Radiology and Radiography (2036DOH)
1/90
Earn XP
Description and Tags
bruh idk what even to dooo
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
what is radiology?
the specialty concerned with radiation for the diagnosis and management/prediction of disease
bitewing radiographs are also known as…
interproximal radiographs
what is a periapical radiograph?
x-ray that includes the tooth from root to tip
what are the two techniques for the periapical radiograph?
paralleling technique
bisecting angle technique
what is an x-ray?
a form of electromagnetic radiation with a short wavelength that can cause ionisation and penetrate through solids
what are some characteristics of an x-ray itself?
high energy waves
no mass
neutral charge
travels at the speed of light
invisible
travels in a straight line
can’t be focused into one point
causes fluorescence
harmful to living tissue
what is ALARA? (IMPORTANT)
as limited as reasonably achieved
term used for radiation safety
along with ALARA (radiation safety), what are some other key areas to consider when taking a radiograph?
infection control
radiographic technique (knowledge and accuracy = correct technique)
name a federal body that regulates radiation
Australian radiation protection and nuclear safety agency: radiation protection in dentistry
why are radiographs essential in dentistry?
IMPORTANT WILL SHOW UP IN EXAM
for diagnosis
treatment planning (eg caries, perio disease, cyst, cracked tooth)
monitoring (bone graft progression, edodont treatment etc)
no exposure to x-rays can be considered completely risk free, so the use of radiation by dentists is accompanied by…
a responsibility to ensure appropriate protection
no dental examination is complete without…
dental radiographs
an intraoral full-mouth examination may or may not involve ________ and ________ radiographs based on your judgement for the patient treatment management
periapical
bitewing
______ ____ + _________ _______ → ________ → ________
clinical exam
radiographic imaging
diagnosis
treatment
list some indications for taking a radiograph
IMPORTANT WILL SHOW UP IN EXAM
primary dental caries
recurrent dental caries
periodontal disease
periapical lesions
endodontics (root canal)
extraction/lesions in bone
advantages of taking periapical radiographs
IMPORTANT WILL SHOW UP IN EXAM
shows entire tooth from top of occlusal surface to 2/3mm below root
shows bony contour (if bone loss in perio disease eg)
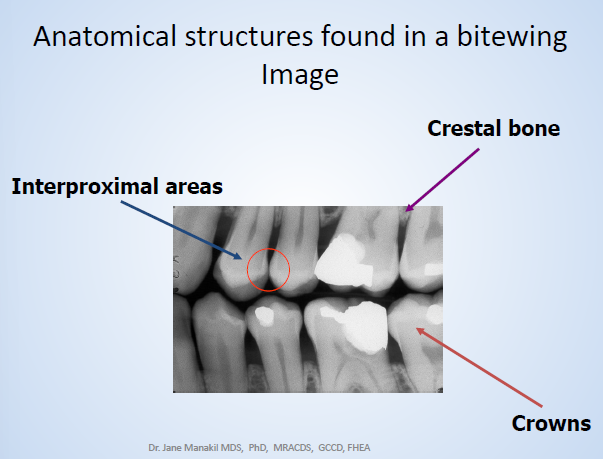
describe the bitewing radiograph
IMPORTANT WILL SHOW UP IN EXAM
shows the upper and lower teeth in occlusion and the interproximal crestal bone view
good for detecting interproximal caries
also shows crestal bone loss
also shows defect in margins
what does OPG stand for and describe it’s benefit
orthopantomograph
overall status of pt (with age, gender)
what is the bitewing radiograph used for?
examining interproximal surfaces of teeth
useful for detection of dental caries/alveolar bone levels/restoration contours
flip over for anatomical structures found in a bitewing image
radiolucency = __________
demineralisation
radiolucency is the darkening in an x-ray
radiopacity = ____/________ _____
crown/amalgam filling
radiopacity means the lighter colour
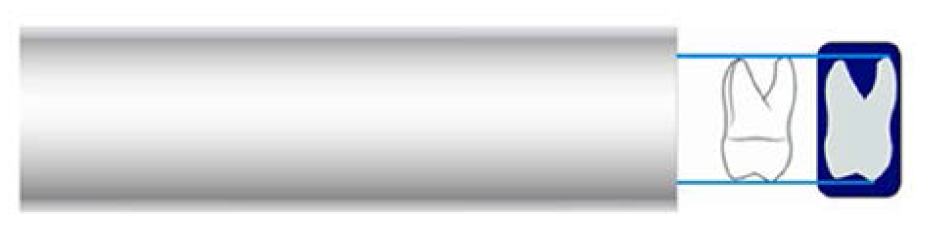
photostimulable phosphor plates (PSP) - how is the image captured and what sizes are available
image captured on the plate is analog info - then converted to a digital format when the plate is processed - INDIRECT IMAGING TECHNIQUE
2 sizes, 1 (child), 2 (adult)
describe the PSP components
polyester base coated with crystalline halide emulsion that converts X-radiation into stored energy
energy in the crystals is released as blue fluoro light when PSP is scanned with helium-neon laser beam
the PSP has two sides, the tube and the tongue side. describe the tube side
white/blue colour (lighter colour)
always faces the radiation source (tube head)
what do receptor holders/positioners do?
hold image receptor in place for exposure in intraoral radiographs
point of entry for the central ray should be in the middle of the image receptor
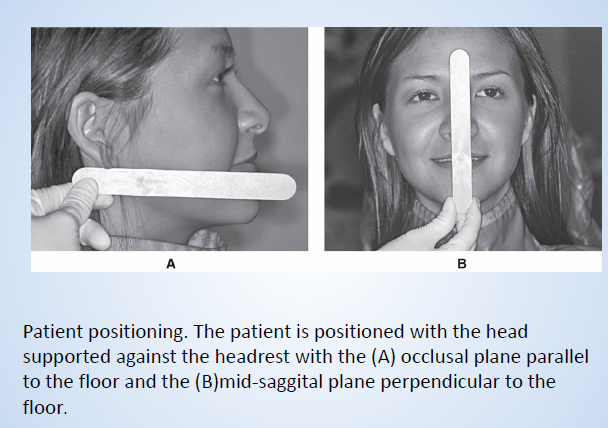
pt position for bitewing
head supported against the headrest
occlusal plane parallel to floor
mid-sagittal plane perpendicular to the floor
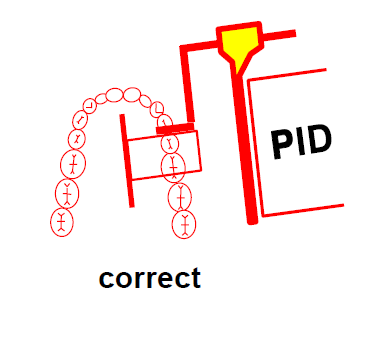
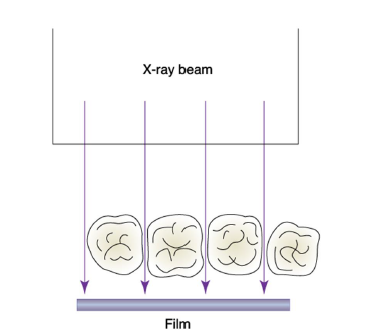
describe horizontal angulation
directing x-ray beam through interproximal spaces
must be positioned parallel to teeth of interest so central ray will also strike the image receptor perpendicularly
if central ray not directed through contacts, overlap of premolar/molar contacts occurs (want to prevent this)
vertical angulation for bitewing in degrees
5-8 degrees either way on actual x-ray machine (one mark after 0)
basically controls height (want top and bottom crowns and alveolar crests in one shot)
basic principles of bitewing
film placed parallel to crowns (on biting surface)
x-ray beam directed through contacts of teeth
patient bites on bitewing tab or film holder
steps for bitewing
receptor placed inside mouth (parallel to crowns of max and mand pos teeth)
pt stabilises receptor by biting on tab/bitewing holder
central ray of x-ray directed through contacts of pos teeth and at 5-8 degree vertical angle
what can be used to stabilise tab/bitewing holder in edentulous areas?
cotton rolls
tab can also be moved forward/back on film to get better support
on a premolar bitewing, the contact between the ______ and the ____ ______ should be clearly visible
canine
first premolar
describe positioning of molar bitewings
centred on 2nd premolar + 1st molar (horizontal) perpendicular to contact between 1st and 2nd molar
PSP shouldn’t be too far back (focus on edentulous area - waste of exposure)
correctly exposing intraoral receptors has 4 basic steps. list them
receptor placement
vertical PID (cone) angulation
horizontal PID (cone) angulation
centring of central ray
are the sensor plate holders for bitewing and periapical paralleling technique the same? why or why not?
not the same
bitewing is more flat
paralleling is rounded shape
describe the peri-apical image and its purposes
shows entire crown and root from occlusal surface/incisal edge to 2-3mm below root to show periapical bone
gives vital info in diagnosis of most common dental diseases: caries, tooth apical lesions, perio bone loss, teeth fractures and bone anatomy
used to diagnose pathologic conditions of the tooth, root and bone and tooth formation and eruption
essential in endodontic and oral surgery procedures
what are the 2 techniques for periapical x-rays?
paralleling
bisecting
periapical radiographs can be taken to examine only….. or they may be prescribed as a…. which is ____
selected areas
full mouth series of radiographs
rare
for periapical radiographs, where should the ‘a’ on the sensor plate be ideally positioned?
at the crown end of the scan - wont get in the way of what you want to see at the root
principle 1 of 5 of radiography
x-rays should be emitted from the smallest source of radiation as possible
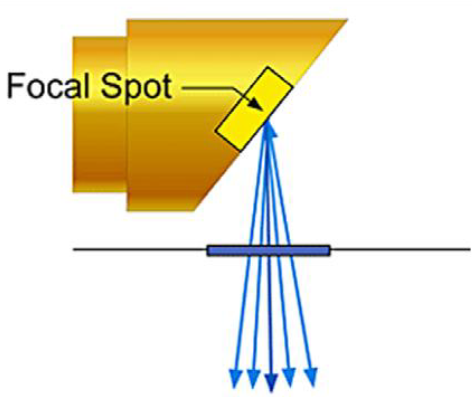
principle 2 of 5 of radiography
the x-ray source-to-object distance should be as long as possible (PID - position indicating device - fancy for the cone)
principle 3 of 5 of radiography
the object-to-receptor distance should be optimised based on the procedure
keep in mind technique and positioning for this
principle 4 of 5 of radiography
the receptor and long axis of the tooth should be parallel to each other
for parallel technique!
principle 5 of 5 of radiography
the x-ray beam should be directed perpendicular to the tooth and receptor
functions of long cone (PID)
beam alignment/angulation
vertical
horizontal
point of entry
centring exposure field
subcategories of horizontal and vertical angulation
vertical
positive
negative
horizontal angulation
positive angles of the PID is generally used for …. and …., and a negative angle is used for …
bitewing exposures
periapical exposures of the maxilla
periapical exposures of the maxilla
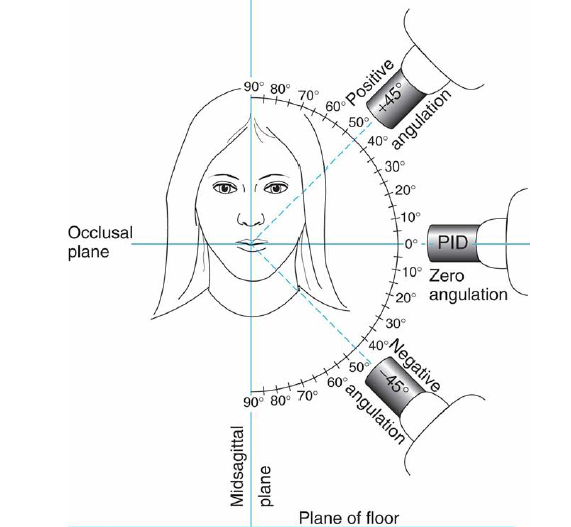
zero angulation is achieved when…
the long axis of the PID is directed parallel to the floor
positive angulation is when the PID is pointed….
negative angulation is when the PID is pointed…
toward the floor
toward the ceiling
(for parallel technique) the instruments used to hold the film parallel to the teeth are…
plastic bite-blocks (Rinn XCP)
indicator rods
plastic locator rings

what do receptor holders/positioners do?
hold the image receptor in place for exposure for intraoral radiographs
the point of entry for the central ray (paralleling technique) should be…
in the middle of the image receptor
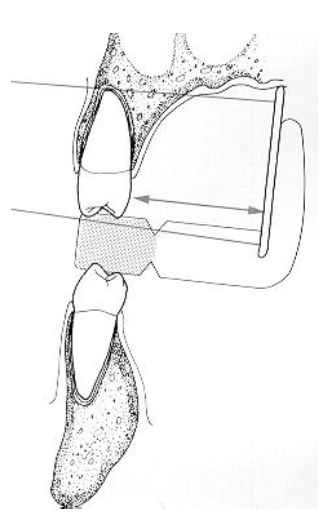
describe the film placement within Rinn XCP holder
stabilises sensor plates in the holder and position behind teeth of interest
place sensory plates parallel to long axes of teeth
stabilise holder against occlusal surfaces of teeth being radiographed (two point contact)
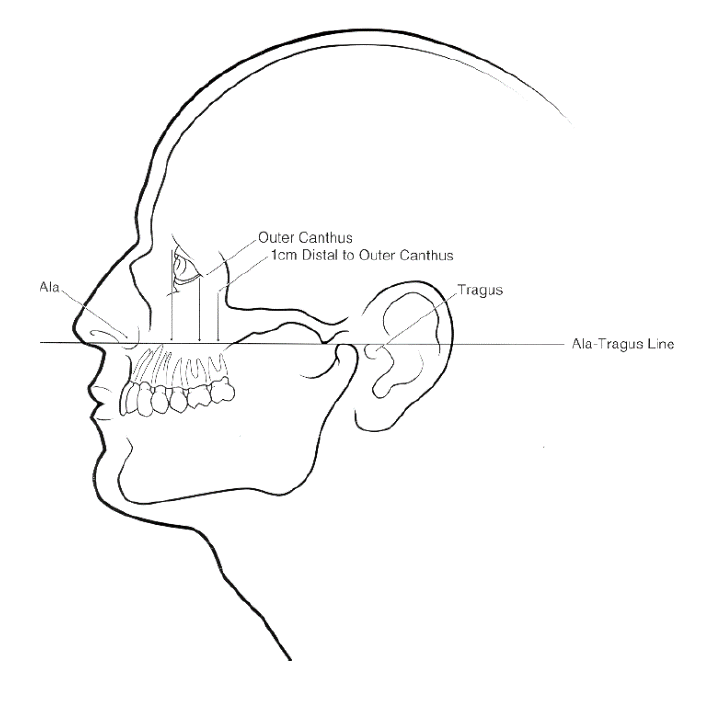
location of apices for maxillary and mandibular teeth
max: a-t line
mand: 1 inch, above inferior border of mandible
central ray point of entry for different teeth
central/laterals - side of nose
canine - side of nostril flap (ala of nose)
premolar - perpendicular line from pupil
molar - outer corner of eye
basic rules of the paralleling technique
position sensor plate so it covers the teeth, parallel to the long axis of the tooth
plate should be placed in rinn xcp holder - and have pt bite on the bite block of the holder
centre x-ray beam on sensor plate to ensure all areas of the plate are exposed
vertical angulation - central ray of x-ray beam perpendicular to the film and long axis of the tooth
horizontal angulation - direct the central ray of the x-ray beam through the contact areas between the teeth
anterior films are always placed _______
posterior films are always placed _________
identification letter ‘a’ on the film is always placed…
always the place the film parallel to…
vertically
horizontally
in the slot of the film holder (dot in the slot)
long axis of the teeth
for paralleling technique, the teeth must be in contact with…
the bite block
make sure pt doesn’t just close lips tight around bite block and not bite
for posterior films, the film should be equidistant from the…
teeth in an anterior-posterior direction
advantages of paralleling technique
decreased primary beam divergence
less exposure to pt
less penumbra (shadow/blurring)
less dimensional accuracy
no superimposition of other anatomical structures - central beam perpendicular to long axis of molars
reduces exposure to thyroid gland and lens of eye (not in path of primary beam)
easier to standardise
pt doesn’t have to be positioned (supine fine)
when is the bisecting angle technique used/recommended?
alternative to paralleling for taking peri-apical images
paralleling technique recommended for routine peri-apical radiography but sometimes difficult due to pt anatomy (like small mouth) / lack of co-operation
the intra- oral peri-apical exposure with bisecting angle techniques can use _______ or ______ ______ to stabilise the film in position
holders
patient finger
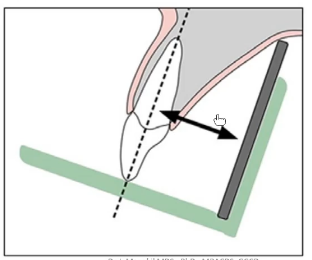
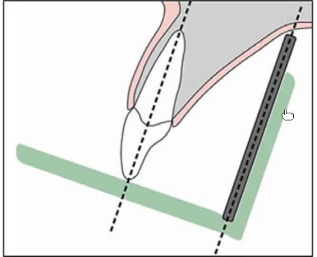
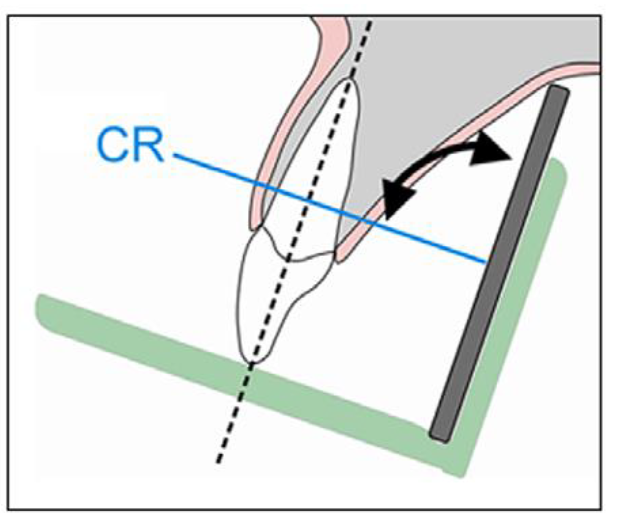
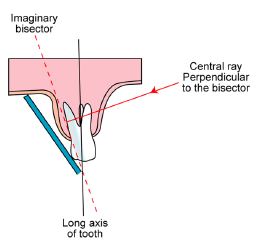
where the the bisecting plane? and the angle formed by? x-ray central beam?
halfway between plane of dental film and long axis of tooth
angle formed by long axis of teeth and plate is bisected!
central ray should be directed perpendicular to bisecting plane (90 degrees)
flip over for bisecting plane image
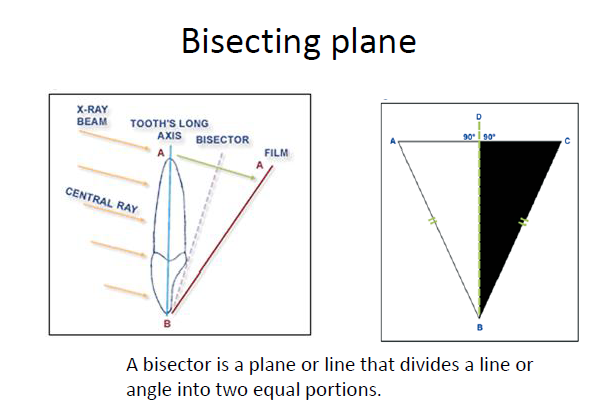
the central ray meets the bisector angle (dotted line) at a 90 degree angle
the ______ angulation remains the same whether you are using the paralleling or the bisecting technique
horizontal
describe the correct horizontal angulation of the central ray for the bisecting angle technique and what happens if it is incorrect
central ray 90 degrees to curvature of arch and through contact areas of teeth
if incorrect: overlapped contact areas, can’t be used to examine the interprox.
does the vertical angulation differ based on technique used? if so, which techniques and how?
PARALLELING
vertical angulation of central ray is perpendicular to film and long axis of tooth
BISECTING
vertical angulation directed perpendicular to imaginary bisector
what happens if the vertical angulation is incorrect vs correct?
incorrect: image isnt same length as tooth (longer or shorter)
correct: image same length as tooth
shorter image happens when angle is too large and vice versa for longer image
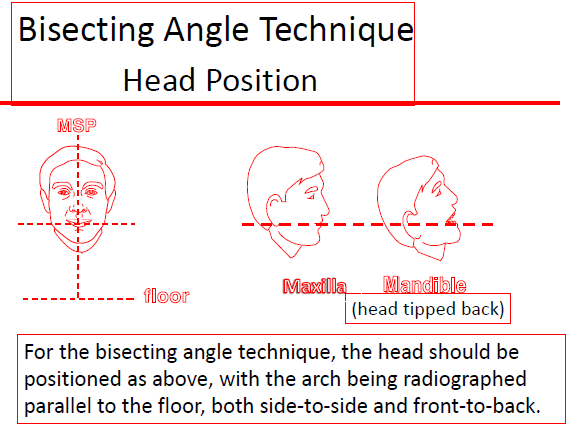
flip over for head position for bisecting angle technique
advantages of bisecting angle technique
more comfy: film placed in mouth at angle to long axis of tooth, sensor doesnt rlly touch the tissues as much
sensor holder isnt needed - pt can hold using finger
sensor can be angled to accommodate different anatomies (no anatomical restrictions)
good for when paralleling cant be used (like if pt has smol mouth or low palatal vaults
disadvantages of bisecting technique
increased exposure to radiation so should only be used when necessary
superimposition of anatomical structures in the image
more chance of distortion (bc film and teeth arent parallel)
harder to position x-ray beam - bc ring not used so difficult to visualise where it should be directed
film less stable when pt uses finger - more chance of moving
more chance of being a short/long image so not easy to reproduce image for review
anatomical situations that interfere with radiography
shallow palate
large palatal torus
shallow/tender floor of moth
short lingual frenum (tongue tie)
similarities between BSA and paralleling
horizontal angulation
film positioning in arch
alignment of central ray to cover film
preparation for BSAT
prepare operatory with infection control barriers
turn on x-ray machine and check basic settings
discuss wtith pt - med history and area of concern
determine no. + type of images to be exposed
inform pt of procedure
positioning the pt for BSAT
seat pt comfy in the chair - back upright and head supported
ask pt to remove glasses and bulky earrings
have pt remove pros
drap pt with lead apron + thyroid collar
wash hands and put on clean exam gloves
proceed with radiographic technique
what type of film holder can be used for the BSAT?
anterior: finger
posterior: snap ray holder
what are some variables you need to consider to produce quality dental radiographs?
knowledge and attention to methods of exposing dental x-ray film, digital sensors within oral cavity
using appropriate technique
setting radiation exposure variables
positioning pt properly
selecting suitable size of PSP/digital sensor
finding out how receptor is to be positioned/held in place
list some errors that may occur when taking a radiograph
pt prep errors
PID angulation/positioning errors
sensor placement
describe the pt prep error
should always explain procedure to pt and tell pt clearly what they can do to help get a quality image and avoid retakes and unnecessary exposure
most common error is movement
factors that contribute to this: discomfort, unsupported head position, gagging/swallowing, or pt disability
describe the operator position error
if you have incorrect position of the tube head you might get elongation or shortening of the image (vertical angle bad)
superimposition (if horizontal angle bad)
cone cut - psp plate not exposed bc not correlating with the cone
when does elongation happen in the BSAT and the paralleling technique?
note: generally for vertical angulation
BSAT
under angulated or too shallow relative to bisecting plane
paralleling
vertical angulation not perpendicular to long axis of teeth
when does foreshortening of the radiographic image happen?
if PID over-angulated (too steep) relative to bisecting plane