PHR 946 - Block 1: Hypertension, Diuretics, Antihypertensives
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
blood pressure
determined by the amount of blood the heart pumps and the resistance to blood flow in the arteries
- ↑ blood from heart = narrowing of lumen of the arteries
hypertension
high blood pressure
- long term force of the blood acting on artery walls
- becomes high enough to produce vascular/ tissue damage
- contributes to heart and vascular disease
- if chronically untreated: contributes to other diseases such as stroke, aneurysm, myocardial infarction, heart failure
HTN numbers
- normal: < 120/80 mmHg
- elevated: systolic 120-129 AND diastolic < 80 mmHg
- stage 1: systolic 130-139 OR diastolic 80-90 mmHg
- stage 2: systolic 140+ OR diastolic 90+
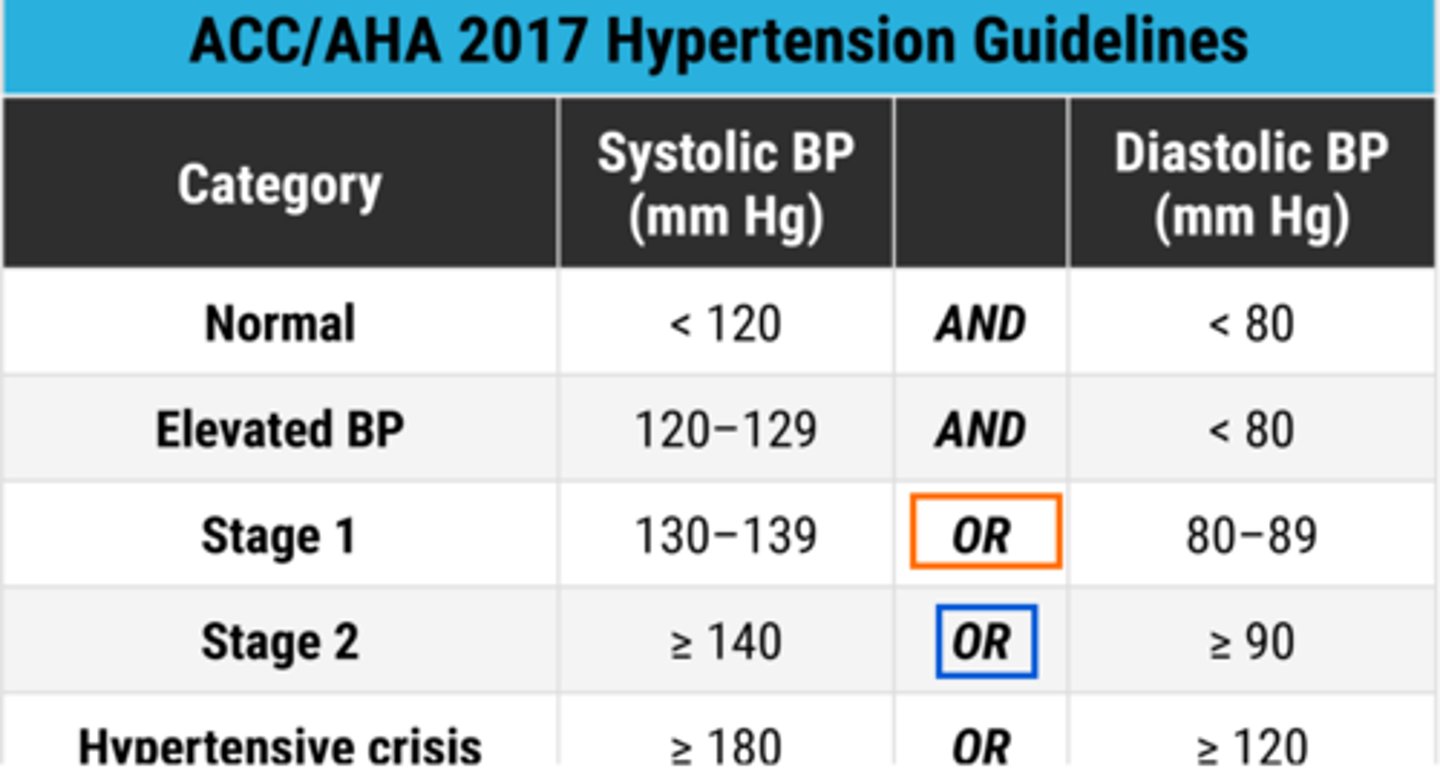
HTN symptoms
- most have no readily observable S&S
> just consistently high BP and mild headache
> many do not know they have high BP
- hypertensive crisis (180+/120+)
> severe headache, confusion, agitation, seizures
> serious and immediately life threatening
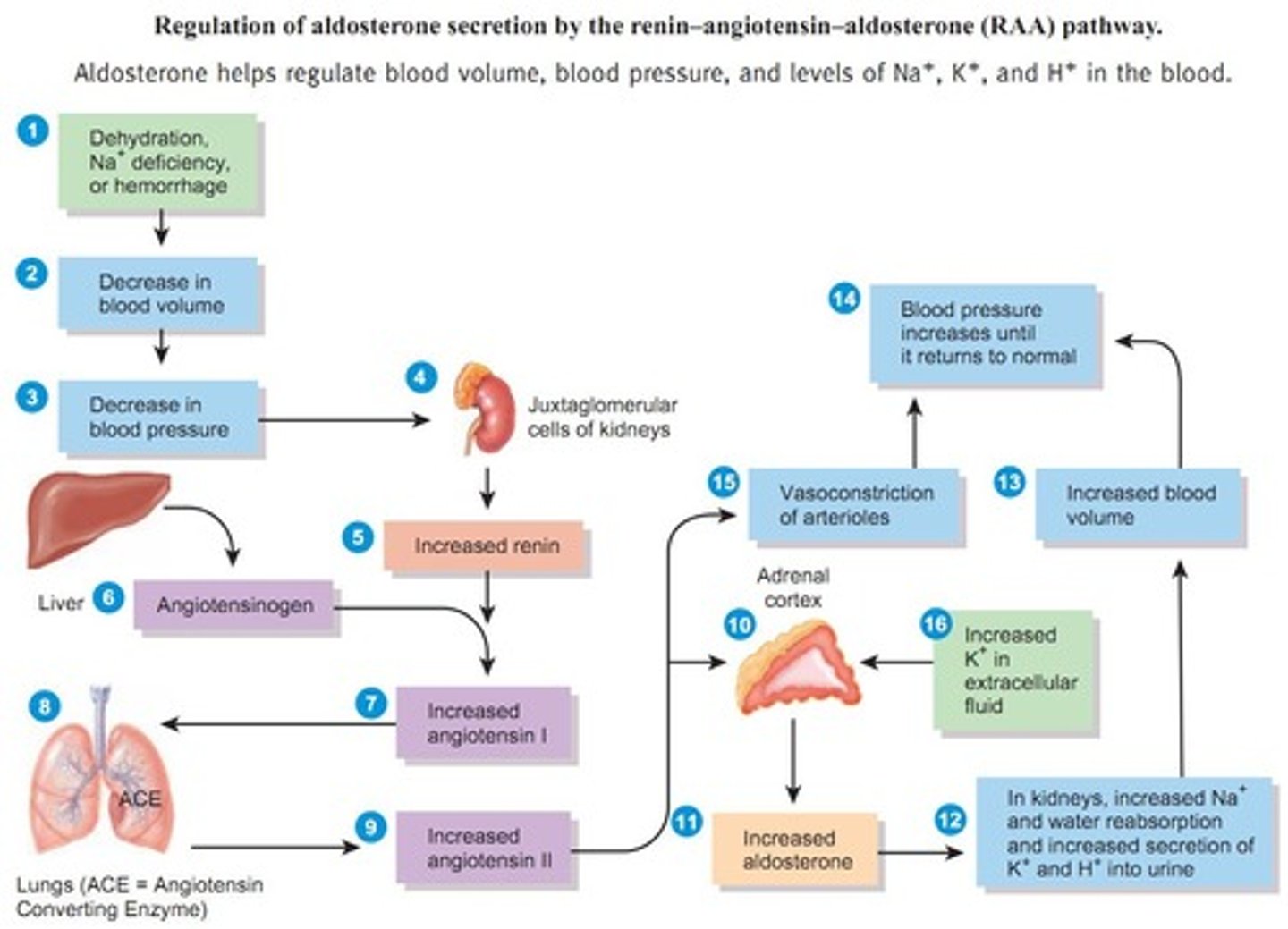
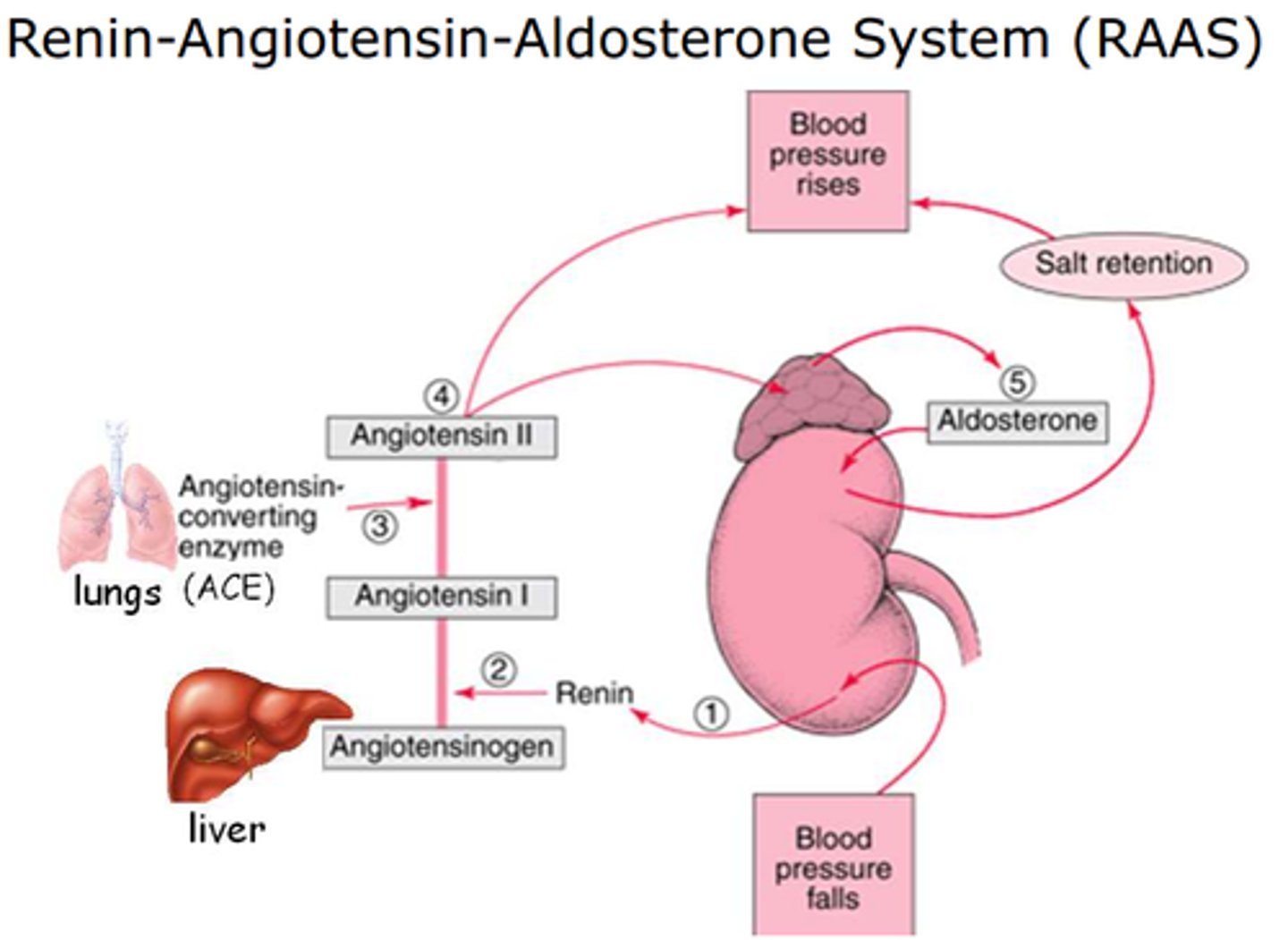
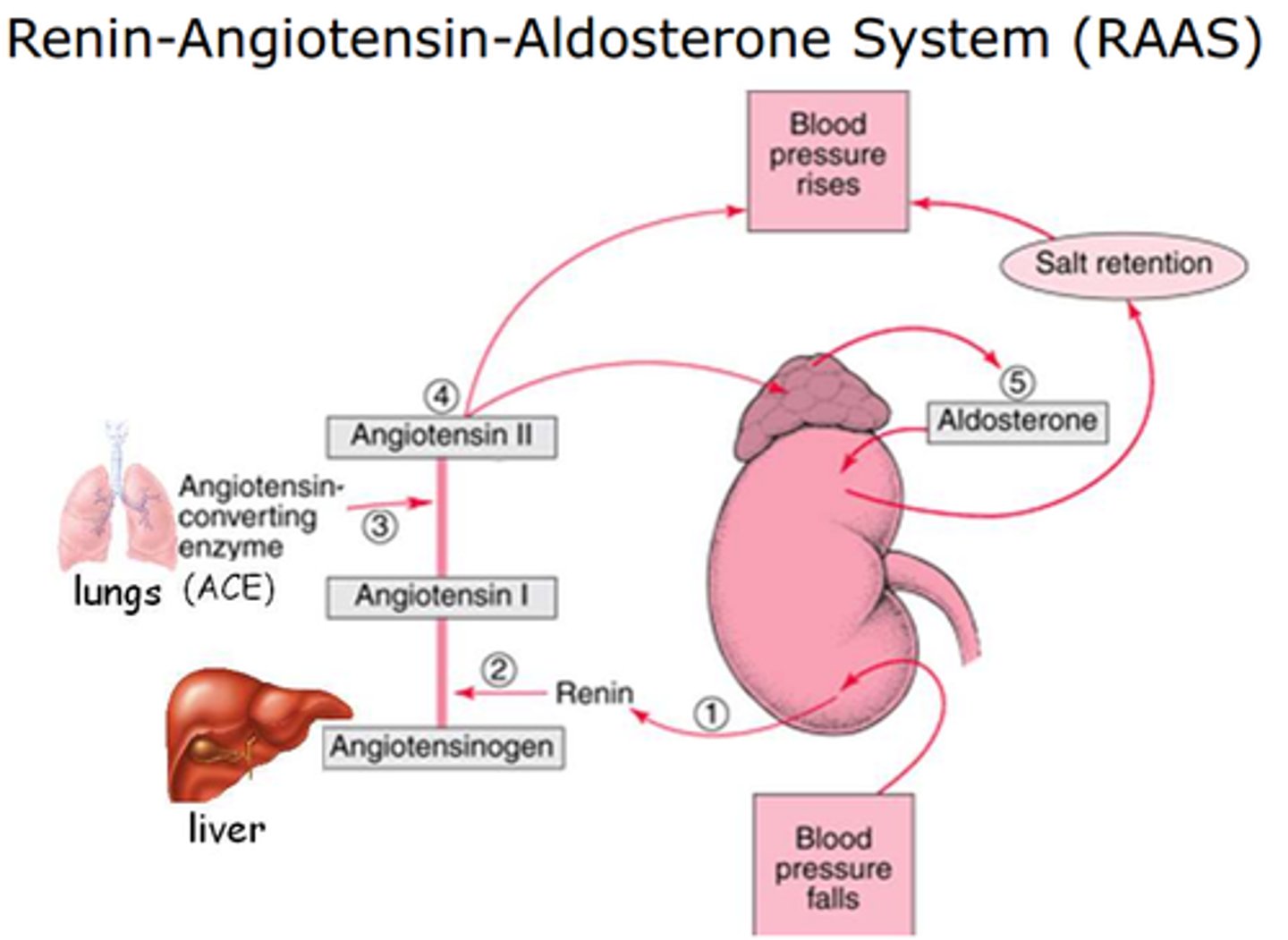
RAAS pathway
renin angiotensin (aldosterone) system
- raises BP by vasoconstriction and sodium/ water retention
- low bp / low renal perfusion → kidneys (juxtaglomerular cells) release renin
- renin: angiotensinogen → angiotensin I
- ACE (angiotensin converting enzyme): angiotensin i → angiotensin I
- angiotensin II: vasoconstriction + ↑ aldosterone
- aldosterone: ↑ sodium + water reabsorption → ↑ blood volume
- result: ↑ blood pressure and perfusion
primary HTN
- no identifiable cause
- 90% of cases
- contributing factors: genetic predisposition (diabetes, obesity, dyslipidemia, age, gender) and environmental factors (stress, smoking, obstructive sleep apnea, diet, alcohol)
- 3 types: moderate or high renin HTN, low renin HTN, resistant HTN
3 types of primary HTN
1. moderate or high renin HTN
- most common
- treated with anti-RAS medications (ACEis or ARBs)
2. low renin HTN
- plasma renin activity is 1/10 of high renin HTN
- treated with diuretics or calcium channel blockers
3. resistant HTN
- often requires 3+ medications
contributors to primary HTN
- impaired renal function
> kidneys fail to recognize and compensate for ↑ BP or volume expansion
> chronic kidney disease is prevalent in pre-HTN (GFR <60)
- excessive sympathetic activity
> stimulation of juxtaglomerular apparatus cells → excessive renin secretion
> leads to excessive AngII, aldosterone, and Na+ recovery causing increases in blood and extracellular fluid
> one treatment is ablation of renal efferent/ afferent nerves
secondary HTN
- occurs secondary to another disease
> need to treat underlying disease to control the HTN
- causes: renal or vascular disease, aldosterone dysfunction, Cushing's, pheochromocytoma, thyroid disease, some medications (steroids, amphetamines, MAOIs)
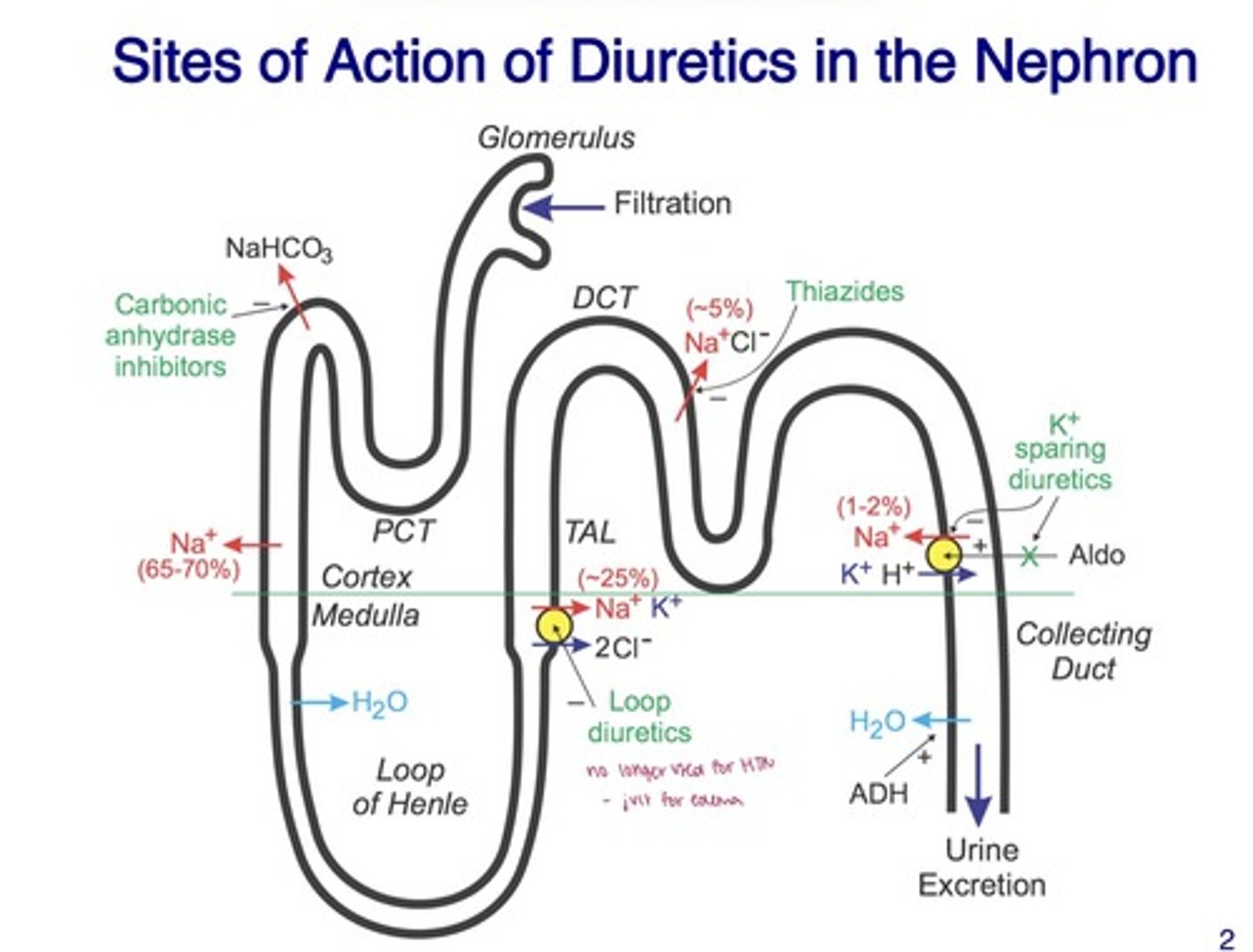
genetic component of HTN
- expression of mutants of a serine/ threonine kinase is associated with elevated BP
> results in elevated expression of the kinase, increasing BP in both hetero and homozygotes
- the kinase phosphorylates Na/K/2Cl transporter in the thick ascending loop of Henle (where loop diuretics target) AND Na/Cl transporter in the distal tubule (thiazide sensitive)
> both are activated, enhancing Na uptake out of the urine and increasing BP
- 20% with european ancestors carry a copy of the mutant gene
sites of action of diuretics in the nephron
carbonic anhydrase inhibitors
- proximal tubule
- ↓ H⁺ secretion → ↓ Na⁺ reabsorption → ↑ urine output
loop diuretics
- thick ascending limb of loop of henle
- inhibit Na⁺-K⁺-2Cl⁻ co-transporter
thiazide diuretics
- distal convoluted tubule
- inhibit Na⁺-Cl⁻ co-transporter
K⁺-sparing diuretics
- collecting duct
- block aldosterone or enaC → prevent K⁺ loss
thiazide diuretics
hydrochlorothiazide (HCTZ), chlorothiazide, indapamide, chlorthalidone
- developed from carbonic anhydrase inhibitors
- MOA: blocks the Na/Cl transporter in the distal convoluted tubule
> lowers BP 15-20 mmHg
- used for HTN (often 1st line!) and edema
- benefits: well tolerated, safe, inexpensive, reduces blood volume and ECF volume
- other effects: reduction in serum K+ (avoid in arrhythmias), reduced Ca++ excretion (avoid in hyperCa), reduced uric acid excretion (avoid in gout)
- ADE: hypoK+, hyperlipidemia, hyperuricemia, hyperglycemia (diabetes), hypersensitivity risk in sulfonamide allergies
thiazide PK
- most well absorbed
- onset within 2 hours (oral)
- dosage depends on potency
> chlorothiazide is oldest and least potent
- t1/2 is from 2 hours - 2 days
- most are renally cleared
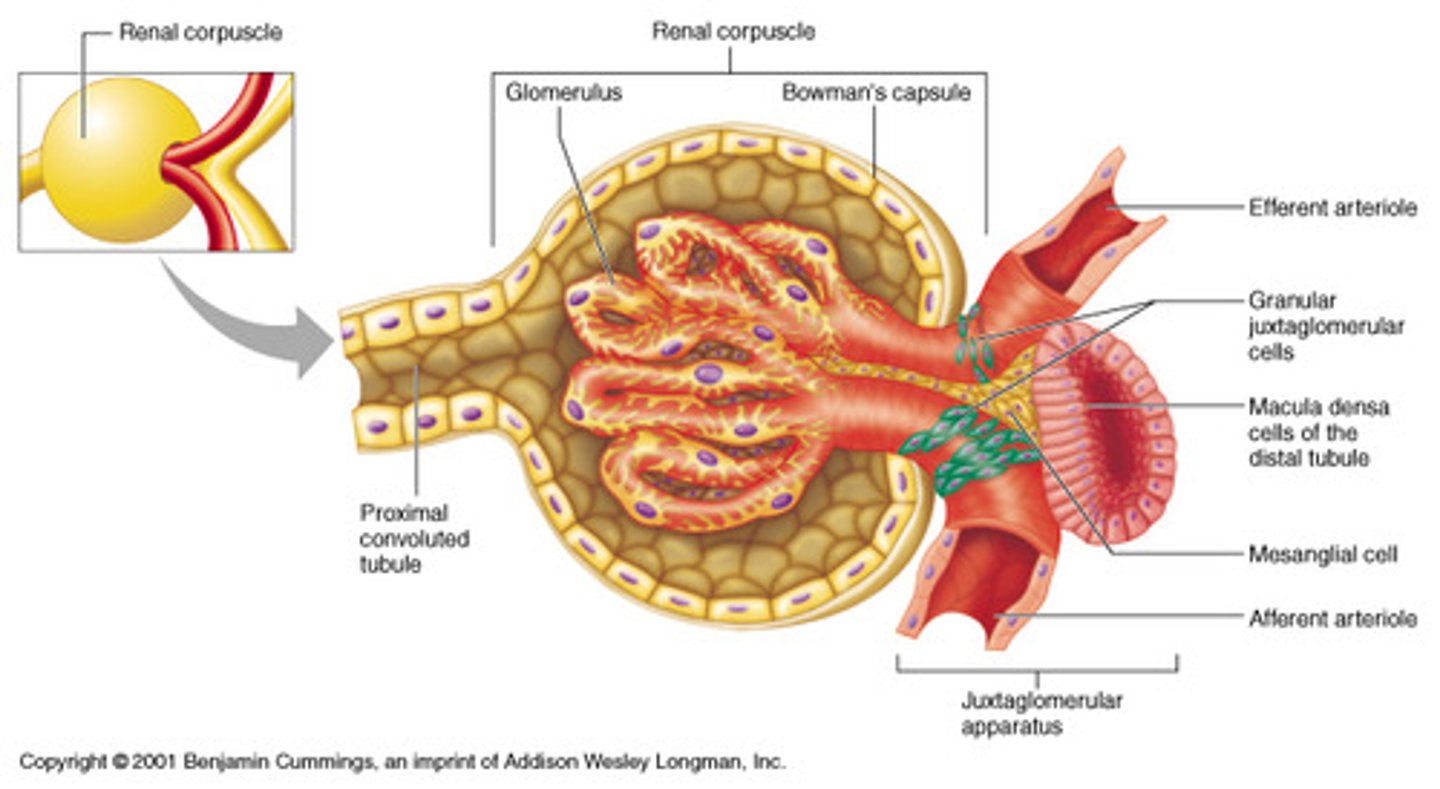
juxtaglomerular apparatus
- a group of cells located between the afferent and efferent arterioles, and the distal tubule in the nephron
- regulates: glomerular blood flow and filtrate rate, renin release
- low levels of filtrate / decreased NaCl delivery in the distal convoluted tubule causes macula densa cells to send signals to the JG cells to stimulates release of renin & decrease release of adenosine (a a vasoconstrictor) that acts on the afferent arteriole
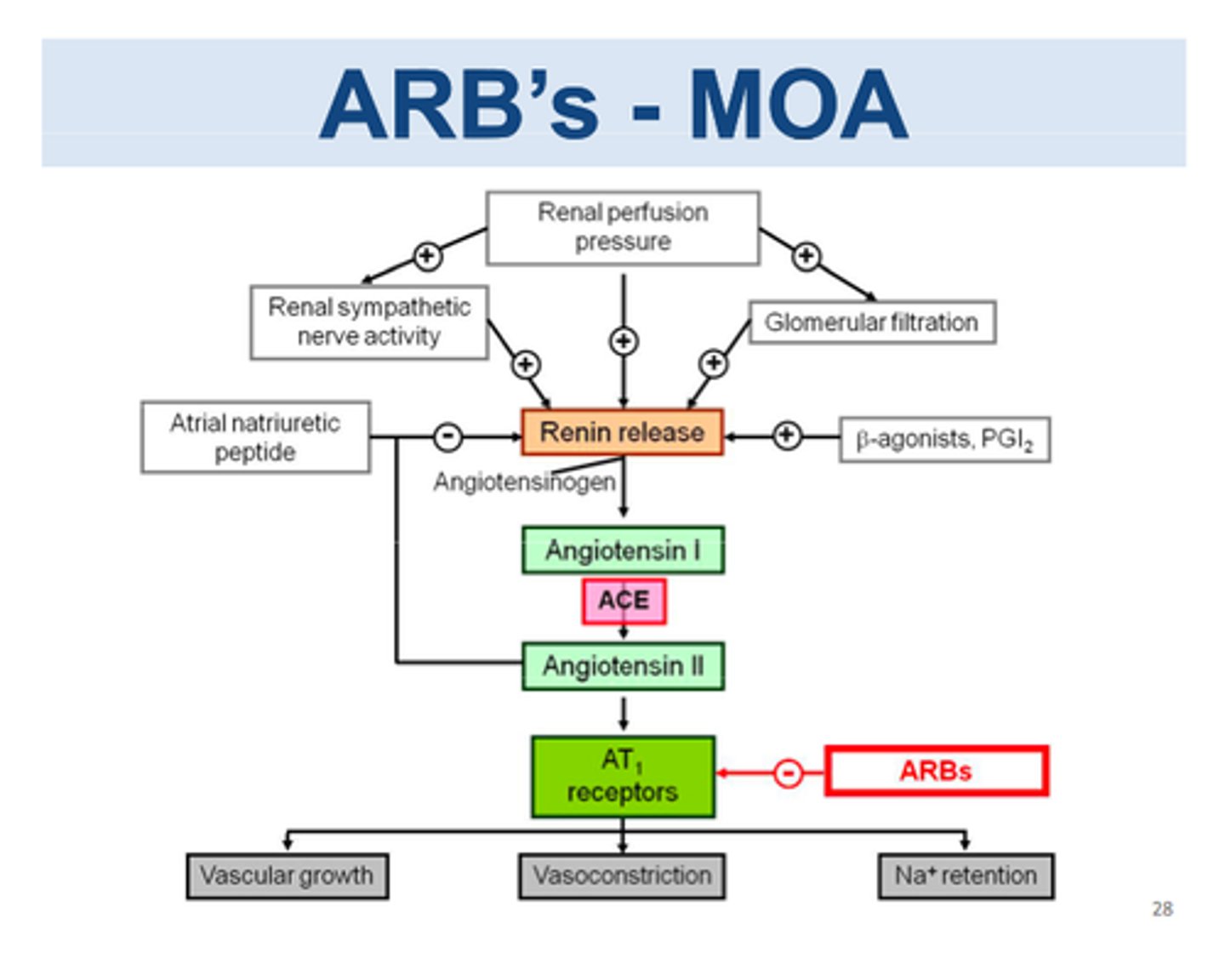
renin angiotensin system (RAS)
- renin is released into the blood by JG cells
> cleaves Ang to Ang I
- angiotensin converting enzyme (ACE) forms Ang II
> ACE is expressed in endothelial cells
> Ang II conserves Na+ and raises blood pressure
angiotensin
a peptide hormone that constricts blood vessels, causes the retention of sodium and water, and produces thirst and a salt appetite
- continually released from the liver
- renin cleaves Ang into 10 amino acids residues to form Ang (rate limiting step)
- once Ang I is formed, it is rapidly converted to Ang II
- Ang plasma levels increase by: corticosteroids, thyroid hormone, and inflammation
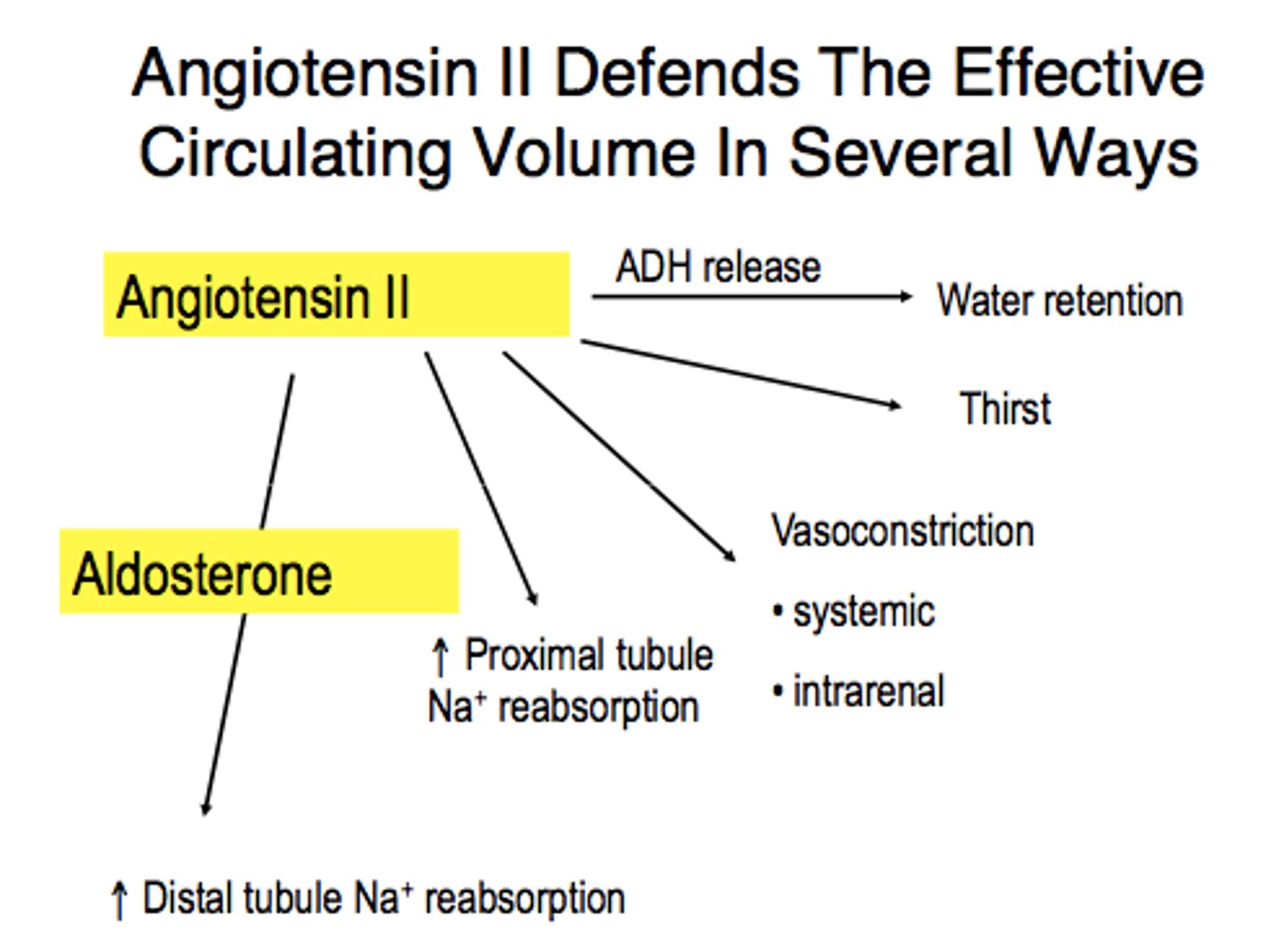
angiotensin II
a potent vasoconstrictor that raises BP
- increases aldosterone synthesis and secretion
- stimulates ADH release
- promotes Na+ reabsorption in the proximal tubule
- stimulates thirst center in hypothalamus
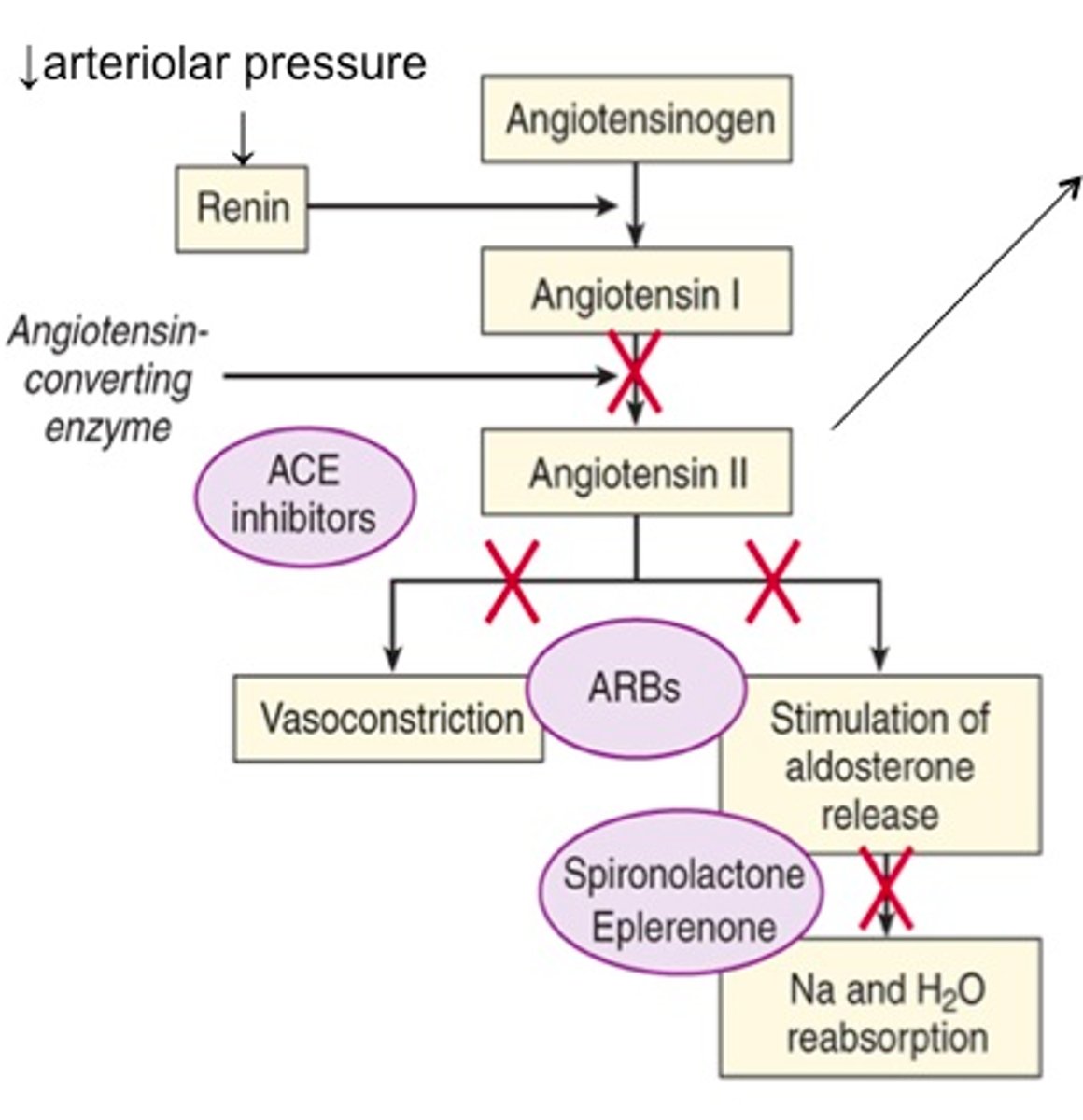
pharmacological targets in the renin-angiotensin pathway
renin
- conversion of Ang to Ang I
> released from kidney JG cells
> inhibitor: aliskiren (Tekturna)
angiotensin converting enzyme (ACE)
- cleaves Ang I to Ang II
> inhibitors: captopril, enalpril (Vasotec), fosinopril, lisinopril (Zestril), rampril
AT1 (Ang II receptor)
- most closely associated with hypertension
> inhibitors: losartan (Cozaar), candesartan (Atacand), valsartan (Diovan)
aliskiren
Tekturna
renin inhibitor antihypertensive
- MOA: direct renin inhibitor
> binds directly to catalytic site of renin and inhibits metabolic activity converting Ang to Ang I
- reduces plasma renin activity by ~60%
- lowers BP by ~10-15
- not recommended over ACEis or ARBs
- ADE: hyperkalemia, hypotension, fetal toxicity
- PK: poorly absorbed (take without food), t1/2 = 24 hrs
angiotensin converting enzyme (ACE)
converts Ang I to Ang II
- also degrades bradykinin (a vasodilator and airway smooth muscle constrictor)
- primarily located on luminal surface of endothelial cells in numerous tissues
- inhibition: decreases Ang II levels, increases bradykinin levels, increases vasodilation
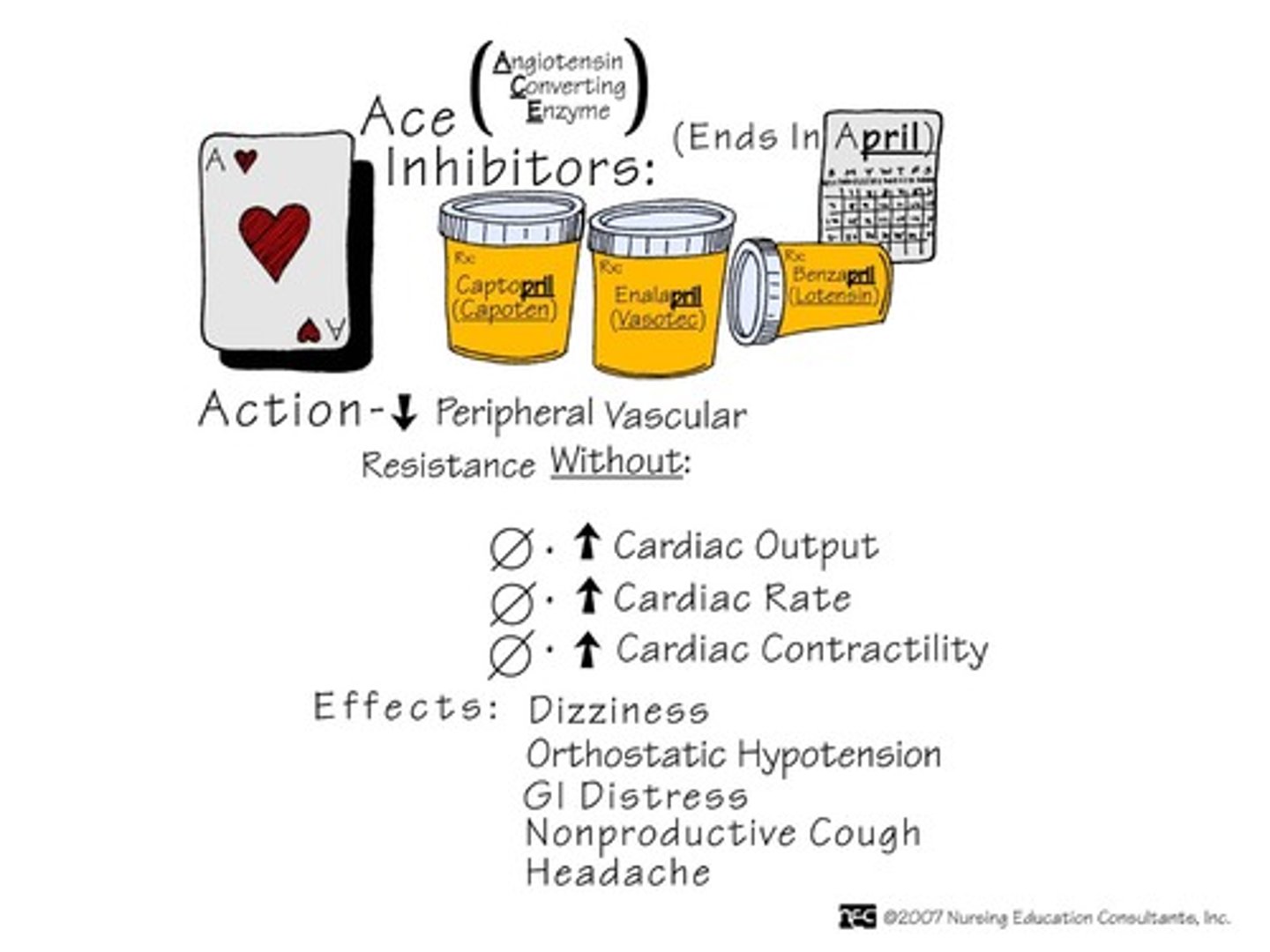
ACE inhibitors
angiotensin converting enzyme inhibitors
captopril, enalapril, lisinopril (-pril)
- MOA: decreases conversion of Ang I to Ang II
> peripheral arteriolar vasodilation and increased large artery compliance
> also reduces aldosterone secretion
- often used for monotherapy, or can be combined with a diuretic or other antiHTN
- ADE: hypotension (start w lower dose), persistent dry cough, angioedema, fetal toxicity, hyperkalemia, reduced renal function/ acute renal failure
- additional indications: heart failure, myocardial infarction w left ventricle dysfunction
angiotensin II receptors
2 types: AT1 and AT2
- both are G-protein coupled receptors (GPCR)
AT1:
- mediate most known effects of Ang II
> vasoconstriction, release of ADH, secretion of aldosterone
AT2:
- mediate vasodilation
angiotensin II receptor blockers (ARBs)
losartan, candesartan, valsartan (-sartan)
- MOA: antagonize Ang II receptors (AT1 with high affinity)
> essentially irreversible
- ADE: (lower than ACEis) cough, angioedema, detal toxicity, hyperkalemia
- additional indications: heart failure, CKD, post myocardial infarction
ACEis vs ARBs
- ARBs reduce activation of AT1 receptors more effectively than ACEis
- ARBs permit activation of AT2 receptors (these receptors mediate vasodilatory effects)
- ACEis increase bradykinin levels (a potentially beneficial vasodilator, but has ADE)
- both decrease systolic BP similarly ~10 mmHg
- both are less effective in low-renin HTN
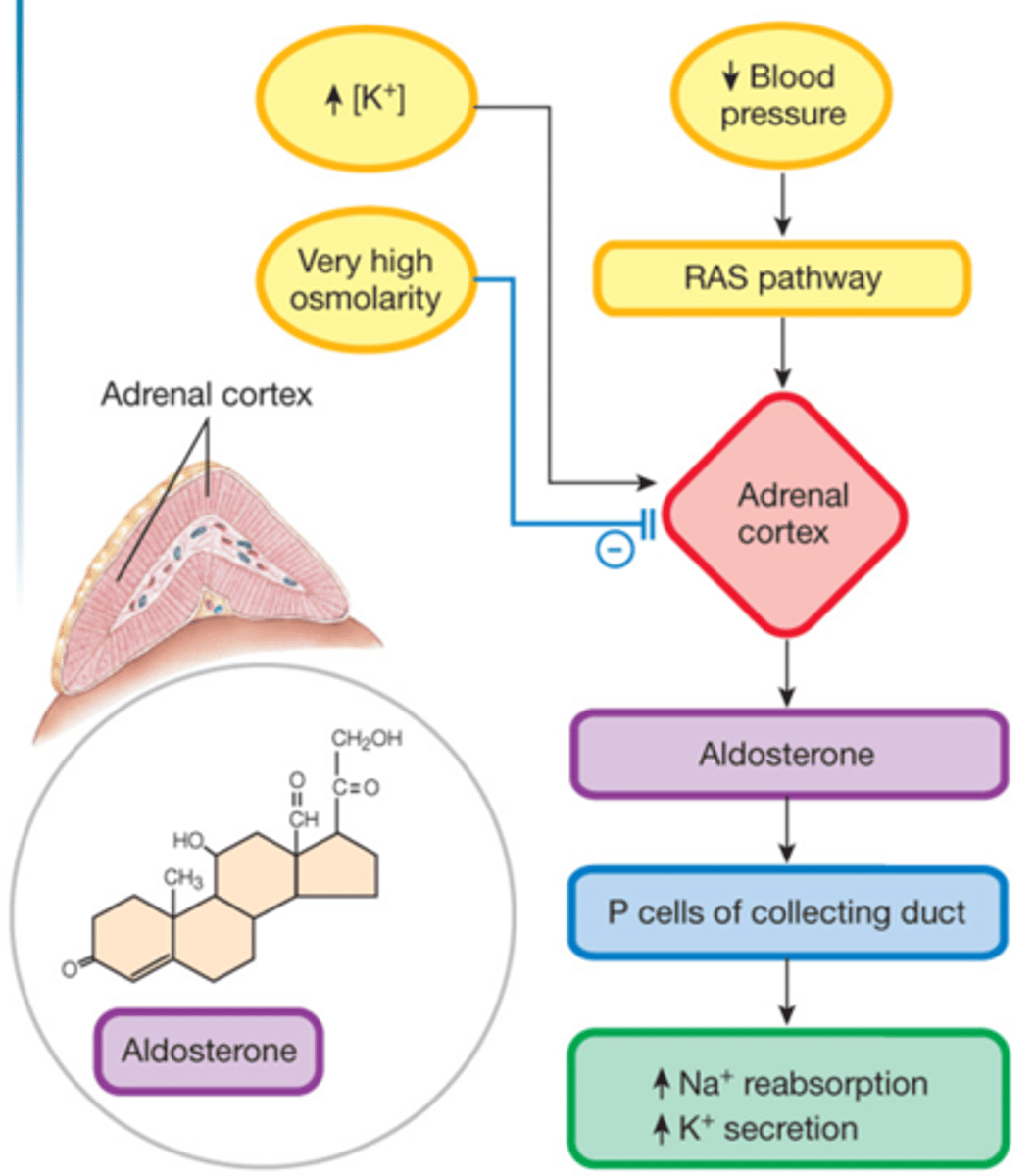
aldosterone
principal mineralocorticoid
- promotes recovery of Na in the late distal tubule and collecting duct
> Na retention = promotes water reabsorption
> promotes K loss in exchange for Na
- synthesized in: adrenal cortex (outermost)
- released in response to: Ang II, hypoNa, hyperK
aldosterone antagonists
spironolactone (Aldactone), eplerenone (Inspra)
- MOA: competitive antagonists of aldosterone at the mineralocorticoid receptor
- used for: HTN unresponsive to other therapies
- ADE: hyperK; activates progesterone and estrogen receptors (spiro only)
- DDI (eplerenone): CYP3A4 inhibitors
- eplerenone has greater specificity for the MR
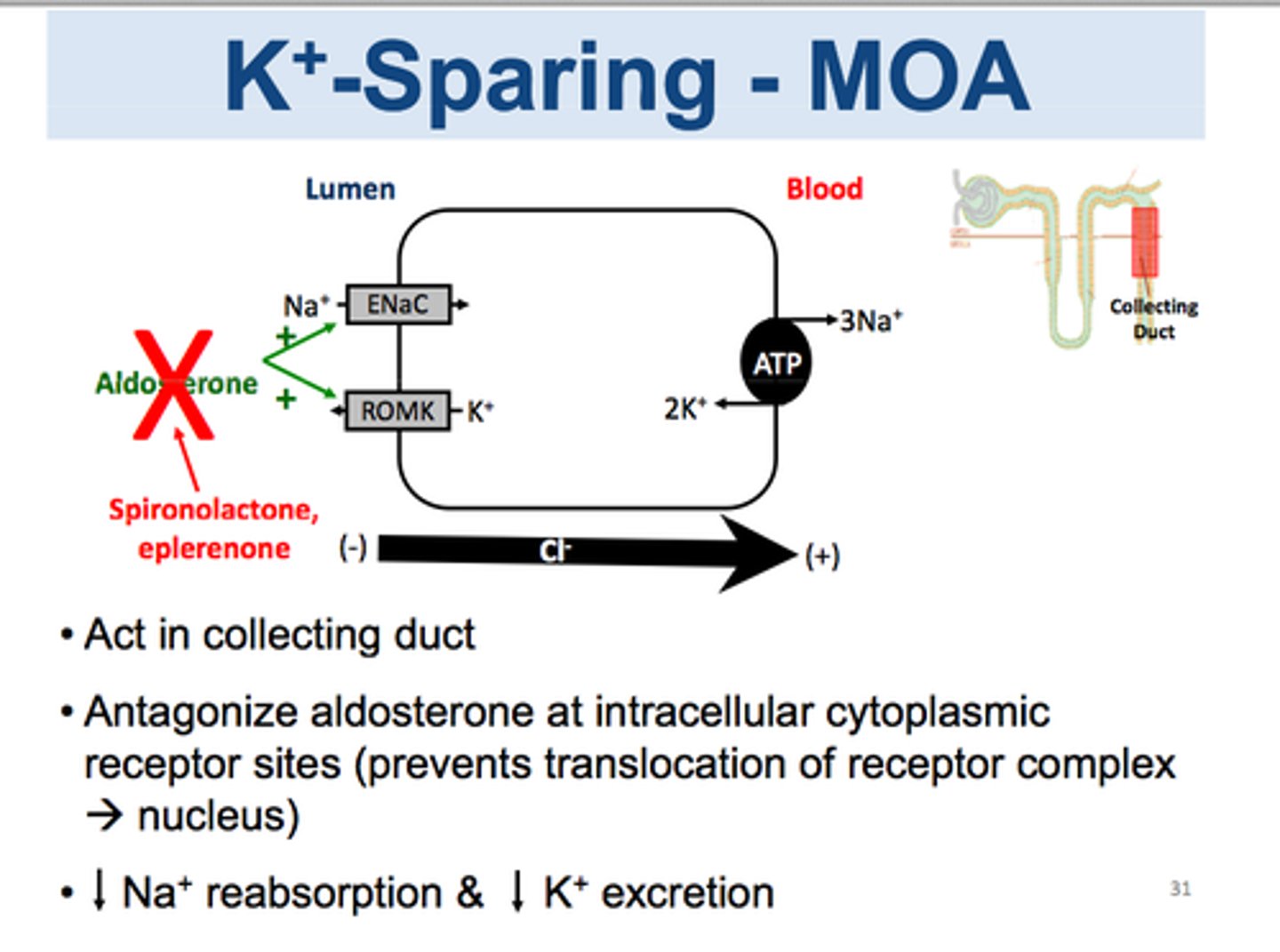
mineralocorticoid receptor (MR)
- MR is a member of the cytosolic steroid/ vit D/ thyroid receptor subfamily
- located in epithelial cells in the late distal tubule and collecting duct
- aldosterone binds to the MR receptor
- leads to increased expression and activity of the epithelial Na channel, increased Na entry into cells, and increased Na recovery into bloodstream
- increased K secretion occurs secondarily
limitations of aldosterone antagonists
- diuretic effectiveness depends on Na delivery to distal tubule and collecting duct
> normally a small amount (2%) of Na reaches this area
> aldosterone antagonists are most effective in combo with other diuretics that help more Na get to this point
- aldosterone antagonists aren't effective in the absence of circulating aldosterone
> diuretic effect = aldosterone levels
hyperkalemia with aldosterone antagonists
- monitor serum K prior to and during therapy
> renal insufficiency increases risk
- may increase hyperK effect of ACEis or ARBs
- K supplements are contraindicated
- avoid combo with other K sparing diuretics
amiloride
another less common K sparing diuretic
- MOA: inhibitor of epithelial Na channels
- [black box]: hyperkalemia
![<p>another less common K sparing diuretic</p><p>- MOA: inhibitor of epithelial Na channels</p><p>- [black box]: hyperkalemia</p>](https://knowt-user-attachments.s3.amazonaws.com/4d0277af-b64d-41d4-969b-607e3948cc74.jpg)
complications of uncontrolled HTN
- increased risk of heart disease and stroke
> leading causes of death in US
- effects on other organ systems (eyes, kidneys, peripheral vasculature)
causes of HTN
1. primary (essential)
- 90% of cases
- likely genetics and environmental factors
2. secondary
- obstructive sleep apnea
- SKD
- drug/ alcohol induced
- thyroid disorders
- primary aldosteronism
dietary factors: high Na, low K, low Ca, low Mg, low fruits/ veggies/ fiber, alcohol, caffeine
nondietary factors: genetics, obesity, low physical activity, obstructive sleep apnea, psychosocial stressors, air pollution
drugs/ substances that may raise BP
OTC
- alcohol
- caffeine
- decongestants (pseudoephedrine, phenylephrine)
- herbal (St Johns Wort)
- black licorice
- recreational drugs (cocaine, bath salts)
Rx
- sudden withdrawal of central-acting sympatholytics (clonidine, tizanidine)
- amphetamines
- antidepressants (MAOIs, SNRIs, TCAs)
- OCPs
- systemic corticosteroids
taking BP at home
- use an automatic, cuff-style, upper arm (bicep) monitor
> make sure it matches size of arm
> make sure it is a validated cuff
- avoid smoking/ caffeine/ exercise for 30+ minutes before
- empty bladder
- do not talk
- relax with legs uncrossed
- rest arm on table
diagnosing HTN
- normal: < 120/80 mmHg
- elevated: systolic 120-129 AND diastolic < 80 mmHg
- stage 1 HTN: systolic 130-139 OR diastolic 80-90 mmHg
- stage 2 HTN: systolic 140+ OR diastolic 90+
must have an average of 2+ readings taken on 2+ visits
- out of office measurements may help diagnose and guide treatment
baseline lab testing for pts with HTN
- complete metabolic panel (CMP)
- complete blood count (CBC)
- lipid profile
- hemoglobin A1C
- thyroid stimulating hormone (TSH)
- urinalysis
- urine albumin:creatinine ratio (UACR)
- 12-lead ECG
HTN lifestyle modifications
- weight loss: 5-10% of body weight
- healthy diet (DASH, Mediterranean)
- sodium restriction: <1500 mg/day
- adequate potassium: 3.5-5 g/day
- exercise: 150+ mins/week
- limit/abstain from alcohol and caffeine
when to treat HTN with drugs
1. treat stage II HTN ALWAYS (BP >140/90)
- add lifestyle modifications too
- 2 first line agents recommended (combo pill is best)
2. treat stage I HTN (>130/80) if pt has one of the following:
- clinical CVD (CAD, stroke, HF)
- CKD
- diabetes
- prevent-CVD risk of 7.5%+
if pt doesn't have one of the above, it is reasonable to initiate lifestyle modifications alone. start pharm treatment if not at goal after 3-6 months of lifestyle modifications
- 1 first line agent recommended
common first line anti HTN agents
- ACE inhibitors (-prils)
- ARBs (-sartans)
- thiazide-type diuretics (-thiazide, -thalidone)
- dyhydropyridine CCB (-ipines)
choosing a 1st line option
- a single antihypertensive will lower systolic BP by ~8-10 mmHg
choose based on:
- side effect profile
- DDIs
- prior antihypertensive trials
- cost, medication access
- compelling indications*
compelling indications
1. chronic kidney disease (CKD)
- eGFR <60 mL/min or UACR >30: ACEi or ARB
- CKD I or II with no albuminuria: any 1st line agent
2. diabetes
- eGFR <60 mL/min or UACR >30: ACEi or ARB
- most patients: any 1st line agent
3. heart failure (HFrEF)
- beta blockers, ACEi, ARB, ARNI, spironolactone, or isosorbide (some pts) are all favored due to improving morbidity and mortality in heart failure
4. stroke
- thiazide-type diuretic
- ACEi or ARB
blood pressure treatment goal and follow up
<130/80 mmHg for all adults
- encouragement to get SBP <120, esp in high risk CV patients
- exceptions: limited predicted lifespan, pts with symptomatic hypotension, pregnancy
initiate non-pharm agent and antihypertensive agent, then reassess in 1 month
- if BP goal met: reassess in 3-6 months
- if BP goal not met: assess and optimize adherence + consider intensification of therapy
HTN special populations
older adults
- goal is the same for most (<130/80)
- consider individualized/ relaxed goals for those with: limited life expectancy, high frailty, significant comorbidities, difficulty tolerating treatment
- older adults may experience more side effects with intensive therapy
- consider: combo therapy, pill burden, polypharmacy
pregnancy
- goal is <140/90
- any higher is hypertensive disorders of pregnancy
> chronic HTN (before 20 wks), gestational HTN (after 20 wks), preeclampsia
- 1st line: labetalol, nifedipine XR
- 2nd line: methyldopa, HCTZ, hydralazine
- AVOID: ACEi, ARB, MRA
antihypertensives monitoring and considerations
1. ACEis and ARBs
monitoring:
- hypotension
- BMP/ CMP for: hyperK, Scr increase
considerations:
- avoid in pregnancy
- do not use if hx of angioedema
- do not use ACEi and ARB together
- if cough with ACEi, change to ARB
2. thiazide diuretics
monitoring:
- hypotension
- BMP/ CMP for: hypoK, hypoNa, hypoMg, Scr increase
- uric acid increase (in pts with history)
considerations:
- photosensitivity
3. CCBs
monitoring:
- hypotension
- no routine monitoring
considerations:
- may cause dose related lower extremity edema
hypotension
BP <90/60 mmHg
- symptoms (if present): dizziness, lightheaded, nausea, fainting, confusion, blurry vision
- orthostatic hypotension: sustained reduction in SBP of at least 20 mmHg or BP of at least 10 mmHg within 3 minutes of standing
- causes: antihypertensives, diuretics
> important to adjust medication and drink water
intensification of therapy
options:
- titrate 1st med to max dose
- add a 2nd med
- do both
> typically wait to add a 3rd med until on max doses of 2 meds
in the real world:
- optimize adherence
- some providers will want more aggressive therapy than others
> need close follow up and individualized plan
resistant hypertension
BP above goal despite treatment with 3 antiHTN medications (including a diuretic) at max tolerated doses
OR
BP at goal but requiring 4+ medications
- exclude pseudoresistance (white coat syndrome, adherence)
- identify & reverse contributing modifiable life factors (obesity, inactivity, alcohol, salt intake)
- stop/ minimize interfering substances (NSAIDs, decongestants, estrogen, amphetamines)
- screen for secondary HTN causes
managing resistant HTN
1st line: mineralocorticoid receptor antagonist (MRA)
- spironolactone or eplerenone
other options:
- amiloride, beta blockers, alpha blockers, central sympatholytic drugs, dual endothelin receptor antagonists, direct vasodilators
mineralocorticoid receptor antagonists (MRA)
spironolactone (Aldactone) and eplerenone (Inspra)
monitoring:
- hyperK, hypoNa
- BMP / CMP within 1 week to monitor K
> do not initiate if K ≥ 5, d/c if K >5.5
- increased Scr
> avoid in eGFR <30 or Scr >2.5
- gynecomastia and impotence (spiro)
- AVOID in pregnancy
additional antihypertensive options
beta blockers
- carvedilol, labetolol, metoprolol, bisoprolol
- alpha / beta activity
- preperred in pts with bronchospastic airway disease
- ADE: bradycardia, hypotension, fatigue, depression, reflex tachycardia if abrupt d/c
K sparing diuretics
- amiloride, triamterene
- not very effective as monotherapy
- monitor K close
loop diuretics
- bumetanide, furosemide, torsemide
- preferred in symptomatic HF and moderate-severe CKD
direct vasodilators
- hydralazine, minoxidil
- ADE: fluid retention, postural hypotension, angina, reflec tachycardia, drug induced lupus (hydr), hirsutism (minox)
alpha-1 antagonists
- doxazosin, prazosin, terazosin
- 2nd/ 3rd line in BPH
- ADE: orthostatic hypotension
alpha-2 antagonists/ central sympatholytic agents
- clonidine, methyldopa, guanfacine
- last line due to CNS effects
- ADE: rebound HTN, dizziness, dry mouth, constipation
direct renin inhibitor
- aliskiren
- ADE: hyperK
- AVOID in pregnancy; AVOID use with ACEi or ARB
dual endothelin receptor antagonist
- aprocitentan
- ADE: mild-moderate fluid retention
- AVOID in pregnancy
renal denervation
procedure to reduce renal sympathetic nerve activity
- a catheter is inserted into renal arteries and ablated to reduced release of hormones contributing to HTN
- lowers BP by 4-6 mmHg within 2-3 months
- reserved for adults w resistant HTN despite optimal treatment/ those who have intolerable side effects
hypertensive emergency
a situation in which blood pressure is severely elevated and there is evidence of actual or probable target organ damage
- if no target organ damage = severe HTN
target end organ damage:
- hypertensive encephalopathy
- intracranial hemorrhage
- ischmic stroke
- acute pulmonary edema
- cardiac ischemia (MI or unstable angina)
- aortic dissection
- acute renal failure
- eclampsia
concerning symptoms
- visual disturbances
- headache
- confusion
- weakness/ numbness of extremities
- shortness of breath
- edema
- sweating
- chest pain/ pressure
- referred arm or jaw pain
treating hypertensive emergency & severe HTN
hypertensive emergency
- admit to ICU
- use short acting or continuous IV medications
severe HTN
- no indication to send to ED or hospital
- do not need aggressive BP lowering
- intensification of oral regimen in outpatient setting
calcium channel blockers (CCB)
2 types: dihydropyridines (amlodipine, nicardipine, felodipine, nifedipine XL) and non-dihydropyridines (diltiazem, verapamil)
MOA: prevents calcium from exciting cardiac
and vascular smooth muscle, preventing
muscular contraction and promoting relaxation
- only L-type channel is sensitive to CCBs
- most effective in low-renin HTN
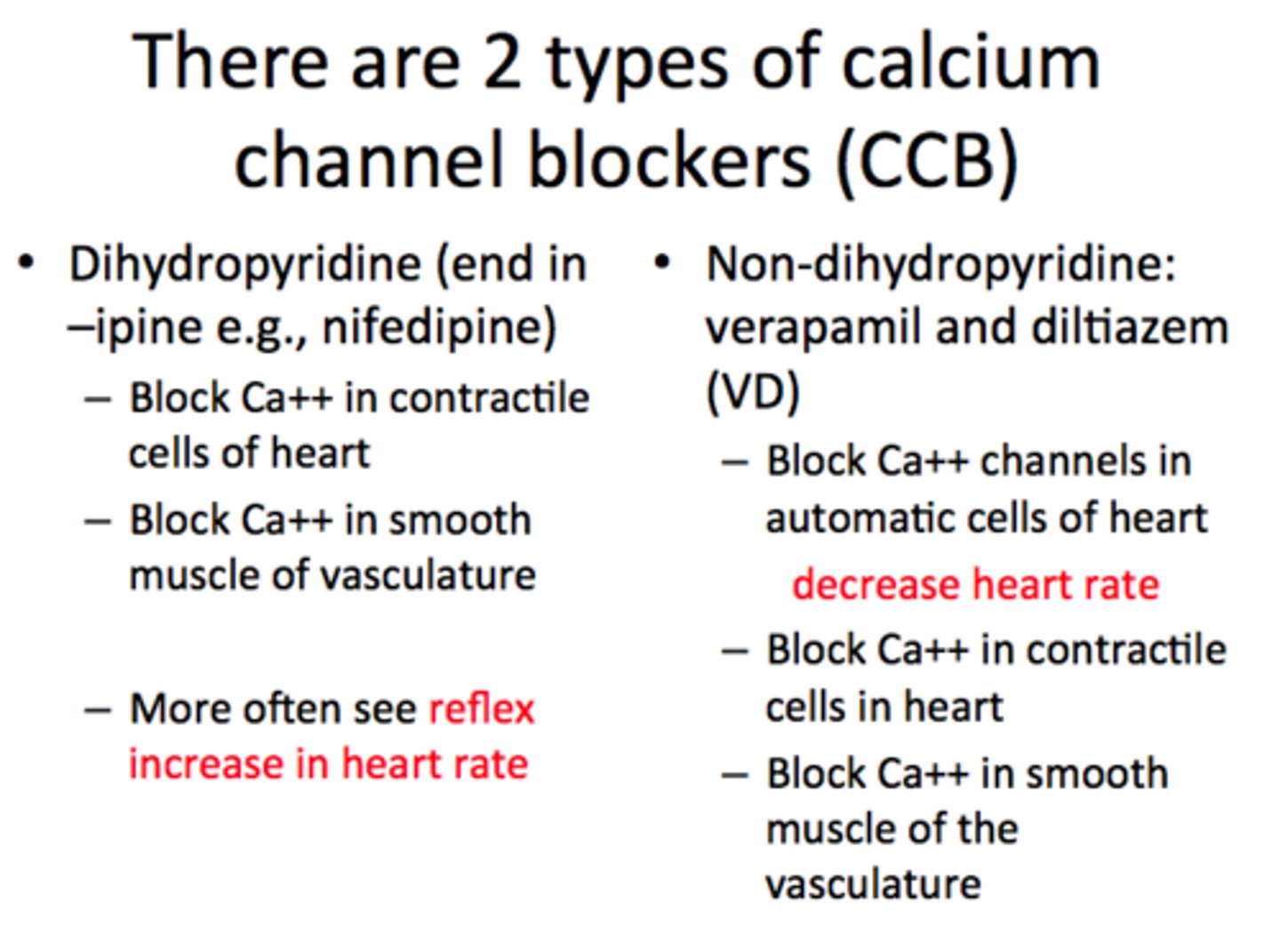
L-type voltage gated Ca++ channel
- made up of multiple subunits
- the voltage-sensitive subunit responds to depolarization of the cell, changing the conformation of pore-forming subunit
- dihydropyridines bind isoform expressed in arteries
- non-dihydropyridines bind isoform expressed in cardiac muscle and cardiac conduction cells
CCB pharmacological properties
decreased Ca++ entry into:
- vascular smooth cells (causes relaxation and arteriolar vasodilation)
- cardiac myocytes (decreases contractility of heart muscle and cardiac output)
- cardiac pacemaker cells (causes slowed conduction and decreased HR)
CCB PK
- well absorbed, but bioavailability is reduced by 1st pass
- highly protein bound
- t1/2 ranges from 3-50 hours
- rapidly absorbed CCBs = rapid BP reduction
- longer acting CCBs = slower onset of action
- can combine a dihydropyridine and non-dihydropyridine because they have different sites of actions
CCB ADE
dihydropyridines
- hypotensive effects (dizziness, headache, syncope)
- peripheral edema (lower legs, ankles)
> increases w higher doses
- mycocardial ischemia
non-dihydropyridines
- bradyarrythmias (verapamil)
- acute decompensated heart failure (verapamil)
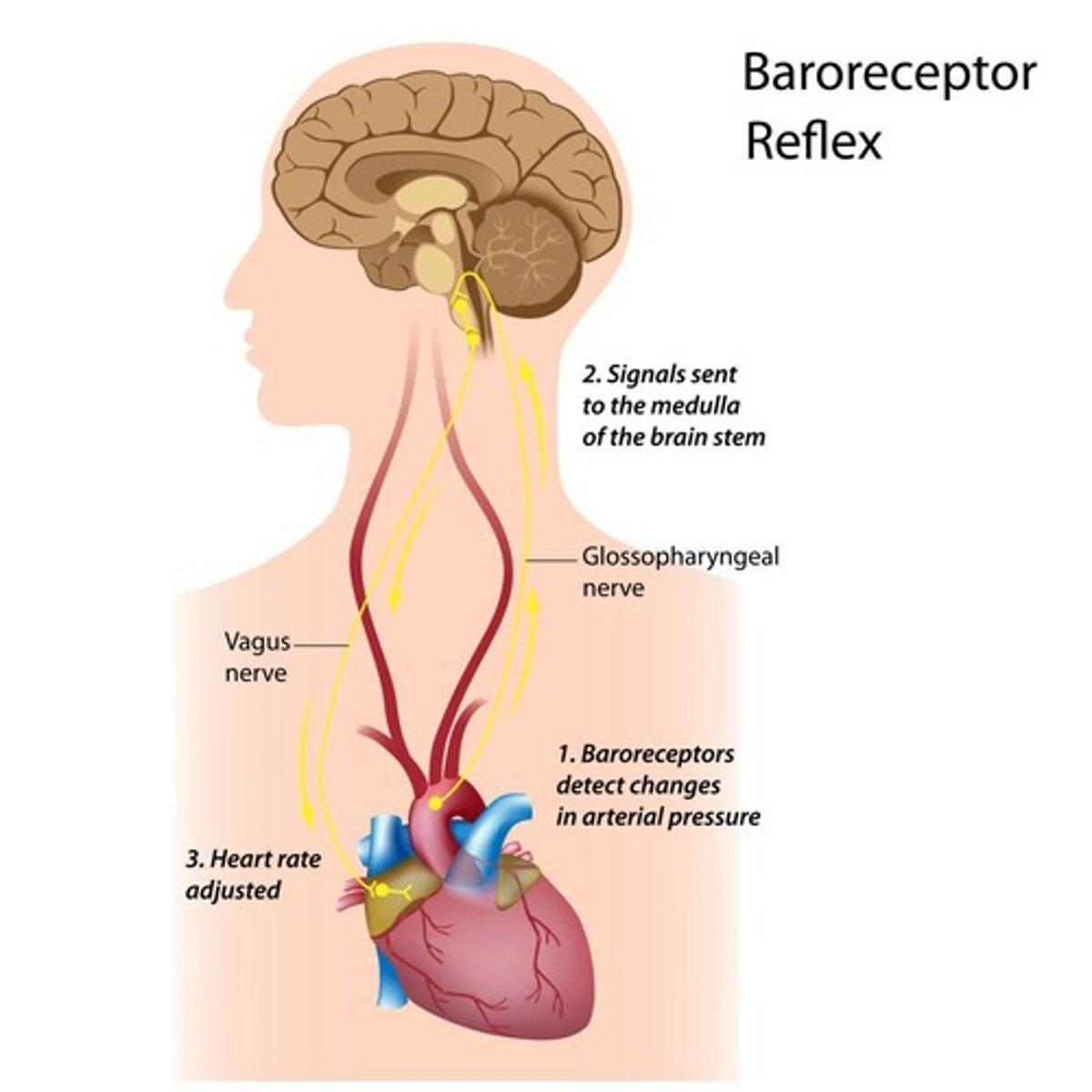
baroreceptor reflex
the primary reflex pathway for homeostatic control of blood pressure
- may cause reflex tachycardia and increase cardiac output (dihyropyridines, alpha-1 blockers, direct vasodilators)
sympatholytics
alpha-1-blockers (-zosins), beta-blockers (-lols), mixed alpha+beta blockers
- MOA: block adrenergic receptors & reduce sympathetic outflow from the CNS
> act on the central or peripheral nervous system
- not recommended as 1st line therapy for HTN
alpha-1-receptor antagonists
prazosin (Minipress), terazosin (Tezruly), doxazosin (Cardura)
- MOA: block the post-synaptic alpha-1-receptor
(alpha-1 receptors on vascular smooth muscle cause vasoconstriction)
> no effect on alpha-2 (NE) receptors
- not recommended for initial monotherapy, use when pt not well-controlled on other medications
- increased risk of HF compared to TZD
- may be used with other HTN drugs
alpha-1-receptor antagonists pharmacological effects
produces:
- arteriolar vasodilation and venodilation (blocks vasoconstricting alpha-1 receptors)
- postural hypotension (with first dose)
- inhibition of smooth muscle contraction
alpha-1-receptor antagonists PK, ADE, DDI
PK:
- t1/2: 3-20 hours
- dosing: 1x - 3x daily dosing
> start with low dose and titrate to desired BP. must restart titration if interrupted
- elimination: extensive hepatic metabolism
ADE:
- dizziness
- postural hypotension
DDI:
- other anti-HTN drugs: causes excessive fall in BP
beta-receptor antagonists
beta-1 selective: acebutolol, atenolol (Tenormin), betaxolol, metoprolol (Lopressor, Toprol XL), nebivolol (Bystolic)
non-selective: propranolol (Inderal), nadolol, timolol, carvedilol (Coreg), labetalol (Normodyne)
- effectiveness is independent of beta-1 selectivity
- heart has 80% beta-1 receptors and 20% beta-2 receptors
partial agonists with intrinsic sympathomimetic activity (ISA)
- produce less reduction in: heart rate, force of cardiac contraction, cardiac output, blood pressure
- for hypertension, generally avoid these (acebutolol, pindolol, labetalol)
vasodilating beta-blockers
carvedilol (Coreg), labetalol (Normodyne), nebivolol (Bystolic)
carvedilol
- non-selective
- reduces HR and CO, produces vasodilation to lower total peripheral resistance (TPR)
labetalol
- non-selective with ISA
- modest effect on reducing HR and CO
nebivolol
- highest specificity for beta-1 of any blocker
- beta-3 adrenergic receptor antagonist: activates NO synthase in endothelial cells = vasodilation and relaxation of smooth muscle cells
beta-blockers
- bronchoconstriction (only beta-1 selective agents are safe in COPD)
- bradycardia
- HF patients may not tolerate initial drop of cardiac output
- insulin-dependent diabetes (masks sympathetic nervous system accompanying hypoglycemia)
- CNS effects (fatigue, dizziness, depression)
- [black box]: abrupt withdrawals = cardiac ischemic in pts with ischemic heart disease
centrally acting alpha-2 agonists
clonidine (Catapres), guanfacine (Intuniv)
- MOA: decreased BP by reducing sympathetic outflow
> act by presynaptic alpha-2 stimulation to decreased central NT release
ADE: hypotension, bradycardia, withdrawal syndrome w sudden d/c, seddation, lethargy, depression, tachycardia, excessive BP
- generally last line therapy for resistant HTN, has significant CNS adverse effect
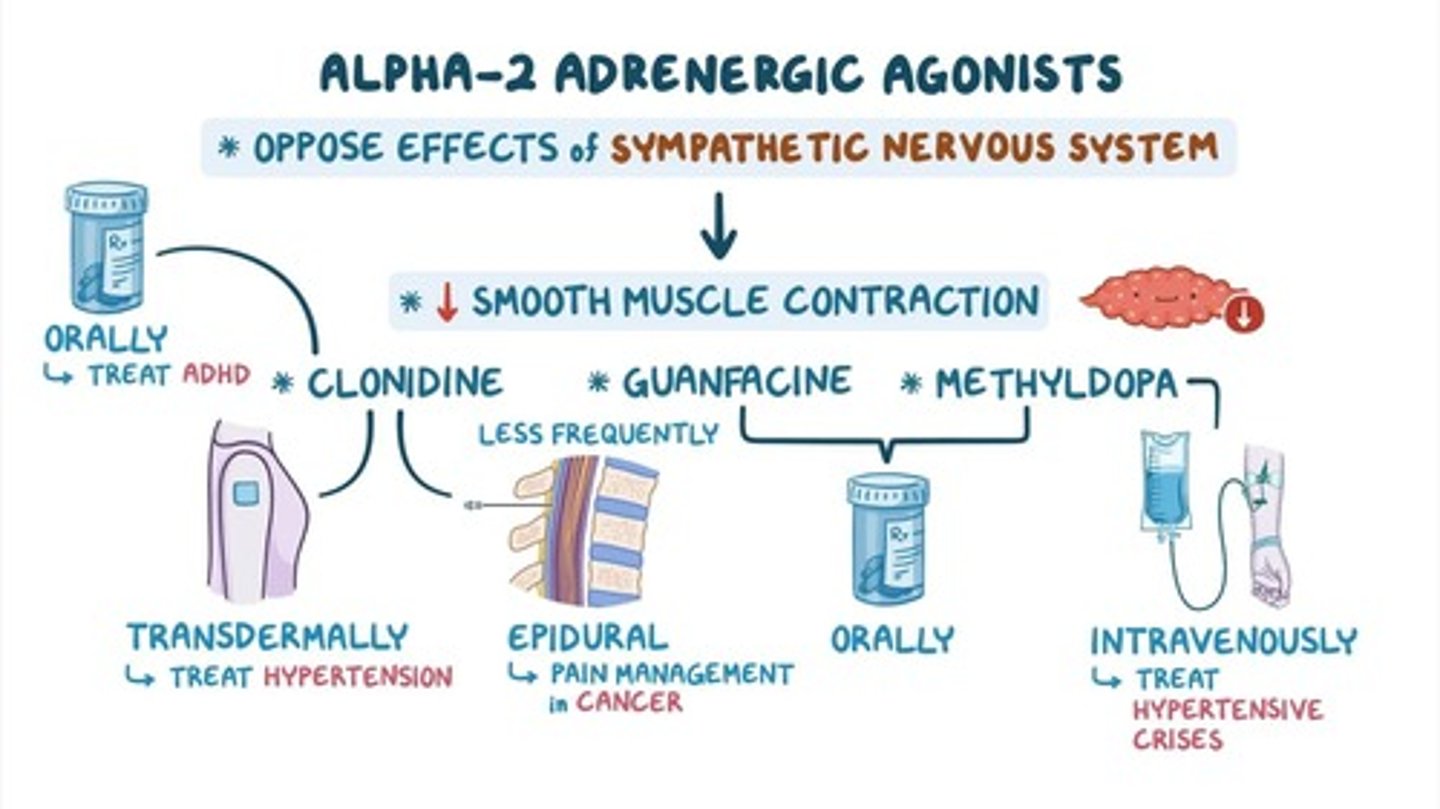
methyldopa
centrally-acting alpha-2 agonist
analog of DOPA
- metabolized to alpha-methylnorepinephrone (MNE) which is a selective alpha-2 agonist
> acts in brainstem to reduce sympathetic outflow
- MNE is NOT degraded by monoamine oxidase, allowing it to accumulate more than NE levels
ADE: sedation, depression, inattention, hypotension, bradycardia, syncope
direct vasodilators
hydralazine (Apresoline), minoxidil
- MOA: directly relax arteriole smooth muscle
> does not affect sympathetic NS and does not cause venodilation
- can be used in combination w other anti-HTN drugs
> diuretics, beta blockers
direct vasodilators pharmacological effects
causes:
- reduction in blood pressure caused by arterial vasodilation
> activates neural compensatory reflexes (↑ sympathetic NS = ↑ vasoconstriction, CO, HR, renin release)
> activation of humoral compensatory reflexes (JG cells detect reduced BP and increase renin secretion)
hydralazine
direct vasodilator
- MOA: inhibits calcium release from arterial smooth muscle sarcoplasmic reticulum
> inhibits myosin phosphorylation, actin interaction, and contraction
- used for moderate to severe HTN not controlled by other medications
minoxidil
direct vasodilator
- MOA: activates K+ channel opening to increased outward flow of K+
> reduces intracellular Ca, reduces interaction of actin & myosin to decreased contraction
- used for HTN not controlled with max doses of a diuretic + 2 other anti-HTN agents
- ADE: headache, vertigo, reflex tachycardia, palpitations, fluid retention, pericardial effusion (black box)