IMED1001 - Genital Anatomy I (Testicular System) (Week 11)
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
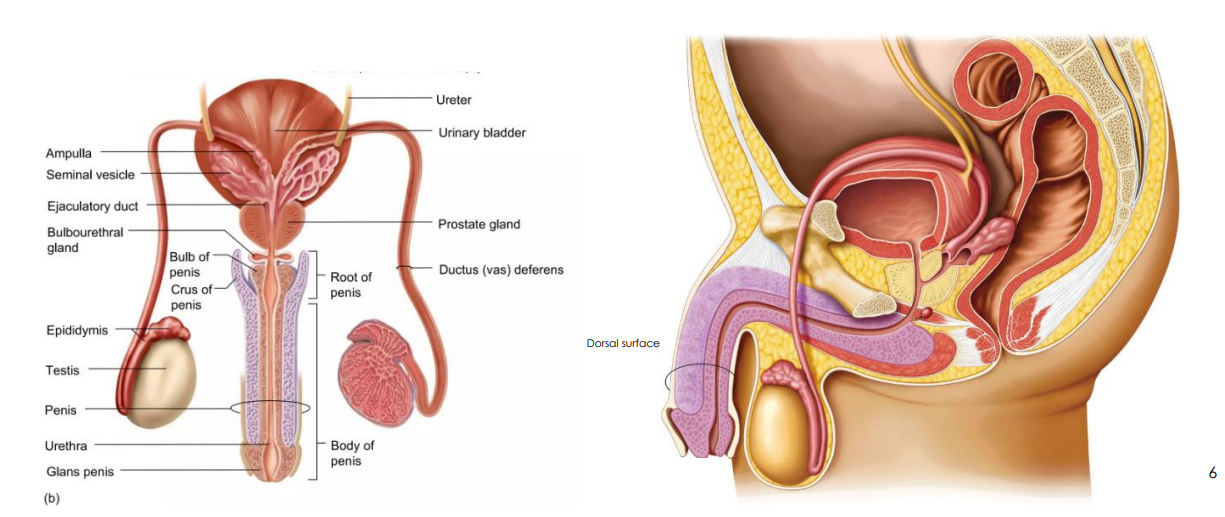
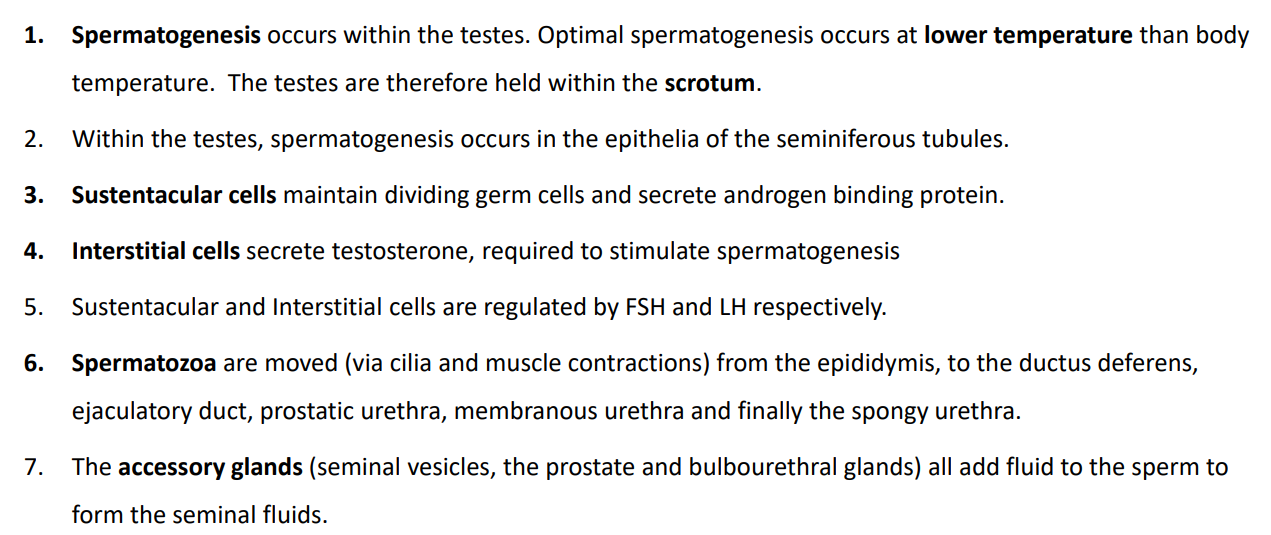
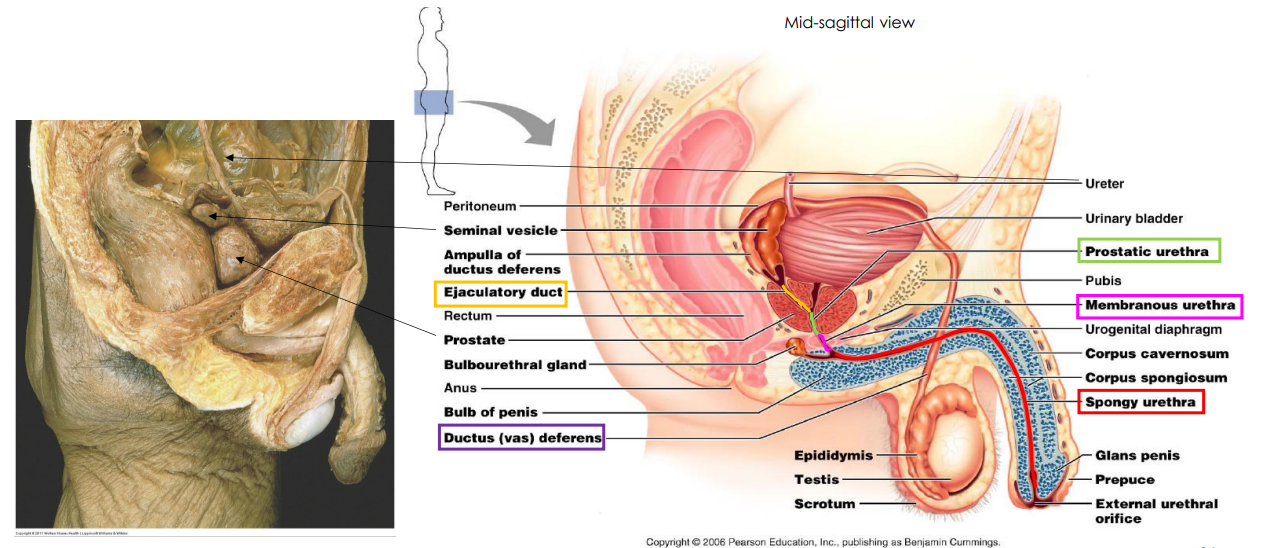
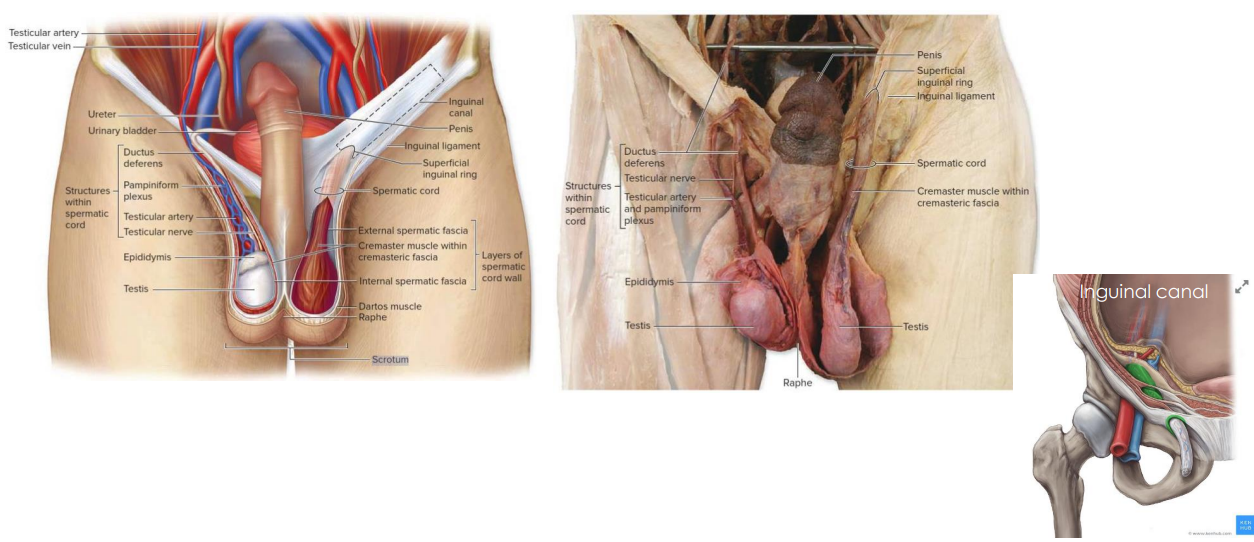
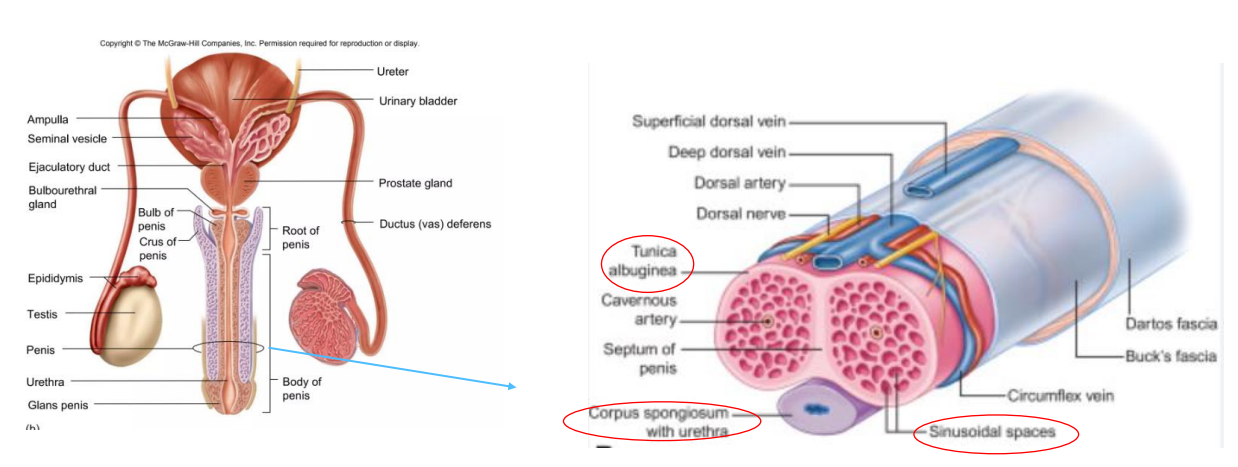
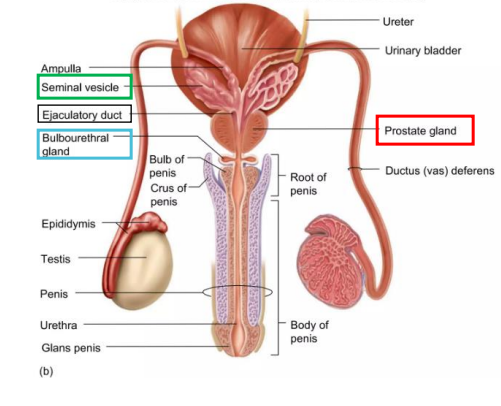
Diagram of the Testicular System
- spermatogenesis is best few degrees below body temp hence testes is outside body
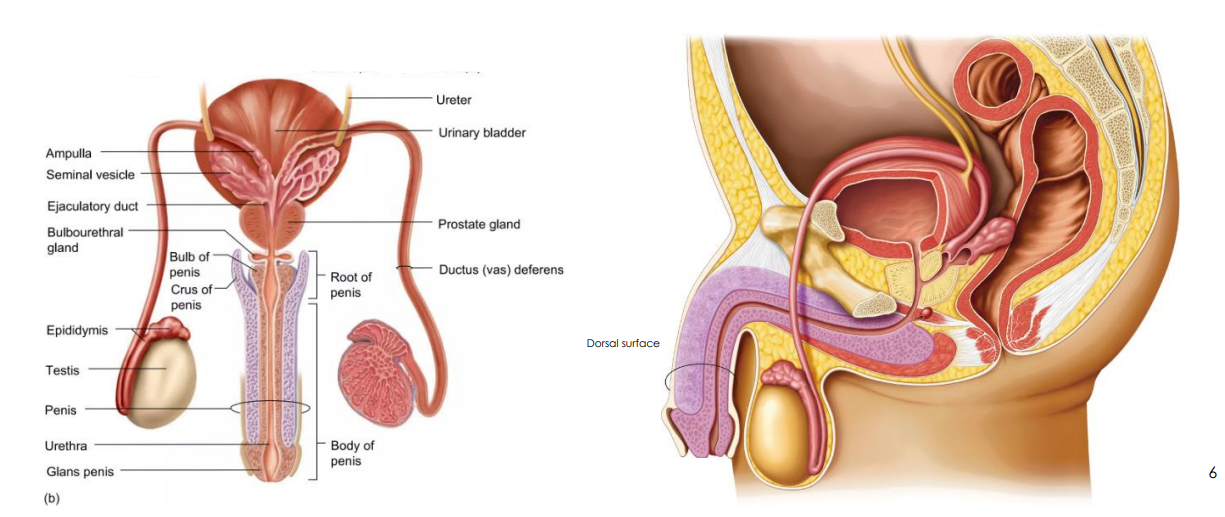
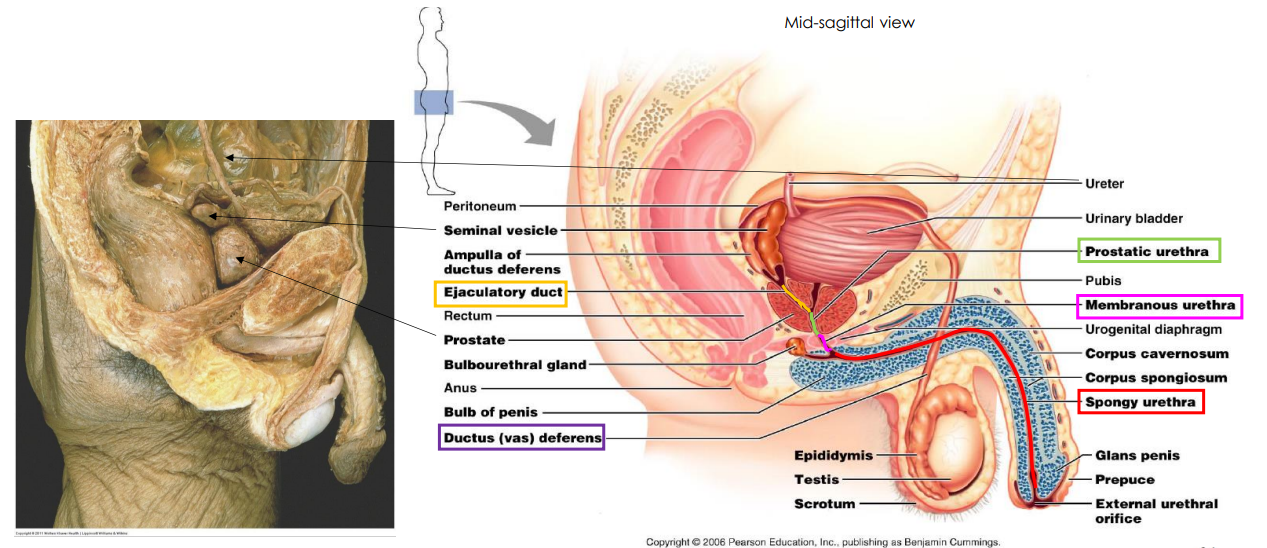
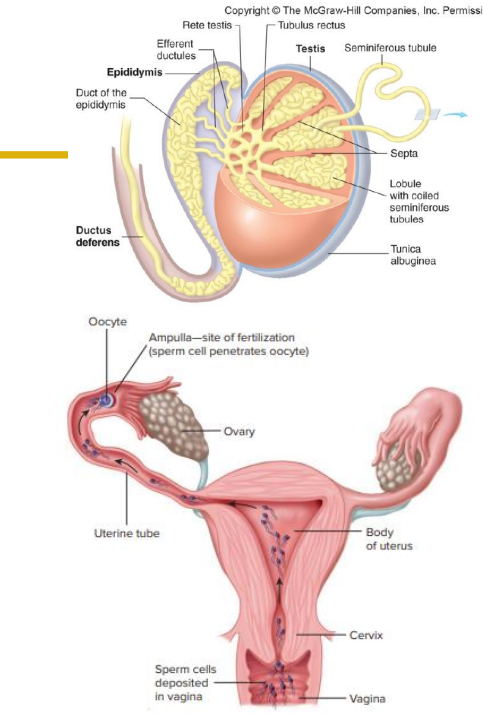
Ducts for Sperm DIAGRAM
DIAGRAM ON SLIDE 8 and 9
- note the ejaculatory duct and ductus (vas) deferens
- also note the prostatic urethra
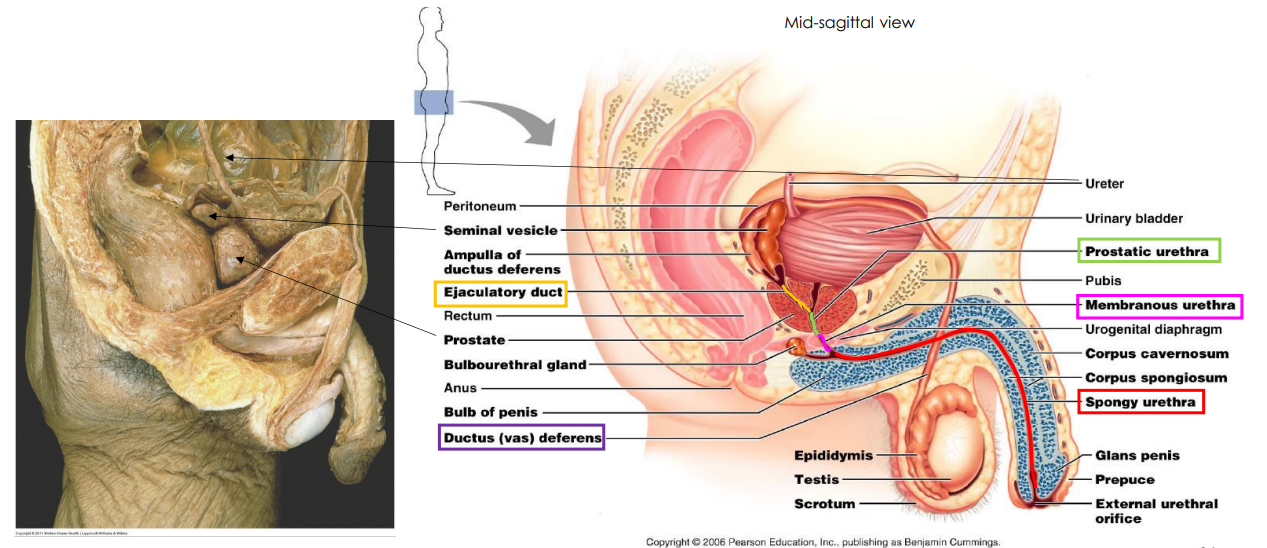
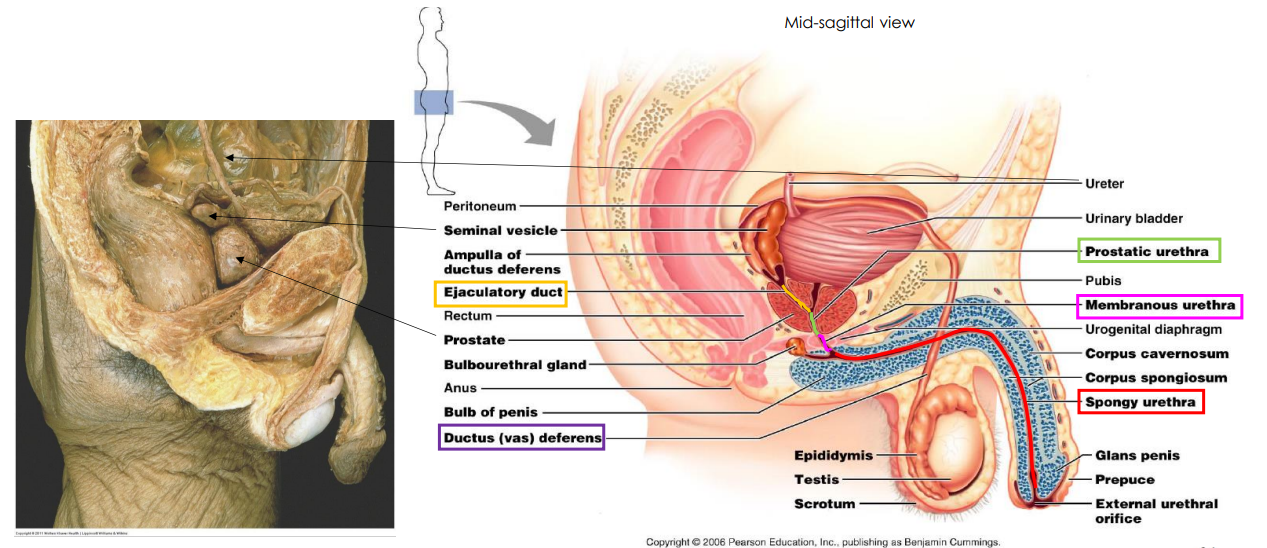
Testes DIAGRAM
DIAGRAM ON SLIDE 9
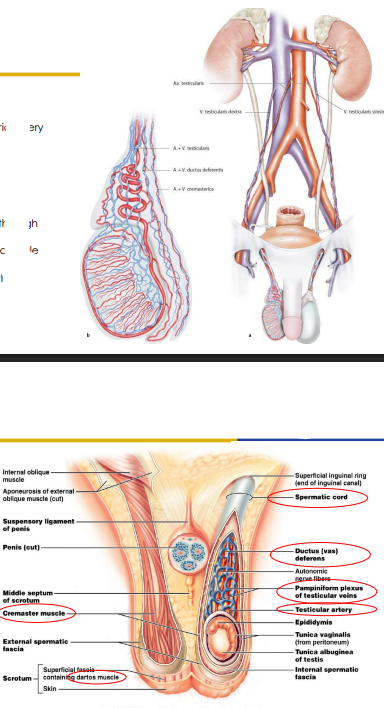
Blood Supply to Scrotum
- Arterial supply: testicular artery, cremasteric artery and ductal artery
- Venous Drainage: Pampiniform plexus enters the abdomen through the deep inguinal ring and coalesce into a single testicular vein that drains into the IVC on the right, and into the renal vein on the left
- pampiniform plexus is a convoluted system of veins that runs alongside the arteries in order to take heat away from the arteries so blood cools down
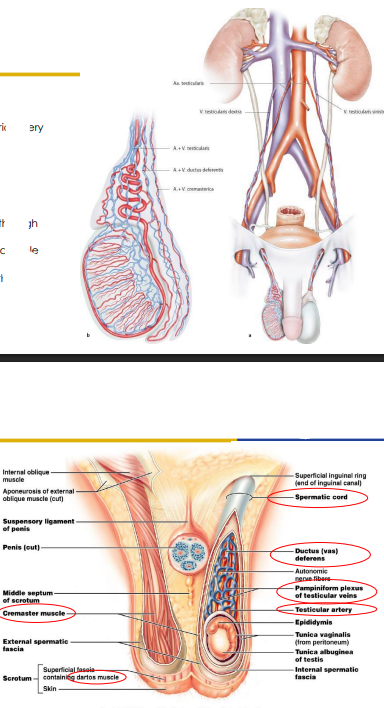
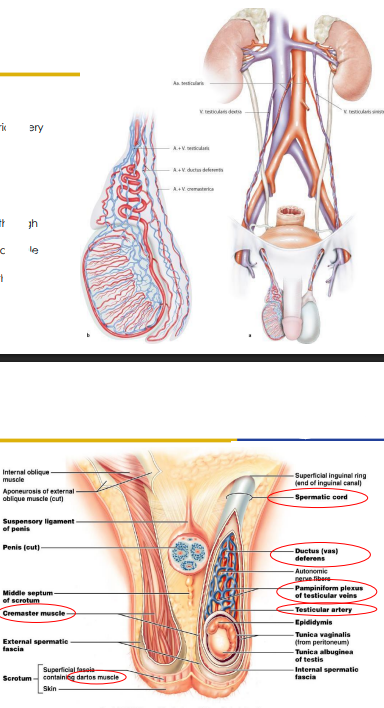
Details about the Scrotum
- Scrotum covers the testes: Optimal spermatogenesis at 2-3C below body temp
- Spermatic Cord: Testicular artery (Branches aorta, Pampiniform plexus, Ductus deferens, Cremaster muscle)
- Cold: dartos muscle retracts scrotal skin, cremaster muscle elevates testes
- cremaster muscle is important to move the testes higher or lower to promote heating (closer to both to promote heating, and it relaxes to lower testes when it needs to cool)
- dartos is involved in cooling
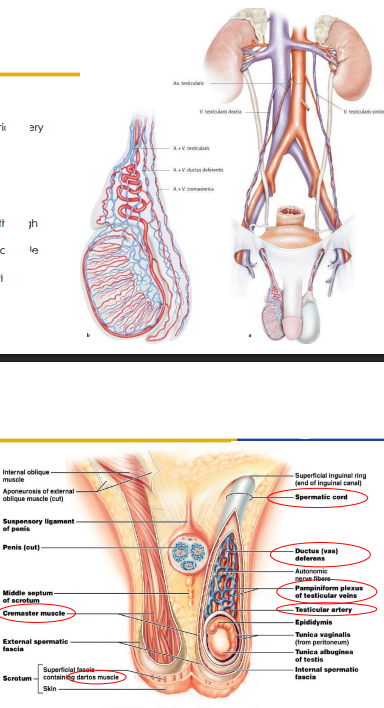
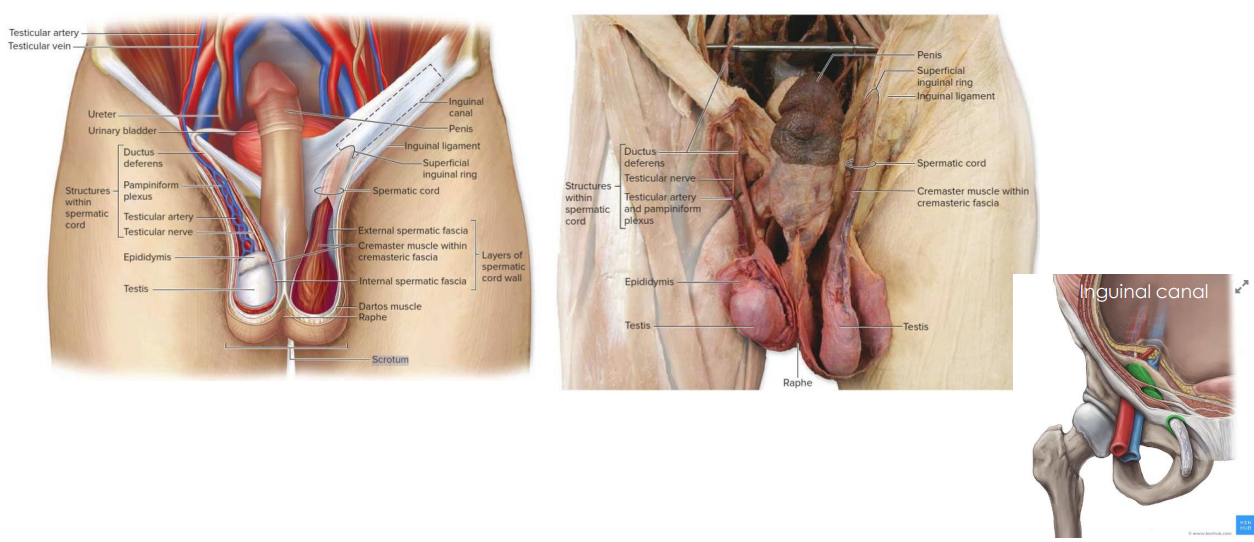
Diagram of Scrotum
DIAGRAM ON SLIDE 12
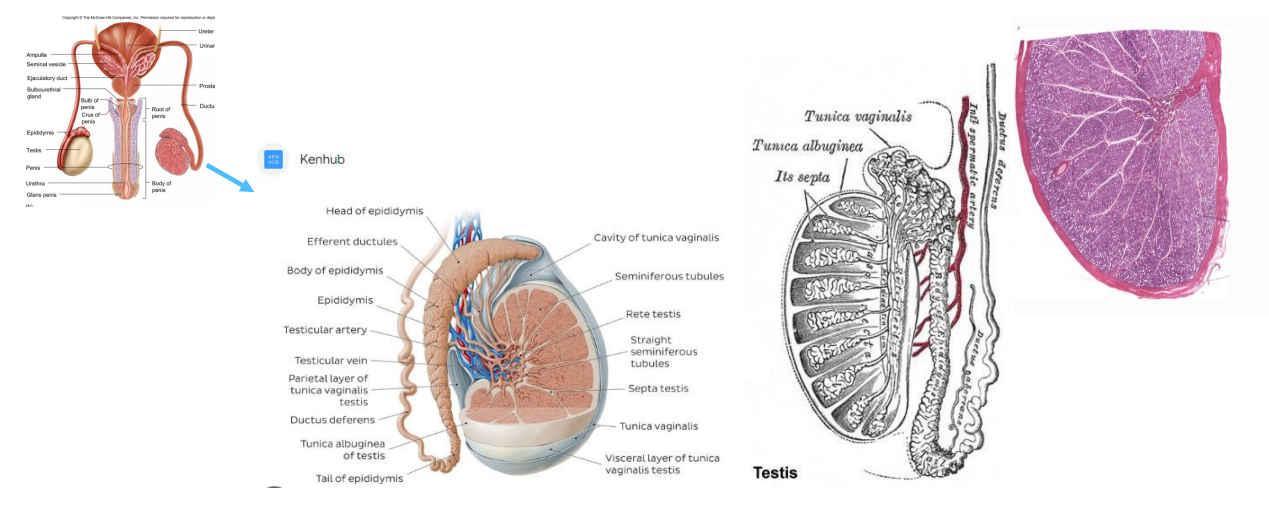
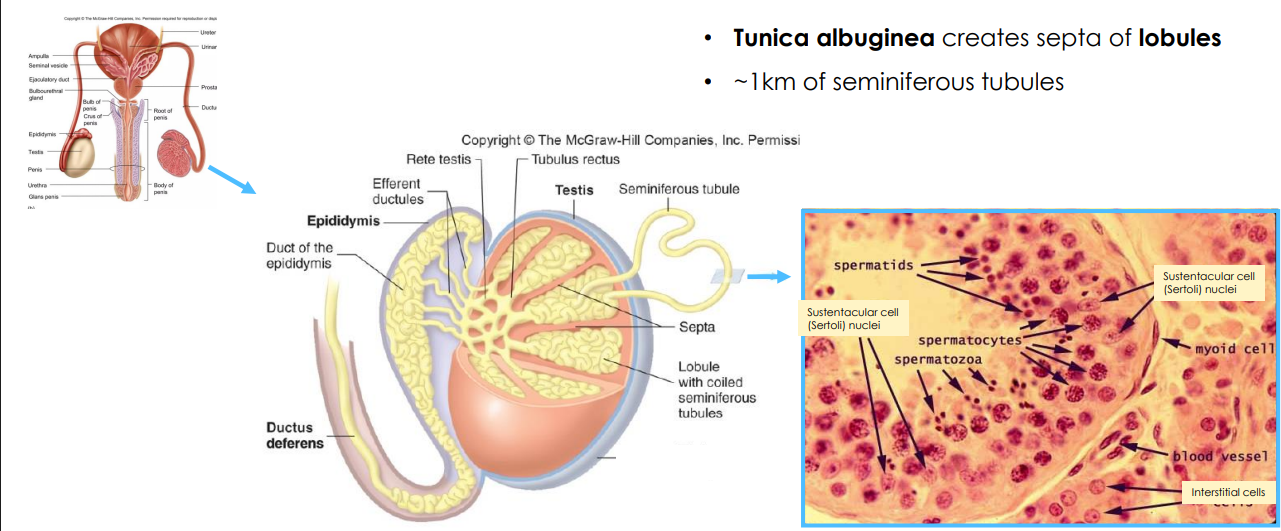
Testes Diagram
- seminiferous tubules form into lobules and the septum (space between lobules) is formed by that same layer which is tunica albuginea)
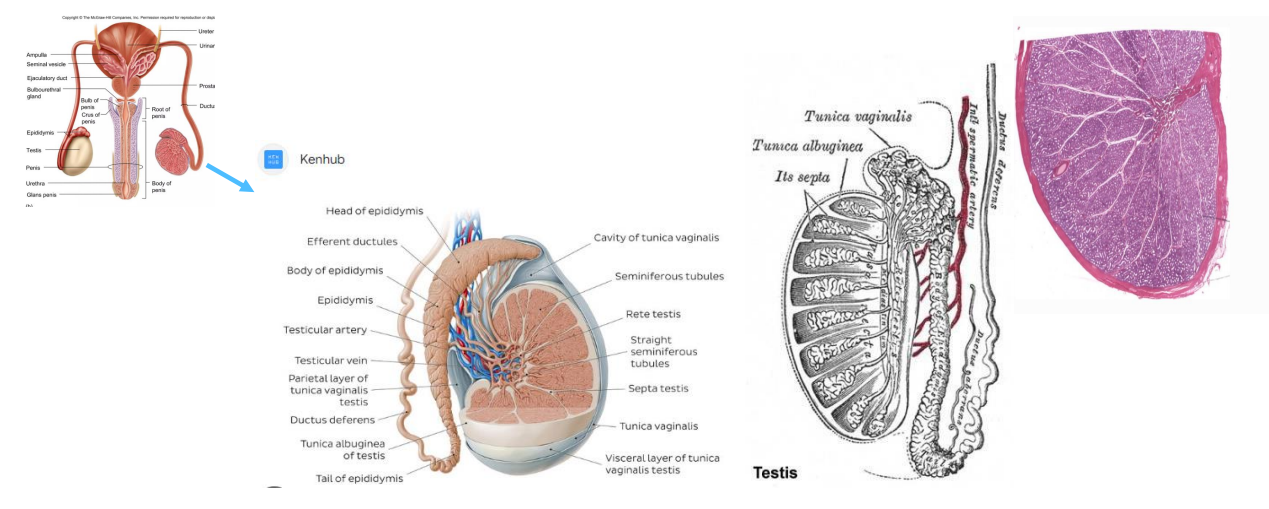
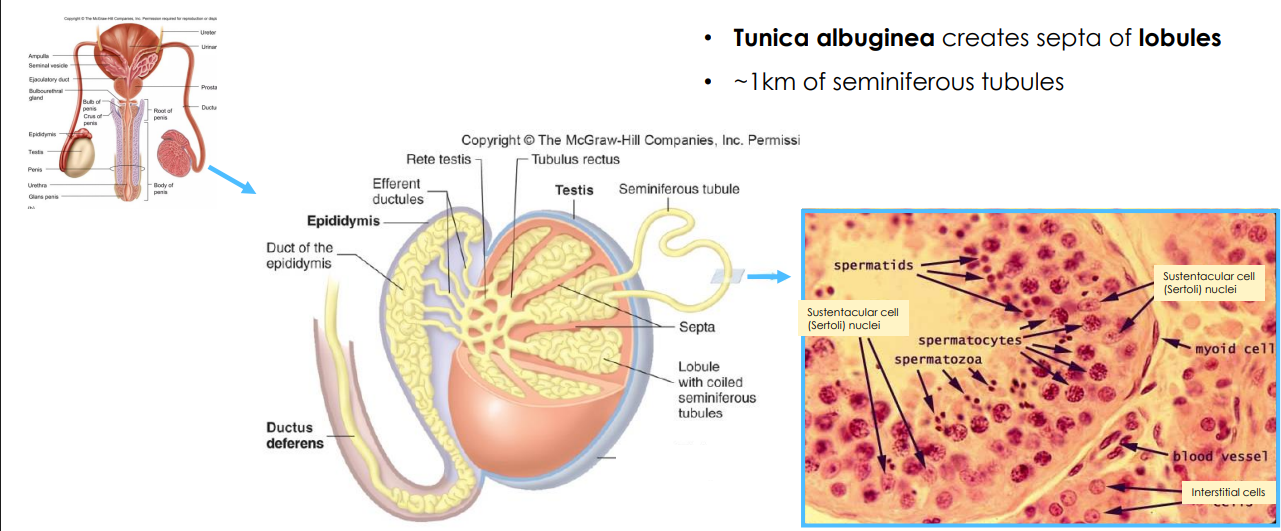
Tunica Albuginea
- creates septa of lobules (around 1km of seminiferous tubules)
- efferent means exit
- interstitial cells are sitting between the tubes
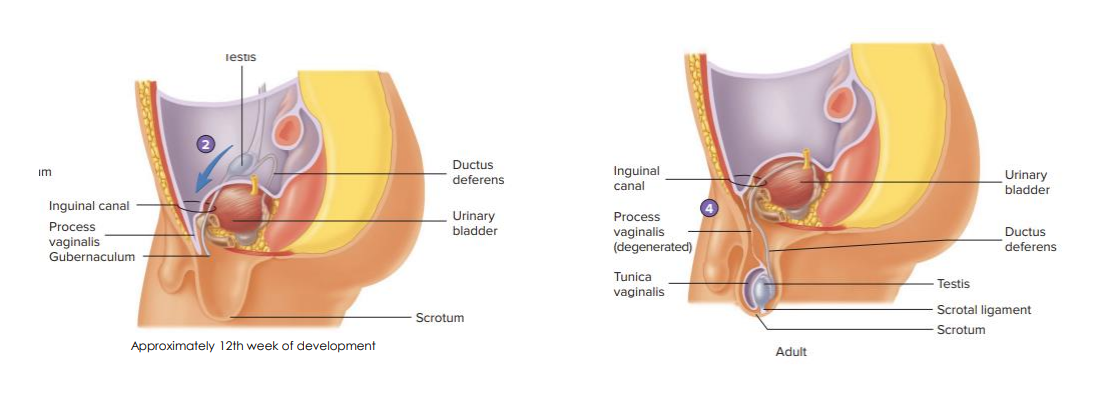
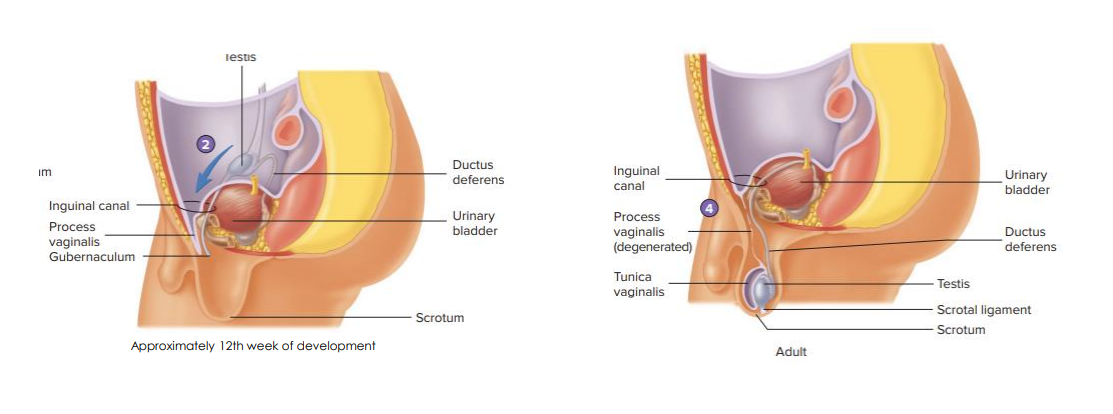
Testes Descent
- shows that the testes start at the kidneys at birth and descend through life
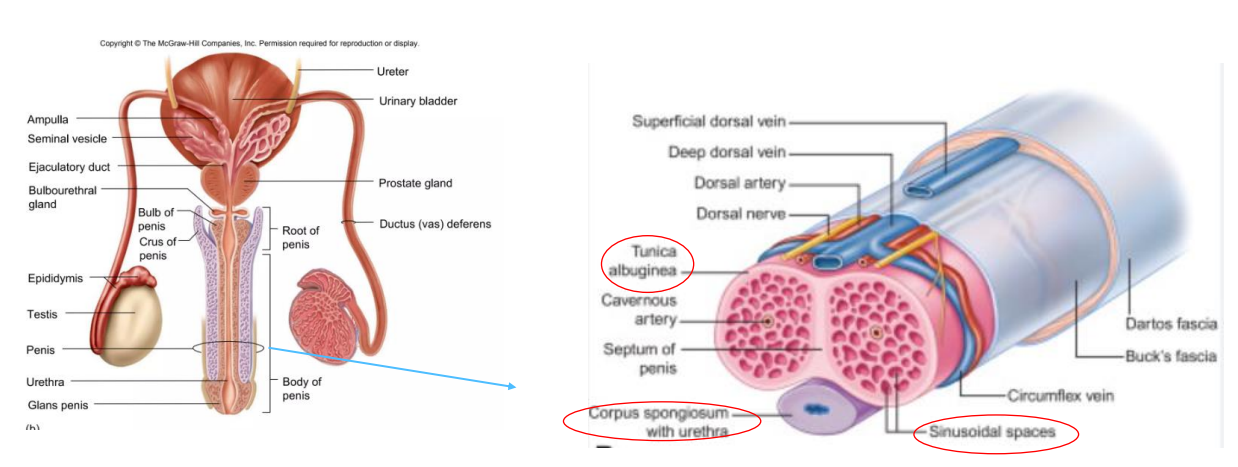
Cross Section of the Penis
- corpus spongiosum with urethra
- sinusoidal means there are sinuses (holes)
- tissue is covered in tunica albuginea
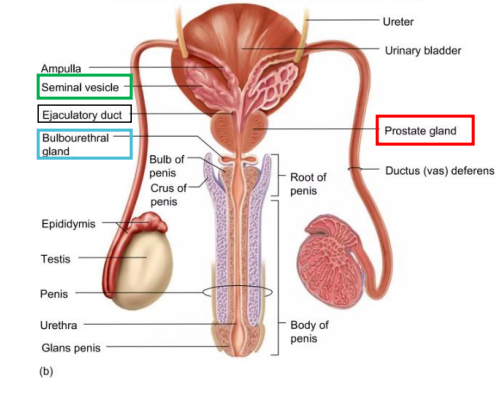
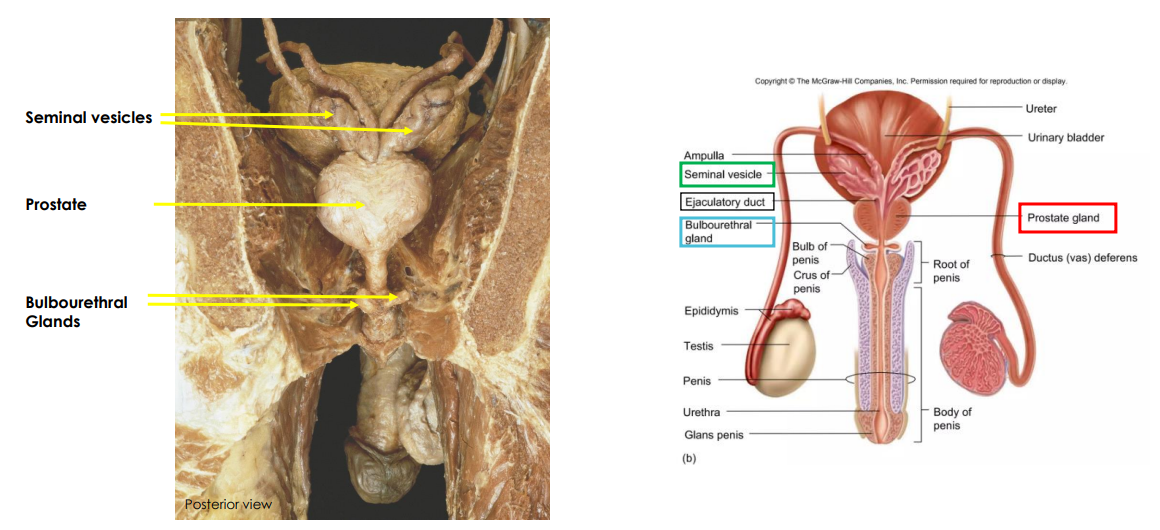
Acessory Glands (NAMING ONLY)
Seminal Vesicles, Prostate Gland, Bulbourethral (Cowper's Gland)
- 95% of semen is from these, 5% is from the sperm
Seminal Vesicles
- coiled glands, around 5-7cm long
- posterior to bladder, forms ejaculatory duct
- Produces around 60% of seminal fluid, contains fructose, citric acid, prostaglandins, and fibrinogen all of which increase sperm motility
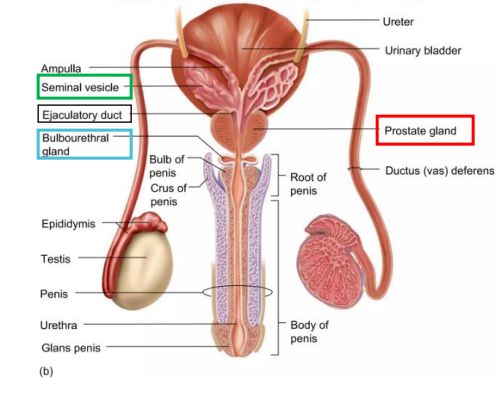
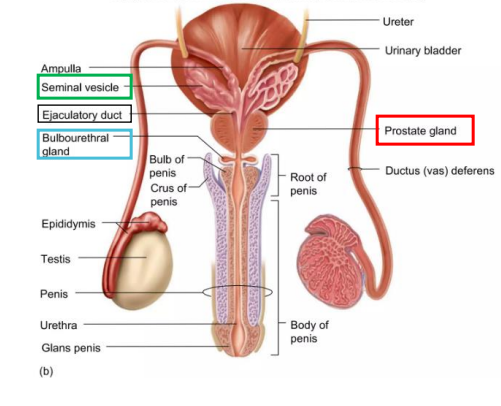
Prostate Gland
- thick gland, directly beneath bladder
- produces around 30% of seminal fluid, enzyme rich fluid to activate sperm, clotting factors (fibrinogen to fibrin)
- fibrinolysin and prostate specific antigen (PSA) (anti-coagulants)
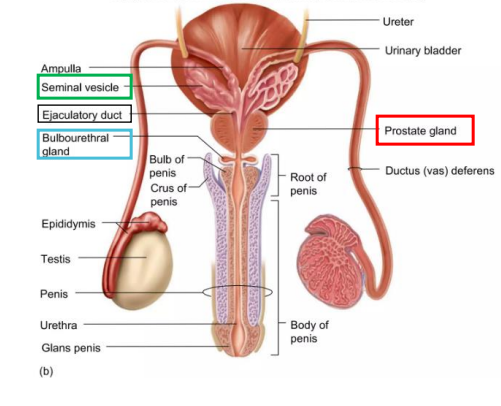
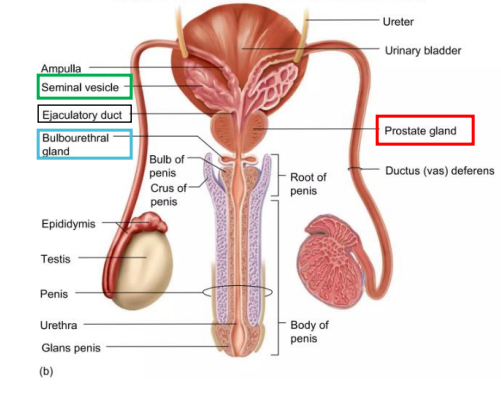
Bulbourethral (Cowper's) Gland
- small, inferior to prostate
- Produces around 5% of seminal fluid, clear mucus lubricates
- its alkaline fluid to neutralise the urine
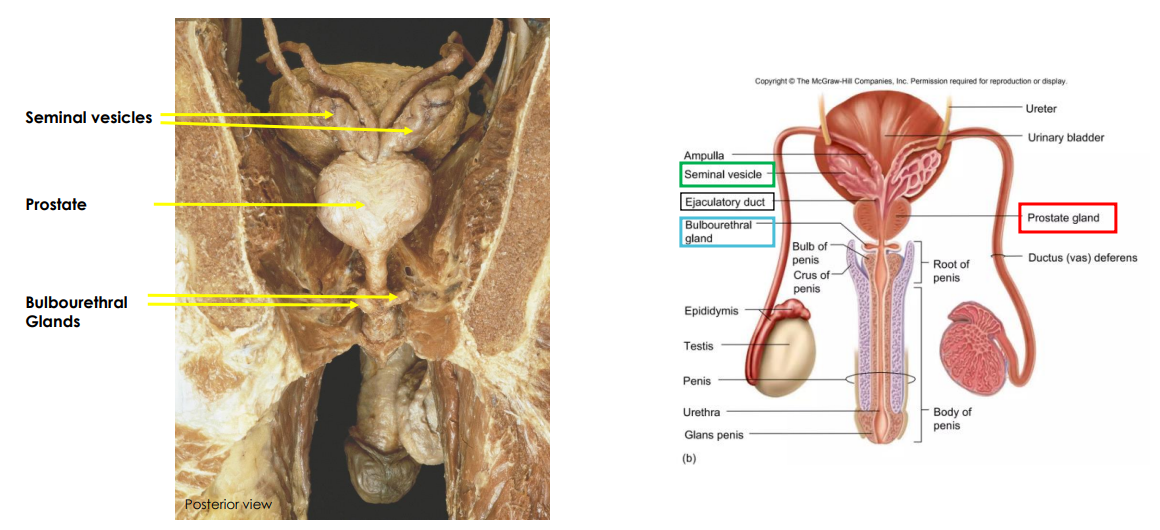
Accessory Glands Cadaveric Image
DIAGRAM ON SLIDE 18
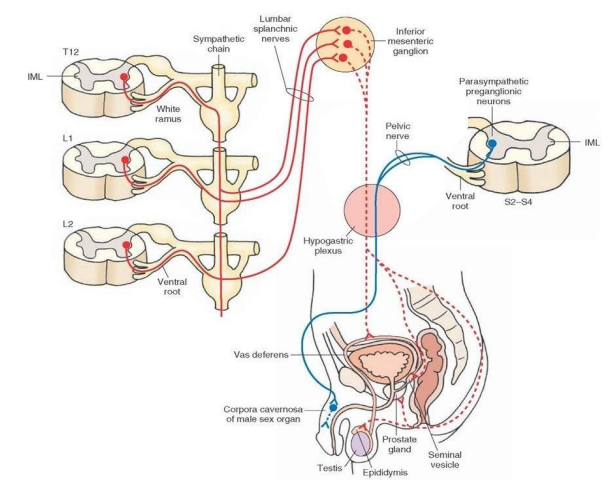
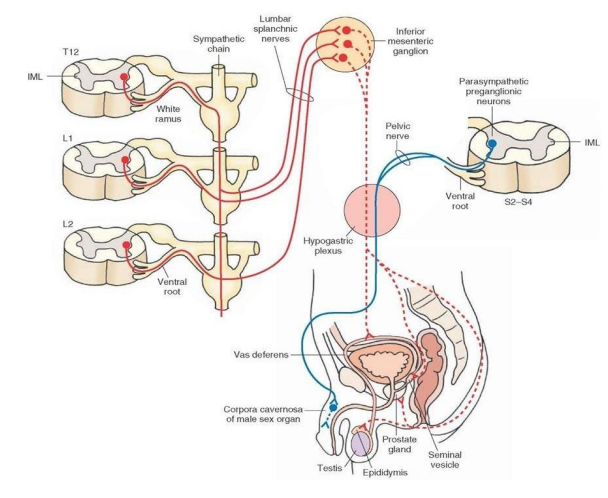
Autonomic Innervation
- Parasympathetic: pelvic splanchnic (S2-S4) (engorgement/erection)
- Sympathetic: Least/lumbar splanchnic (T12-L2) (emission, contraction and ejaculation)
splanchnic means “relating to internal organs (viscera) in the abdomen (usually)
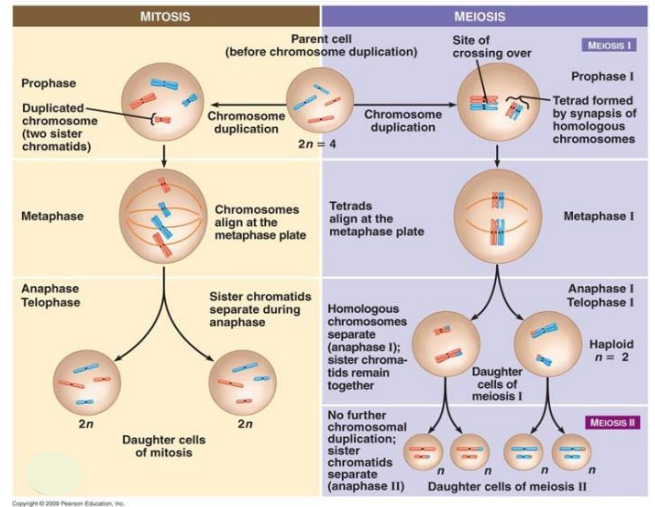
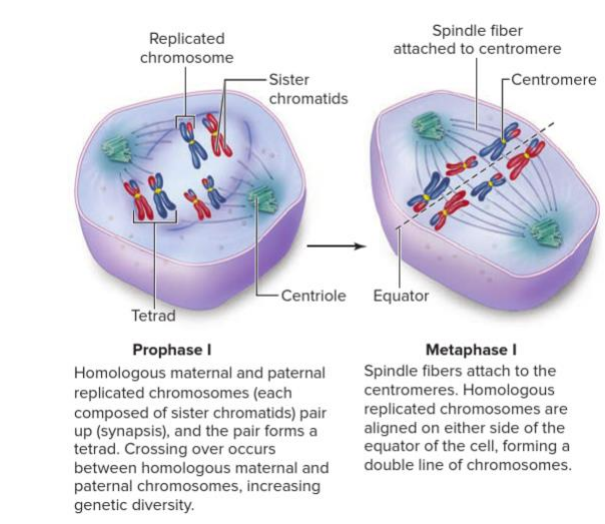
Mitosis vs Meiosis
- Humans diploid number (2n) is 46 chromosomes (23 pairs)
- Mitosis results in 2 daughter cells that are diploid and identical to the parent cell
- Meiosis results in 4 daughter cells that are haploid and genetically different to the parent cell and eachother
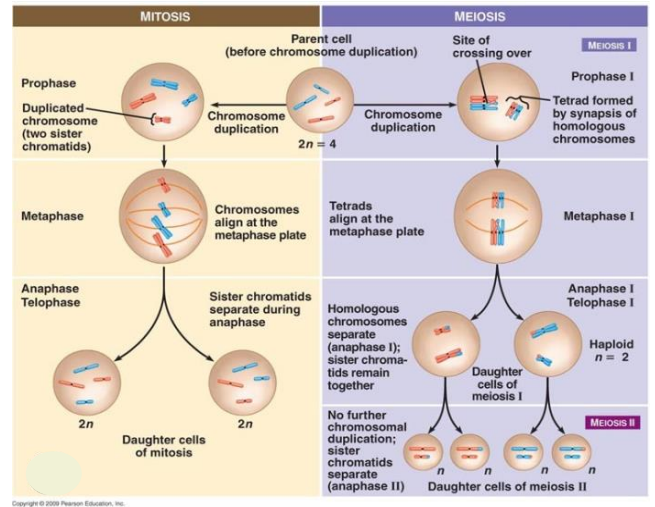
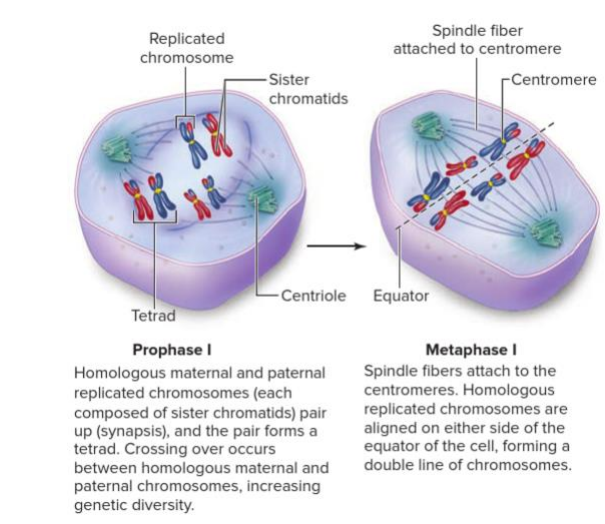
Important Meiosis Events
- Meiosis is important for increasing genetic variability of the species. This occurs due to:
1. Crossing Over during prophase 1
2. Random (independent) assortment in Metaphase 1
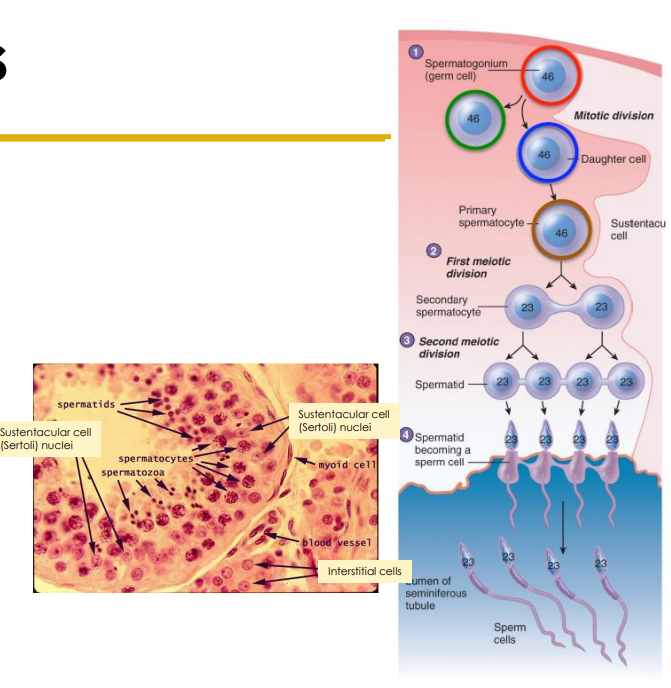
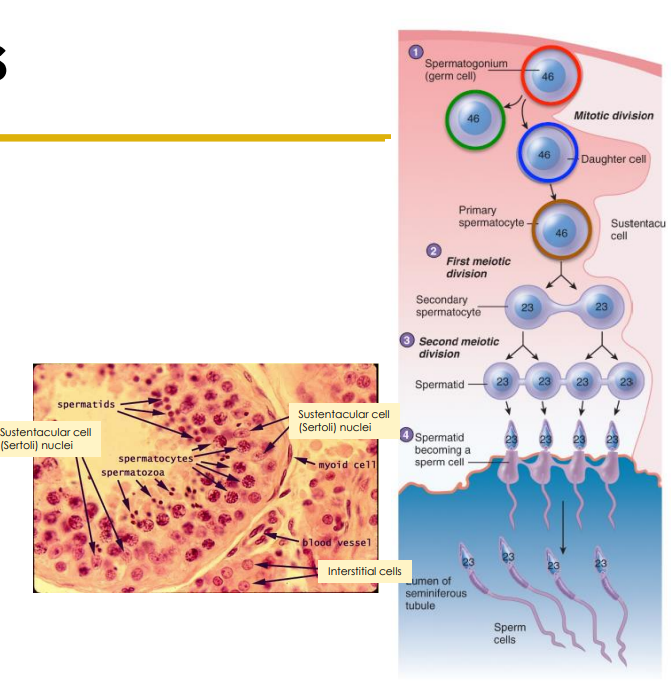
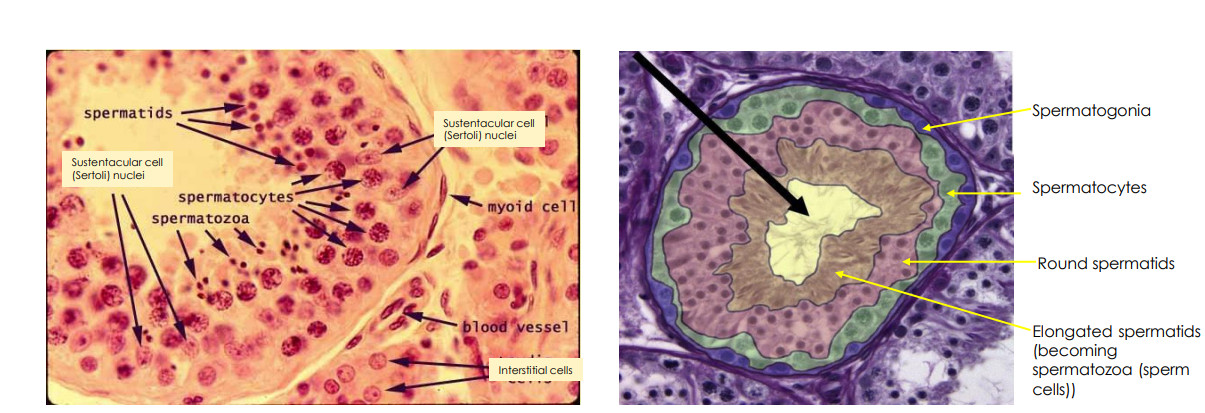
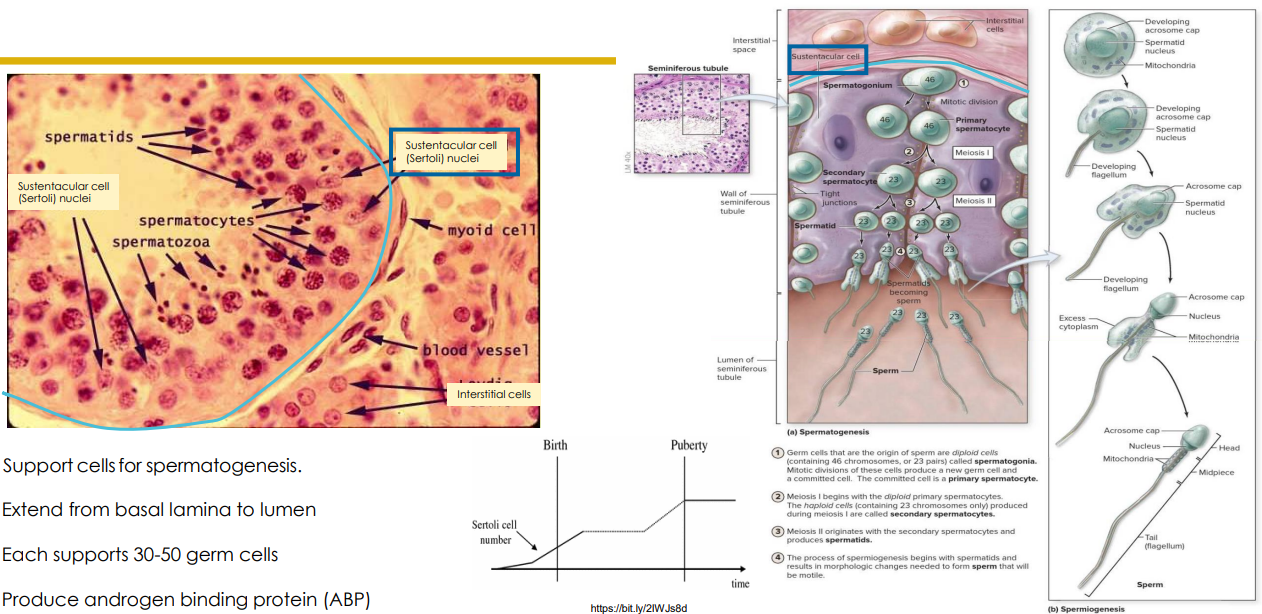
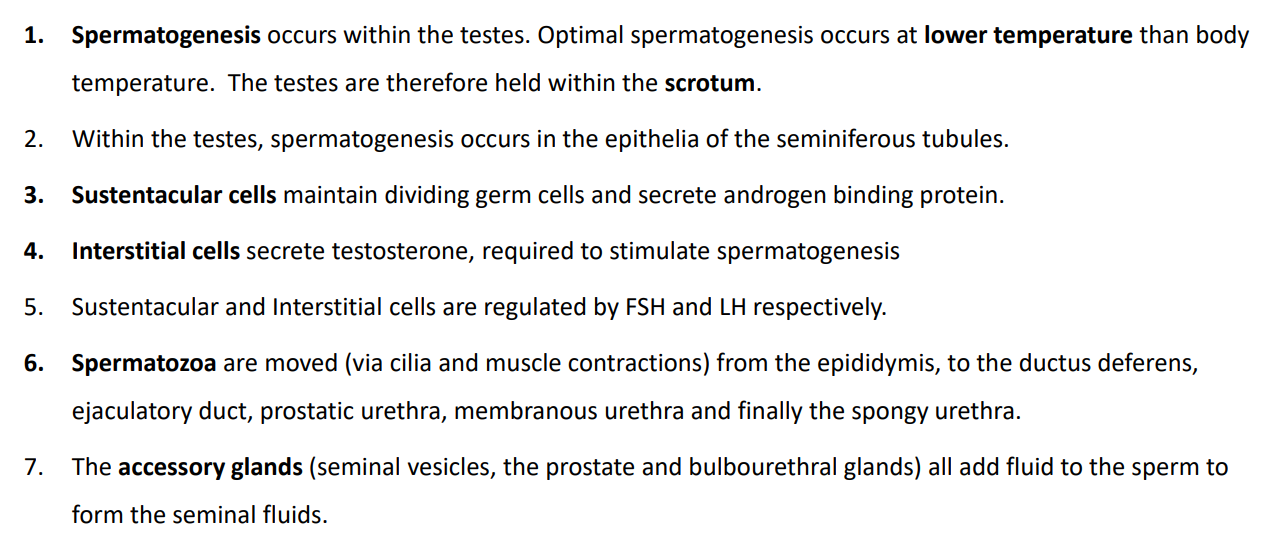
Spermatogenesis
- spermatigonia (stem cells) in outer layer of seminiferous tubules undergo mitosis. Results in Type A (2n) and Type B (2n) daughter cells
- Type B becomes primary spermatocyte (2n) and undergoes meiosis to produce the spermatids (n)
- spermatids undergo spermiogenesis to become spermatozoa (sperm cells)
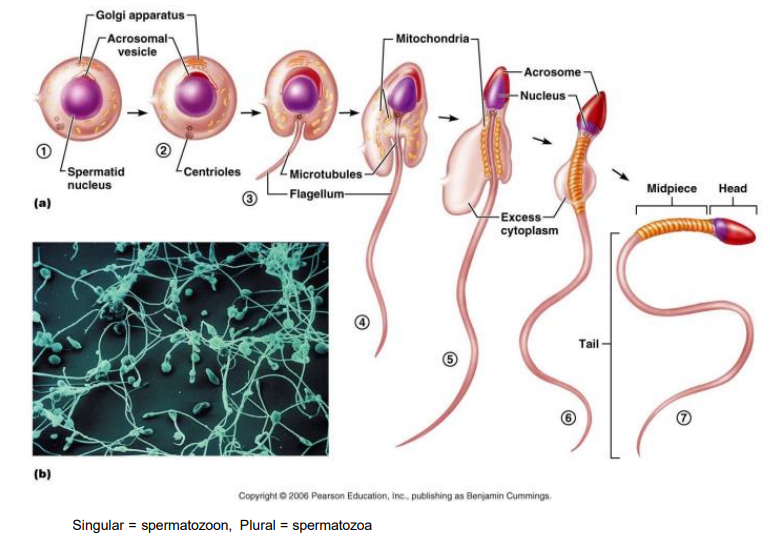
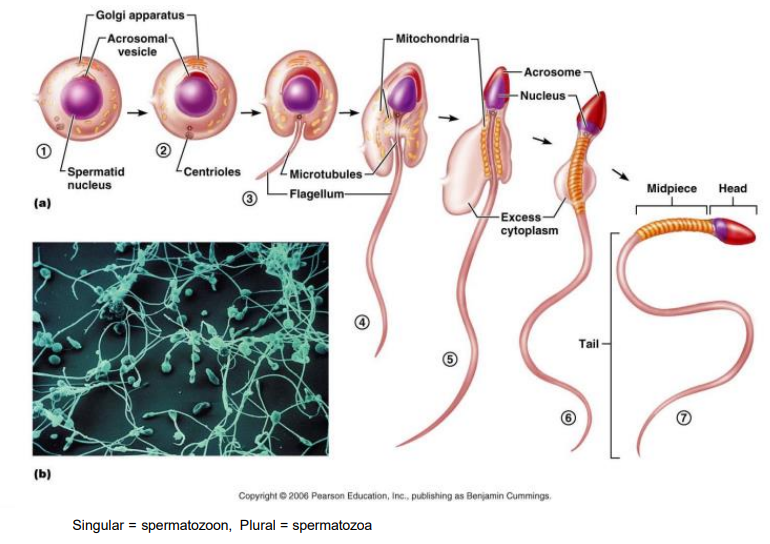
Spermiogenesis
- spermatids continue to mature as they are stored and move through the epididymis
- Head formed of acrosome (enzymes to penetrate ovum) and nucleus (DNA)
- midpiece = mitochondria
- Tail propel
- Some are motile when leave epididymis (most require capacitation)
- Leave as spermatozoa
Spermatogenesis Diagram
DIAGRAM ON SLIDE 25
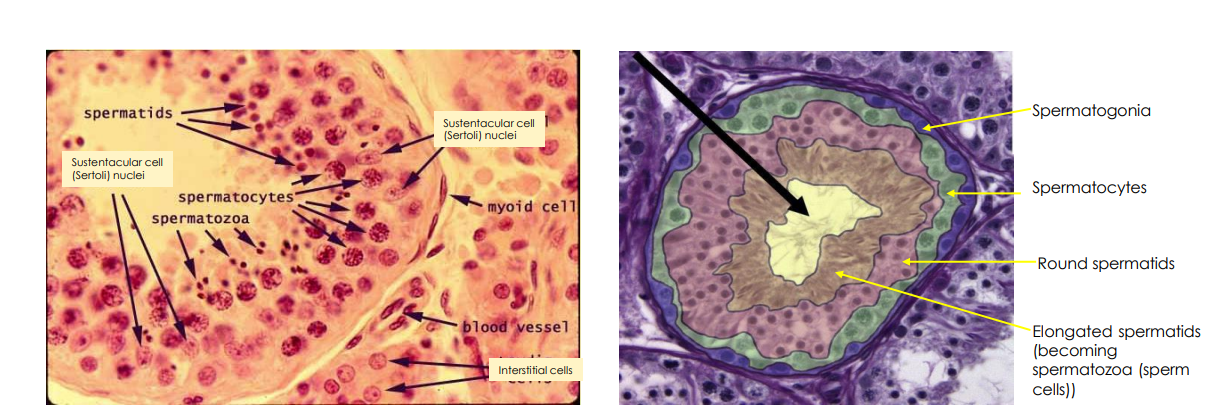
Sustentacular Cells
support and nourish the spermatogenic cells
- provides sustenance
- produce androgen binding protein
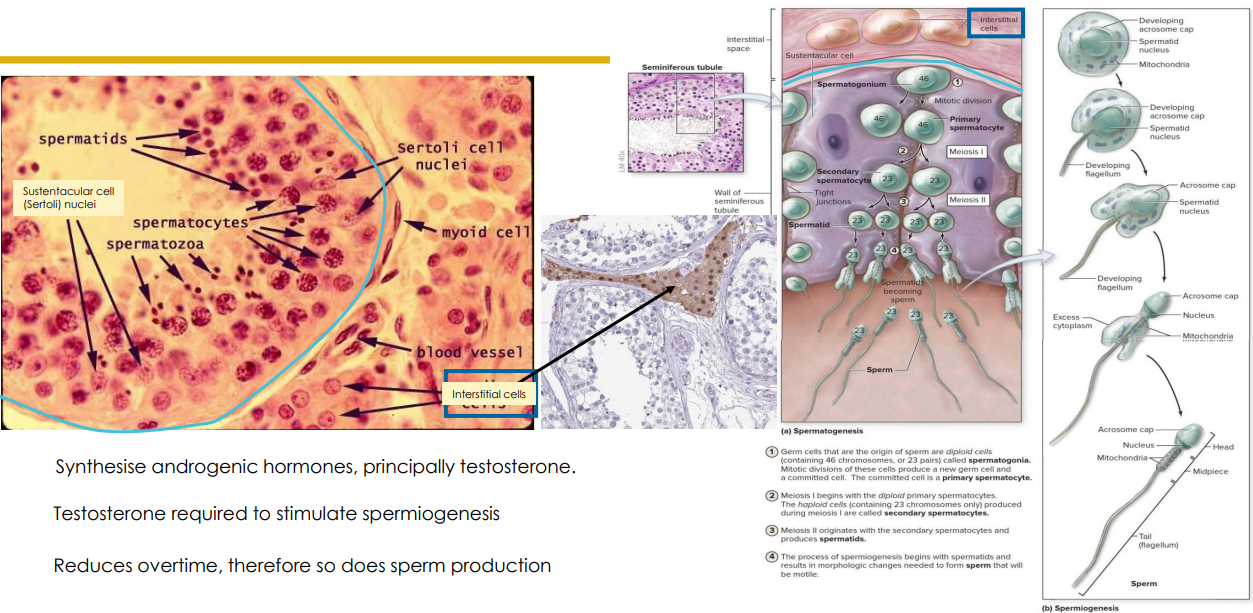
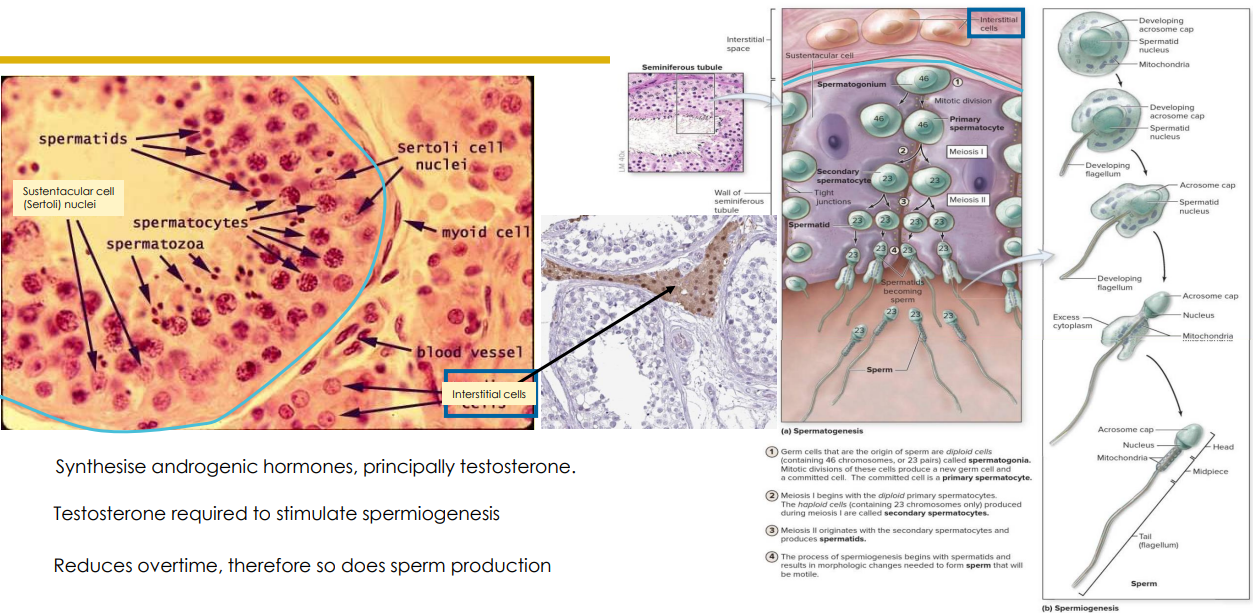
Interstitial Cells
- synthesise androgenic hormones, principally testosterone
- Testosterone required to stimulate spermiogenesis
- Reduces overtime, therefore so does sperm production
- stimulated by Lutenizing hormone (LH)
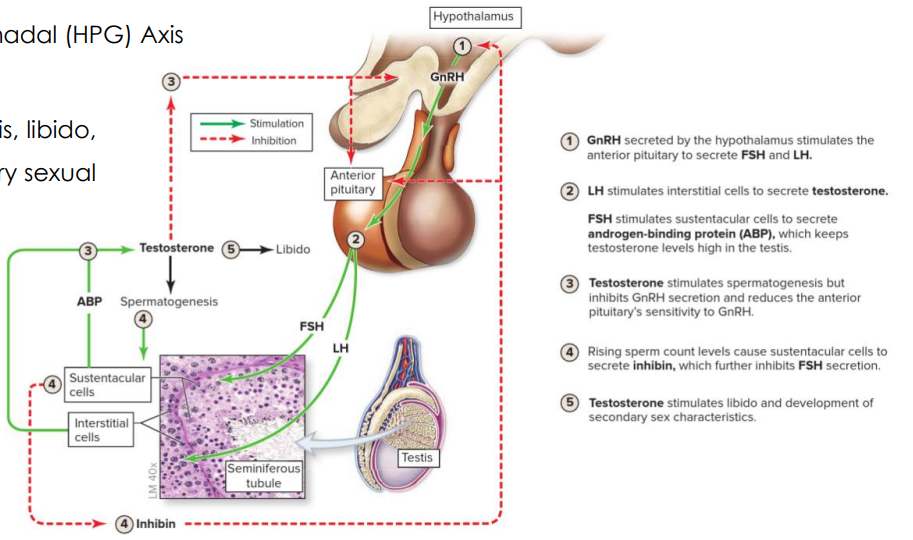
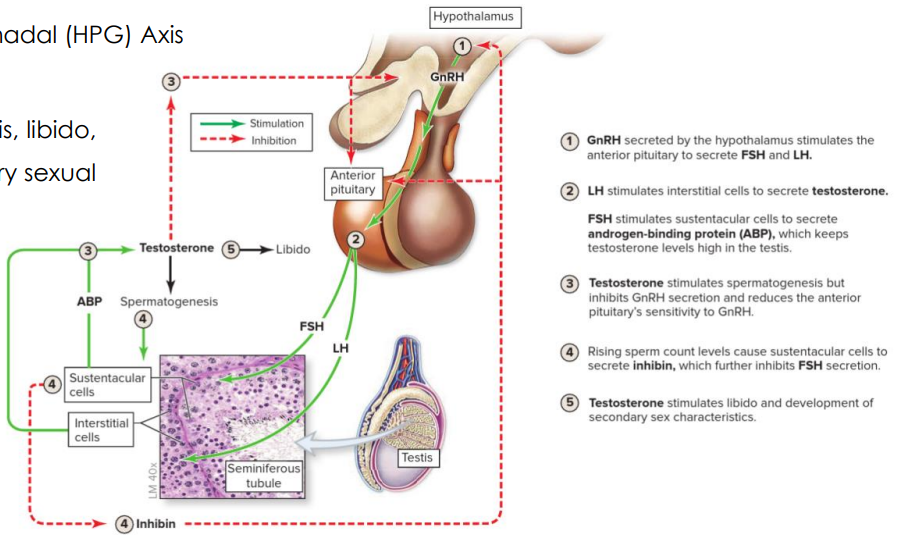
Testicular HPG Axis
Hypothalamo-Pituitary-Gonadal (HPG) Axis
- maintains spermatogenesis, libido, development of secondary sexual characteristics
- gonadotropin releasing hormone released by hypothalamus stimulates anterior pituitary secrete FSH and LH
- FSH stimulates sustenacular cells to secrete Androgen Binding Protein (ABP), which keeps testosterone levels high in testes
- LH stimulates interstitial cells to secrete testosterone
- Testosterone stimulates spermatogenesis but inhibits GnRH secretion and reduces the Anterior pituitary's sensitivity to GnRH
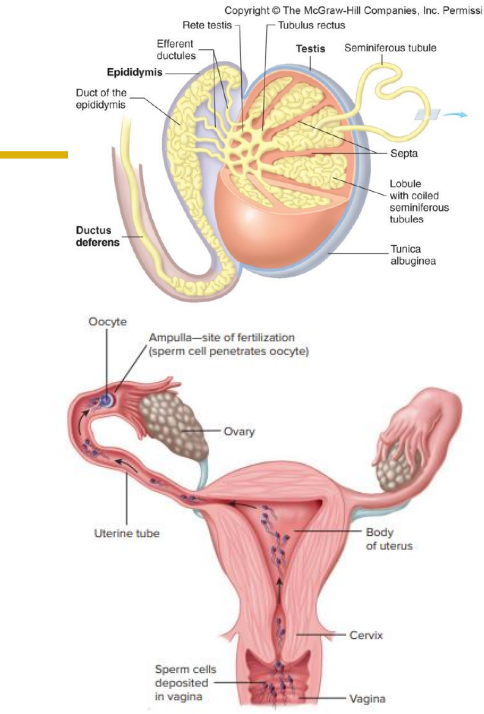
How do sperm move
- produced in seminiferous tubules
- ciliated efferent ductules sweep non-motile sperm into epididymis
- mature in epididymis (however most not fully motile yet)
- move through ducts via peristaltic (smooth muscle) contractions
- Capacitation: sperm become fully functional following exposure to seminal fluids and vaginal environment
- site of fertilisation is ampulla of oviduct. Sperm motility and uterine contracts
- Parasympathetic NS stimulates an erection. Sympathetic NS stimulate emission and ejaculation
TAKE HOME MESSAGES
DIAGRAM ON SLIDE 33