Unit 6 - Advanced Ventilatory Support, Lung Transplantation, and Pediatric Respiratory Support
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
61 Terms
Ventilation
movement of air in/out of lungs (not just oxygen delivery)
Noninvasive Ventilation
Positive pressure via mask, no artificial airway
Invasive ventilation
Uses airway adjuncts (ETT, tracheostomy)
Noninvasive and Invasive Ventilation
Positive pressure aids ventilation
Driving air into alveoli
Splinting airways open
Increasing lung volume
Decreasing work of breathing
Noninvasive and Invasive Ventilation
Indications
Type I failure = poor oxygenation
Type II failure = poor CO₂ removal
Noninvasive and Invasive Ventilation
PTs
should note pressure/FiO₂ to gauge severity and risk
PEEP
pressure at end of exhalation
Keeps alveoli open, improves oxygenation
CPAP
One continuous pressure throughout breathing cycle
Used for OSA, pulmonary edema, post-op atelectasis
BiPAP
PAP (inhalation) + EPAP (exhalation = PEEP)
Adds pressure support to assist ventilation
Ideal for COPD, hypercapnic respiratory failure
CPAP and BiPAP
PT considerations
Higher pressures = sicker patient
Monitor tolerance, ensure mask seal during activity
CPAP may be maintained during exercise in select cases (e.g. HF)
Mechanical Ventilation
Positive-pressure ventilation
replaces or augments spontaneous breathing
Mechanical Ventilation
Delivers set tidal volume, rate, FiO₂, and PEEP via ETT or tracheostomy
Mechanical Ventilation
Indications
airway protection, hypoxemia (Type I), hypercapnia (Type II), ↓ WOB
Mechanical Ventilation
Goals
improve gas exchange, ↓ work of breathing, stabilize overall status
Mechanical Ventilation
PTs
coordinate with ICU team to assess readiness, monitor stability, and promote mobility
Airway Adjuncts
Oropharyngeal
Oral; for unconscious patients; triggers gag reflex; temporary
Airway Adjuncts
Nasopharyngeal
Nasal; tolerated when semi-conscious; used for suctioning or patency
Airway Adjuncts
Endotracheal tube
Oral/nasal; for mechanical ventilation; prevents speech/eating; high monitoring needs
Airway Adjuncts
Tracheostomy
Surgical; long-term ventilation; allows speech/oral intake; more stable for PT
Airway Adjuncts
PT Role
Identify device, ensure airway safety, coordinate care, plan safe mobilization
Ventilator Modes
determine how much support the ventilator provides and can be interpreted to understanded patient readiness for activity
Ventilator Modes
Assist Control (AC)
Full support; set volume/pressure for every breath
No spontaneous effort required
Often early critical illness; low activity tolerance
Ventilator Modes
Synchronized Intermittent Mandatory Ventilation
Partial support; set breaths + unassisted spontaneous breaths
Encourages muscle use; common in weaning
May tolerate upright activity if stable
Ventilator Modes
Pressure Support Ventilation (PSV)
All breaths initiated by patient; pressure aids inspiration
Requires drive and effort; used in weaning
Monitor for fatigue or distress
Ventilator Modes
Ventilator Screen for PTs
Check mode, FiO₂, PEEP, rate, tidal volume
Confirm settings match expected clinical status
Unexpected changes may signal decompensation
Mobilizing While On Mechanical Ventilation
Use standard safety criteria to guide decision-making
Assess FiO₂, SpO₂, RR, mode before mobilization (e.g., FiO₂ < 0.6, RR < 30)
Confirm hemodynamic and neurological stability (e.g., stable HR/BP, able to follow commands)
Begin with positioning, progress to sitting, standing, walking as tolerated
Monitor tubing integrity and secure airways to prevent accidental extubation
PTs must coordinate with the care team to ensure safe and appropriate progression
Acute Respiratory Distress Syndrome (ARDS)
Acute lung inflammation → impaired gas exchange & respiratory failure
Rapid onset following infection, trauma, or systemic insult
Hallmark = severe hypoxemia unresponsive to oxygen therapy
Acute Respiratory Distress Syndrome (ARDS)
Common Causes: Direct
Pneumonia, aspiration, pulmonary contusion, inhalational injury
Acute Respiratory Distress Syndrome (ARDS)
Common Causes: Indirect
Sepsis, trauma, burns, pancreatitis, massive transfusion
Acute Respiratory Distress Syndrome (ARDS)
Diagnosis
Bilateral opacities on imaging (not explained by heart failure)
Must rule out cardiac cause of pulmonary edema
Acute Respiratory Distress Syndrome (ARDS)
Clinical Importance
High ICU mortality, especially with comorbidities
Early recognition is critical for appropriate intervention
Acute Respiratory Distress Syndrome (ARDS)
Three phases
Exudative → Proliferative → Fibrotic
Acute Respiratory Distress Syndrome (ARDS)
Exudative phase
Alveolar-capillary damage → fluid leak → surfactant loss → alveolar collapse
Acute Respiratory Distress Syndrome (ARDS)
Proliferative phase
Alveolar repair and fluid reabsorption begin; fibroblasts active
Acute Respiratory Distress Syndrome (ARDS)
Fibrotic phase
Scar tissue replaces alveoli → stiff, noncompliant lungs
Acute Respiratory Distress Syndrome (ARDS)
PT implications
Exudative = passive movement, careful monitoring
Proliferative = begin active mobilization, breathing retraining
Fibrotic = focus on rehab, endurance, managing long-term restriction
Acute Respiratory Distress Syndrome (ARDS)
Medical Management and PT considerations —> Goal
Support oxygenation, protect lungs, aid recovery
Acute Respiratory Distress Syndrome (ARDS)
Medical Management and PT considerations —> Proning
12–16 hrs/day)
Improves oxygenation and survival
PTs assist with safe, pressure-relieving positioning
Acute Respiratory Distress Syndrome (ARDS)
Medical Management and PT considerations —> PT focus
Early: PROM, positioning, monitoring
Later: Sitting, transfers, mobility as tolerated
COVID-19 Overview
a major cause of ARDS since 2020
Virus enters via ACE2 receptors in lungs and other organs. Triggers cytokine storm → widespread inflammation
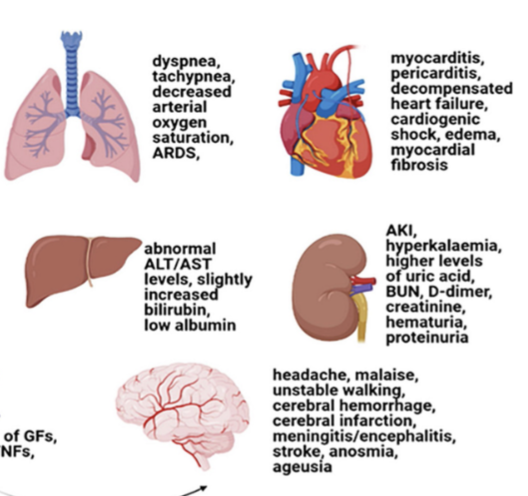
COVID-19 Overview
Multi-organ effects
Lungs → ARDS, hypoxemia
Heart, kidneys, liver, brain also affected
COVID-19 Overview
PT in acute phase
Positioning, PROM, monitor vitals/O₂
Caution with oxygen desaturation, fatigue
COVID-19 Overview
PT in subacute phase
Mobilization, breathing retraining, reconditioning
Consider multi-system impairments during rehab
Long COVID
Common symptoms impacting function
Fatigue, dyspnea, brain fog, dizziness, joint/muscle pain
Post-exertional symptom exacerbation
Autonomic dysfunction (e.g. POTS), cognitive decline
Long COVID
PT screening priorities
History of COVID (even mild)
Monitor vitals: HR, SpO₂, orthostatic response
Screen for activity intolerance, PEM, and cognitive
issues
Long COVID
Exercise approach
Start low, go slow – titrate to symptom tolerance
Use pacing, frequent breaks, and energy conservation
Emphasize function, not intensity
Long COVID
Collaborative care
Refer for cognitive, mental health, or speech support if needed
Educate on realistic goals and symptom self-monitoring
Lung Transplantation
Most common for Emphysema and Pulmonary Fibrosis. Other indications include Cystic Fibrosis, Pulmonary Hypertension, Sarcoidosis
Rigorous evaluation process
Pulmonary function testing, 6MWTs, frailty, and psychosocial factors
Prioritizes those most likely to benefit
Rising transplant numbers with need still exceeding supply
Lung Transplantation
Prehabilitation
Rehab evaluation prior to transplant assesses pulmonary function, functional capacity, and secretion clearance.
Prehabilitation includes cardiovascular training, resistance exercise, airway clearance, and breathing retraining.
Strength training focuses on proximal muscle groups to support function and recovery.
Airway clearance training prepares patients for post-op secretion management.
Breathing retraining encourages diaphragmatic breathing to reduce accessory muscle use.
Education on pacing, energy conservation, and oxygen use promotes safe activity participation.
Typical frequency is 30–40 minutes of combined training, 3–5 times per week, progressed based on tolerance
Lung Transplantation
Postoperative Rehab & Precautions —> Rehab begins within 24 hours in ICU
Focus: positioning, breathing exercises, airway clearance
Strict infection control due to immunosuppression
Lung Transplantation
Postoperative Rehab & Precautions —> Early mobilization as tolerated
Goal: reduce ICU-acquired weakness and pulmonary complications
Lung Transplantation
Postoperative Rehab & Precautions —> Airway clearance is essential
Denervated lungs impair cough reflex
Lung Transplantation
Postoperative Rehab & Precautions —> Therapist role includes education & vigilance
Monitor for signs of infection, rejection, or desaturation
Prepare patient for discharge and outpatient rehab
Pediatric Respiratory Conditions
Issues related to prematurity (infants born <37 weeks)
Example: Respiratory Distress Syndrome (RDS)
Bronchopulmonary dysplasia (BPD)
Meconium aspiration syndrome (MAS)
Cystic fibrosis (CF)
Childhood asthma
Early understanding of developmental origins guides appropriate care strategies
Respiratory System Development
Begins 4th week of gestation
Respiratory System Development
Maturation of lungs
Pseudoglandular (weeks 5-16)
Canalicular (weeks 16-26)
Terminal Saccular (week 26-birth)
Alveolar (32 weeks- 8 years)
Respiratory System Development
Anatomical considerations
Rib cage is circular & horizontal, lacking bucket handle orientation
Narrower airways can become obstructed easily
50% fewer type I muscle fibers than adults
Airways are narrower, more compliant, and fatigue more easily
Respiratory Distress Syndrome
Caused by surfactant deficiency in premature infants
Leads to alveolar collapse, low compliance, and V/Q mismatch
Presents with tachypnea, grunting, nasal flaring, and retractions
“Ground-glass” appearance with air bronchograms on chest X-ray
Treated with CPAP, ventilation, and exogenous surfactant
Bronchopulmonary Dysplasia
Chronic lung disease from prolonged oxygen or ventilation after RDS
Caused by inflammation, fibrosis, and impaired alveolar development
Clinical signs: tachypnea, wheezing, oxygen dependence, delayed growth
Radiograph shows scarring, atelectasis, emphysema, and cystic changes
Treatment includes gentle ventilation, oxygen, diuretics, steroids, and developmental therapies
Meconium Aspiration Syndrome (MAS)
Caused by inhalation of meconium-stained amniotic fluid before or during birth
Leads to airway obstruction, inflammation, surfactant inactivation, and V/Q mismatch
Clinical signs: respiratory distress, cyanosis, retractions, and patchy infiltrates on X-ray
Treatment includes suctioning, oxygen/ventilation, surfactant, and inhaled nitric oxide
May require ECMO in severe cases; PT supports breathing and positioning once stabilized
Treatment Strategies
Age appropriate and fun (play based)
In the least restrictive environment
Focused on developmental progression when appropriate
Practical for family carryover
Meaningful to the family
Settings include: inpatient hospital (acute & rehab), outpatient, early intervention centers, home, school