6- Principles of homeostasis and negative feedback, control of blood glucose levels, RP11, control of blood water potential
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
Describe homeostasis in mammals
maintenance of a stable internal environment within restricted limits
by physiological control systems (normally involve negative feedback)
Examples- core temperature, blood pH, blood glucose concentration, blood water potential
Explain the importance of maintaining stable core temperature
If temperature is too high:
hydrogen bonds in tertiary structure of enzymes break
enzymes denature; active sites change shape and substrates can’t bind
so fewer E-S complexes
If temperature is too low
not enough kinetic energy so fewer E-S complexes
Explain the importance of maintaining stable blood pH
Above or below optimal pH, ionic/ hydrogen bonds in tertiary structure break
Enzymes denature; active sites change shape and substrates can’t bind
So fewer E-S complexes
Explain the importance of maintaining stable blood glucose concentration - too low (hypoglycaemia)
not enough glucose (respiratory substrate) for respiration
so less ATP produced
active transport etc can’t happen= cell death
Explain the importance of maintaining stable blood glucose concentration - too high (hyperglycaemia)
water potential of blood decreases
water lost from tissue to blood via osmosis
kidneys can’t absorb all glucose= more water lost in urine causing dehydration
Describe the role of negative feedback in homeostasis
Receptors detect change from optimum
Effectors respond to counteract change
Returning levels to optimum/ normal
EXAMPLES: control of blood glucose conc, blood pH, core temperature and blood water potential
Explain the importance of conditions being controlled by separate mechanisms involving negative feedback
departures in different directions from the original state can all be controlled/ reversed
giving a greater degree of control (over changes in internal environment)
Describe positive feedback
Receptors detect change from normal
Effectors respond to amplify change
Producing a greater deviation from normal
NOT involved in homeostasis
EXAMPLES: onset of contractions in childbirth, blood clotting
Describe the factors that influence blood glucose concentration
consumption of carbohydrates= glucose absorbed into blood
rate of respiration of glucose e.g. increases during exercise due to muscle contraction
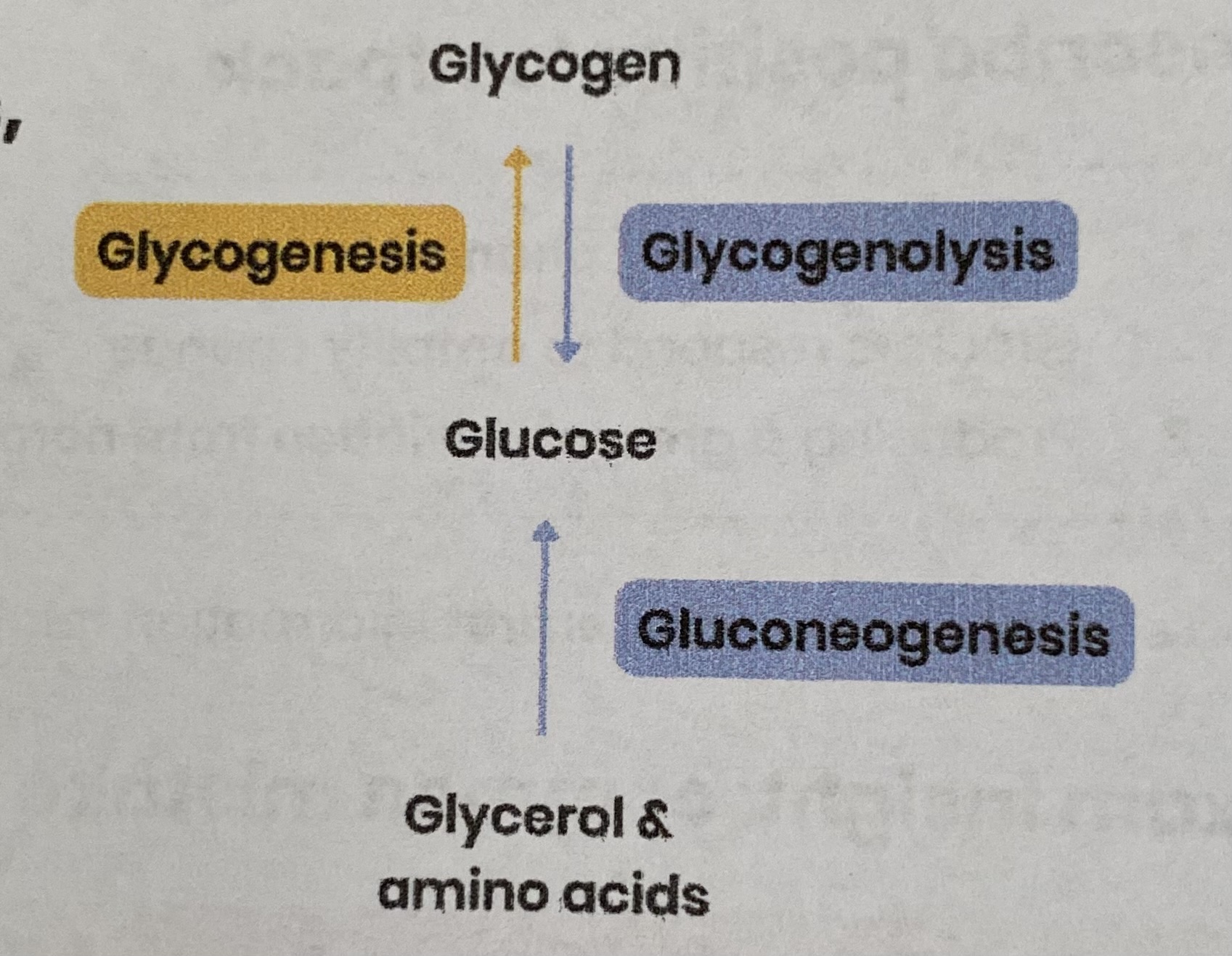
Describe the role of the liver in glycogenesis, glycogenolysis and gluconeogenesis
GLYCOGENESIS:
converts glucose= glycogen
GLYCOGENOLYSIS:
converts glycogen= glucose
GLUCONEOGENESIS:
converts amino acids and/ or glycerol= glucose
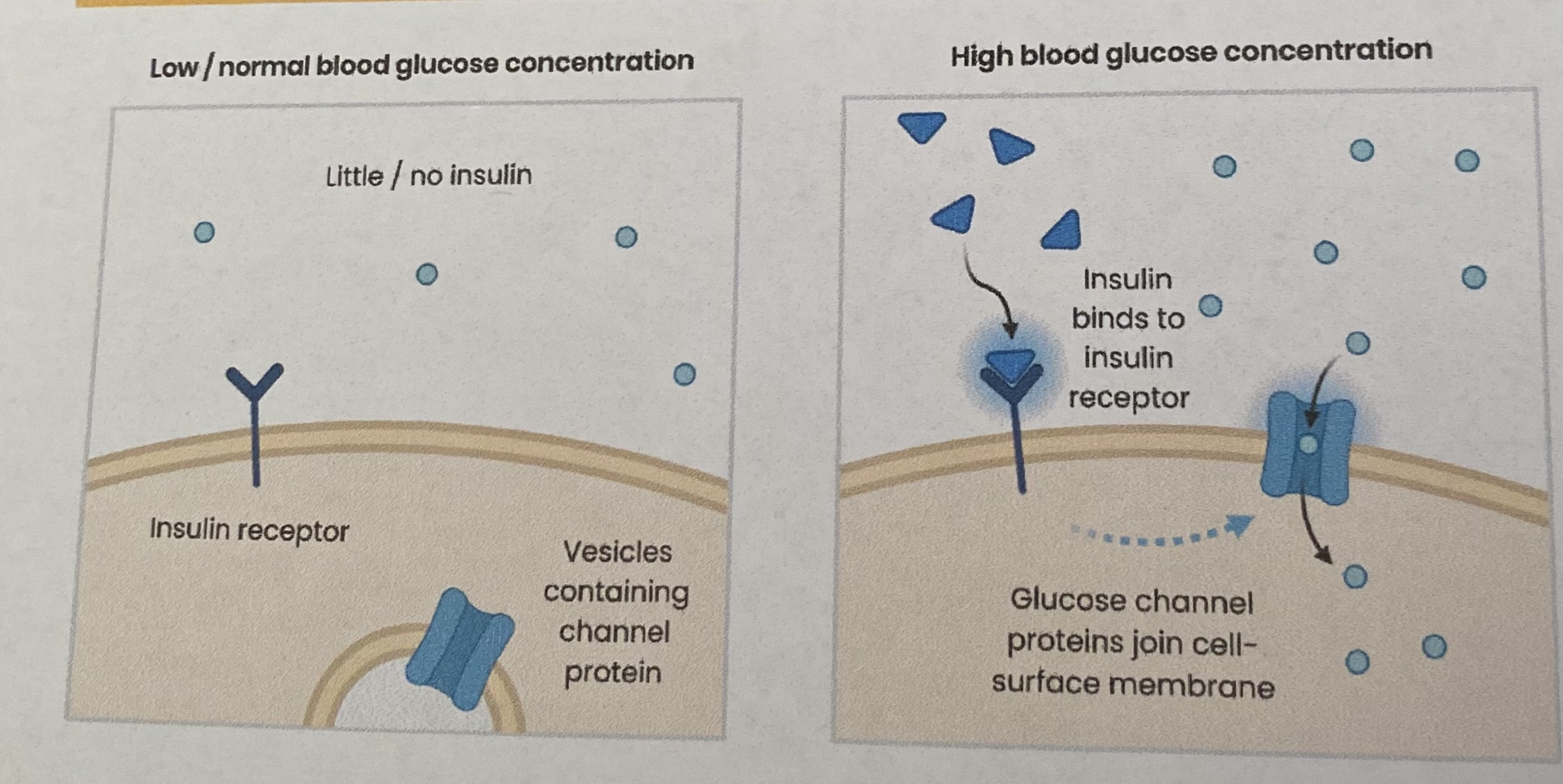
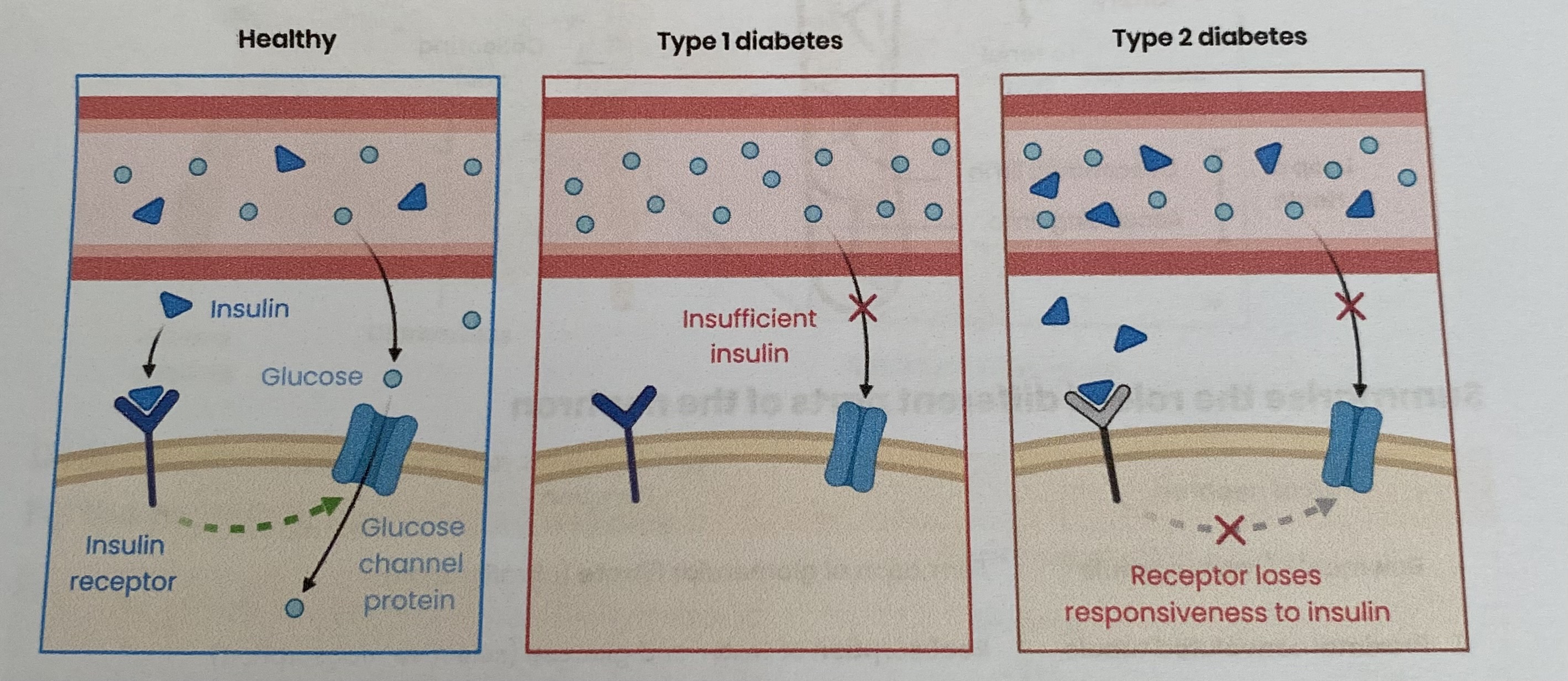
Explain the action of insulin in decreasing blood glucose concentration
Beta cells in islets of Langerhans in pancreas detect blood glucose concentration is too high= secrete insulin:
Attaches to specific receptors on cell surface membranes of target cells e.g. liver/ muscles
This causes more glucose channel proteins to join cell surface membrane
increasing permeability to glucose
so more glucose can enter cell by facilitated diffusion
This also activates enzymes involved in conversion of glucose to glycogen (glycogenesis)
lowering glucose concentration in cells, creating a concentration gradient
so glucose enters cell by facilitated diffusion
Explain the action of glucagon in increasing blood glucose concentration
Alpha cells in islets of Langerhans in pancreas detect blood glucose conc is too low= secrete glucagon:
Attaches to specific receptors on cell surface membranes of target cells e.g. liver
Activates enzymes involved in hydrolysis of glycogen to glucose (glycogenolysis)
Activates enzymes involved in conversion of glycerol/ amino acids to glucose (gluconeogenesis)
This establishes a concentration gradient= glucose enters blood by facilitated diffusion
Explain the role of adrenaline in increasing blood glucose concentration
Fear/ stress/ exercise= adrenal glands secrete adrenaline:
Attaches to specific receptors on cell surface membranes of target cells e.g. liver
Activates enzymes involved in hydrolysis of glycogen to glucose (glycogenolysis)
This establishes a concentration gradient= glucose enters blood by facilitated diffusion
Describe the second messenger model of adrenaline and glucagon action
Adrenaline/ glucagon (first messengers) attach to specific receptors on cell membrane which:
Activates enzyme adenylate cyclase (changes shape)
Which converts many ATP to many cyclic AMP (cAMP)
cAMP acts as the second messenger= activates protein kinase enzymes
Protein kinases activate enzymes to break down glycogen to glucose
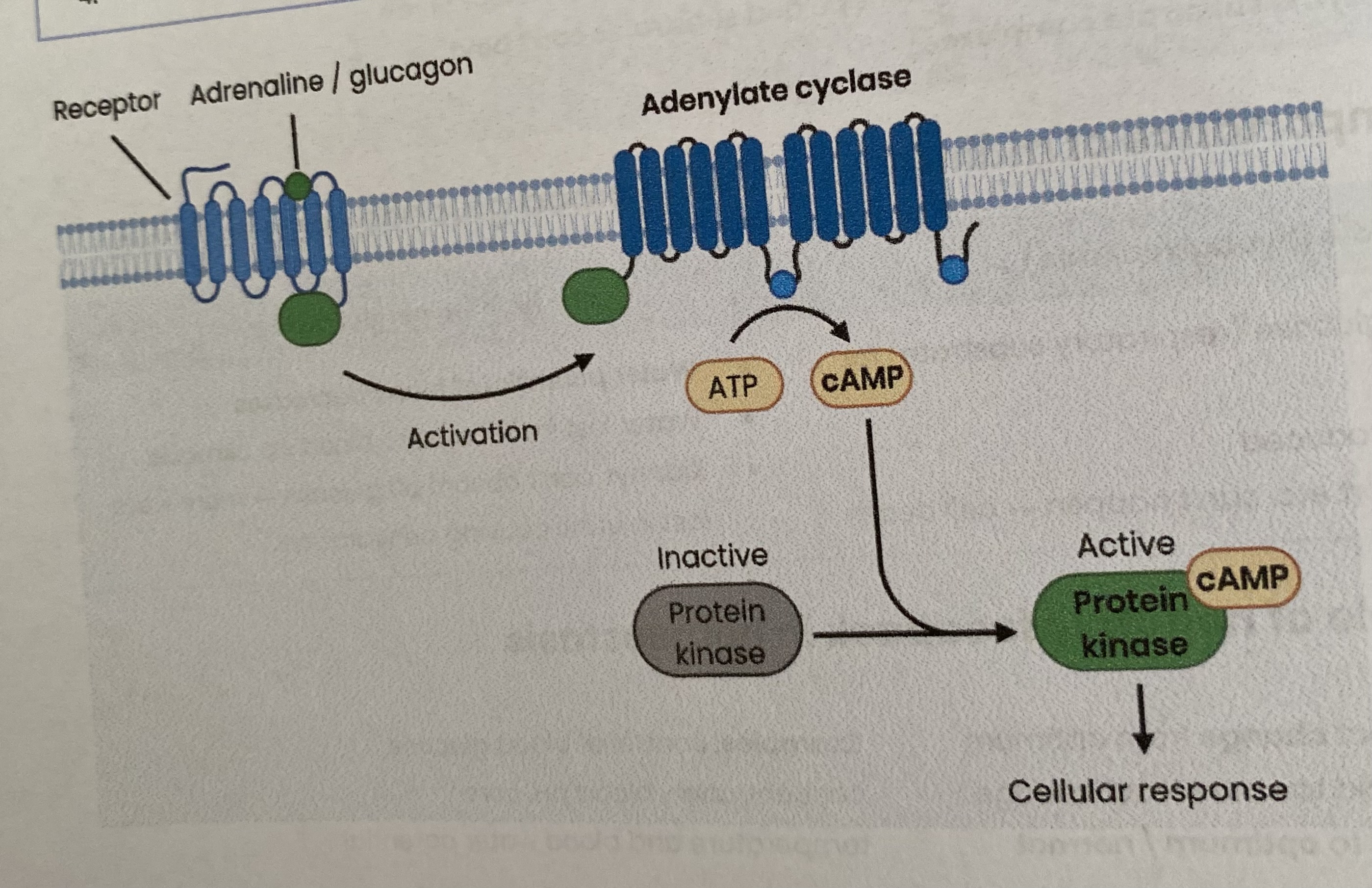
Suggest an advantage of the second messenger model
Amplifies signal from hormone
As each hormone can stimulate production of many molecules of second messenger (cAMP)
Which can in turn activate many enzymes for rapid increase in glucose
Compare the causes of types I and II diabetes
BOTH- higher and uncontrolled blood glucose concentration; higher peaks after meals and remains high
TYPE I:
key point= Beta cells in islets of langerhans in pancreas produce insufficient insulin
normally develops in childhood due to an autoimmune response destroying Beta cells of islets of Langerhans
TYPE II:
key point= receptor (faulty) loses responsiveness/ sensitivity to insulin (but insulin still produced)
so fewer glucose transport proteins= less uptake of glucose= less conversion of glucose to glycogen
risk factor= obesity
Describe how of type I diabetes can be controlled
Injections of insulin (as pancreas doesn’t produce enough)
Blood glucose conc monitored with biosensors; dose of insulin matched to glucose intake
Eat regularly and control carbohydrate intake e.g. those that are broken down/ absorbed slower
to avoid sudden rise in glucose
Suggest why insulin can’t be taken as a tablet by mouth
insulin is a protein
would be hydrolyses by endopeptidases/ exopeptidases
Describe how of type II diabetes can be controlled
Not normally treated with insulin injections (as pancreas still produces it) but may use drugs which target insulin receptors to increase their sensitivity
to increase glucose uptake by cells/ tissues
Reduce sugar intake (carbohydrates)/ low glycaemic index= less absorbed
Reduce fat intake= less glycerol converted to glucose
More (regular) exercise= uses glucose/ fats by increasing respiration
Lose weight= increased sensitivity of receptors to insulin
Describe how you can evaluate the positions of health advisers and the food industry in relation to the increased incidence of type II diabetes
Consider both arguments:
Health advisers aim- reduce risk of type II diabetes due to health problems caused (e.g. kidney failure)
so need to reduce obesity as it is a risk factor
Food industry aim- maximise profit
What is RP11?
Production of a dilution series of a glucose solution and use of colorimetric techniques to produce a calibration curve with which to identify the concentration of glucose in an unknown ‘urine’ sample
RP11- Describe how a calibration curve could be produced for glucose
Use distilled water and a glucose solution of unknown concentration to produce a dilution series (of glucose solutions of known concentrations)
Heat a set volume of each solution with a set volume of Benedict’s solution
Measure absorbance (of light) of each solution using a colorimeter
Plot a graph of absorbance (y axis) against concentration of glucose solution (x axis) and draw a line/ curve of best fit
NOTE- the calibration curve will vary e.g. if precipitate was removed before using the colorimeter
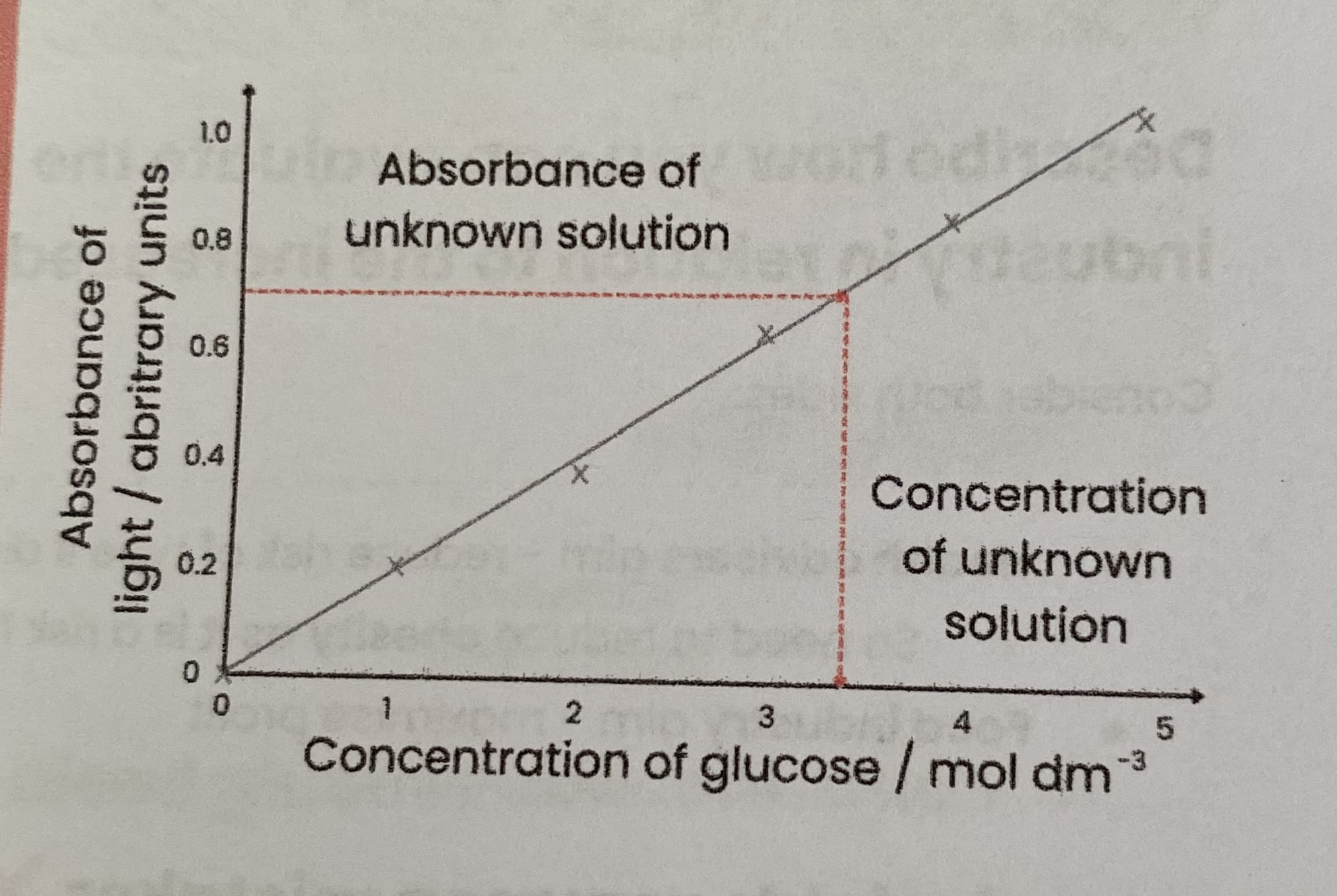
RP11- Describe how the concentration of glucose in an unknown ‘urine’ sample can be identified using a calibration curve
Perform Benedict’s test on sample using same volumes of solutions used in producing calibration curve
Measure absorbance using a colorimeter
Absorbance value for ‘urine’ sample read off calibration curve to find associated glucose conc
RP11- Give examples of variables that should be controlled (2 marks)
volume of sample used
volume of Benedict’s solution
temperature of water bath
time samples were heated for in water bath
RP11- Explain why a high blood glucose conc can cause glucose to be present in the urine of a diabetic person (2 marks)
not all glucose reabsorbed at proximal convoluted tubule
as glucose carrier/ cotransporter proteins are saturated/ working at maximum rate
Describe the structure of a nephron
Nephron= basic structural and functional unit of the kidney (millions in the kidney)
Associated with each nephron are a network of blood vessels
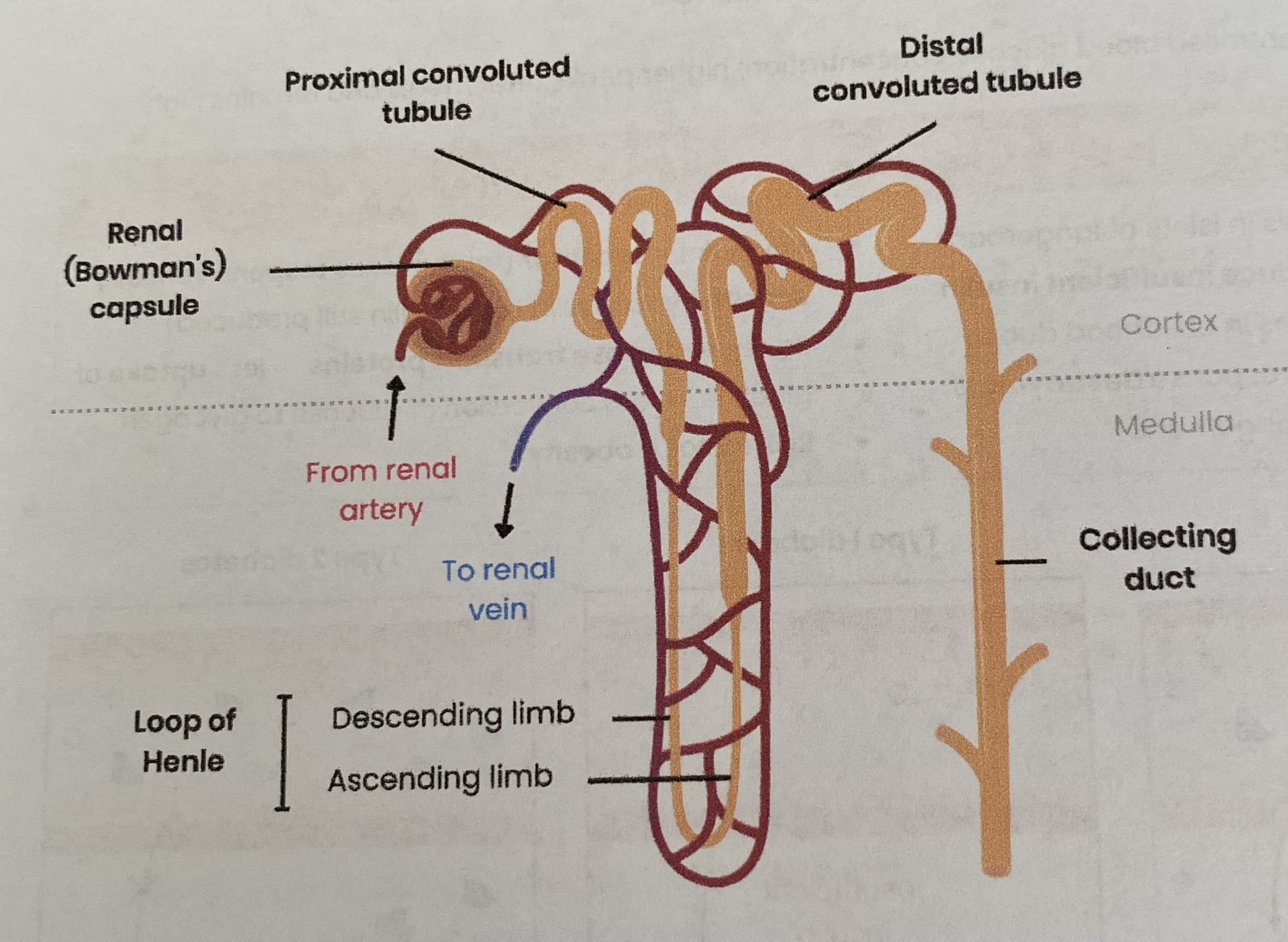
Summarise the role of different parts of the nephron
Bowman’s/ renal capsule= formation of glomerular filtrate (ultrafiltration)
Proximal convoluted tubule= reabsorption of water and glucose (selective reabsorption)
Loop of Henle= maintenance of a gradient of sodium ions in the medulla
Distal conoluted tubule= reabsorption of water (permeability controlled by ADH)
Collecting duct
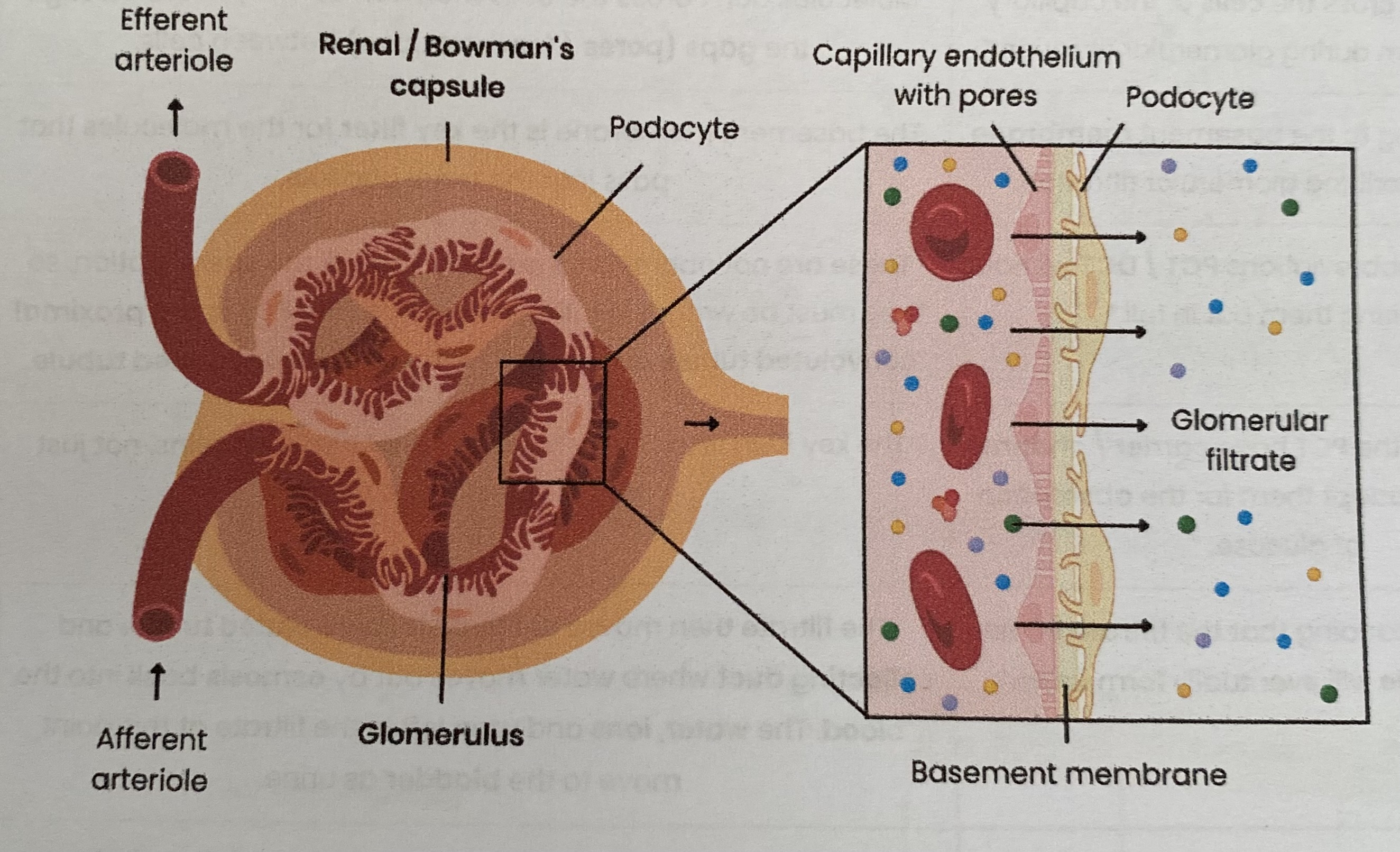
Describe the formation of glomerular filtrate
High hydrostatic pressure in glomerulus
as diameter of afferent arteriole (in) is wider then efferent arteriole (out)
Small substances e.g. water, glucose, ions, urea forced into glomerular filtrate, filtered by:
pores/ fenestrations between capillary endothelial cells
capillary basement membrane
podocytes
Large proteins/ blood cells remain in blood
Describe the reabsorption of glucose by the proximal convoluted tubule
Na+ actively transported out of epithelial cells to capillary
Na+ moves by facilitated diffusion into epithelial cells down a conc gradient, bringing glucose against its conc gradient
Glucose moves into capillary by facilitated diffusion down its conc gradient
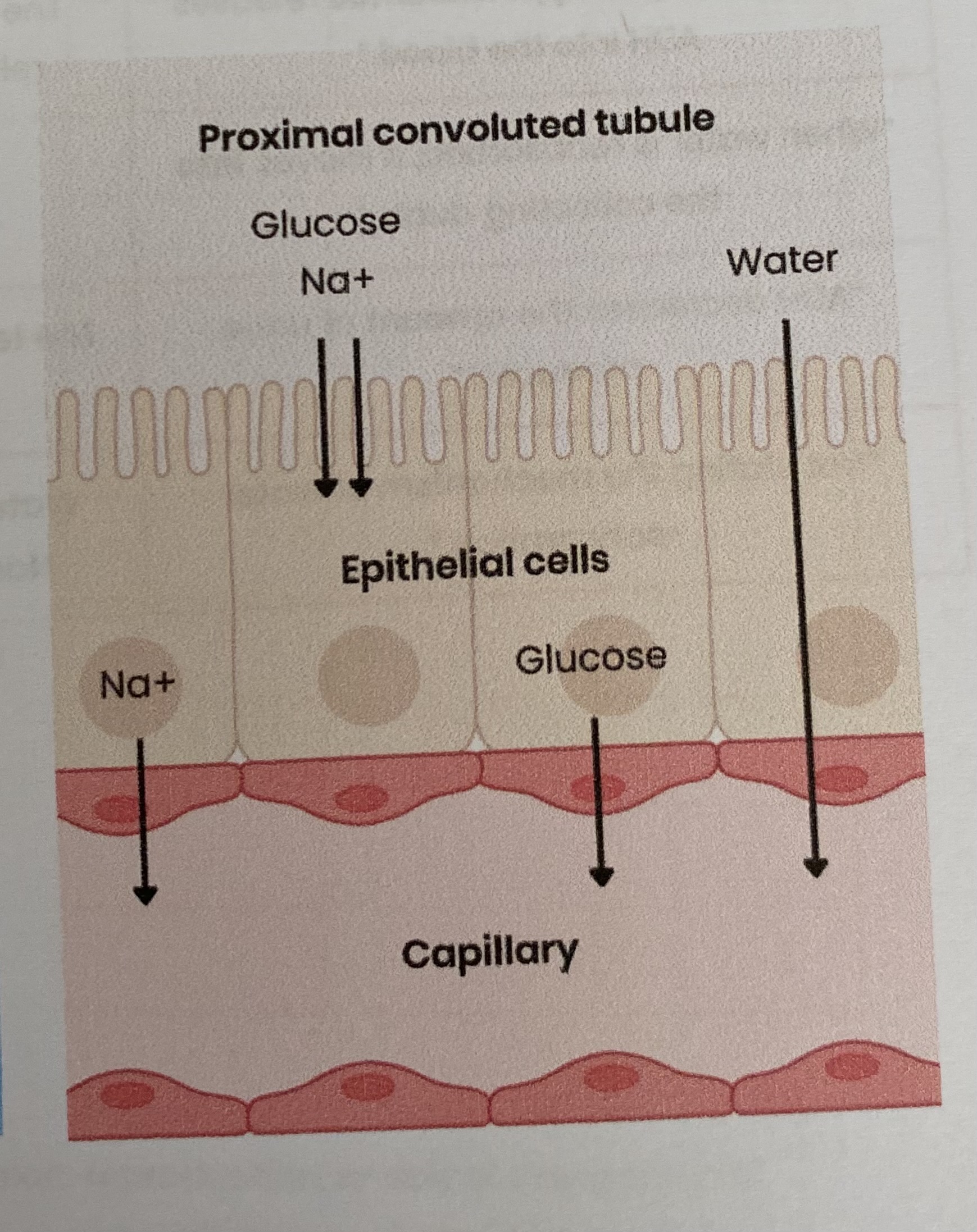
Describe the reabsorption of water by the proximal convoluted tubule
Glucose etc in capillaries lower water potential
Water moves by osmosis down a water potential gradient
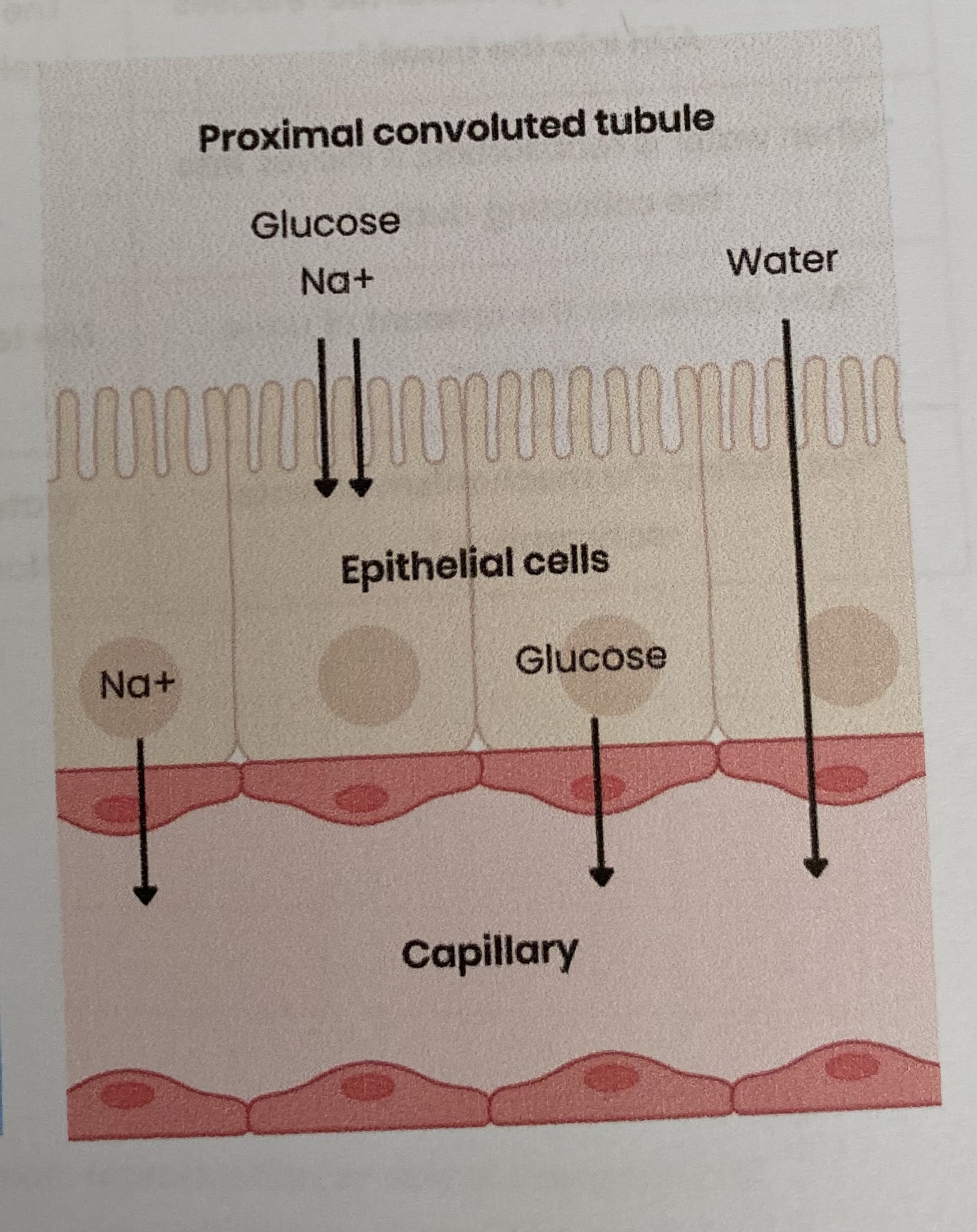
Describe and explain how features of the cells in the PCT allow the rapid reabsorption of glucose into the blood
Microvilli/ folded cell-surface membrane= provides a large SA
Many channel/ carrier proteins= for facilitated diffusion/ co-transport
Many carrier proteins= for active transport
Many mitochondria= produce ATP for active transport
Many ribosomes= produce carrier/ channel proteins
Suggest why glucose is found in the urine of an untreated diabetic person
Blood glucose conc is too high so not all glucose is reabsorbed at the PCT
as glucose carrier/ cotransporter proteins are saturated/ working at maximum rate
Explain the importance of maintaining a gradient of socium ions in the medulla (conc increases further down)
so water potential decreases down the medulla (compared to filtrate in collecting duct)
so a water potential gradient is maintained between the collecting duct and medulla
to maximise reabsorption of water by osmosis from filtrate
Describe the role of the loop of Henle in maintaining a gradient of sodium ions in the medulla
In the ascending limb:
Na+ actively transported out (so filtrate conc decreases)
water remains as ascending limb is impermeable to water
this increases conc of Na+ in the medulla, lowering water potential
In the descending limb:
water moves out by osmosis then reabsorbed by capillaries (so filtrate conc increases)
Na+ ‘recycled’= diffuses back in
The loop of Henle act as as a countercurrent multiplier (you don’t need to know why)
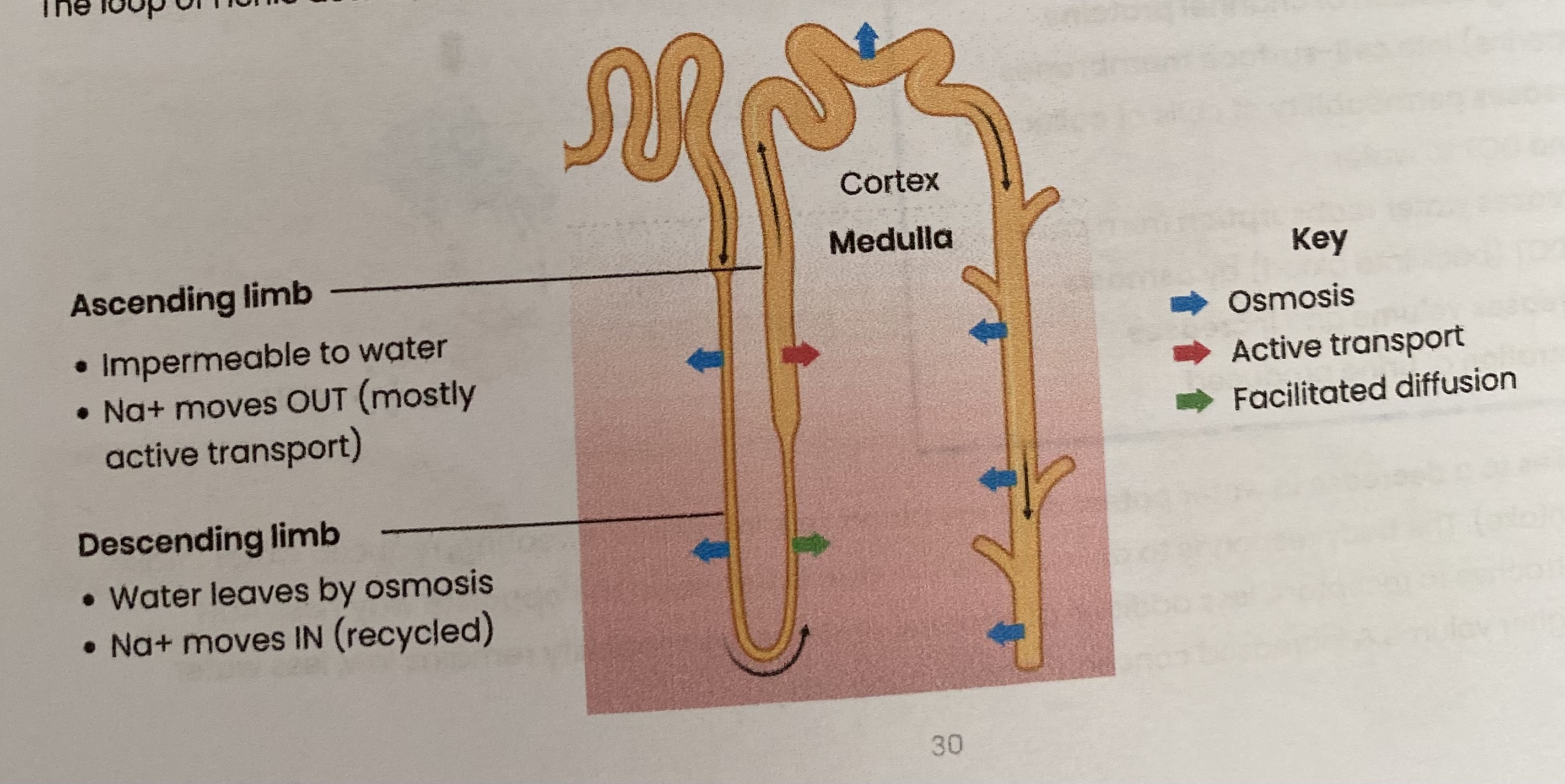
Suggest why animals needing to conserve water have long loops of Henle (thick medulla)
more Na+ moved out= Na+ gradient is maintained for longer in medulla/ higher Na+ conc
so water potential gradient is maintained for longer
so more water can be reabsorbed from collecting duct by osmosis
Describe the reabsorption of water by the distal convoluted tubule and collecting ducts
water moves out of distal convoluted tubule & collecting duct by osmosis down a water potential gradient
controlled by ADH which increases their permeability
What is osmoregulation?
control of water potential of the blood (by negative feedback)
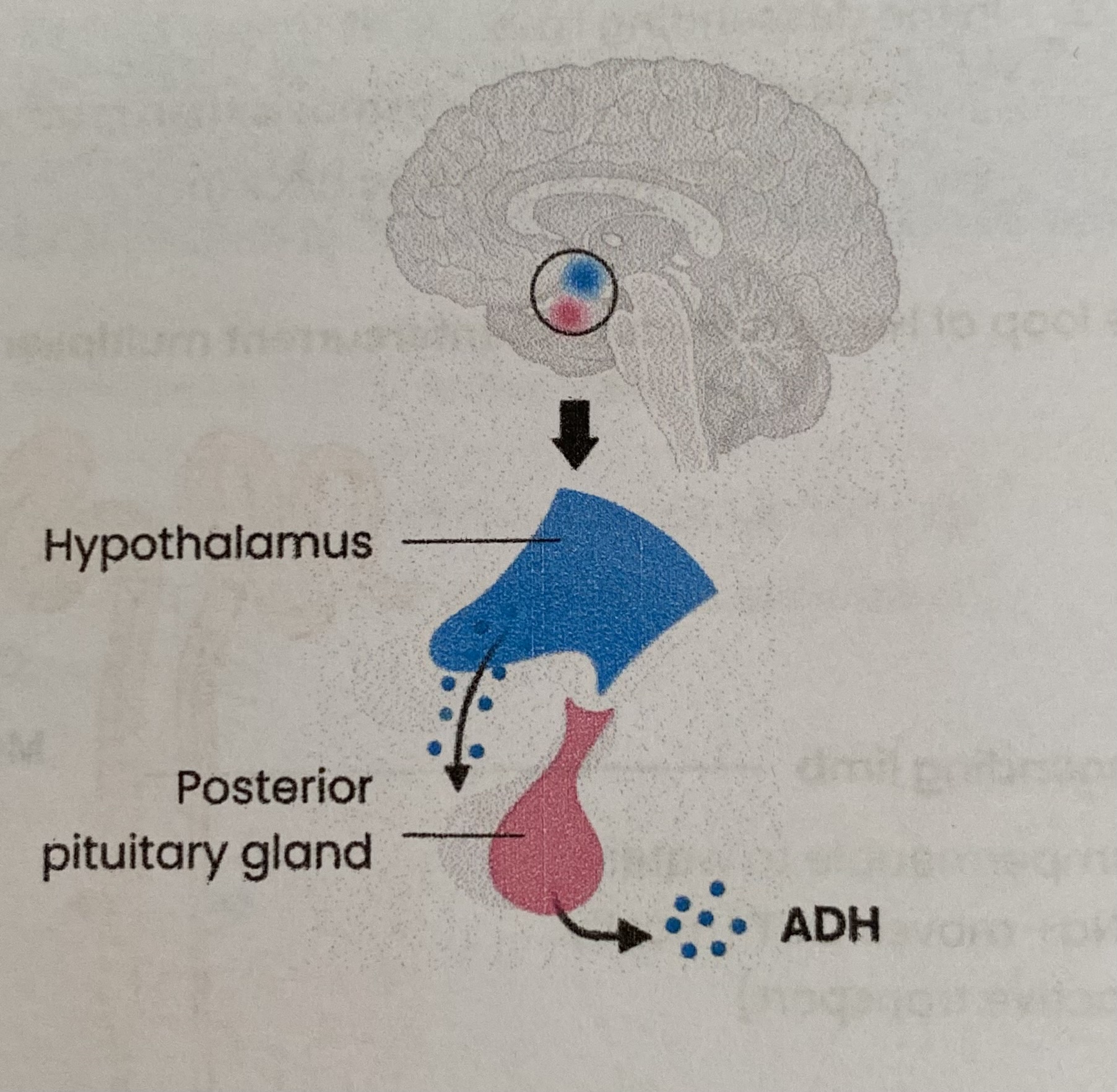
Describe the role of the hypothalamus in osmoregulation
Contains osmoreceptors which detect increase OR decrease in blood water potential
Produces more ADH when water potential is low OR less ADH when water potential is high
Describe the role of the posterior pituitary gland in osmoregulation
secretes (more/ less) ADH into blood due to signals from the hypothalamus
Describe the role of antidiuretic hormone (ADH) in osmoregulation
Attaches to receptors on collecting duct (and distal convoluted tubule)
Stimulating addition of channel proteins (aquaporins) into cell-surface membranes
So increases permeability of cells of collecting duct and DCT to water
So increases water reabsorption from collecting duct/ DCT (back into blood) by osmosis
So decreases volume and increases conc of urine produced
The above applies to a decrease in water potential of the blood (e.g. increases sweating, reduced water intake, increased salt intake). The body responds to an increase in water potential in the opposite way (less ADH secreted, less attaches to receptors, less addition of channel proteins, permeability remains low, less water reabsorption, higher volume & increased conc of urine etc)