Blood Flow & Metabolism
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
Describe the process of gas exchange between the alveoli and the pulmonary capillaries, including the principles of diffusion and perfusion.
Analyze the pathophysiology of respiratory disorders that affect pulmonary blood flow and gas exchange, such as pulmonary embolism, pulmonary hypertension, and acute respiratory distress syndrome (ARDS).
Textbook of Medical Physiology, Guyton and Hall, 12th edition:
Chapter 38, Pg 477 - 484 (already in the AIRWAYS AND AIRFLOW SET)
Physiology, Costanzo, 6th edition:
Chapter 5, Pg 216 - 224
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
I. OVERVIEW: What Determines Pulmonary Blood Flow?
Pulmonary blood flow (Q) depends on:
Ventilation (V) — air reaching alveoli
Gravity — affects regional perfusion
Pulmonary Vascular Resistance (PVR) — resistance of pulmonary vessels
Right ventricular output
Local alveolar oxygen levels (hypoxic vasoconstriction)
Because the pulmonary circulation is low pressure and highly compliant, small changes in these factors greatly alter perfusion.
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
II. EFFECT OF VENTILATION ON BLOOD FLOW
Ventilation regulates blood flow primarily through alveolar oxygen levels.
1. Alveolar Hypoxia → Hypoxic Pulmonary Vasoconstriction
If a region of the lung is poorly ventilated (low PO₂):
↓ PAO₂ → local pulmonary arteriole constriction
This is opposite of systemic circulation, where hypoxia causes dilation.
Physiologic purpose
Diverts blood AWAY from poorly ventilated alveoli
Sends blood to better-ventilated areas
Optimizes V/Q matching
Pneumonia
Mucus plugging
Atelectasis
Poor ventilation → hypoxic vasoconstriction → ↓ blood flow to that region.
2. Global Hypoxia → Generalized Vasoconstriction
Global Hypoxia occurs in:
High altitude
Advanced COPD (due to to emphysema and chronic bronchitis)
In COPD, especially emphysema and chronic bronchitis (airways are fully constricted in chronic bronchitis):
Many alveoli are destroyed
Many have mucus plugging
Many have very low PAO₂
Hypoxia is diffuse, not isolated
Neonatal persistent pulmonary hypertension (PPHN)
Result:
Marked increase in PVR
Right ventricular strain → co rpulmonale
cor → Latin “heart”
pulmonale → Latin “pulmo/pulmonis” = lung
Literal meaning: “Heart condition caused by the lungs”
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
effect of gravity on pulmonary blood flow
III. EFFECT OF GRAVITY ON PULMONARY BLOOD FLOW
Gravity causes a vertical gradient in perfusion.
Apex (top) of lung
Lowest blood flow AND lowest pressure lowest pressure
V/Q ratio high (more ventilation than perfusion)
Base (bottom) of lung
Highest blood flow
Vessels distend under hydrostatic pressure
V/Q ratio low (more perfusion than ventilation)
Why this happens
Hydrostatic pressure in pulmonary vessels is lower than systemic, so gravity dramatically affects perfusion
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
what is the PVR at low and high volume
what is the PVR at FRC?
IV. PULMONARY VASCULAR RESISTANCE (PVR)
PVR is the resistance offered by the pulmonary vasculature to blood flow.
PVR is LOW at the Functional Residual Capacity (FRC).
FRC = the volume of air remaining in the lungs after a normal, passive exhalation.
1. Effect of Lung Volume on PVR High Lung Volumes (inspiration)
Alveoli enlarge → stretch alveolar vessels
Capillaries are compressed
→ PVR increases
Alveoli expand
Their walls stretch outward
This stretches—and compresses—capillaries embedded in alveolar walls
Capillary diameter decreases → capillary resistance ↑
Therefore: PVR increases
Low Lung Volumes (forced expiration)
Extra-alveolar vessels collapse
→ PVR increases
Elastic recoil decreases
Radial traction decreases
Extra-alveolar vessels become floppy
Their diameter decreases
PVR increases
Lowest PVR occurs at FRC
(where alveolar and extra-alveolar vessel diameters are both optimal)
3. At FRC (end of normal tidal expiration) (this is an explanation for what happens above)
The FRC is the sweet spot where:
A. Alveolar capillaries are not over-stretched
Alveoli are moderately inflated
Capillaries are open but not compressed
Alveolar vessel resistance is low
B. Extra-alveolar vessels receive enough radial traction
Lung elastic recoil is present
Surrounding parenchyma gently pulls vessels open
Extra-alveolar resistance is also low
C. The two opposing resistances cancel each other out
Alveolar capillaries: lowest resistance at moderate volume
Extra-alveolar vessels: lowest resistance at moderate volume
→ Total PVR = minimal at the midpoint between the extremes
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
sympathetic nervous system
SYMPATHETIC NERVOUS SYSTEM → TENDS TO DECREASE PVR
…but with some nuance.
Receptors involved β₂ receptors (dominant)
Located on pulmonary vascular smooth muscle
Activated by circulating epinephrine
Effect: Vasodilation → PVR ↓
epinephrine binds to b2 receptors
α₁ receptors (minor role)
Located on large pulmonary arteries
Activated by norepinephrine from sympathetic nerves
Effect: Vasoconstriction → PVR ↑ (small effect)
norepinephrine binds to a1 receptors to cause vasoconstriction.
Net effect Because the lung vasculature is thin-walled, compliant, and has low resting tone, β₂-mediated dilation dominates (fight or flight means you need more oxygen so vasodilation occurs)
Overall: sympathetic activation tends to ↓ PVR.
When does sympathetic tone really matter?
Exercise → CO ↑ → recruitment + β₂ dilation → prevents pulmonary hypertension
Shock → sympathetic drive ↑, but pulmonary vessels are relatively protected
Asthma medications (β₂ agonists) → small pulmonary vasodilatory effect
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
PARASYMPATHETIC NERVOUS SYSTEM → INCREASES PVR
PARASYMPATHETIC NERVOUS SYSTEM → INCREASES PVR
Vagus nerve → acetylcholine (ACh)→ M3 receptors → vasoconstriction.
Mechanisms M₃ receptors
Cause pulmonary vasoconstriction
Increase intracellular Ca²⁺ in vascular smooth muscle
Effect: PVR ↑
Secondary effects
Parasympathetic activation → bronchoconstriction
Increases airway resistance → hypoventilation of some units
Regional alveolar hypoxia → hypoxic pulmonary vasoconstriction
→ PVR increases even more (indirect mechanism)
Parasympathetic activation increases PVR.
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
thromboxane A2, Prostacyclin, Leukotrienes
Thromboxane A2 is a powerful local vasoconstrictor of both arterioles and veins.
TXA₂ is made by platelets → designed for hemostasis
Platelets synthesize TXA₂ during vascular injury.
Its biological purpose is to stop bleeding, and the fastest way to do that is:
constrict the vessel to reduce blood loss
aggregate platelets to plug the hole
TXA₂ therefore evolved to be a potent constrictor.
If a vessel is cut or injured: you want both arteries and veins squeezed shut.
Prostacyclin (prostaglandin I2), also a product of arachidonic acid metabolism via the cyclooxygenase pathway, is a potent local vasodilator. It is produced by lung endothelial cells.
WHY DOES THE LUNG ENDOTHELIUM PRODUCE PGI₂?
Because prostacyclin is the lung’s “anti-clotting, keep-flowing” molecule.
Pulmonary circulation has special needs:
extremely low-resistance
receives the entire cardiac output
cannot tolerate microthrombi (or the alveoli lose perfusion)
must prevent platelet aggregation on delicate capillaries
So lung endothelial cells use PGI₂ as a protective mechanism.
Endothelium expresses prostacyclin synthase
Arachidonic acid → COX → PGH₂ → PGI₂
Lung endothelial cells have high PGI₂ synthase → they make PGI₂ constantly.
leukotrienes, another product of arachidonic acid metabolism (via the lipoxygenase pathway), cause airway constriction.
1) Leukotrienes are made by the cells that mediate inflammation in the airways
Produced by:
Mast cells
Eosinophils
Basophils
Macrophages
These immune cells sit in the airway mucosa and are activated during:
Asthma
Allergies
Infections
Anaphylaxis
So leukotrienes are released directly into the airway environment, right where smooth muscle is.
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
recruitment and distension (during exercise)
3. Recruitment & Distension (during exercise)
The pulmonary bed is compliant:
Recruitment: Previously unperfused capillaries open
Distension: Perfused capillaries widen as pressure rises
Both decrease PVR, allowing pulmonary blood flow to increase during exercise without increasing pulmonary artery pressure significantly.
Explain the factors that regulate pulmonary blood flow, including the effects of ventilation, gravity, and pulmonary vascular resistance.
V. SUMMARY TABLE (Exam-Ready)
Factor | Effect on Pulmonary Blood Flow | Mechanism |
|---|---|---|
Ventilation (alveolar O₂) | ↓ PO₂ → ↓ blood flow | Hypoxic pulmonary vasoconstriction |
Gravity | ↑ Blood flow at base; ↓ at apex | Hydrostatic pressure gradient |
Lung Volume | ↑ PVR at high & low volumes | Alveolar vs. extra-alveolar vessel compression |
Chemical Factors | Hypoxia, hypercapnia → ↑ PVR; NO/PGI₂ → ↓ PVR | Smooth muscle contraction/relaxation |
Exercise | ↑ Flow with ↓ PVR | Recruitment & distension |
Describe the process of gas exchange between the alveoli and the pulmonary capillaries, including the principles of diffusion and perfusion.
what are the characteristics of the respiratory membrane?
what is the structure of the respiratory membrane?
I. OVERVIEW OF GAS EXCHANGE
Gas exchange = the movement of O₂ from alveoli → blood and CO₂ from blood → alveoli, driven entirely by passive diffusion (no ATP required).
It occurs across the respiratory membrane, which is extremely:
Thin (~0.5 μm)
Large in surface area (~70 m²)
Highly perfused
Describe the process of gas exchange between the alveoli and the pulmonary capillaries, including the principles of diffusion and perfusion.
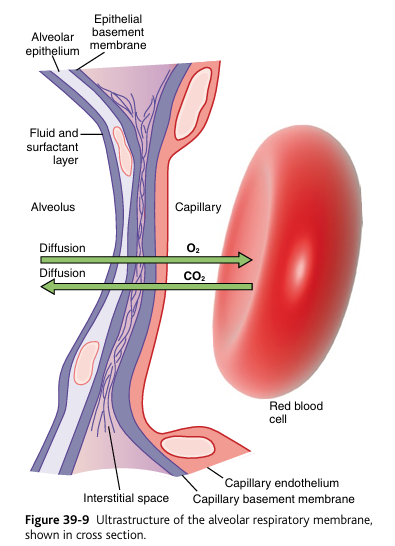
II. STRUCTURE OF THE RESPIRATORY MEMBRANE
Gas must cross:
1) fluid surfactant layer
2) Alveolar epithelium (Type I pneumocytes)
3) epithelial basement membrane
4) interstitial space
5) capillary basement membrane
6) capillary endothelium
7) red blood cell
epithelium “epi”: top, the “layer that lies on top of the surface”
IMPORTANT NOTE: Basement membranes are usually fused
In ~90% of the alveolar surface:
the alveolar epithelial basement membrane
is fused with the capillary endothelial basement membrane
→ making the diffusion barrier extremely thin (~0.2–0.6 μm)
This is why diffusion is so fast in healthy lungs.
Thin membrane + large surface area = rapid diffusion
Describe the process of gas exchange between the alveoli and the pulmonary capillaries, including the principles of diffusion and perfusion.
principles of diffusion
III. PRINCIPLES OF DIFFUSION
Gas exchange follows Fick’s Law of Diffusion:
Rate of diffusion ∝ (Surface Area × Pressure Gradient × Solubility) ÷ Membrane Thickness
1. Pressure gradients drive the exchange Oxygen
Alveolar PO₂ ≈ 104 mmHg
Pulmonary capillary PO₂ ≈ 40 mmHg
→ O₂ diffuses from alveoli into blood until capillary PO₂ ≈ 100 mmHg
Carbon Dioxide
Pulmonary capillary PCO₂ ≈ 45 mmHg
Alveolar PCO₂ ≈ 40 mmHg
→ CO₂ diffuses from blood into alveoli
2. Solubility differences
CO₂ is 20× more soluble than O₂ → diffuses easily despite smaller pressure gradient.
3. Diffusion limitations
Diffusion slows down if:
Membrane thickens (fibrosis, edema, pneumonia)
Surface area is lost (emphysema)
Blood transit time is shortened (exercise + diffusion impairment)
Describe the process of gas exchange between the alveoli and the pulmonary capillaries, including the principles of diffusion and perfusion.
principles of perfusion
IV. PRINCIPLES OF PERFUSION
Perfusion = blood flow through pulmonary capillaries.
Adequate gas exchange requires:
Sufficient blood flow
Proper matching of ventilation (V) and perfusion (Q)
1. V/Q Matching
Optimal gas exchange happens when:
Ventilation (V) ≈ Perfusion (Q)
Low V/Q (shunt physiology)
Perfusion but poor ventilation
→ pneumonia, airway obstruction, atelectasis
→ blood leaves poorly oxygenated
High V/Q (dead space)
Ventilation but poor perfusion
→ pulmonary embolism
→ wasted ventilation, no oxygen uptake
Describe the process of gas exchange between the alveoli and the pulmonary capillaries, including the principles of diffusion and perfusion.
gas exchange process
V. GAS EXCHANGE PROCESS (Step-by-Step)
1. Fresh air enters alveolus
PO₂ rises; PCO₂ falls.
2. Large pressure gradient for O₂
High PO₂ in alveolus
Low PO₂ in venous blood
→ rapid O₂ diffusion into blood
3. O₂ dissolves in plasma, then binds hemoglobin
Hb greatly increases O₂ carrying capacity
O₂ content rises until equilibrium is reached
4. CO₂ moves in opposite direction
Higher PCO₂ in venous blood
Lower PCO₂ in alveolus
→ CO₂ diffuses into alveoli
5. Blood becomes oxygenated
Capillary blood leaves alveoli with:
PO₂ ~100 mmHg
PCO₂ ~40 mmHg
6. Gas exchange completes in ~0.25 seconds
Even though RBCs remain in the capillary for 0.75 seconds.
Describe the process of gas exchange between the alveoli and the pulmonary capillaries, including the principles of diffusion and perfusion.
what is the difference between perfusion-limited and diffusion-limited for O2?
does CO2 ever problems with exchange?
VI. KEY POINT: Diffusion vs. Perfusion Limitations O₂
Normally perfusion-limited (limited by blood flow, not diffusion), it’s in the name.
Can become diffusion-limited in disease: fibrosis, edema, pneumonia
CO₂
Diffusion is so efficient that CO₂ is rarely diffusion-limited
Even with thick membranes, CO₂ exchange is usually preserved.
Analyze the pathophysiology of respiratory disorders that affect pulmonary blood flow and gas exchange, such as pulmonary embolism, pulmonary hypertension, and acute respiratory distress syndrome (ARDS)
pulmonary embolism
1. Pulmonary Embolism (PE)
“embolism: a plug”
pulmonary embolism: A plug thrown into (and blocking) the lung’s blood vessels
Primary problem: obstruction of pulmonary arteries → impaired perfusion (Q)
pulmonary artery: carries blood from the right ventricle to the lungs (only deoxygenated artery in the body)
Pathophysiology
A blood clot (usually from a Deep Vein Thrombosis) travels to the pulmonary arterial tree.
DVT = a blood clot in one of the deep veins, usually of the legs or pelvis.
Embolus blocks blood flow to part of the lung.
Ventilation continues normally, but perfusion is absent (because there is blocked blood flow)
Effects on Gas Exchange
A. V/Q Mismatch — Dead Space
Ventilation without perfusion → V/Q → ∞
Called physiologic dead space
O₂ cannot enter blood because no blood is present to receive it.
dead space → hypoxia (because no tissue is receiving the oxygen)
B. Hypoxemia Mechanisms
Loss of perfused capillaries → ↓ diffusion surface area
Reflex bronchoconstriction → worsens V/Q mismatch
Hyperventilation → ↓ CO₂ (respiratory alkalosis)
C. Hemodynamic Effects
Large Pulmonary Embolism → severe:
↑ Pulmonary vascular resistance
Acute right ventricular strain → right sided heart failure.
A large PE blocks the pulmonary artery, so the Right Ventricle suddenly has to pump against a massively increased resistance.
Shock if obstruction is massive
PE = perfusion failure → dead space → hypoxemia → RV strain.
Analyze the pathophysiology of respiratory disorders that affect pulmonary blood flow and gas exchange, such as pulmonary embolism, pulmonary hypertension, and acute respiratory distress syndrome (ARDS)
Pulmonary Hypertension (PH)
2. Pulmonary Hypertension (PH)
hypertension: a lot of pressure
pulmonary hypertension has NOTHING to do with hypertension of heart, it’s hypertension of lungs due to high PVR.
Primary problem: increased pulmonary vascular resistance (PVR)
hypertension= lots of vascular resistance.
Pathophysiology
Chronic (constant) vasoconstriction, vascular remodeling, or obstruction → ↑ PVR
Causes include:
Left heart disease
Left heart disease → backward transmission of pressure into the pulmonary circulation → pulmonary venous hypertension → pulmonary arterial hypertension → right heart strain.
This is the most common cause of pulmonary hypertension.
Chronic lung disease (COPD, ILD)
Recurrent PE
Idiopathic pulmonary arterial hypertension
Hypoxia (high altitude)
Vascular Changes
Medial hypertrophy (smooth muscle thickening)
Intimal fibrosis
In severe disease → plexiform lesions
Effects on Blood Flow & Gas Exchange (compensation)
A. Decreased Perfusion (Q)
Capillaries narrow → ↓ blood flow through well-ventilated alveoli
Capillaries narrow in pulmonary hypertension because the pulmonary vascular system remodels in response to chronically elevated pressure.
This produces high V/Q ratio (dead space–like physiology)
B. V/Q Mismatch
Some lung units are ventilated but underperfused
Creates wasted ventilation
↓ O₂ uptake
C. Right Ventricular Failure
Chronic pressure overload → RV hypertrophy → cor pulmonale
D. Hypoxemia mechanisms
Reduced perfusion
Destruction of capillary bed (e.g., in emphysema)
Consequence of increased dead space
PH = high PVR → perfusion deficits → V/Q mismatch → progressive hypoxemia → RV failure.
Analyze the pathophysiology of respiratory disorders that affect pulmonary blood flow and gas exchange, such as pulmonary embolism, pulmonary hypertension, and acute respiratory distress syndrome (ARDS)
Acute Respiratory Distress Syndrome (ARDS)
hyaline membrane formation
3. Acute Respiratory Distress Syndrome (ARDS)
acute: sudden
respiratory: respiratory
distress: Severe difficulty (in this case, difficulty breathing or oxygenating).
syndrome: a group of symptoms
ARDS occurs when diffuse inflammation and injury to the alveolar–capillary membrane cause increased permeability → protein-rich pulmonary edema → loss of surfactant → alveolar collapse → severe V/Q mismatch and shunt.
ARDS is not one disease — it is a final common pathway of many insults:
Direct lung injury
Pneumonia (most common)
Aspiration
Inhalational injury
Near-drowning
Lung contusion
Indirect injury (systemic inflammatory states)
Sepsis (most common overall)
Trauma
Pancreatitis
Massive transfusion
Burns
All of these trigger massive inflammatory activation.
Mechanism
Inflammatory mediators cause:
Damage to alveolar epithelium (Type I and II cells)
Capillary endothelial injury
Protein-rich fluid floods alveoli → noncardiogenic pulmonary edema
Surfactant is lost → alveolar collapse
type II pneumocytes that produce surfactant are injured, destroyed, or functionally shut down by the inflammatory damage to the alveolar–capillary membrane.
Hyaline membranes form
leak into the alveoli and then organize into a glassy (hyaline) layer.
Severe ↓ compliance (stiff lungs)
Effects on Gas Exchange
A. Diffusion Limitation
Thickened respiratory membrane
Fluid + protein-filled alveoli
↓ O₂ diffusion capacity
CO₂ diffusion is often preserved early
B. Severe V/Q Mismatch 1. Shunt physiology (Q > V)
Blood flows past unventilated or collapsed alveoli
Does NOT improve with supplemental oxygen (key clinical sign)
C. Decreased Compliance
Stiff lungs require high pressures to inflate
↓ tidal volumes → ↓ ventilation
D. Hypoxemia
Profound
Due to shunt + diffusion barrier + V/Q mismatch
Summary
ARDS = alveolar flooding + collapse → shunt → refractory hypoxemia + low compliance.
Physiology, Costanzo, 6th edition:
Chapter 5, Pg 216 - 224
put the flashcards from the book here, you need everything, and the stuff highlighted.