Lecture 15: Minor Ailments & Responding to Symptoms in Community Pharmacy | Allergy & Hay Fever
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
18 Terms
What is allergy?
Immune system reacting to a normally harmless substance
Hypersensitivity disorder
Allergen - a substance that triggers allergy
Risk factors - heredity, gender, race and age
Environmental factors - pollution allergen levels aand dietary changes
Atopy:
Genetic predisposition to make IgE antibodies in response to allergen exposure
Atopic disorders most commonly affect the nose, eyes, skin & lungs
Allergic rhinitis (e.g., hay fever), allergic asthma, atopic dermatitis (eczema) - most common manifestations of atopy
Examples
Typical Allergens
Proteins e.g. foreign serum, vaccines
Plant pollens e.g. rye grass, ragweed, timothy grass
Drugs e.g. penicillin
Foods e.g. nuts, seafood
Insect products e.g. bee venom
Mold spores
Allergic reactions
Allergens enters the body > activates B cells (plasma cells) to produce immunoglobulin (IgE) > antibodies to the allergen: released into blood stream, bind mast cells which become primed
Future exposure to the allergen:
Primed mast cell degranulation
Histamine release into local tissue
Type I (immediate) hypersensitivity reaction
Allergy vs Sensitisation
Sensitisation
Initial ‘learning’ phase of an allergic response (primes immune system to react to a specific allergen)
Occurs before the developement of Type I hypersensitivity reaction
Asymptomatic or mild reaction
Allergic reaction
Repeated exposure - more serious reaction
Limited exposure to very small amount of allergen can trigger a severe ‘full-blown’ reaction
Type I hypersensitivity reaction:
Earlu phase (seconds/minutes < 1 hour) - rapid degranulation releasing histamines, leukotrienes, prostaglandines and other inflammatory mediators. Severe cases ( anaphulaxis)
Late phase (4-12 hours) - inflammation sustained by recruitment of eosinphils, neutrophils, basophils, moncytes and Th2 cells
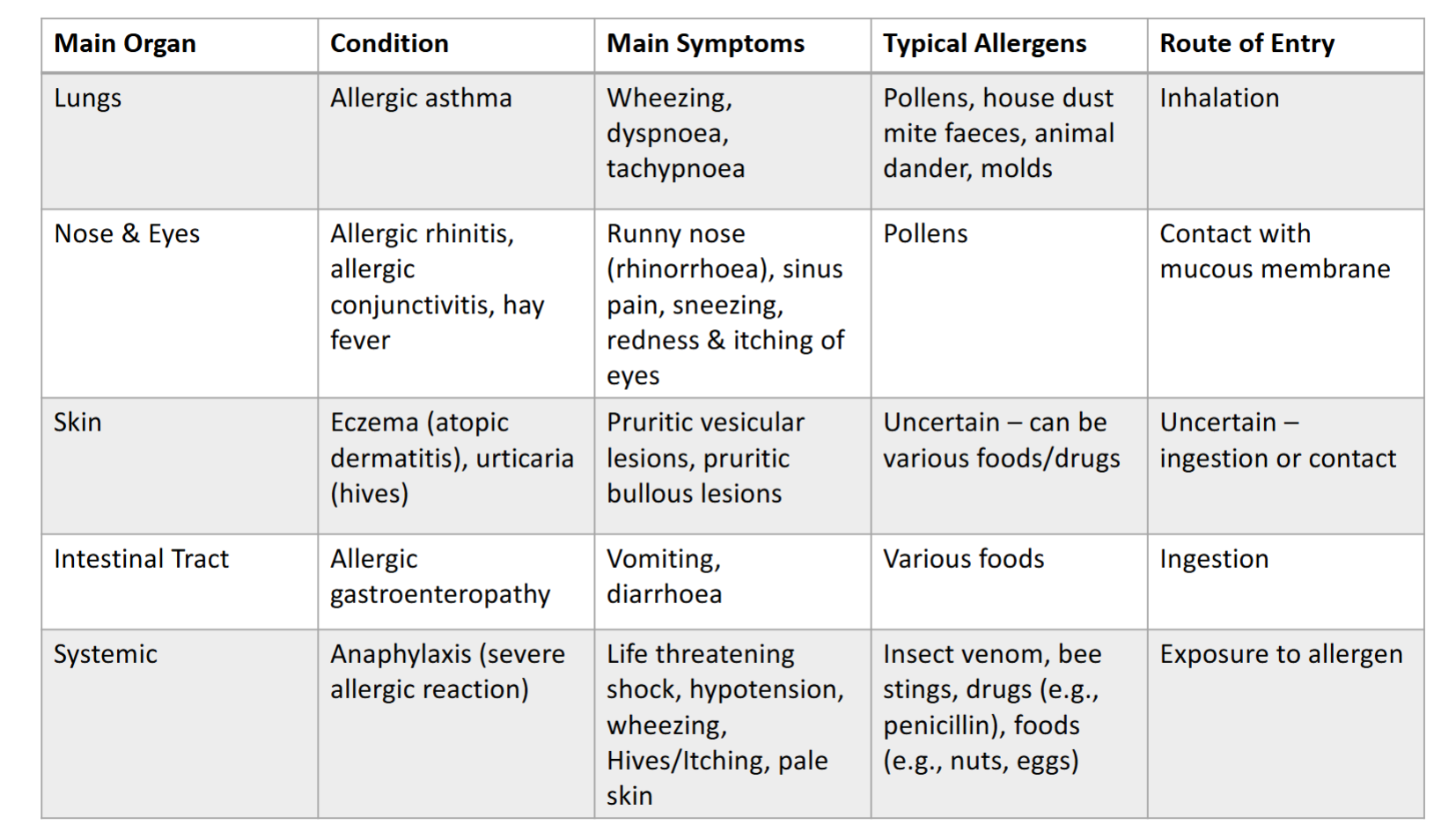
Allergic symptoms
Type I hypersensitivity:
Early phase symptoms:
Vasodilation > redness ad swelling
Increased muscular vascular permeability > fluid leakage, wheals
Smooth muscle contraction > bronchoconstriction
Mucus secretion > runny nose, congestion
Late phase symptoms:
Examples: prolonged symptoms like asthma, dermatitis, chronic rhinitis
Actions of histamine on H1 receptors
Local hormone (autocoid)
Blood vessels - dilatation + capillary increased
Smooth muscle - contraction
Stimulation of sensory nerves
Increased gland secretion
Anaphylactic shock - circulation collapse & bronchoconstriction - largely mediated by histamine
Prevention
Allergen avoidance - good history taking, read labels
Serious allergic reaction - medical ID tag, carry emergency medicines
Allergic Rhinitis
Inflammation of the inside of the nose resulting in sneezing attacks & nasal discharge or blockage
Can have profound impact on quality of life, work and education
Long-term problems due to inflammation
Nasal polyps
Sinusitis
Middle ear infections
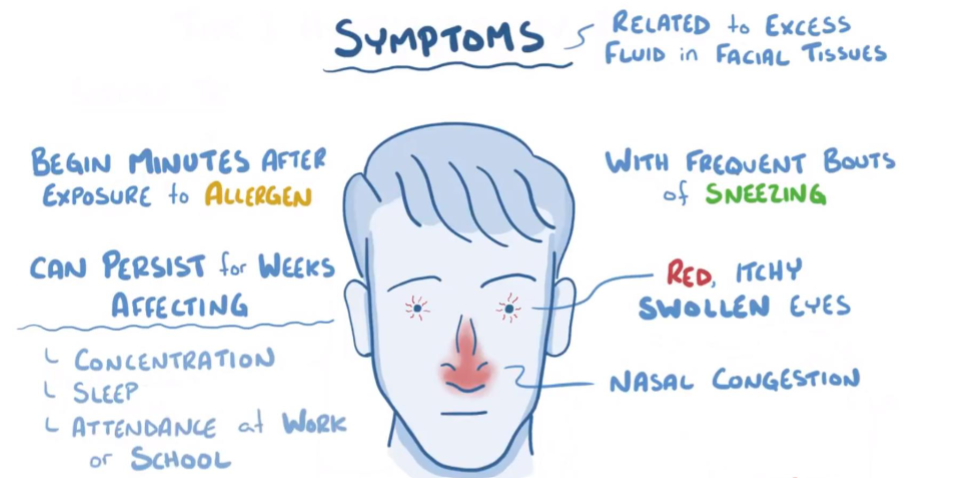
Allergic Rhinitis
Seasonal (hay fever)
Usually outdoor allergens, pollens, moulds
Symptoms > 1hr a day
Perennial
Indoor allergens e.g. house dust mites, moulds, animals
Symptoms year-round constant
Occupational
Allergens at work e.g. dust from eood, flour, latex
Management
Non-pharmacological
Allergen avoidance
Hay fever
Monitor pollen counts
Keeps windown closed
Persistent allergic rhinitis
Exclude pets from certain living areas
Acaricidal sprays & bedroom cleaning regimens
Pharmacological
H1 receptor antagonists
Mast cell stabilisers
Intranasal corticosteroids
Intranasal decongestants
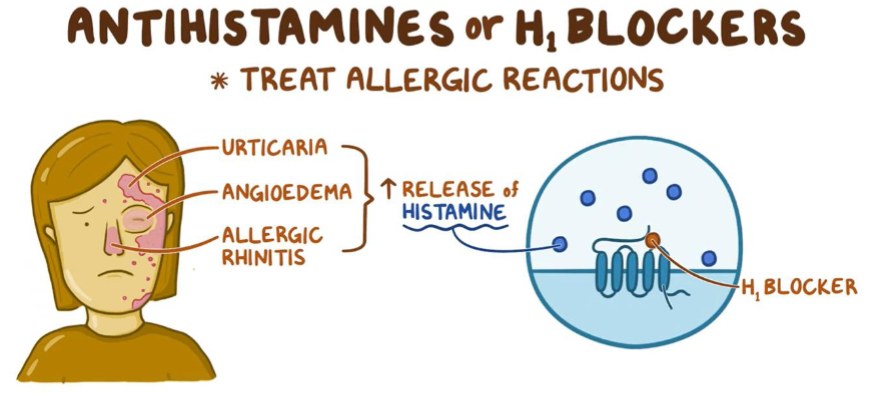
Antihistamines
H1 receptor antagonists
Reversible binding to the H1 receptor
More efective at preventing than reversing symptoms
Block triple response of Lewis
Partially prevent hypotensive effect
No effect on gastric secretions
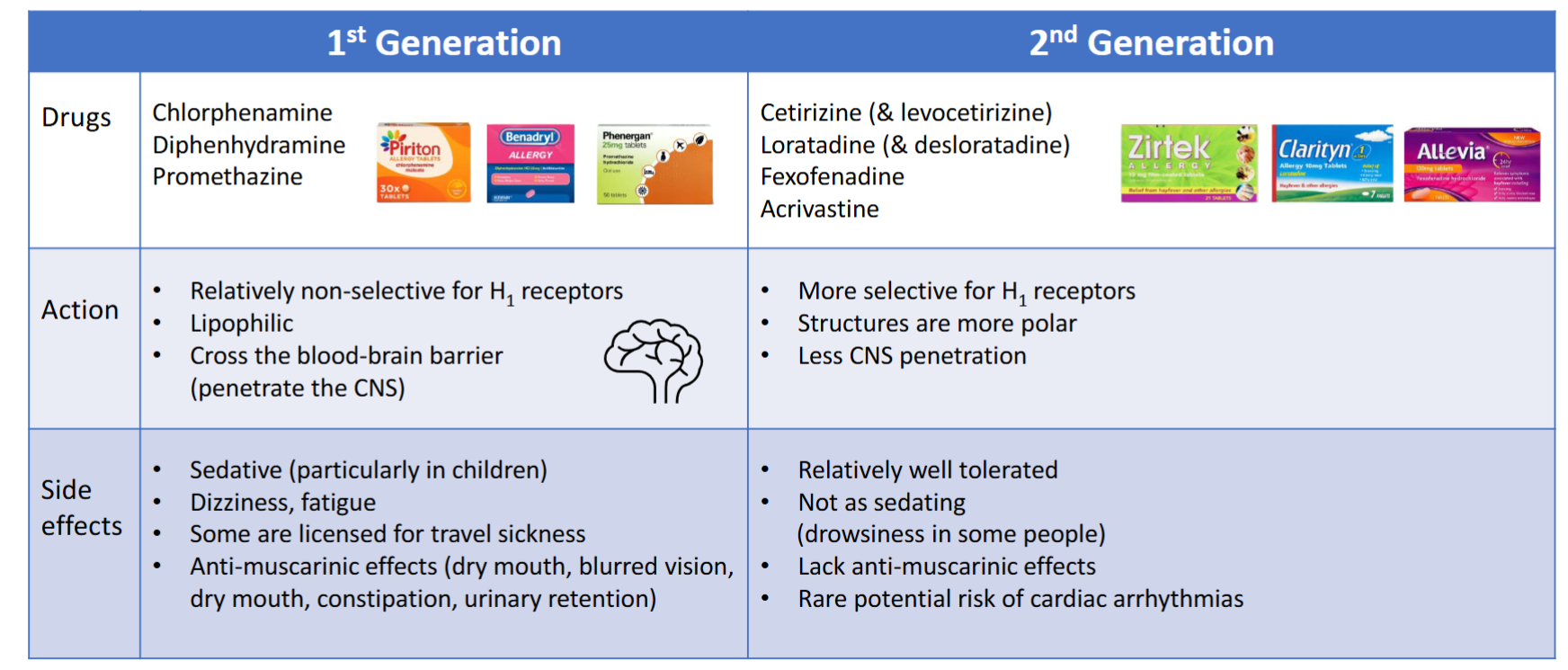
Antihistamine examples
Usually first line
Oral (systemic action)
2nd generation preferable to 1st
Some available as solid & liquid dosage forms licensed for children & adults
GSL, POM & P
Add eye drops and/pr intranasal corticosteriod sprays nasal, if eye or nasal symptoms persist
Eye drops
Mast cel stabilisers
Prevent histamine release - need to be used regularly while exposed
Sodium cromoglicate
For itchy & runny eyes
P medicine
Intranasal Corticosteriods
Beclometasone, budesonide, fluticasone, triamcinolone, mometasone
Most effective treatment for allergic rhinitis
Reduce local inflammatory response
Improve rhinorrhea, itchiness, sneezing, congestion
Systemic absorption is minimal (local action)
Advantage reduces side effects compared to oral dosage forms
Several days to obtain effect & several weeks for full effect
Can be used with oral antihistamines
GSL, P & POM dependent on number of unit doses
GSL, P only licensed for adult only
Under 18 years old - POM
Local Vasoconstrictors ‘nasal decongestants’
Phenylephrine (works within ~15 minutes, short-acting, lasts up to 4 hours), oxymetazoline, xylometazoline (works within a few minutes, lasts up to 8 hours)
Mimic noradrenaline, bind alpha-adrenoreceptors to constrict dilated arterioles in the nasal mucosa & reduce airway resistance
Nasal drops or spray
Rapid action
Reduced systemic effects (compared to oral decongestants)
Not recommended for use with antihistamines
Rhinitis medicamentosa
Rebound congestion following vasoconstriction (avoid by 7-day max. use limit)
Pathophysiology unknown, possibly due to decreased local production of noradrenaline
Only occurs with local vasoconstrictors
Recovery reported to take up to a year in cases of long-term overuse
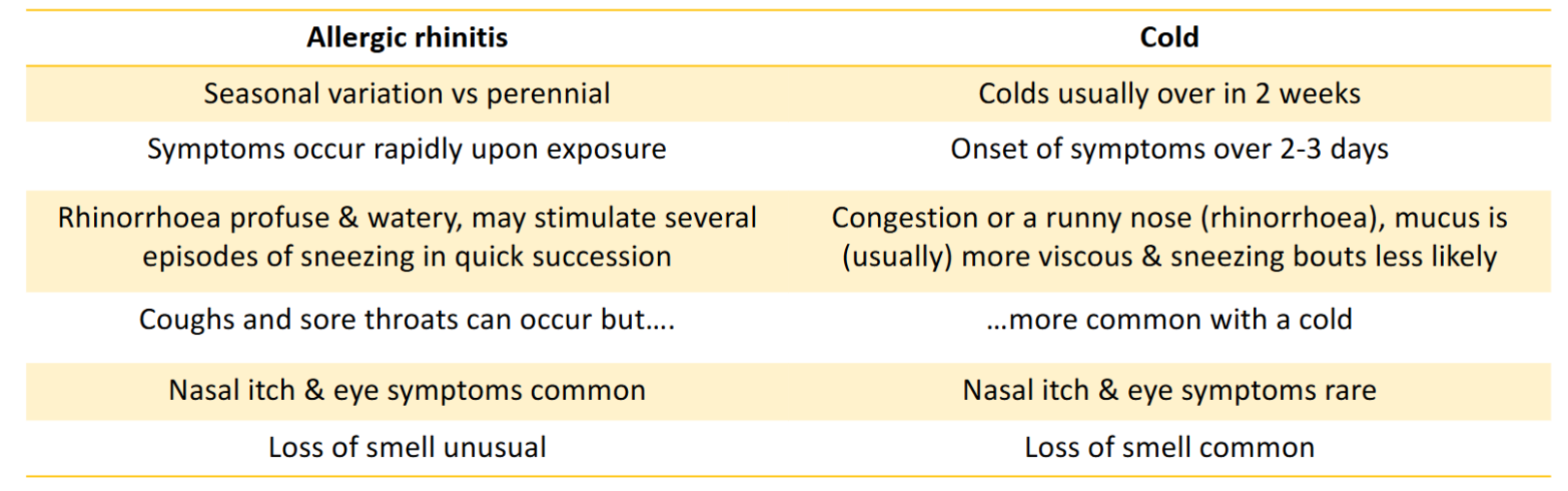
Allergic rhinitis or cold?
Family history of atopy (asthma, eczema, hay fever)
Clinical symptoms & when they get worse
When to refer
Where allergic rhinitis symptoms aren’t controlled despite antihistamine, eye drops & nasal corticosteriod:
Sleep disruption
Impairing ability to work/study
Nasal obstruction fails to clear
Symptoms only appearing on 1 side
A blocked nose with no other symptoms
Orbital cellulitis - infected eyelids causeing swelling, pain, photophobia, recurrent nosebleeds (epistaxis)