PT 606-608 FINAL
1/1004
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
1005 Terms
The percentage of patients who report ongoing pain and disability 12 months post-whiplash injury is:
50%
Common sxs of WAD
- MOI linked to trauma or whiplash
- referred shoulder girdle/UE pain
- nonspecific concussive sxs
- dizziness and nausea
- headache, concentration, memory difficulties, confusion
Exam findings for WAD
- (+) cranial cervical flexion test
- (+) neck flexor endurance
- (+) pressure algometry
- strength/endurance deficits
- neck pain w mid range and worsens w/ end range
- postural balance/control/proprioceptive deficit
Early evidence suggests that factors associated with poor recovery post-WAD include:
a. Pain catastrophizing
b. Poor coping strategies
c. Fear avoidance behavior
d. All of the above
All of the above!
The following factors have no impact on prognosis
a. Direction of impact
b. Presence of a headrest
c. Awareness of impending collision
d. All of the above
d. All of the above
(this is stupid. and i disagree.)
(T/F) Positive expectations of recovery are associated with less pain and disability
True
Which of the 6 red flags are most relevant after MVA?
Fracture
Cervical instability
CAD
What changes might we expect to see on the radiograph post-whiplash injury
- loss of lordosis (muscle guarding, large/uncontrollable ROM, muscles spasm)
- Hyperflex/extend
- Abnormal Alignment
- Soft tissue swelling
After pain, the most common complaint(s) associated with chronic whiplash is/are:
Dizziness and Unsteadiness
Pt reports dizziness with R Cx rot. R rot with eyes closed improves the patient symptoms. This finding strengthens the case for which system(s)?
Visual system
The movement coordination impairment classification is diagnosed by
history and subjective information
examining osteo and arthrokinematics
Whiplash-associated disorders (WAD)
- Sxs arising from rear or side impact (predominantly MVA)
- Acceleration-deceleration mechanism for energy transfer to the neck
- 50% fully recover, other half have persistent symptoms
Cervicogenic dizziness defined as:
c/o lightheaded, unsteady, off balance
Impact MVCs
Factors that DO NOT affect prognosis
- Angular deformities of the neck
- Impact direction
seating position in the vehicle
- awareness of impending collision
- headrest in place at the time of the collision
- stationary or moving when hit
- older age
Quebec task force grades of WAD
Grade I (least)
Grade II
Grade III
Grade IV (severe)
Grade I Quebec task force WAD
no physical neck.upper back signs
Grade II Quebec task force WAD
Neck/upper back musculoskeletal signs
- decreased ROM
- point tenderness
Grade III Quebec task force WAD
Neck/upper back neurological signs:
- decreased reflexes
- decreased sensation
- decreased strength
Grade IV Quebec task force WAD
Neck/upper back fracture/dislocation
What Quebec grade is most common
WAD II is most common
- subgroup is very broad
Sterling 2004 classification
Differences in physical and psychological impairments (recovered v persistent pain/disability)
- accounts for motion, sensory, and psychological dysfunction
Recovery trajectories classifications
Mild
Moderate
Severe Disability
Yellow flags in WAD
headache
arm pain / paresthesia
head injury
neck OA
prior affective/poor coping strategies, catastrophizing
job, family, finances
RIsk factors for persistent problems
- High pain intensity
- High self-report disability
(greatest prognostic value)
Alar ligament and upper cervical instability
Hx: trauma, RA, down's
AROM: cord sx (worse in flex)
Tests: alleviate/provoke
Neuro: cord signs
Alar ligament Origin and Insertion
O: lateral side of Upper part of dens
I: medial side of occipital condyles
Transverse ligament Origin and Insertion
O: medial aspect of the lateral masses of C1
I: dens of axis (C2)
Spinal cord compression (due to upper cervical (structural) instability
- Clumsy gait, loss of dexterity
- paresthesia worsens w/ AROM flexion
- neuro signs of myelopathy
- sensory disturbance b/l
- b/l UE weakness
- hyper- DTR
- incontinence
Cervicogenic dizziness (swivel stool test)
- Seated on stool, swivel back and forth => dizzy?
- eyes closed, improves = visual
- remains the same, hold head, rotate body = vestibular
- if closing/open eyes, head held/not does not improve sxs, test for cervical afference (proprioceptive)
rule in/our swivel test
- Visual = close eyes (eliminate)
Visual out, still dizzy = rule out
- Vestibular = keep head still
Vestibular out, still dizzy = rule out
- Cervical = separate test (laser)
true vertigo
patient reports self spinning or environment spinning
cervicogenic dizziness (vs vertigo)
- onset soon after trauma
- Pt. c/o disorientation or vague dizziness
- exacerbated by neck movement or pain
- relief associated with relief of neck pain
Cervical position sense training
- head-mounted laser
- outside target = altered cervical proprioception
- overshoot neutral
Determination of stage: acute, subacute, chronic
acute: high irritable, pain at rest or w initial movement
subacute: mod. irritability, pain with mid-range, worse w/ end range
chronic: low degree of irritability, pain worsens with end range (sustained) or overpressure into resistance
what do we do for each stage- acute
- Education
- HEP
- monitor progress
- minimize collar use
what do we do for each stage- subacute
- education
- exercise (add manual + physical agents)
- supervised exercise (postural coordination+ stabilize)
what do we do for each stage- chronic
- education
- manual therapy + exercise
Exercise! towel snags
cross your arms across your chest and grab the towel
- stabilize with one hand, mobilize and twist with the other

what else could cause WAD
bicycle, skiing, etc (trauma)
- Most common: rapid deceleration and what the spine does in response
Alar ligament test
passive bending of upper cervical spine
- pulling alar ligament forward
- when taut = palpate C2, can feel it move to the other side
Sxs of Instability
- Intolerance to prolonged static postures
- fatigue and inability to hold head up
- better w/ external support
- need for self-manip
- feeling of instability/lack of control
- acute attacks
- sharp w/ sudden movement
neck skin crease
hypermobility @ creases
hypomobility above and below
aberrant motion
movement that deviates from the typical or expected movement pattern
- associated with low back dysfunction or instability
myofascial pain
chronic
tension
prolonged posture
tenderness of muscle
trigger points
pain with stretch
Upper crossed syndrome
stabilizers: weak, hypOtonic, inhibited
Movers: tight, hypERtonic, facilitated
Upper crossed syndrome pic
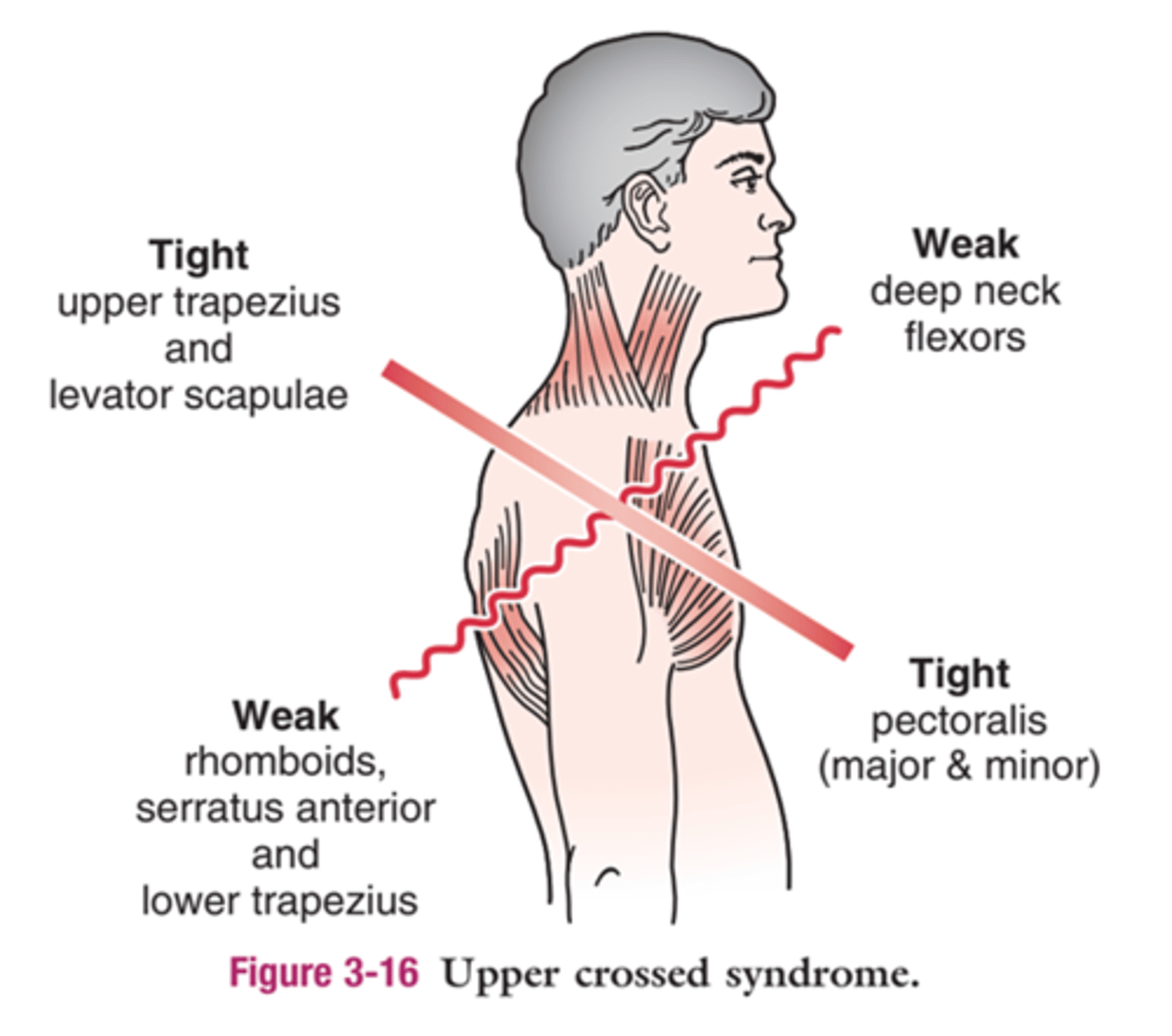
Common muscles (upper crossed) shortened/tight/overactive
Upper Trapezius
Levator Scapulae
Sternocleidomastoid (SCM)
Pectoralis Major & Minor
Suboccipitals
Common muscles (upper crossed) lengthened/weak/inhibitied
Deep Cervical Flexors (longus colli and longus capitis)
Lower Trapezius
Serratus Anterior
Rhomboids
Middle Trapezius
neck flexor muscle endurance test
maximal cervical retraction (chin tuck)
- raise head 1-2 inch. off bed and hold
W/o neck pain: 39s
W neck pain: 24s
cranial cervical flexion test
cuff under upper cervical spine, inflate to 20 mmhg
- tongue to roof of mouth, lips together, teeth apart
STAGE I
- nod to 22,24,26...30 w/ 2-3 second hold (ensure pt. can perform test)
STAGE II
- repeat each lvl. with 10 second hold, 3 reps at each level, 10 s rest between each level
What is the baseline for the cranial cervical flexion test
the highest level that the patient can hold for 3x10 seconds
cervical position sense training (JPE)
head-mounted laser
- pt stands/sits 35 inches from the target
(+) impairment = any error in the test (red or off the paper)
*ONLY 1 ERROR NEEDED TO FAIL THE TEST*
Functional Instability is Diagnosed by
A. History and subjective information
B. Examining osteo- and arthrokinematics
C. Radiographs
D. A and B
E. All of the Above
A and B
history and subjective information and examining osteo/arthrokinematics
Aberrant motion describes
a. Sudden accelerations with movement
b. Sudden decelerations with movement
c. Motion that is outside of the intended plane
d. All of the above
All of the above
progression for JPE (laser)
progression: standing, foam pads under feet
Regression: smaller ROM (dont turn to max rotation), eyes opened then eyes closed (alt. sets)
progression to deep neck flexor endurance test and exercise
progress: add conjunctive exercise, chest on yoga ball + chin tuck, chin tuck + ITY, chin tuck + row
regression to deep neck flexor endurance test and exercise
raise head of bed (less distance to travel)
Disability index in relation to outcomes
Lower = get better sooner (3-6 months)
Higher (+ older, + fearful) = progress into chronic pain
Integration of primitive reflexes, such as the Asymmetrical Tonic Neck Reflex, is essential for the emergence of head control. (T/F)
TRUE
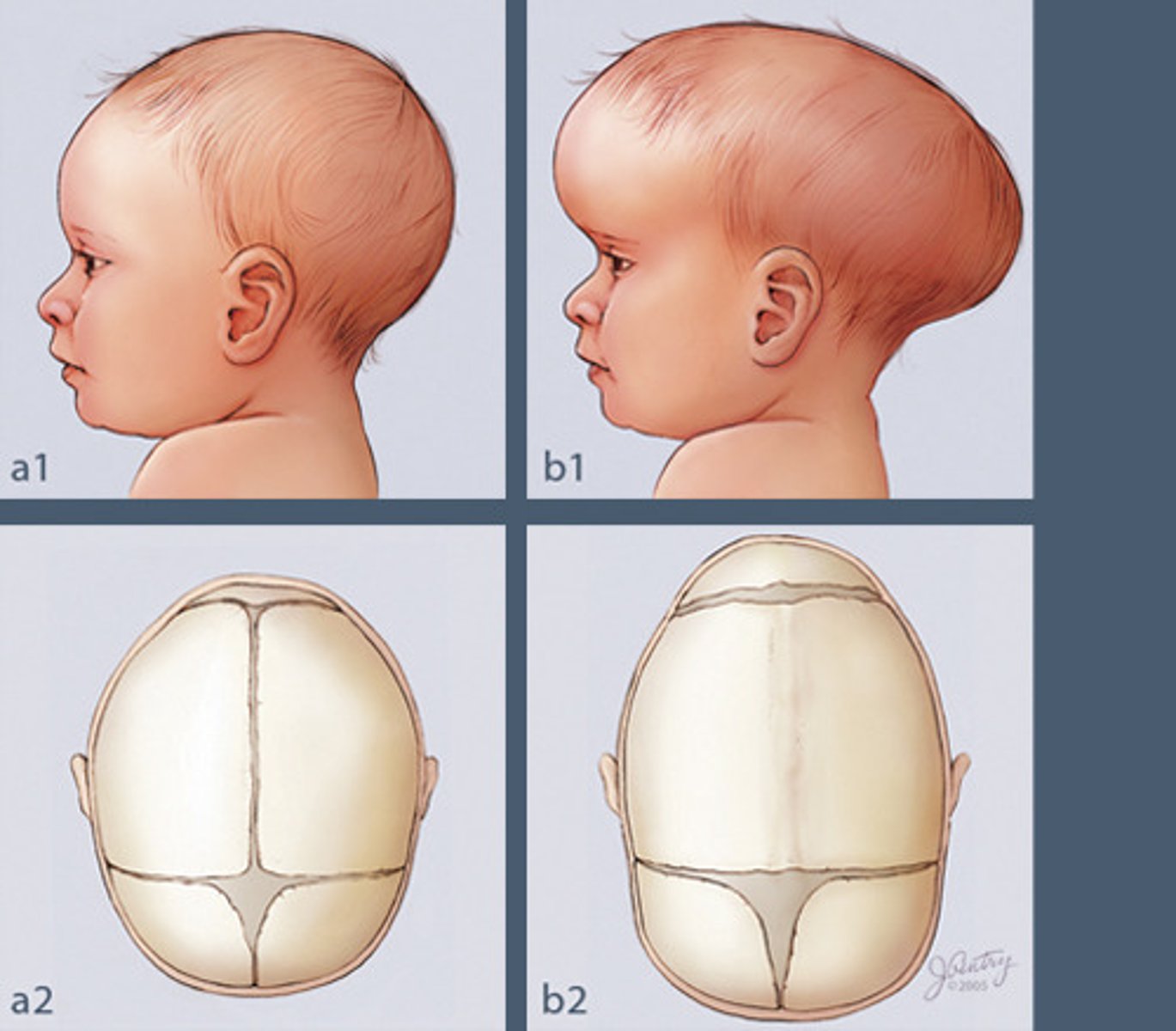
Plagiocephaly could be best described as:
a. Unilateral shortening of the sternocleidomastoid
b. Cranial flattening due to mechanical forces
c. Premature closure of cranial sutures
B- cranial flattening due to mechanical forces
(A= CMT, C= cranial stenosis)
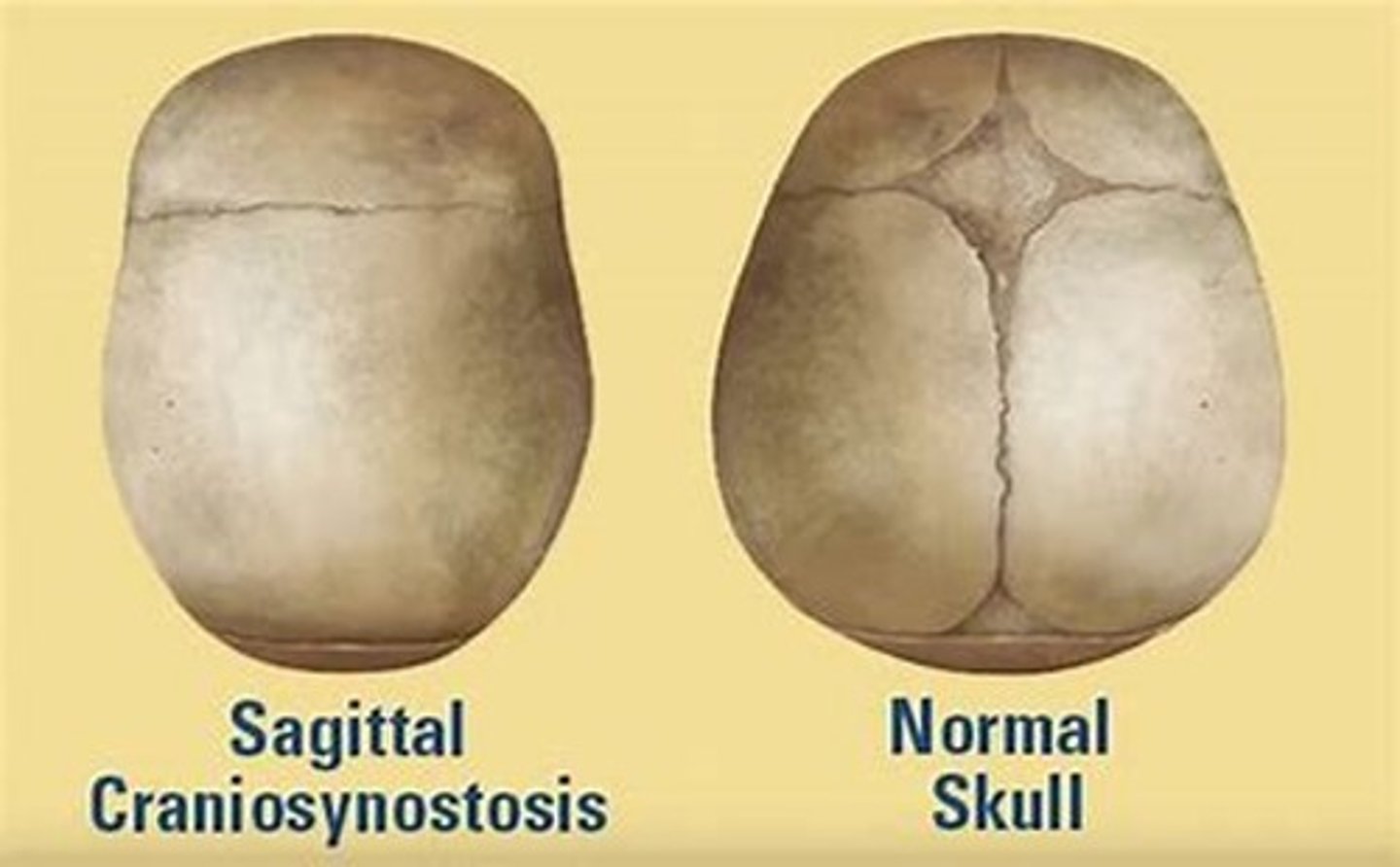
Cranial Stenosis
premature fusion of fontanelles and cranial sutures can lead to cranial vault abnormalities
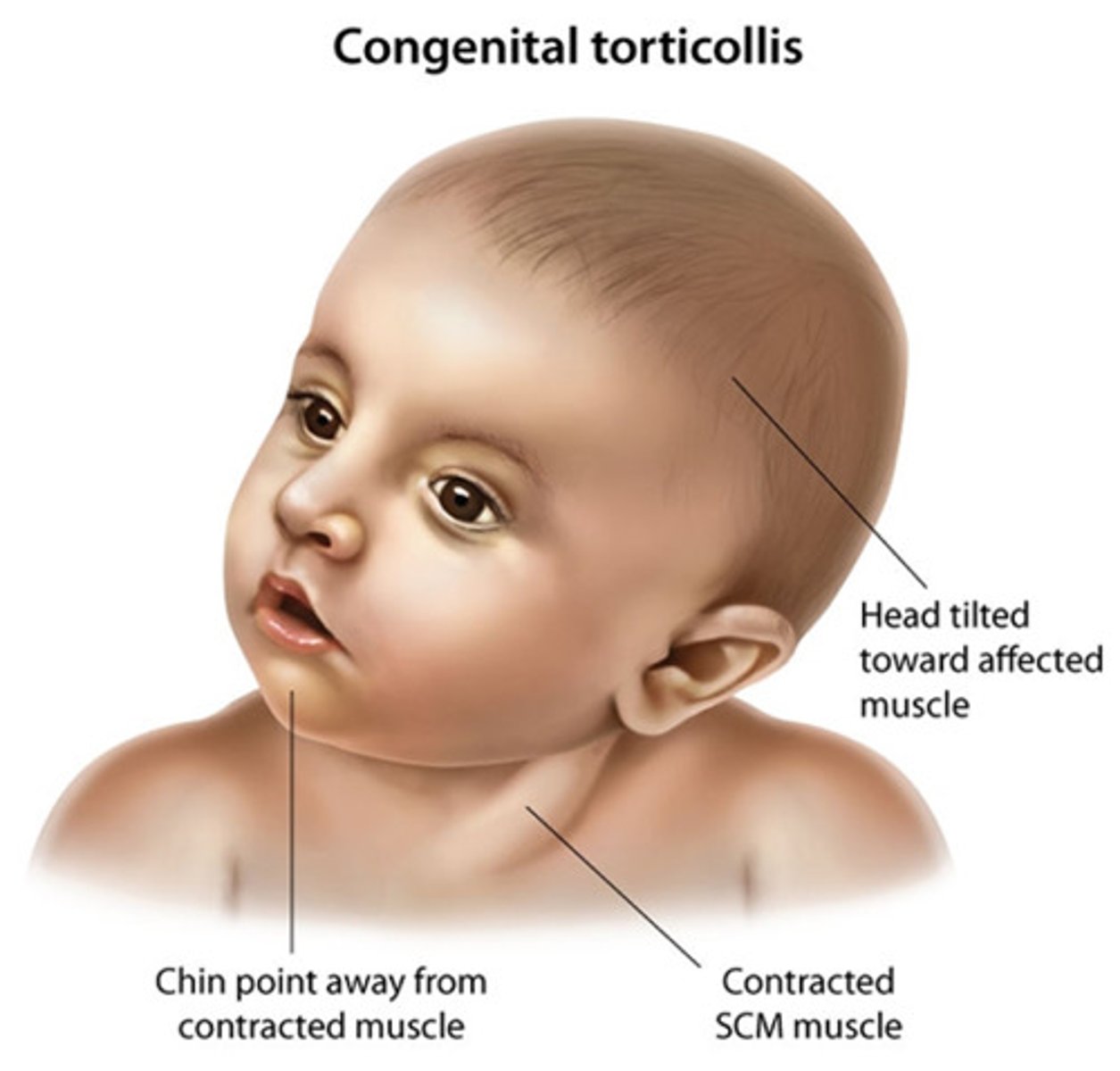
CMT
unilateral shortening of the SCM
ex: left-sided shortening, the child shows lateral flexion toward the shortened side and rotation to the opposite
All of the following are associated with a higher risk of CMT, except:
a. Cephalic position (Head first)
b. Longer birth body length
c. Primiparity (1st time giving brith)
d. Family history
a- cephalic position (head first is typical)
The physical therapy intervention for CMT is should primarily focus on the stretching and strengthening of the sternocleidomastoid muscle. (T/F)
False
- should focus on stretching and parent education, not strengthening
Current evidence for CMT management is primarily derived from clinical expertise or opinions rather than actual research. (T/F)
False
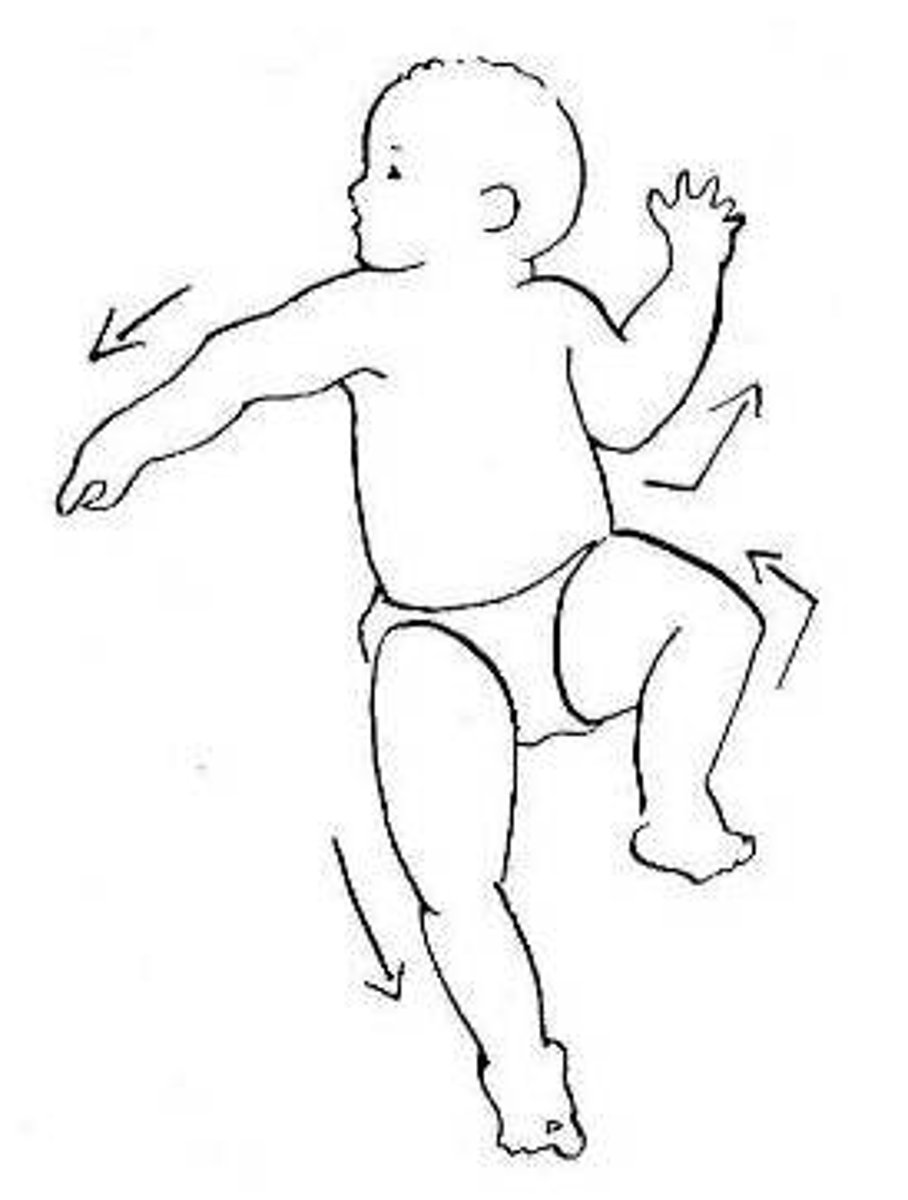
Asymmetrical tonic reflex (ATNR)
*Primitive reflex*
- fencers position
- onset ~ 37 wk
- integrated ~4-6 mo.
Extension of the arm and leg on the "face" side
Flexion of the arm and leg on the skull side
Craniosynostosis
Premature closure of cranial structures or fontanelles
- cranial asymmetry
Fontanelle closure (A,P,AL, PL)
Anterior: 12-26 month
Posterior: 1-2 month
Anterolateral (sphenoidal): 2-3 month
Posterolateral (mastoid): 12-18 month
Clinical relevance of fontanelle closure
- they are soft and flexible, allow for easy delivery
- can put infant at risk for skull fracture
ex: forceps used during deliver, head trauma post birth (MVA, mishandling)
Head control development, birth-6 months
Birth: limited capacity
2 month: hold head in midline
3 month: can hold neck vertically for long periods, can visually track
4-6 month: head in line w body when moved from supine to sit (pull-to-sit task)
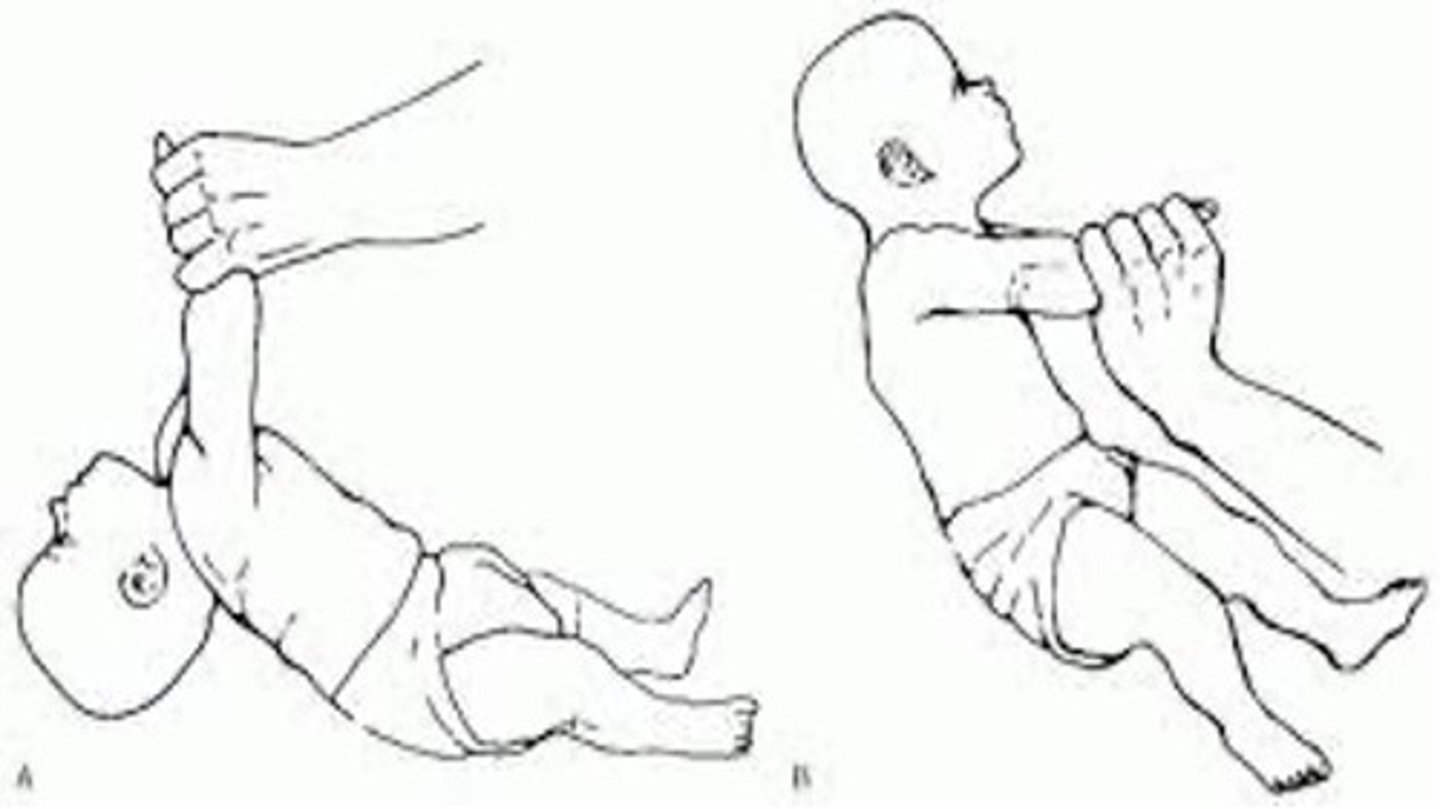
Pull-to-sit test
Newborn: complete head lag
3 months: slight lag
4-6 months: no lag
> 6 months: lift head spontaneously and repeatedly in anticipation
Congenital muscular torticollis (CMT)
wry neck, twisted neck
- unilateral shortening of SCM
- lateral neck flexion to one side and rotation to others
Congenital muscular torticollis (CMT) accompanied by other conditions:
cranial deformity
developmental
dysplasia (hips)
Brachial plexus injury
Etiology of CMT
excessive fibrosis, hyperplasia, and atrophy of SCM
(some have palpable fibrotic nodule = more severe than w/o)
Risk factors for CMT
prenatal: intrauterine crowding, malposition, ineffective myositis
perinatal: breech, forceps used during delivery
postnatal: positional preference, cranial deformity
*history of CMT in family, primiparity, longer birth length
Prognosis CMT
PT before 3 month = excellent prognosis = greater tolerance to stretching before voluntary head control development
Positive prognostic factors CMT
- participation in PT
younger @ initiation
- decrease difference in PROM b/w L and R sides
- decreased difference in SCM thickness b/w L and R
- caregivers adherence to HEP
Negative prognostic factors for CMT
- motor asymmetry
- older age at initiation
- restriction of PROM or increased severity of head tilt
- increased thick/stiff SCM
- SCM mass
- low birth weight, breech
PT Exam for CMT
- infants posture: supine, sit, prone, stand
- look @ asymmetries
- positional preference
- PROM
- AROM
- strength + endurance
PT intervention for CMT
- manual stretching
- AROM neck and trunk
tummy time (assisted or independent)
- parent education
Discharge/discontinue PT CMT
- passive neck ROM within 5 degrees of the non-affected side
- no visible head tilt
- age-appropriate motor development
- symmetrical active movement patterns
- caregivers understanding/monitor adherence to exercise
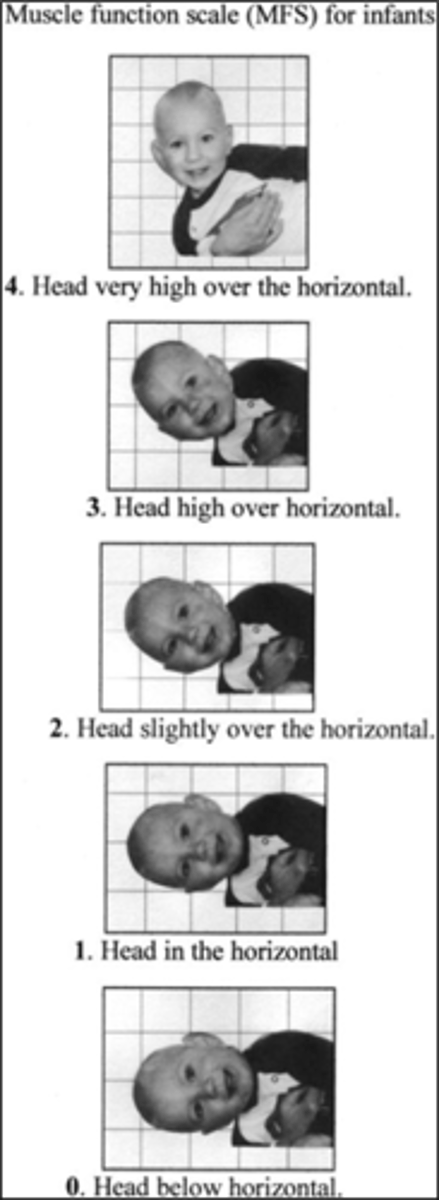
Measurement of infant strength and motor control of the head and neck using MFS
trigger points
hyperirritable spots in skeletal muscle that are associated w/ palpable nodules and taut bands of muscle fibers
latent trigger point
non-constant, provoked w/ palpation
active trigger points:
provoked when touched, compressed, etc.
can be spontaneous
referred pain
characteristic of trigger points
tender spot in muscle
tense band of muscle
decreased stretch
referred pain w palpate
sweating, vasoconstrict
interventions for trigger points
direct pressure application w/w/o PROM,AROM,stretch
- enough pressure to reproduce sxs
- 10 sec-1 min of pressure
- release, add passive stretch, active contraction
- ice/heat
-dry needling
- injection
which of the following anterior muscles is commonly inhibited in persons presenting with neck pain
Longus coli
longus capitus
which of the following muscles are commonly tight in persons with neck pain
pectoralis major and minor
Providing equitable care begins with using the correct terminology. Gender identity is:
a) The patient's internal sense of who they are
b) Is assigned at birth
c) Is aligned with gender expression
d) All of the above
A- the patient's internal sense of who they are
While many have different feelings about the term microaggression, this term is commonly used to describe:
a) verbal, behavioral, and environmental indignities
b) can be overt or subtle
c) Are consistently intentional slights that target a person or group
d) All of the above
e) A & B
A and B
- verbal, behavioral, and environmental indignities that can be overt or subtle
If you commit a microaggression, you should
a) Identify the harmful behavior
b) Focus on the intent of the behavior rather than the impact
c) Create a plan to change behavior
d) All of the above
e) A & C
A and C
- identify the harmful behavior and create a plan to change
To manually stretch the R upper trapezius, the therapist would position the patient's neck in slight flexion, L SB and ...
a) Slight L rotation with overpressure on the acromion
b) Slight R rotation with overpressure on the acromion
c) Slight L rotation with overpressure on the spine of the scapular
d) Slight R rotation with overpressure on the spine of the scapular
b) Slight R rotation with overpressure on the acromion
Acting unilaterally, contraction of the right sternocleidomastoid results in:
a) Right cervical side bending and left rotation
b) Left cervical side bending and left rotation
c) Right cervical side bending and right rotation
d) Left cervical side bending and right rotation
a) Right cervical side bending and left rotation
Which prominent muscle of the anterolateral neck attaches to the mastoid process?
a. upper trap
b. lev. scap
c. sternocleidomastoid
d. mylohyoid
c. sternocleidomastoid
Patients categorized as having non-traumatic neck pain with movement coordination impairments often present with a pattern of muscle imbalance known as "upper crossed syndrome". All of the following is characteristic of upper crossed syndrome, EXCEPT:
a) Shortened, hypertonic suboccipital muscles with weakened, hypotonic longus coli muscles.
b) Shortened, hypertonic upper trapezius muscles with weakened, hypotonic levator scapula muscles
c) Shortened, hypertonic pectoralis major and minor muscles with weakened, hypotonic serratus anterior muscles
d) Shortened, hypertonic sternocleidomastoid muscles with weakened, hypotonic lower trapezius muscles
b) Shortened, hypertonic upper trapezius muscles with weakened, hypotonic levator scapula muscles
According to Childs et al (2004), all of the following statements are true of patients in the "Conditioning and Increased Exercise Tolerance" category, EXCEPT:
a. While strengthening and endurance training for some upper trunk muscles is often helpful for patients in this category, clinical experience suggests that there is no additional benefit from specific stretching of shortened muscles in the upper trunk or shoulder girdle.
b. Patients in this category are often characterized by lower disability and pain scores and a longer history of neck symptoms.
c. Patients in this category often do not present with significant limitations during examination of active range of motion.
d. Many patients in this category are regarded as having ''clinical instability'', meaning that they may have segmental hypermobility and poorly controlled or aberrant patterns of movement
a. While strengthening and endurance training for some upper trunk muscles is often helpful for patients in this category, clinical experience suggests that there is no additional benefit from specific stretching of shortened muscles in the upper trunk or shoulder girdle.
Based on Rebbek (2017) therapists should select exercises for patients with whiplash and associated disorders absed on
a. the presence of a specific impairment
b. symptom responsiveness
c. the absence of pain
d. A and C
e. A and B
A and B
- presence of a specific impairment and the symptom responsiveness
After pain, the most common complaint(s) associated with chronic whiplash is/are:
a. loss of active ROM of the cervical spine
b. dizziness
c. unsteadiness
d. B and C
B and C
- dizziness and unsteadiness