54. Cysts and tumours of the ovaries (surface epithelial, germ cell, sex cordstromal tumours, tumours, metastases)
1/55
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
56 Terms
Functional unit of the ovary?
Ovarian follicle
Comprised of:
- Oocyte surrounded by granulosa- and theca cells
Theca cells: responds to LH by producing androgens from cholesterol
Granulosa cells: Responds to FSH by converting androgens into estrogens like estradiol - aromatase enzyme does the conversion
Estradiol's function on the oocyte?
- Stimulates the oocyte to mature
- Stimulates proliferative phase of the endometrium -> prepares it for egg to implant
What happens with the ovarian follicle after ovulation?
It becomes corpus luteum -> which starts to secrete progesterone
Progesterone:
- Stimulates growth of endometrial stroma
- Inhibits secretion of FSH and LH from the pituitary
Types of ovarian cysts?
- Follicular cysts
- Corpus luteal cysts
- Chocolate cysts
Follicular cysts?
Follicles in the ovary can degenerate and form follicular cysts
- Most women have some, as it is very common
Are normally asymptomatic - but they can rupture & cause acute abdominal pain
Corpus luteal cysts?
When an egg is not fertilized - the corpus luteum usually breaks down
- Sometimes: it fills w/ blood or serous fluid = and becomes a cyst
Are very common
- They could rupture - causing acute abdominal pain
Chocolate cysts?
Endometriosis in the ovary
- Menstrual products that form chocolate-brown cysts in the ovary
Polycystic ovary syndrome?
Poorly understood condition
- More frequent in adolescent women
- Endocrine disorder -> caused by increased LH compared to FSH
What is Polycystic ovary syndrome characterized by?
Characterized by three things:
1. Ovulatory dysfunction
2. Androgen excess
3. Polycystic ovaries
(There is often excess estrogen as well)
PCOS etiology?
Exact etiology is unknown
- There is high concordance -> genetic component
- The disease can occur in the absence of ovaries
=> the ovaries are probably not the cause, but rather a symptom of the disease
Potential risk factors PCOS?
- Obesity/insulin resistance
- Positive family history
- Diabetes
Insulin resistance in PCOS women?
Women with PCOS usually have much higher insulin resistance than their body weight would normally indicate
Morphology PCOS?
- Ovaries are twice the normal size -> filled with cysts around 1cm
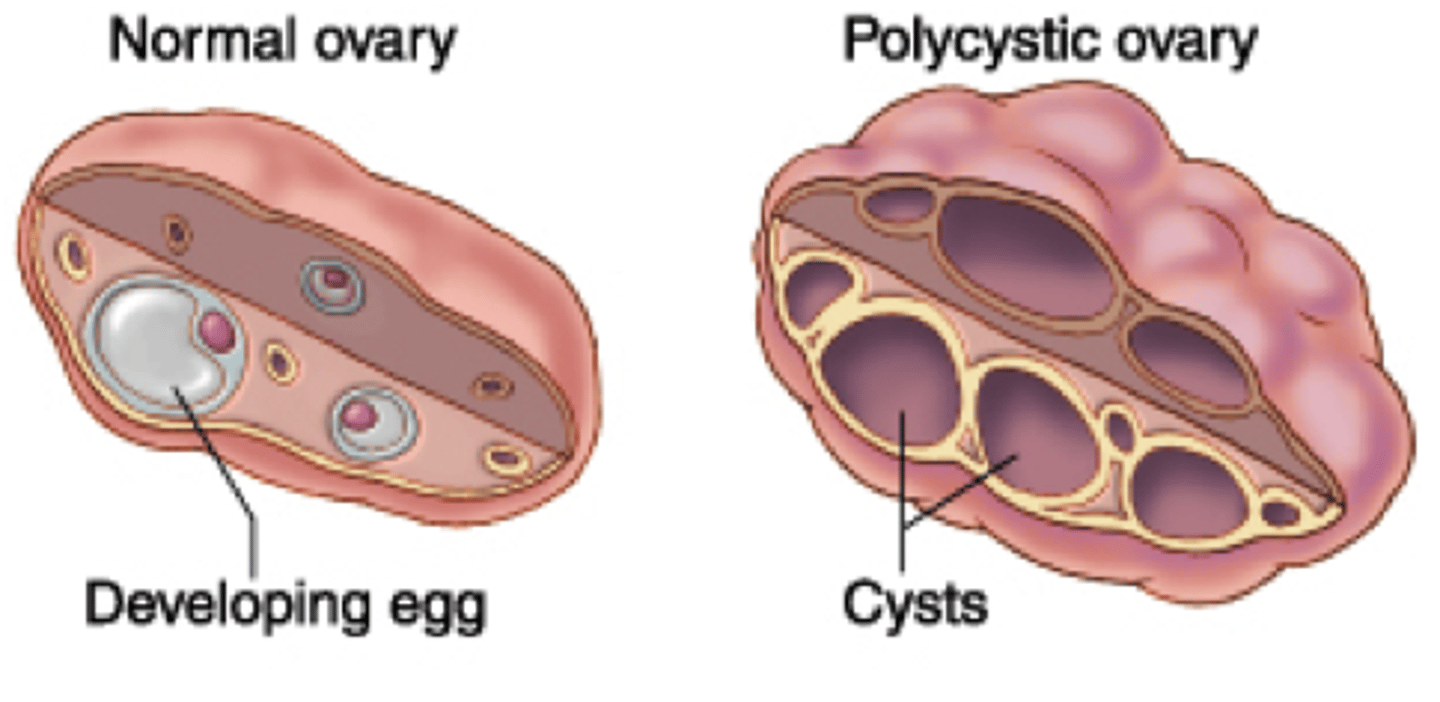
Pathomechanism PCOS?
Is unknown
- Hyperinsulinism may be involved
- Something causes LH to increase -> extra LH causes theca cells to produce more androgens
- As the FSH level is normal, the granulosa cells will not convert all these androgens to estrogens
= The excess androgens will be released into the blood
What happens to the androgen released into the blood (PCOS)?
Some of these androgens will be converted into estrogens by peripheral adipose tissue
= These estrogens will inhibit FSH secretion from pituitary -> worsening the problem
What are the adverse effect of the abnormal LH:FSH ratio in PCOS?
Causes the maturation of ovarian follicles to be impaired
- Instead of maturing properly, the follicles will become cysts
Clinical features of PCOS?
- Excess androgens in the blood causes development of male characteristics like facial hair
- As follicles are not maturing properly -> sterility can occur
- Abnormal uterine bleeding
- Increased circulating estrogens in the blood -> increased risk for endometrial carcinoma
Ovarian tumors?
4 types of ovarian tumors
- Metastasis is one type
Ovary consists of three cell types:
- Surface epithelium
- Totipotent germ cells
- Sex-cord stroma (theca & granulosa)
Primary tumors: mostly unilateral
Metastases: are bilateral
Why are often metastases found in ovarian cancers?
Because they cause symptoms very late in the cancer disease, causing the diagnosis very late also
Where does ovarian cancers often spread?
They disseminate to the peritoneum
= Peritoneal carcinosis -> can cause ascites
Symptoms of ovarian tumors?
Varies from type to type
Generally:
- Ascites
- Abdominal pain
Due to ascites, affected women often notice that their clothes no longer fit properly around the waist
Classification of ovarian tumor?
- Surface epithelium tumors
- Germ cell tumors
- Sex cord tumors
- Ovarian metastases
How is diagnosis of ovarian tumors made?
Transvaginal ultrasound
Tumor markers in the different types:
- Epithelial tumors - CA-125
- Yolk sac tumor - AFP
- Choriocarcinoma - hCG
Epidemiology ovarian cancers?
Peak incidence depends on the type of tumor:
- Germ cell tumor - 15-30 y/o
- Benign epithelial tumor 35-40y/o
- Malignant epithelial tumor - 60-70y/o
Surface epithelium tumors?
- Account for 70% of all ovarian tumors - but 90% of all malignant ovarian tumors
These tumors present late with symptoms - therefore carries poor prognosis
Pathogenesis - surface epithelium tumors?
Most prevalent theory:
- These tumors develop from endometrium or fallopian tube epithelium that seeded into the ovary
- Microenvironment of the ovary promotes neoplastic formation
What supports the prevalent theory of the pathogenesis of surface epithelium tumors?
- Dysplastic precursor can be found in the fallopian tubes, and not in the ovaries
- Tubal ligation reduces the incidence of many ovarian epithelial tumors
- These tumors are highly associated with endometriosis
Risk factor - surface epithelium tumors?
- Nulliparity
- Endometriosis
- Positive family history
- BRCA1 or BRCA2 germ-line mutation
Five subtypes of surface epithelium tumors?
- Serous
- Mucinous
- Endometrioid
- Clear cell carcinoma
- Transitional cell tumor
Each of these are further sub-divided into:
- Benign
- Borderline
- Malignant
types
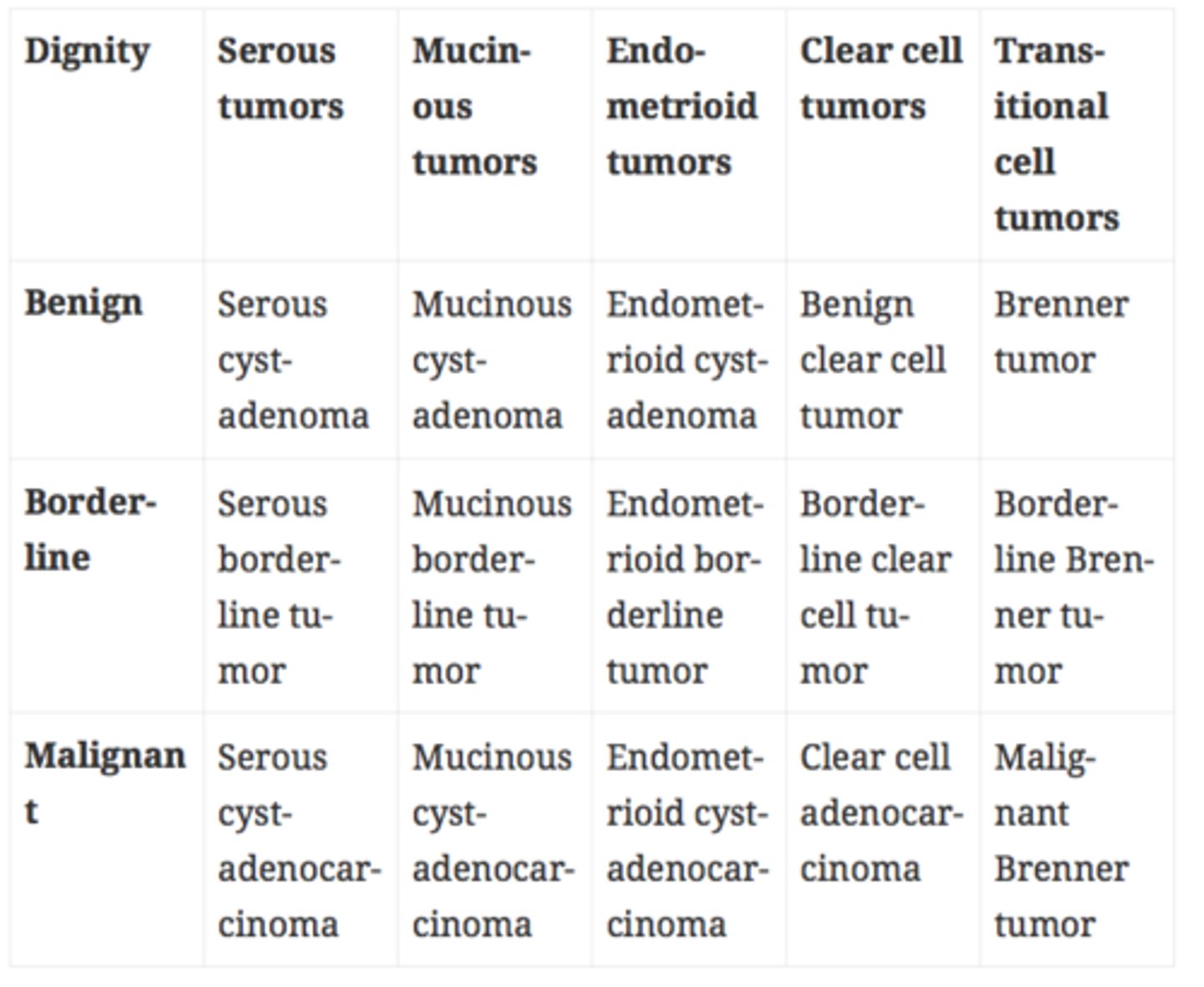
Borderline tumors?
Low-grade malignant tumors with low invasive potential
- Carry better prognosis than the malignant form
They usually do not invade, but they can metastasize
Prognosis - surface epithelium tumors?
As they are usually found late:
-> The stage of the tumor rather then the histological subtype is the major determinant of the outcome
Serous tumor (epithelial type) of the ovary?
Most common subtype
- Cystic tumors contain serous fluid
Serous cystadenoma:
Usually a single, simple cyst with simple squamous lining
Serous cystadenocarcinoma?
Not simple cysts, but rather complex, multiloculated cysts - Containing serous fluid
- Lined by thick epithelial lining
- Most frequent in postmenopausal women
- Epithelial tissue invades nearby tissue (malignancy)
- BRCA1 mutation
Often have psammoma bodies
Mucous tumor (epithelial type) of the ovary?
Similar to serous tumor, except that the tumor cells produce mucin fluid instead
- Less likely to be bilateral than the serous tumors
Endometrioid tumors? (epithelial type)
Histologically very similar to endometrium
- Malignant form: Endometrioid cystadenocarcinoma - is more common than the benign or borderline type
- Are bilateral in 30% of cases
What is Endometrioid tumors associated with?
Endometriosis
- This cancer sometimes co-exists with endometrioid carcinoma of the endometrium
= Therefore endometrium should also be tested
Clear cell tumors (epithelial type)?
Rare
- These tumors are comprised of clear cells
- Associated with endometriosis
Transitional cell tumor "Brenner tumors" (epithelial type)?
Not cystic, but rather solid
- Often unilateral tumors
- Comprised of urinary-tract-like transitional epithelium
- Most frequently benign
Germ cell tumors of the ovaries?
Second most frequent tumors of ovaries
- More common in reproductive age -> younger women
- Similar to germ cell tumors in males (most of the information applies in female GCT also)
Important subtypes of Germ cell tumors of the ovary?
• Teratoma:
- Dermoid cyst (mature teratoma)
- Immature teratoma
- Struma ovarii
• Dysgerminoma
• Yolk sac tumor
• Embryonal carcinoma
• Choriocarcinoma
Dermoid cyst?
Accounts for 90% of all ovarian teratomas
- Benign
- A cyst
- Can contain mature tissues, like hair, teeth or nests of GI epithelium
Immature teratomas?
Accounts for 10% of all ovarian teratomas
- They are malignant
- Tumors are bulky and solid, not cystic
- Histology: tissues of the tumor are immature
What does Grade and prognosis depend on in immature teratomas?
Depends on how much neuroepithelial tissue there is; the more, the higher the grade is
Struma ovarii?
Rare teratoma composed entirely of mature thyroid tissue
- Causes hyperthyroidism
Dysgerminoma?
Is the ovarian counterpart of the testicular seminoma
- All are malignant -> but is very sensitive to irradiation therapy
Tumor cells:
- Clear cytoplasm due to high glycogen content
Yolk sac tumor?
Produces AFP
Embryonal carcinoma?
Necrotic and hemorrhagic masses
- Tumors are aggressive
Choriocarcinoma?
Produce hCG
- Spread haematogenously very early
Sex cord stromal tumors of the ovary?
- Granulosa cells
- Theca cells
- Sertoli cells/Leydig cells
... any combination thereof
Three important sex cord tumors?
- Granulosa-theca cell tumor
- Thecofibroma
- Sertoli-Leydig cell tumor
Granulosa-theca cell tumor?
Frequently produce estrogen
- They increase the risk for breast and endometrial carcinoma
Thecofibroma?
Theca cells + fibroblasts comprise the tumor
Sertoli-Leydig cell tumor?
Malignant sex-cord ovarian neoplasm that is associated with virilization
- Tumors may produce androgens -> masculinization
Sertoli cells may produce tubules
Virilization?
Development of male physical characteristics (such as muscle bulk, body hair, and deep voice) in a female, typically as a result of excess androgen production.
Ovarian metastases?
Usually metastasize from
- GI-tract
- Breast
- Lung
- Endometrium
Krukenberg tumor?
Bilateral ovarian metastases
- Originate from GI-tract
- Most commonly from the diffuse type (signet ring cell) stomach carcinoma
Are often mucinous & can be hard to distinguish from primary mucinous epithelial tumors