L15 Cardiac Muscle
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
What are key structural features of cardiac muscle cells? (4)
Single nucleus per cell
Branched cells
Many mitochondria
Joined by intercalated disks
Less organized sarcomeres
What do intercalated disks contain? (2)
Desmosomes and gap junctions.
What is the function of desmosomes in cardiac muscle?
Connect intermediate filaments and transmit mechanical force between cells
What is the function of gap junctions in cardiac muscle?
Electrically couple cells — allow APs to pass directly cell-to-cell.
What do tight junctions and adherens do
stop paracellular transport
Transmit force and connect actin filaments
What acts as the main pacemaker of the heart?
The sinoatrial (SA) node. it generates rhythmicity
How long is ventricular AP and what is its resting potential
250ms and resting potential -90mV
What do the purjunkie fibers and bundle of hiss do
They are cardiac tissues specialized for transmission of AP. They transmit electrical signals from the ATV to other parts of the heart
Transmission of AP from the ATV
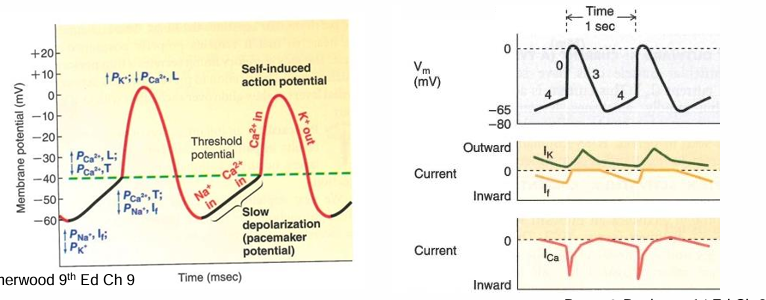
Explain pacemaker activity/AP step by step (8)
Pacemakers don’t have a stable resting membrane potential
Depolarization to threshold -40mV opens VGCC L type channel
Calcium influx in pacemaker cells
Repolarization occurs from delayed closing of L type channels and opening of Kv channels
Potassium moves out causing membrane potential to be more negative
Closure of Kv channels reduce potassium permeability causing depolarization
repolarization opens the funny channel (HCN- hyperpolarization cyclic nucleotide channels)
Sodium comes in via the funny current If making the cell more positive

What initiates the pacemaker potential?
Decrease in K⁺ permeability, Na⁺ influx through the funny current (Iₑf), and slight Ca²⁺ influx.

Explain ventricular AP step by step
Cell has a very negative resting potential -90mV
Nav channels open resulting in quick sodium influx making the cell more positive
Nav channels closing causes a slight repolarization (down tick)
L type calcium channels open causing a plateau as its balanced by potassium efflux
Closing of sodium channels and opening of potassium voltage channels repolarizes cells

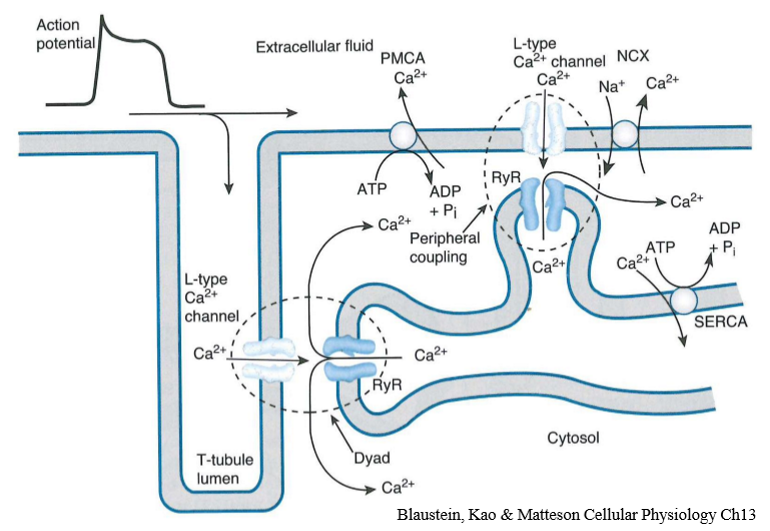
Explain excitation contraction coupling of cardiac muscle (4)
Calcium enters cell through L type channels causing calcium induced calcium release of calcium store in the sarcoplasmic reticulum (CICR
Calcium is released through ryanodine channels which are a calcium gated calcium channels
Calcium then binds troponin, moves tropomyosin so actin myosin cross bridges can form
Calcium is removed by SERCA back into the SR, plasma membrane calcium ATPase and sodium calcium exchanger
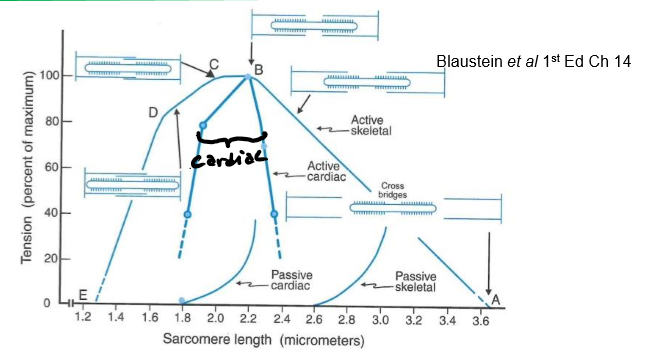
How does the cardiac length–tension curve differ from skeletal?
Active force curve is narrower.
Passive force curve increases steeply.
Relaxed cardiac muscle is stiffer due to more connective tissue.
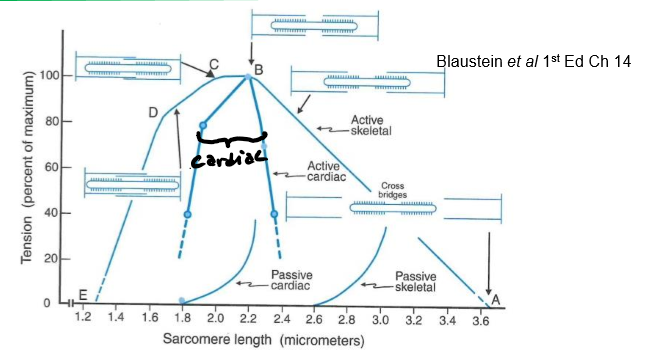
What is the Frank Starling law
Increased cardiac filling (preload) stretches fibers → improved actin–myosin overlap → stronger contraction → increased stroke volume.
What neurotransmitter increases heart rate?
What neurotransmitter decreases heart rate?
Noradrenaline (NA).
Acetylcholine (ACh).
How does noradrenaline increase HR? (4)
NA binds to β₁-adrenergic receptors activating Gs which increases cAMP)
Decreases K⁺ permeability at rest
Increases funny current (Iₑf)
Depolarizes pacemaker cells faster → quicker threshold → faster HR
How does ACh slow heart rate?
ACh: M₂-muscarinic receptors (Gi → ↓cAMP)
Increases K⁺ permeability (hyperpolarization)
Decreases funny current (Iₑf)
Slower depolarization to threshold
What is inotropy?
What increases it?
The force of cardiac contraction.
Sympathetic stimulation (NA, adrenaline)
Digitalis
Increased extracellular Ca²⁺
What is chronotropic
Increase in heart rate
How do β₁-adrenergic receptors increase inotropy?
Activate Gs → ↑cAMP → activate PKA (Protein Kinase A)
PKA phosphorylates L-type Ca²⁺ channels → more Ca²⁺ entry
PKA increases SERCA activity → more Ca²⁺ in SR
More Ca²⁺ release from RyR → stronger contraction
What are β₁-adrenergic receptors
G protein coupled receptors linked to Gs
How does ACH have negative inotropic actions
It activates m2-muscurinic receptors linked to Gi which inhibit PKA preventing calcium release