Exam 1
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
81 Terms
chronologic age
length of time since birth
perceived age
people’s estimation of someone’s age
subjective age
person’s perception of their age
functional age
reflects the cumulative effect of medical & psychosocial stressors on the aging process
More clinically relevant
ageism
stereotypes or generalizations (usually negative) applied to older adults grounded on the basis of age
aging anxiety
fears and worries regarding detrimental effects associated with aging
age attributions
tendency to automatically attribute problems to aging process instead of pathologic treatable conditions
Examples: problems with memory discounted as “a senior moment” or complaints of pain as “part of getting older”
myths
By 75 yrs, people are quite homogeneous as a group
Families no longer care for older people
By age 70 yrs, psychological growth is complete
Increased disability is due to age-related changes
Most older adults are constipated primarily due to age-related changes
realities
Older adults are diverse with different values and lifestyles just like young people
In the US, 80% of older adults’ care is provided by their families
Some brain functions decline but others continue to develop
Many problems attributed to old age are pathological and respond to treatment
Constipation is prevalent among older adults primarily due to risk factors and pathological changes
gender distributions of aging
Women live longer
At age 65 or older
23 million women (57%)
17.5 million men (43%)
Age 85 or older
70% are women
Men who are alive are more likely to be married
change in cultural groups in older adults
Trend toward population aging:
↑ racial/ethnic diversity
↑ proportion of foreign-born older adults (14% of older adults are foreign born)
Cultural diversity implications:
Values, communication, health beliefs & health behaviors are affected
african americans
Heterogeneous, have a wide range of socioeconomic conditions
Less likely to live alone, may have multi-generational household
Consequences of racism are still present and linked to health disparities
Factors contributing to poor health outcomes include discrimination, cultural barriers, and lack of access to health care.
Suspicion of health care providers linked to history of disparities
Trusted leaders/providers in community provides pathway to care—sometimes associated with religious institutions
asian americans
There is a large amount of diversity within the group
Strong value on care of older family members
Less likely to use nursing homes
More accepting of mental decline in older adult
Health is physical and spiritual harmony
hispanic american
Diverse group
Strong cultural respect for family and for older people
Older adults frequently live with family members
Health is a gift or reward given as G-d’s blessing
Most in US speak both Spanish and English
native
Value older members of the community, particularly with regard to their roles as grandparents and story tellers.
Strong traditions related to spirituality and religious practices, with each tribe having unique expressions
Belief in the connection among body, mind, and spirit
High rates of all of the following conditions: diabetes, tuberculosis, heart disease, substance abuse, and certain cancers (e.g., liver, cervix, kidney, gallbladder, and colorectal
Poorer health associated with low economic conditions, cultural barriers, access to care, and mistrust of health providers
strategies to mitigate bias
Cultural Self-Assessment:
An awareness-raising tool for gaining insight into the health-related values, beliefs, attitudes, and practices that have shaped and informed the person the nurse has become when providing care
Leverage available resources to learn more about cultural groups that are
frequently under your care
Ethnogeriatrics
the component of geriatrics that integrates the influence of race, ethnicity, and culture on health and well-being of older adults (1987).
Realize that educational materials about cultural groups provide general info about particular groups, but each group is made up of unique individuals.
Hence, the info should be used as a beginning point for a personalized assessment
All health care professionals are encouraged to contact local organizations to obtain culturally specific information about groups that reside in their locale
Healthy aging
no illness and preserved function
Active aging
high physical and cognitive function
Productive aging
social participation & engagement
Effective aging
the capacity to manage age related life challenges
Successful aging
full concept of aging well
compression of morbidity
Delay of onset of morbidity to shorten the time that morbidity is acquired between onset and death
wear and tear theory
Human ‘machine’ declines over time. Longevity affected by genetics & care provided
free radical theory
organisms age because they accumulate oxidative damage. Fix with antioxidants
vitamins
Immunosenescence theory
Age-related decline in immune system heightens susceptibility, may lead to autoimmune conditions such as RA
program theory
lifespan of every species/cell predetermined by a genetic program
Caloric restriction theory
Reducing calorie intake by 30-40% without malnutrition ↑lifespan in animals
relevance of biologic theories
Primary role: identify and address modifiable factors that lead to diseases, disability, death, as well as health-promoting factors
Nurses need to understand not only the relationship between aging and disease but also what “causes” healthy aging and longevity
Nurses serve as teachers and advocate for older adults
Attitudes of health care professionals
Perspective of “what do you expect, you’re old” interferes with treatable conditions
Attitude of hopelessness with subscribing to aging as a fatal disease
activity theory
older people remain socially and psychologically fit if they are actively engaged in life. Volunteering improves QoL
subculture theory
old people interact more among themselves, & status is based on health & morbidity
age stratification theory
address interdependencies between age as an element of the social structure and the aging of people in cohorts as a social process
person environment fit theory
Older individuals with functional limitations need to adapt to their environments in order to remain independent
relevance of sociological theories
View older adults in relation to society and environments
A better understanding of influences, e.g., culture, family, education, community, ascribed roles, cohort effects, home & living settings, personal & political economics
Emphasizes the importance of assessing environmental factors that influence the functioning of an older person
life course theories
Maslow Human Needs Theory: address the concepts of motivation and human needs
Hierarchical order of basic human needs
Erikson’ life-course theory: 8 stages of life
Trust vs. mistrust, autonomy vs. shame and doubt, initiative vs. guilt, industry vs. inferiority, identity vs. identify diffusion, intimacy vs. self-absorption, generativity vs. stagnation, and ego integrity vs. despair
psychological theories
The theory of selective optimization with compensation
Older adults can search for goals while disassociating from others and find resources for those goals
Can compensate for reduced skills with other skills
Hearing aids
Socio-emotional selectivity theory
Gero-transcendence theory: shifting from materialistic to a transcendent vision (1990)
relevance of psychological theories
Nurses can use psychological theories to address response to losses, continued emotional development
Maslow’s hierarchy of needs framework is useful for conceptualizing the nature of interventions in institutional or home settings
Devoting time and energy to life review and self-understanding can be beneficial for older adults
Nurses can facilitate this process by asking sensitive questions and by listening attentively to older adults as they share information about their past
Reminiscence: positive experience
Functional consequences theory
a framework to promote wellness, function, and quality of life for older adults
Reflects the evolving understanding of wellness as integral aspect of focused care of older adults
Goal: address unique relationships among concepts of person, health, nursing, and environment in context of promoting wellness for older adults
age related changes with FTC
Age-related changes are inevitable, irreversible & progressive and are not caused by extrinsic or pathologic conditions
On physiologic level: changes are typically degenerative
On psychological & spiritual levels: potential for growth
underlying concepts for FTC
Age-related changes & risk factors increase vulnerability to negative functional consequences
Nurses assess age-related changes, risk factors, and functional consequences
Goal: to identify factors that can be addressed through nursing interventions
Wellness outcomes enable functioning at the highest level despite presence of age-related changes & risk factors
FTC risk factors
Conditions that are likely to occur in older adults and have a significant detrimental effect on their health and functioning
Sources of risk factors: environments, acute and chronic conditions, psychosocial conditions, or adverse medication effects
Risk factors can be modified or eliminated to improve functioning and quality of life for older adults
A major focus of wellness-focused nursing is to identify risk factors that can be addressed through health promotion interventions
functional consequences
Observable effects of actions, risk factors, and age-related changes that influence the quality of life or day-to-day activities of older adults.
Actions: purposeful interventions initiated by either older adults (i.e., self-care) or nurses (i.e., nursing interventions) and other caregivers.
Risk factors can originate in the environment or arise from physiologic and psychosocial influences.
Negative functional consequences: interfere with a person’s level of function or quality of life or increase a person’s dependency
Positive consequences: facilitate the highest level of performance and the least amount of dependency
wellness outcomes
Context of the interplay among the many factors that influence health and aging
Determinants of living long and well:
Inherit good genes
Avoid oxidative damage
Protect from oxidative damage with antioxidants from natural sources
Maintain optimal weight
Engage in physical exercise
Engage in meaningful social interactions
Develop close personal relationships
Maintain a sense of spiritual connectedness
Reject ageist stereotypes
wellness outcome for MS changes
Decrease fall incidence and improve MS function
ADLS vs IADLS
ADLS
Dressing, Eating, Toileting, Bathing
IADLS
cooking, transportation, managing finances
assessing decision making capacity
Occurs over time -- not a one-time occurrence
Decisional Capacity may fluctuate “window of lucidity”
Decision specific & directly related to risk
MacArthur Competency Assessment Tool for Treatment (MacCAT-T) is widely used
Nursing responsibility – document specifically and descriptively what are patient’s/surrogate’s understanding & wishes
Elder Abuse
a) intentional actions that cause harm or create a serious risk of harm (whether or not harm is intended) to a vulnerable elder by a caregiver or other person who stands in a trust relationship, or
b) failure by a caregiver to satisfy the elder’s basic needs or to protect the elder from harm.
Any knowing, intention, or negligent act that causes harm or a serous risk of harm to a vulnerable older adult
Physical Abuse
Inflicting pain or injury on an older adult
Hitting, slapping, punch, kicking, bruising, restraining by physical or chemical means
Signs
Broken bones
Bruises
Head trauma
Bruising on areas of body like abdomen/back
Signs of strangulation
Inconsistent stories or stories that don’t line up
Sexual Abuse
Nonconsensual sexual contact
Remember that those with neurocognitive disorders may not be able to give consent
Signs:
Unexplained STIs
Bruises on thighs/genitals
Bleeding on thighs/genitals
Inappropriate relationships between caregiver and elder
Financial Abuse
Illegal taking, misuse, or concealment of funds/property/assets of an older adult for someone’s benefit
Signs:
Large sums of money missing from bank statements
Cannot access own bank records
Provides monetary gifts in exchange for companionship
Unexplained transactions
Emotional Abuse
Inflicting mental pain, anguish, instilling fear or distress on an older adult through verbal or nonverbal acts
Signs:
Hesitation to talk freely
Isolation
Suffering from anxiety/depression
Neglect
Failure to provide food, shelter, healthcare, or protection to a vulnerable older adult by the caregiver
Signs:
Pressure ulcers
Lack of basic hygiene
Missing medical supplies (walkers, dentures, medications)
Uninhabitable living condition
Abandonment
Desertion of vulnerable older adult for anyone who has assumed the responsibility or custody of care of the individual
Signs:
Being left alone without food
If they cannot care for themselves and are left alone
Scams
Phone and email scams are incredibly prevalent
Important to educate the older adult about to help avoid becoming the victim of this type of elder abuse
Self-neglect
Failure of a person to perform essential self-care tasks
Threatens their own health/safety
Signs:
Failure to thrive
Can warrant involuntary hospitalization
risk factors for elder abuse
Functional dependence or disability
Poor physical health
Cognitive impairment
Low income
Being Female
Financial Dependence
Race/ethnicity (Hispanic experience lowest rate of elder abuse)
Perpetrator risk factors
Ageism
Cultural norms
Perpetrator Risk factors
Mental health issues
Substance use issues
Dependency on older adult
Ineffective coping – high rates of stress
elder abuse screening
United States Preventive Services Task Force
Insufficient evidence to recommend for or against routine screening for elder
abuse
Only recommended in pregnant women/women of childbearing age
Screening tool: Elder Mistreatment Assessment
Patients should be interviewed by themselves to avoid intimidation by possible abusers
Asked about family situation and living arrangements
Patients should be asked directly about abuse, neglect or exploitation:
Has anyone at home ever hurt you?
Has anyone ever touched you without your consent?
Has anyone taken anything that was yours without asking?
Are you alone a lot of the time?
Should look for indicators of abuse, including poorly explained injuries; evidence of neglect
(dehydration, malnutrition, poor hygiene, lack of medical compliance); isolation; fear of a caretaker; or transfer of funds to a caretaker
nurse responsibilities
Mandated Reporting
Any person having reasonable cause to believe that an older adult, or someone within the state who is 60 years of age or older, is in need of protective services may report such information to the agency which is the local provider of protective services
The first obligation of nurse is to assure the safety of the older adult.
A home visit may sometimes be needed to make that determination → collaboration with case managers, community workers, etc.
Adult Protective Services reporting
Reserve
inherent ability to maintain homeostasis amidst external stressors
Resilience
ability to recover quickly from illness
Atypical presentation
vague presentation, altered presentation or non-presentation of illness
vital sign changes
Core body temperature
Circadian fluctuation less pronounced.
Reduction in fever response—slight increase in temp may indicate serious infection in the oldest
Resting heart rate often slightly higher.
Maximal heart rate decreases.
Heart rate variability decreases – decreased ability to respond to stress
Apical pulse more accurate.
Respiratory rate generally unchanged at rest; increase to compensate for decreased minute volume.
Increases risk for pulmonary infection.
Blood pressure – systolic hypertension with widened pulse pressure often occurs.
Arterial wall stiffness requires higher pressures to achieve forward flow.
Decline in autonomic sensitivity—increased risk for hypotension
Worry about high diastolic
cosmetic changes
Skin becomes fragile, loose, and transparent (hands/forearms); purple patches/macules called actinic purpura are frequently seen.
Risk for skin tears increases.
Nails lose luster, yellow, and thicken, especially toes
Hair loses pigment and hairline recedes; also loss of hair occurs elsewhere such as trunk, pubic area, axillae and limbs, which is normal
Turnover rate of cells decreases with age –takes longer to re- epithelialize, i.e. wounds take longer to heal
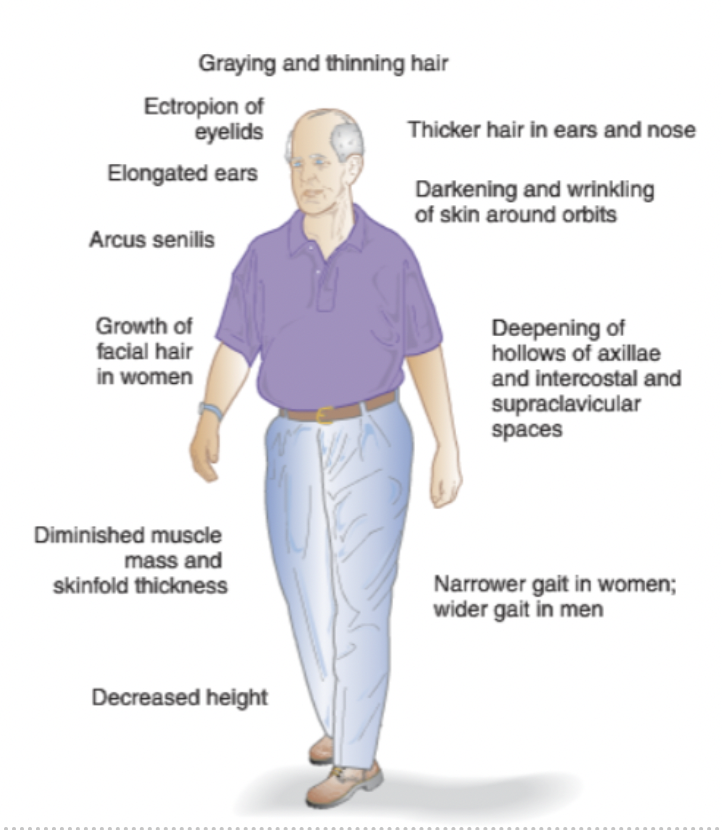
sensory changes
eyeballs recede into orbit
corneas lose luster
pupils become smaller
dry eyes are a common complaint
presbyopia occurs to nearly everyone.
Need for “Readers”
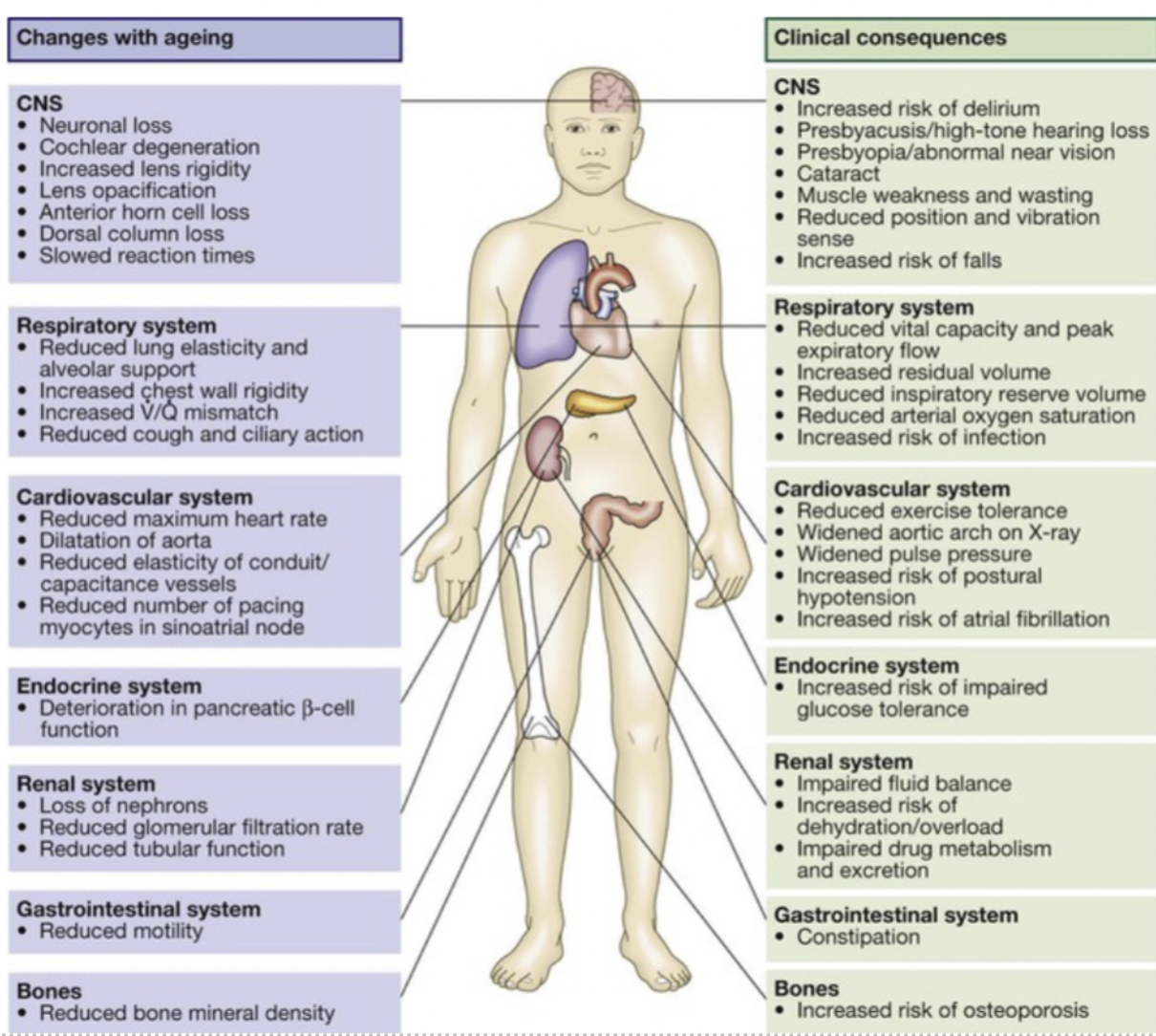
respiratory function
Clinical implications of age-related changes:
↓Cough & gag reflexes
Increased risk of aspiration pneumonia
Compromised chest expansion.
↑Use of accessory muscles.
↓Efficiency of gas exchange.
Diminished lung sounds.
No effect in daily functional activity
Diminished pulmonary reserve: fatigue with stressors, ↑risk of infection
Risk Factors
Tobacco use
Secondhand smoking
Lack of immunization (e.g., pneumonia & influenza vaccine)
Immobility
Exposure to air pollution
Pathological conditions
COPD/Other lung diseases (e.g., URTI, pneumonia, etc)
cardiac changes
Arteries with less elasticity -increased peripheral resistance- Increase in BP
Decreased ability to compensate to stressor
Decreased cardiac contractility- cardiac output
Decrease integrity of heart valves
No effect in daily functional activity
These result in decrease in cardiac reserve:
↓Exercise tolerance
Fatigue, SOB with exercise
Slower recovery from tachycardia
Intolerance of volume depletion
GU changes
Kidneys
Decrease in volume and weight of the kidneys
Decline in the total # of glomeruli Decreased GFR
80 yr old – 50
90 yr old – 40
Normal is greater than 60
Decreased creatinine clearance risk of drug toxicity
Bladder
Bladder capacity decreases
Decrease in detrusor muscle contractility
Alterations in sensation of needing to void
Prostate
Proliferation of prostate epithelial and stromal tissue, known as benign prostatic hyperplasia, 90% of men >age 80 have symptomatic BPH
genitalia changes
Female genitalia: menstrual periods cease between ages 48 and 55; women often experience hot flashes for up to five years and may have vaginal dryness, incontinence, or dyspareunia; within 10 years, the ovaries are usually no longer palpable
Male genitalia: sexual interest remains intact with aging but frequency declines; ; gradual decline in fertility; decreased sperm production; erection is more dependent on tactile stimulation
endocrine changes
Progressive deterioration in number and function of insulin- producing beta cells
Decrease in lean body mass with relative increase in adiposity
Increased insulin resistance
Decrease in renal concentrating function with even mild hyperglycemia can lead to osmotic diuresis
May develop (transient) hyperglycemia especially with stress (surgery)
MS changes
Significant shortening becomes obvious in old age with most loss of height occurring in the trunk as intervertebral discs become thinner and vertebral bodies shorten/collapse from osteoporosis
Bone loss: increased bone resorption, diminished calcium absorption, impaired regulation of osteoblast activity
Skeletal muscles decrease in bulk and power: size & number of fibers, loss of motor neurons, replacement of muscle tissue by connective tissue, eventually fat tissue
Joints: range of motion diminishes
nervous system changes
Aging may affect all aspects of the nervous system, from mental status to motor and sensory function and reflexes
Reaction times decrease – issues driving
Most older adults do well on mental status exam, but selected impairments become evident
Nerve cells in the brain decrease a small loss of brain mass
Decrease in the synthesis & metabolism of the major neurotransmitters
Autonomic nervous system performs less efficiently orthostatic hypotension
Neurologic changes affect gait and balance
GI changes
Dysphagia (difficulty swallowing)
Gastric mobility slow modestly -> delayed emptying of stomach contents and early satiety
Constipation is not a normal aspect of aging even though gastric motility slows
Diminished secretion of gastric acid and pepsin, result of pathologic conditions rather than normal aging
Diminished absorption of nutrients in the small intestine (calcium and vitamin D)
At increased risk of constipation (constipation is still not normal)
health promotion
Patient Centered Decision Making
Risks and Benefits
Cultural and Socioeconomic Considerations
Silver Sneakers and other Medicare Programs availible
orthostatic hypotension
A drop in SBP by ≥20 mmHg or DBP by ≥ 10 mmHg within 3 mins of standing from a supine or sitting position
Affects >30% of older adults. May lead to falls,↓ function & ↓ QoL
Orthostatic vital signs are indicated for:
Patients at risk for falls, hypovolemia
History of syncope or near syncope (dizziness, fainting)
Management
Drink 1.5-2 L of water/day
Avoid excess alcohol
Incorporate more salt into diet if no other contraindications
When waking in the morning, sit on the edge of the bed for 5 min before standing
Sleep with head of bed elevated 15-20 degrees
Wear compression socks
Perform calf exercises
postprandial hypotension
a condition in which there is a systolic blood pressure drop of 20mm Hg in a supine/sitting position within 120 minutes after eating a meal.
PPH occurs more often than postural hypotension (PH), and infrequently together with PH, among older adults.
Studies from long-term care facilities suggest prevalence of PPH at 24-36%
Management
Adjust activities around meals, lying down or walking may help after meals
Adjust drug timing: should not take antihypertensive drugs within an hour before meals
Eating small, low-carbohydrate meals more frequently rather than large meals
Avoid alcohol before and after meals
Changes in renal function
↓ renal blood flow
↑ half life of many drugs
↓ GFR & renal tubules function
After age 40, creatinine clearance ↓ an average of 8 mL/min/1.73 m2/decade
Note: Despite the ↓ Cr clearance, older adults' serum Cr may be normal because they produce less creatinine. It is critical to evaluate creatinine clearance: Cockcroft and Gault equation: CrCl = [(140 - age) x IBW] / (Scr x 72) (x 0.85 for females):
Hepatic changes
↓ hepatic blood flow
↓ first pass effect
↓ Detoxification & conjugation
Changes in enzymatic function esp. cytochrome P-450 system
Warfarin and phenytoin levels may be higher because of altered metabolism
Note: Beware of food effects (e.g., grapefruit juice contains chemicals that inhibit CYP3A4)
Body Composition
↑ adipose tissue = ↑ volume of distribution = prolonged action (increased half-life) of lipophilic drugs (e.g., diazepam)
↓ total body water = ↓ volume of distribution = higher concentration of water-soluble drugs (e.g., atenolol)
↓ lean muscle mass may lead to hypoalbuminemia and ↓ distribution of protein-bound drugs (e.g., warfarin) thus ↑ concentration of unbound (free or active) form of drugs
Note: In patients with an acute disorder or malnutrition, rapid ↓ in serum albumin may lead to ↑ serum concentrations of unbound drug and enhanced drug effects/toxicity.
Receptor sensitivity
↑receptor sensitivity to narcotics, alcohol, bromides, ACEIs, diazepam = ↑potency
↓receptor sensitivity to beta blockers, furosemide, dopamine, propranolol = delayed signs of toxicity
Multiple drugs acting on the same or interrelated receptor sites: additive, synergistic/antagonistic effects
Baroreceptor sensitivity decreases with age
medication interactions
narrow therapeutic index
aminoglycosides, digitalis, lithium, heparin, coumadin (warfarin)
affecting vital physiology of the body
antihypertensive, anti-diabetics, anticoagulants
with high plasma protein binding capacity
NSAIDs, Warfarin, Sulfonylureas
common drugs
warfarin
insulin - really excreted
oral anti platelets
oral hypoglycemic agents
benzos, NSAIDs
HEDIS and BEERS drugs
ADE risk factors
>6 chronic disease
>12 doses/day
≥ 9 medications
Low BMI (<22kg/m2)
Age >85 years
Creatinine clearance < 50 mL/min
History of prior ADE
BEERS criteria
Consensus-based list of potentially inappropriate medications for older adults
Published 1991, latest revision 2019
Statistical association with ADEs has been documented
Adopted for nursing-home regulation
Does not account for the complexity of the entire medication regimen
Anticholinergic medications
Decongestants
Hypertension
Bladder outflow obstruction
Meperidine
Benzodiazepines