Meg/Surg: CJMM, Pain, sleep, infection, fluids/electrolytes
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
64 Terms
acute pain
define
results from
characteristics
results from
The unpleasant sensory and emotional experience associated with tissue damage that results from acute injury, disease, or surgery.
Acute pain often results from sudden, accidental trauma (e.g., fractures, burns, lacerations) or from surgery, ischemia, or acute inflammation.
characteristics:
• Has short duration
• Usually has a well-defined cause
• Decreases with healing
• Is usually reversible
• Initially serves a biologic purpose (warning sign to withdraw from painful stimuli or seek help)
• When prolonged, serves no useful purpose
• Ranges from mild to severe intensity
• May be accompanied by anxiety and restlessness
• When unrelieved, can increase morbidity and mortality and prolong length of hospital stay
breakthrough pain
Additional pain that “breaks through” the pain being managed by the mainstay analgesic drugs
neuropathic pain
The result of abnormal processing of stimuli believed to be associated with damage to or dysfunction of the parasympathetic nervous system (PNS) and/or central nervous system (CNS).
nociceptive pain
The result of actual or potential tissue damage or inflammation; often categorized as being somatic or visceral.
pain
An unpleasant sensory and emotional experience associated with actual or potential tissue damage. The most reliable indication of pain is the patient’s self-report.
self-report is always the most reliable indication of pain
persistent/chronic pain
define
characteristics
Pain that persists or recurs for an indefinite period, usually for more than 3 months. It often involves deep body structures, is poorly localized, and is difficult to describe.
characteristics:
• Usually lasts longer than 3 months
• May or may not have well-defined cause
• Usually begins gradually and persists
• Serves no useful purpose
• Ranges from mild to severe intensity
• Often accompanied by multiple quality-of-life and functional adverse effects, including depression; fatigue; financial burden; and increased dependence on family, friends, and the health care system
• Can impact the quality of life of family members and friends
patient-controlled analgesia (PCA)
An interactive method of management that allows patients to treat their pain by self-administering doses of analgesics
placebo
Any medication or procedure, including surgery, that produces an effect in a patient because of its implicit or explicit intent, not because of its specific physical or chemical properties.
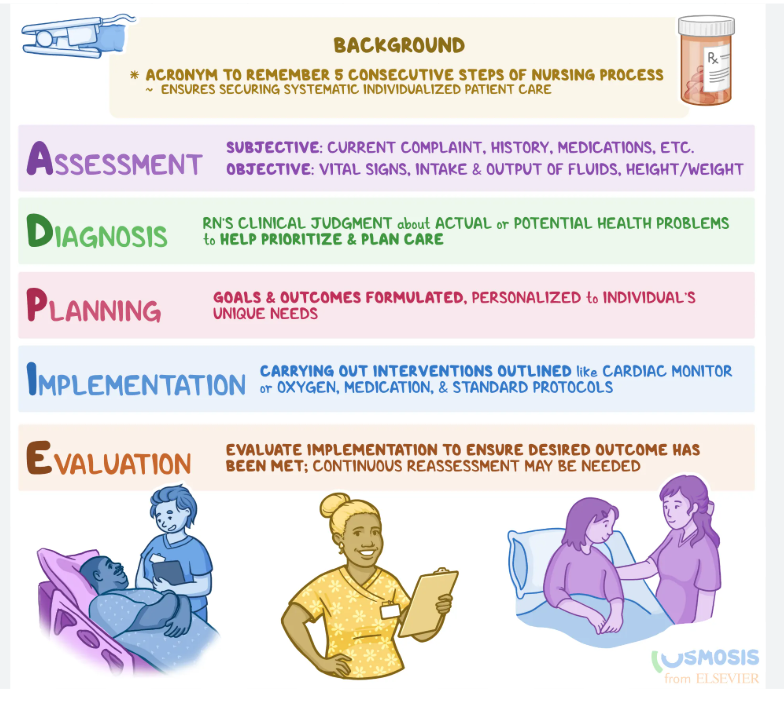
ADPIE Nursing process
Assessment
Diagnosis
Planning
Implementation
Evaluation
what SBAR
what information goes with each step
Situation:
identify self & site/unit person calling from
Identifying individual (Name + DOB)
Symptom onset & severity
Background:
Date/time of admission
Admitting diagnosis
relevant medical history
Lab/diagnostic results
notable changes
assessment finding: vitals
Assessment:
suspected underlying cause or concerns
Recommendation:
clear/specific about urgency or request & expected time frame

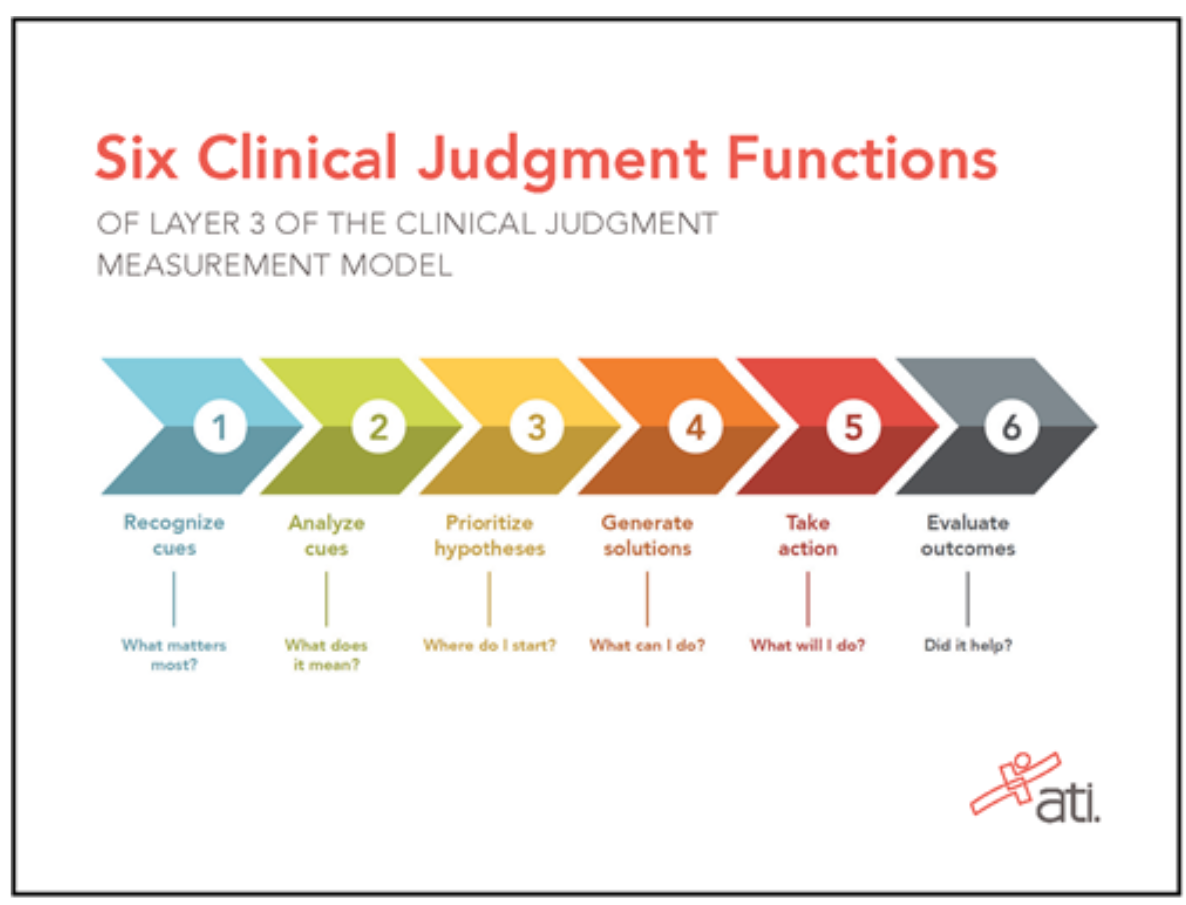
Model of Clinical Judgment
Recognize Cues: Assessment
what matters most (assessment findings, patient statements, labs, vitals)
Analyze Cues: Analysis
What does this mean (Make sense of the data. Look for patterns, decide what’s normal vs. abnormal, and connect the dots)
Prioritize Hypotheses: Analysis
Where do I start (Sorting the “possible problems” into most likely/most dangerous vs. less likely/less urgent)
Generate Solutions: Planning
What can I do
Take Actions: Implementation
What will I do
Evaluate Outcomes: Evaluation
Did it help
concept: infection
Defined
Categories of Infection
Sepsis
Common Risk Factors for Infection
Physiologic Consequences of Infection:
Localized infection:
systemic infection:
Assessment of Infection
Health Promotion Strategies to Prevent Infection
Interventions to Manage Patients With Infection
Defined:
the invasion of pathogens (harmful microbes) into the body that multiply and cause disease or illness. The primary interrelated concepts are pain, immunity, inflammation, and tissue integrity.
Classification of Infection:
an be classified by type of microorganism, by extent of its spread throughout the body, or by the length of time that the infection exists, acute or chronic, localized (one area) or systemic (whole body, can lead to sepsis).
• Bacteria
• Viruses
• Fungi
• Parasites or protozoa
Sepsis:
is a life-threatening condition that occurs when the body's immune system overreacts to an infection, leading to widespread inflammation and organ damage
Common Risk Factors for Infection:
• immunocompromised individuals
• Have chronic illnesses (comorbidities)
• Are of advanced age: because immune function declines as part of normal aging
• Are very overweight or obese
• Live in a crowded or unsanitary environment
• Ingest contaminated food or water
• Have impaired tissue integrity: (causing an interruption in the body’s first line of defense against infection)
• Are exposed to individuals who have highly contagious infections: such as influenza or tuberculosis
• Experience continuous or frequent stress
Physiologic Consequences of Infection:
depend on whether it is localized or systemic.
Localized infection:
typically causes inflammation: Signs and symptoms of inflammation include redness/hyperpigmentation, warmth, pain, and swelling.
If localized infection is not treated or does not respond to treatment, it may spread and affect the entire body, causing a systemic infection
systemic infection:
affects the entire body, the response of the body is also systemic.
fever and an increased white blood cell count (WBC), also known as leukocytosis.
If the infection is not treated or does not respond to treatment, the patient may become septic and experience decreased perfusion, causing hypotension and eventually organ failure (septic shock).
Assessment of Infection:
take a thorough history to determine the patient’s risk for and exposure to infection.
Observe for signs and symptoms of local infection if visible, such as redness/hyperpigmentation, warmth, pain, and swelling.
Elevated temperature may be present in patients who have systemic infection.
Ask about changes in elimination, including urinary burning and urgency, diarrhea, and nausea/vomiting. These changes may be indications of urinary or GI system infection.
Monitor laboratory test results, including:
Elevated WBC count with differential (especially lymphocytes and neutrophils)
Increased erythrocyte sedimentation rate (ESR)
Increased C-reactive protein
Positive culture and sensitivity
Positive antigen testing for infectious agents
Health Promotion Strategies to Prevent Infection:
Health promotion related to infection may be categorized as primary and secondary prevention
Primary prevention includes measures to prevent infection, such as immunizations against common illnesses and boosters as needed
Secondary prevention involves screening for existing infection, such as when sexually transmitted infections (STIs) are suspected or the patient is at a high risk for STIs
Interventions to Manage Patients With Infection:
if infection not able to be self treated at home with rest fluids and OTC drugs:
• Antimicrobial drug therapy (type depends on type of pathogen)
• Increased fluids and electrolyte replacement
• Sufficient rest
• Adequate nutrition
concept: Pain
Definition of Pain
Categories of Pain
Common Risk Factors for Pain
Physiologic and Psychosocial Consequences of Pain
Assessment of Pain
Health Promotion Strategies to Prevent Pain
Interventions to Manage Patients With Pain
Patient education
Definition of Pain
Pain is generally defined as an unpleasant sensory and emotional experience.
Because pain is a subjective symptom, nurses and other health care professionals must respect the patient’s description of pain.
Categories of Pain
Pain can be categorized by duration as acute or persistent (chronic).
Acute pain is short-lived, temporary, and typically confined to an injured area of the body (localized). It serves a biologic purpose to activate the sympathetic nervous system and other physiologic responses.
Persistent (chronic) pain does not serve this purpose and tends to last more than 3 months. It is often described as diffuse and not confined to one area of the body. The two major types of persistent pain are persistent cancer pain and persistent noncancer pain
Pain can also be categorized by its underlying mechanism into nociceptive and neuropathic pain.
Nociceptive pain results from skin or organ damage or inflammation.
Neuropathic pain involves a set of mechanisms related to the nervous system with or without tissue damage
Common Risk Factors for Pain
Anyone is at risk for pain, and many adults have experienced one or more types of pain sometime in their lives.
Specific risk factors include individuals who experience acute trauma or have chronic diseases
Physiologic and Psychosocial Consequences of Pain
Patients experiencing acute pain usually have one or more sympathetic nervous system signs and symptoms including nausea, vomiting, diaphoresis (sweating), increased blood pressure, increased respiratory rate, increased pulse, and dilated pupils. Fight or flight!!!
This “flight or fight” reaction does not occur in patients with persistent pain. Persistent pain can cause psychosocial issues, including anxiety and depression.
Assessment of Pain: PQRST
P: what makes the pain worse and better
Q: describe the pain
R: where is the pain or point to the pain and does it spread
S: on a scale from 0-10 (0 being no pain, 10 being the worst pain imaginable)
T: How long does the pain last and low long they have been experiencing it
Health Promotion Strategies to Prevent Pain
Acute pain is often unavoidable.
Avoiding high-risk activities can help prevent trauma from accidental injury and thus prevent severe acute pain.
After surgery or a trauma event, acute pain must be well controlled to prevent persistent pain that may last for months or years.
Interventions to Manage Patients With Pain
Nursing and collaborative management of pain may be categorized by pharmacologic and nonpharmacologic interventions.
Evidence-based pharmacologic interventions involve a variety of analgesics and are determined on the basis of severity, type, and source of pain.
Analgesics may be divided into nonopioid drugs and opioid drugs.
Nonopioid drugs may be used without concern related to abuse or addiction; however, they have side and adverse effects that require careful monitoring.
Patient education
teach patients to take drug therapy for persistent pain on a continuous regimen basis for the best control.
Persistent cancer pain often requires opioids at the end of life to provide comfort and prepare for a “good death.”
Nonpharmacologic patient-centered interventions depend on the patient’s preferences.
Impact of Unrelieved Pain
Physiologic Impact- 7
Quality-of-Life Impact- 3
Financial Impact- 3
Physiologic Impact:
• Prolongs stress response
• Increases heart rate, blood pressure, and oxygen demand
• Decreases GI motility
• Causes immobility
• Decreases immune response
• Delays healing
• Increases risk for development of chronic pain
Quality-of-Life Impact:
• Interferes with ADLs
• Causes anxiety, depression, hopelessness, fear, anger, and sleeplessness
• Impairs family, work, and social relationships
Financial Impact:
• Billions of dollars per year due to:
• Increased length of hospital stay
• Lost income and productivity
Cancer Pain
what’s common
treatment
causes acute and chronic
common at diagnosis, worse in advanced stages
Treatment: usually controlled with oral opioids, but often undertreated
Causes (persistent pain):
Tumor growth
Nerve compression
Tissue invasion
Bone metastasis (very painful)
Causes (acute pain):
Procedures (e.g., blood draws)
Surgery
Chemo & radiation side effects
Procedural pain
linked to
poor control leads to
risk
linked to medical/surgical procedures, usually acute
Poor control leads to:
Worse patient outcomes
Higher readmission rates
Patient dissatisfaction
Increased health care costs
Risk:
chronification of pain: untreated acute pain → chronic pain
Nociceptive pain
defined
characteristics
treatment
results from actually or potential skin or organ damage or inflammation.
involves the normal functioning of physiologic systems that process noxious stimuli, with the ultimate result being that the stimuli are perceived to be painful.
characteristics:
somatic pain
visceral pain
treatment: CBT, distraction, imagery can alter perception
Nociceptive pain process
steps
Four overlapping steps: transduction → transmission → perception → modulation.
Transduction is the first process of nociception and refers to the ways that noxious events activate neurons that exist throughout the body (in skin, subcutaneous tissue, and visceral [or somatic] structures) and have the ability to respond selectively to specific noxious stimuli.
Transmission: signals travel via fibers → CNS
A-delta: fast, sharp, localized
C fibers: slow, aching/burning, diffuse, continuous
Perception: conscious awareness of pain → emotions + cognition involved
Modulation: regulates pain signals (not detailed here but part of process)
Neuropathic Pain
defined
characteristics
involves a set of mechanisms related to the nervous system with or without tissue damage
is sustained by the abnormal processing of stimuli.
characteristics:
“burning,” “shooting,” “tingling,” and “feeling pins and needles.”
Physiologic Sources of Nociceptive Pain
Physiologic Structure
Characteristics of Pain
Sources of Acute Postoperative Pain
Sources of Chronic Pain Syndromes
Somatic Pain:
Cutaneous or superficial: skin and subcutaneous tissues
Deep somatic: bone, muscle, blood vessels, connective tissues
Visceral Pain
Physiologic Sources of Neuropathic Pain
Physiologic Structure
Characteristics of Pain
Sources of Acute Postoperative Pain
Sources of Chronic Pain Syndromes
Peripheral or central nervous system: nerve fibers, spinal cord, and higher central nervous system
Poorly localized, Shooting, burning, fiery, shock like, tingling, painful numbness
Phantom limb pain, postmastectomy pain, nerve compression
HIV-related pain, diabetic neuropathy, postherpetic neuralgia, chemotherapy-induced neuropathies, cancer-related nerve injury, radiculopathies
Cutaneous or superficial pain
Physiologic Structure
Characteristics of Pain
Sources of Acute Postoperative Pain
Sources of Chronic Pain Syndromes
skin and subcutaneous tissues
Well localized, Sharp, throbbing
Incisional pain, pain at insertion sites of tubes and drains, wound complications, orthopedic procedures, skeletal muscle spasms
Bony metastases, osteoarthritis and rheumatoid arthritis, low back pain, peripheral vascular diseases
Deep somatic pain
Physiologic Structure
Characteristics of Pain
Sources of Acute Postoperative Pain
Sources of Chronic Pain Syndromes
bone, muscle, blood vessels, connective tissues
Dull, aching, cramping
Same as Cutaneous or superficial:
Same as Cutaneous or superficial:
Visceral Pain
Physiologic Structure
Characteristics of Pain
Sources of Acute Postoperative Pain
Sources of Chronic Pain Syndromes
Organs and the linings of the body cavities
Poorly localized, Diffuse, deep cramping or pressure, sharp, stabbing
Chest tubes, abdominal tubes and drains, bladder distention or spasms, intestinal distention
Pancreatitis, liver metastases, colitis, appendicitis
Preemptive analgesia
involves the administration of local anesthetics, opioids, and other drugs (multimodal analgesia) in anticipation of pain along the continuum of care during the preoperative, intraoperative, and postoperative periods.
designed to decrease pain severity in the postoperative period, reduce analgesic dose requirements, prevent morbidity, shorten hospital stay, and avoid complications after discharge.
What is the best route for analgesic administration
The oral route is the preferred route of analgesic administration.
Why:
the least expensive, best tolerated, easiest to administer, and replicable at home once the patient is discharged.
patient-controlled analgesia (PCA)
defined
pt education
An interactive method of management that allows patients to treat their pain by self-administering doses of analgesics.
ACTION ALERT:
Teach patients how to use the PCA device and to report side effects such as dizziness, nausea and vomiting, and excessive sedation.
Around-the-Clock Dosing (ATC)
purpose/use
goals
designed to control pain for patients who report it being present for 12 hours or more during a 24-hour period
(1) preventing pain
(2) maintaining a level of pain control that allows the patient to function and have an acceptable quality of life.
PRN
defined
purpose/use
for intermittent pain
such as before painful procedures, and breakthrough pain
with all opioids, monitor the patient’s..
sedation level and respiratory status at least every 2 hours. Promptly decrease the opioid dose (i.e., discontinue basal rate) if increased sedation is detected.
Acetaminophen vs NSAIDS
Acetaminophen
relieve pain by underlying mechanisms in the CNS. It has analgesic and antipyretic properties but is not effective for treating inflammation.
NSAIDs
analgesic, antipyretic, and anti-inflammatory properties. These drugs produce pain relief by blocking prostaglandins through inhibition of the enzyme cyclooxygenase (COX) in the peripheral nervous system
Opioid Analgesics
used for
function
unwanted effects
what to be aware of
the main management of moderate to severe nociceptive types of pain
produce their effects by interacting with opioid receptor sites located throughout the body, including in the peripheral tissues, the GI system, and the spinal cord and brain. When an opioid binds to the opioid receptor sites, it produces analgesia
unwanted effects such as constipation, nausea, sedation, and respiratory depression.
be aware of:
can cause Physical dependence: occurs with repeated administration of an opioid for several days.
can cause Tolerance: is also a response that occurs with regular administration of an opioid and consists of a decrease in one or more effects of the opioid (e.g., decreased analgesia, sedation, or respiratory depression)
can cause Opioid addiction is a treatable chronic neurologic and biologic disease. causes impaired control over drug use, compulsive use, continued use despite risk or actual harm, and craving.
Pseudoaddiction: can be a mistaken diagnosis of addictive disease. When a patient’s pain is not well controlled, the patient may begin to manifest symptoms suggestive of addictive disease
Opioid Antagonists
function
purpose
examples
Block mu and kappa receptors → no pain relief.
Reverse opioid effects (respiratory depression, sedation).
Examples: naloxone (NARCAN), naltrexone.
Key Principles of Opioid Administration
Individualize choice
Titrate dose: cancer pain, acute/post-op pain
goal
Which type of opioid has no ceiling effect, what does this mean
Timing based on
IV opioids doses can be increased every
How long to wait before changing a Transdermal fentanyl dose
range orders?
Individualized Choice – Consider type/intensity of pain, age, comorbidities, other meds, and patient preference.
Titration – Adjust dose up or down based on pain relief and side effects.
Cancer pain → usually titrate upward.
Acute/post-op pain → titrate downward as pain improves.
Goal: smallest effective dose with least side effects.
No Ceiling for Pure Agonists – Doses can keep increasing for more relief, but side effects may limit how much is given.
Timing Matters – Dose adjustments depend on drug onset/peak.
IV opioids: can increase every 5–15 min.
Transdermal fentanyl: wait 24 hrs before changing dose.
Range orders– Providers may order a dose range (e.g., morphine 2–5 mg IV q2h PRN). Nurse uses clinical judgment and pain assessment to pick the right dose within the range
Medical Marijuana (Cannabis)
uses
side effects
persistent and neuropathic pain,
increased heart rate, increased appetite, dizziness, decreased blood pressure, dry mouth, hallucination, paranoia, altered psychomotor function, and impaired attention
Local Anesthetics
relieve pain by blocking the generation and conduction of the nerve impulses necessary to transmit pain.
non-drug things that can help with pain
• Application of heat, cold, or pressure
• Therapeutic massage
• Vibration
• Transcutaneous electrical nerve stimulation (TENS)
• Physical therapy
• Occupational therapy
• Aquatherapy
• Functional restoration (also has cognitive-behavioral components)
• Acupuncture
• Low-impact exercise programs such as slow walking and yoga
common side effects of analgesics
sedation
constipation
Nausea
vomiting
respitory distress
Opioid naïve versus opioid tolerant
opioid-naïve:
person has not recently taken enough opioid on a regular basis to become tolerant to the effects of an opioid.
opioid-tolerant:
person has taken an opioid long enough at doses high enough to develop tolerance to many of the effects including analgesia and the undesirable effects such as nausea and sedation.
There is no set time for the development of tolerance, with wide individual variation among
people. - -Some patients do not develop tolerance at all.
Equianalgesia
means approximately “equal analgesia.”
An equianalgesic chart provides a list of analgesic doses, both oral and parenteral (IV, subcutaneous, and IM), that are approximately equal to one another in ability to provide pain relief.
short acting, fast acting, immediate release (IR), and normal release
vs.
extended release (ER), sustained release (SR), and controlled release (CR)
vs
long acting
to describe oral opioids that have an onset of action of about 30 minutes and a relatively short duration of 3 to 4 hours. Oral transmucosal and intranasal formulations are referred to as ultrafast acting because they have a peak effect of 5 to 15 minutes, depending on formulation.
to describe opioids that are formulated to release over a prolonged period of time
should never be crushed, broken, or chewed
long acting: applied to drugs with a long half-life such as methadone.
Oxycodone:
Oral only.
Alone or combined with acetaminophen/ibuprofen.
Used for mild → severe pain; also part of multimodal post-op plans.
Liquid form available.
Dual Mechanism Analgesics
function
Tramadol & Tapentadol
route
used for
risks
Mechanism: Weak mu-opioid receptor binding + block reuptake of serotonin/norepinephrine → more neurotransmitters available to reduce pain.
Tramadol:
Oral (short-acting, ER, or with acetaminophen).
Used for acute & chronic pain; 2nd-line for neuropathic pain.
Risks: lowers seizure threshold, can interact with SSRIs → risk of serotonin syndrome (agitation, diarrhea, BP/HR changes, loss of coordination).
Tapentadol:
Oral (short-acting, ER).
Used for acute & chronic pain.
Benefits: no active metabolites, fewer GI side effects than opioids.
Intraspinal Analgesia
epidural
Intrathecal (Spinal)
intrathecal pumps
side effects
nursing role
Routes: Epidural (needle/catheter in epidural space) or Intrathecal (into CSF). Used for acute (post-op) and chronic pain.
Epidural
Delivery: bolus, continuous infusion, or patient-controlled (PCEA).
Common drugs: opioid (hydromorphone, fentanyl) + local anesthetic (bupivacaine, ropivacaine).
Benefit: multimodal → lower doses, fewer side effects.
Intrathecal (Spinal)
Usually single bolus for acute pain or continuous pump for chronic pain.
Morphine used most often (hydrophilic → small doses effective near spinal site).
Side Effects
Opioids: same as systemic (respiratory depression, N/V, itching, etc.).
Local anesthetics: urinary retention, hypotension, leg numbness/weakness. Severe block = emergency.
Complications rare but serious: infection, CSF leak, pump/catheter issues, hematoma/abscess → can cause paralysis.
Nursing Role
Frequent neuro + respiratory checks.
Manage infusion devices, refill reservoirs, monitor for side effects/complications.
Do not delegate neuro assessments.
Drug Alerts / Safety
For epidural local anesthetics: check ability to bend knees/lift buttocks, monitor numbness/tingling. Report inability to bear weight or severe hypotension.
For intrathecal pumps:
Monitor RR, O2 sat, LOC q1–2h for 12h post-op.
Binder to keep pump flat. No heat over pump site.
Teach: no lifting >5 lb, avoid twisting/bending for 6 weeks.
Watch for infection, CSF leak (headache/swelling), catheter problems, pump malfunction.
Never abruptly stop baclofen (→ resp depression) or clonidine (→ hypertension, stroke).
Nursing Interventions for Opioid Side Effects
Constipation
No tolerance → always prevent.
Assess habits; track BMs.
Stool softener + stimulant laxative (not bulk laxatives).
Encourage fluids, fiber, activity, privacy.
If unresolved → suppository, enema, or OIC meds (e.g., lubiprostone, methylnaltrexone).
Nausea/Vomiting
Use antiemetics (e.g., dexamethasone + ondansetron).
Identify and remove causes.
Reduce dose if possible.
Tolerance develops with long-term use.
Switch opioid if unresolved.
Sedation
Sedation comes before respiratory depression → monitor closely, especially first 24h.
Use sedation scale.
Lower dose if too sedated.
Avoid other sedating drugs if possible (antihistamines, muscle relaxants, etc.).
Tolerance develops with chronic use.
Caffeine/stimulants may help.
Switch opioid if unresolved.
Respiratory Depression
Don’t just count RR → check depth, quality, chest rise.
Snoring = obstruction → intervene immediately.
Stop opioid, stay with patient, support respirations, call for help.
Consider naloxone if severe.
Adverse Effects of Opioid Analgesics
Common: constipation, nausea, vomiting, itching, sedation.
Most feared: respiratory depression (less common).
Most side effects are dose-related → often improved by lowering dose.
Sedation & Respiratory Depression
Sedation happens early or after dose increases; if untreated → may progress to respiratory depression.
Prevention: lowest effective dose, multimodal analgesia, slow titration, close monitoring.
At-risk patients (e.g., sleep apnea, lung disease, comorbidities) may need capnography or pulse oximetry.
Reduce dose/stop titration if sedation increases (unless end-of-life care).
Drug Interactions
Many drugs used for side effects (antihistamines, antiemetics, anxiolytics) are sedating → additive effect. Monitor closely.
Assessment
Use sedation scale: focus on how easy the patient is to arouse.
Always assess response to first opioid dose and peak effect after bolus doses.
Adjuvant Analgesics
Drugs primarily used for other conditions (e.g., antidepressants) that also relieve pain.
Most diverse analgesic group.
Selection and dosing based on clinical experience and evidence-based guidelines.
Adjuvant Analgesics: Anticonvulsants & Antidepressants
Anticonvulsants (AEDs)
Mechanism: Block sodium & calcium channels → reduce pain transmission.
Common drugs: Gabapentin, Pregabalin (gabapentinoids) → mainly for neuropathic pain.
Side effects: Sedation, dizziness (often improve with time).
Pregabalin-specific: Euphoria → controlled substance; may cause weight gain, hypersensitivity (angioedema); caution with CNS depressants → risk of breathing problems.
Antidepressants
Mechanism: Block norepinephrine & serotonin reuptake in descending pain pathway.
Types:
TCAs (e.g., amitriptyline, nortriptyline) → persistent pain.
Side effects: dry mouth, sedation, dizziness, mental clouding, weight gain, constipation, orthostatic hypotension.
Serious: cardiotoxicity in patients with heart disease.
SNRIs (e.g., duloxetine) → persistent/neuropathic pain.
Better tolerated than TCAs.
Side effects: nausea, headache, sedation, insomnia, weight gain, impaired memory, sweating, tremors.
Local Anesthetics (LAs)
topical and patch therapy
Sustained-Release Local Anesthetics
Regional & Peripheral Nerve Blocks
Mechanism: Block nerve impulse generation/conduction → prevent pain transmission.
High dose → complete anesthesia
Low dose → analgesia
Safety: Allergy rare; side effects dose-related.
CNS toxicity: tinnitus, metallic taste, irritability, seizures
Cardiotoxicity: tingling, numbness, bradycardia, dysrhythmias, cardiovascular collapse
Topical & Patch Therapy
Lidocaine 5% patch: minimal systemic absorption, applied 12h on/12h off.
Topical creams: EMLA, lidocaine/prilocaine → slow onset (30–60 min).
Newer technique: liquid lidocaine via compressed gas → analgesia in 1–3 min.
Side effects rare; usually local skin reactions.
Sustained-Release Local Anesthetics
Liposomal bupivacaine: single-dose wound infiltration → prolonged analgesia, reduces opioid need.
Regional & Peripheral Nerve Blocks
Single-injection nerve block: targets specific nerve/plexus, lasts 4–12 h.
Continuous peripheral nerve block / PCRA: catheter + continuous infusion, may include PCA → longer-lasting analgesia.
Nurses monitor infusion, manage therapy, prevent complications (similar to epidural/intrathecal care).
Placebos
Definition: Any treatment (medication, procedure, or surgery) that produces an effect due to expectation, not its physical/chemical properties (e.g., saline injection, subtherapeutic dose).
Appropriate Use:
Research studies as a control.
Requires informed consent from patient or guardian.
Inappropriate Use:
Clinically, to deceive patients or dismiss their pain report.
Ethical/legal issues: violates nurse-patient trust, denies proper care, invalidates assessment/treatment.
Physical Modalities
Purpose: Reduce pain, improve function, aid recovery, often part of multimodal therapy.
Settings: Acute care, home, ambulatory care.
Common Methods:
Physical therapy, occupational therapy, aquatherapy, functional restoration, acupuncture, low-impact exercise (walking, yoga).
Cutaneous Stimulation:
Heat → increases blood flow (osteoarthritis)
Cold → reduces inflammation/swelling (RA, post-op)
Massage, vibration, topical gels/creams (cryotherapy)
Effects are short-term, patient can self-administer.
Electrical Stimulation:
TENS → battery-powered, electrodes on painful area, adjustable current for “pins-and-needles” sensation.
Spinal cord stimulation → invasive, for intractable neuropathic pain; trial first, permanent implant if successful; patient can adjust device.
Expected Outcomes: ↑ range of motion, strength, function; improved quality of life.
Cognitive-Behavioral Modalities
Purpose: Reduce focus on pain; do not block pain physiologically.
Simple Methods: Prayer, relaxation breathing, artwork, reading, watching TV.
Complex Methods: Mindfulness, meditation, guided imagery, hypnosis, biofeedback, virtual reality.
Distraction Techniques:
Visual (pictures, TV, video games)
Auditory (music, sounds)
Environmental adjustments (reduce noise/bright lights)
Guided Imagery: Requires concentration; patient visualizes pleasant thoughts/events to divert attention from pain.
Mindfulness: Focus on present environment, e.g., nature observation.
Relaxation Techniques:
Physical: Deep breathing, massage, warm bath, comfortable positioning
Psychological: Music, humor, pleasant conversation, relaxation recordings
Aromatherapy: Essential oils (lavender, peppermint, eucalyptus) → reduce postoperative pain via smell.
Normal Sleep
Normal sleep patterns involve uninterrupted breathing and cycling through various sleep stages, allowing for proper rest and physiological restoration.
OSA
- Partial or complete upper airway obstruction during sleep
-Recurring apneic episodes lasting 10 seconds or longer
-Intermittent hypoxia and hypercapnia
-Brief arousals that disrupt sleep cycles
-Decreased gas exchange and blood oxygen levels
Diagnosis of OSA begins with assessment.
A beginning assessment includes having the patient complete a questionnaire regarding perceived sleep quality and extent of daytime sleepiness.
risk factors of OSA
large tongue
short neck
obesity
increases with age
male sex
enlarged tonsils, uvula, or adenoid tissue
Symptoms of OSAS include (9)
fatigue, daytime sleepiness, headaches, waking with gasping or choking sensation, difficulty concentrating, irritability, depression, loud excessive snoring and memory problems
the fundamental physiological differences between normal sleep patterns and obstructive sleep apnea (OSA)
airway patency
breathing patterns
sleep quality
oxygenation
Airway patency: Normal sleep maintains an open airway, while OSA involves airway collapse.
Breathing patterns: Regular breathing in normal sleep vs. periods of apnea in OSA.
Sleep quality: Uninterrupted sleep cycles in normal sleep vs. fragmented sleep in OSA.
Oxygenation: Consistent oxygenation in normal sleep vs. intermittent hypoxia in OSA
Potential implications of undiagnosed or untreated OSA include:
Cardiovascular Complications: Hypertension, Coronary heart disease, Heart failure, & Increased risk of stroke
Metabolic issues: Type 2 diabetes & Insulin resistance
Neurological and Cognitive Effects: Memory problems, Difficulty concentrating, &Increased risk of dementia
Mental Health Concerns: Depression, Irritability, & Mood changes
Daytime functioning: Excessive daytime sleepiness, Increased risk of accidents (e.g., driving)
Quality of Life: Impaired work performance, Strained relationships, & Compromised overall well-being
Respiratory Complications: Chronic hypoxemia & Pulmonary hypertension
Agonist-antagonist opioids (mixed opioids):
Bind to kappa receptors as agonists (provide analgesia) and mu receptors as antagonists.
Because of mu antagonism, they can trigger withdrawal and severe pain in patients already on regular opioids.
Have a dose-ceiling effect: increasing the dose won’t improve pain relief.
Sometimes used in low doses to treat opioid side effects (e.g., itching), but risk reversing pain relief.
Examples: butorphanol, nalbuphine.
Pure (Full) Opioid Agonists:
Bind mainly to mu receptors in the CNS → produce analgesia.
First-line opioids for moderate to severe nociceptive pain.
No dose ceiling → higher doses = more pain relief (dosing adjusted to pain severity).
Can cause euphoria, so they carry abuse potential, but abuse is rare when used correctly for pain.
Examples: morphine, fentanyl, hydromorphone, oxycodone, oxymorphone, hydrocodone.
A polysomnography (PSG)
is a sleep study testing for wakefulness and sleepiness
Nonsurgical Management of OSA
Goal: Reduce airway obstruction & improve restorative sleep.
Lifestyle changes: Sleeping position changes or weight loss may help mild cases.
Devices:
Position-fixing devices: Hold jaw/tongue forward → reduce obstruction.
Can improve airflow, esp. for people with a small/retracted lower jaw.
Bulky, sometimes not tolerated; may cause oral tissue irritation.
CPAP (Continuous Positive Airway Pressure):
Most common treatment. Provides constant positive pressure to keep airways open.
Delivered via facemask, nasal mask, or nasal pillows. Needs a tight fit.
Newer CPAP machines:
Quiet, humidified, smaller masks (better comfort, less tissue breakdown).
Can track apnea episodes, O2 sat, HR, usage time → send to smartphone/provider.
Adherence is critical → reduces health risks of OSA.
Medicare covers cost if used consistently ≥6 hrs/night.
Many patients feel much better after adjustment → improves compliance.
Medications:
Not effective.
Sedatives worsen OSA.
Stimulants help daytime alertness but don’t fix sleep or obstruction.
Self-Management Education for OSA
CPAP Care:
Keep compressor, mask, and tubing clean → prevents infection & skin breakdown.
Use distilled water in humidifier (reduces fungal risk).
Clean mask/pillows daily with manufacturer-approved agents.
Do not share CPAP equipment.
Post-Surgical Care:
Normal: small blood-tinged saliva/mucus after coughing.
Report immediately: new bleeding, clots, or bright red blood.
Use a mirror twice daily to check throat size/swelling.
Go to ER if: throat narrows, difficulty swallowing, drooling, or signs of airway obstruction.
Pain/swallowing should improve daily → soft foods, cool liquids, humid air, warm saltwater gargles help.
Report infection signs: ↑ swelling, pus, “beefy red” mucosa, worsening pain, fever, taste change, bad breath.
Activity restrictions: no lifting or Valsalva maneuver (per surgeon’s orders).
Anxiety Management:
Provide written/digital instructions and resource contacts for CPAP or surgery concerns.
Reassure:
CPAP use takes adjustment but improves with time.
After surgery, pain & swallowing problems should improve within a week.
Snoring/apnea may persist briefly until swelling subsides.