canine midterms
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
Functions to carry vital oxygen into the body and expel carbon dioxide, a metabolic waste, out of the body
2 portions:
upper airways: nasal passage, sinus, pharynx and larynx
lower airways: trachea, bronchi, bronchioles, alveoli, and lungs
Respiratory system
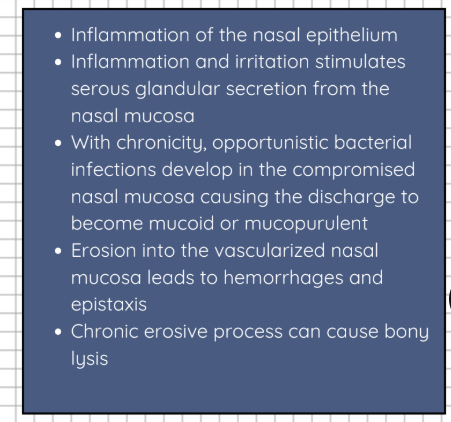
Rhinitis
Causes of Rhinitis
Fungal disease: _______________
Tooth rooth abscess
Foreign body
Parasitic: ___________
Neoplasia (i.e adenocarcinoma)
Allergy
Canine Distemper
Bordetella bronchiseptica
**case may progress into pneumonia when agents colonizes the lower respiratory tract
Aspergillus fumigatus, Penicillum spp., Rhinosporidium seeberi, Blastomyces dermatitidis, Cryptococcus neoformans
Pneumonyssoides caninum (nasal mite), Capillaria aerophagia
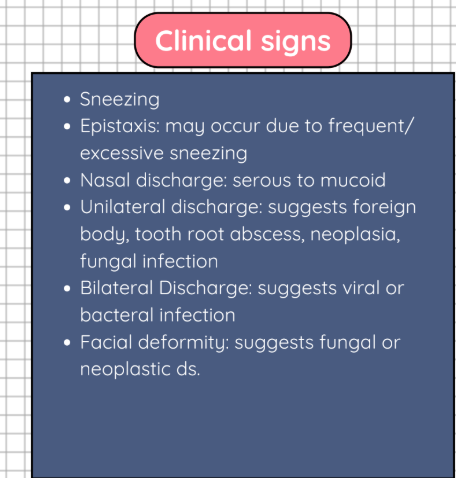
Rhinitis
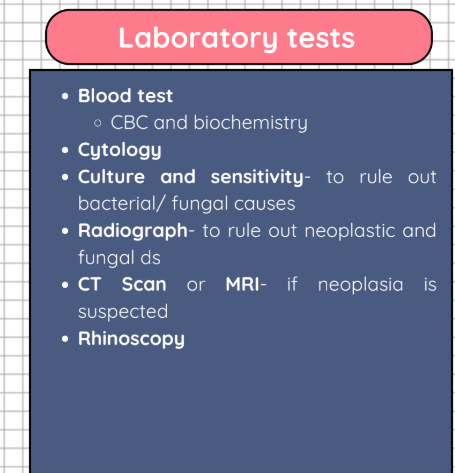
Lab tests of Rhinitis
Rhinitis treatment
Depends on the underlying cause
Antibiotics: for primary and secondary bacterial rhinitis
Antifungals: for fungal rhinitis
1.-
2.-
3.-
IV
Nebulized
_______-
Steroid/ antihistamine: for allergic
rhinitis
Ketoconazole
Itraconazole
Flucoconazole
Amphotericin B
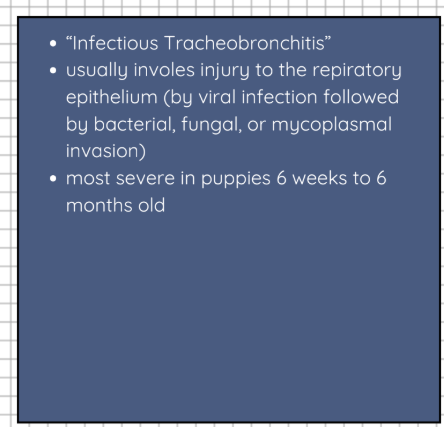
Kennel cough
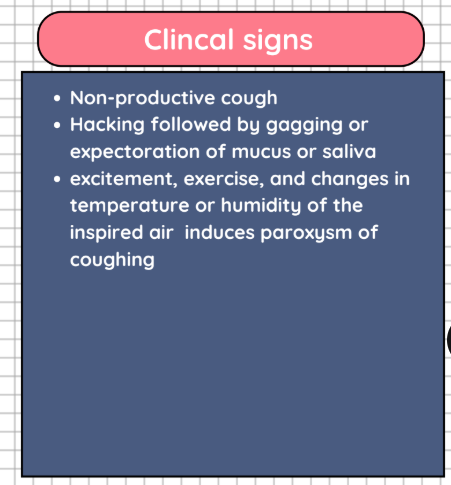
Kennel cough
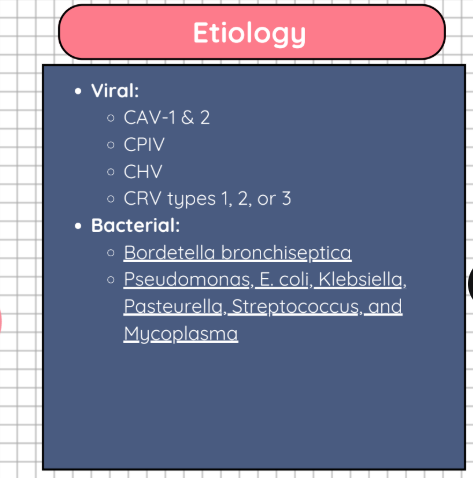
Etiology of Kennel cough
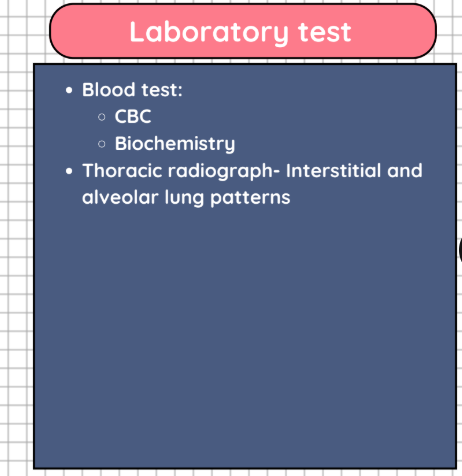
Lab tests of kennel cough
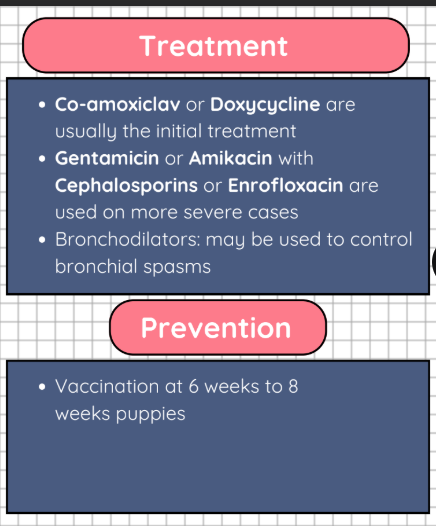
Tx for Kennel cough
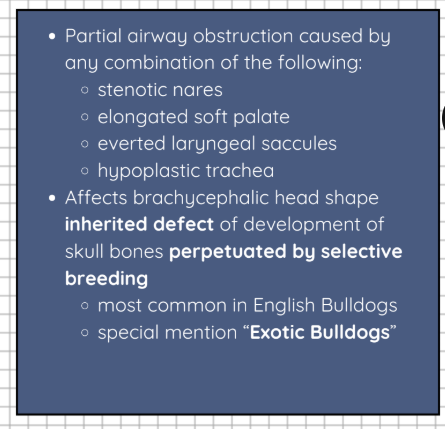
BOAS
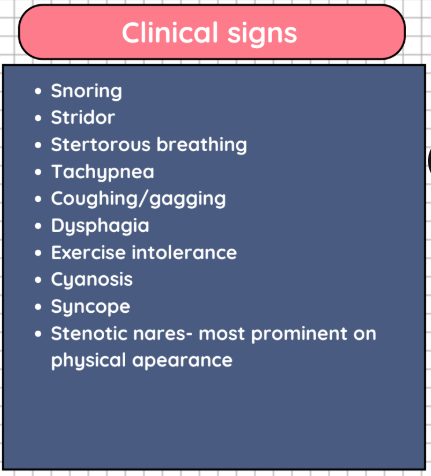
BOAS
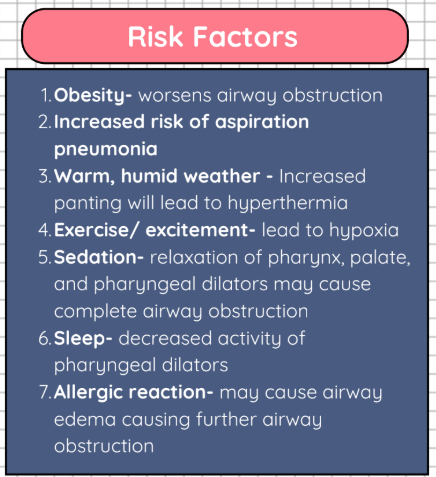
RISK FACTOR OF BOAS
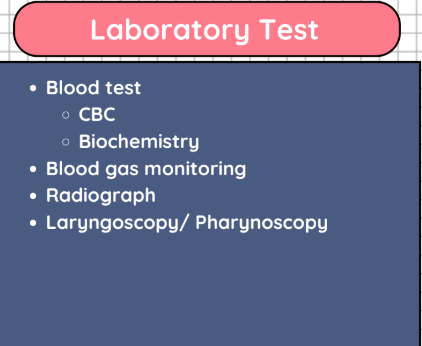
LAB TESTS FOR BOAS
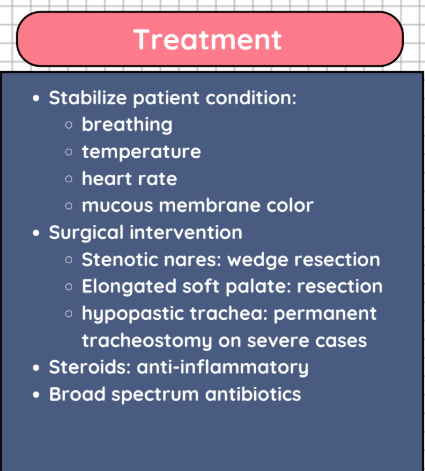
TX FOR BOAS
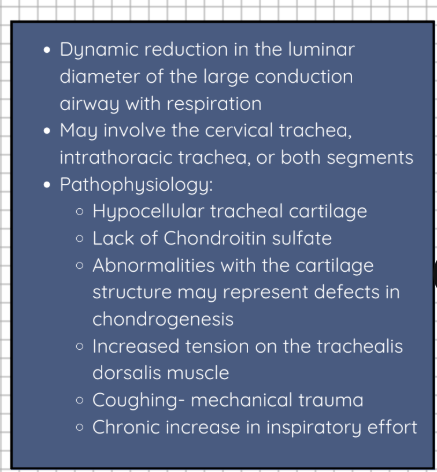
TRACHEAL COLLAPSE
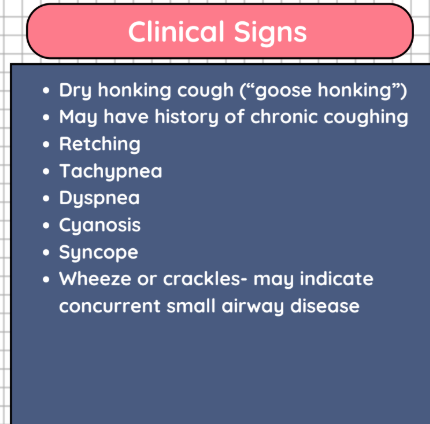
TRACHEAL COLLAPSE
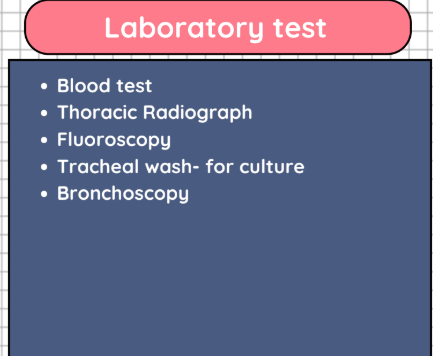
LAB TESTS FOR TRACHEAL COLLAPSE
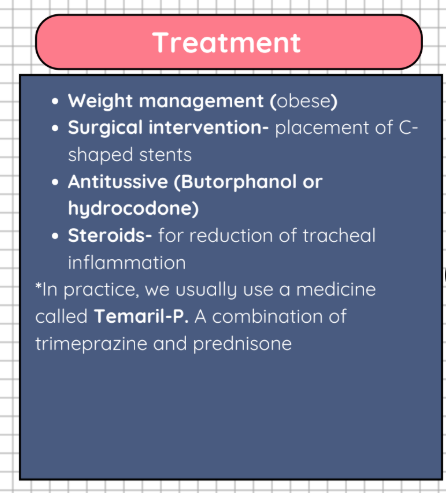
TX FOR TRACHEAL COLLAPSE
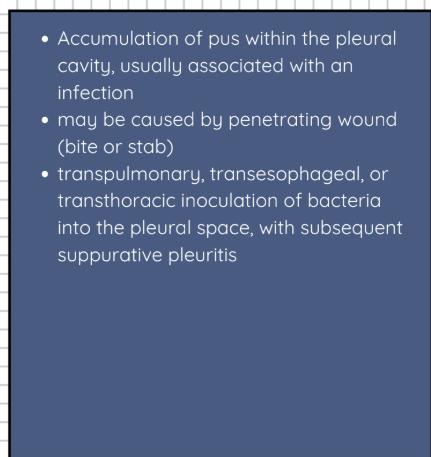
PYOTHORAX
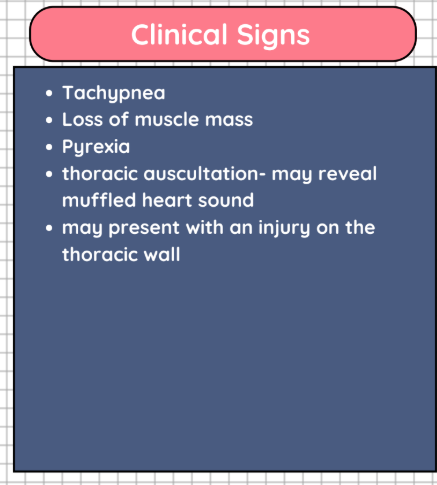
pyothorax
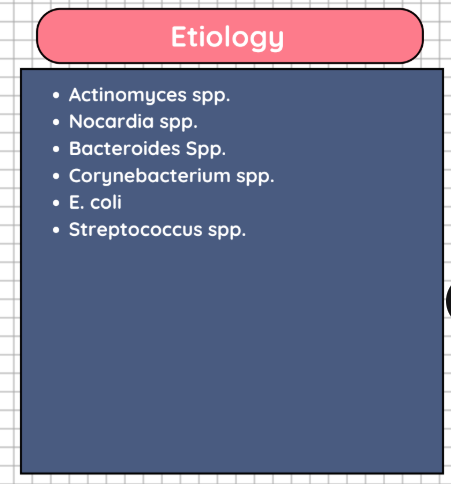
Etiology of Pyothorax
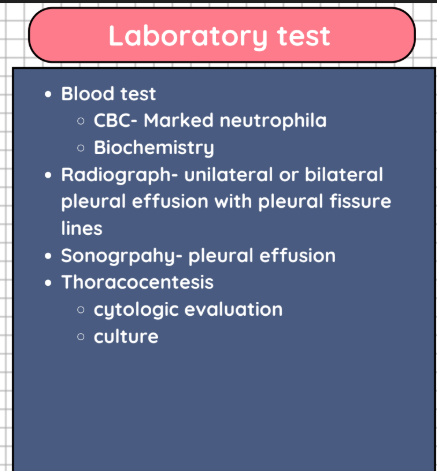
Lab tests for pyothorax
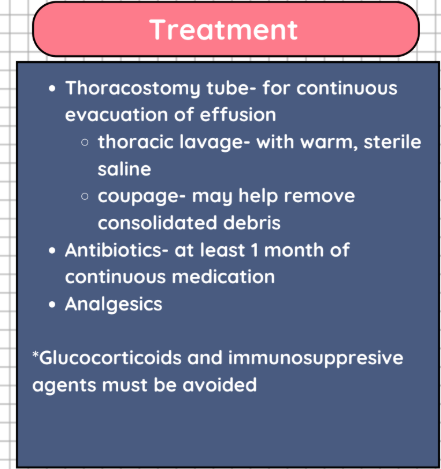
Tx for pyothorax
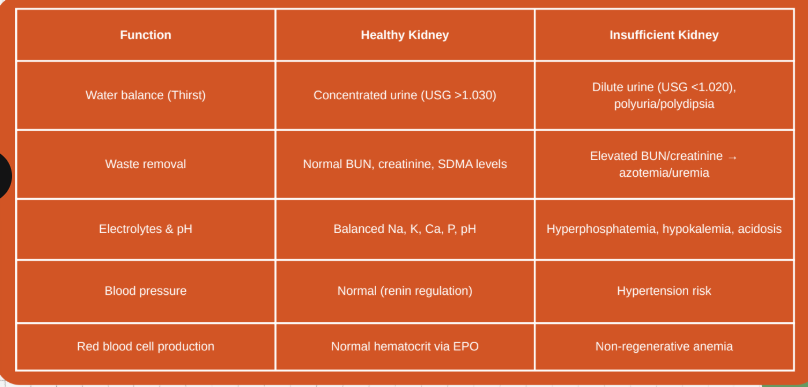
Functions of the Kidneys
Waste Removal
Fluid and Electrolyte Balance
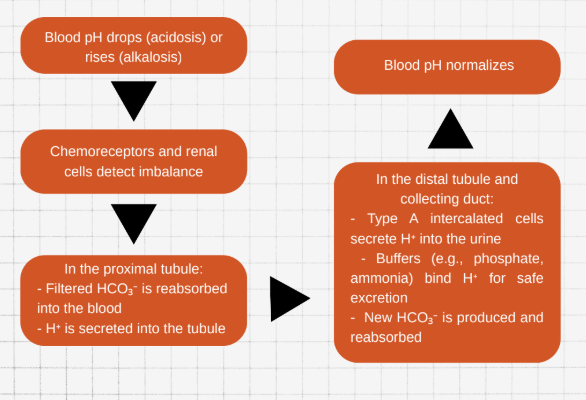
Acid Base Balance
Hormone Production
Blood Pressure Monitoring
Conversion of Vit. D to its active
form
Waste Removal & Fluid and Electrolyte Balance
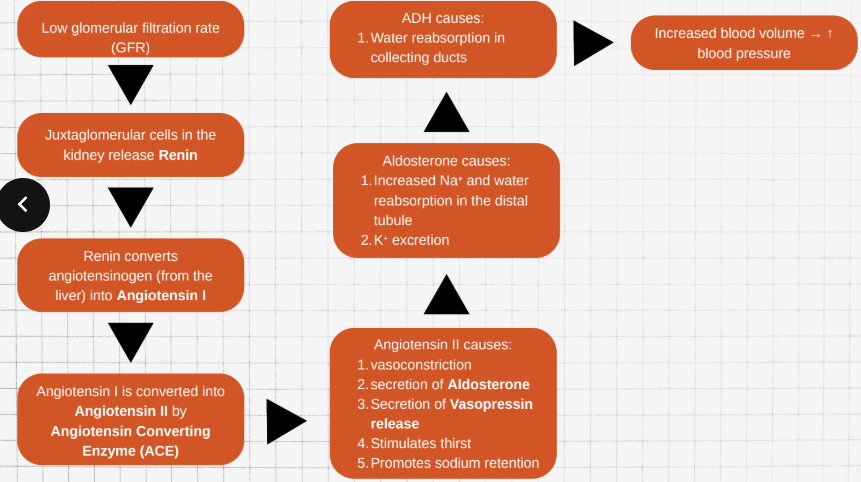
Blood Pressure Monitoring
Acide Base Balance
Source of EPO
Peritubular interstitial cells
(mainly in the renal cortex)
Stimulates bone marrow to produce red blood cells in response to hypoxia
EPO
Source of Renin
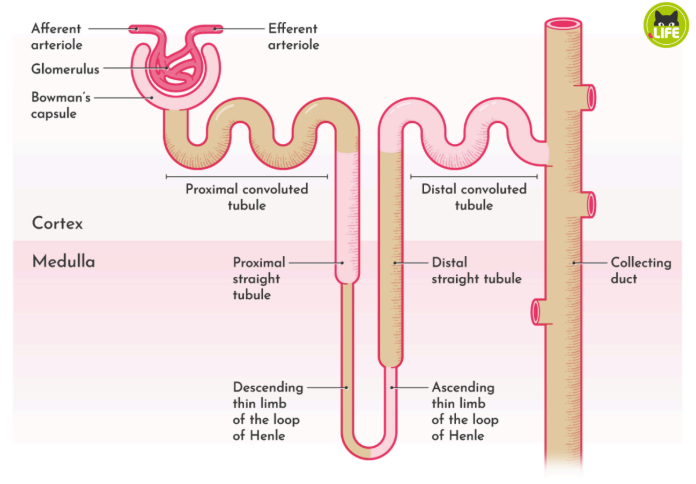
Juxtaglomerular (JG) cells
(afferent arteriole)
Triggers RAAS to increase blood
pressure and conserve
sodium/water
Renin
Source of Calcitriol (active vitamin D3)
Proximal tubule (via 1α-
hydroxylase enzyme)
Increases calcium and
phosphate absorption from gut,
reabsorption from kidneys;
regulates bone mineralization
Calcitriol (active vitamin D3)
Laboratory Tests
Urine Specific Gravity
Protenuria
Creatinine
UPC
SDMA
to help evaluate renal function by assessing whether water is being excrete or conserved appropriately, according to need.
It is measured using a __________
Dogs:______________ (It is important to note that any USG value could be
considered 'normal' in a patient, depending on certain other factors, including the patient's _______ status)
Specific gravity
refractometer
1.015 - 1.045
hydration
Adequately concentrated urine
Kidneys can concentrate → Likely pre-renal
cause (e.g., dehydration) if azotemic
> 1.030
Minimally concentrated
May indicate early CKD if persistent and
azotemia is present
1.013–1.029
Isosthenuria (same as blood plasma)
Suggests renal azotemia or loss of
concentrating ability
1.008–1.012
Hyposthenuria
Indicates active dilution, seen in diabetes
insipidus, psychogenic polydipsia, or early
CKD
<1.008
The presence of protein in the urine
The urine of healthy dogs and cats contains only a small amount of ___________ and other proteins
Persistent proteinuria with an inactive urine sediment is a marker of __________ in dogs and cats
2 major mechanisms:
Loss of selective glomerular filtration- resulting in an increased amount of plasma protein in the filtrate
Impaired tubular resorption of the filtered protein.
Proteinuria
albumin (< 1 mg/dl)
chronic kidney disease (CKD)
Non-proteinuric (NP)
Normal — no significant protein loss in urine
< 0.2
Borderline proteinuric (BP)
Monitor — may be early or transient; consider
rechecking
0.2 – 0.5
Proteinuric (P)
Abnormal — suggests glomerular or tubular
dysfunction; requires further evaluation and
often treatment
> 0.5
A metabolic byproduct of muscle breakdown, excreted almost entirely by the kidneys. It is a traditional marker of renal function used to estimate the glomerular filtration rate (GFR)
Limitations:
Affected by ________
not sensitive to _________
Creatinine
muscle mass
early kidney diseases
___________ or “SDMA”
A methylated form of the amino acid arginine, produced by all nucleated cells and primarily excreted by the kidneys.
SDMA increases on average with______ and as little as _____ loss of kidney function versus___, which does not increase until up to 75% of kidney function is lost
Symmetric Dimethylarginine
40%
25%
creatinine
Detects early CKD
SDMA
Affected by muscle mass
Creatinine
Rises only after 75% GFR lost
Creatinine but SDMA rises at 40% GFR loss
Used for IRIS staging
Crea is primary, SDMA is supplementary
A rapid and significant loss of renal function, leading to the accumulation of nitrogenous waste products, fluid imbalance and electrolyte disturbances (classically, ______)
Reflects a wide range of parenchymal damage, from mild, hardly detectable nephron injury to severe, life-threatening failure of the kidneys
3 causes:
Pre-renal: occurs when there is ________ to the kidney. This can be caused by severe hypotension, shock, and general anaesthesia.
Renal: results from _____ to any part of the kidney itself. (i.e. toxins, medications and/or infection)
Post Renal: occurs due to __________. In these cases the obstruction puts pressure on the kidneys, reducing glomerular filtration and causing __________
AKI
hyperkalaemia
reduced blood flow
injury
urinary tract obstruction
azotaemia
Causes Pre-renal ds:
hypovolemia
hypotension
decreased cardiac output
systemic vasodilation
Causes of renal ds:
toxins
ischemia
infection
glomerulonephritis
immune mediated disease
Causes of post renal ds:
Obstruction (urolithiasis, prostatic hyperplasia, tumor/neoplasia)
Non-azotemic but ↑ SDMA, abnormal urine,
imaging, or renal biomarkers (e.g. proteinuria,
casts)
Grade 0 - normal
Clinical signs suggest AKI (e.g., PU/PD,
inappropriate USG, elevated SDMA)
Grade I - <1.4 (non-azotemic)
Mild azotemia, stable or worsening
Grade II - 1.4–2.0
Moderate azotemia
Grade III - 2.1–5.0
Severe azotemia
Grade IV - 5.1–10.0
Clinical Signs of AKI:
Polyuria
Polydipsia
Lethargy
Depressed mentation
Hyporexia/ Anorexia
*Oliguria (urine output <0.5ml/kg/hour)
Stranguria
Anuria
AKI in cases of UT obstruction
Vomiting (the vomited material may have blood in it)
Diarrhea (that may contain blood)
A strange breath odor
Ulcers in the mouth
Seizure
Lab tests for AKI
Blood test
CBC
Biochem: Comprehensive or Kidney specific profiling + SDMA
hyperkalemia is a common finding
decreased potassium excretion
metabolic acidosis
cell lysis: damaged cells release intracellular potassium
Urinalysis
USG (Usually < 1.030)
UPC
Radiograph
Sonograph (Check renal structure)
Treatment for AKI
IV fluid- Appropriate fluid therapy is probably the cornerstone of the medical therapy of AKI, and it aims at restoring hydration and normovolemia.
Manage Hyperkalemia (i.e decreased renal excretion, oliguria/anuria, cell lysis, and/ or metabolic acidosis)
Correction of fluids
Insulin + Glucose: promoting the movement of potassium from the extracellular fluid (blood) into the intracellular space (inside cells)
Sodium Bicarbonate
Antibiotics- if with infection or secondary infection is expected
Supportive medication (renal probiotics, supplements, etc.)
Erythropoietin- If anemia is present
Dialysis- process of externally removing toxins and accumulated waste products from the bloodstream when the kidneys stop functioning
hemodialysis
peritoneal dialysis
Also known as renal failure and chronic kidney insufficiency
Progressive, irreversible loss of kidney function over weeks to months
Inability of the kidneys to efficiently filter the blood of waste products
Risk factors:
Age
Breed
Diet (high protein levels)
Certain medications
AKI
Concurrent diseases (i.e Hypercalcemia, periodontal ds, Cardiac ds., etc.)
Urine always in an isothenuric state (that is why urine of patients with CKD may always appear diluted) having a fixed specific gravity (1.008-1.0012)
kidneys unable to concentrate or dilute urine
occurs due to:
loss of nephron
tubular damages
CKD
Clinical signs of CKD
Polyuria
Polydipsia
Lethargy
Weakness
Dehydration
Anorexia/inappetence
Weight loss
Poor coat quality
Vomting
Marked weight loss
Uremic breath
Neurologic signs
Laboratory Tests for CKD
Blood tests
CBC- Anemia is a common finding
Biochem- Comprehensive or Kidney specific profiling + SDMA
Urinalysis
low USG
Proteinuria
Blood pressure monitoring
Hypertension
Radiograph
Sonograph
IRIS recommends confirming the stage with at least ______ fasting samples taken 2–4 weeks apart.
2
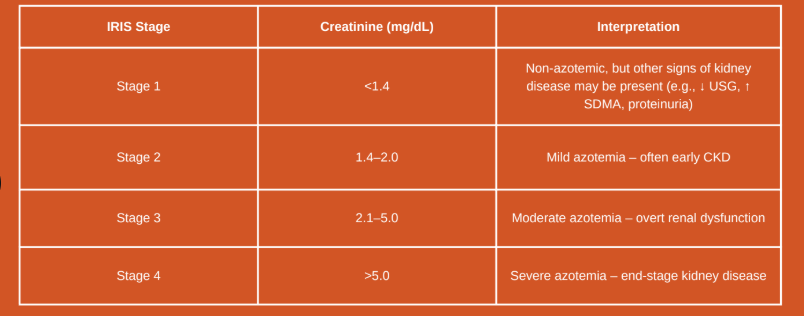
Creatinne
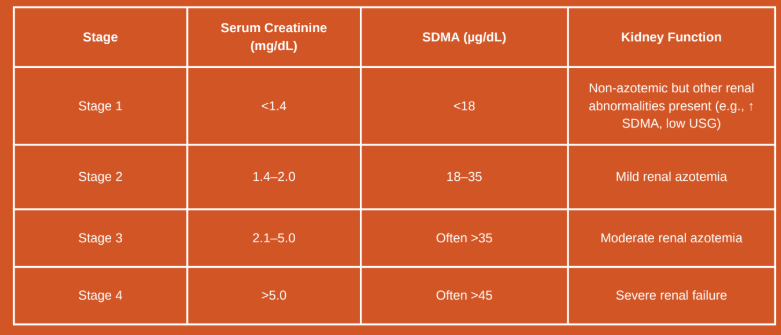
Stage 1(Creatinine
<1.4 mg/dL)
Stage 2 (Creatinine 1.4–2.0 mg/dL)
Stage 3 (Creatinine 2.1–5.0 mg/dL)
Stage 4 (Creatinine >5.0 mg/dL)
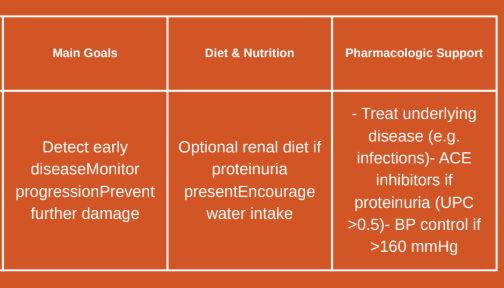
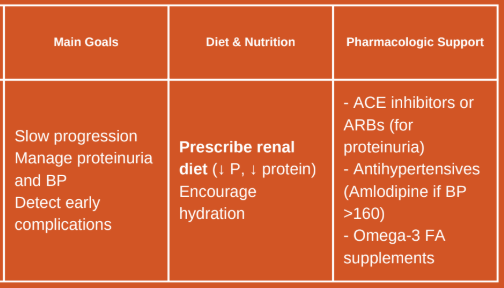
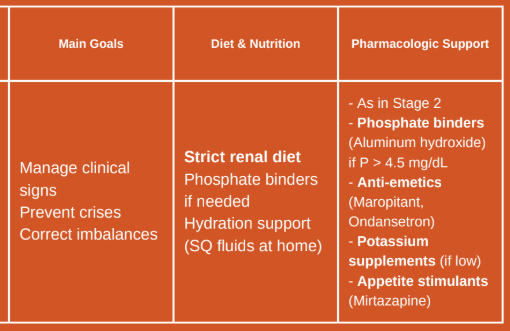
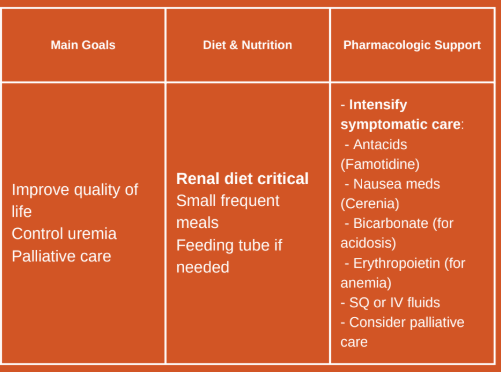
CKD Treatment
Treatment summary:
1.Diet- management- Low in phosphorus and protein
2.Control proteinuria- ACE inhibitors
3.Manage hypertension- add Amlodipine if ACE inhibitor is not enough
4.Phosphorus control- add phosphate binders
5.Hydration support- IVF, SQF, encourage drinking
6.Symptomatic care- antiemetics, potassium supplements, erythropoietin, etc.
7.Regular monitoring- usually done every month