Social anxiety disorder
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
22 Terms
Social anxiety disorder DSM criteria
Must have all of the following:
Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others
The individual fears that they will act in a way or show anxiety symptoms that will be negatively evaluated
The social situations almost always provoke fear or anxiety
The social situations are avoided or endured with intense fear or anxiety
The fear or anxiety is out of proportion to the actual threat posed by the situation and to the sociocultural context
The fear, anxiety, or avoidance is persistent (+6 months)
The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
What is the lifetime prevalence of SAD in Canada?
8-13%
Higher prevalence than PD
What is the prevalence of SAD in Canada over the last year (12 months)?
6.7%
T or F: SAD is 2x as common in women compared to men
TRUE
What course would SAD take if absent treatment?
Chronic course
Stable
T or F: SAD is highly comorbid
TRUE!
66.2% of individuals with SAD have at least one other disorder
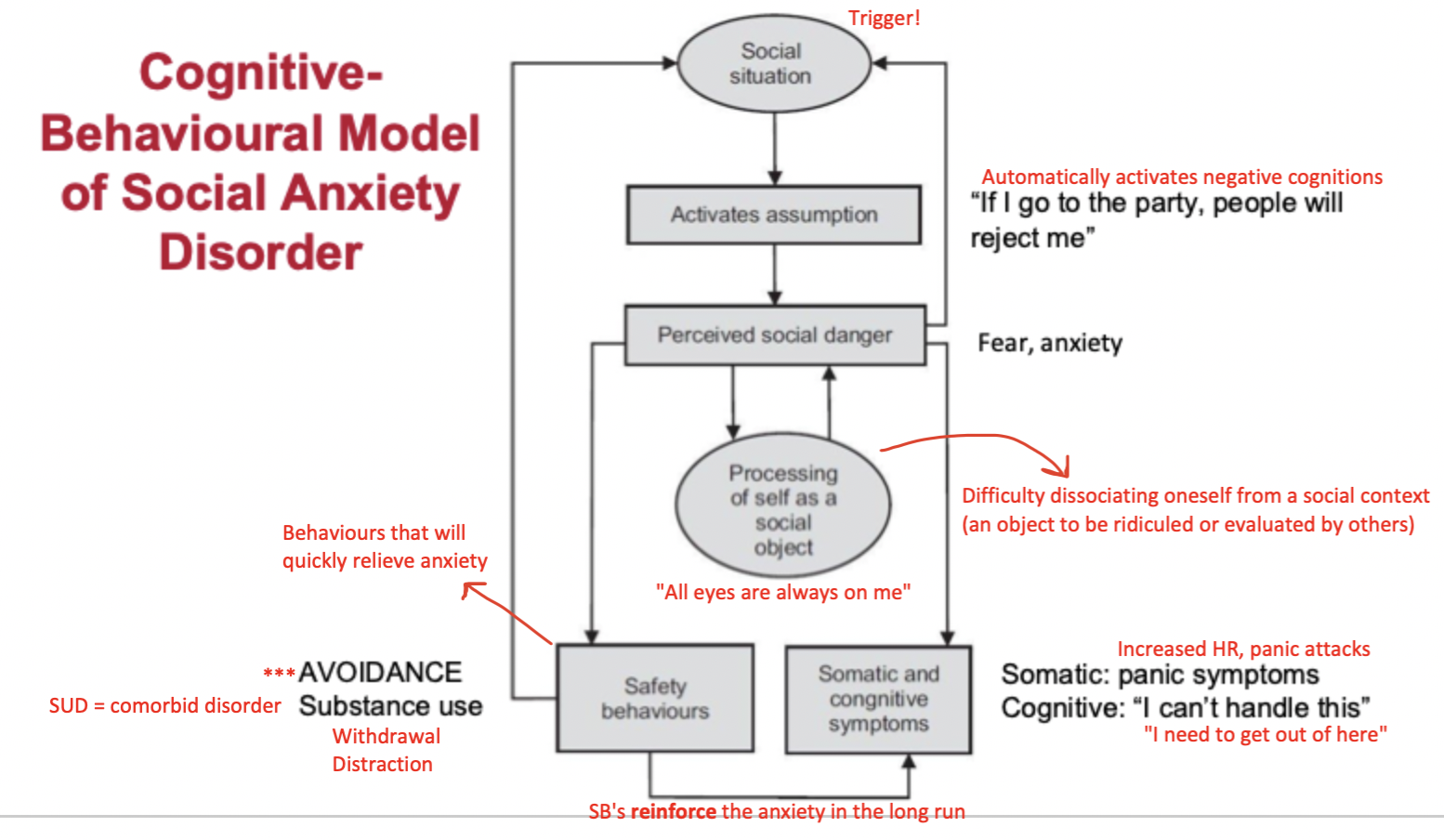
Cognitive-behavioural model of SAD
Study providing evidence for the cognitive-behavioural model of SAD (Boll et al., 2016)
Background: SAD is associated with increased vigilance to social threat cues
Purpose: Use eye-tracking methods to examine gaze behaviours in individuals with SAD vs. controls in response to angry, fearful, happy, and neutral faces
Hypothesis: Individuals with SAD will show early, reflexive attentions shifts towards eye region
Eyes = very expressive + most informative part of the face
Findings SUPPORTED hypothesis: Individuals with SAD showed proportionally more saccades (eye movements) from mouth -> eyes
Even though all participants made more eye shifts from mouth to eyes (rather than eyes to mouth), this shift was greater/quick in individuals with SAD
Why do these findings make sense?: Individuals with SAD look to others' eyes as cues of their emotions, so that they can determine whether they are being negatively evaluated (THEY FEAR THE EYES)
How do these findings support the model: Supports the idea that our attention is drawn to the things we fear (AKA people with sad are drawn to others eyes, which they fear because eyes can indicate negative evaluation)
What is a main psychological vulnerability for developing SAD?
Behavioural inhibition = an early childhood temperament factor that involves fear of novelty
Related to shyness and social reticence in preschool + elementary school years
Toddlers who have higher behavioural inhibition are at a much larger risk of developing SAD in later childhood/early adolescence
People with high behavioural inhibition are ~8x more likely to develop SAD
Diathesis-stress model
Psychopathology results from the interaction of internal vulnerability factors (genetics, temperament) + external triggers (stress learning/modeling)
What are some environmental moderators involved in SAD?
Parental anxiety -> can be a diathesis (internal vulnerability factor, genetics) and/or stress (external trigger, modelling, learning)
Insecure attachment -> high parental rejection, low parental warmth
Stressful social experiences -> rejection, victimization
Minority stress theory (environmental moderators)
Adverse mental health outcomes in sexual minority individuals result from:
External stressors = discrimination, rejection, violence, non-affirmation of gender identity
Internal stressors = fear of future discrimination, mistrust of others, internalized negative beliefs about one's identity, stress of concealment
How does the minority stress theory relate to SAD?
Repeated exposure to discrimination, victimization, and rejection (external stressors) -> leads to expectations of future negative experiences
Nonaffirmation of gender identity (external stressor) -> leads to embarrassment, shame or threat -> further leads to avoidance of social situations
Internalized transphobia (internal stressor) -> leads to expectations of rejection -> further leads to avoidance of social situations
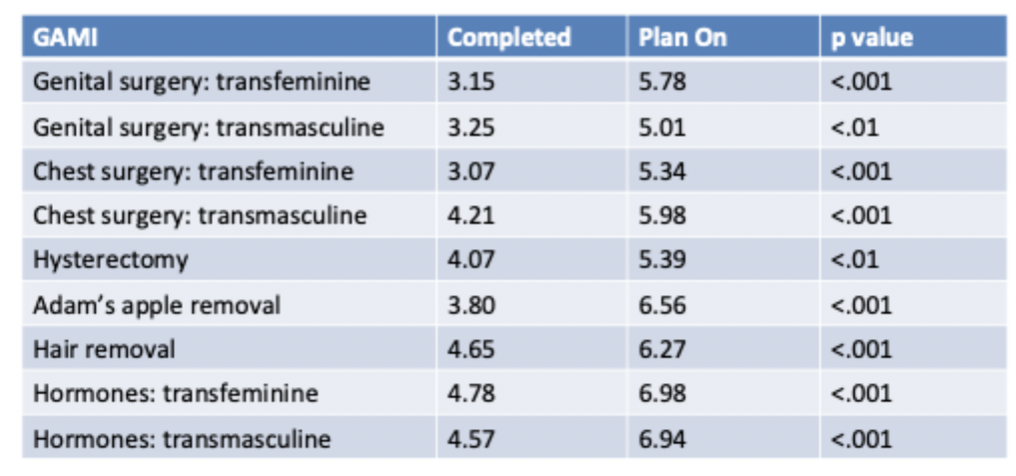
What is the role of gender-affirming medical interventions on SAD symptoms?
Found that gender-affirming medical care lead to significantly reduced SAD symptoms in trans individuals (compared to individuals who were planning on having interventions done in the future)
Gender-affirming care = great treatment for SAD
NOTE: trans individuals who had no interest in gender-affirming care did not significantly differ in SAD symptoms
What is the most common type of exposure used in CBT for anxiety disorders?
In vivo exposure = gradual exposure to feared situations in order to extinguish fear
What are common in vivo exposure targets for SAD?
Public speaking
Eating in front of others
Performing in front of others
Social outings
Talking to others
How are avoidance hierarchies used in SAD treatment?
Working collaboratively with the client to come up with a hierarchy regarding the things they would like to do the exposure therapy to
The content of the hierarchy is up to the client! (you as the therapist can't impose what youthink would be the most important things to put on the hierarchy)
Situations in the hierarchy are ranked based on:
Subjective units of distress (SUDs level)
0 = not anxiety provoking
100 = UNBEARABLY anxiety provoking
Avoidance rating
0 = could do
100 = would WANT TO avoid AT ALL COSTS
Clients typically start with situations that are lowest on the hierarchy
Therapist = "Notice how that things you find most anxiety provoking you also find most likely to avoid. What do you make of that?" (Socratic question + guided discovery)
Allow them to make the discovery (internalizing the learning)
How are exposure homework recording forms used in SAD treatment?
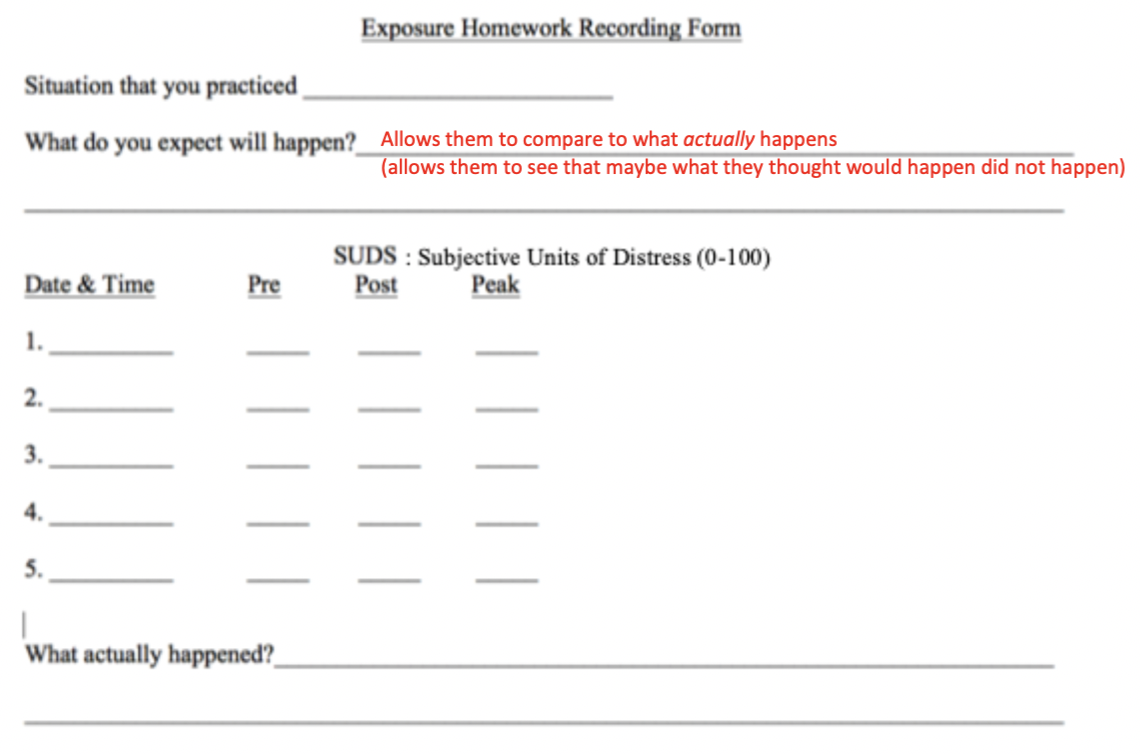
Based on the philosophy that practice makes perfect!
What are common elements of CBT for anxiety disorders?
Cognitive:
Encourages client to take a 3rd person / observer perspective (looing at the situation with new eyes)
What is the evidence that maladaptive thoughts are true?
Catastrophizing = "What is the worst that could happen?"
Probability overestimation = "How likely is [***] to happen?"
NOTE: gap between what client thought would happen vs. what actually happened
Cultural competence
Explore and validate thoughts and feelings around sexual identity and exposure to minority stress
Link those thoughts and feelings to current avoidance
Reasons for cognitions in SAD?
Client escapes situation before they get evidence to the contrary
Client thinks past events aren't good predictors of future events
Client thinks they have only survived before because of luck
Client takes panic symptoms as evidence of worst case scenario
How are thought-tracking forms used in SAD treatment?
Eventually schemas about the things they fear will wear down
Cognitions can change simply through exposure
How effective is CBT for SAD vs PD?
Study looked at the end of the treatment period (~12-15 weeks), how many individuals do not met DSM criteria for their diagnosis? (this does not necessarily mean they have 0 symptoms)
CBT = ~80% effective for SAD
Around the same efficacy as medication (SSRIs)
BUT medication is associated with higher relapse rates over time (more acute)…
CBT does better at keeping people well over the long-term!
CBT = 90% effective for PD