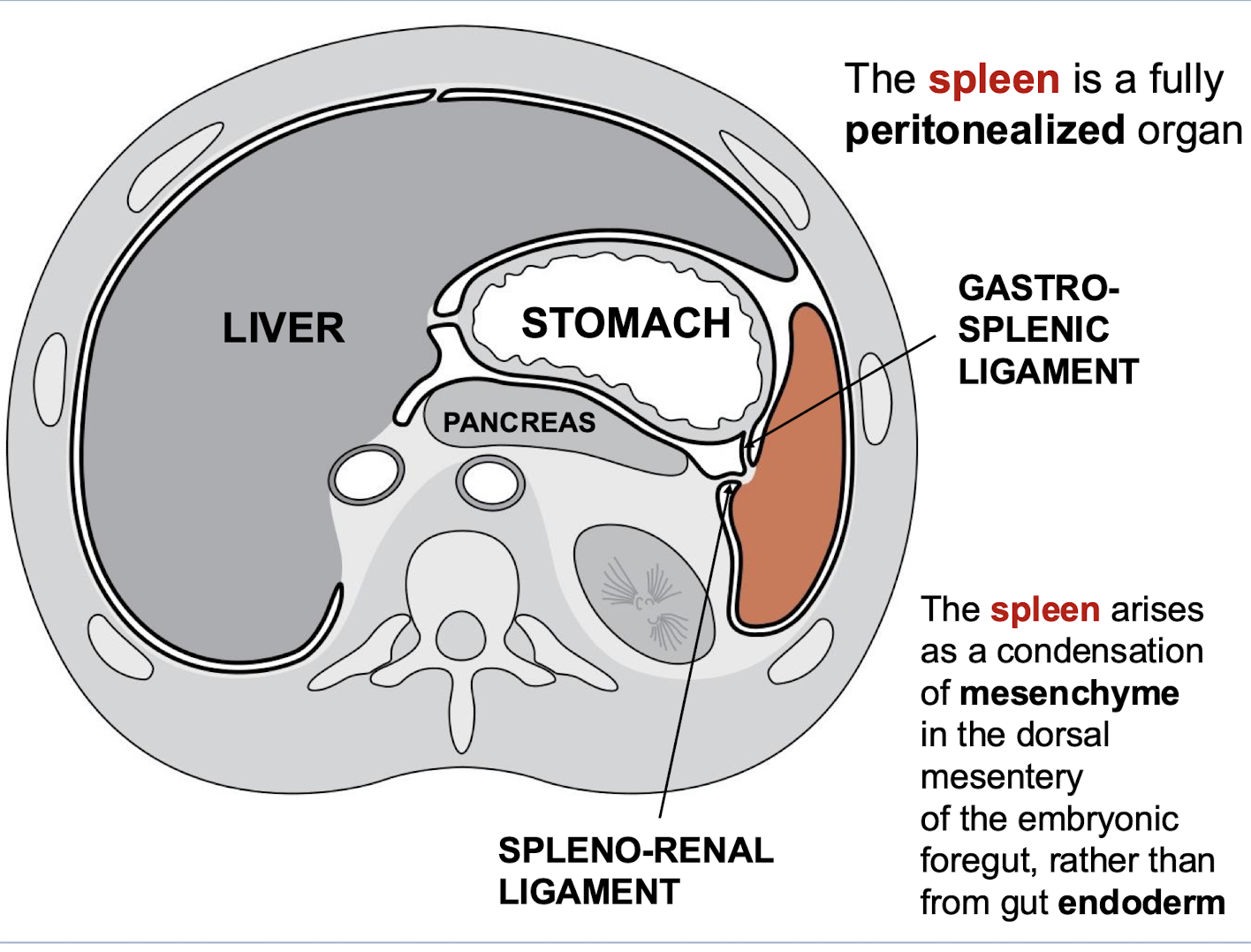
From what embryonic structure does the spleen arise
A condensation of mesenchyme in the dorsal mesentery of the embryonic foregut. rather than from gut endoderm
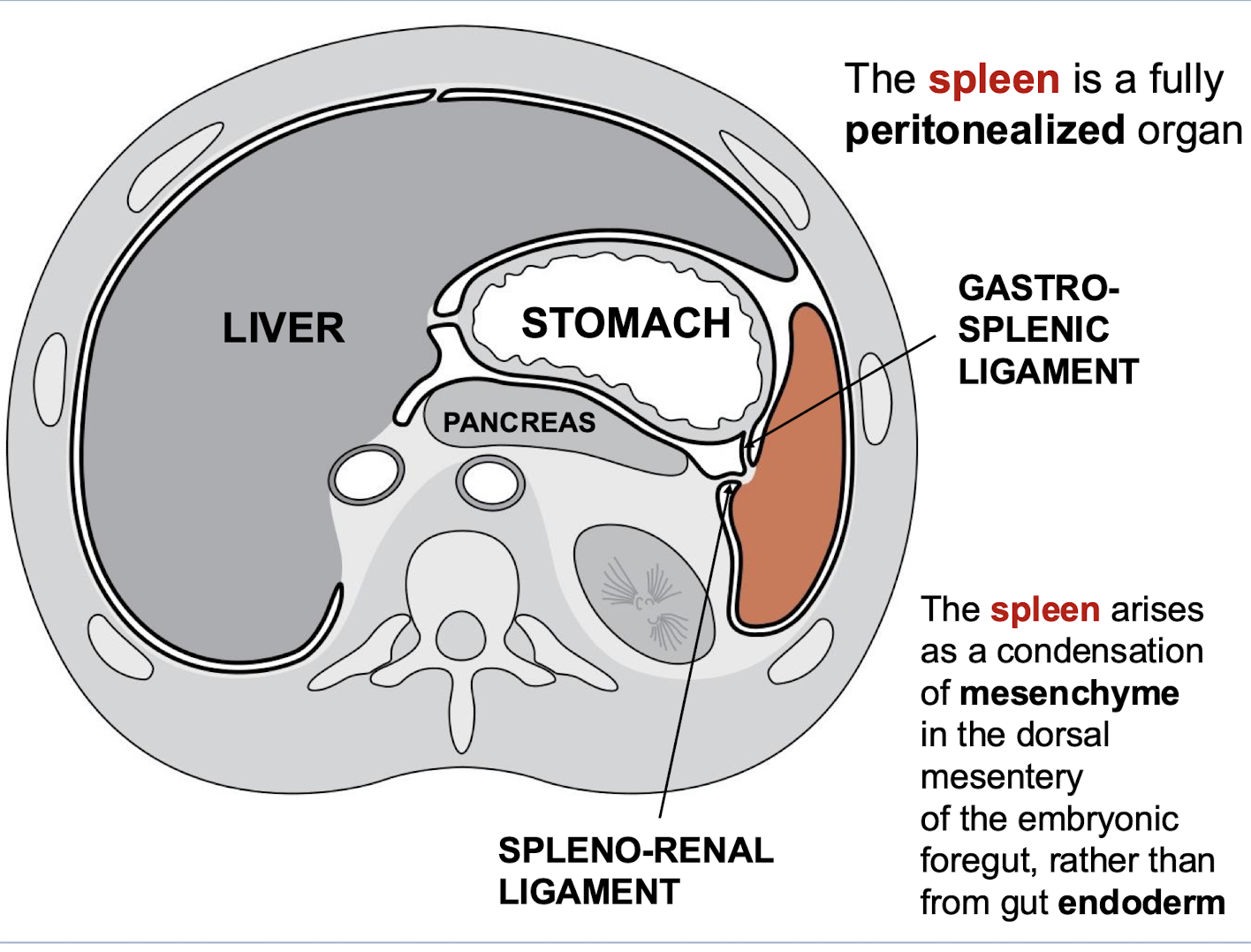
What is seen passing when the stomach is removed and its dorsal mesentery opened
The splenic artery and vein through the spleen’s hilum as it lies in the left upper quadrant.
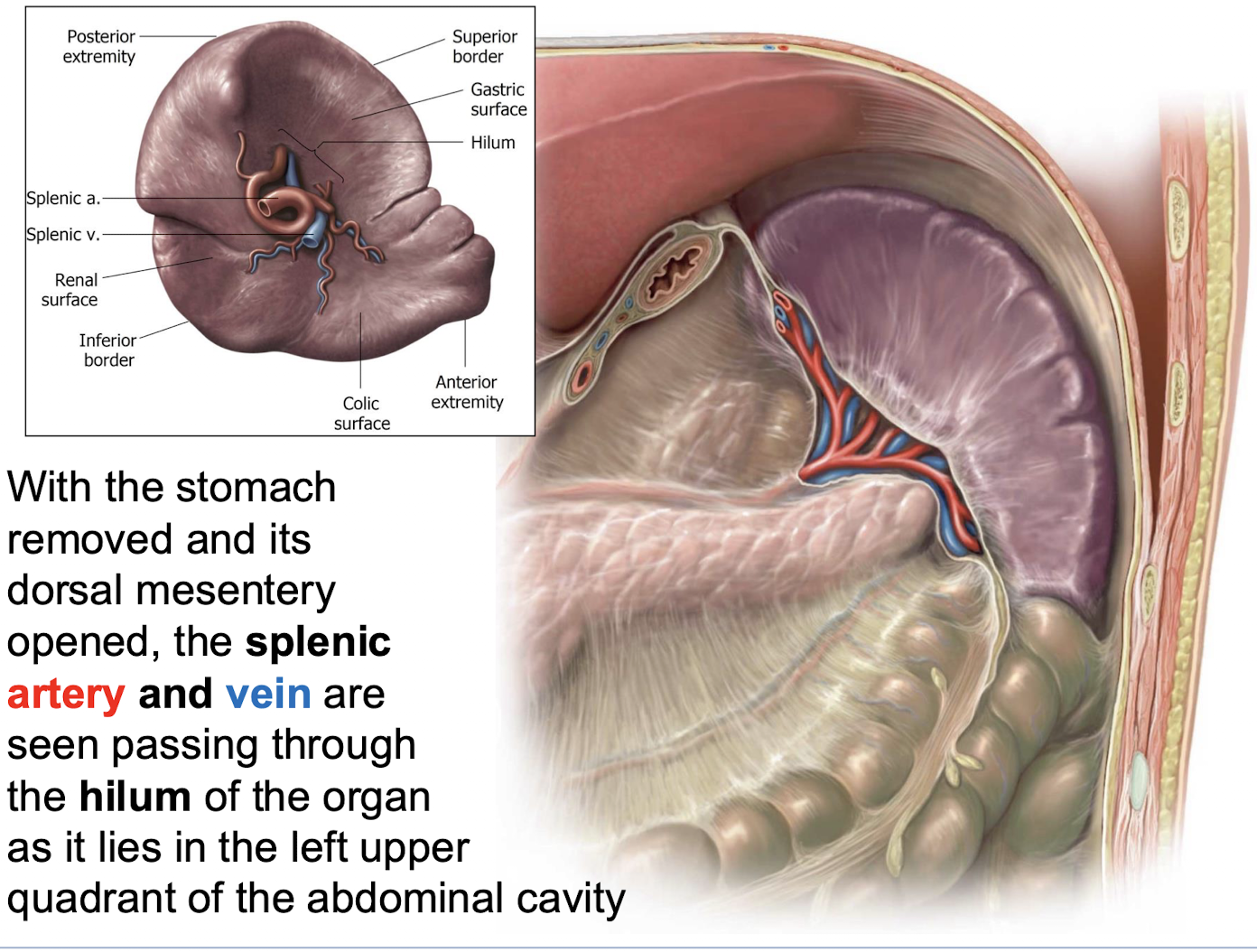
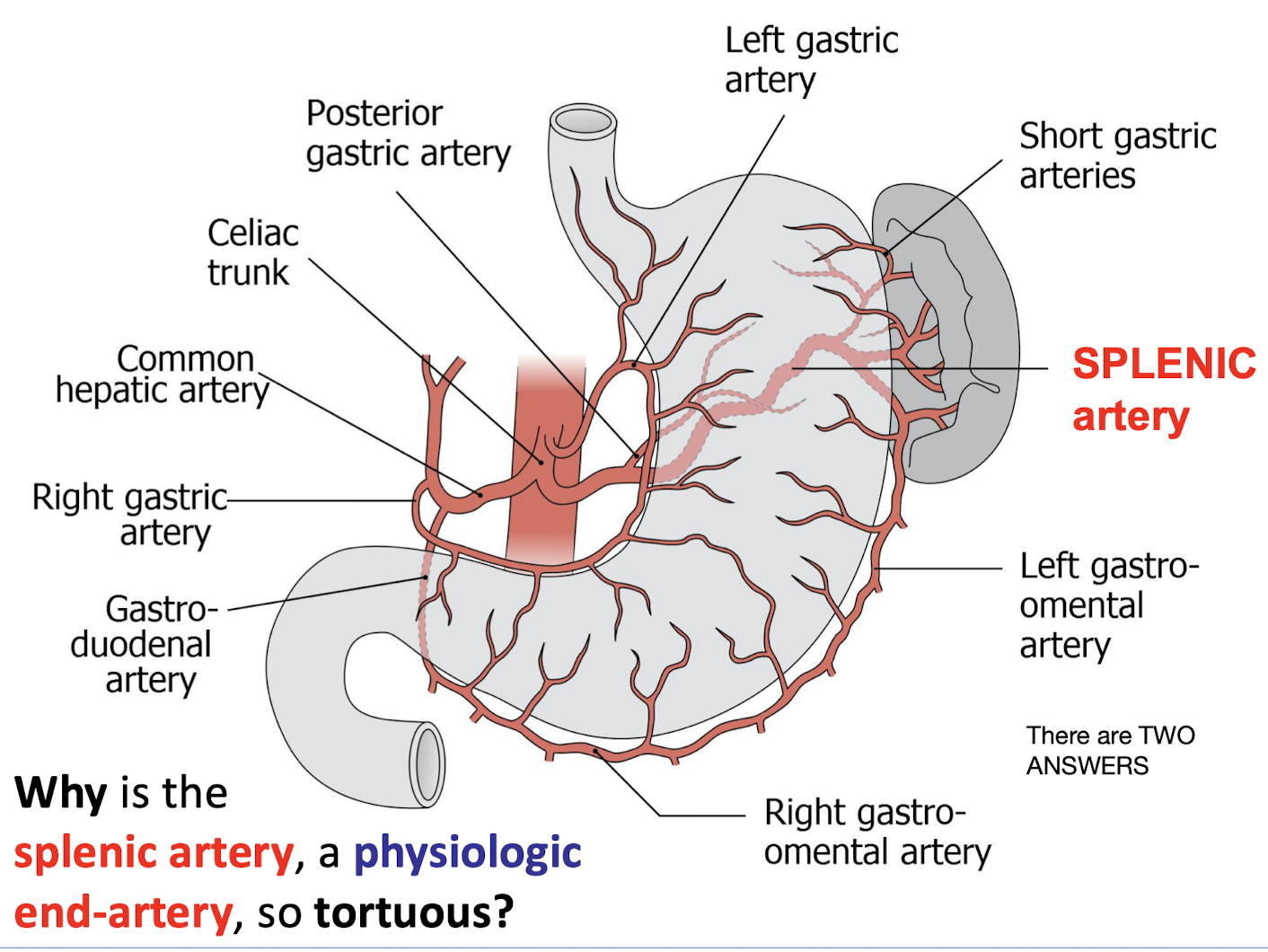
Why is the splenic artery, a physiologic end-artery, so tortuous?
The stomach is a constantly moving organ due to its churning smooth muscle, so the splenic artery must accommodate this motion.
The spleen holds a large volume of blood, meaning blood flow into it faces significant resistance.
Additionally, tortuous (‘kinky’) arteries are often seen in individuals with peripheral hypertension.
What may cause splenomegaly?
Splenomegaly may result from
• viral or parasitic infections
• hemolytic anemias
• blood cancers
Why is the spleen predisposed to relatively easy rupture
Its location immediately deep to fragile ribs; coupled with the organ's vascularity and its living consistency, predisposes the organ to rupture by external trauma
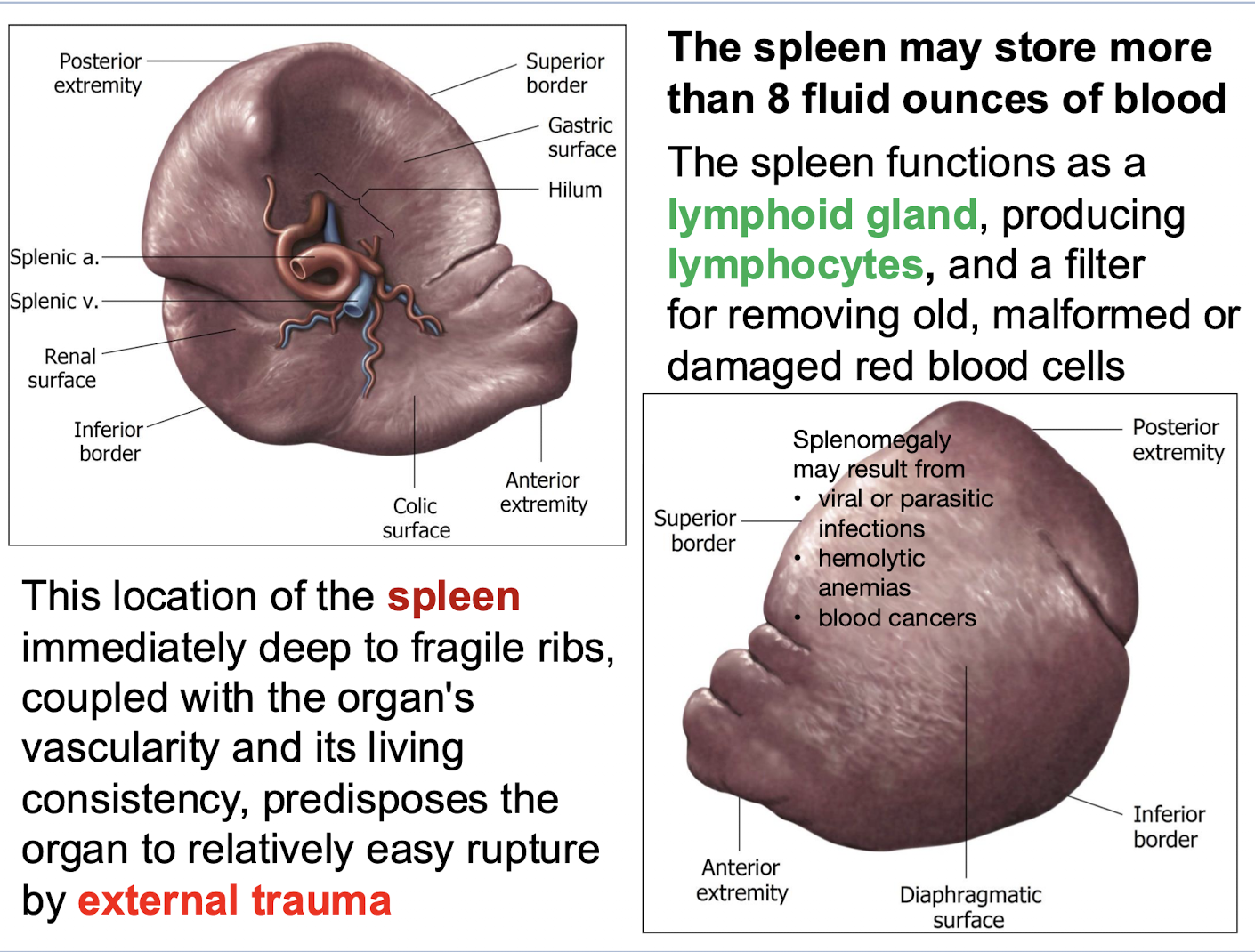
What are the primary functions of the spleen
It functions as a lymphoid gland producing lymphocytes, and a filter for removing old, malformed or damaged red blood cells
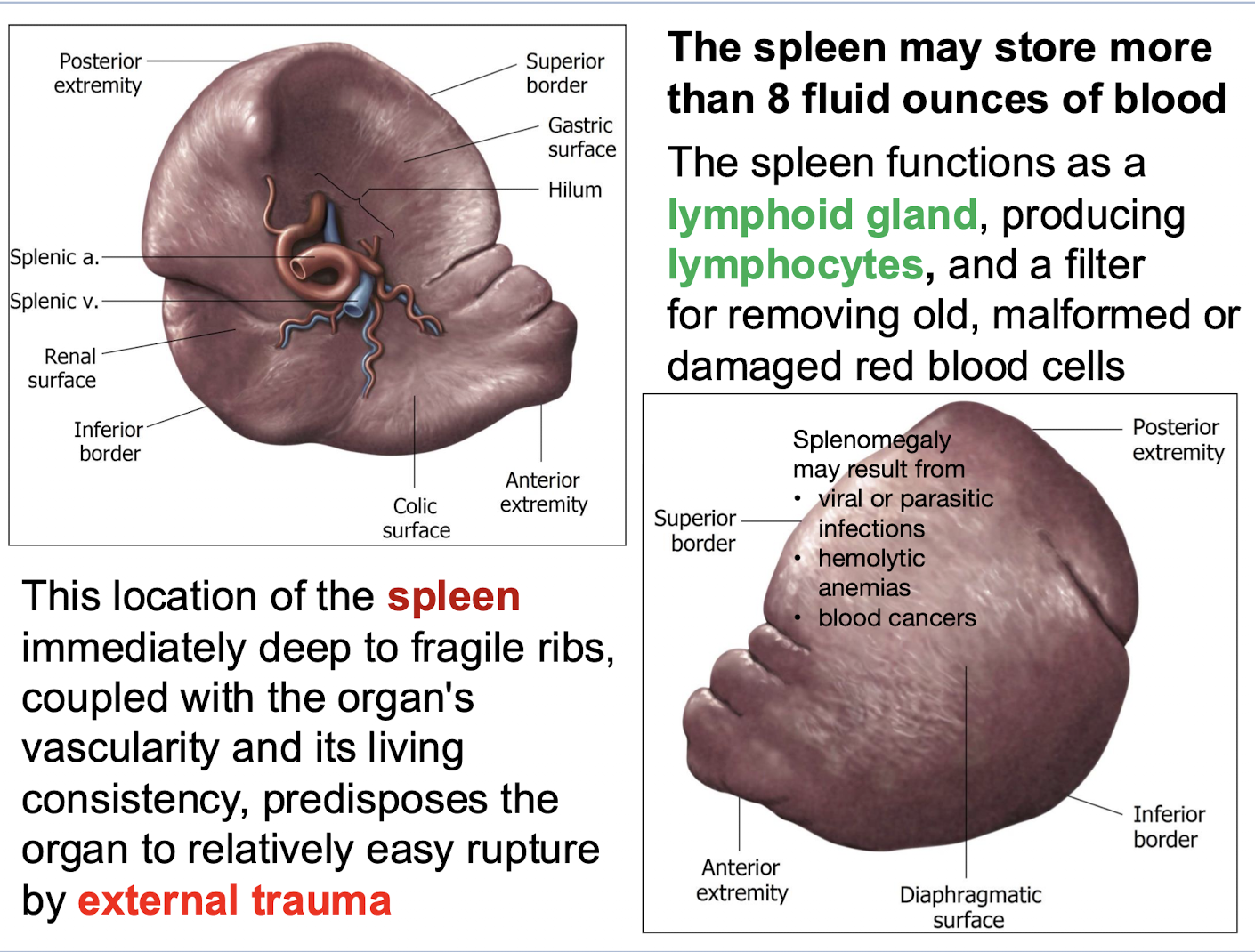
How much blood may the spleen store
More than 8 fluid ounces of blood.
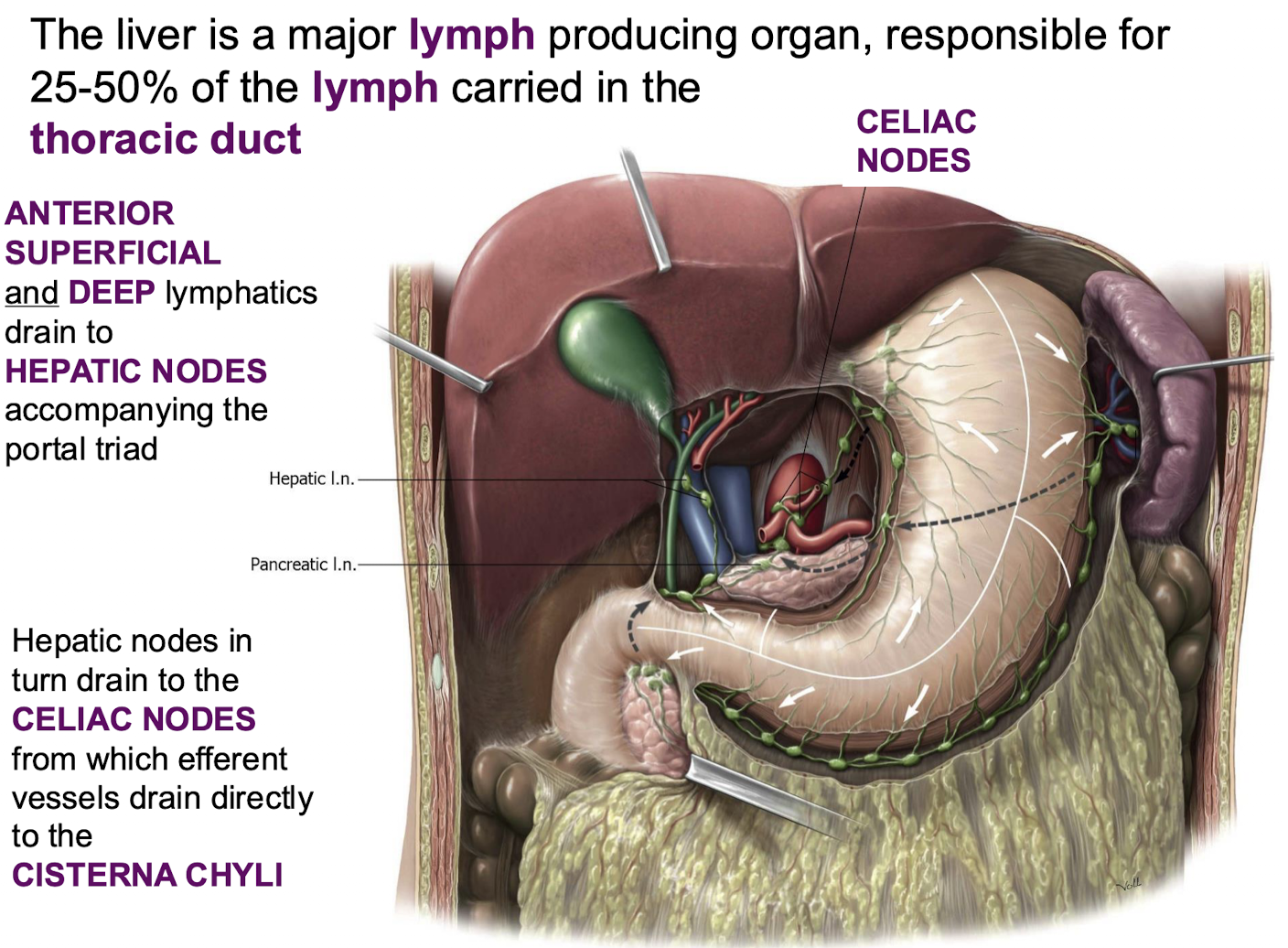
What percentage of lymph carried in the thoracic duct is produced by the liver
25-50%.
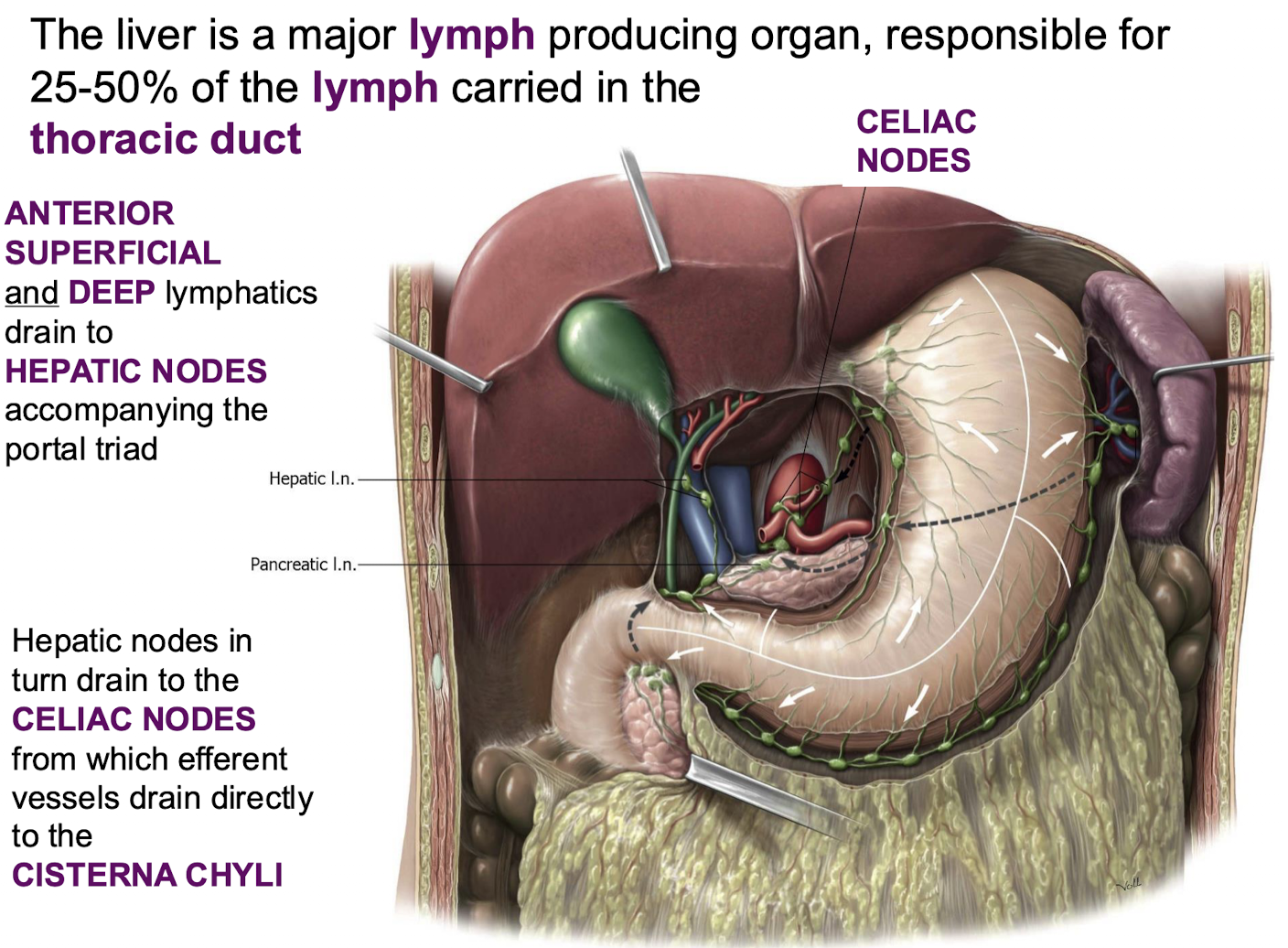
What is the general drainage pathway for liver lymphatics
ANTERIOR SUPERFICIAL and DEEP lymphatics drain to HEPATIC NODES accompanying the portal triad; which in turn drain to the CELIAC NODES; from which efferent vessels drain directly to the CISTERNA CHYLI (a dilated, sac-like structure that serves as the abdominal origin for the thoracic duct).
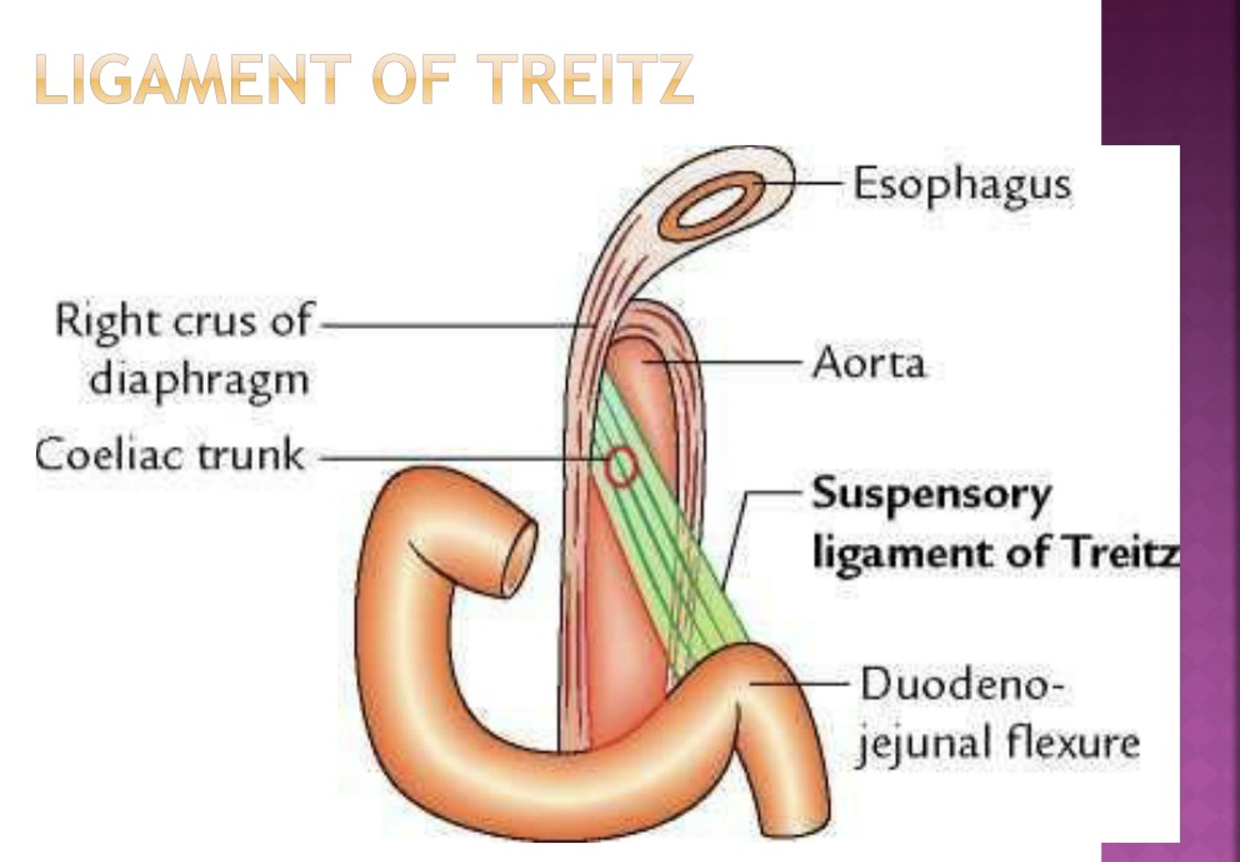
A patient undergoes surgery where the DUODENOJEJUNAL JUNCTION needs stabilization. What structure is implicitly responsible for suspending this junction and maintaining its patency?
The fibers of the Ligament of Treitz, a diaphragmatic extension
Important for surgery
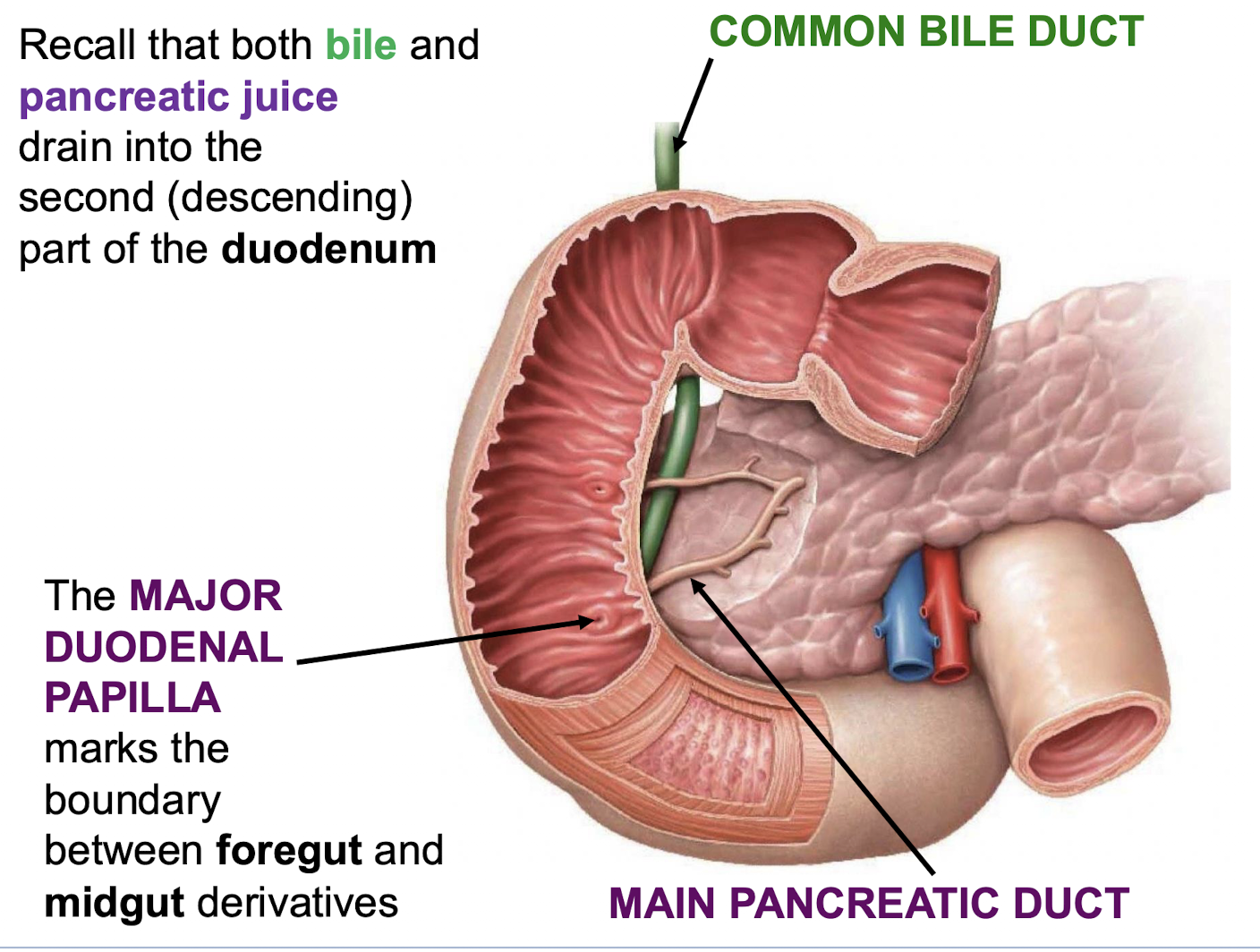
What landmark marks the boundary between foregut and midgut derivatives
The MAJOR DUODENAL PAPILLA.
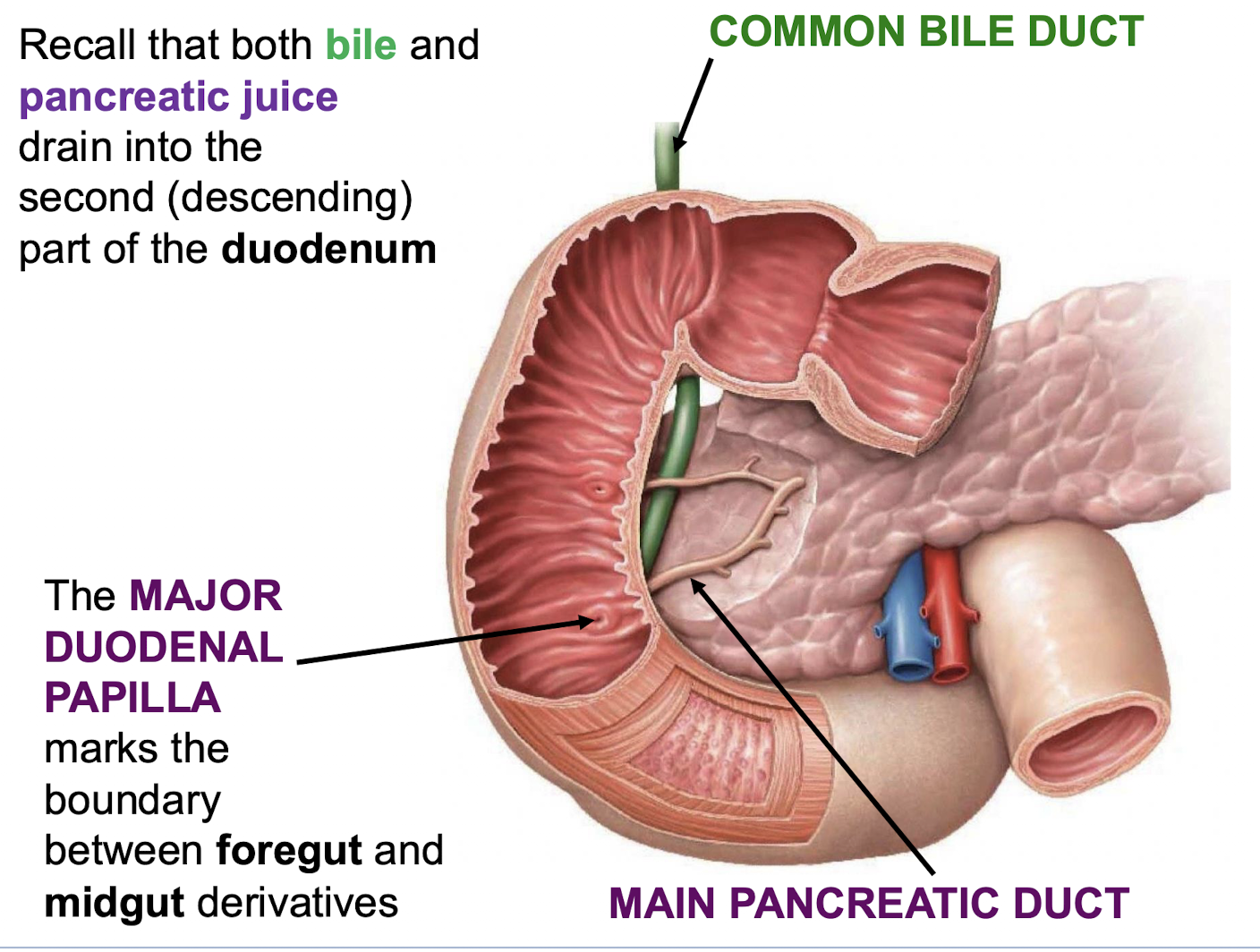
Into what part of the duodenum do bile and pancreatic juice drain
The second (descending) part of the duodenum.
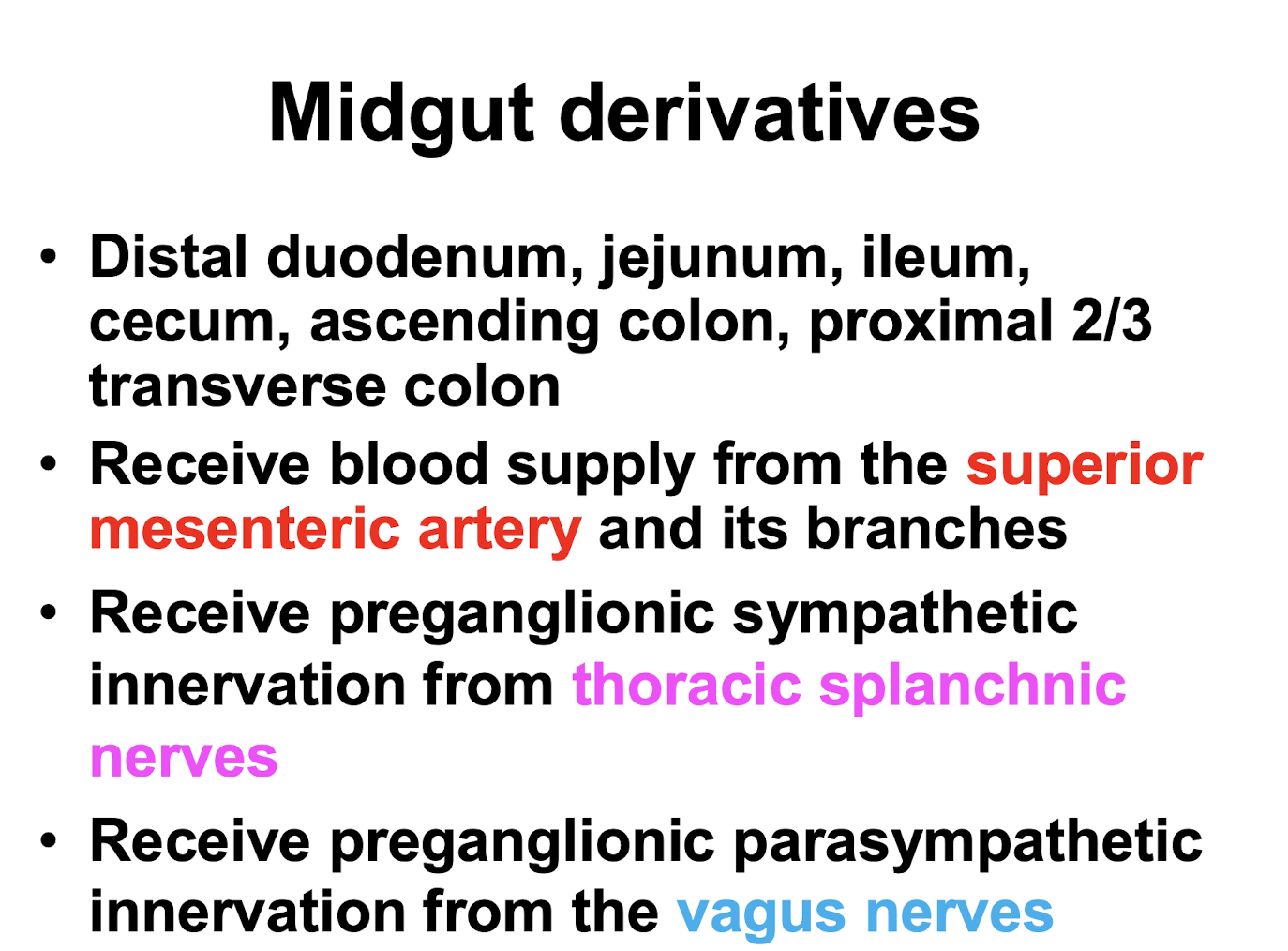
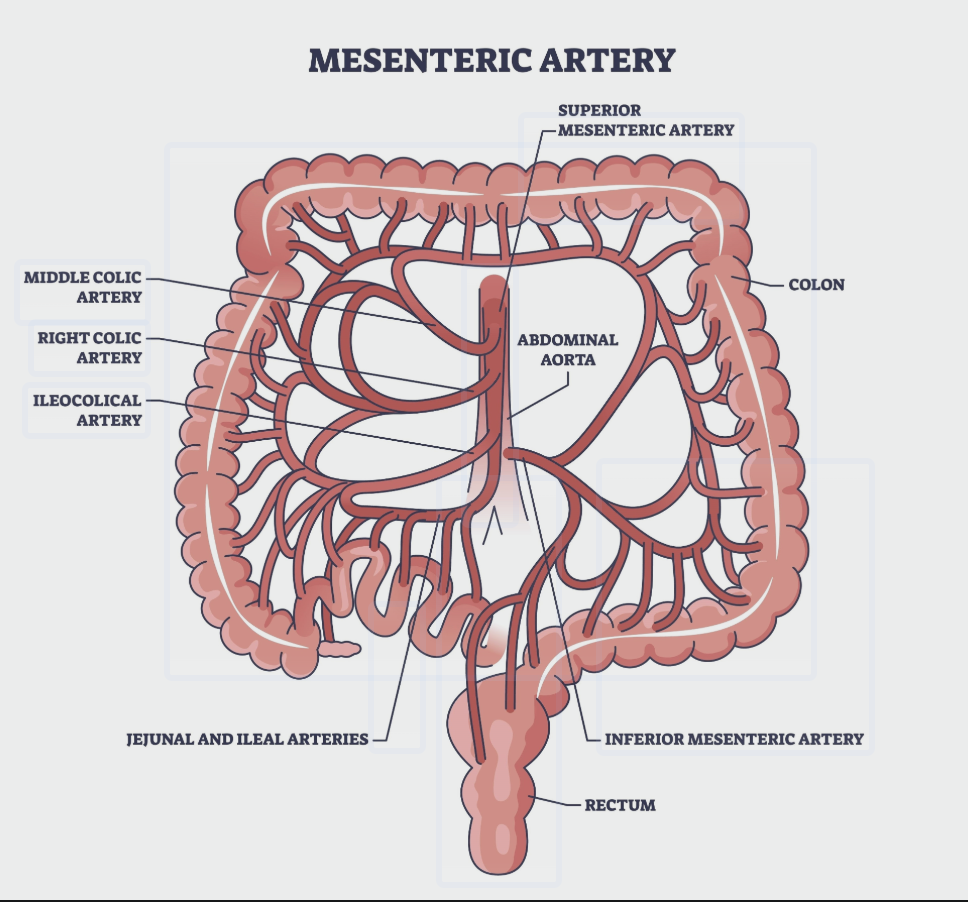
What are the derivatives of the embryonic midgut
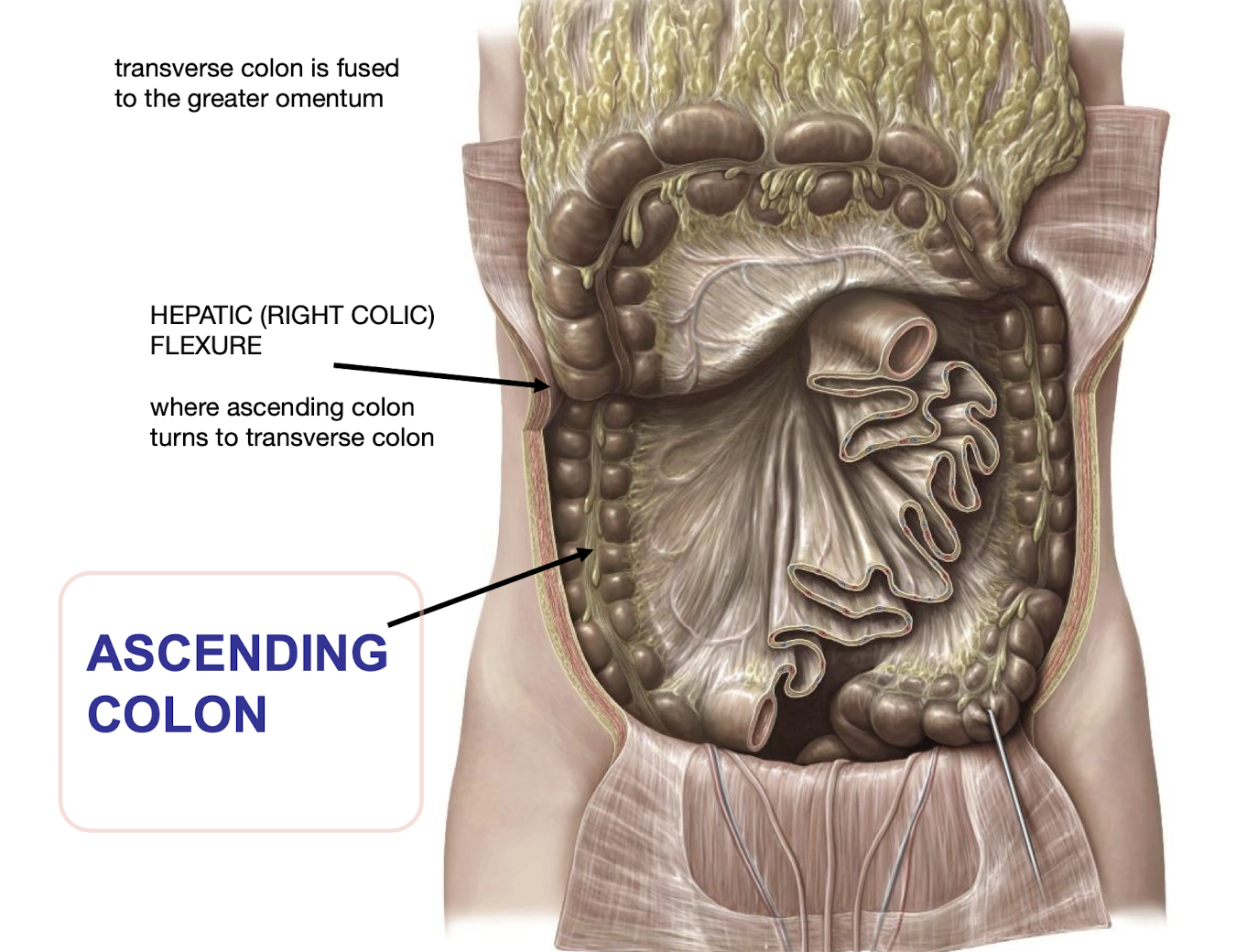
Distal duodenum; jejunum; ileum; cecum; ascending colon; proximal 2/3 transverse colon.
What provides the blood supply to the midgut derivatives
The superior mesenteric artery (SMA) and its branches.
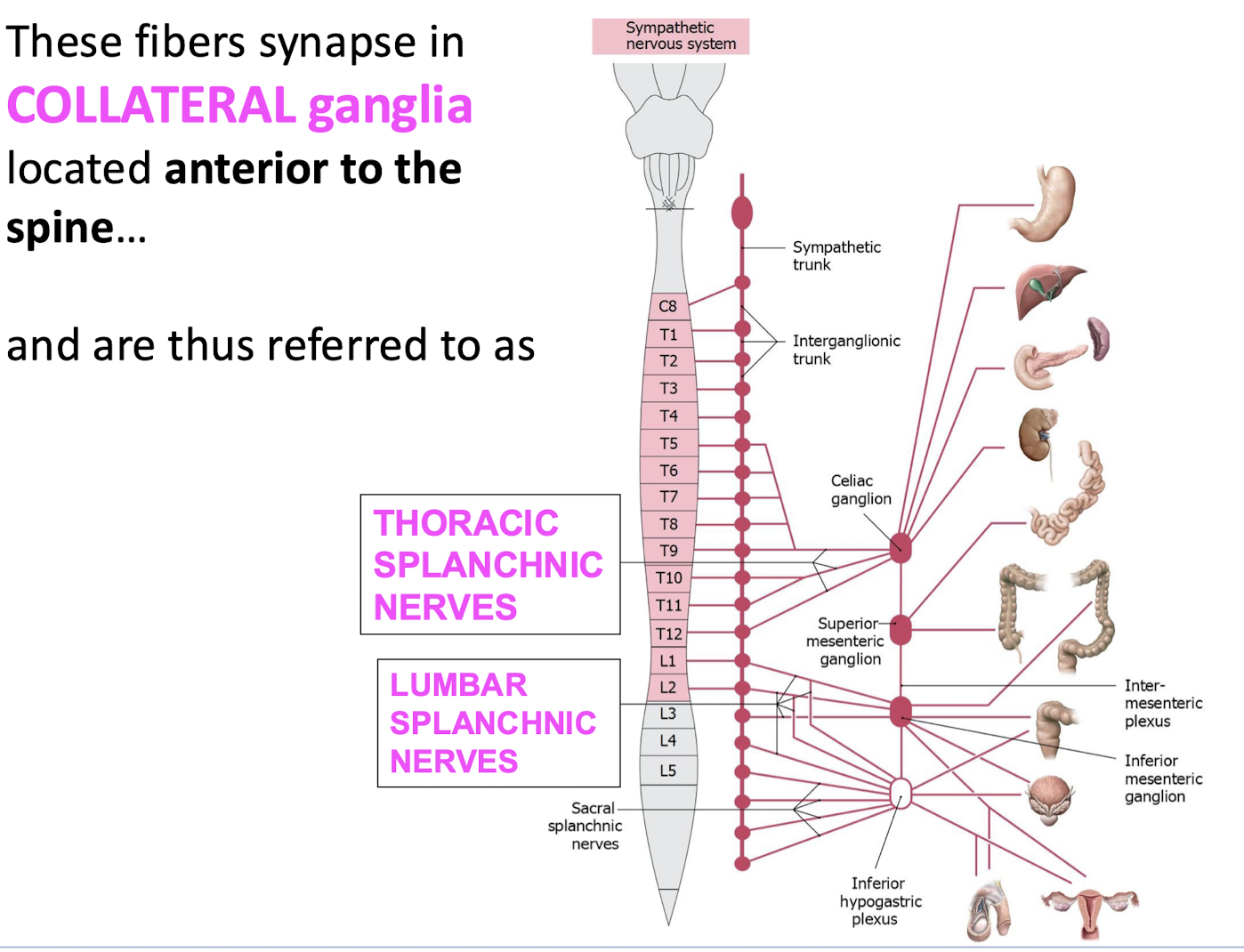
From where do midgut derivatives receive preganglionic sympathetic innervation
Thoracic splanchnic nerves.
From where do midgut derivatives receive preganglionic parasympathetic innervation
The vagus nerves.
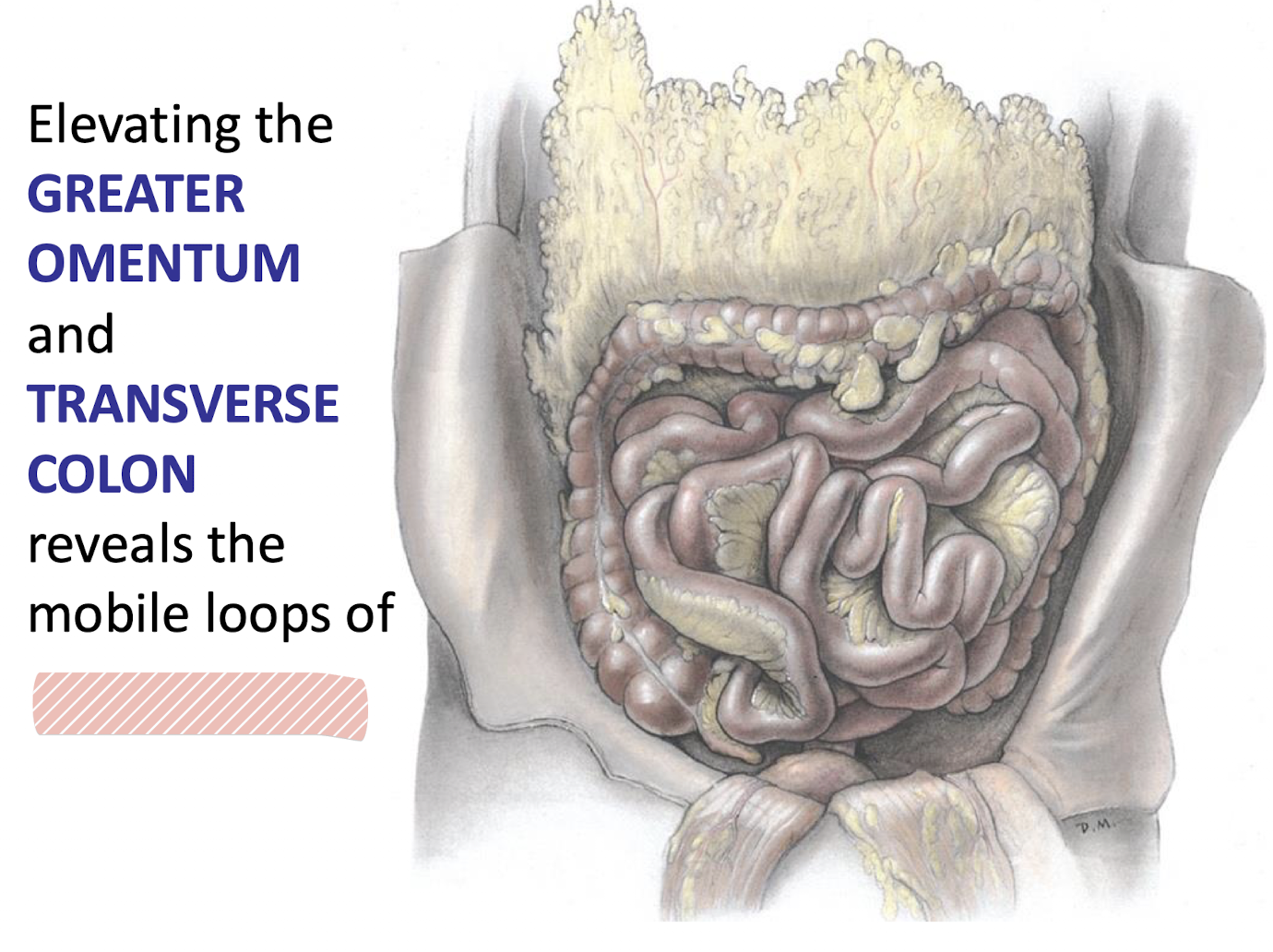
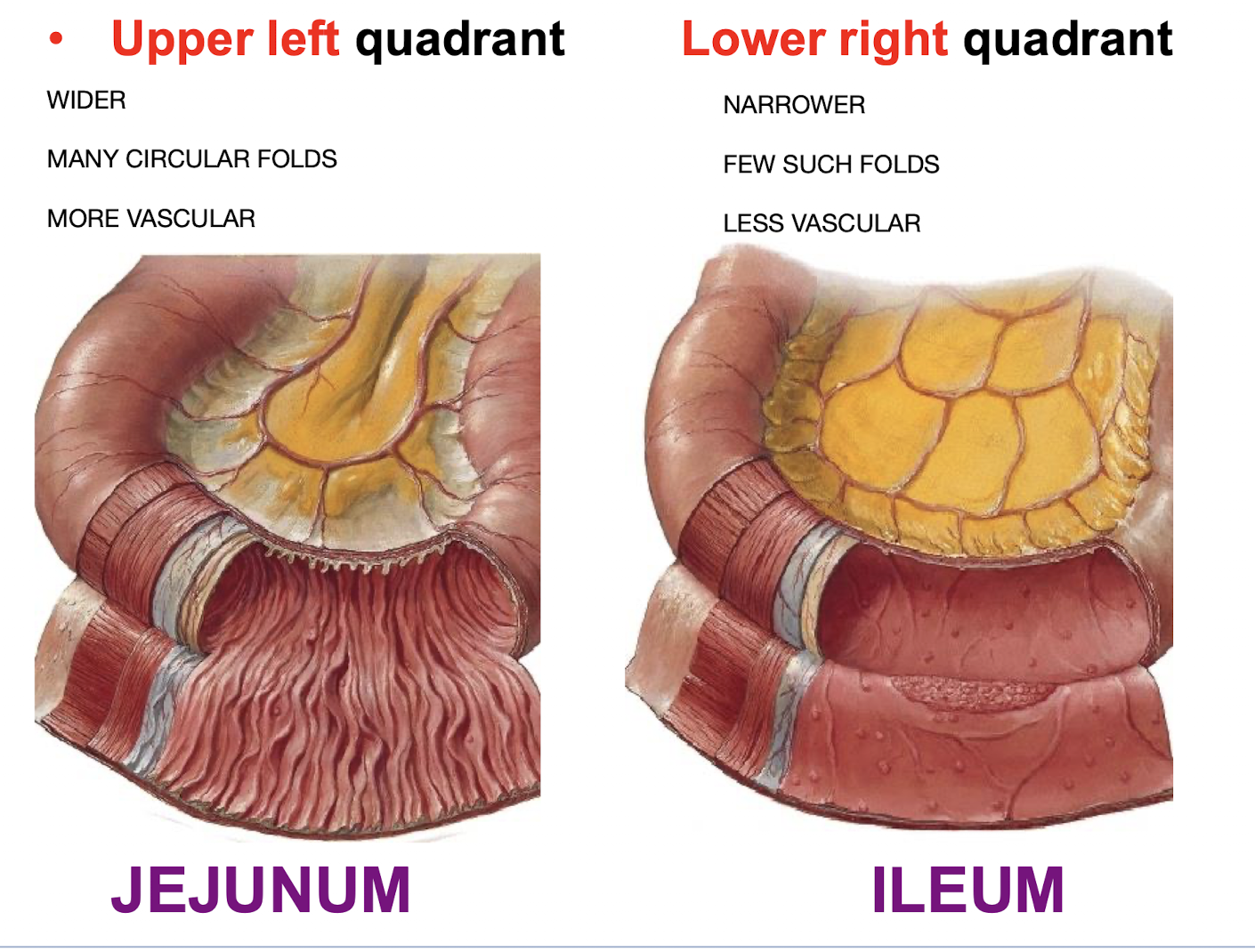
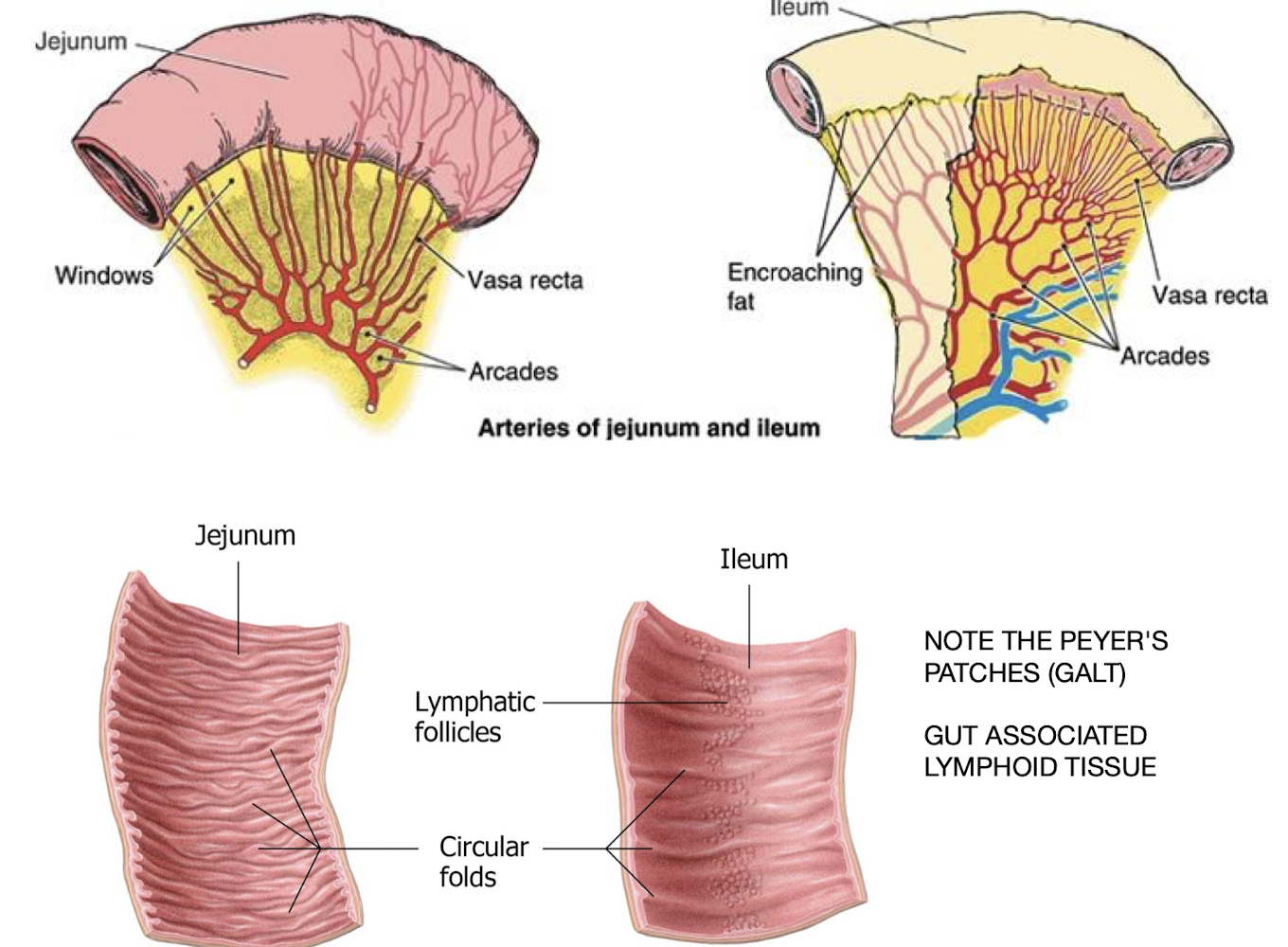
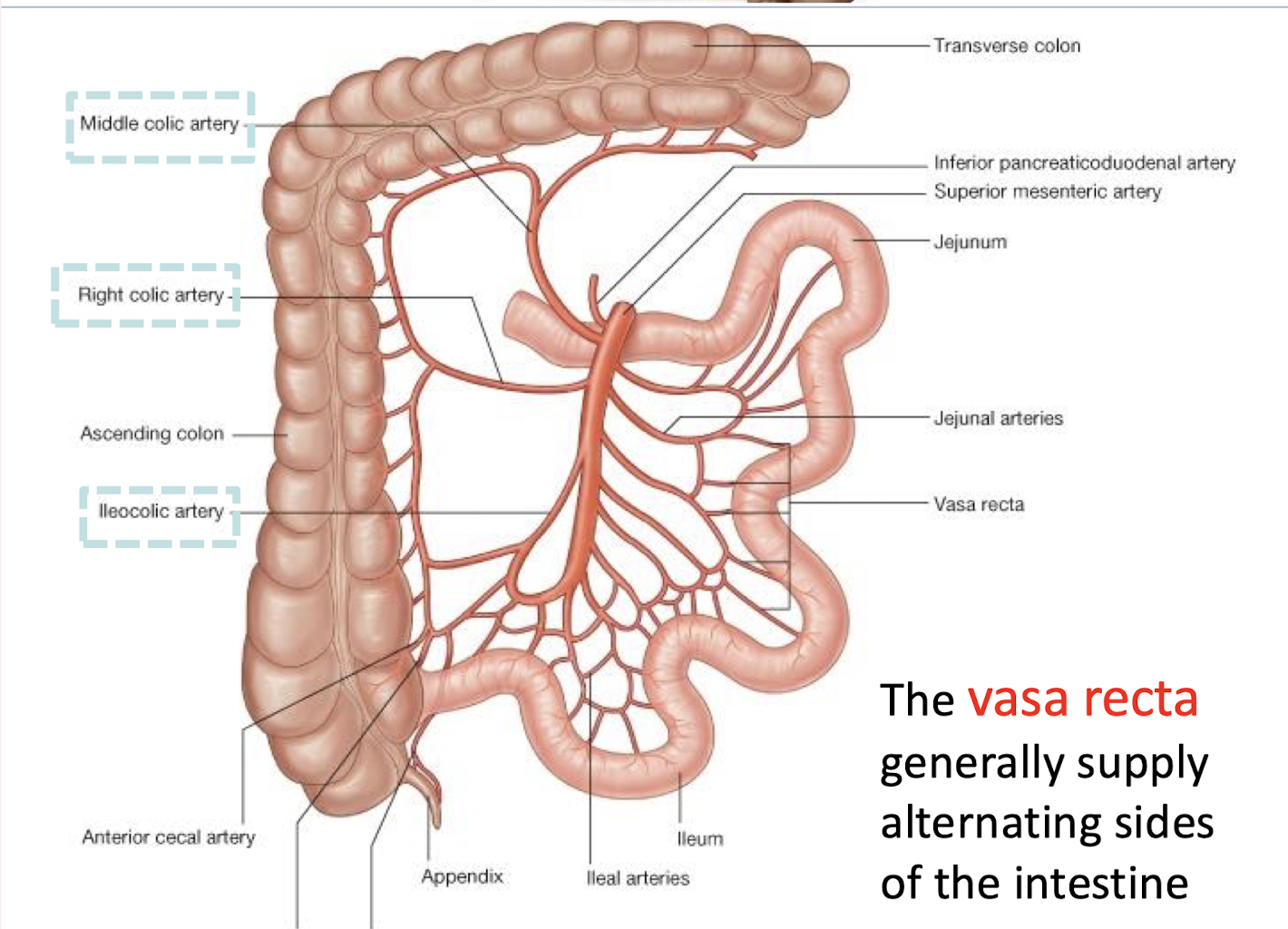
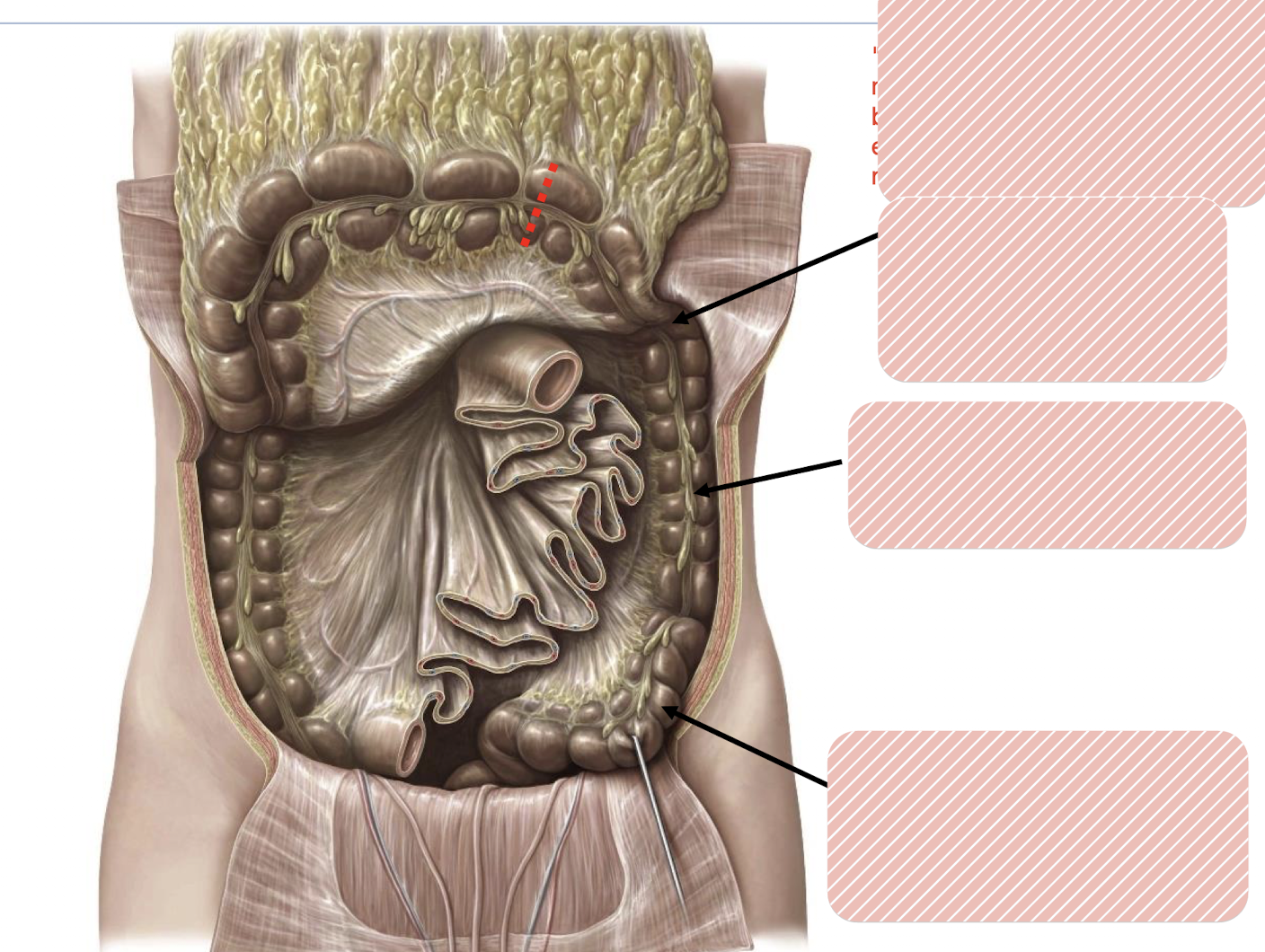
Jejunum and Ileum which have much in common in terms of both structure and peritoneal relationships
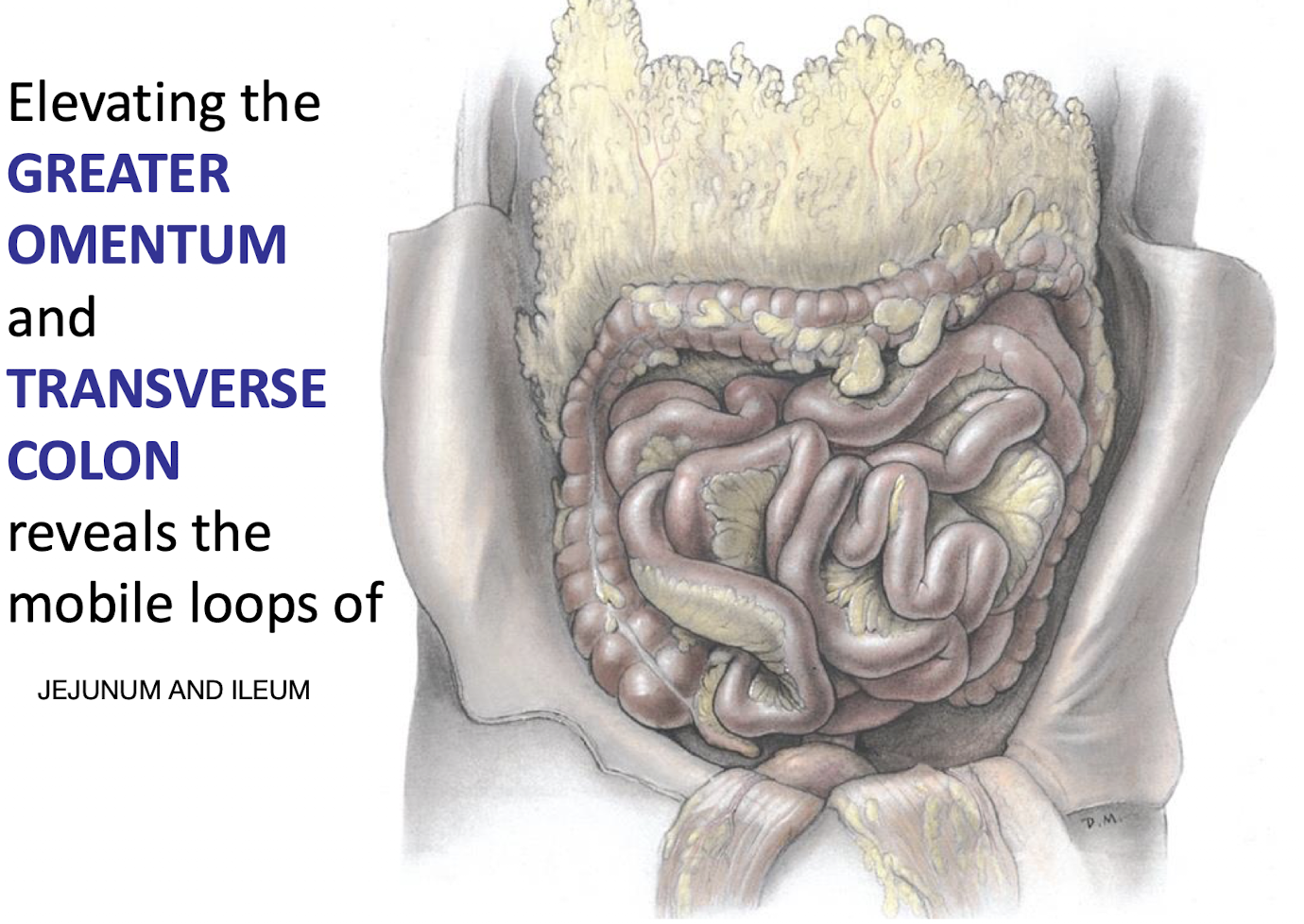
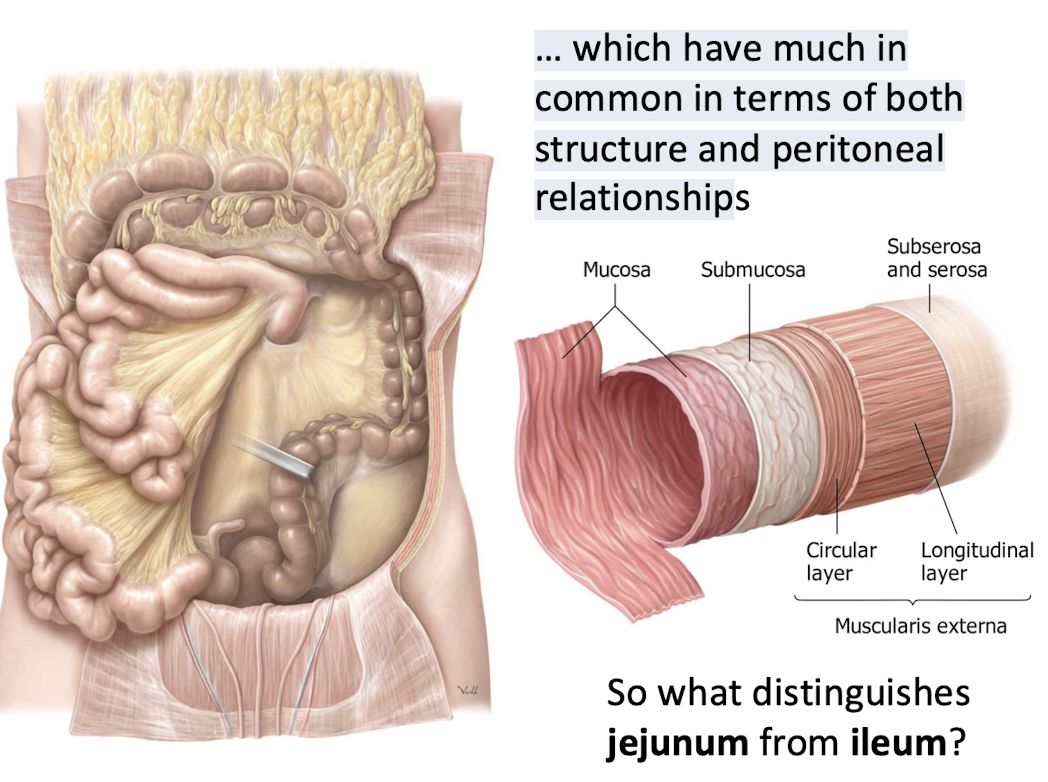
Compare and contrast the jejunum and Ileum. Including location in the abdomen, physical and internal architecture, and vasculature
Where is GALT located and what is its significance?
In the ILEUM
Plays a key role in immune defense against pathogens entering via the gut
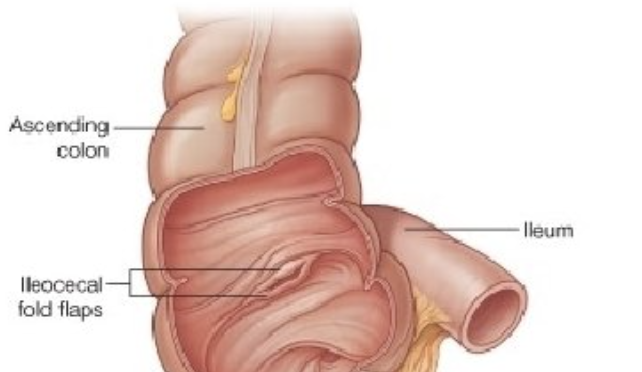
What is the function of the ileo-cecal valve ?
It prevents reflux of bacteria-laden cecal contents into the small intestine.
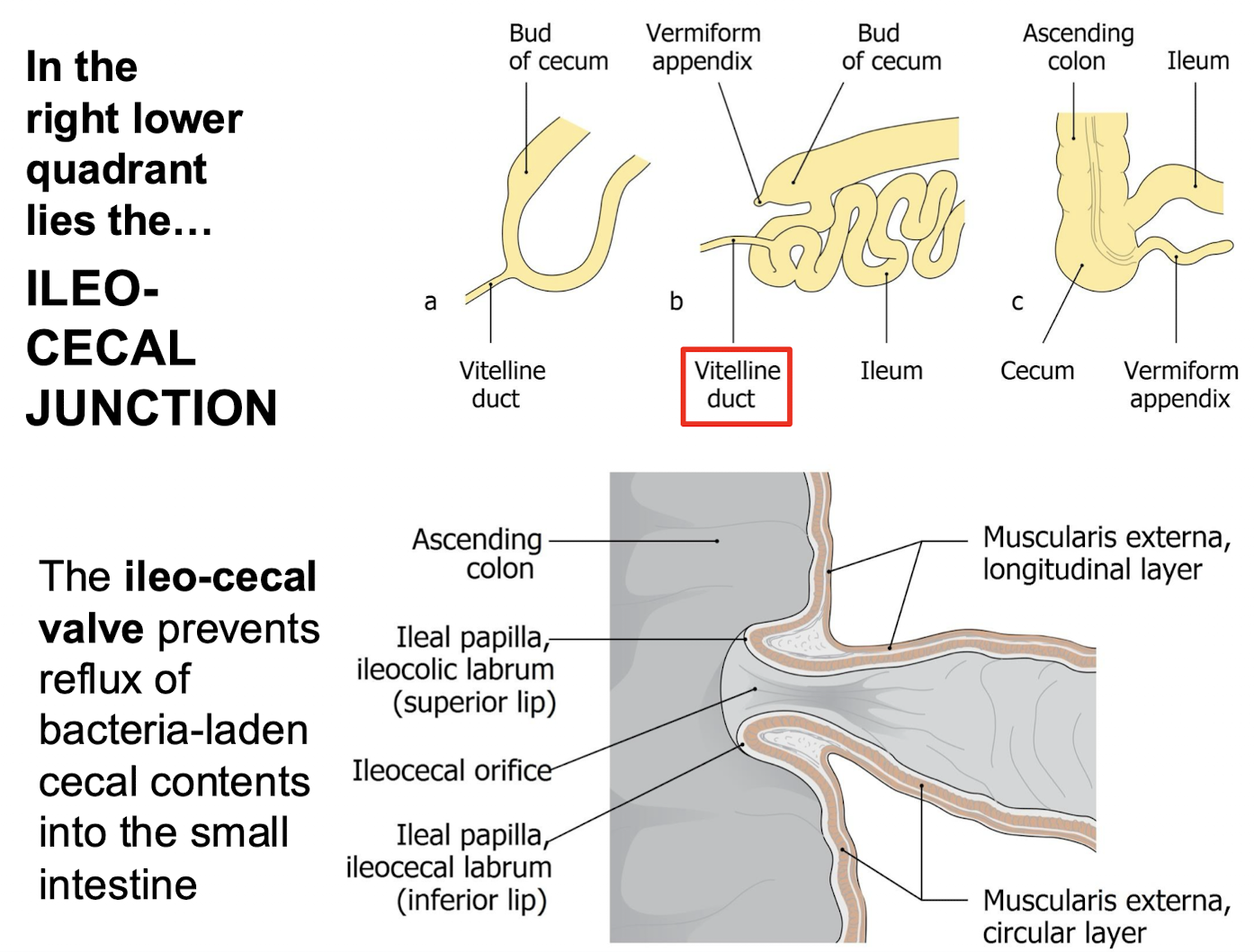
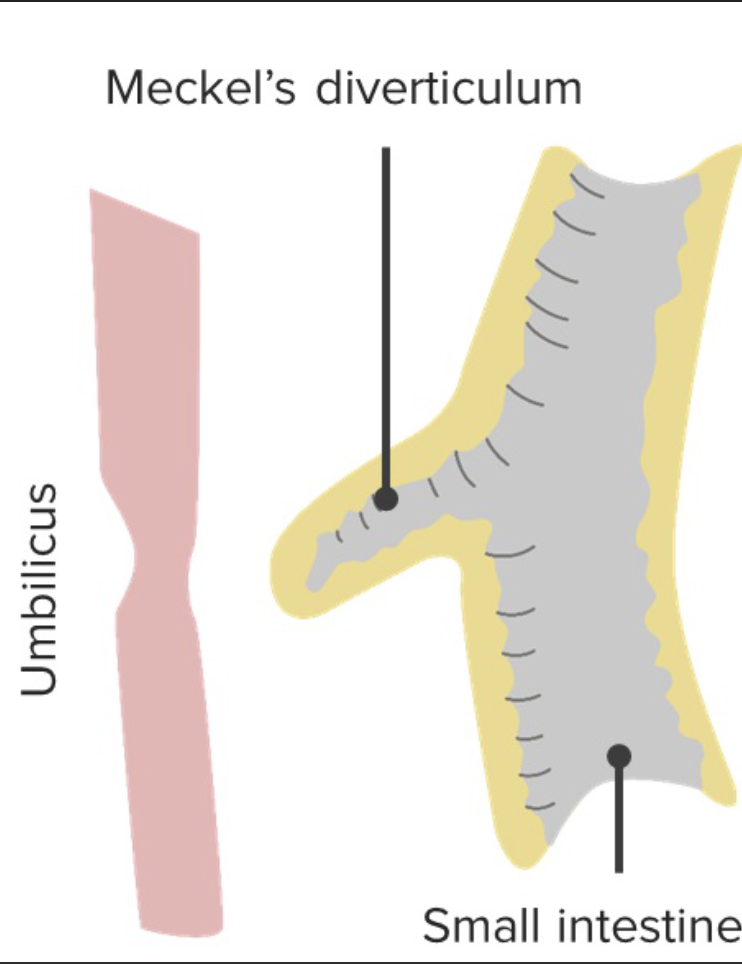
What structure lies in the right lower quadrant and what is a common congenital anomaly there
Ileocecal Junction
Clinical Note:
About 2% of people have a Meckel’s diverticulum near this region
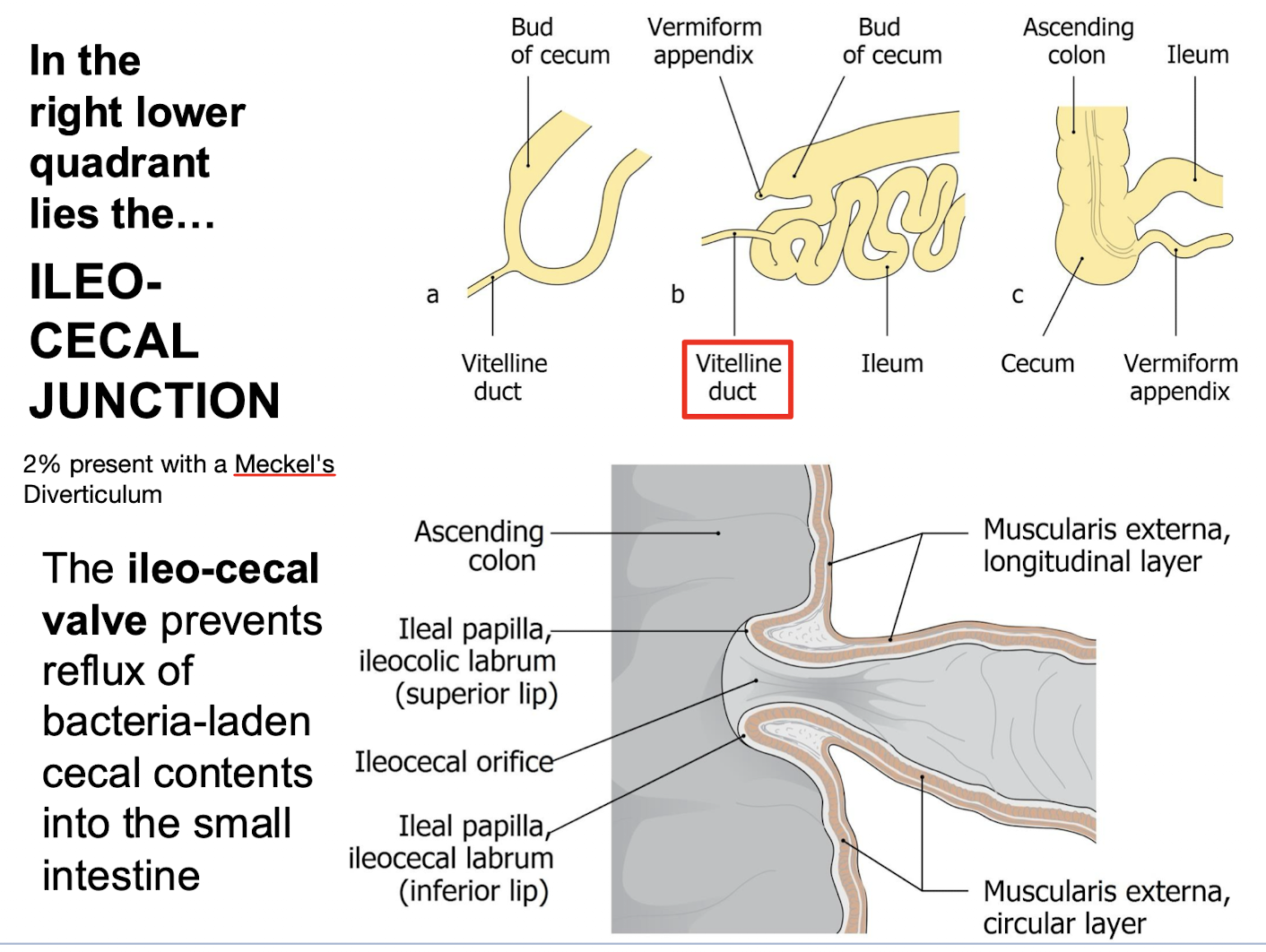
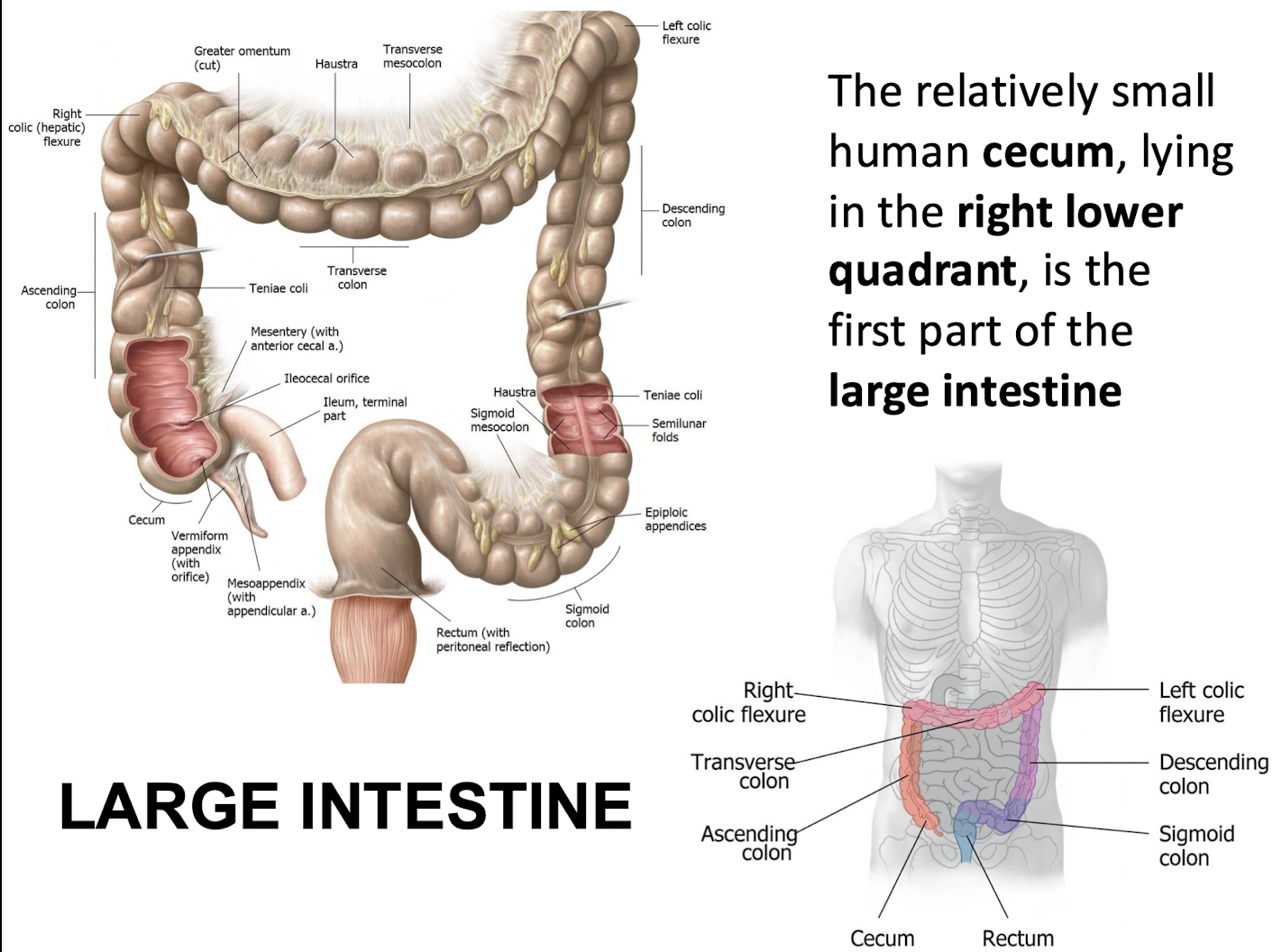
What is the first part of the large intestine and where is it located?
The relatively small human cecum; lying in the right lower quadrant.
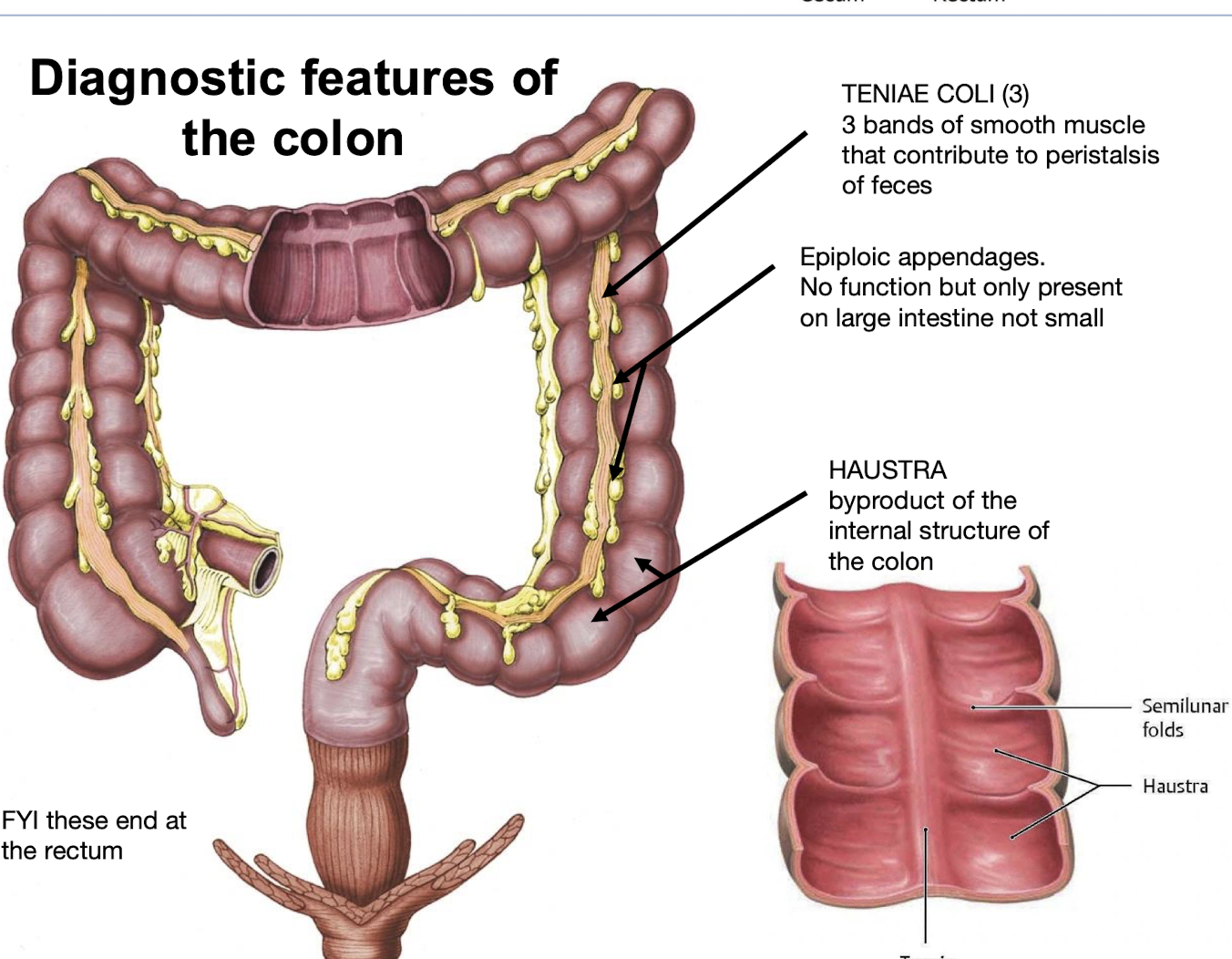
What are the diagnostic features of the colon?
Teniae Coli
Three bands of smooth muscle that contribute to peristalsis of feces.
Epiploic Appendages
Fat-filled pouches; no function but only present on the large intestine (not small).Haustra
Sacculations formed by the internal structure of the colon; appear between semilunar folds.
FYI these end at the rectum
Where does the VERMIFORM APPENDIX open into the large intestine
Open to the cecum inferior to the ileo-cecal valve.
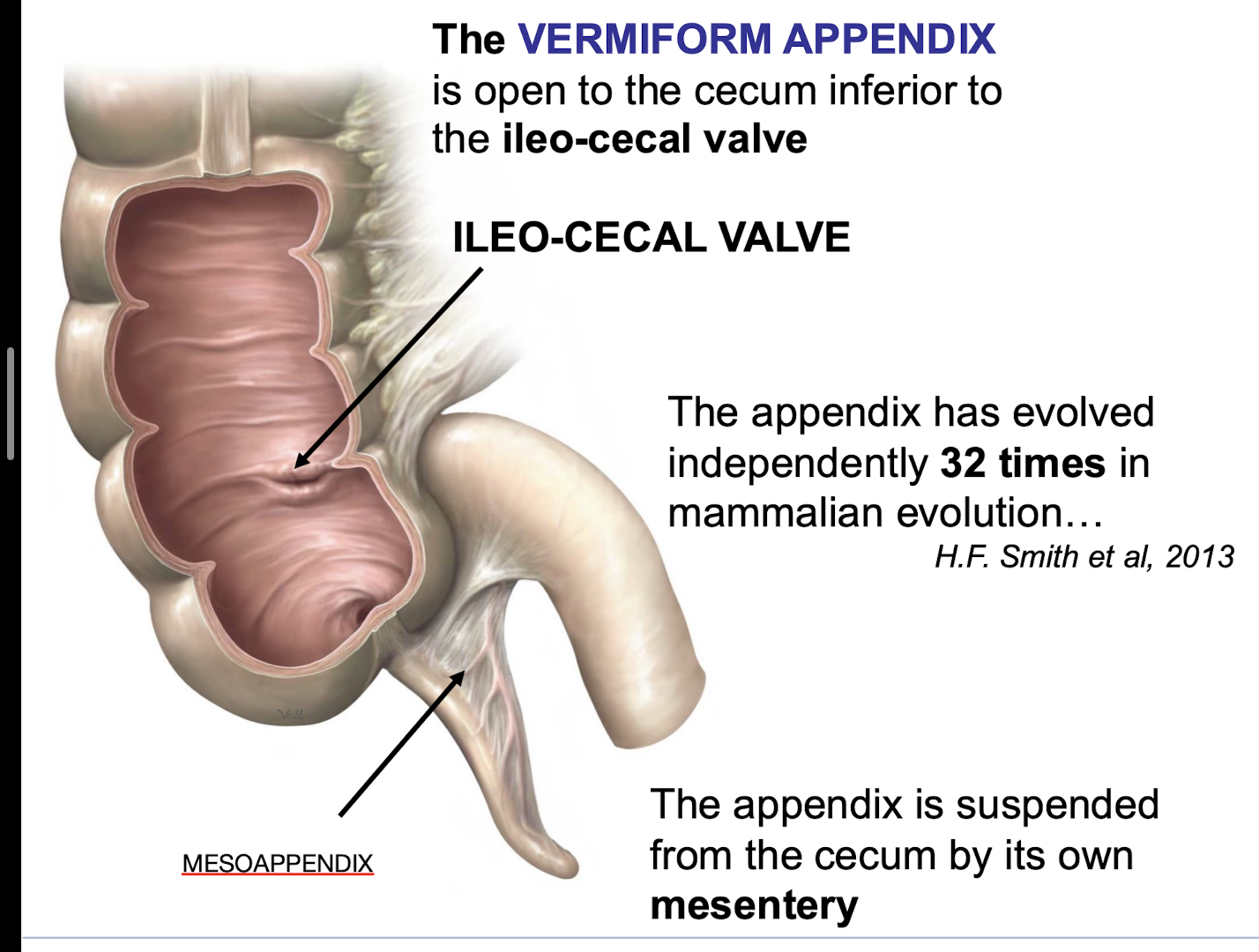
What suspends the appendix from the cecum
Its own mesoappendix
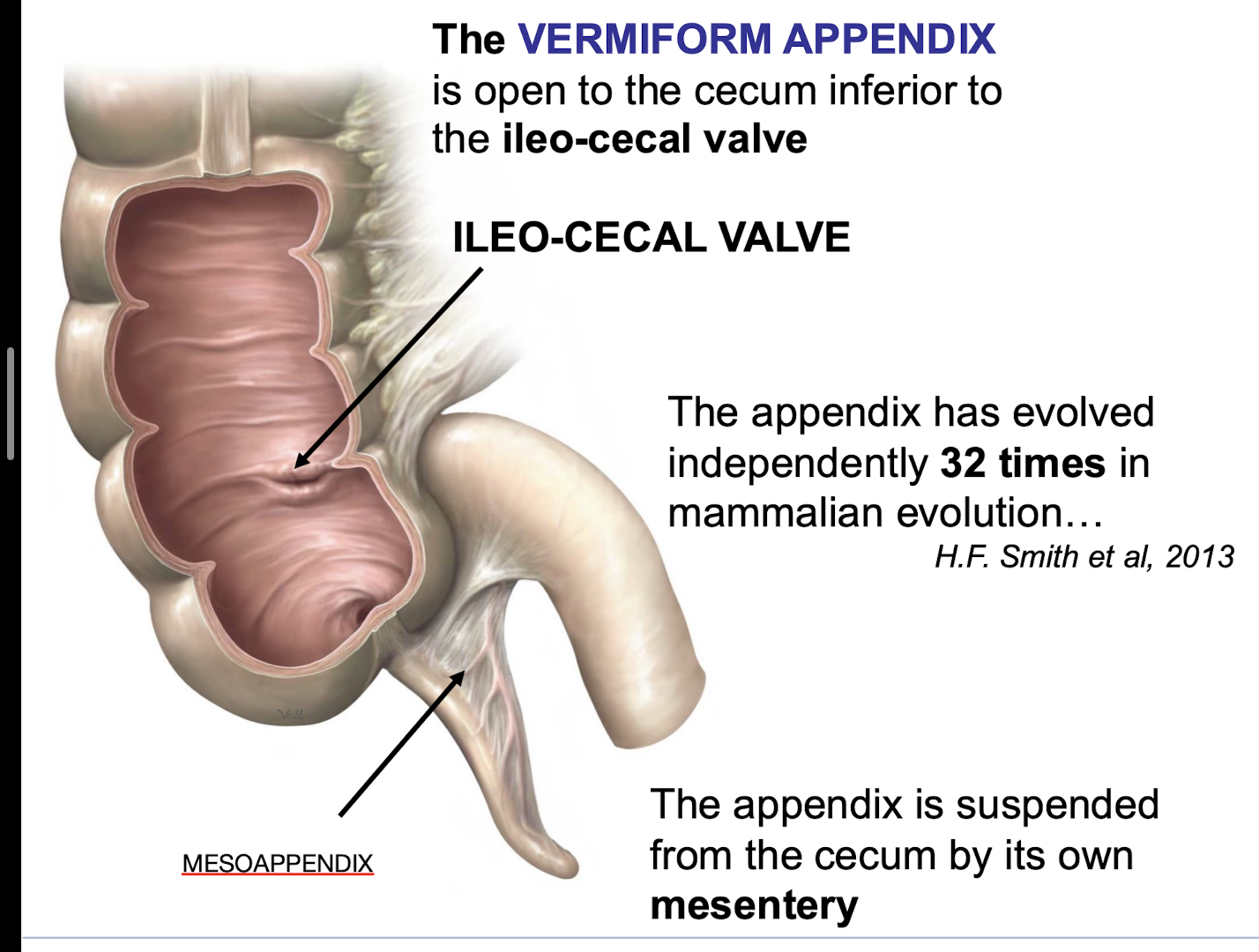
What is the immunological role of the appendix
Acting as a "safe house” for beneficial gut bacteria that help train the immune system and usually prevent disease by outcompeting dangerous pathogenic bacteria.
The theory holds that when dangerous microbes prevail and overrun the gut, beneficial bacteria retreat to the safety of the appendix; once the immune system has defeated the infection, the beneficial bacteria emerge to recolonize the gut
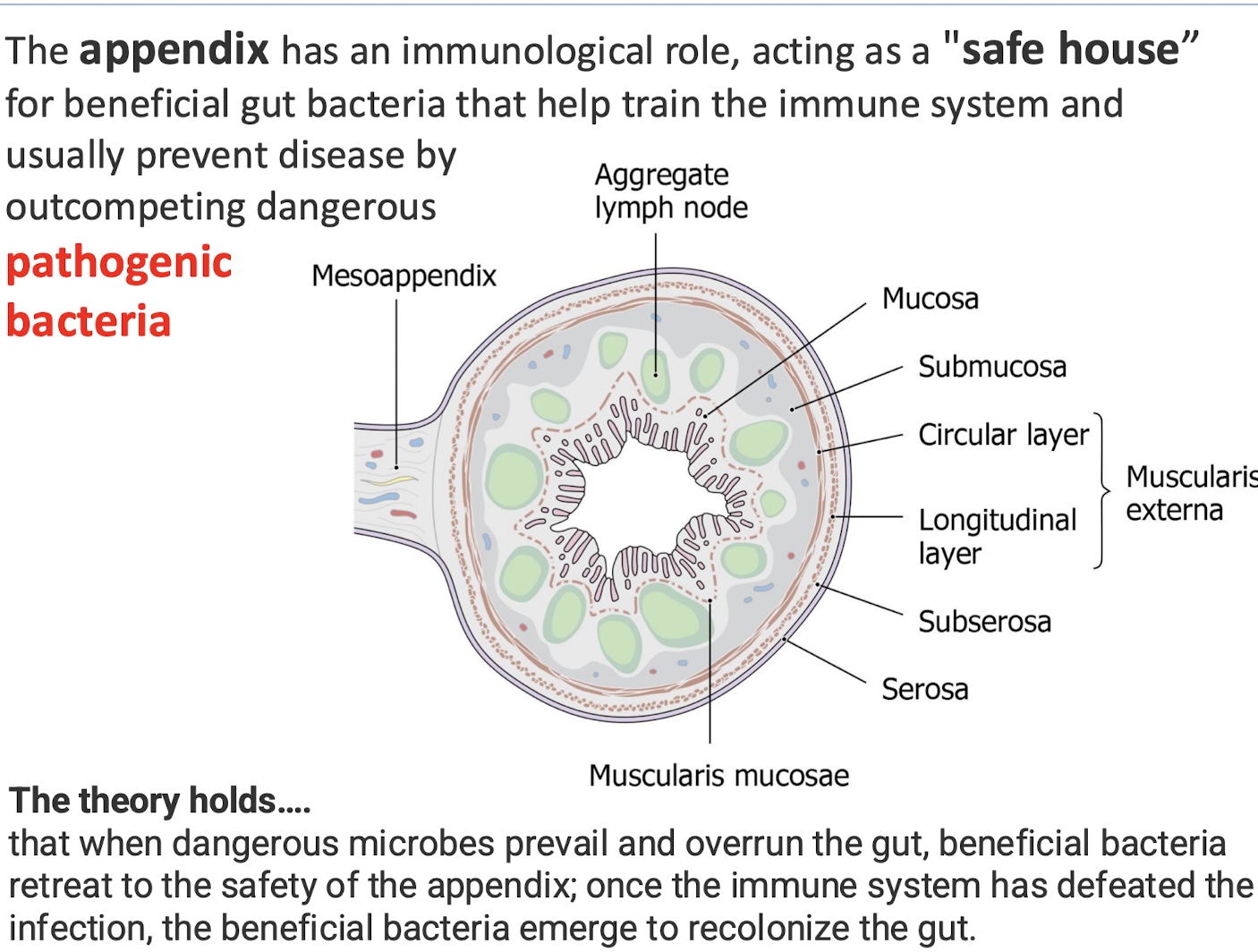
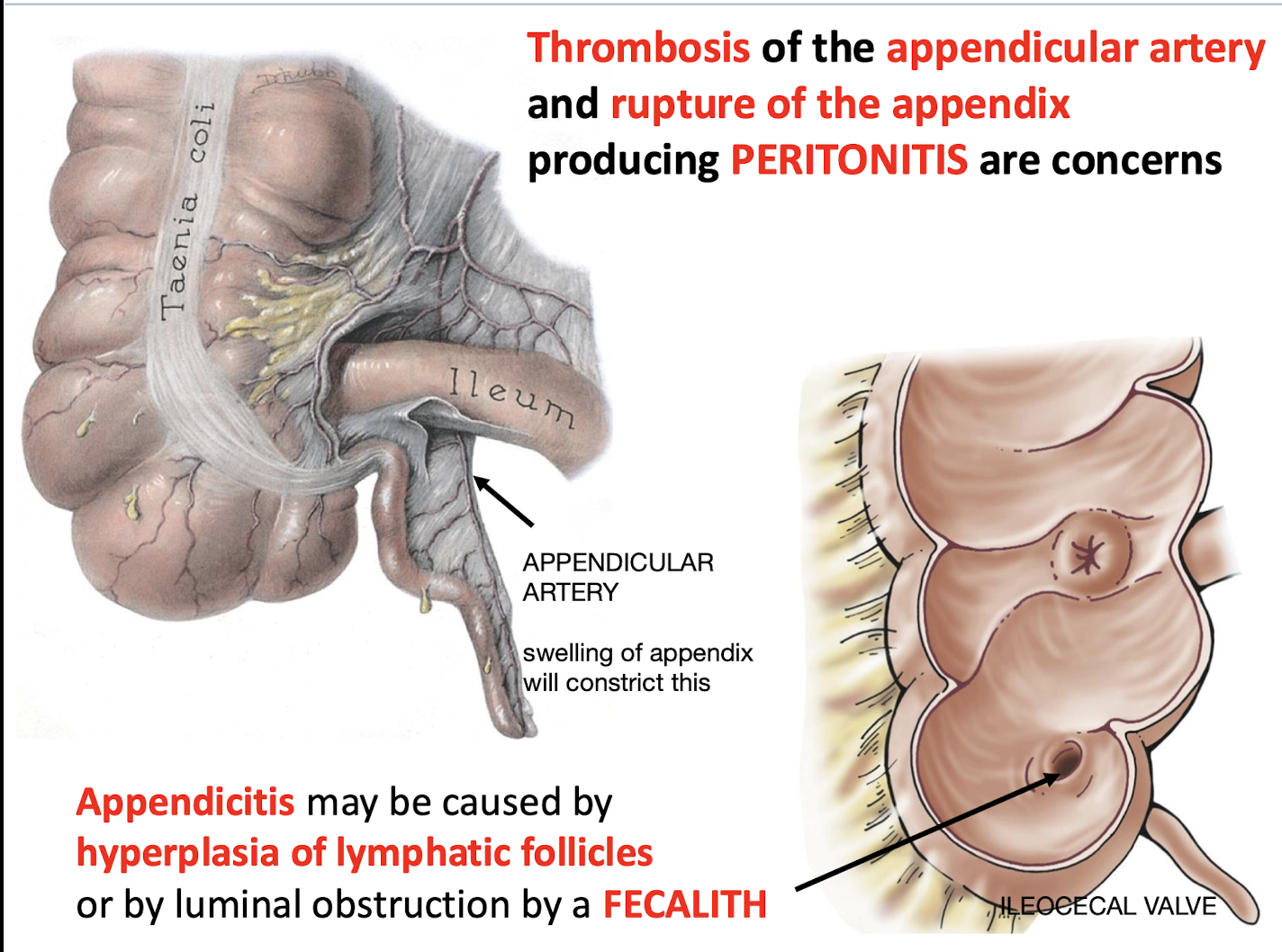
What are common causes of Appendicitis
Hyperplasia of lymphatic follicles or by luminal obstruction by a FECALITH.
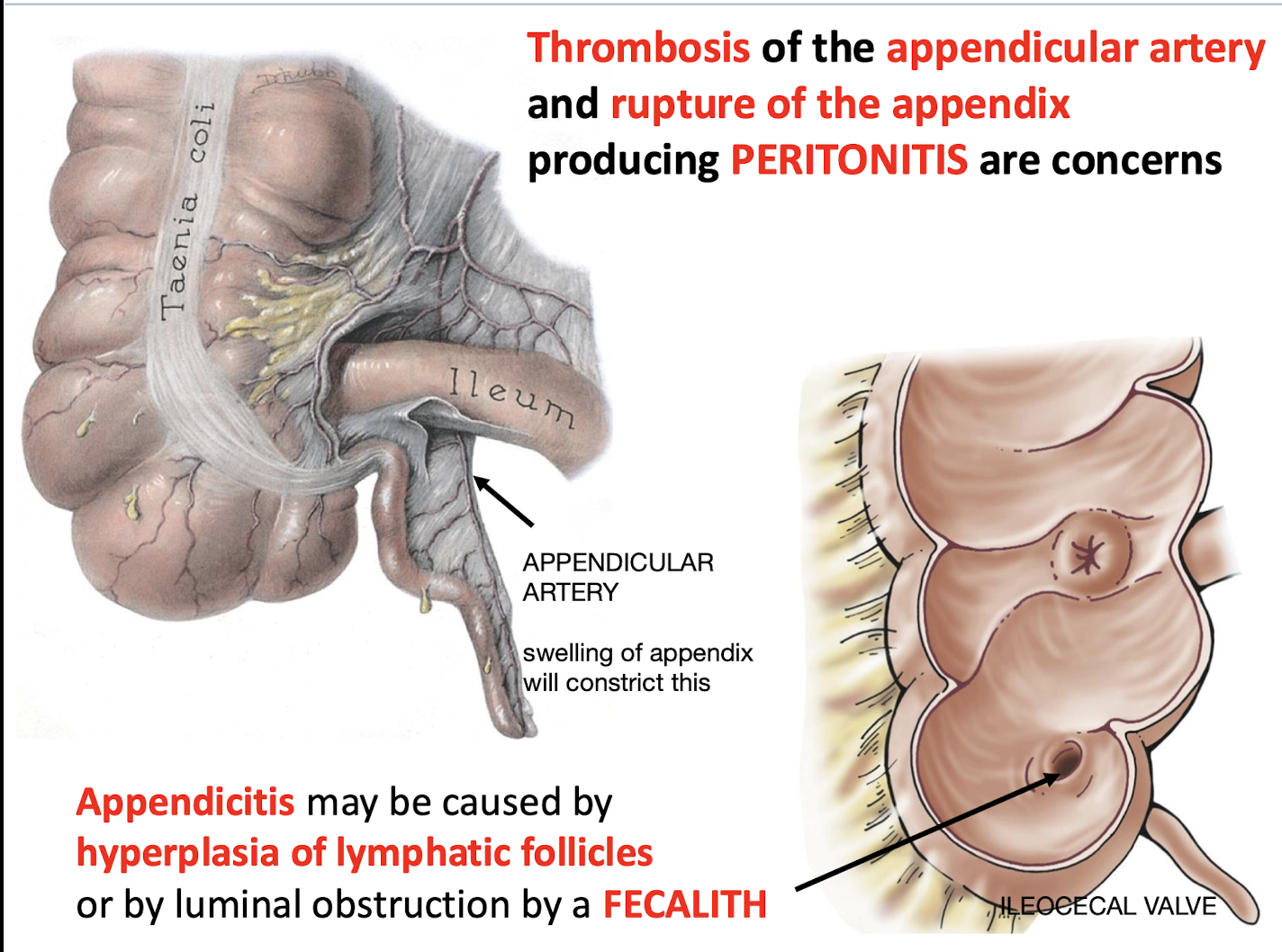
What are serious concerns associated with appendicitis progression
Thrombosis of the appendicular artery and rupture of the appendix producing PERITONITIS.
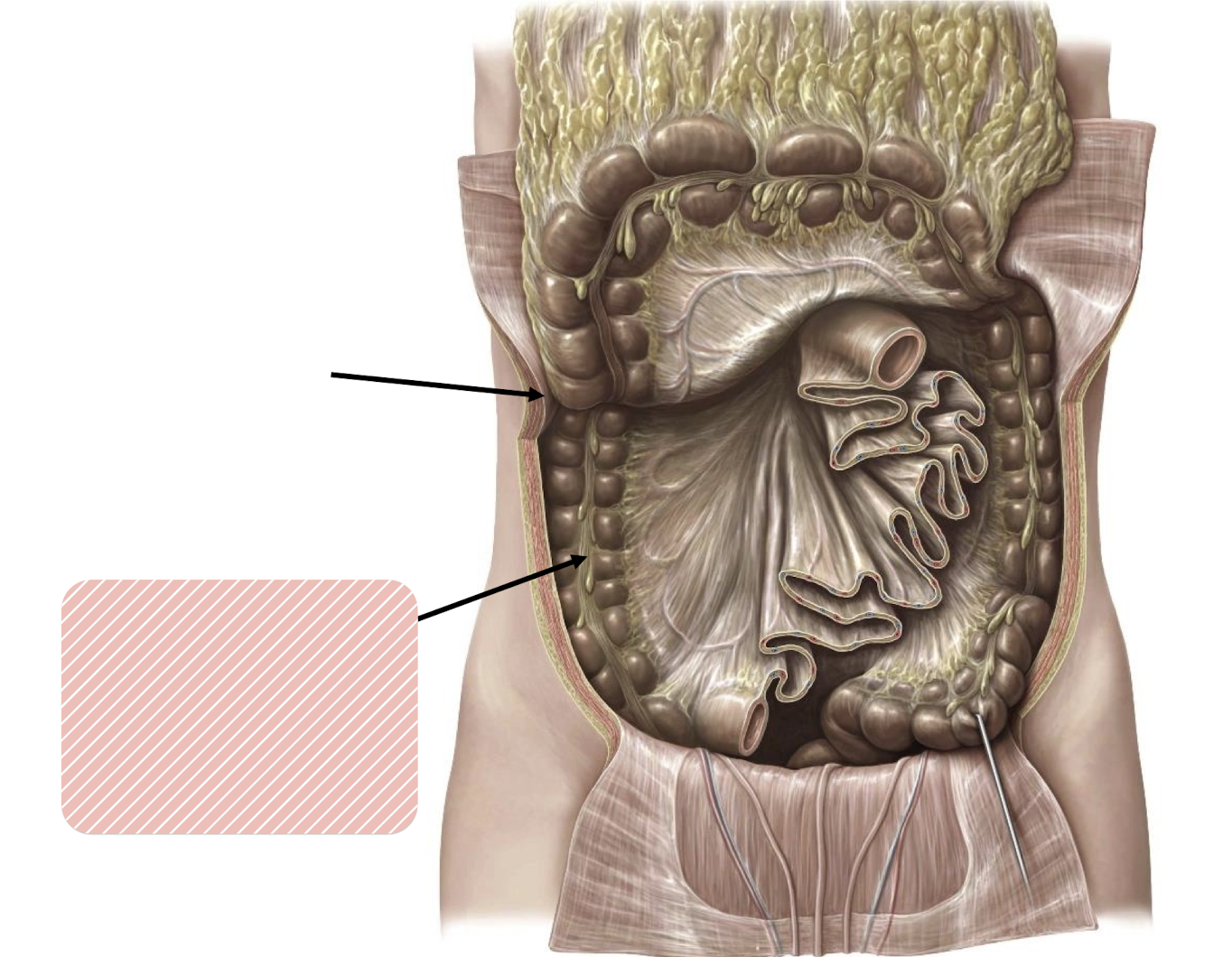
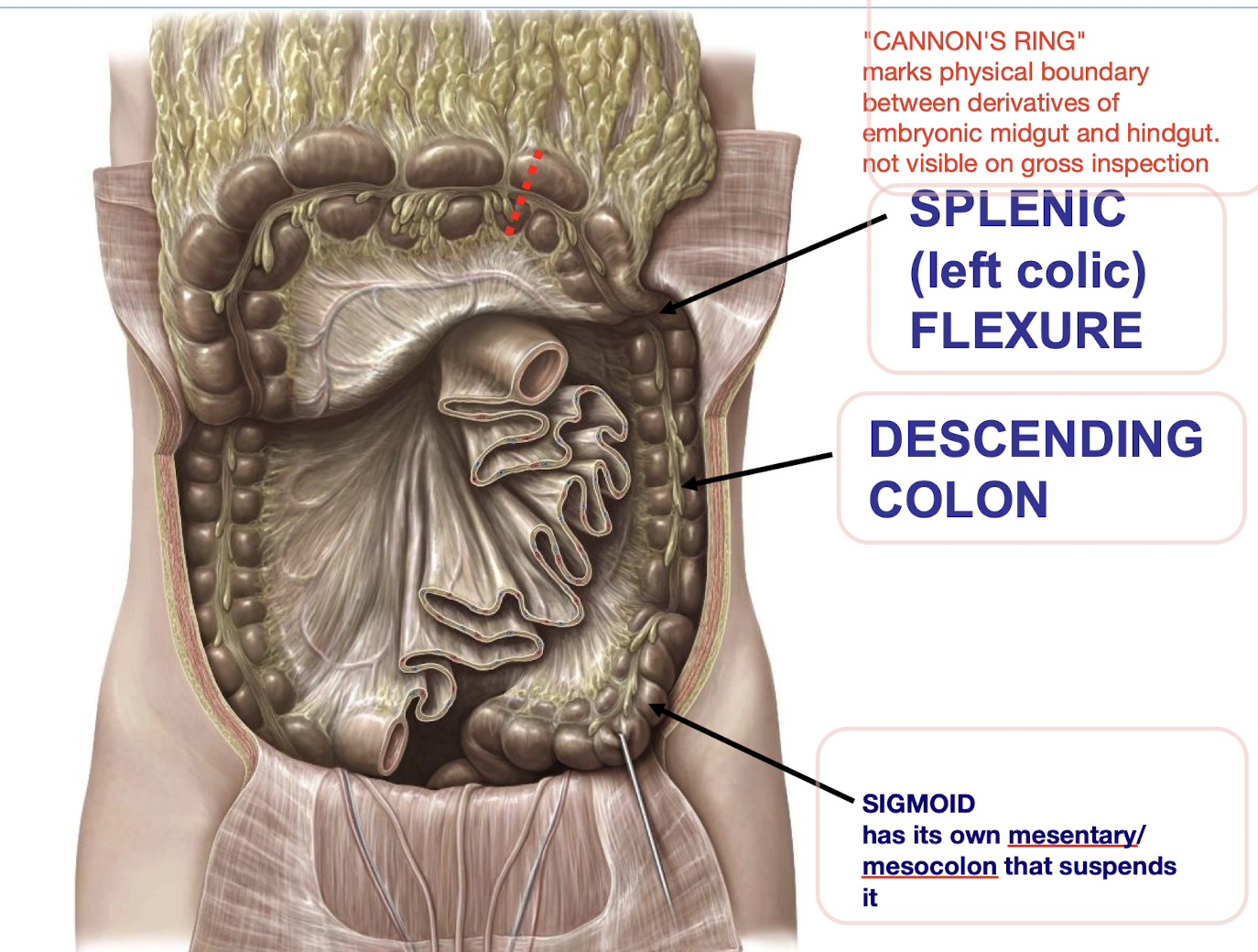
Identify the two structures
Identify the unlabeled branches of the SUPERIOR MESENTERIC ARTERY
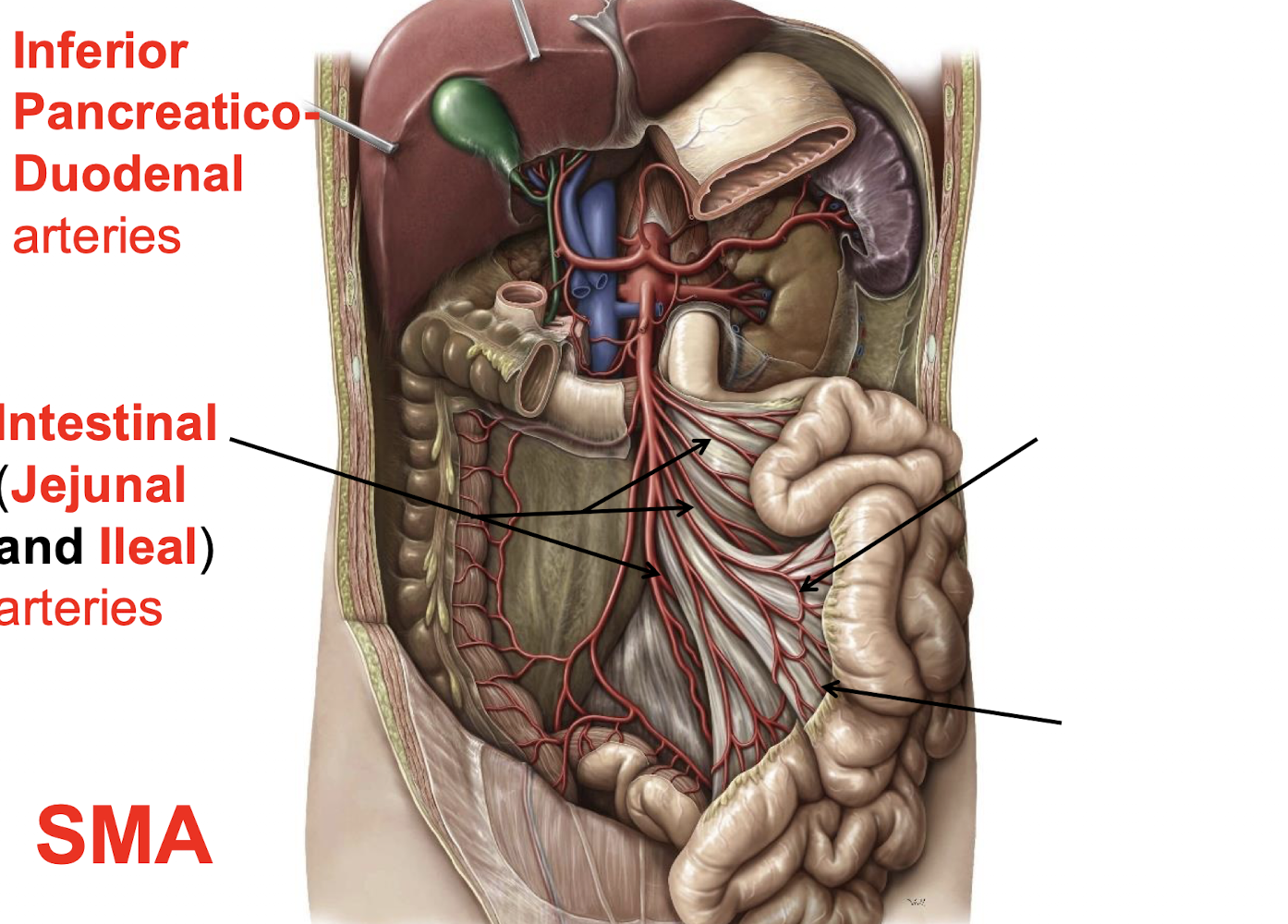
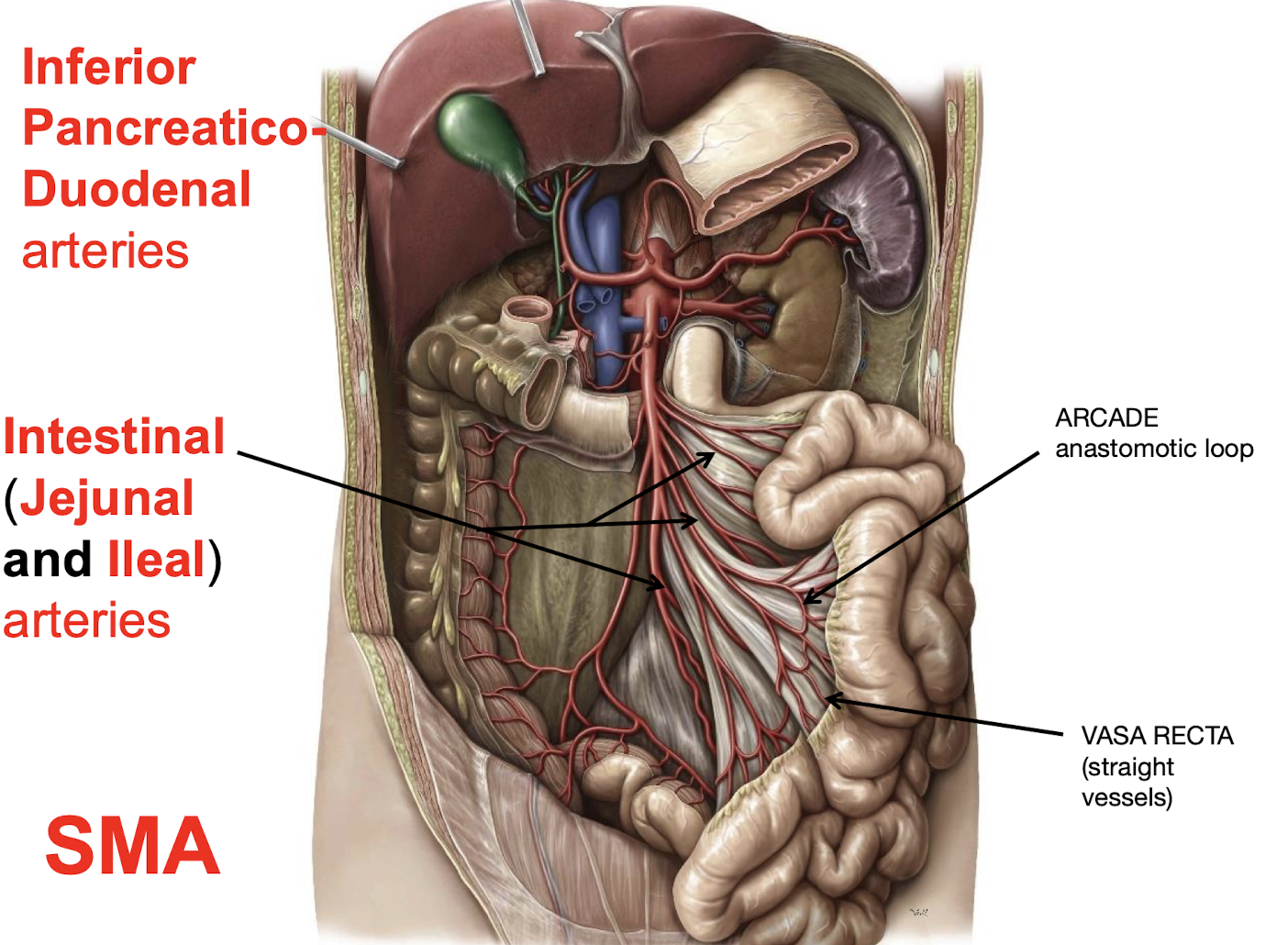
What is the function of the vasa recta derived from the SMA branches
They generally supply alternating sides of the intestine.
What are the derivatives of the embryonic hindgut
Distal 1/3 transverse colon; descending colon; sigmoid; rectum.
What provides the blood supply to the hindgut derivatives
The inferior mesenteric artery (IMA) and its branches.
From where do hindgut derivatives receive preganglionic sympathetic innervation
Lumbar splanchnic nerves.
From where do hindgut derivatives receive preganglionic parasympathetic innervation
The pelvic splanchnics (S2-S4).
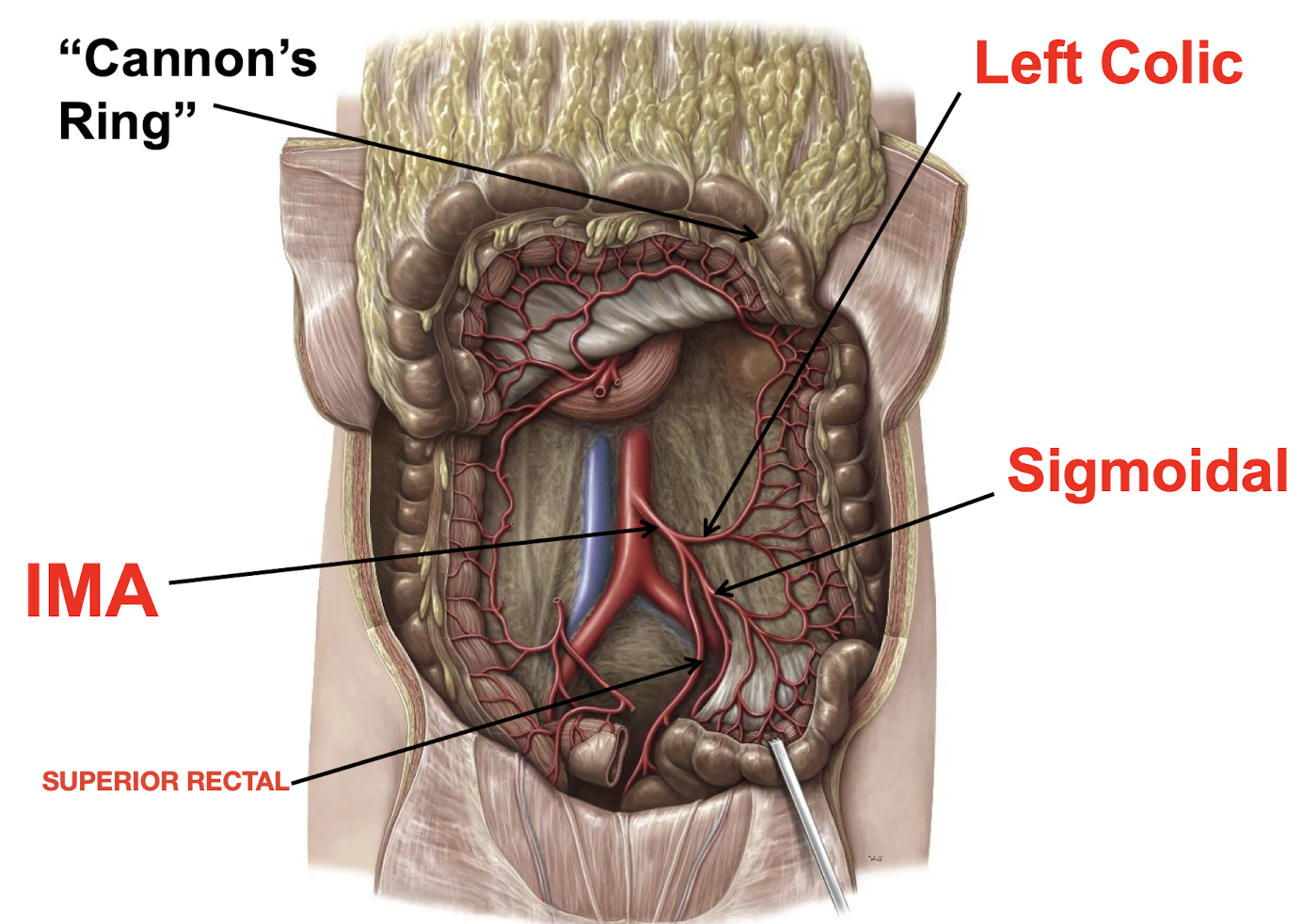
What artery is that and what vertebral level is it at?
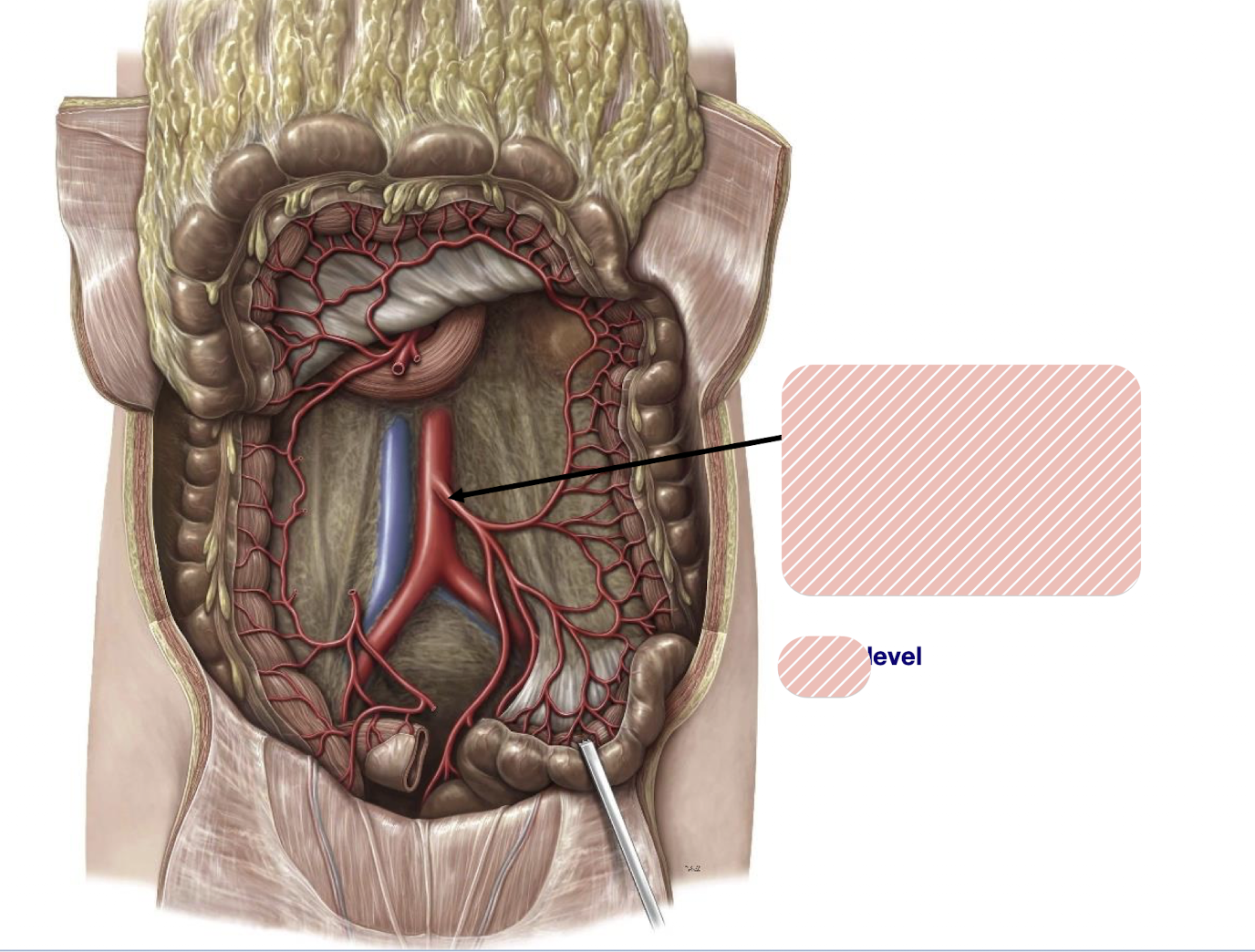
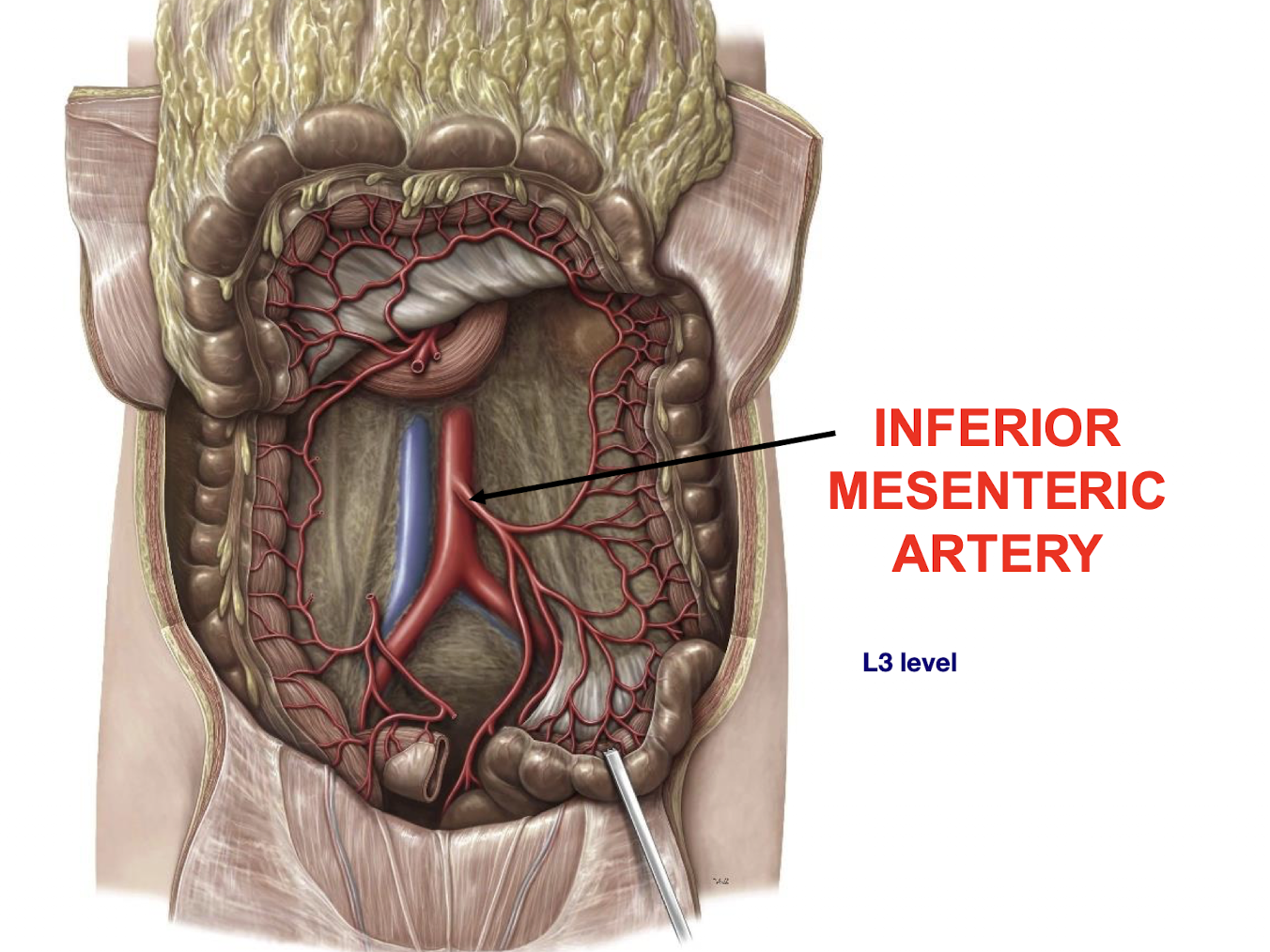
What are key branches of the INFERIOR MESENTERIC ARTERY (IMA) mentioned
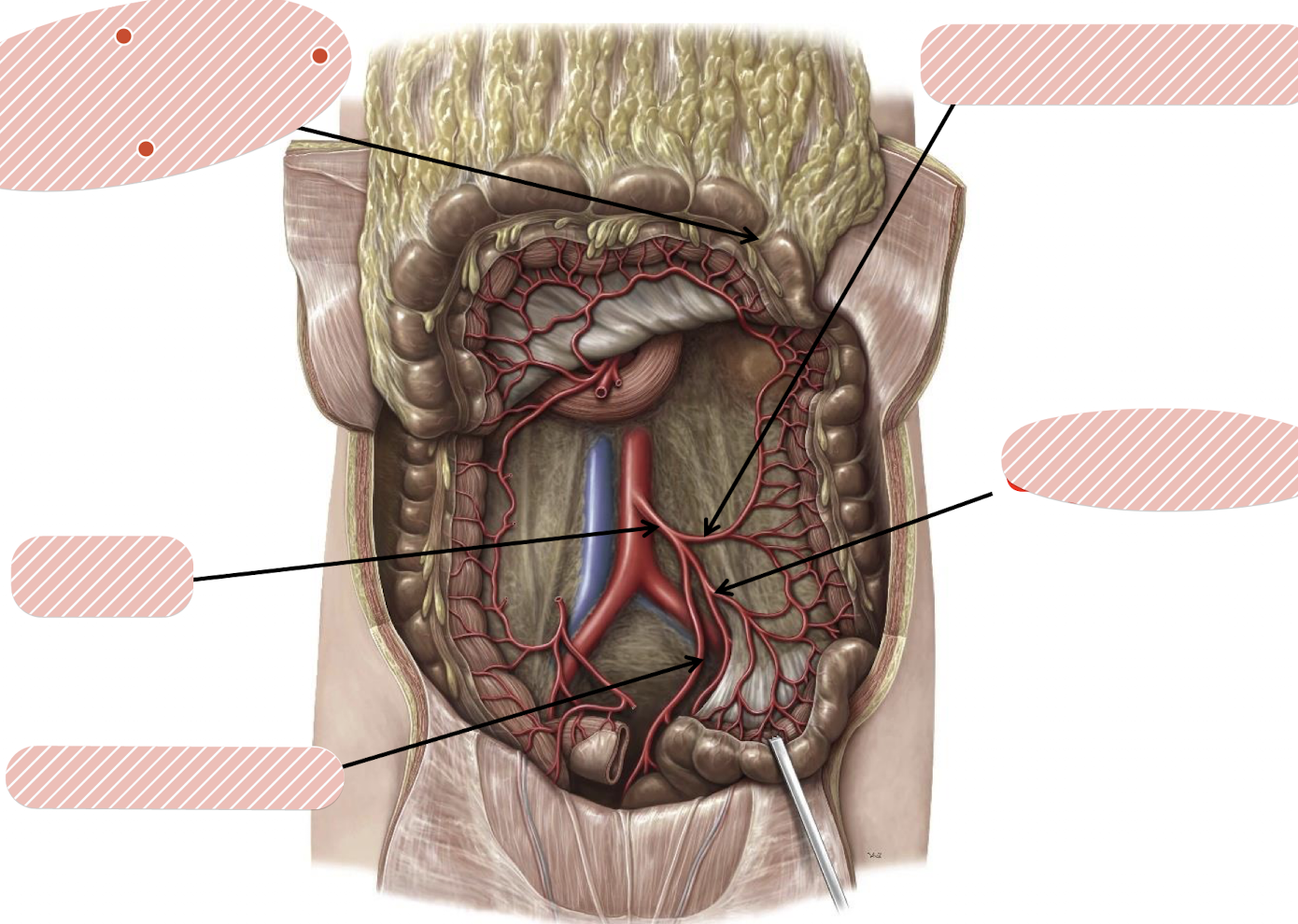
Left Colic; Sigmoidal, SUPERIOR RECTAL
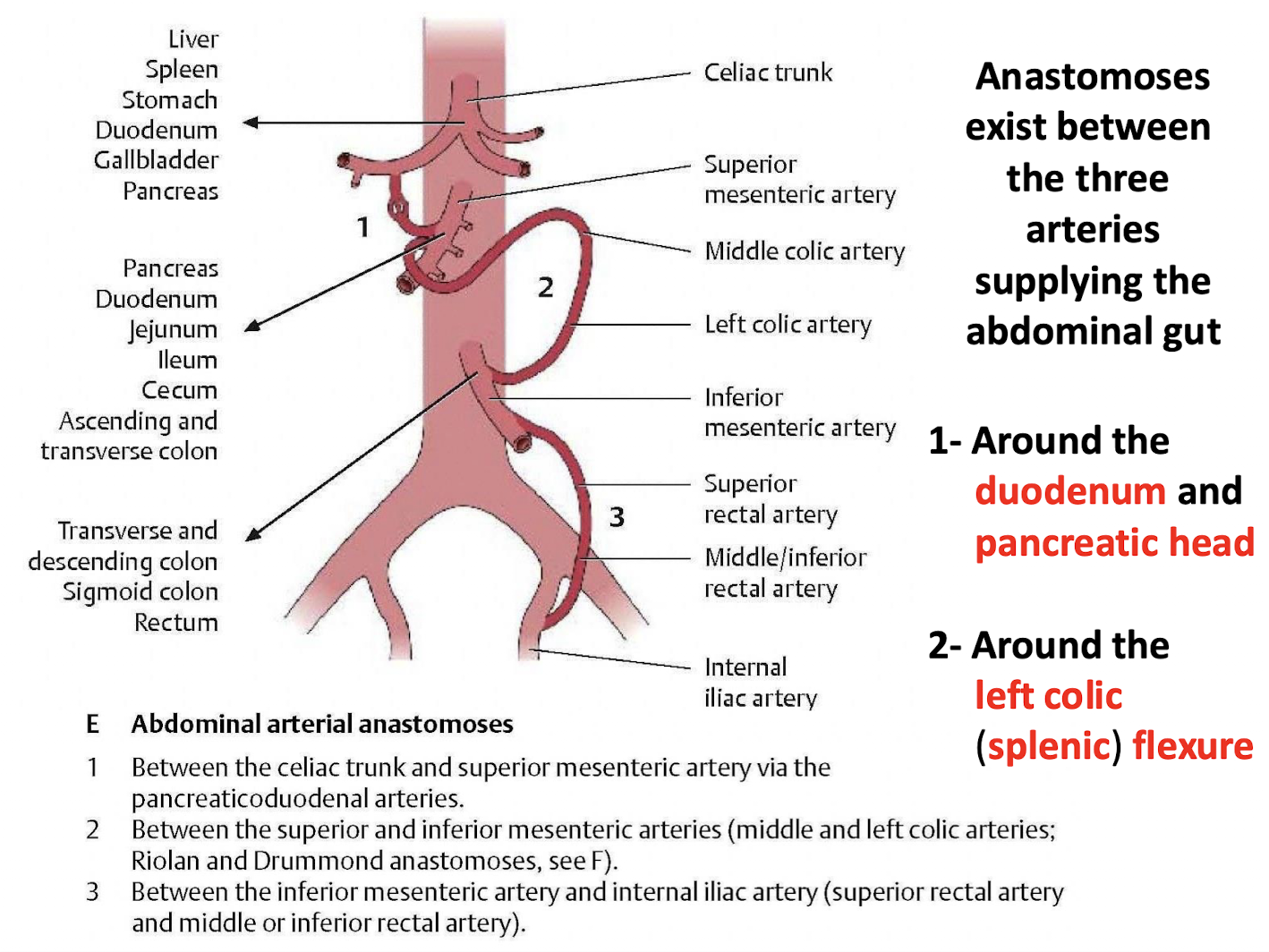
What important vascular phenomenon exists regarding the abdominal gut blood supply
Anastomoses exist between the three arteries supplying the abdominal gut (celiac trunk, superior and inferior mesenteric).
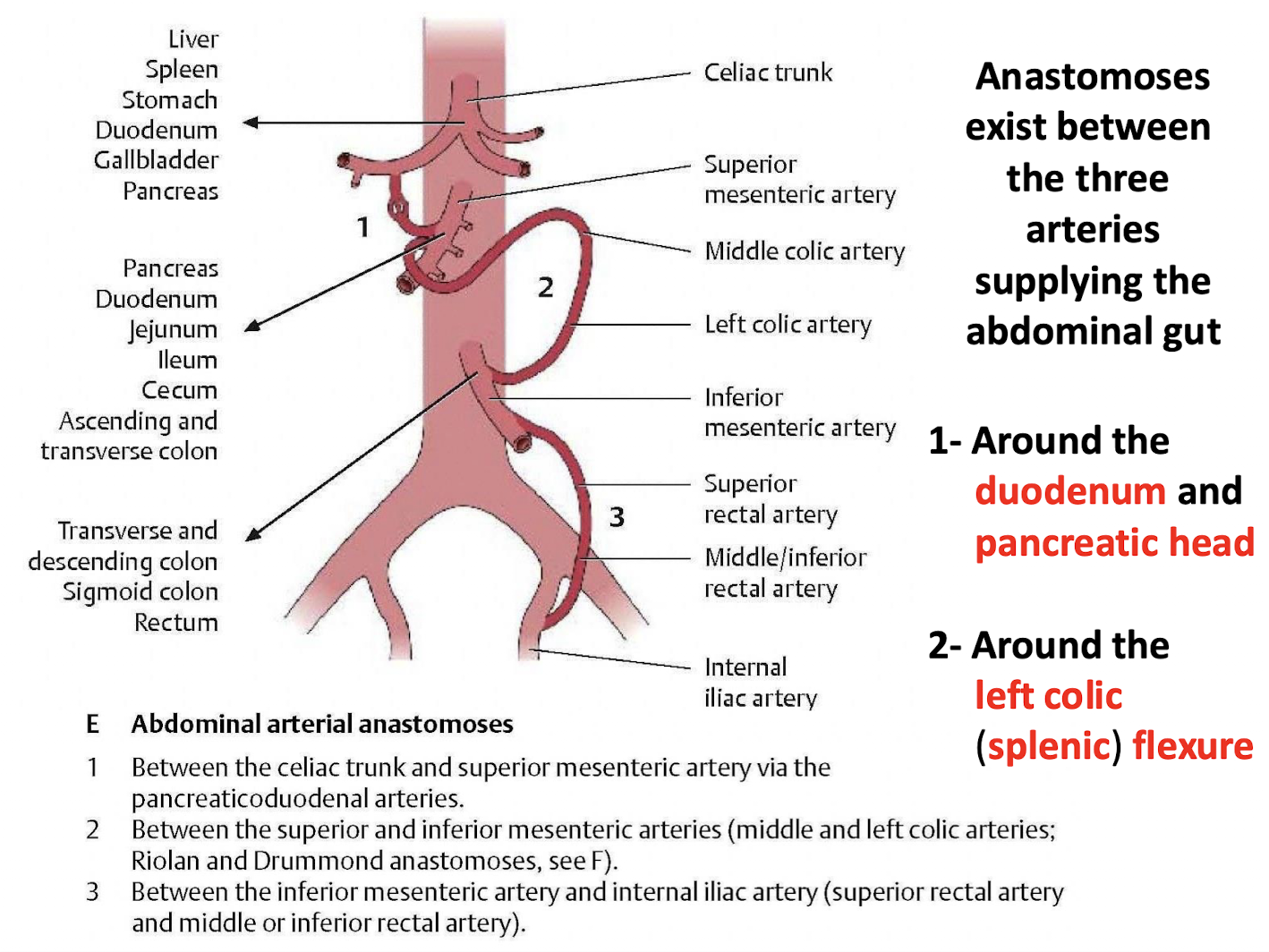
What two specific regions are noted for significant vascular anastomoses in the GI tract
1- Around the duodenum and pancreatic head; 2- Around the left colic (splenic) flexure.
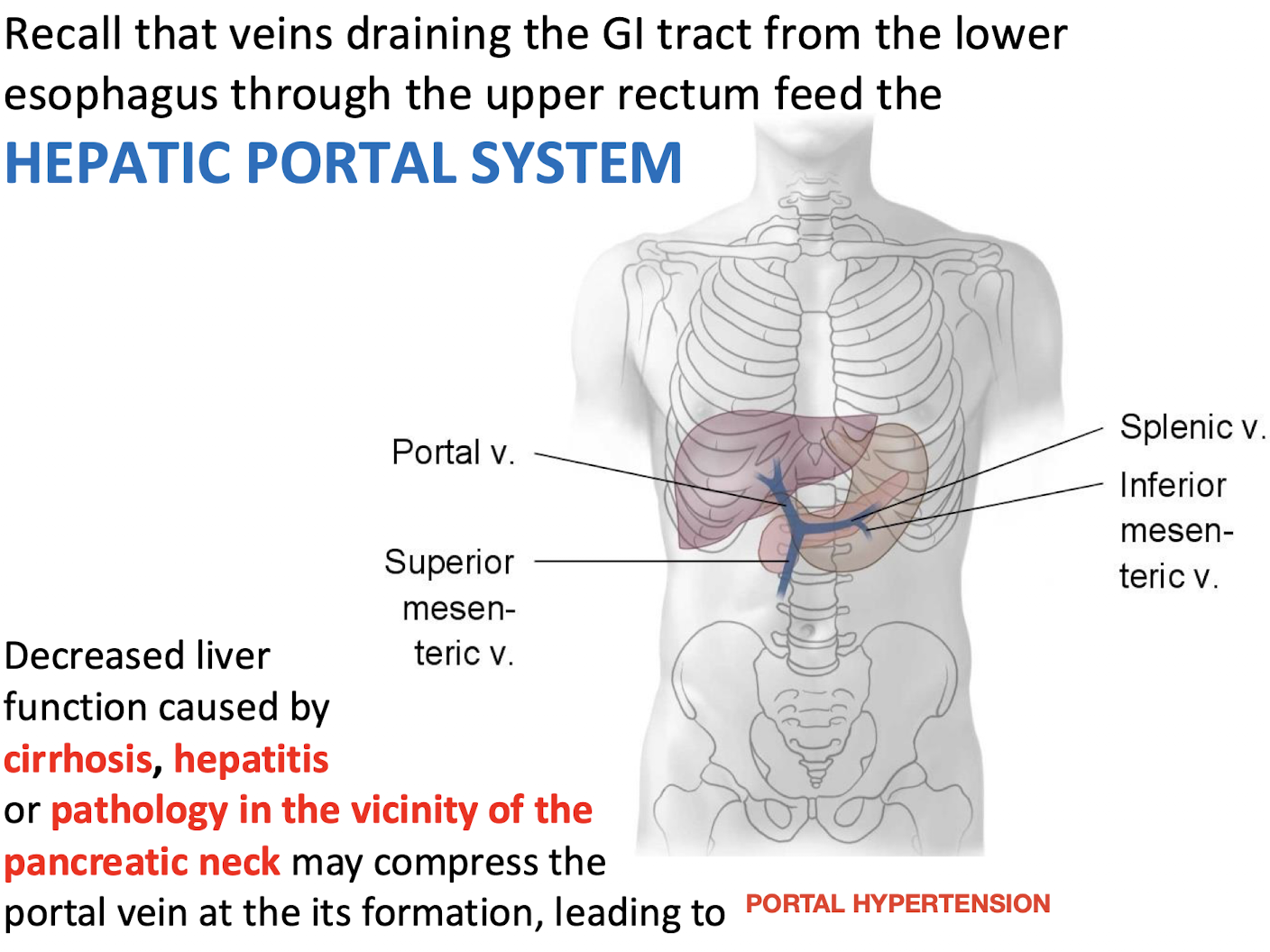
Which venous system is fed by veins draining the GI tract from the lower esophagus through the upper rectum
The HEPATIC PORTAL SYSTEM.
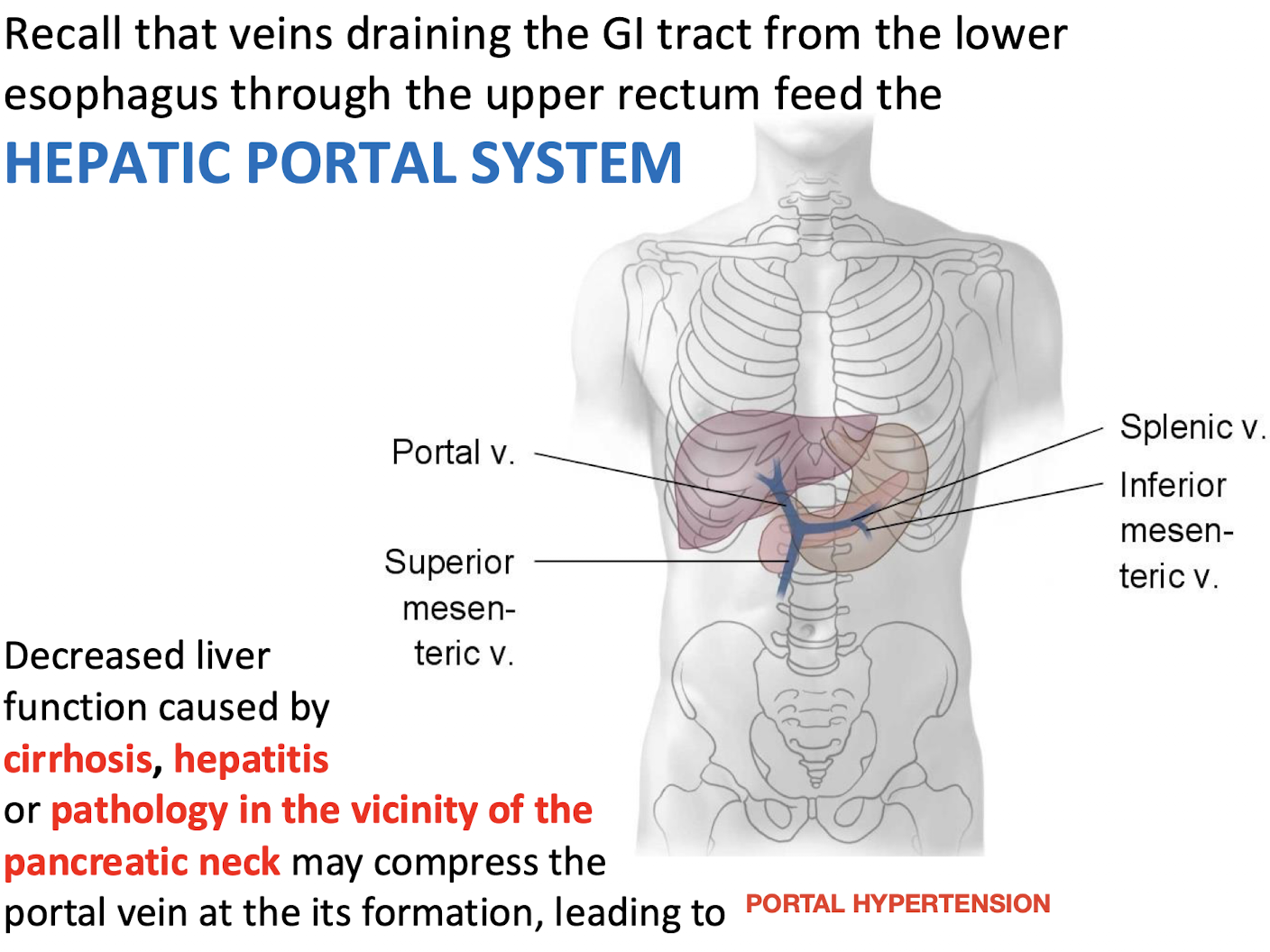
What condition can result from decreased liver function or compression of the portal vein at its formation?
Portal Hypertension
Caused by decreased liver function (e.g., cirrhosis, hepatitis) or pathology near the pancreatic neck that compresses the portal vein at its formation.
Why do anastomoses exist between tributaries of the hepatic portal system and the caval system
Primarily having to do with the prenatal development of the GI tract.
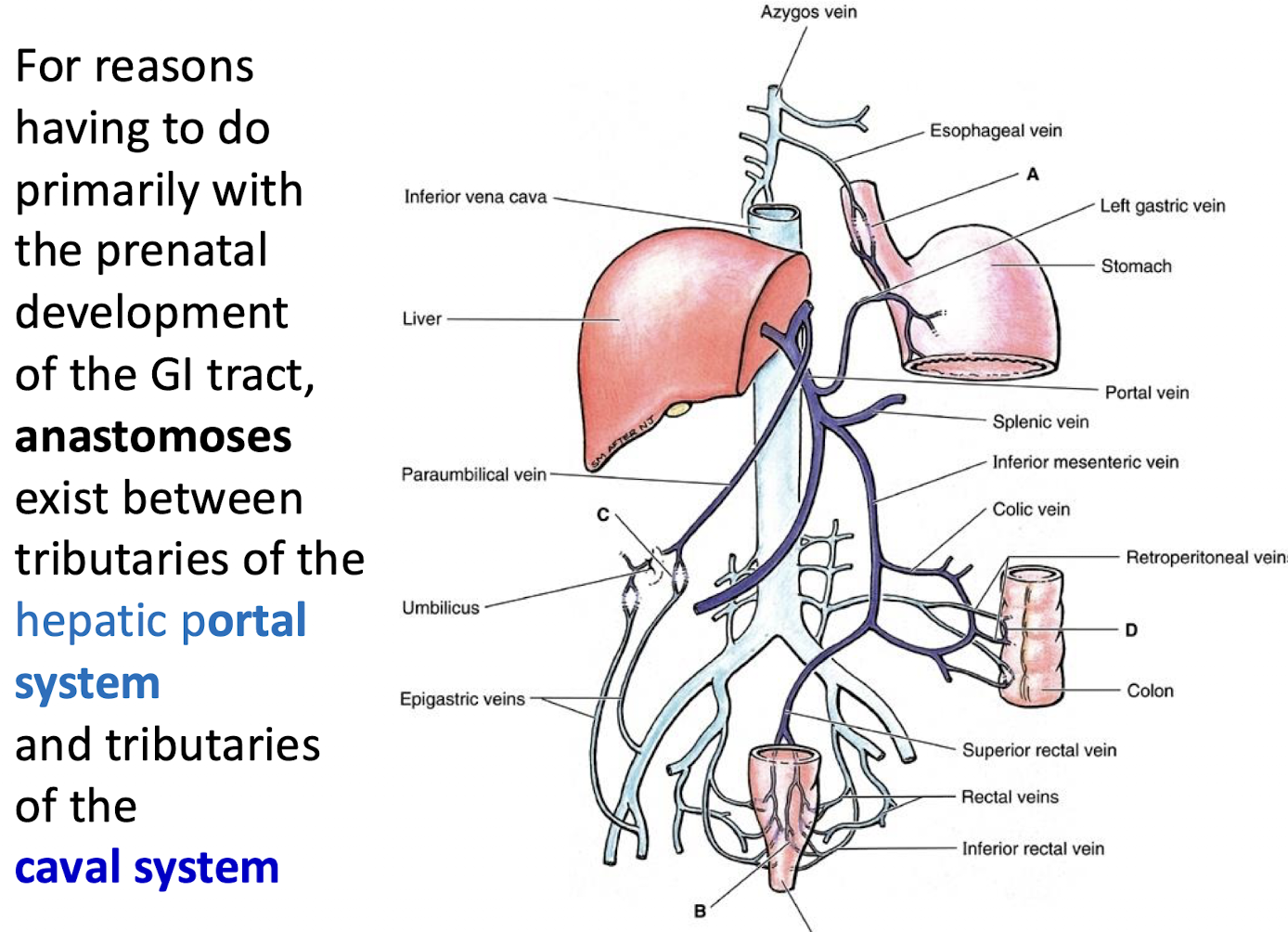
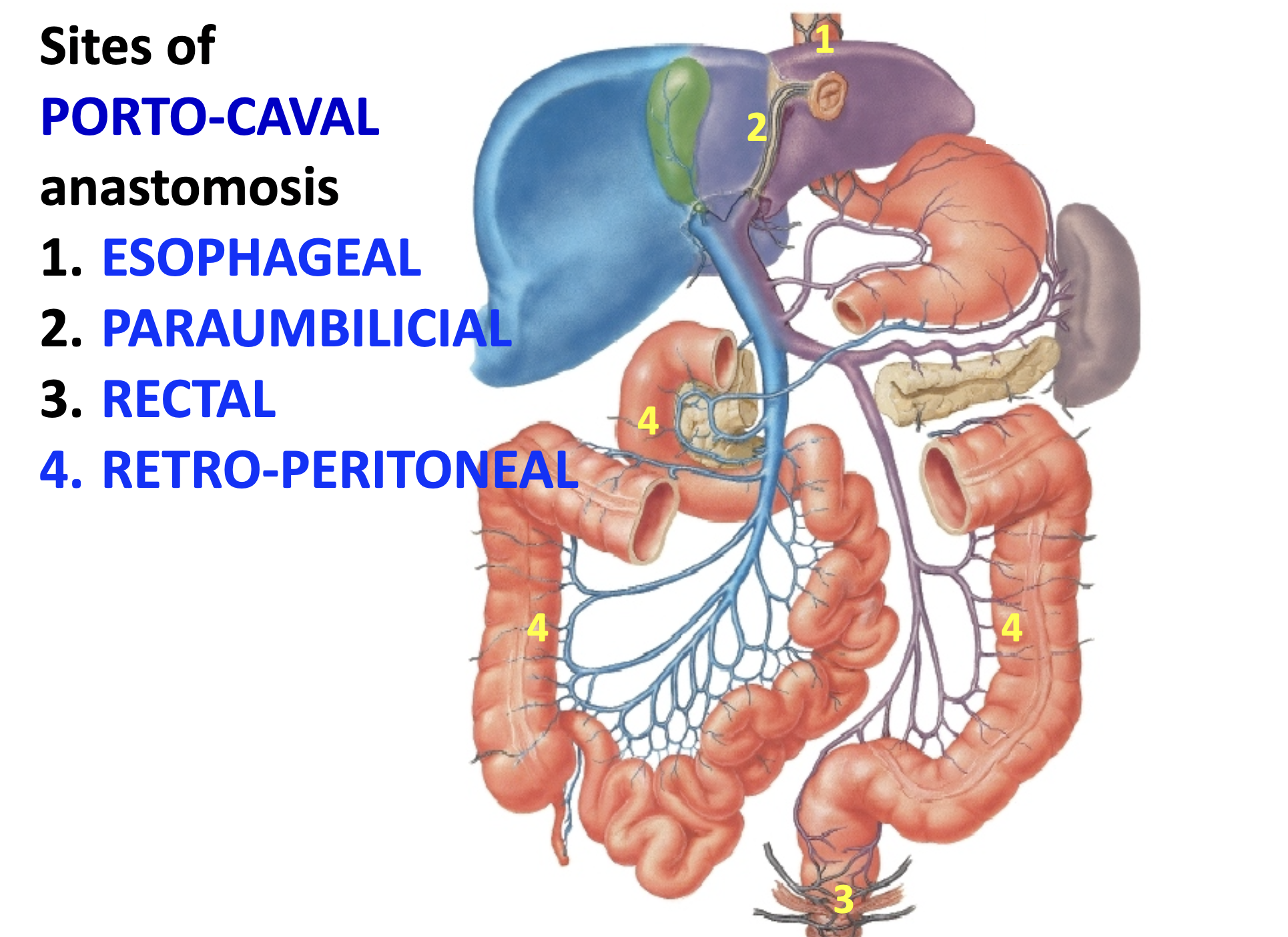
What are the four sies of porto-caval anastomosis
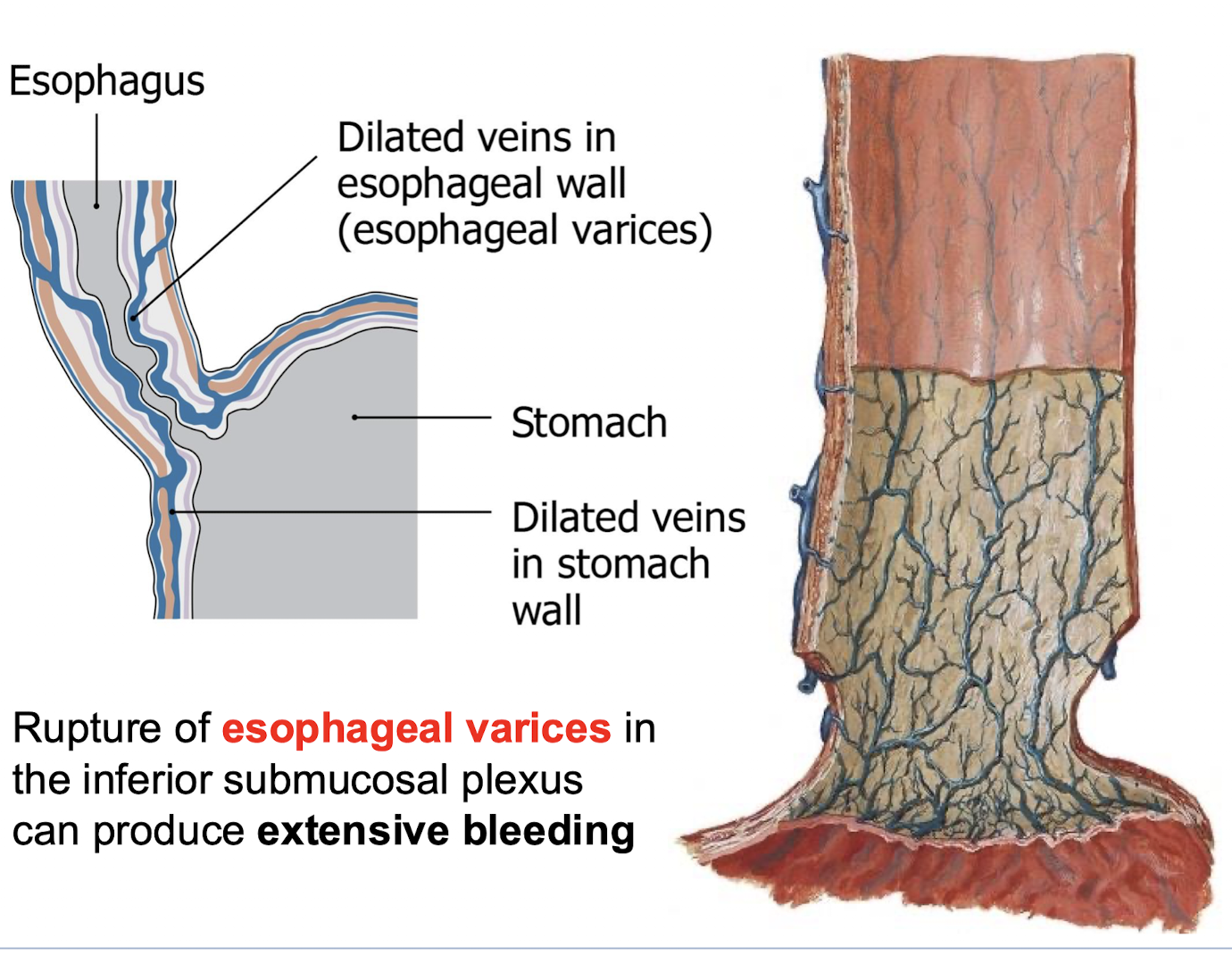
1. ESOPHAGEAL
2. PARAUMBILICAL
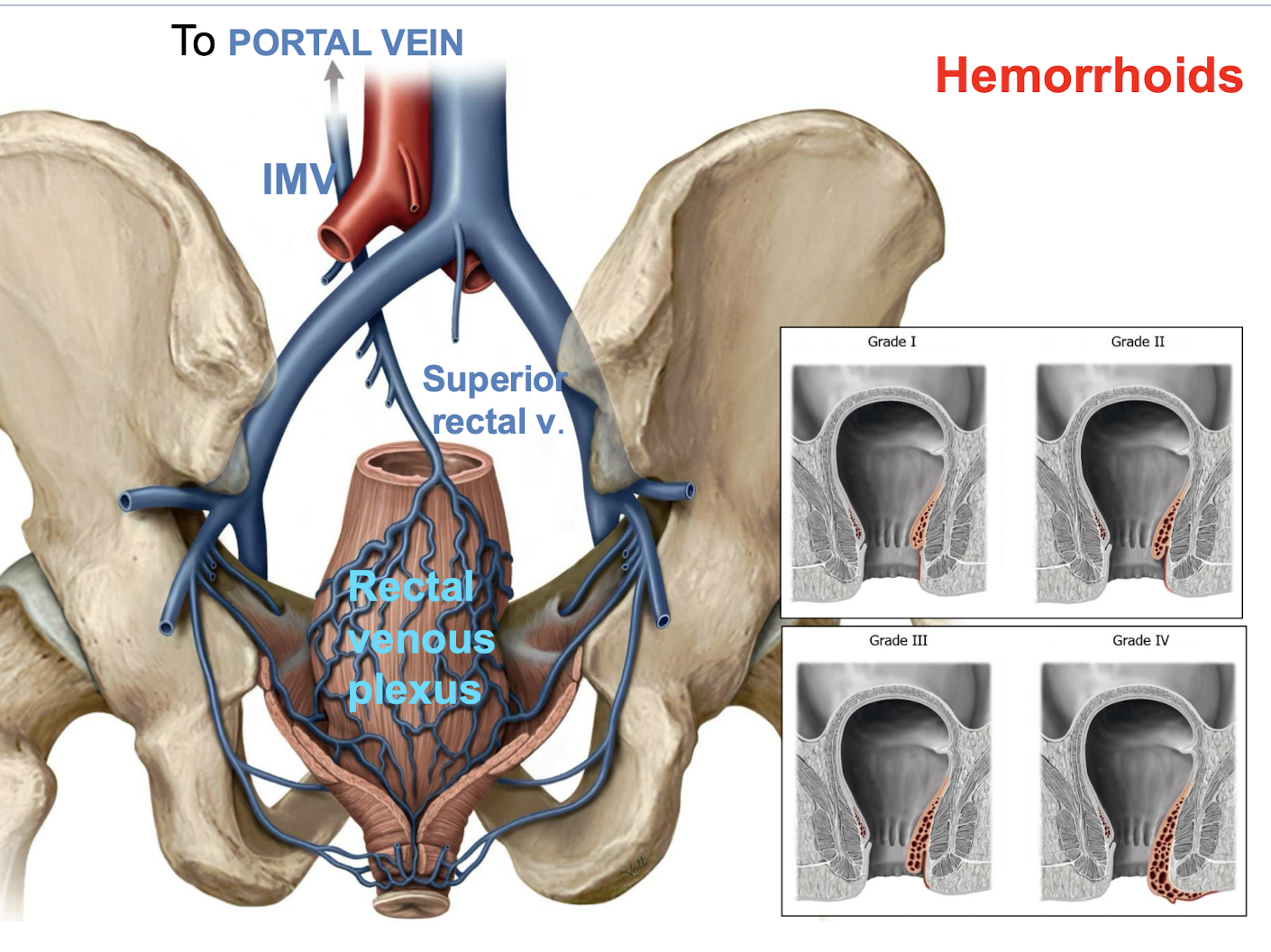
3. RECTAL
4. RETRO-PERITONEAL
What complications can arise from dilation of portosystemic anastomoses due to portal hypertension?
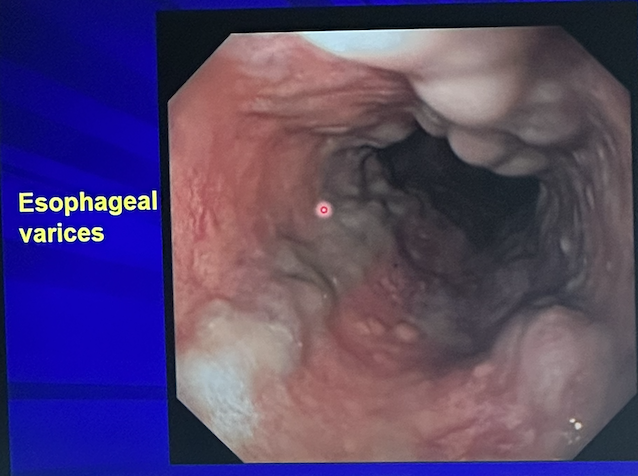
Esophageal Varices
Dilated veins in the esophagus, risk of rupture and bleeding.
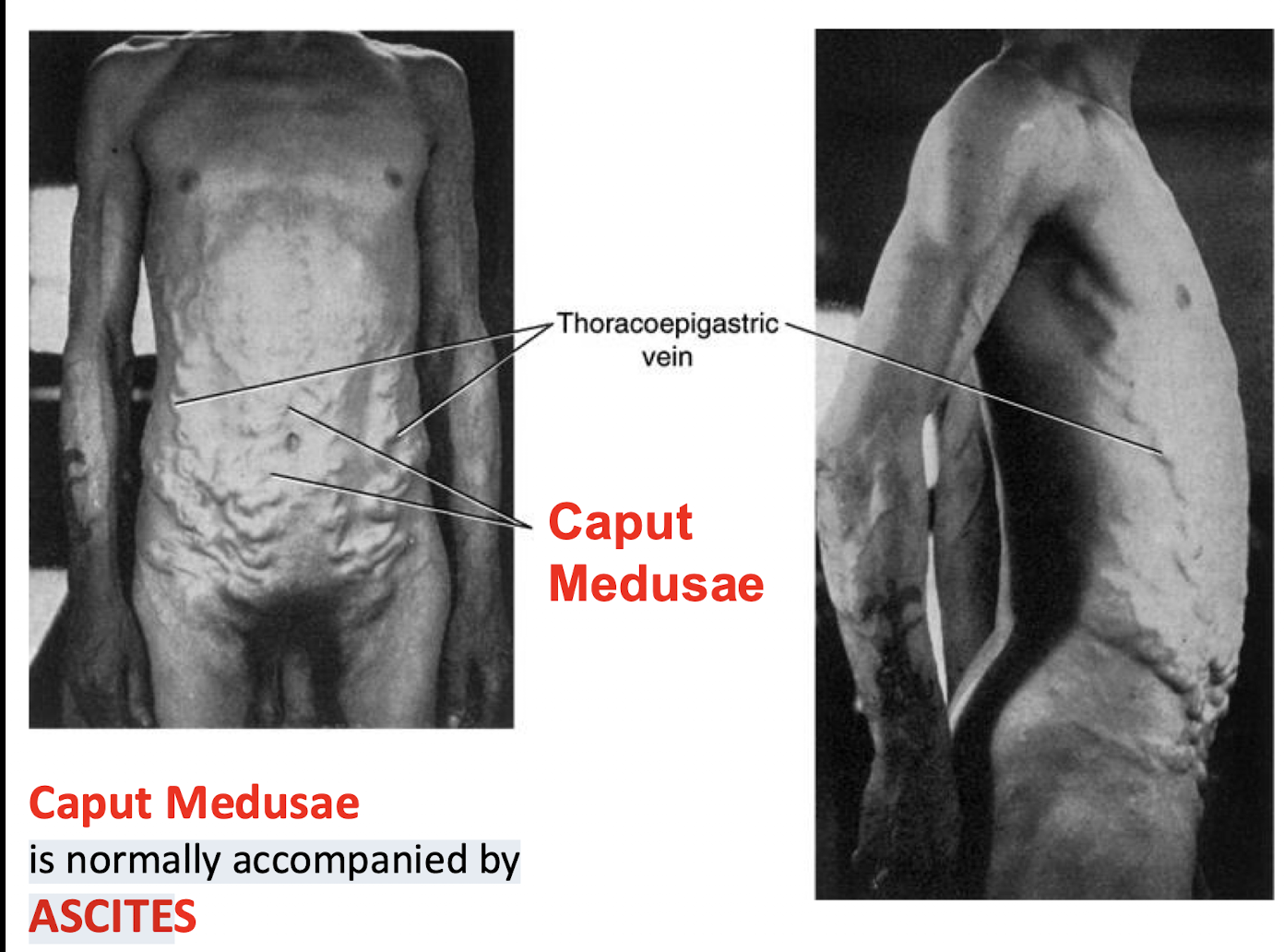
Caput Medusae
Dilated veins radiating from the umbilicus.Hemorrhoids
Dilated veins in the rectal region.
(Portal hypertension is often caused by cirrhosis, which involves destruction of hepatocytes.)
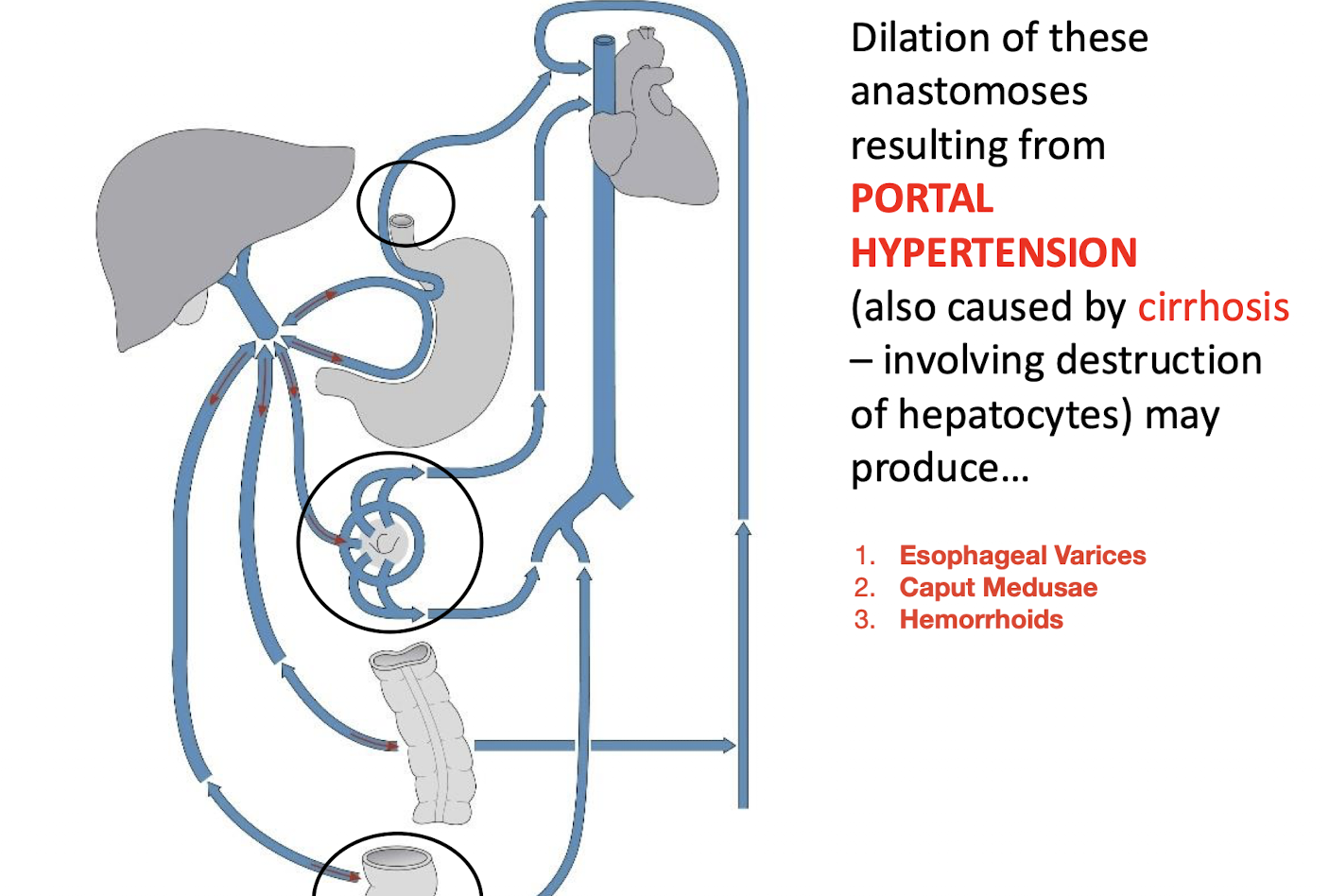
What clinical sign is associated with dilated periumbilical porto-caval anastomoses. What is it normally accompanied by?
Caput Medusae.
It is normally accompanied by ASCITES
What condition involves the rectal venous plexus due to porto-caval anastomosis
Hemorrhoids.
What severe complication can result from the rupture of esophageal varices in the inferior submucosal plexus
Extensive bleeding.
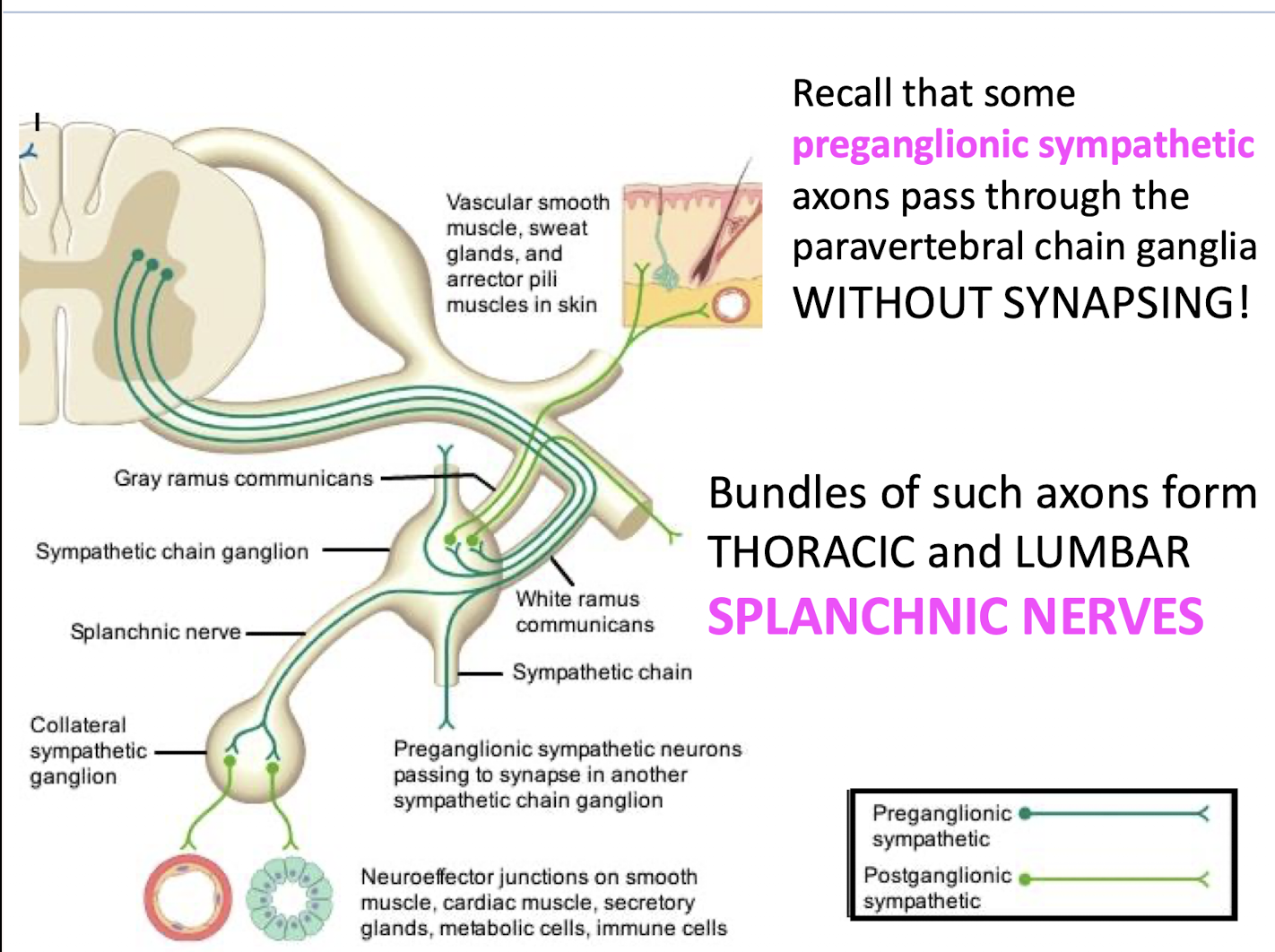
Complete Pathway of Preganglionic Sympathetic Fibers destined for abdominal viscera
Origin/Bypass, Nerve names, Synapse & Location
Origin/Bypass: Axons leave the spinal cord and pass through the Paravertebral Chain Ganglia (Sympathetic Trunk) WITHOUT SYNAPSING.
Nerve Name: Bundles of these axons form the Thoracic and Lumbar Splanchnic Nerves.
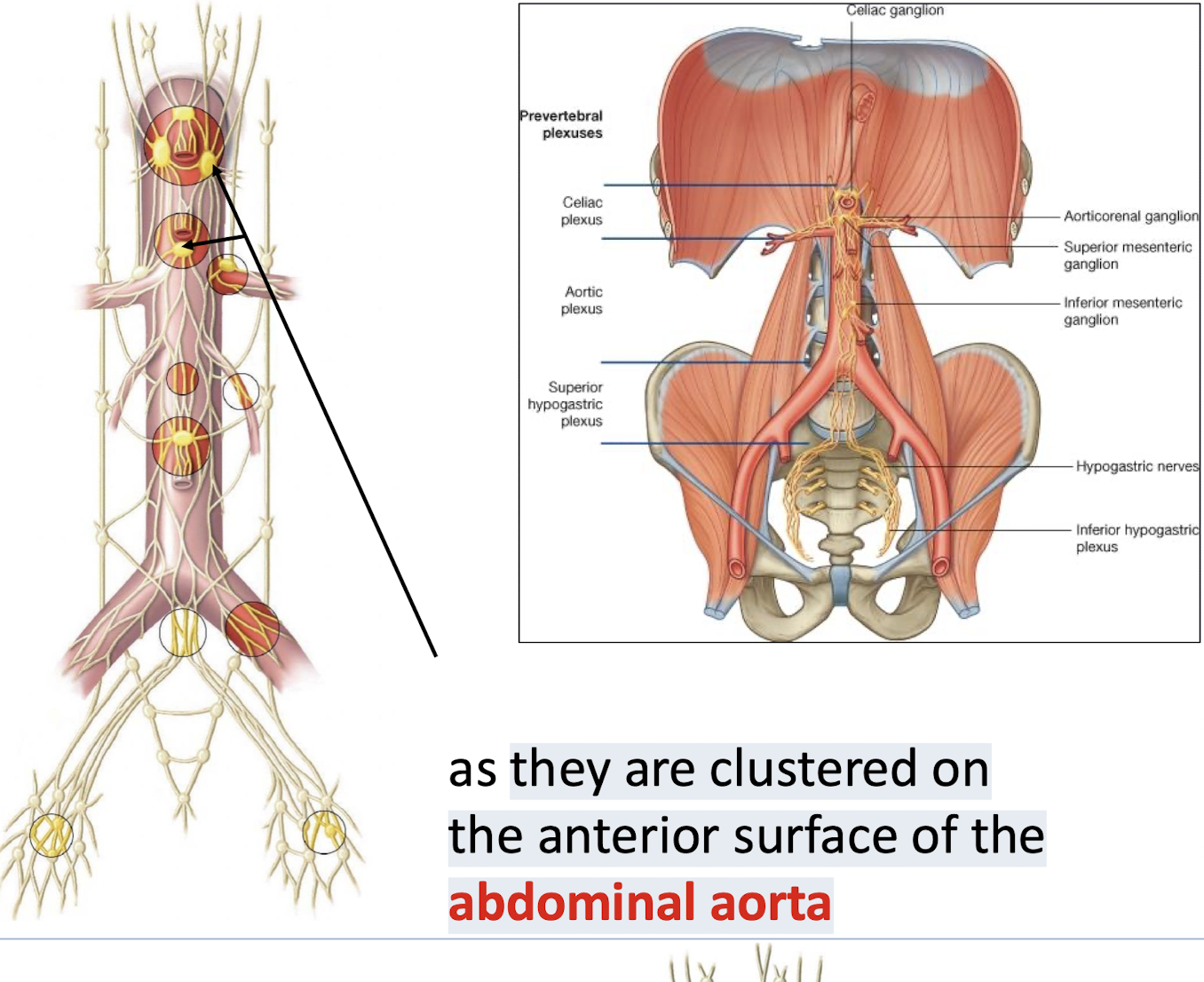
Synapse: The fibers synapse in Collateral (Prevertebral) Ganglia (e.g., Celiac, Superior/Inferior Mesenteric Ganglia) located anterior to the spine.
Location: These nerves travel to ganglia clustered on the anterior surface of the abdominal aorta (Prevertebral location).
What type of fibers do the autonomic plexuses associated with sympathetic ganglia also contain
Preganglionic parasympathetic fibers.
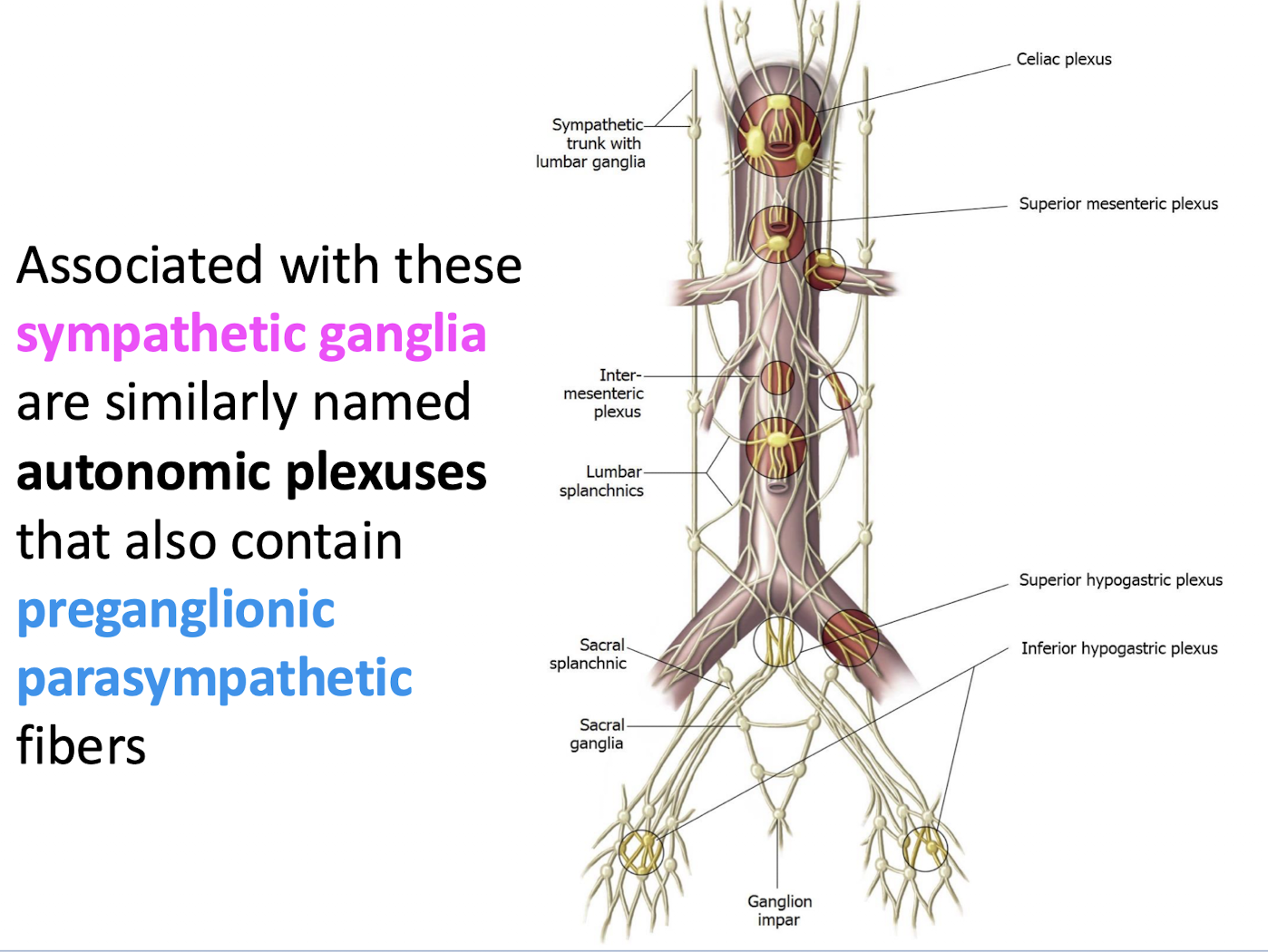
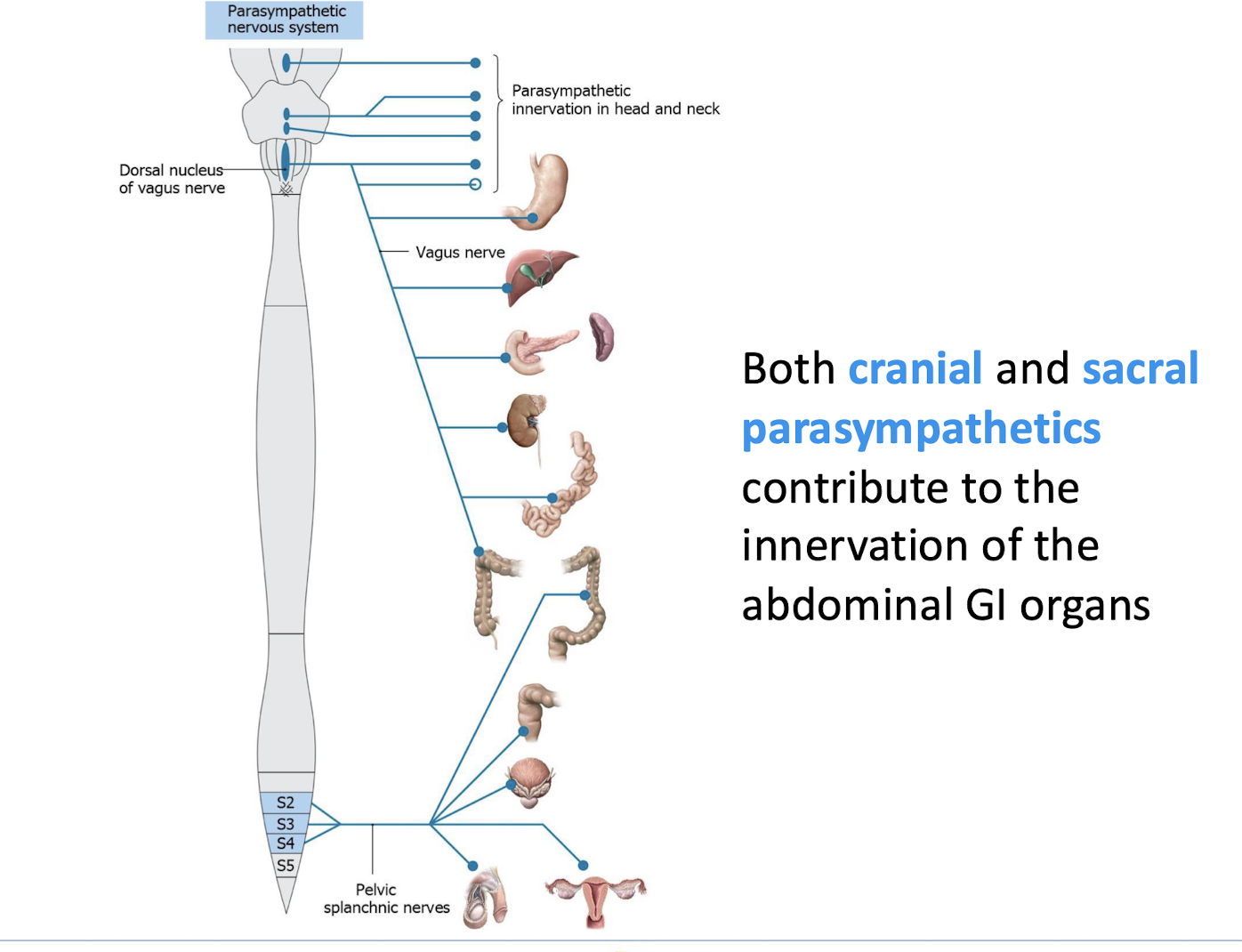
What two sources contribute parasympathetic innervation to the abdominal GI organs
Both cranial and sacral parasympathetics.
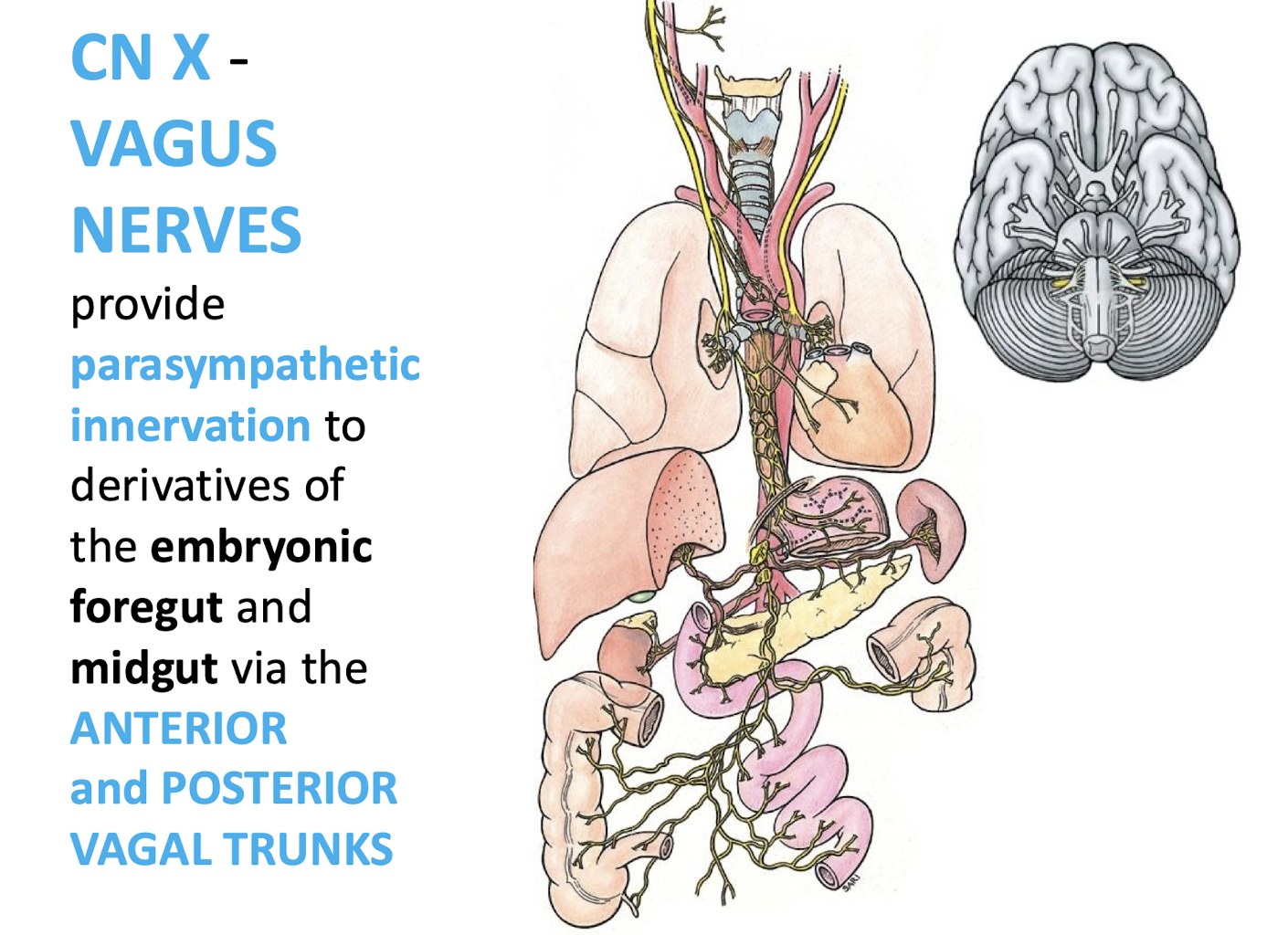
What cranial nerve provides parasympathetic innervation to the embryonic foregut and midgut derivatives
CN X - VAGUS NERVES.
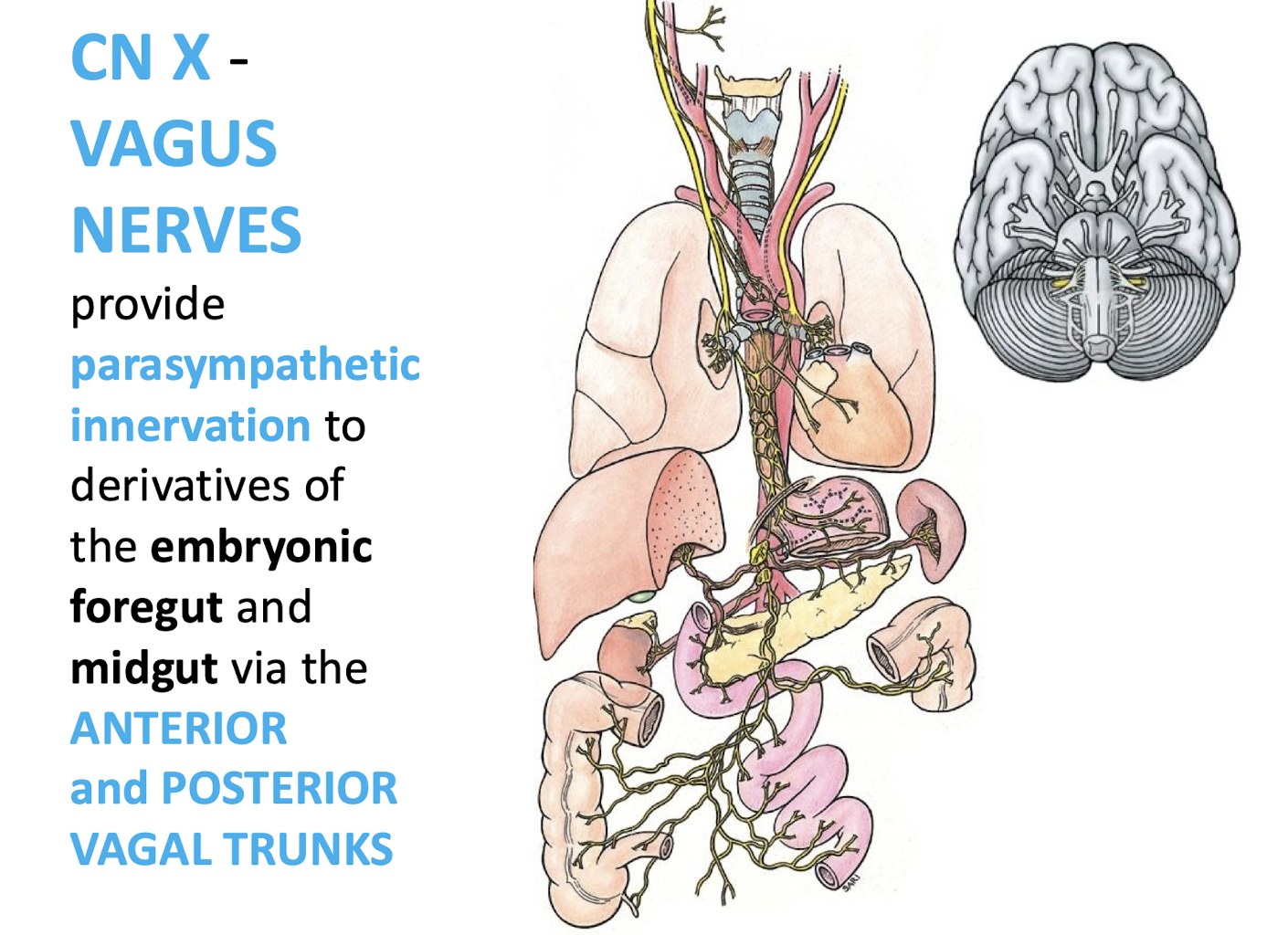
What structures transmit the vagal innervation to the foregut and midgut targets
The ANTERIOR and POSTERIOR VAGAL TRUNKS.
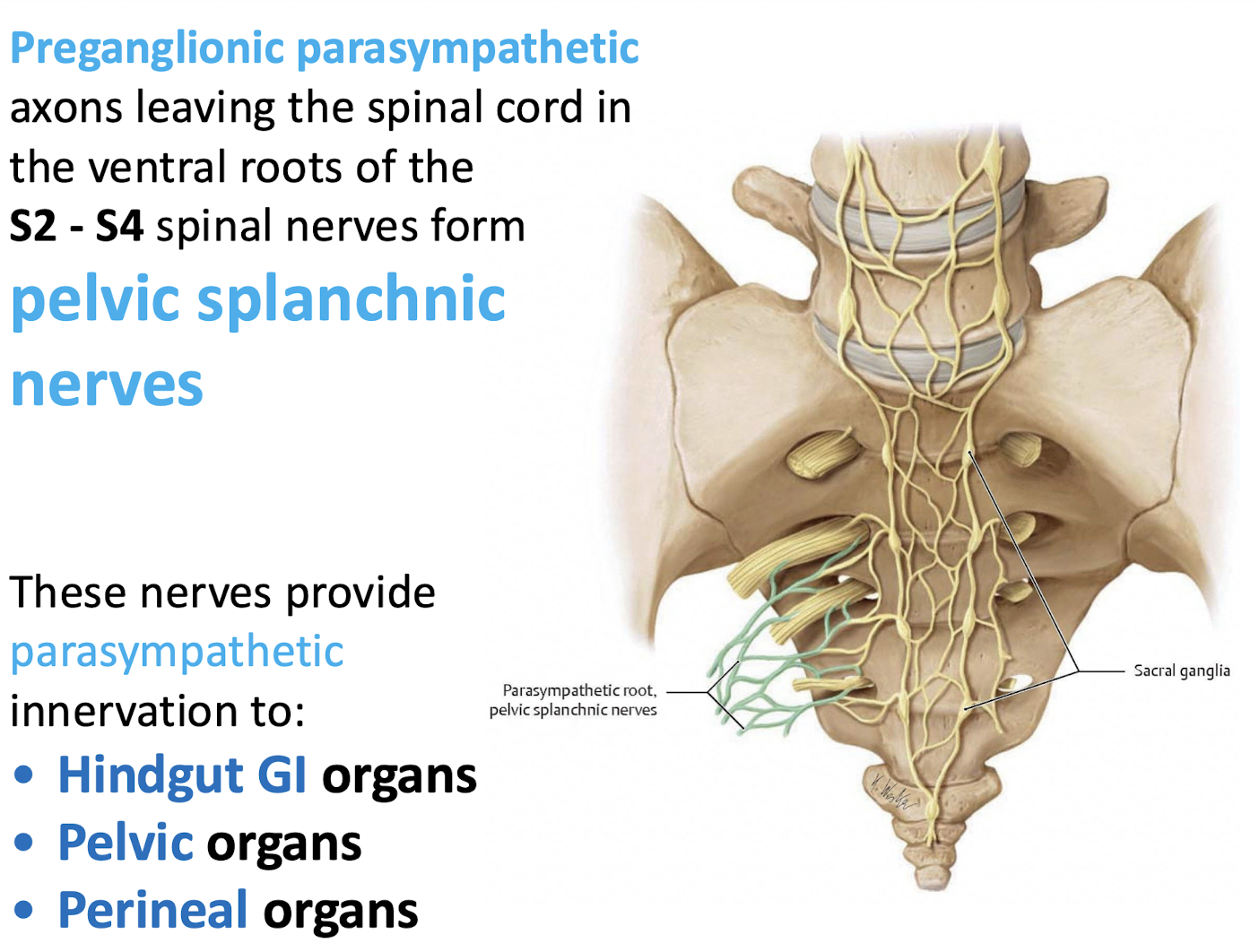
What forms the pelvic splanchnic nerves
Preganglionic parasympathetic axons leaving the spinal cord in the ventral roots of the S2 - S4 spinal nerves.
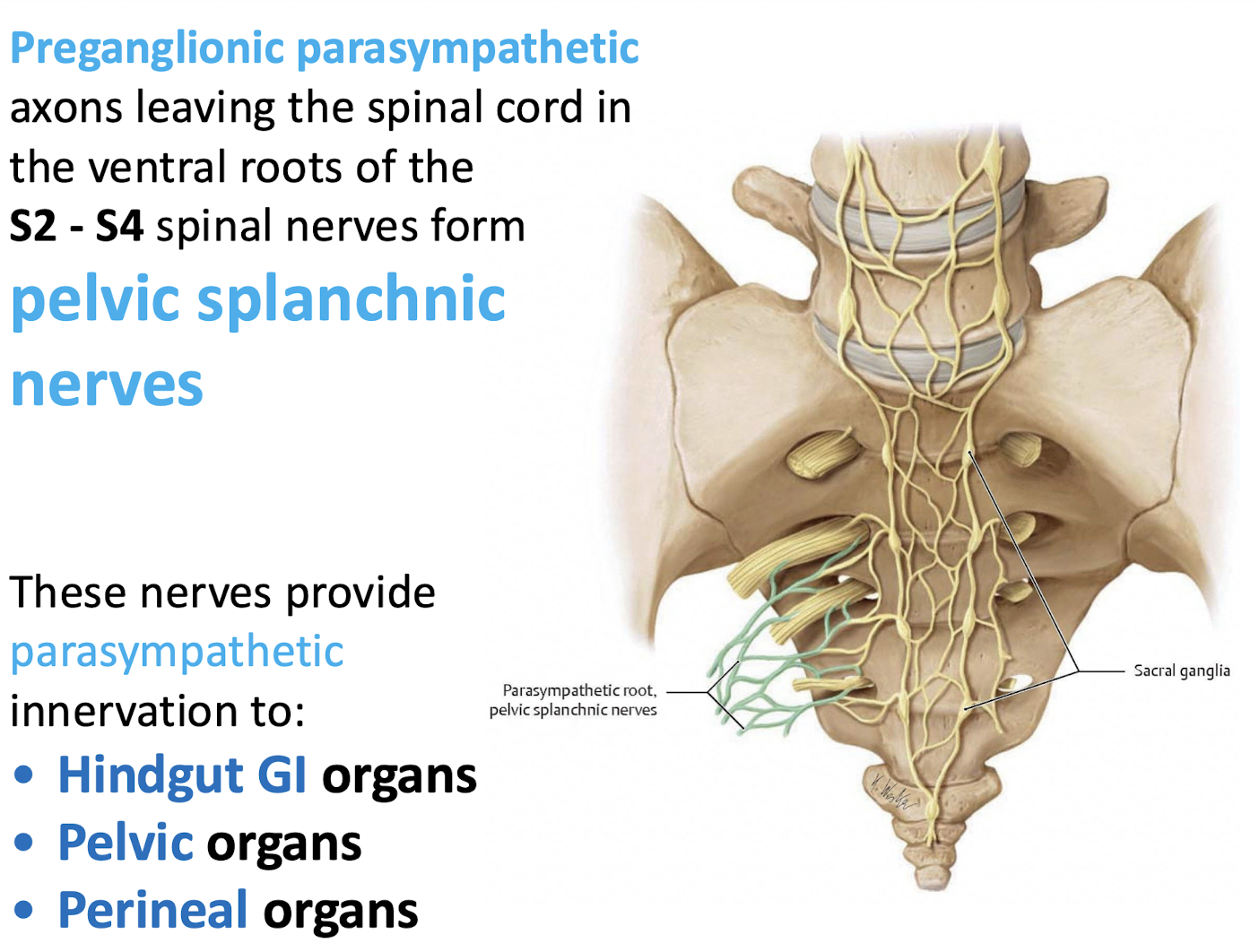
What organs do the pelvic splanchnic nerves innervate
Hindgut GI organs, Pelvic organs, and perineal organs
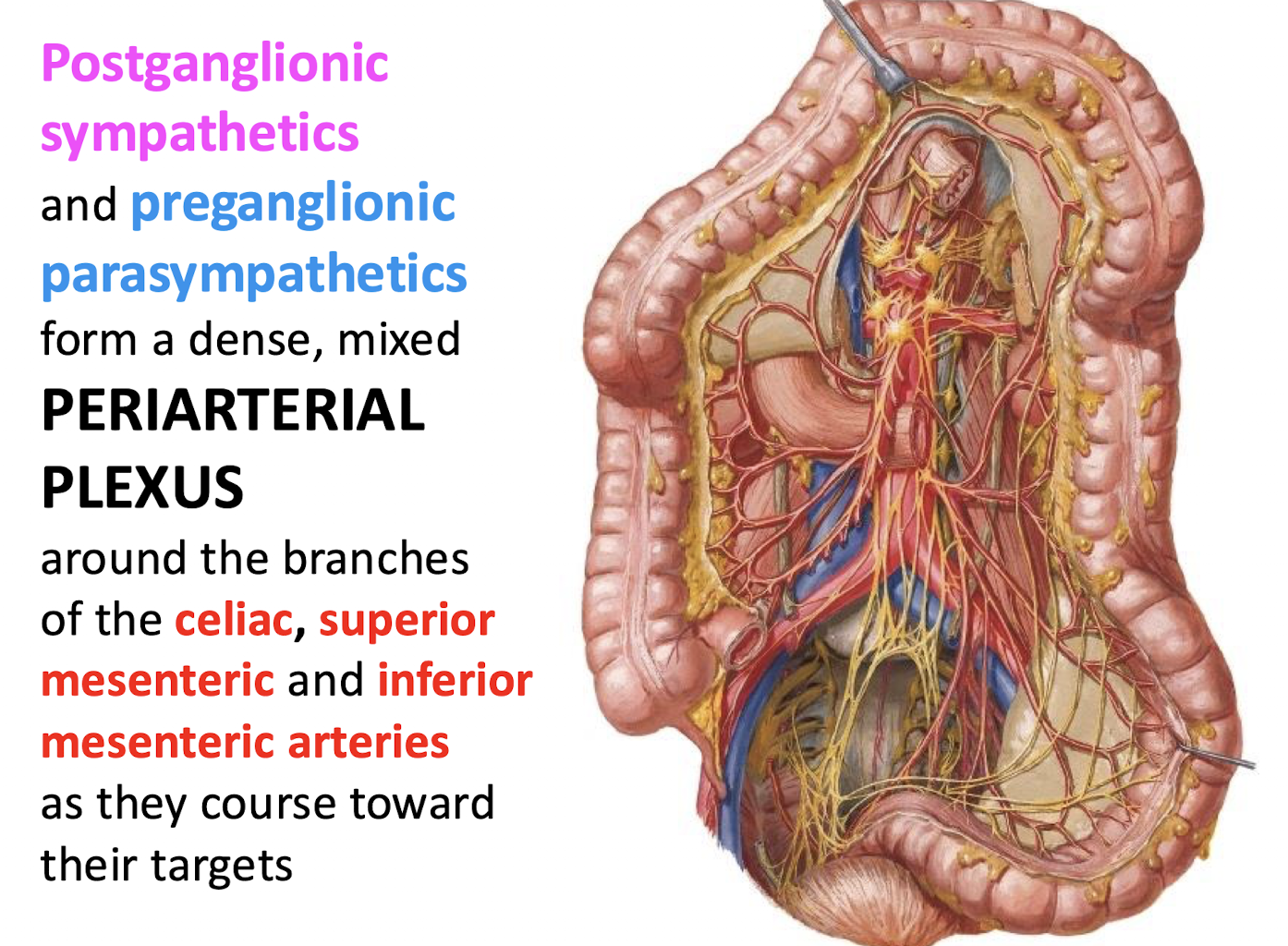
What type of plexus is formed by postganglionic sympathetics and preganglionic parasympathetics around the major GI arteries. What are the GI arteries?
A dense; mixed PERIARTERIAL PLEXUS around the branches of the celiac, superior mesenteric and inferior mesenteric arteries
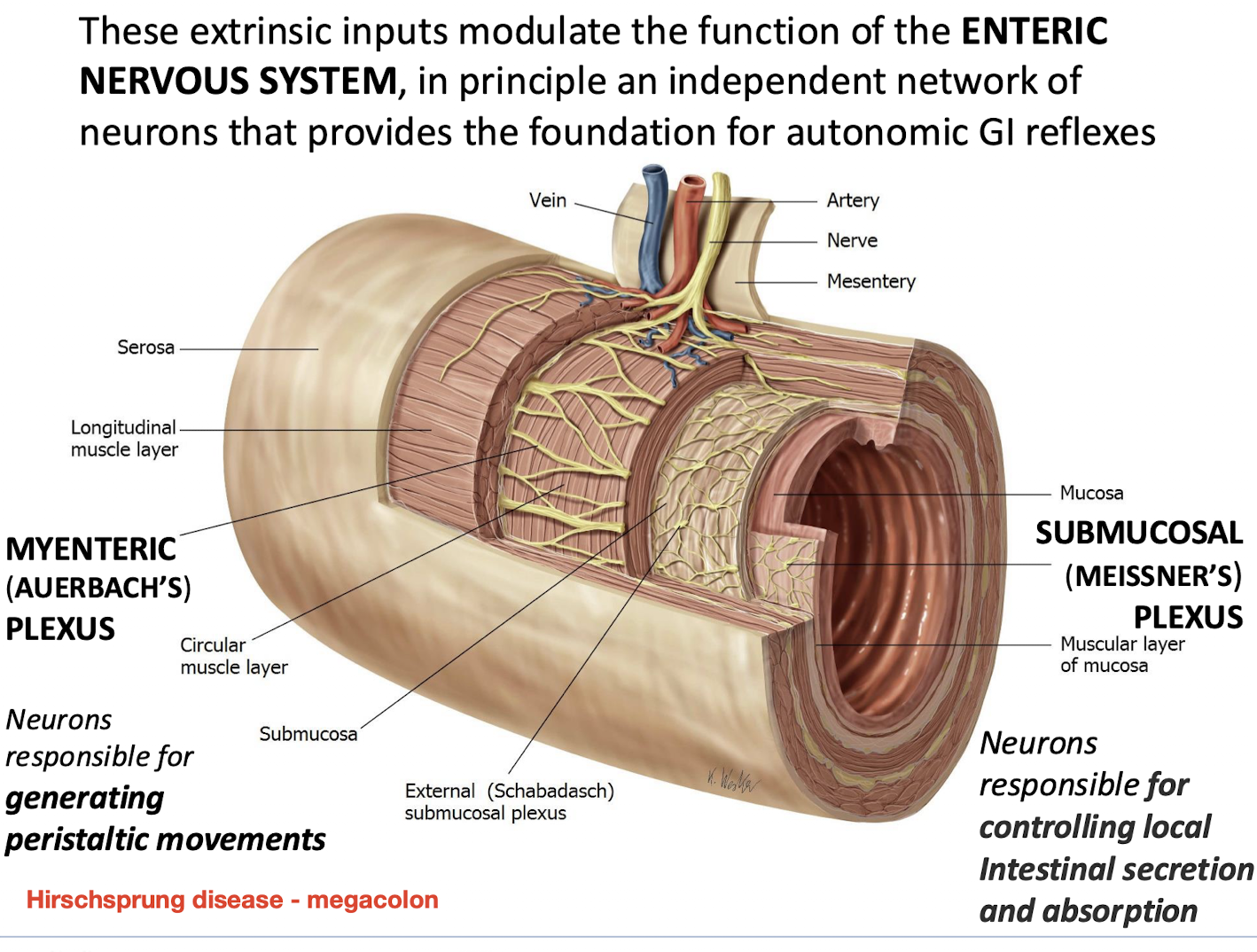
What is the function of the ENTERIC NERVOUS SYSTEM (ENS)
It is an independent network of neurons that provides the foundation for autonomic GI reflexes.
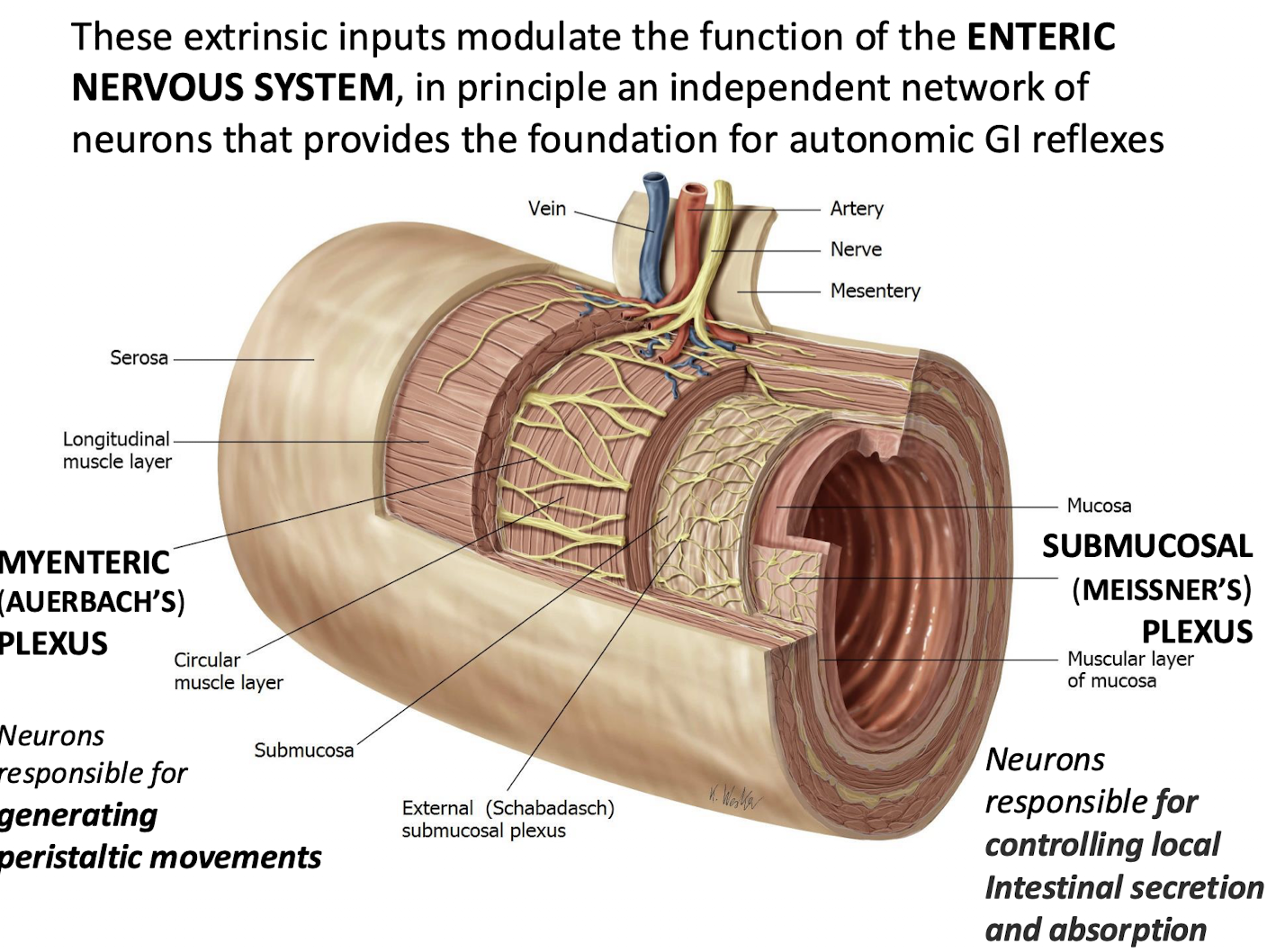
Which plexus of the ENS is responsible for generating peristaltic movements
MYENTERIC (AUERBACH’S) PLEXUS.
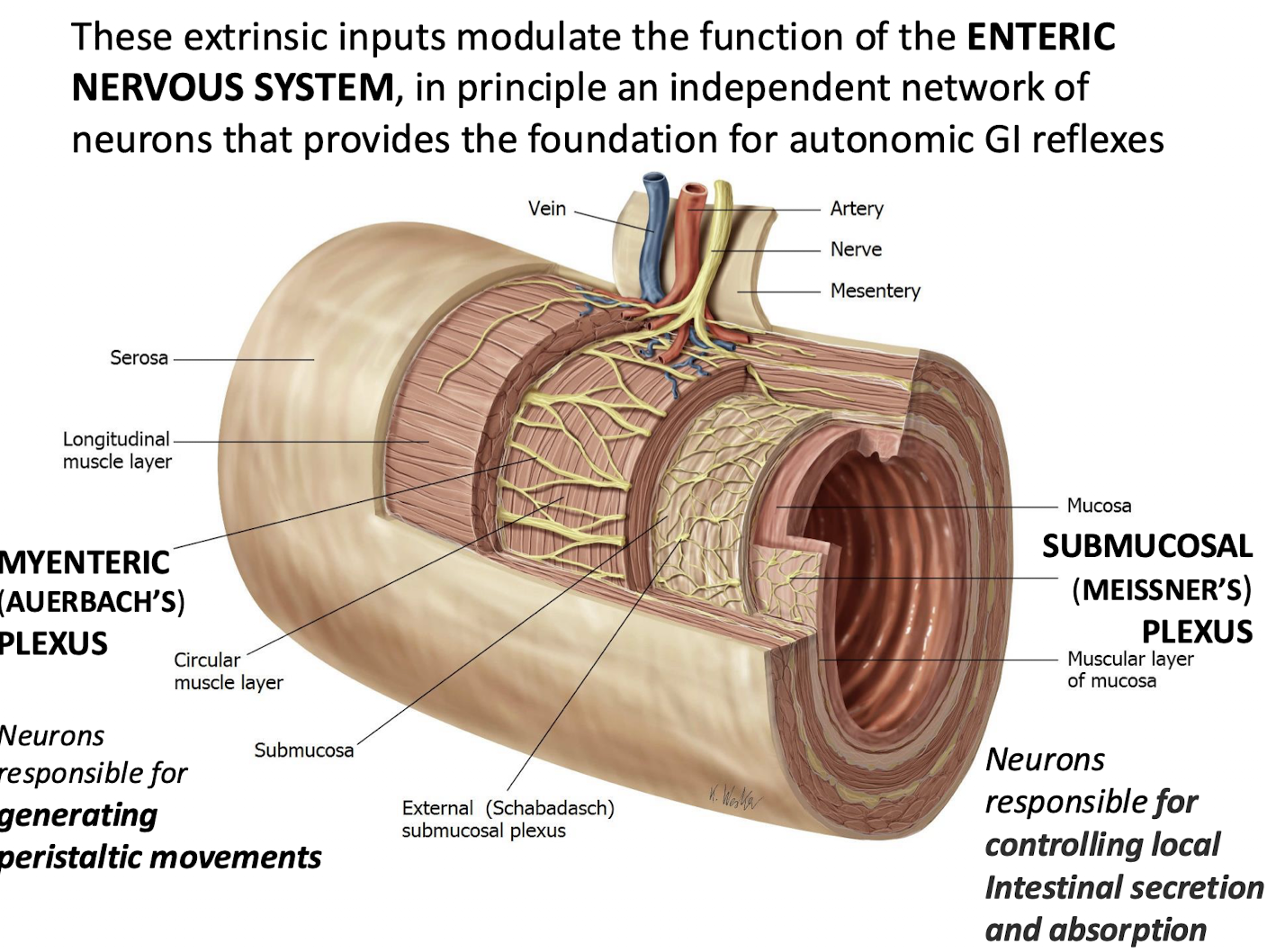
Which plexus of the ENS is responsible for controlling local intestinal secretion and absorption
SUBMUCOSAL (MEISSNER’S) PLEXUS.
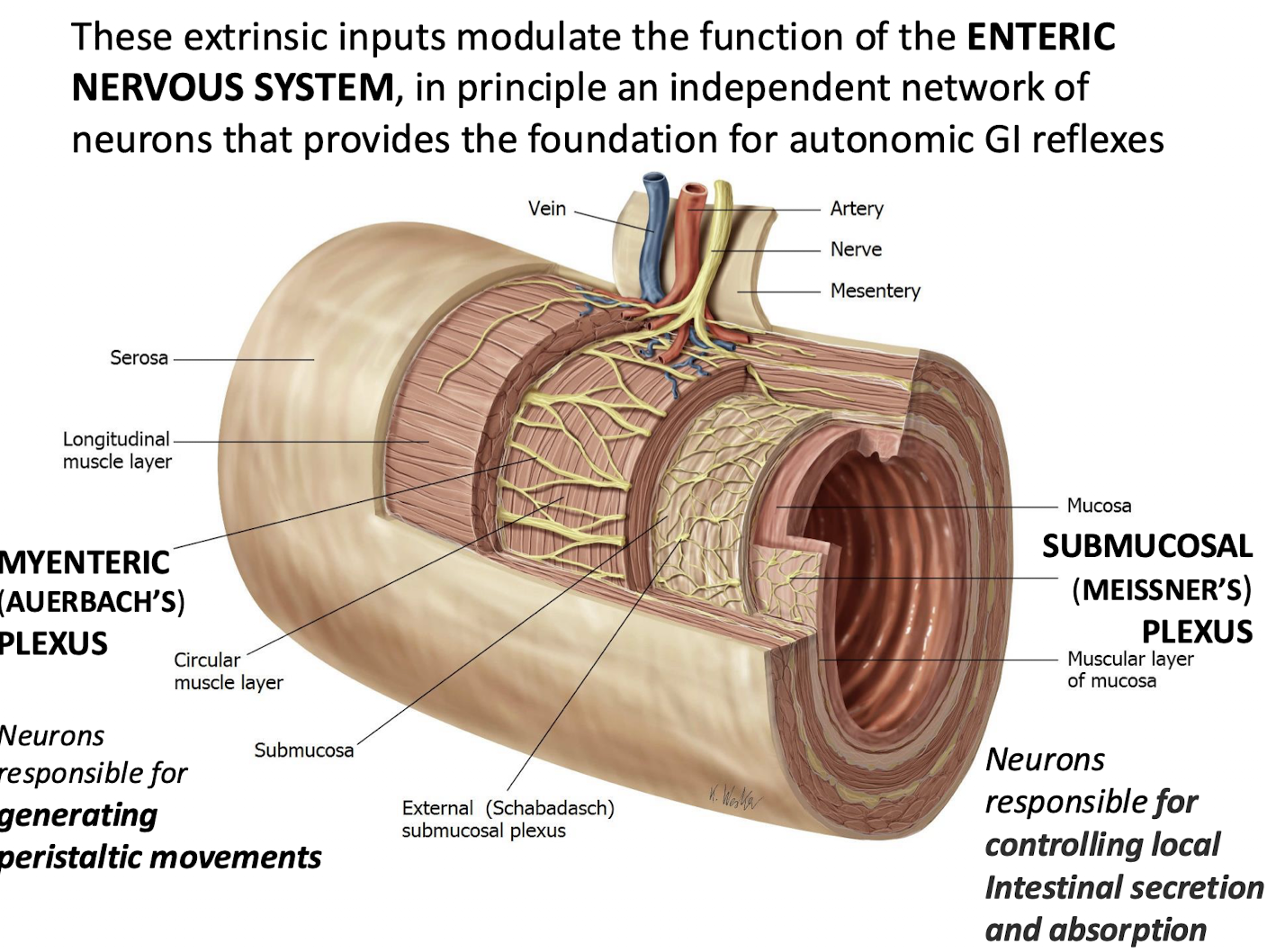
What condition is associated with the absence of enteric neurons in the colon, leading to megacolon?
Hirschsprung disease
Caused by congenital absence of ganglion cells in the myenteric (Auerbach’s) and submucosal (Meissner’s) plexuses.
Leads to failure of peristalsis → functional obstruction → megacolon.
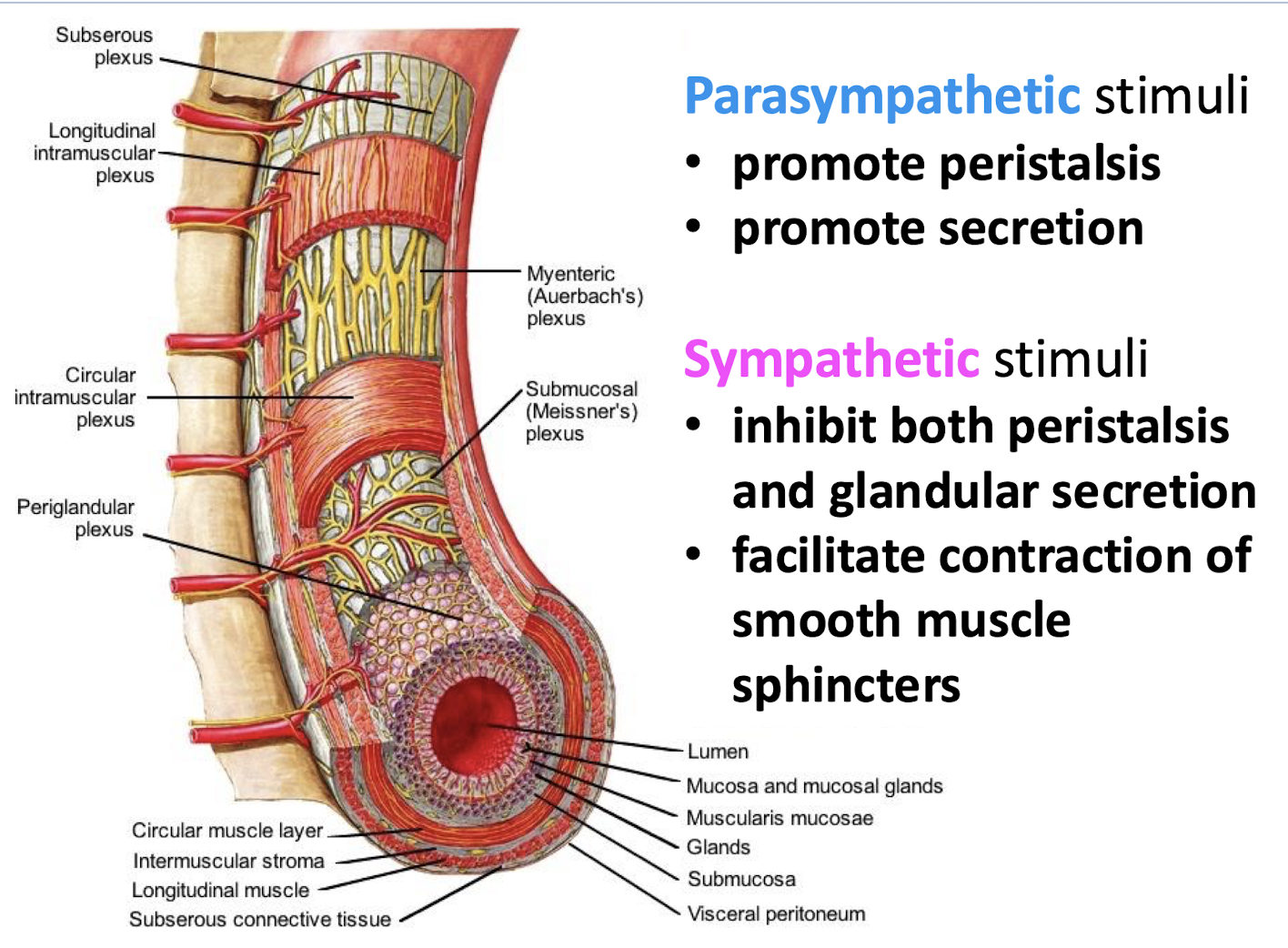
What effects do parasympathetic stimuli have on GI function
They promote peristalsis; and promote secretion.
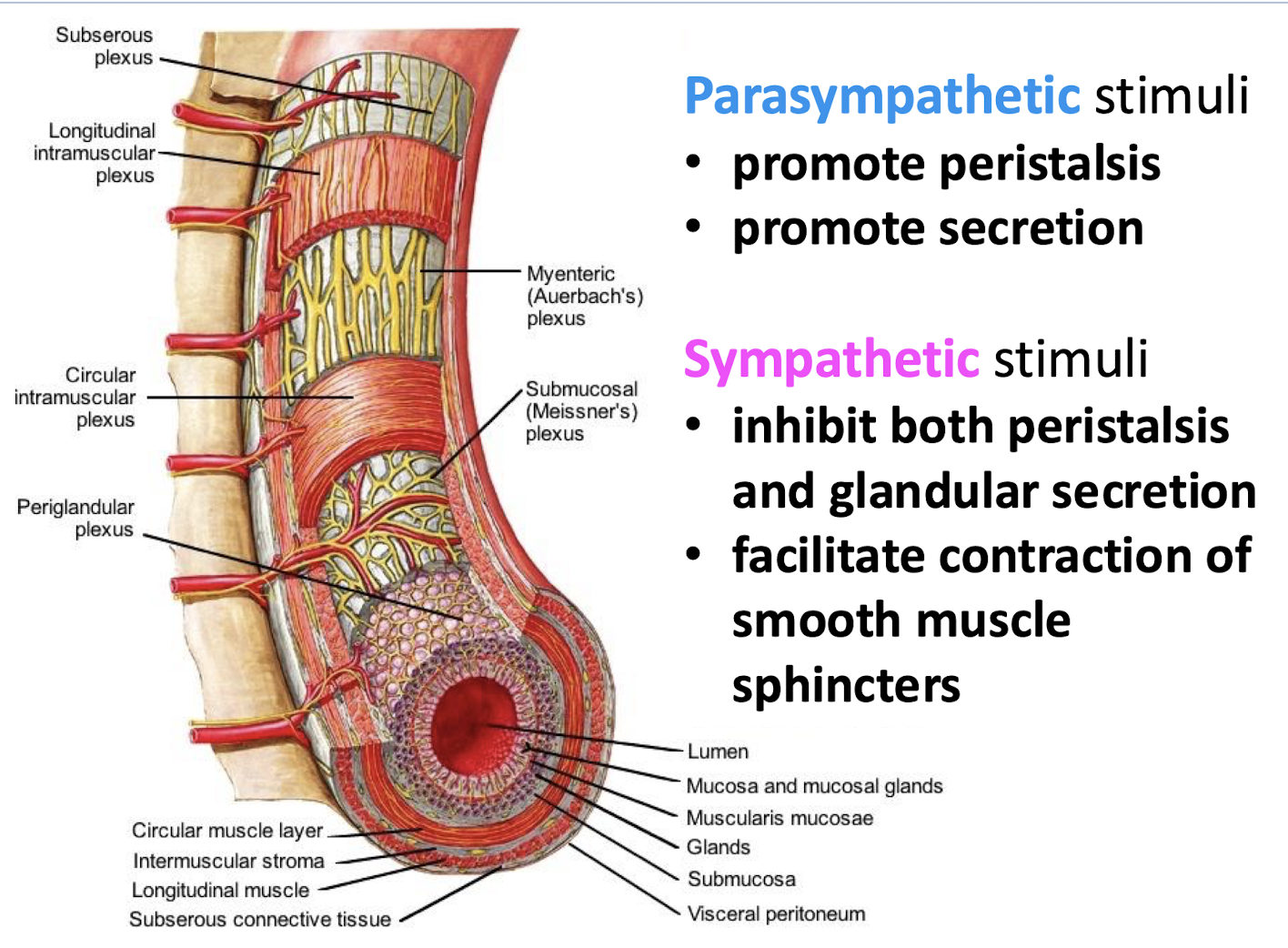
What effects do sympathetic stimuli have on GI function
They inhibit both peristalsis and glandular secretion.
They faciliate contraction of smooth muscle sphincters.
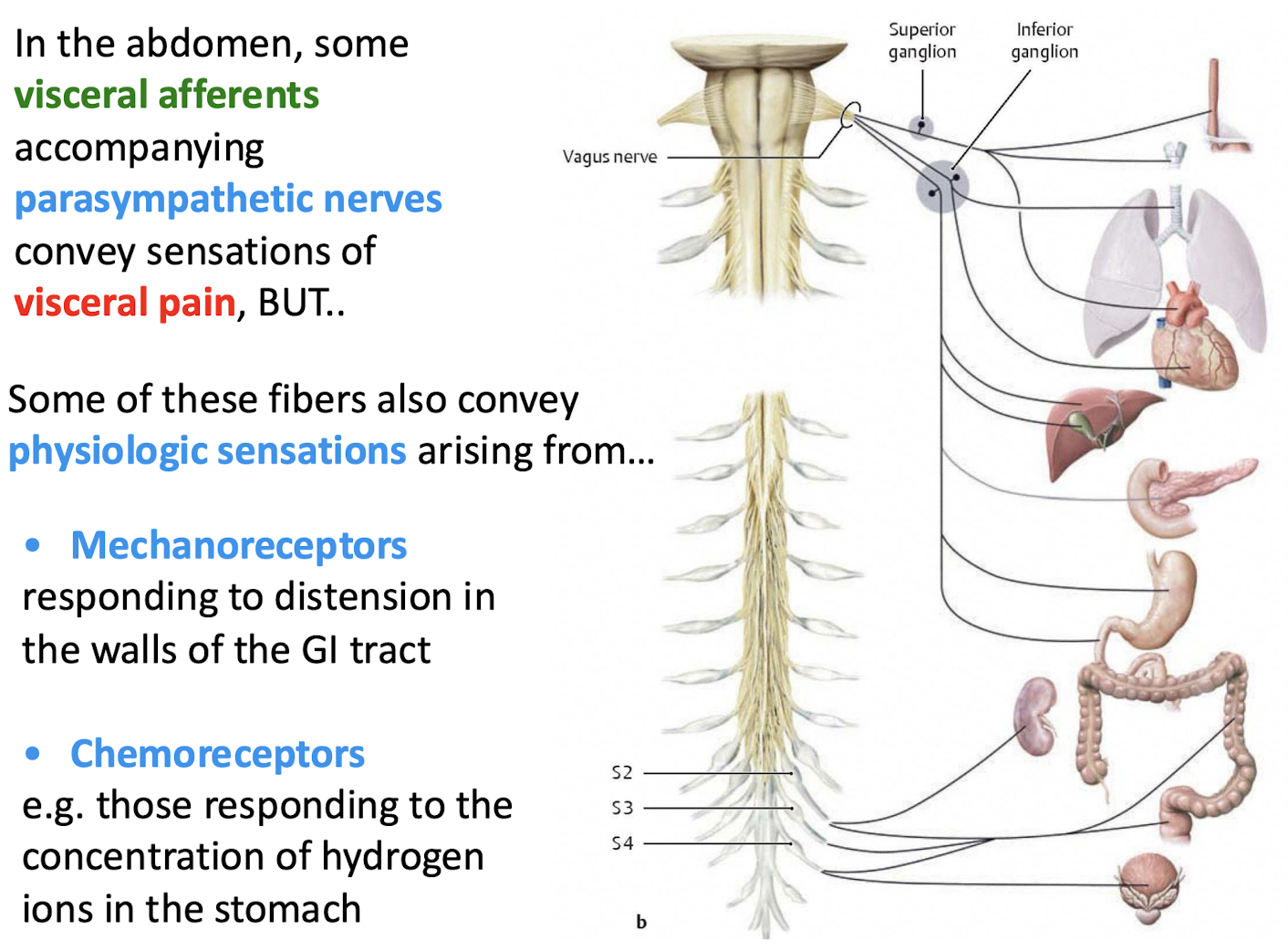
What sensations do visceral afferents accompanying parasympathetic nerves convey
Sensations of visceral pain; and physiologic sensations arising from Mechanoreceptors responding to distension in the walls of the GI tract; or Chemoreceptors e;g; those responding to the concentration of hydrogen.
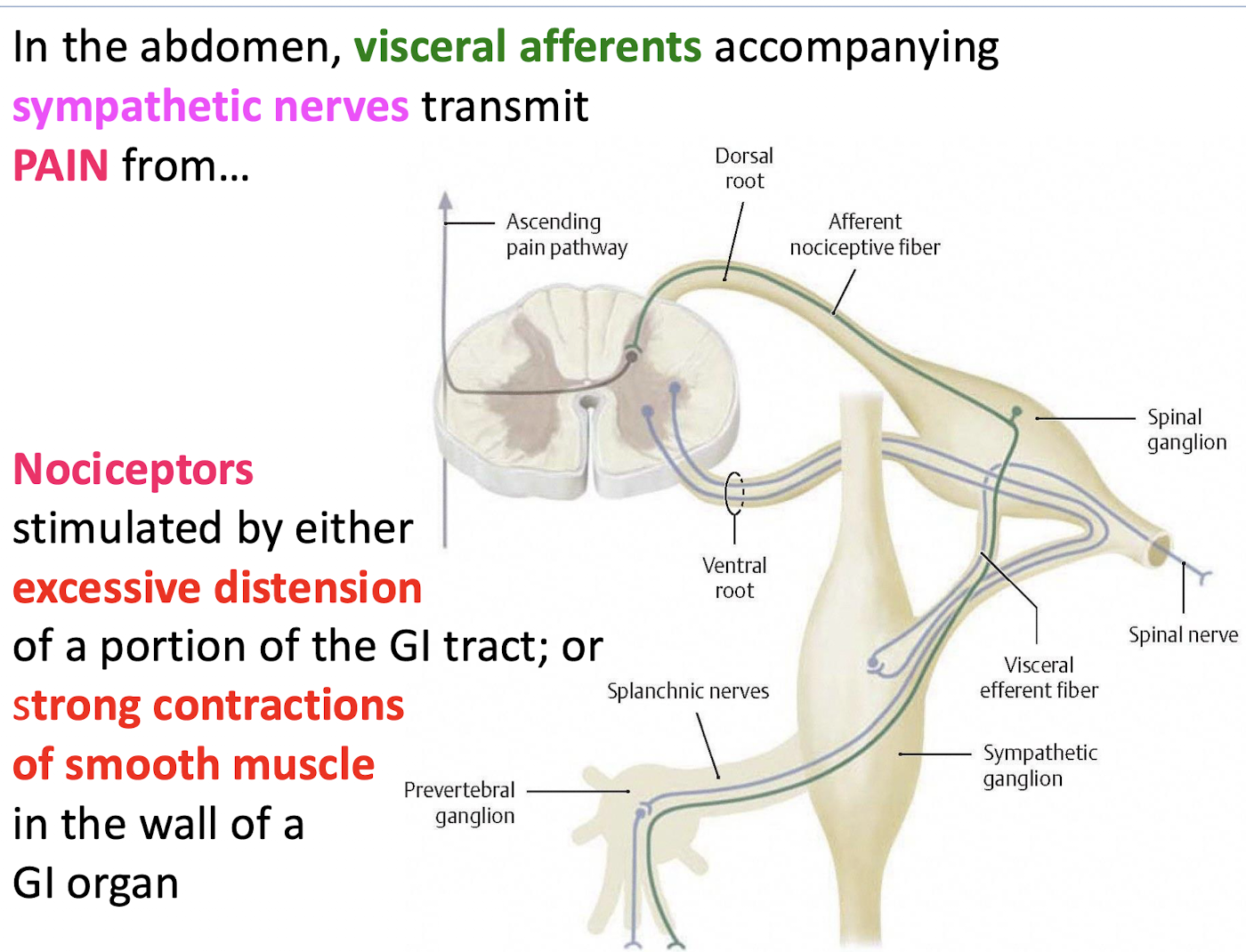
What primarily stimulates the nociceptors (pain receptors) whose visceral afferent fibers travel with sympathetic nerves?
Either excessive distension of a portion of the GI tract; or strong contractions of smooth muscle in the wall of a GI organ.
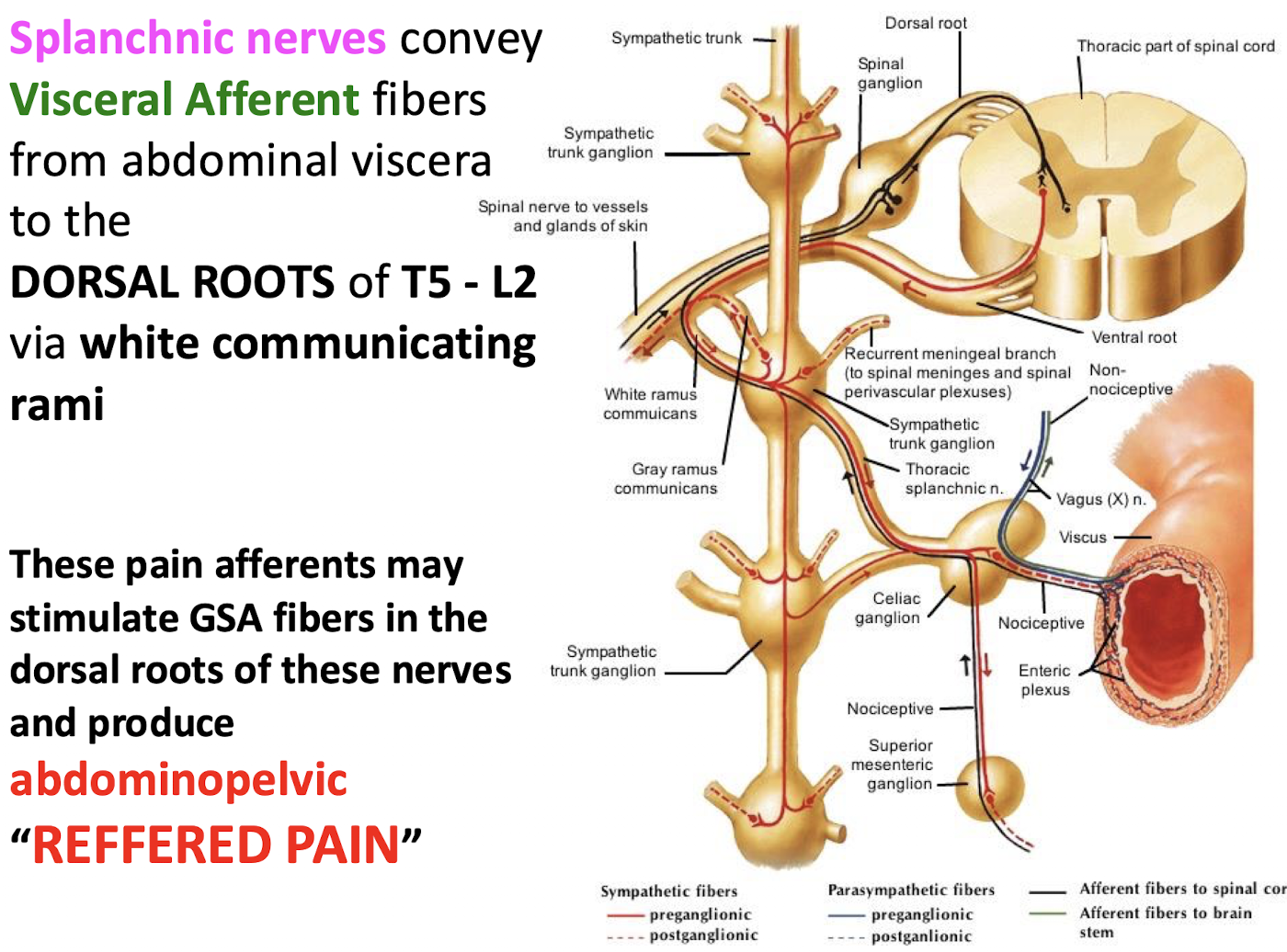
Which spinal cord levels (and through what pathway) do Visceral Afferent fibers enter the dorsal roots after traveling in Splanchnic Nerves?
The fibers enter the Dorsal Roots of spinal cord levels T5 through L2 via the White Communicating Rami.
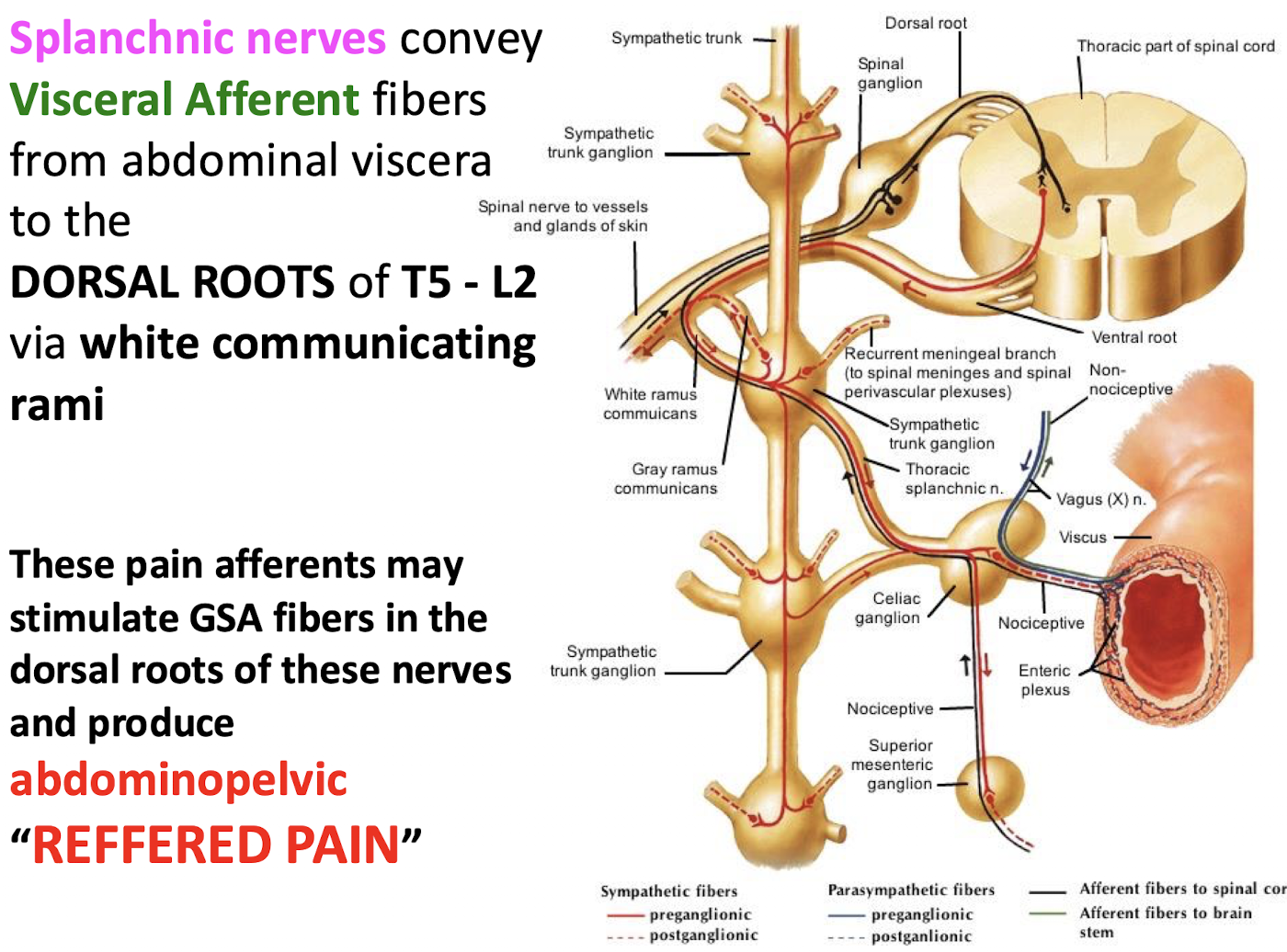
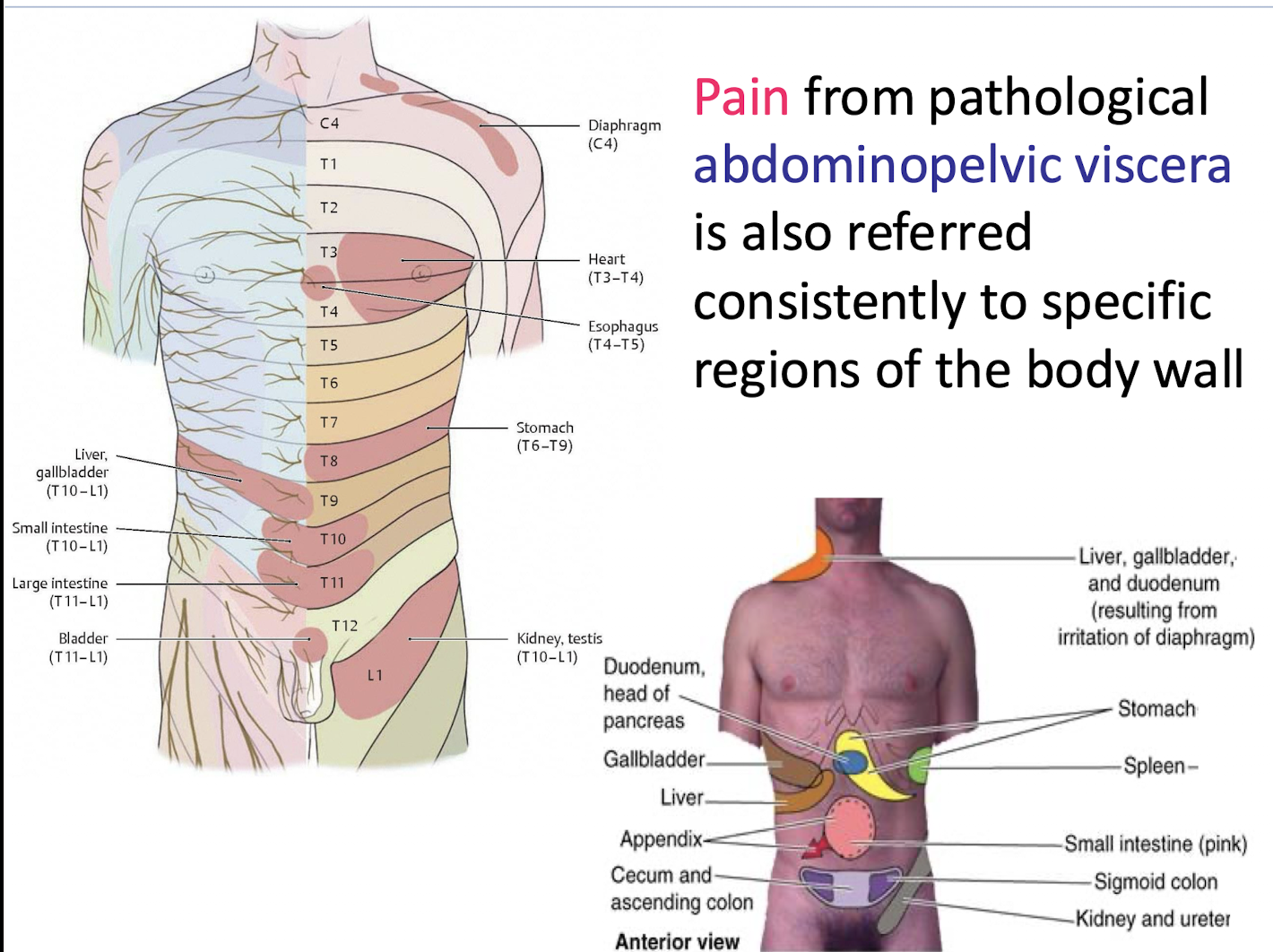
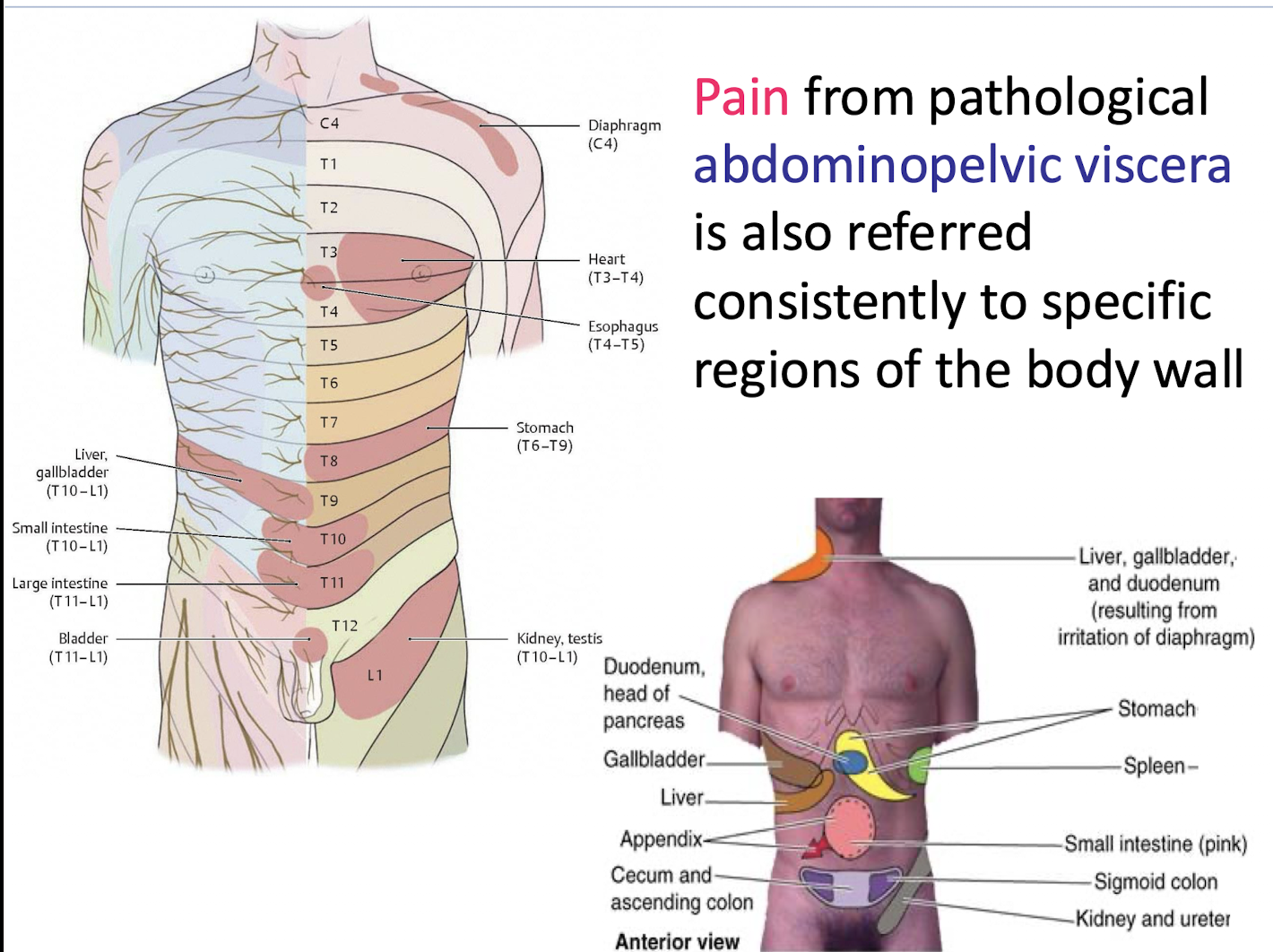
What is the mechanism by which visceral pain produces "REFFERED PAIN"
Visceral afferent (GVA) pain fibers stimulate General Somatic Afferent (GSA) fibers (from the body wall) that enter the same dorsal root level (T5–L2). The brain interprets the signal as coming from the more sensitive somatic (body wall) location.
Just FYI
Pain signals from diseased or injured abdominopelvic organs are consistently referred to specific, predictable regions of the body wall.
What organs are associated with the following bony landmarks:
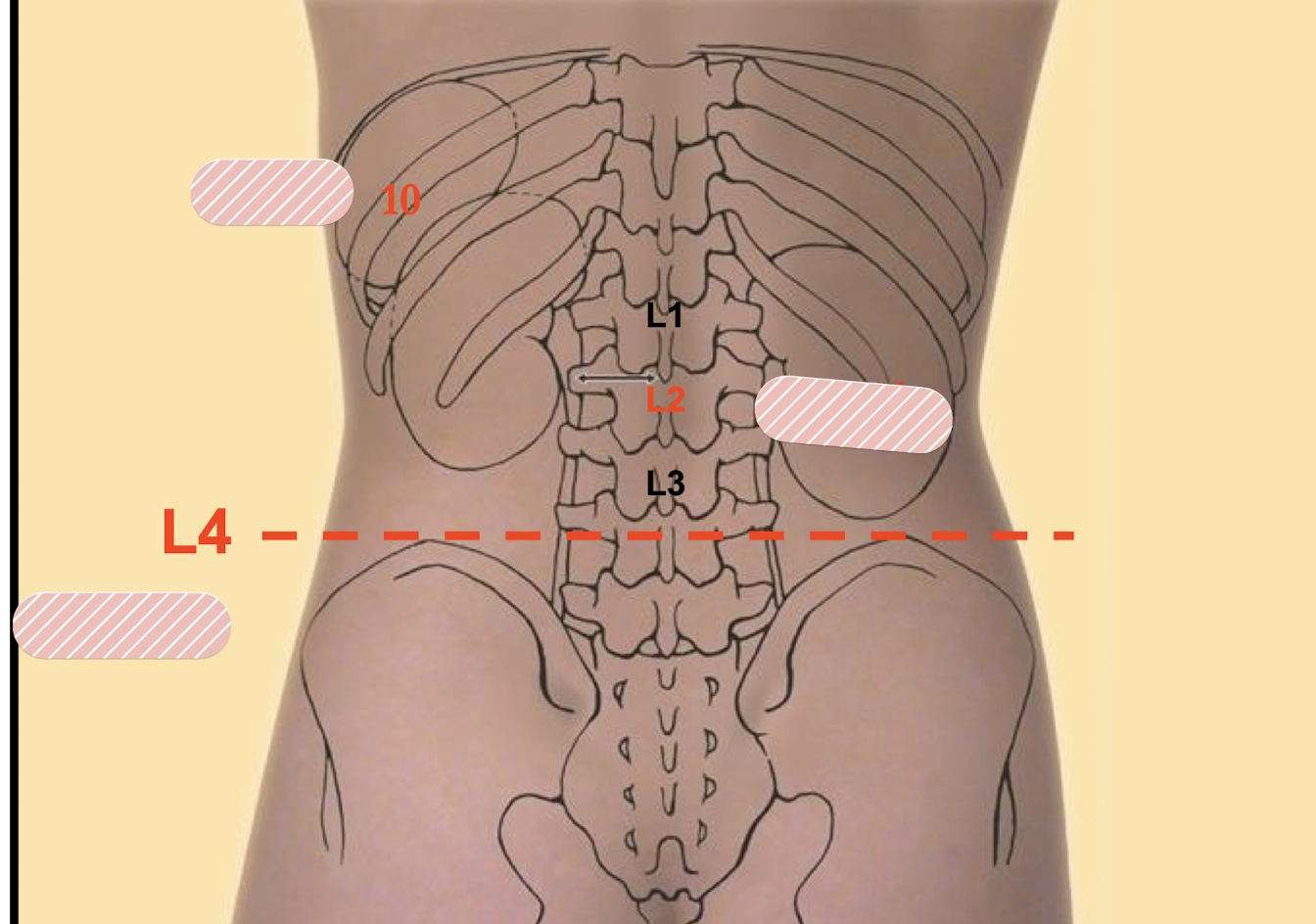
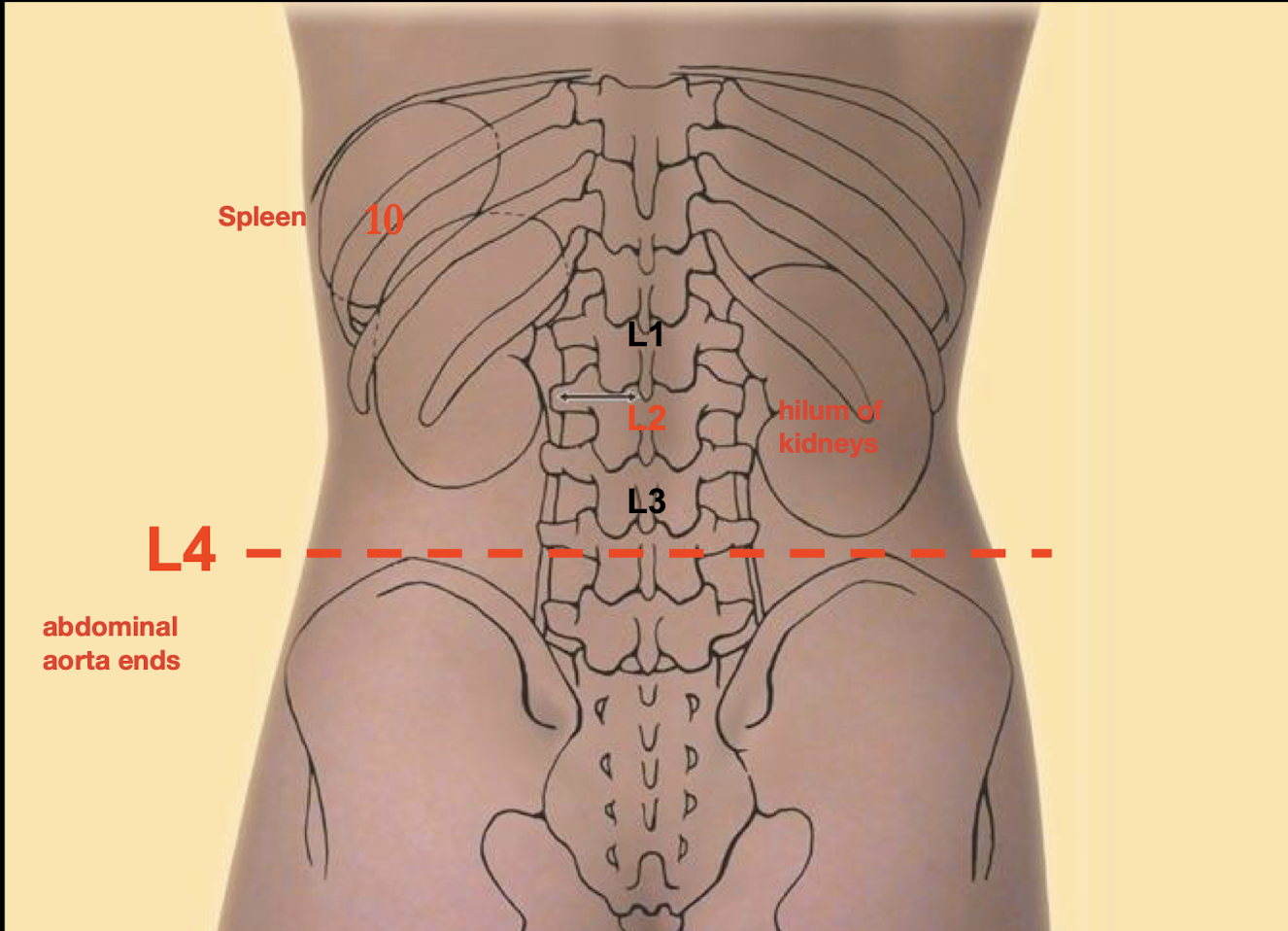
L4 is also start of Iliac crest
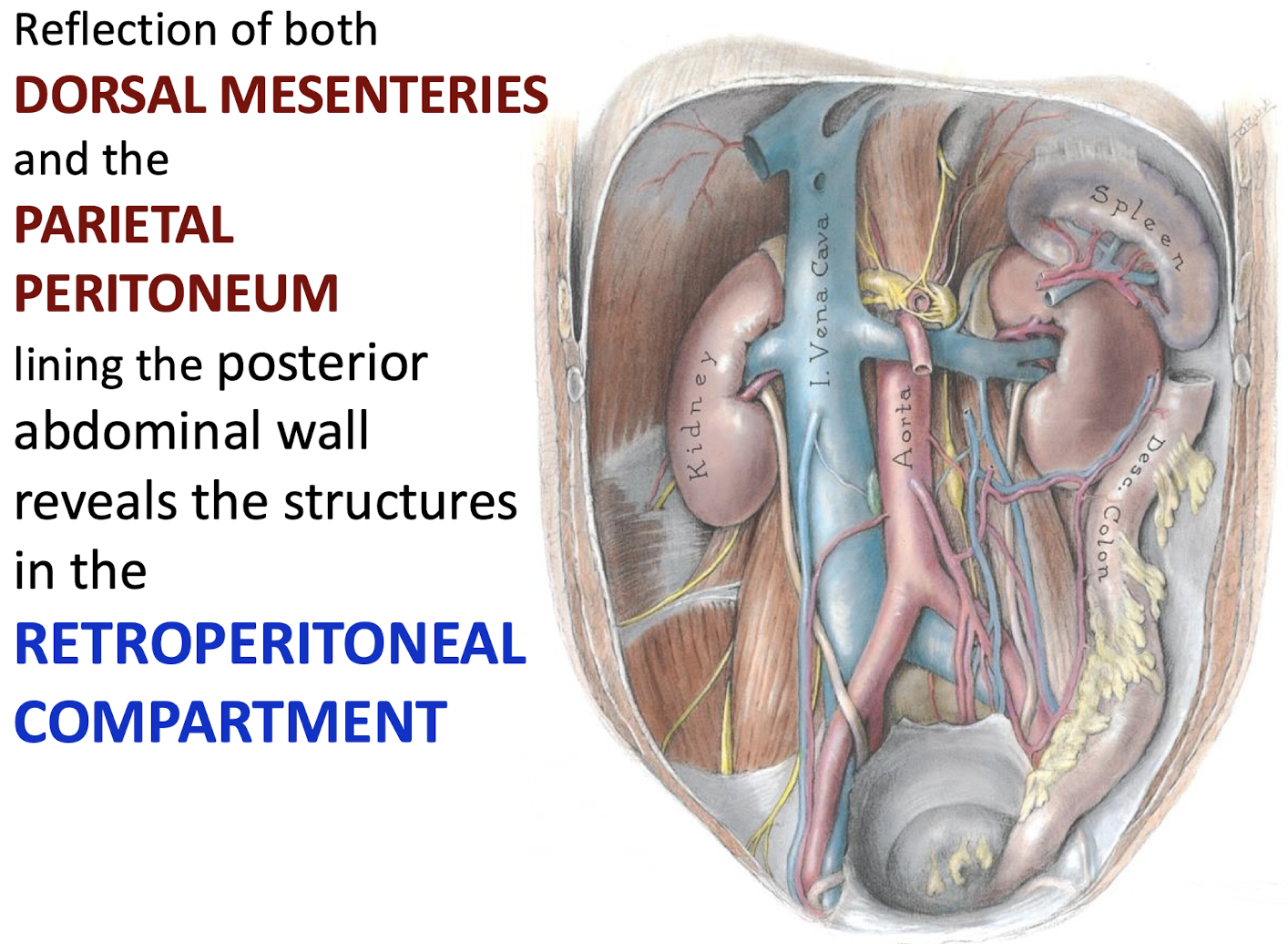
What structures are revealed upon reflection of both DORSAL MESENTERIES and the PARIETAL PERITONEUM lining the posterior abdominal wall
The structures in the RETROPERITONEAL COMPARTMENT.
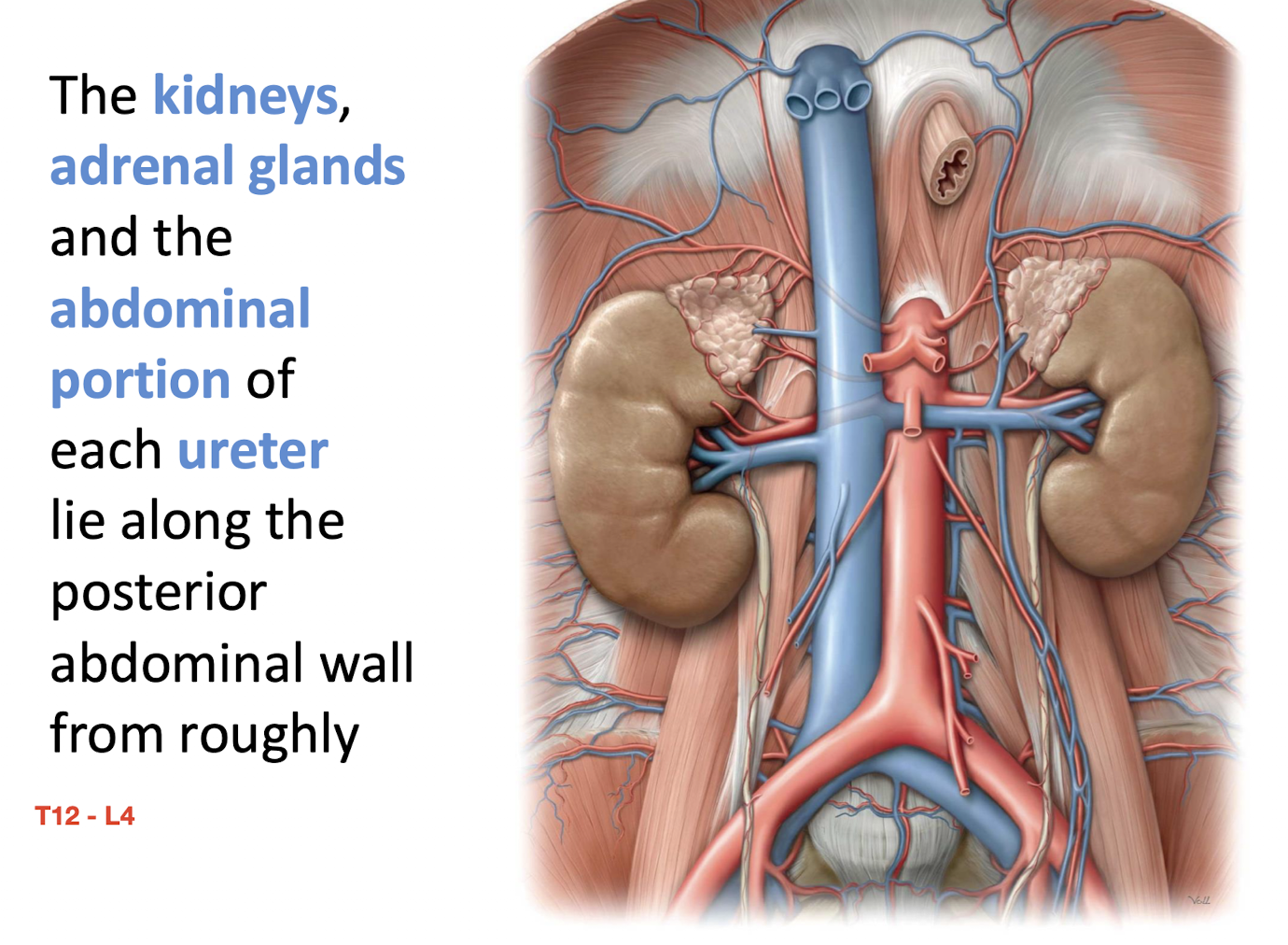
What primary organs lie along the posterior abdominal wall within the retroperitoneal compartment? What are the bony landamarks for this?
The kidneys; adrenal glands; and the abdominal portion of each ureter.
T12-L4
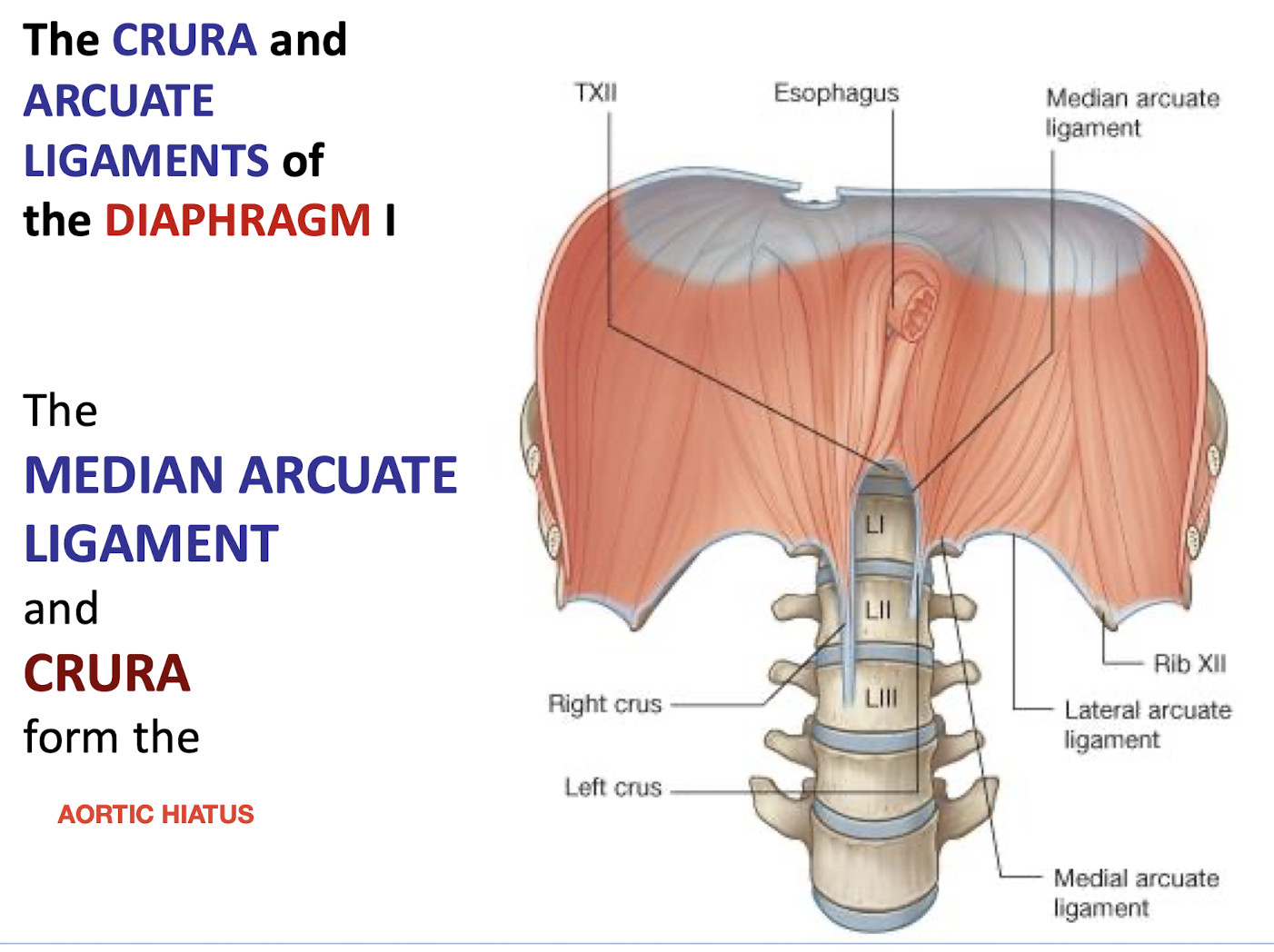
What forms the aortic hiatus in the diaphragm?
Median arcuate ligament and crura of the diaphragm
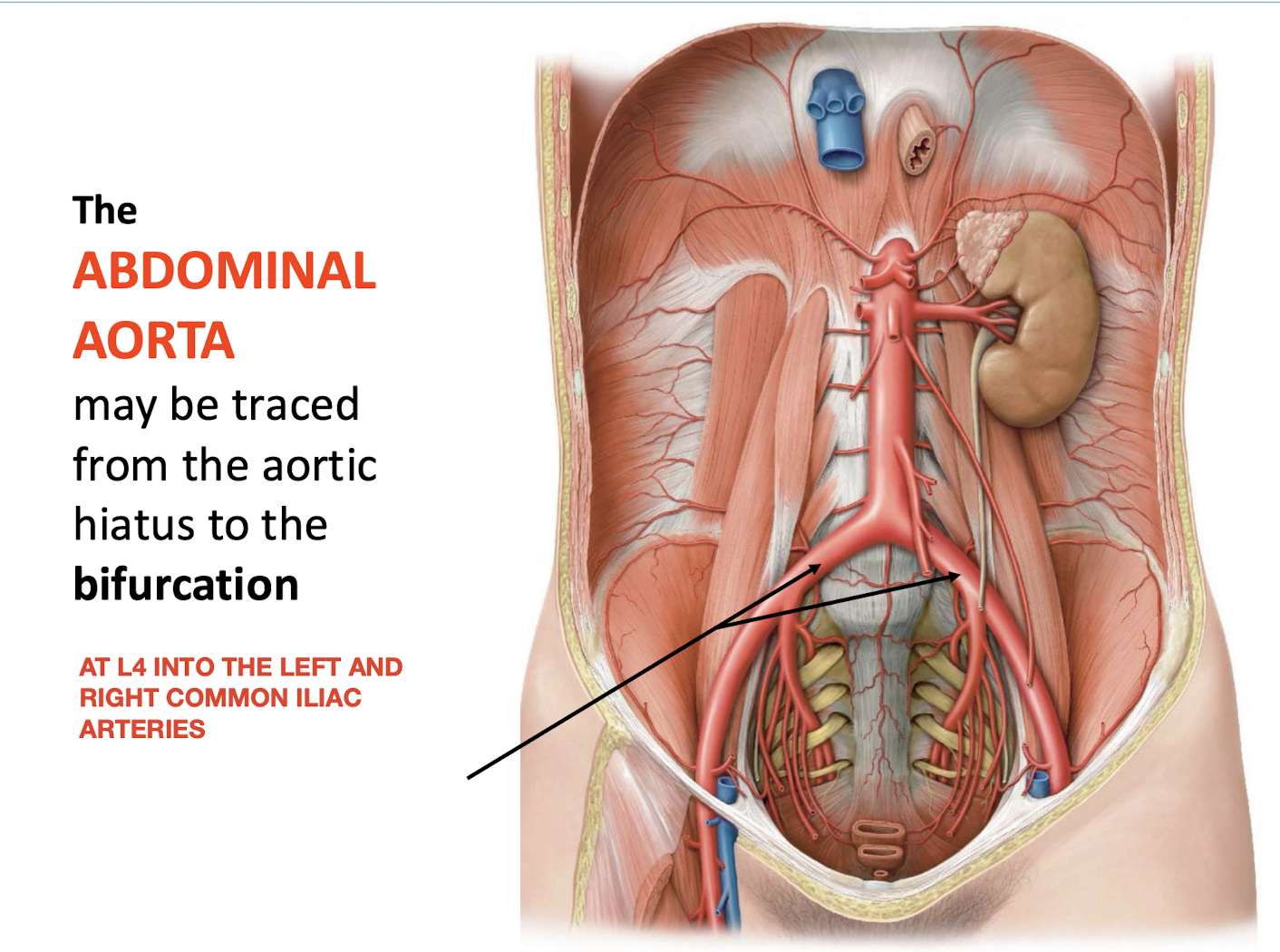
Where does the abdominal aorta begin and end, and what does it bifurcate into?
Begins at the aortic hiatus (formed by median arcuate ligament and crura of diaphragm).
Ends at L4, where it bifurcates into left and right common iliac arteries
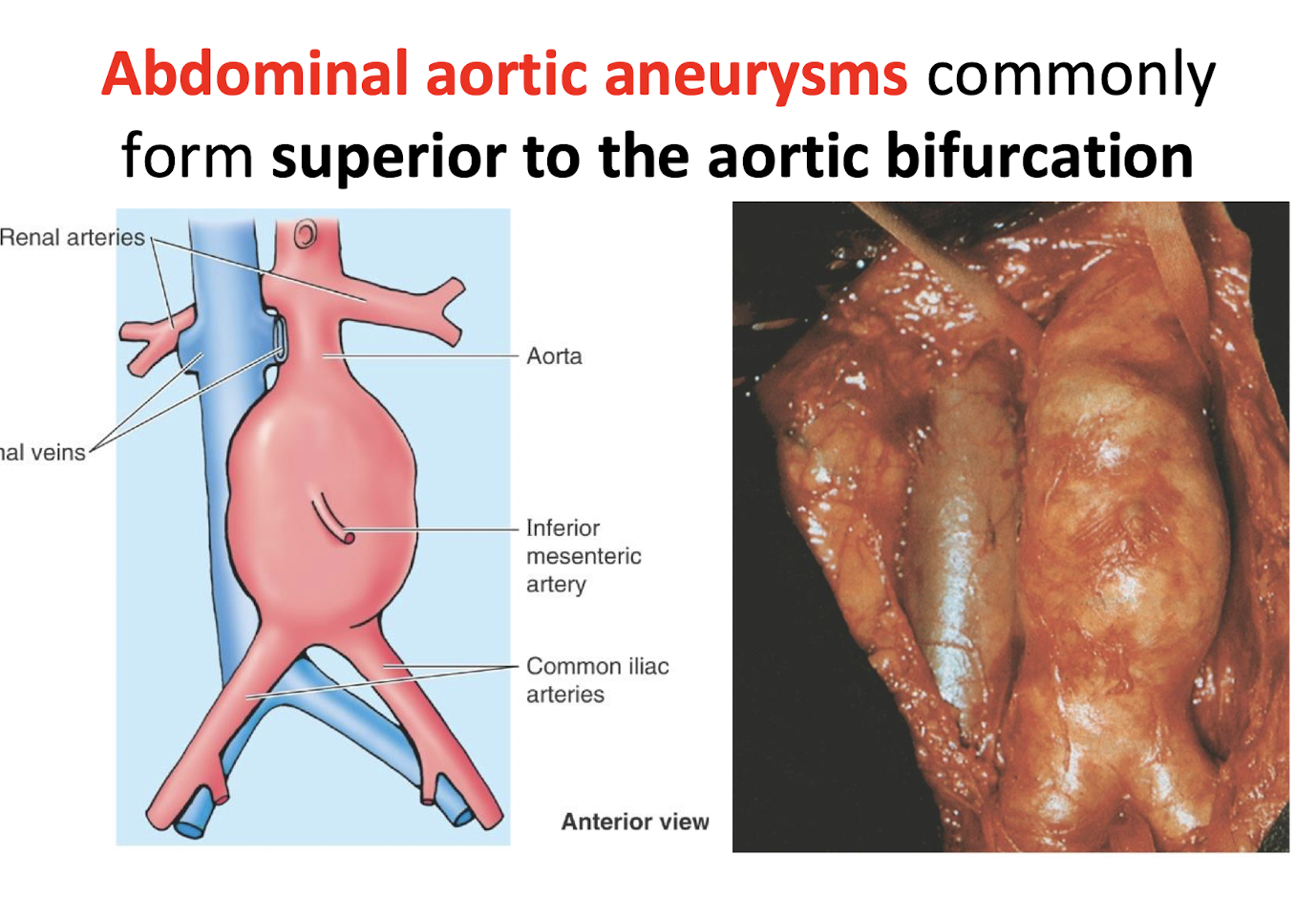
Where do Abdominal aortic aneurysms (AAAs) commonly form. Why are they particularly problematic?
Superior to the aortic bifurcation.
UP TO 75% ARE ASYMPTOMATIC
Can cause back pain and erosion of the vertebrae
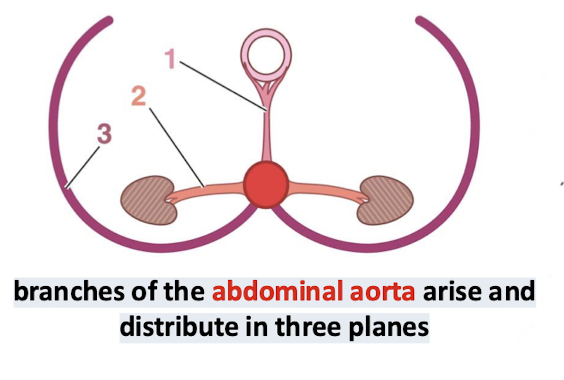
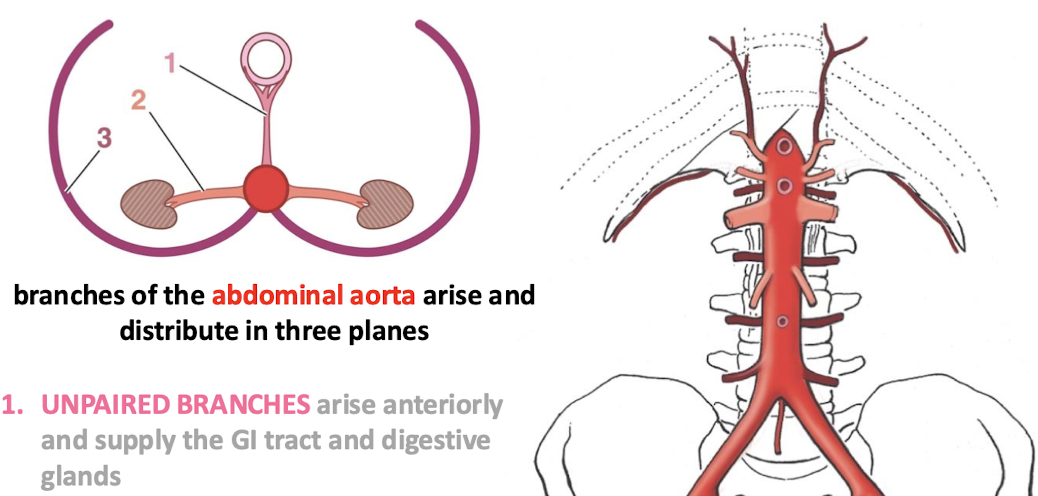
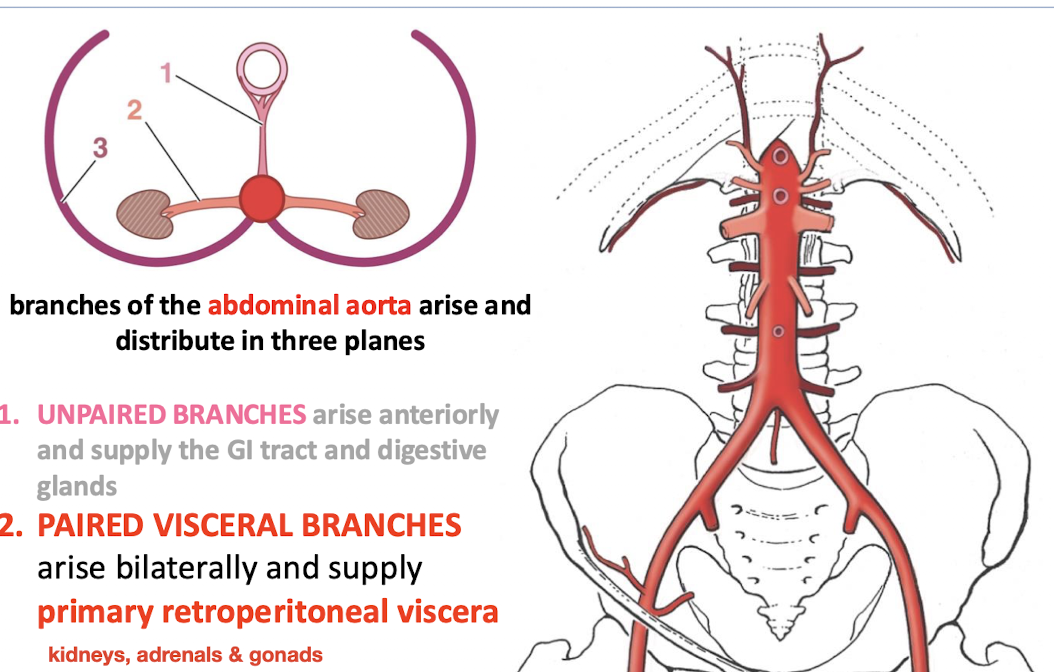
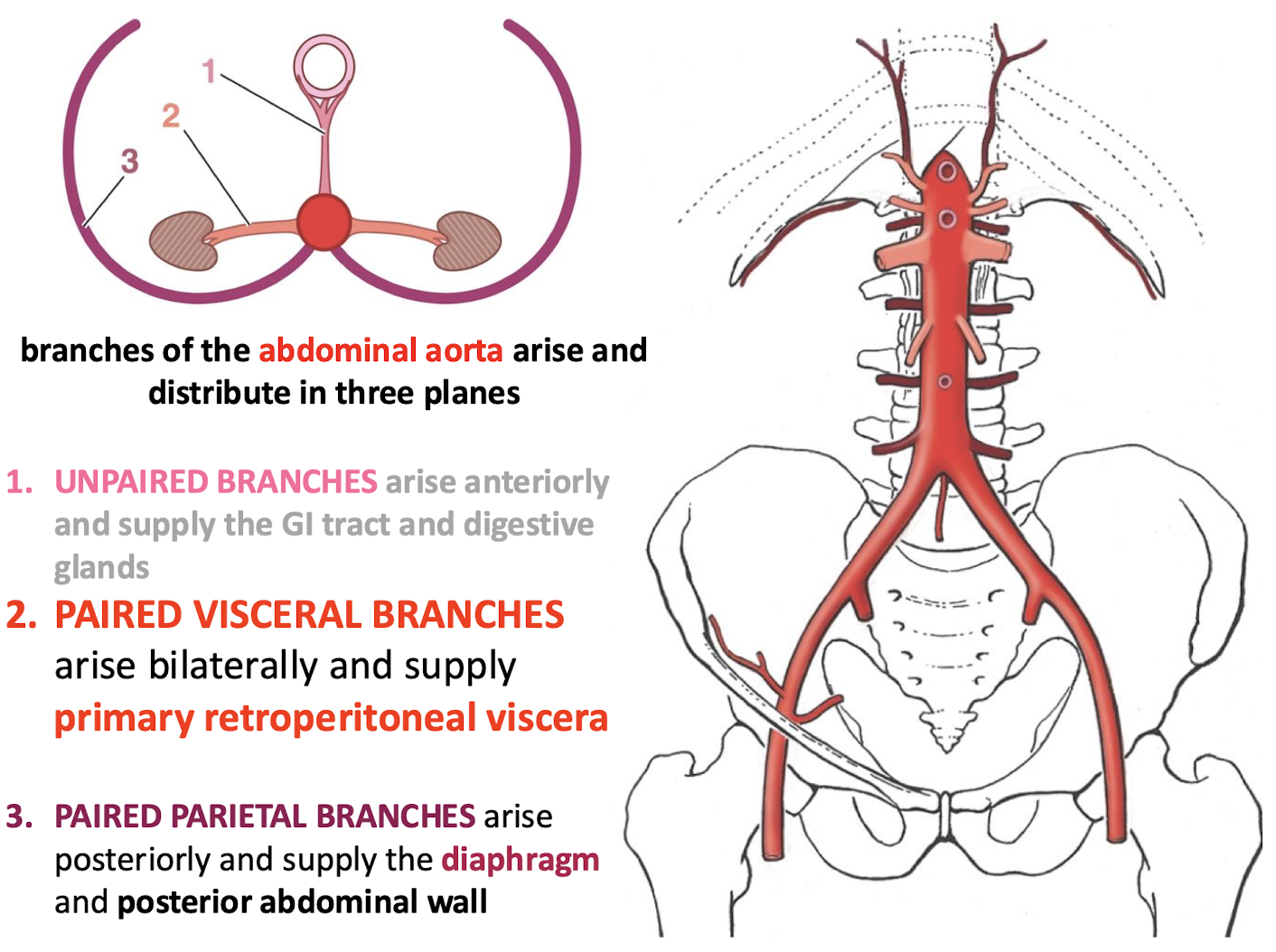
How do the branches of the abdominal aorta arise and distribute?
In three planes
UNPAIRED BRANCHES of the abdominal aorta arise from which aspect and supply which structures?
They arise anteriorly and supply the GI tract and digestive glands
PAIRED VISCERAL BRANCHES of the abdominal aorta arise from which aspect and supply which structures? Name examples
They arise bilaterally and supply primary retroperitoneal viscera. (The kidneys, gonads, and adrenals)
PAIRED PARIETAL BRANCHES of the abdominal aorta arise from which aspect and supply which structures?
They arise posteriorly and supply the diaphragm and posterior abdominal wall
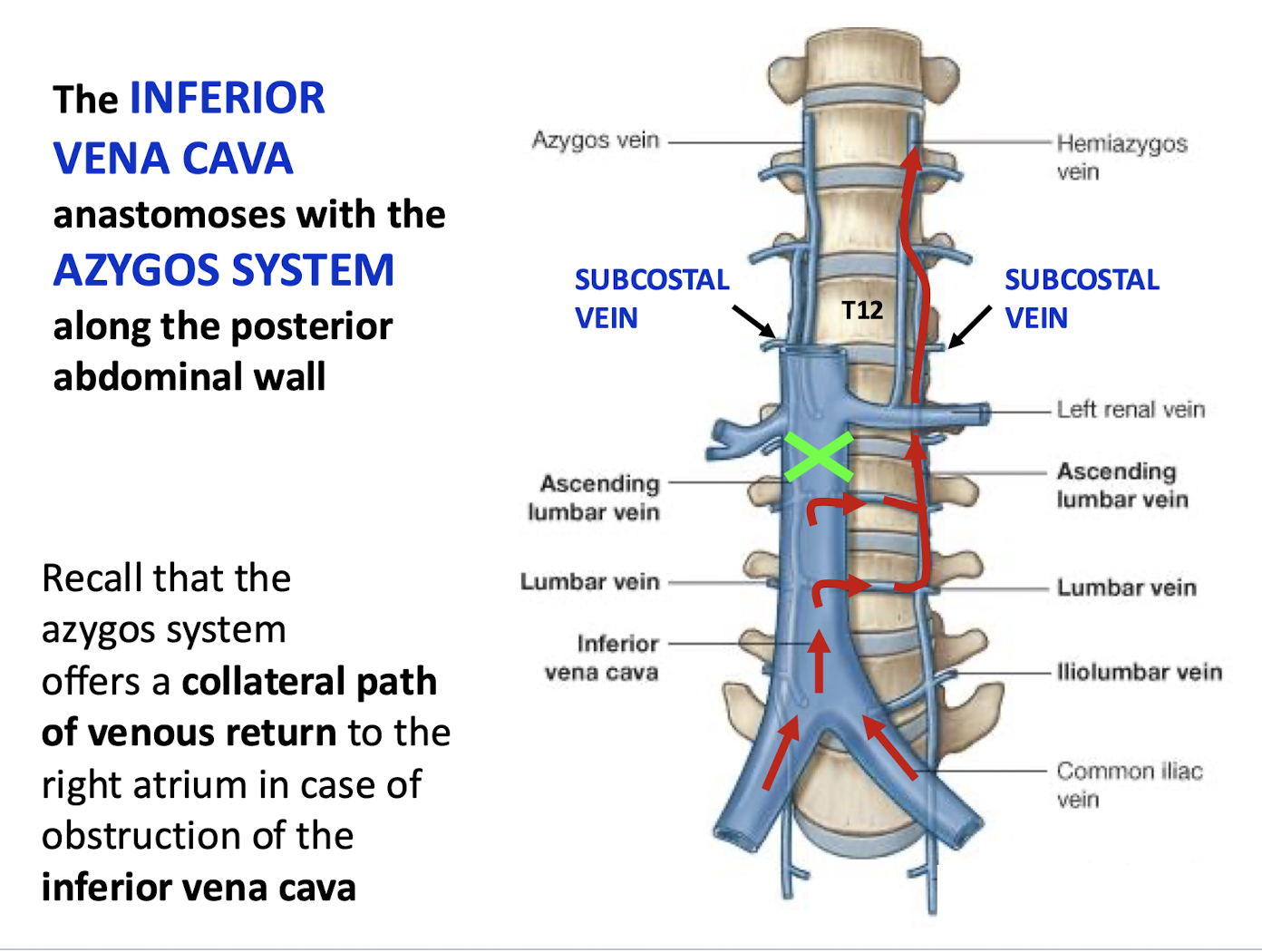
What system does the INFERIOR VENA CAVA (IVC) anastomose with along the posterior abdominal wall
The AZYGOS SYSTEM.
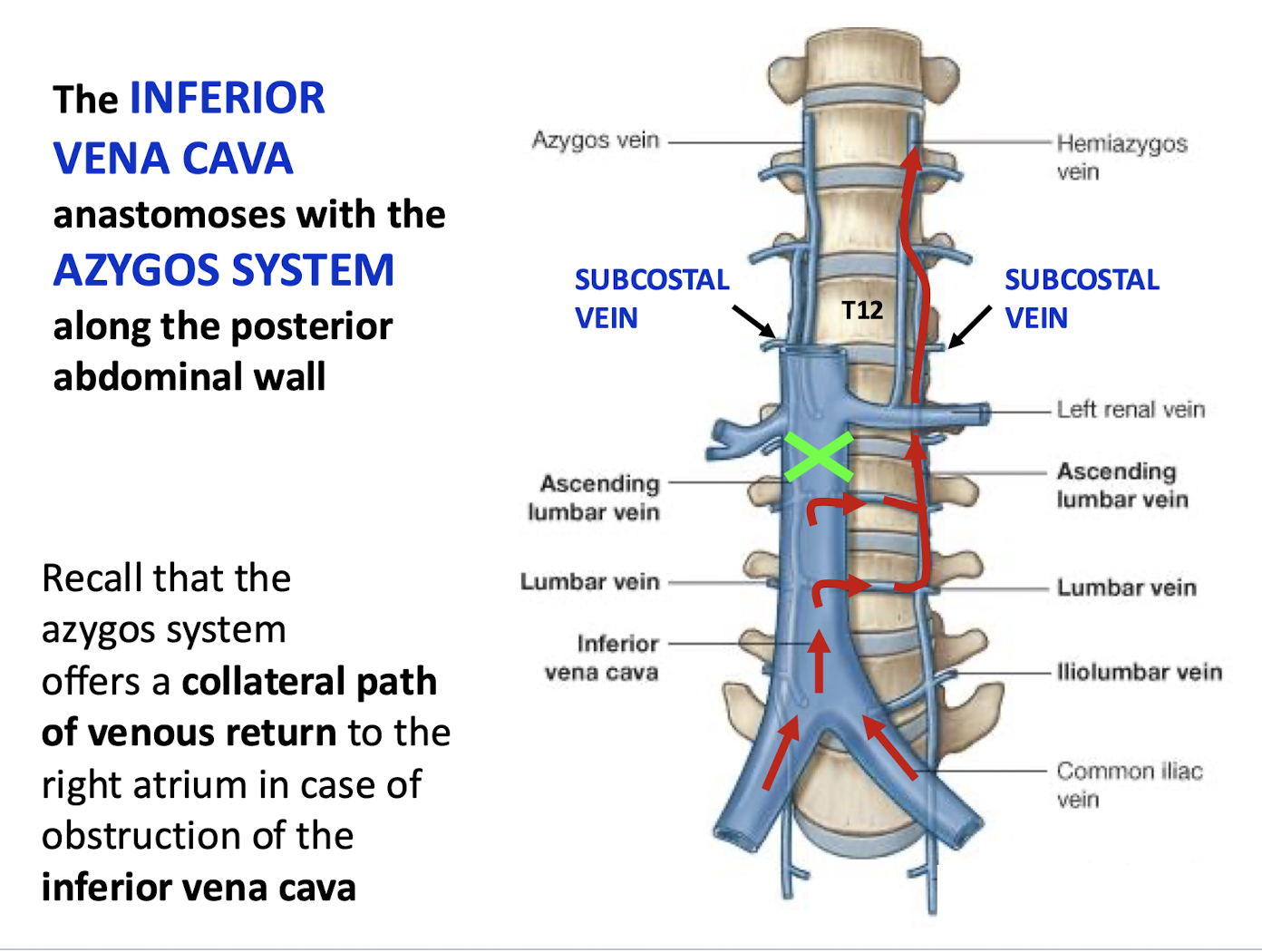
Why is the azygos system clinically significant regarding the IVC
It offers a collateral path of venous return to the right atrium in case of obstruction of the inferior vena cava.
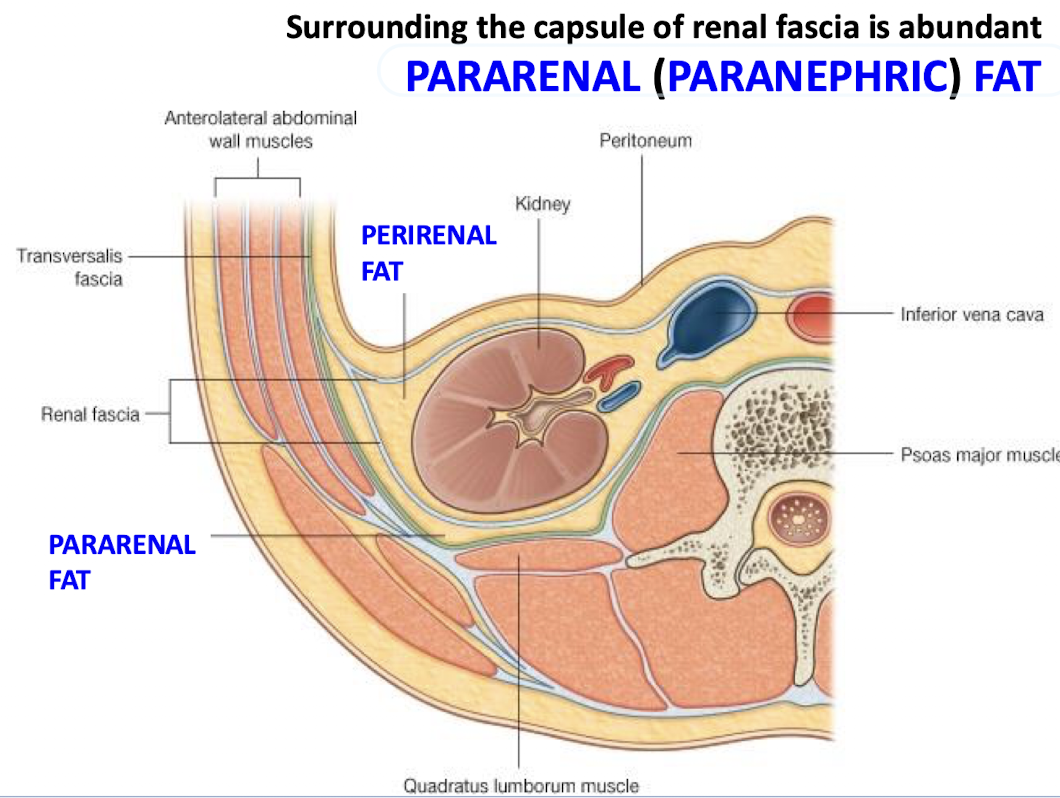
Which organs are classified as PRIMARY RETROPERITONEAL viscera
Kidneys; ureters; and adrenals.
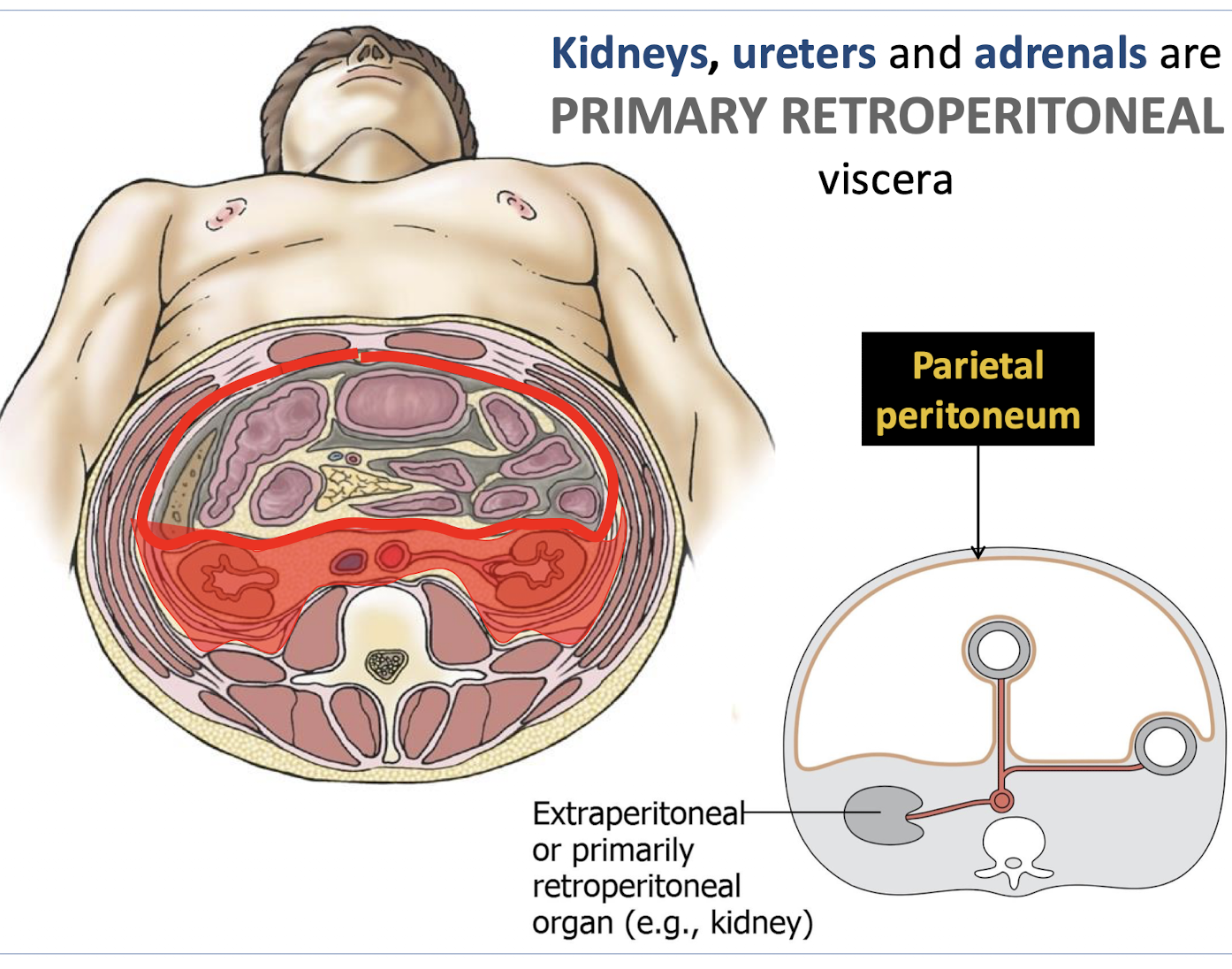
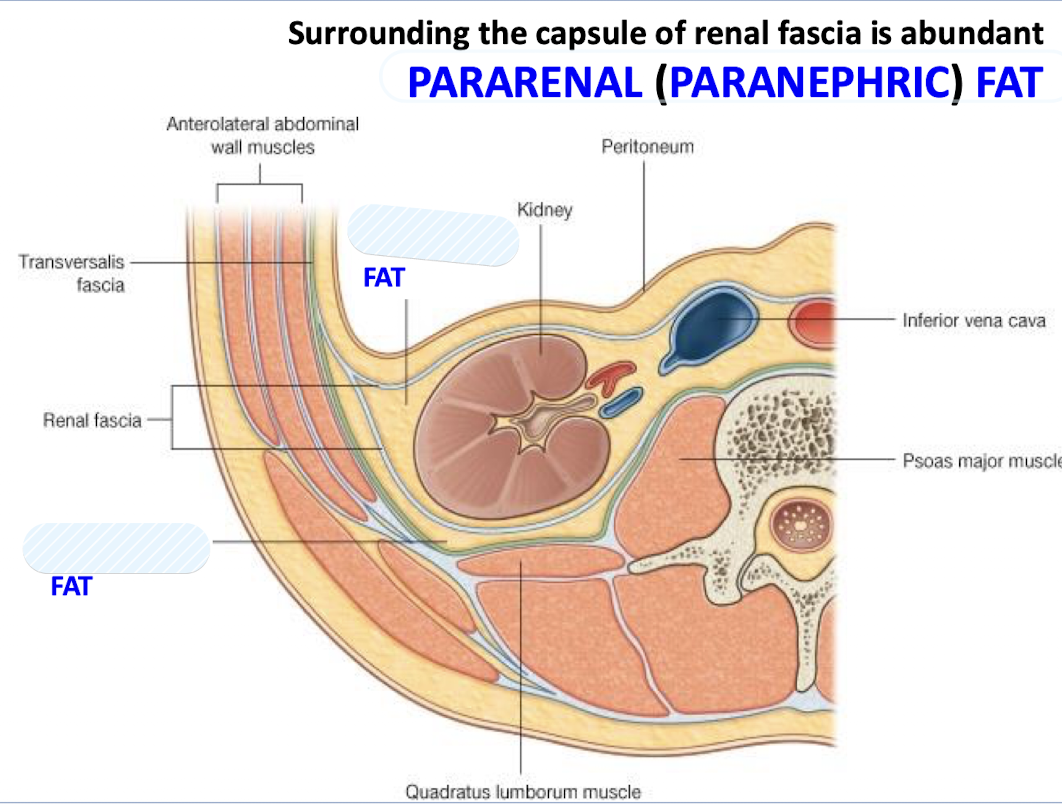
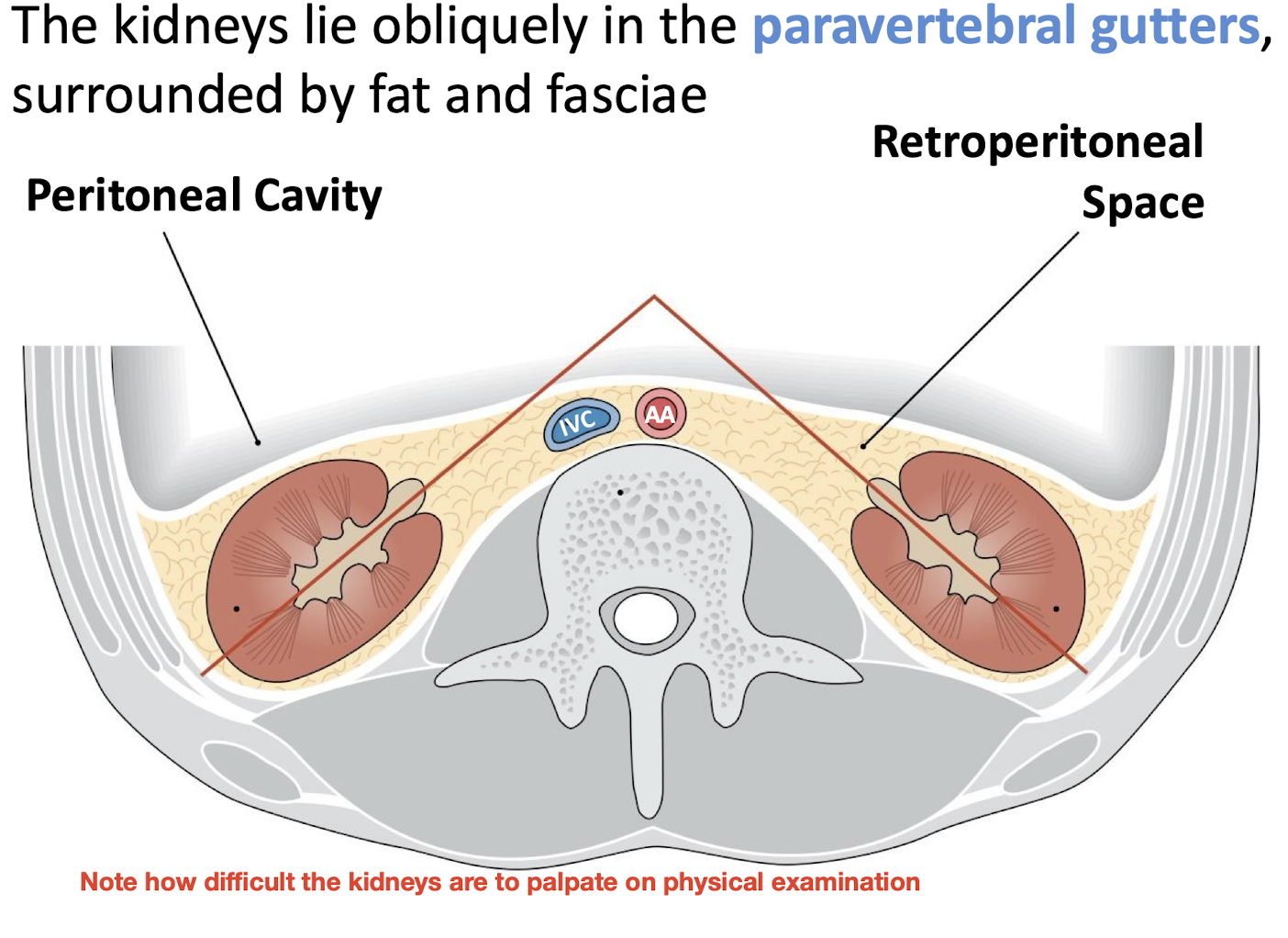
Where are the kidneys anatomically located
Obliquely in the paravertebral gutters; surrounded by fat and fasciae.
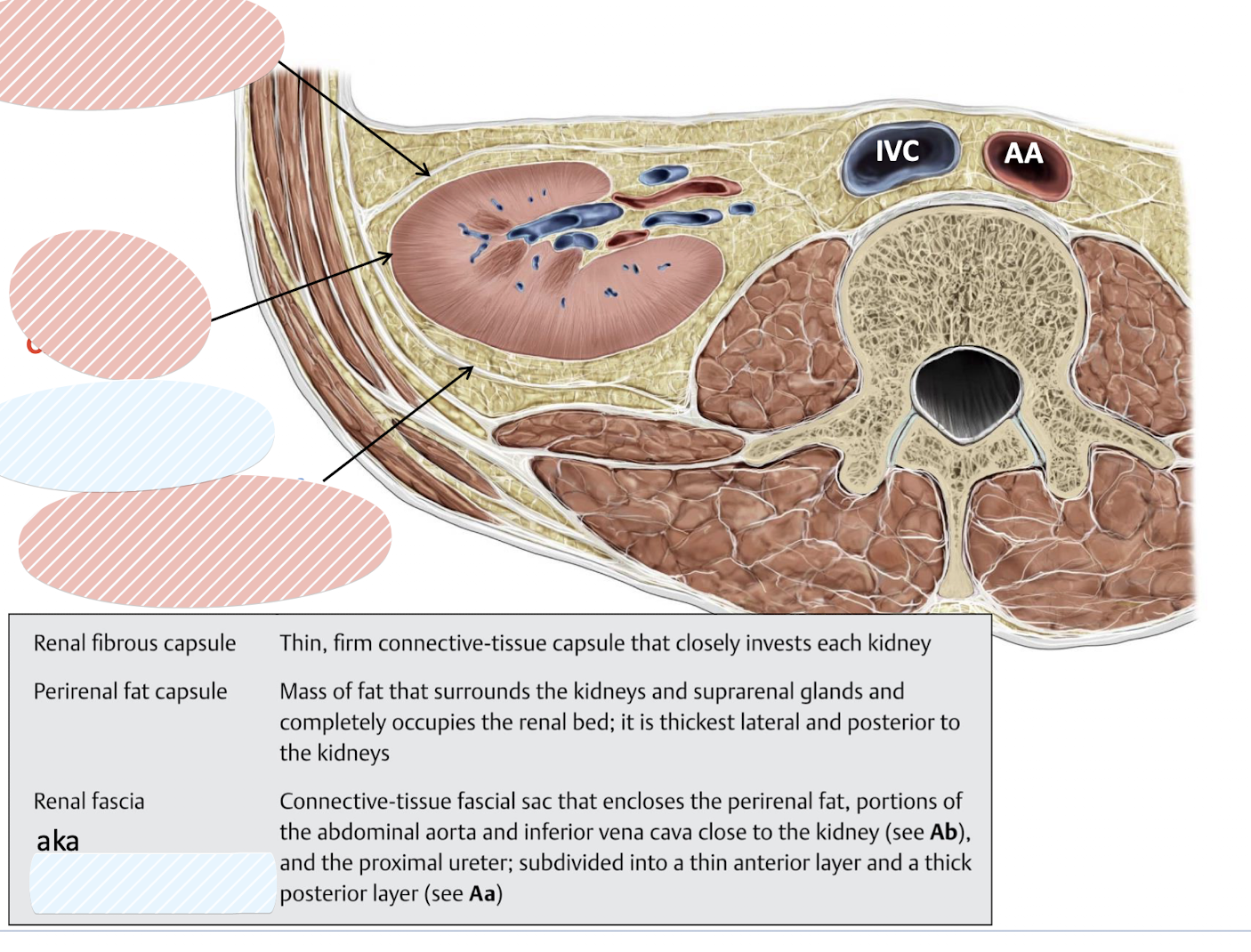
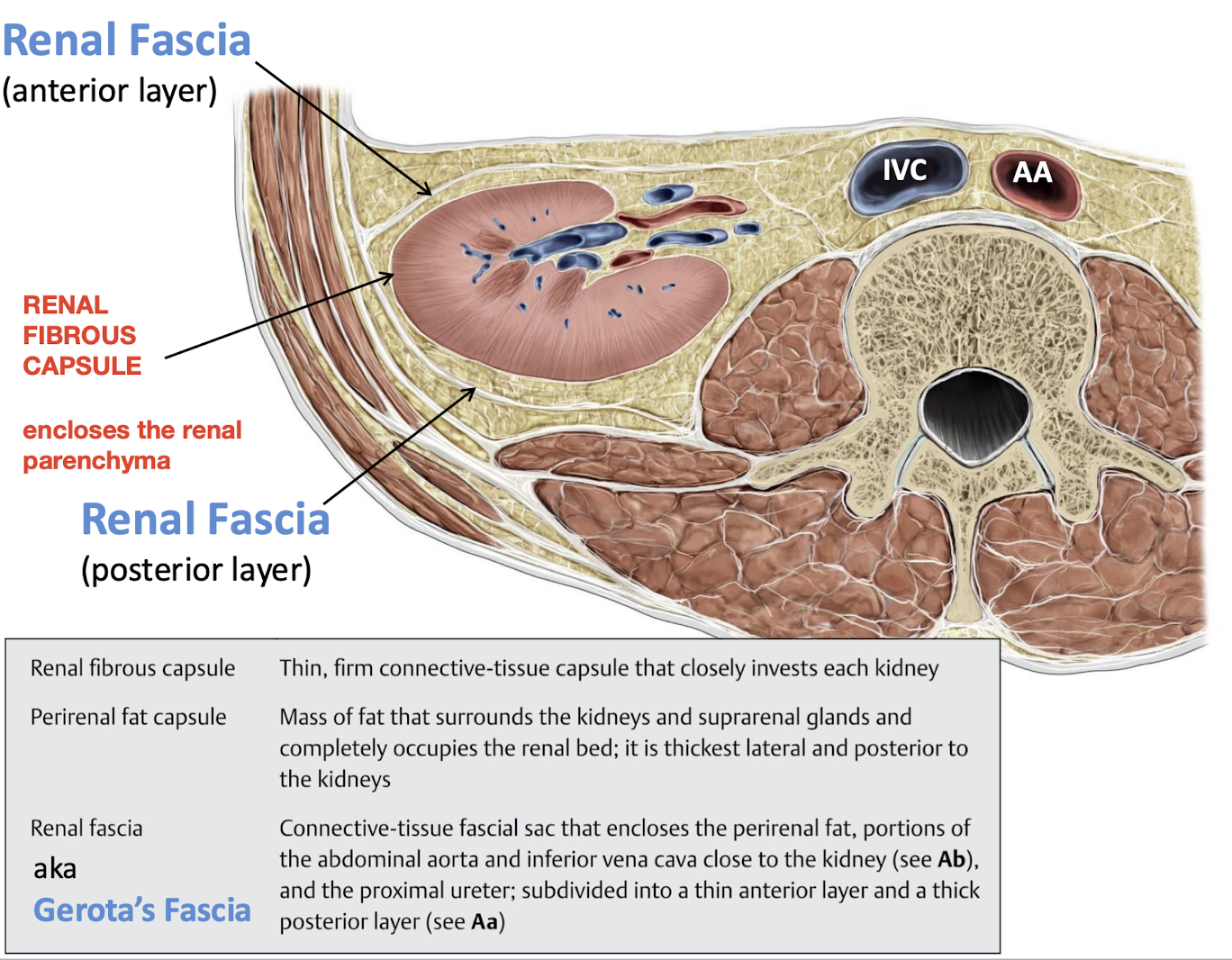
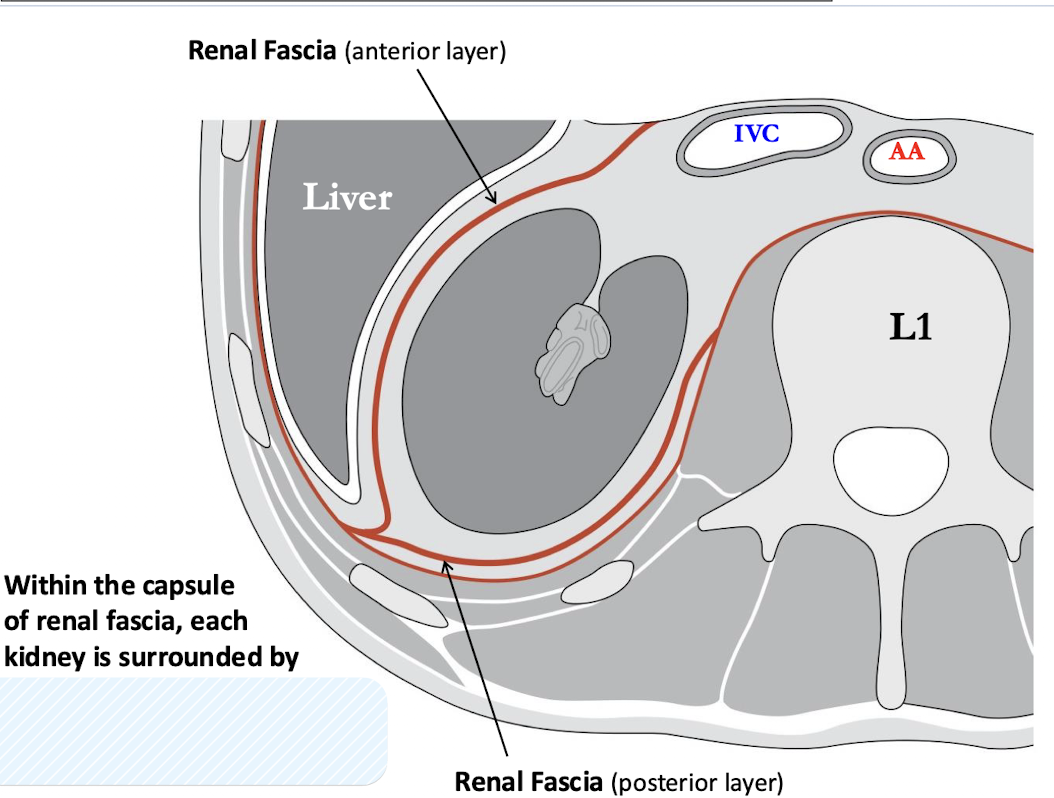
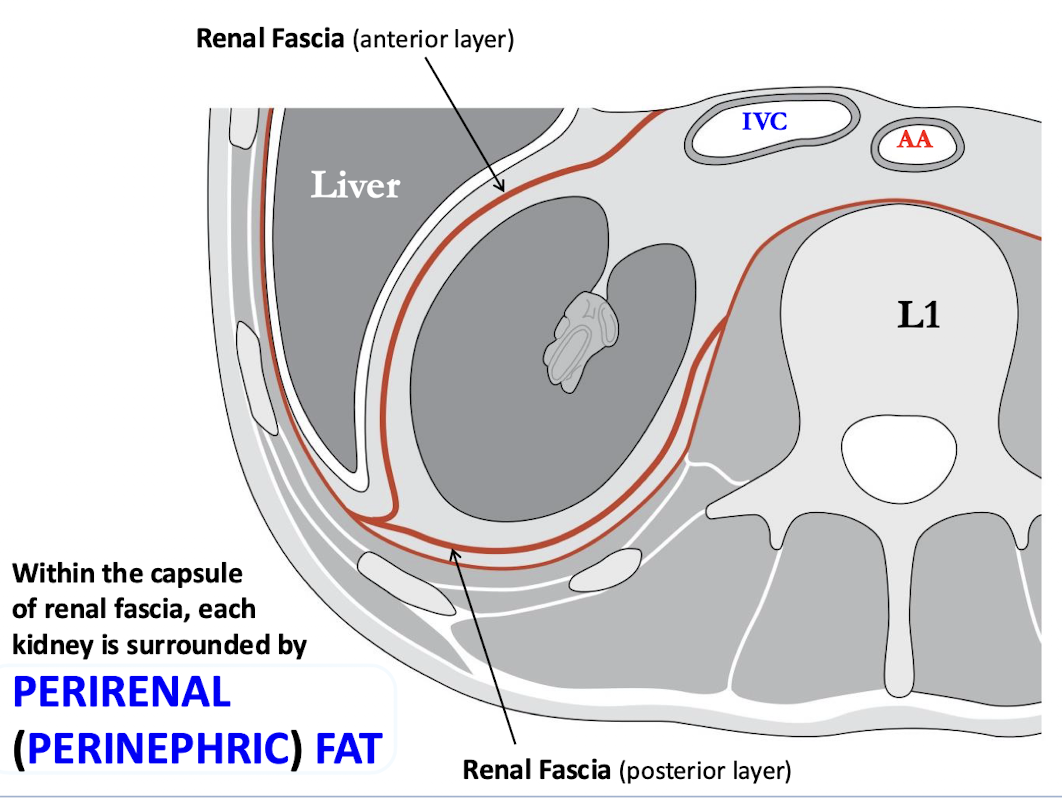
Renal Fascia aka Gerota’s Fascia