Lecture 2: Inflammation
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
Inflammation is a protective response to…(3)
eliminate the initial cause of cell injury (foreign invaders and necrotic tissue) with WBC
clean infection and other noxious stimuli
initiate repair of injured tissue
In which instances can inflammation be a harmful reaction if it is also a protective response?
too strong
prolonged
inappropriate (autoimmune disease)
T/F: the goal of inflammation is to bring cells of host defense such as leukocytes and plasma proteins to the site of infection or injury
true
The inflammatory reaction develops in stages known as the 5 R’s, what are they?
recognition of injurious agent
recruitment of leukocytes
removal of agent
regulation of the response
resolution/repair
Describe the onset, cellular infiltrate, tissue injury, fibrosis, and local and systemic signs of acute and chronic inflammation
Acute
onset: fast - min to hours
cellular infiltrate: neutrophils
tissue injury: mild and self-limited
fibrosis: non
local and systemic signs: prominent (bug bite)
Chronic
onset: slow - days
cellular infiltrate: monocytes/macrophages and lymphocytes
tissue injury: significant
fibrosis: in severe and progressive instances
local and systemic signs: variable, usually modest
When does fibrosis occur?
In response to long standing damage.
In times the body is unable to regenerate tissue leading to scarring
What are the cardinal signs of inflammation?
heat (calor)
redness (rubor)
swelling (tumor)
pain (dolar)
loss of function (functio laesa)
Which cell types arrive to the injury site in acute inflammation?
leukocytes and plasma proteins
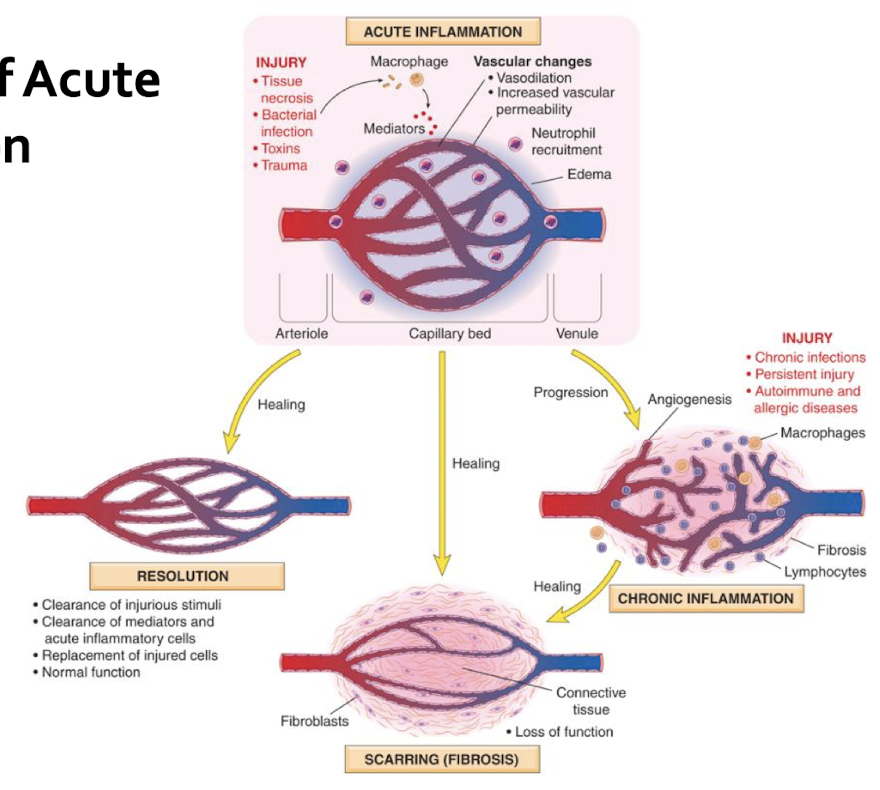
What are the two components of acute inflammation
Vascular changes
vasodilation and increased vascular permeability allow plasma proteins to leave circulation
the endothelial cells are activated and that increases migration of leukocytes
Cellular events
leukocytes (mostly neutrophils) are recruited allowing for elimination of agent
What are the stimuli of acute inflammation?
infection
trauma
tissue necrosis
foreign body
immune reactions (hypersensitivity)
How does acute inflammation recognition occur?
Microbes, necrotic cells, and foreign substances are recognized by receptors (toll-like receptors TLR) on phagocytes, dendretic cells and epithelial cells on the PM
Inflammasome recognize dead cell products
activate cytokine interleukin 1B which recruits leukocytes
Compare the intracellular and extracellular pathway for recognizing acute inflammation
Extracellular
receptors on the cell surface or in the extracellular environment to detect microbes and tissue injury
TLR receptors detect bacterial cell wall components
release extracellular mediators (histamine, prostaglandins) producing vasodilation, vascular permeability, neutrophil, and chemotaxis
Intracellular
sense infection or damage inside the cell with macrophages, dendritic cells, and neutrophils
Inflammasomes detect
can trigger inflammatory cell death
In acute inflammation, what occurs during vascular changes?
vasodilation causes increased permeability bringing cells and proteins to injury site
arteriolar vasodilation increases blood flow causes erythema and warmth
Microvasculture increases blood viscosity = slowing circulation to prevent movement of bacteria
Neutrophils accumulate at vascular surface
protein rich fluid (exudate) moves into the extravascular tissues causing an increase in osmotic pressure causing more water in the tissues = causing edema
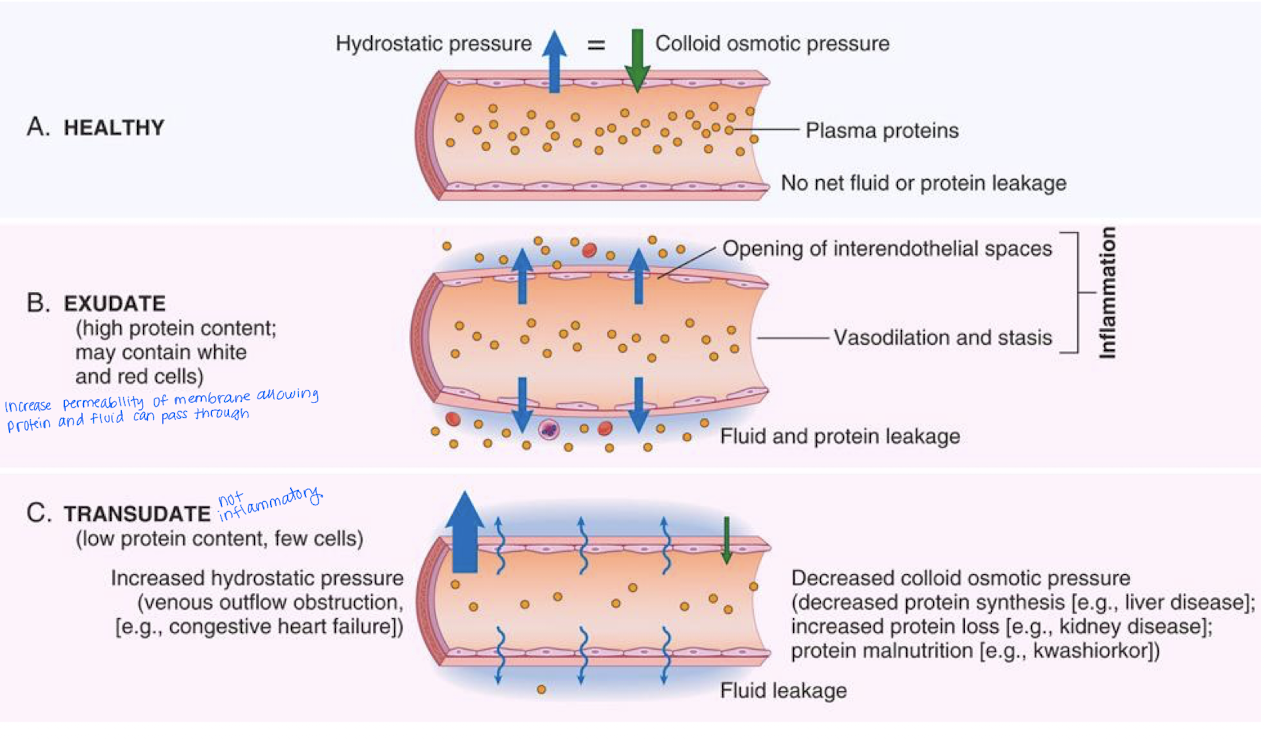
Exudate vs Transudate
Exudate - protein rich fluid (opaque) and a response to inflammation
Transudate - intersitiual fluid accumulation caused by increased hydrostatic pressure
low protein concentration
non-inflammatory response
What is included in leukocyte recruitment in an acute inflammation?
leukocyte rolls along the vessel wall by selectins (proteins)
Adhesion to the endothelium with integrins (proteins)
migrates between endothelial cells
migrates in the interstitial tissue toward a chemotactic stimulus (following a chemical signal) to the macrophage (possibly to interstitial tissue where edema is ocurring due to inflammation)
During an acute inflammation, leukocyte activation includes phagocytosis. What are the 3 steps?
Recognition and attachment of particle to the ingesting leukocyte
Engulf the phagocytic vacuole (phagosome)
kill and degrade ingested material
______ are extracellular fibrillary networks produced by neutrophils in response to pathogens and inflammatory mediators. They trap microbes to prevent their spread and cause cell death
Neutrophil extracellular traps (NETs)
acute inflammation - leukocyte activation
How can leukocytes induce tissue injury/ in which circumstances?
Bystander tissue is injured during defense reaction
attempt to clear damaged and dead tissues (after MI)
inflammatory response directed at host tissues (autoimmune or allergic diseases)
What are 3 outcomes of acute inflammation
Complete resolution: regneration and repair
inflammatory response is terminated
necrotic debris, edema fluid, and inflammatory cells are cleared by phagocytes and lymphatic drainage + leukocytes secrete cytokines to initiate repair
Healing by CT replacement: scarring or fibrosis
Progression to chronic inflammation

Which morphologic pattern exemplifies:
accumulation of serum-like protein-rich exudates
skin blistering (burn/viral infection) - accumulation of serous fluid or beneath damaged epidermis
Serous inflammation
Which morphologic pattern exemplifies:
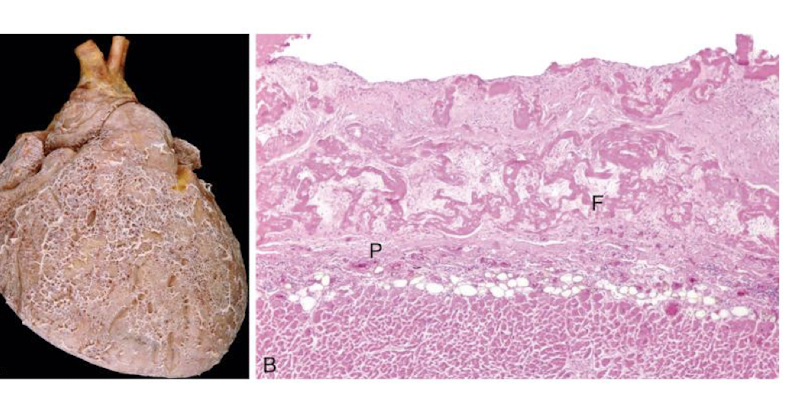
characteristic of inflammation in the lining of body cavities including the meninges, percardium, and pleura
ex: fibrinous pericarditis
occurs with severe injury increasing vascular permeability and fibrinogen passes through the endothelial barrier
Fibrinous inflammation
Which morphologic pattern exemplifies:
collection of purulent exudate with presence of abscess
ex: pyogenic (pus forming) organism - staphylococci
Suppurative (purulent) inflammation and abscess formation
focal collection of pus caused by seeding of pyogenic organisms into a tissue
Abscess
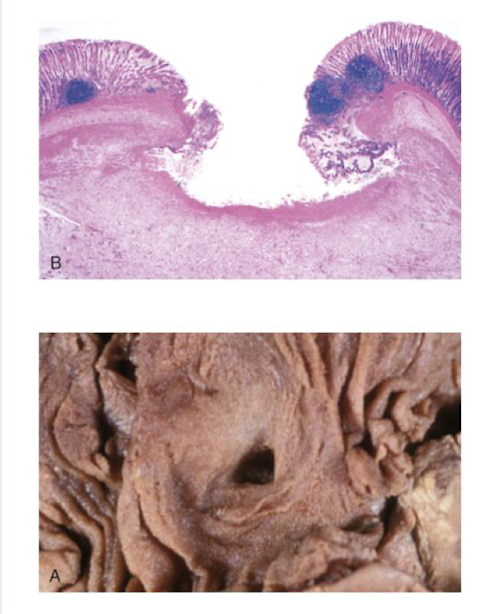
Which morphologic pattern exemplifies:
local defect of the surface of an organ or tissue
produced by necrosis of cells sloughing off necrotic and inflammatory tissue
occurs in GI mucosa
ex:diabetes
Ulcer
What are chemical mediators?
are substances (usually small molecules, peptides, or proteins) that are released by immune cells, damaged tissues, plasma proteins, or microbes.
They initiate, regulate, and resolve the inflammatory response.
They explain the cardinal signs of acute inflammation
Vasodilation is induced by _______ and is the cause of erythema and stasis of blood flow
chemical mediators
What is the role or function of histamine?
a chemical mediator that causes arteriolar dilation and increased vascular permeability
can be released by vasodilation, mast cells, platelets
stimulated by substances inducing inflammation, IL-1 and IL-8
What is the MAC complex and what is its role in the compliment system?
Stands for membrane attack complex and it creates holes in the target cell’s membrane leading to loss of osmotic balance (water rushes in) and cell lysis.
What is the function of the Coagulin and Kinin systems
Coagulation cascade will stop bleeding but also produces by-products that promote inflammation by recruiting leukocytes and increasing permeability.
Kinin system produces bradykinin a mediator of inflammation and pain.
both are activated by factor 12 (Hageman factor)
Togther they function to seal an injury, recruit immune cells, increase vascular changes, and signal pain to the brain
When would we see chronic inflammation (give examples)
Persistent infections (TB, syphilis)
Immune-mediated inflammatory disease (RA, psoriasis)
Prolonged exposure to toxic agents (cholesterol crystals = atherosclerosis)
What is the role of macrophages?
Occur in an chronic inflammation response
ingest and eliminate microbes and dead tissue
initiate process of tissue repair
secrete mediators of inflammation (cytokines)
display antigens to T-lymphocytes
Chronic inflammation: What are eosinophils?
found in inflammatory sites around parasitic infections and immune reactions mediated by IgE
recruited by adhesion molecules and chemokines
Chronic inflammation: What are mast cells?
participate in acute and chronic inflammation
when antigen is encountered, mast cells release histamine causing vascular changes of acute inflammation (anaphylactic shock)
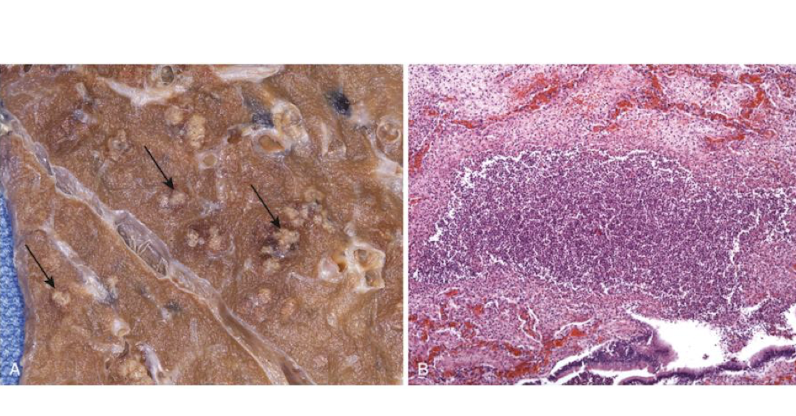
Chronic inflammation: What is granulomatous inflammation?
A form of chronic inflammation characterized by the formation of granulomas, which are aggregates of macrophages
Give examples of granulomatous inflammation
TB
leprosy
syphilis
Cat-stratch disease
sarcodiosis
Crohn disease
Systemic effects:
which leukocytes would we see dominate in a bacterial condition?
viral?
allergy such as hay fever, asthma or parasitic infection?
neutrophils
lymphocytosis
eosinophilia
Chemical mediators can be _____ and ______ derived
plasma, cell
Which chemical mediators are cell derived?
Histamine and serotonin