Clinical Exercise Physiology Exam Review: Cardiovascular & Pulmonary
1/96
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
97 Terms
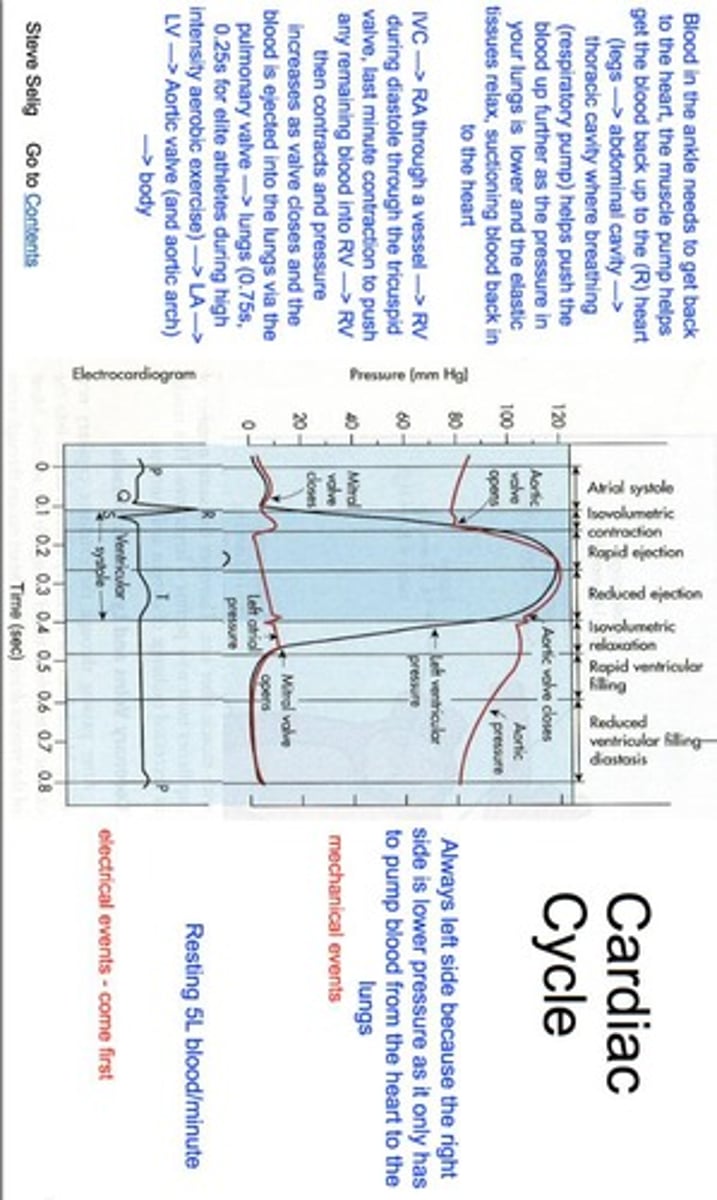
Cardiac cycle
The sequence of events in the heart from the beginning of one heartbeat to the beginning of the next.
Dyspnoea
Shortness of breath associated with hypoxemia and hyperventilation.
COPD
Chronic obstructive pulmonary disease, characterized by chronic bronchitis and emphysema.
Chronic bronchitis
Mucus positive cough most days of a month, for 3 months of a year for 2 successive years, with thickened, inflamed bronchi producing sputum.
Emphysema
Shortness of breath (SOB) due to damage to the alveoli elastin by neutrophil elastase, which is normally neutralized by anti-proteinase (AAT) produced in the liver.
Exercise Benefits for COPD
reduced respiratory demand, reduced breathlessness and fatigue, increased respiratory muscle fitness, increased exercise endurance, improved health-related quality of life, and increased self-efficacy.
Pink Puffers
Individuals with destruction of alveoli and bronchioles leading to increased ventilation (VE) to maintain arterial oxygen pressure (PaO2), resulting in increased work of breathing.
Blue Bloaters
Individuals with reduced airway diameter and increased resistance leading to decreased PO2 in alveoli and arterial blood, resulting in tissue hypoxia.
PAOD
Peripheral Arterial Occlusive Disease, characterized by systemic atherosclerosis and narrowing of arteries distal to the aortic arch, causing intermittent claudication.
Claudication pain
Pain that occurs during walking, which is less than walking speed and below the angina pain threshold.
Benefits of Exercise for PAOD
Includes improved biomechanics, increased circulation, increased pain tolerance, increased muscle oxidative capacity, reduced blood viscosity, reduced red cell aggregation, and regression of atherosclerosis.
Pericardial tamponade
Very rapid accumulation of fluid in the pericardium leading to acute heart failure and angina-like pain.
SABA
Short acting beta agonist, a bronchodilator (e.g., Ventolin) used for acute relief of asthma symptoms and protection against exercise-induced asthma (EIA).
CPAP
Continuous Positive Airway Pressure, a mechanical aid to keep the airway open by maintaining positive pressure inside the airway.
Exercise Stress Test
A test aimed at reaching a target heart rate of 85% of heart rate maximum, calculated as (220-age) x 85%.
Commercial Driving Requirements
New guidelines require reaching a target heart rate of 90% of heart rate maximum, calculated as (220-age) x 90%.
Pharmacological stress tests
Tests conducted when contraindications to routine exercise stress exist or when patients cannot exercise due to debilitating conditions.
Hospital based exercise assessments for PAOD
In hospital: peripheral ischemic threshold < angina threshold < STOP intensity; Out of hospital: peripheral ischemic threshold < STOP intensity < angina threshold.
Mean arterial pressure
Average arterial blood pressure during a single cardiac cycle, calculated as MAP = cardiac output x stroke volume.
Exercise in COPD
Includes endurance training, strength training, interval training, flexibility, inspiratory muscle training, and balance training.
Monitoring in COPD Exercise
Includes monitoring of RPE (Rate of Perceived Exertion), RPB (Rate of Perceived Breathing), O2SAT%, heart rate (HR), and blood pressure (BP).
Cystic fibrosis (CF)
Recessive genetic condition characterized by increased secretion of thick, sticky mucus drawing salt through exocrine ducts.
Pathophysiology of CF
Pulmonary deterioration leading to respiratory failure, decreased pancreatic function, excess mucus preventing digestion to the small intestine, malnutrition, poor growth, and liver cirrhosis.
Management of CF
Includes medications such as bronchodilators, antibiotics, steroids, pancreatic replacement enzymes, bisphosphonates, airway clearance techniques, and lung transplant.
Graded Exercise Testing in CF
Measures VO2, VE, HR, BP, RPE, SOB, and O2SAT%.
6MWT
Measures distance, heart rate (HR), and O2SAT%.
COPD
Chronic obstructive pulmonary disease, characterized by fixed obstruction, acute obstruction (asthma), and chronic obstruction (bronchitis).
Pathophysiology of COPD
Includes degranulation of mast cells, mucus plugs, hyperinflation of alveoli, smooth muscle constriction, mucus accumulation, and right heart failure.
Risk factors for COPD
Smoking, genetics, exposure to fumes, dust, chemicals, and bacterial/viral infections.
Management of COPD
Includes smoking cessation, medication, pulmonary rehabilitation, exercise, and CPAP or oxygen therapy.
Exercise Testing in COPD
Considers current treatment, co-morbidities, and cardiopulmonary tests to determine safety and factors contributing to exercise limitation.
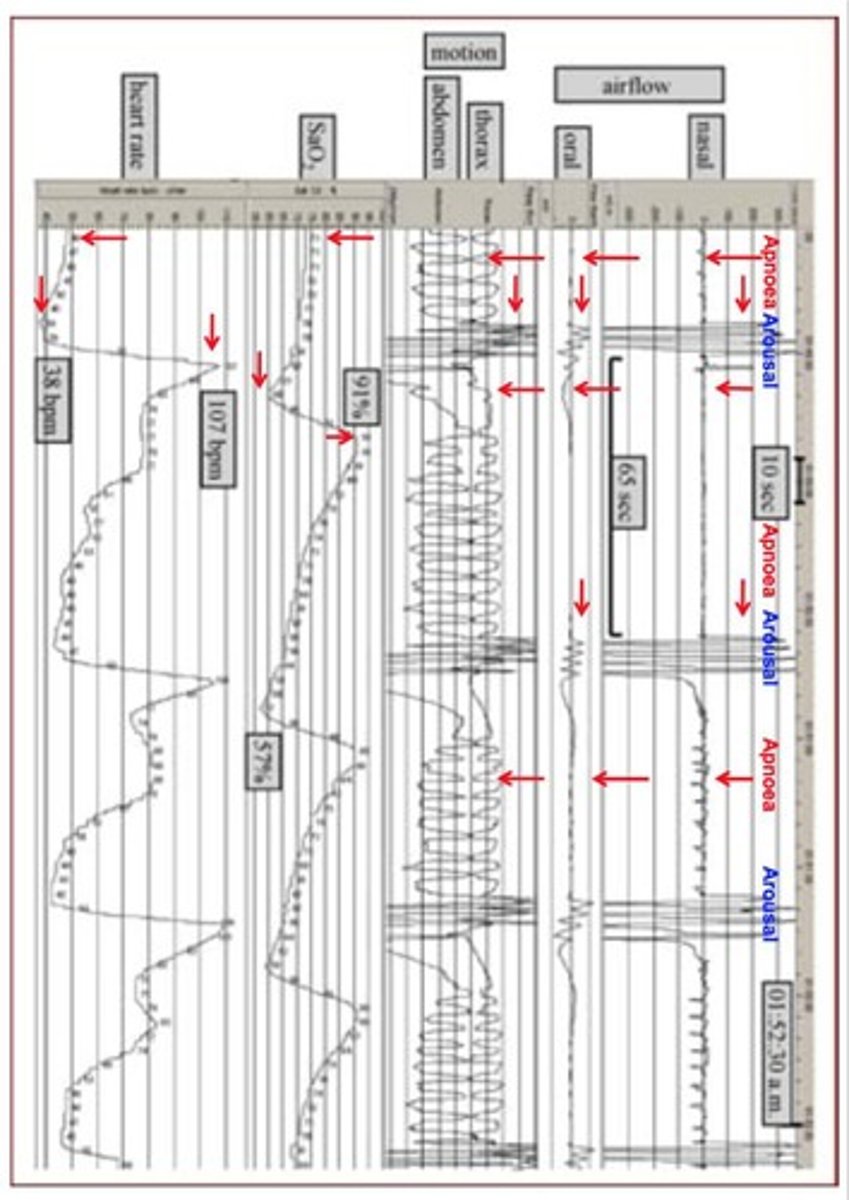
OSA
Obstructive sleep apnea, a sleep disorder characterized by repetitive, short-duration blockages of the upper airway resulting in episodic cessation of breathing or reduction of airflow.
Pathophysiology of OSA
Upper airway narrowing/blockage due to lack of muscle tone or movement of the tongue and palate, leading to occlusion of the nasopharynx and oropharynx.
Risk factors for OSA
Obesity, alcohol and other sedatives, and anatomical narrowing of upper airways.
Management of OSA
Includes weight reduction, avoiding nocturnal sedatives, cessation of evening alcohol, avoiding supine sleeping position, and CPAP.
Asthma
A condition characterized by widespread, reversible airway narrowing.
Pathophysiology of Asthma
Bronchiolar smooth muscle contraction leading to inflammation, increased mucus production, overinflation, increased work of breathing, and respiratory muscle fatigue.
Triggers of Asthma
Allergens, drugs, foods, chemicals, tobacco smoke, stress, exercise, cold air, and respiratory infections.
Management of Asthma
Includes SABA for intermittent asthma and daily preventer therapy for persistent asthma.
Exercise Testing in Asthma
Should not be performed if asthma is not under control, if using a reliever more than 4 times a week, if the patient is sick, or when peak flow meter is reading 80% of the usual best.
Exercise induced asthma
Characterized by a decrease in FEV1 due to increased rate of inspiration and expiration, leading to loss of water in the lungs and release of bronchoconstrictors.
Management of Exercise induced asthma
Includes exercise in warm environments, swimming, walking, cycling, and using Ventolin or a sport-specific preventer.
Breathing reserve
Defined as maximal voluntary ventilation (MVV) minus minute ventilation at peak exercise (VEpeak), with BR = MVV - VEpeak.
Well controlled asthma
Characterized by a breathing reserve greater than 40 L.min-1 or greater than 40% of MVV.
Poorly controlled asthma
Characterized by a breathing reserve less than 40 L.min-1 or less than 40% of MVV.
Pacemaker
A small device that's paced in the chest/abdomen to help control abnormal heart rhythm.
Bradycardia
A condition where the heart beats slower than normal.
Heart Blocks
A condition where the electrical signals in the heart are partially or completely blocked.
Electrodes
Devices that detect electrical activity and send data to a computer in the generator.
Ischemic Threshold
The level of exercise intensity above which the heart may not receive enough oxygen.
Bruce Protocol
A low level exercise testing protocol used for cardiac patients.
Naughton Protocol
Another low level exercise testing protocol used for cardiac patients.
Ventricular Assist Device (VAD)
Single system device with an external power source that's surgically attached to the LV and aorta for LV support.
Bridge to Transplant
A temporary solution for patients waiting for a heart transplant.
Bridge to Recovery
A method to unload heart pressure and promote reverse remodeling.
Destination Therapy
A permanent treatment option for patients ineligible for heart transplant.
Mean Arterial Pressure (MAP)
A measure of blood pressure that must be above 65mmHg for safe exercise.
6MWT
Six-Minute Walk Test, a common exercise test for assessing functional capacity.
Implantable Cardioverter Defibrillator (ICD)
A pulse generator that assists the heart to synchronize electrical conductivity with a shock.
Ventricular Tachycardia (VT)
A fast heart rhythm originating from the ventricles.
Ventricular Fibrillation (VF)
A life-threatening heart rhythm that results in rapid, inadequate heartbeat.
Low Energy Shock
A programmed therapy that converts abnormal heart rhythm back to normal.
High Energy Shock
A therapy used when arrhythmia is severe and the heart is dying.
Prostaglandin E1 (alprostadil)
Prevents premature closure of the ductus arteriosus in patients with Patent Ductus Arteriosus.
Leukotrienes
Triggers smooth muscle constriction of bronchioles, causing inflammation in asthmatics.
Eosinophil Chemotactic Factor
Reduces cilia activity and increases inflammatory mediators, damaging epithelium.
Neutrophil Chemotactic Factor
Attracts neutrophils and causes damage via infection.
Alveolar Elastin
Elastic connective tissue of the alveoli that allows them to expand and recoil.
Neutrophil Elastase
Causes damage to alveolar elastin during inflammation, reducing elastic recoil.
Alpha 1-antitrypsin
A protease inhibitor that protects tissues from enzymes of inflammatory cells.
Beta-blocker
Blocks effects of epinephrine & adrenaline, reducing BP, angina, AMI risk & arrhythmias.
Statin
Reduces cholesterol production and stabilizes lesions.
ACEI
Reduces BP; acts as a vasodilator in congestive heart failure.
Diuretic
Blocks reabsorption of Na+, reducing blood volume and venous pressure.
Digoxin
Increases cardiac contractility in heart failure and treats arrhythmias.
Nitrate
Acts as a vasodilator, increasing oxygen supply to the heart and reducing ischemic pain.
Bradyarrhythmias
Prolonged apnoea and hypoxemia elicits the diving reflex leading to simultaneous cardiac vagal activation and sympathetic activation to the periphery, resulting in decreased heart rate and peripheral blood flow to protect central blood flow to major organs.
Tachyarrhythmias
Apnoea and hypoxemia episodes terminate with CNS arousals and increased sympathetic activity, resulting in tachyarrhythmias and increased blood pressure.
Aortic Stenosis Severity - Mild
1.5 cm2, mean gradient < 25 mmHg, or jet velocity < 3m/second.
Aortic Stenosis Severity - Moderate
1.0 - 1.5 cm2, mean gradient 25 - 40 mmHg, or jet velocity 3 - 4m/second.
Aortic Stenosis Severity - Severe
< 1.0 cm2, mean gradient > 40 mmHg, or jet velocity > 4m/second.
O2 Saturation Levels to Start Exercise - Healthy
Greater than 95%.
O2 Saturation Levels to Start Exercise - COPD
Greater than 92%, but some patients can tolerate much lower O2 saturation percentage at rest.
O2 Saturation Levels to Stop Exercise - Healthy
Less than 88%.
O2 Saturation Levels to Stop Exercise - COPD
Less than 85%, but some patients can tolerate much lower O2 saturation during exercise.
FVC
Forced Vital Capacity is the maximum volume of air that can be expired (or inspired) during a manoeuvre using maximal effort.
SVC
Slow Vital Capacity is the maximum volume of air that can be exhaled 'slowly' following a full inspiration (or inhaled after a complete expiration).
FEV1
Forced expiratory volume in 1 second is the volume of air that has been exhaled at the end of the first second from a maximally forced expiratory effort.
FEV1/FVC Ratio
The FEV1 expressed as a percentage of the FVC, providing a clinically useful indicator of airflow obstruction.
FEF25-75%
Forced Expiratory Flow between 25 & 75 percent of the FVC is the average expired flow over the middle half of the FVC manoeuvre, regarded as a more sensitive but more variable measure of narrowing of the smaller airways than provided by FEV1.
PEF
Peak Expiratory Flow is the maximal expiratory flow rate achieved, occurring very early in the forced expiratory manoeuvre.
FEF50% and FEF75%
FEF at 50% or 75% of FVC is the maximal expiratory flow measured at the point where 50% or 75% of the FVC has been expired.
Polysomnograph
Records continuous airflow by a nasal cannula pressure transducer, nasal and oral airflow via a thermistor, rib cage & abdominal motion for breathing efforts, arterial O2 saturation & heart rate by pulse finger oximetry, and synchronized, single- or multichannel ECG.
Heart Rate Characteristics of a Transplanted Heart
Increased resting heart rate (~20 beats or around >90 bpm), elevated resting blood pressure, attenuated increase in heart rate during submaximal work, lower peak heart rate and peak stroke volume, decreased systolic pressure at peak exercise, delayed slowing of heart rate in recovery, cardiac output only 60-70%, and continued exercise intolerance after surgery that is about 40-50% below that of age-matched normal individuals.
Fluid Overload Effects on the Heart
Can be caused by congestive heart failure where the left ventricle cannot meet demands of the body, leading to increased pressure in the circulatory system and forcing fluid into alveoli of the lungs.
Fluid Overload Causes
Fluid overload can result from kidney failure or intravenous fluid therapy, hypertensive emergency, pericardial effusion with tamponade, severe heart attack, or abnormal heart valve affecting blood flow out of the heart.
Pulmonary Oedema
Occurs when the alveoli are flooded, preventing the bloodstream from getting enough oxygen and the body from expelling carbon dioxide properly.