Inflammation, bleeding, and dry eye
1/25
Earn XP
Description and Tags
As part of anterior segment disorders
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
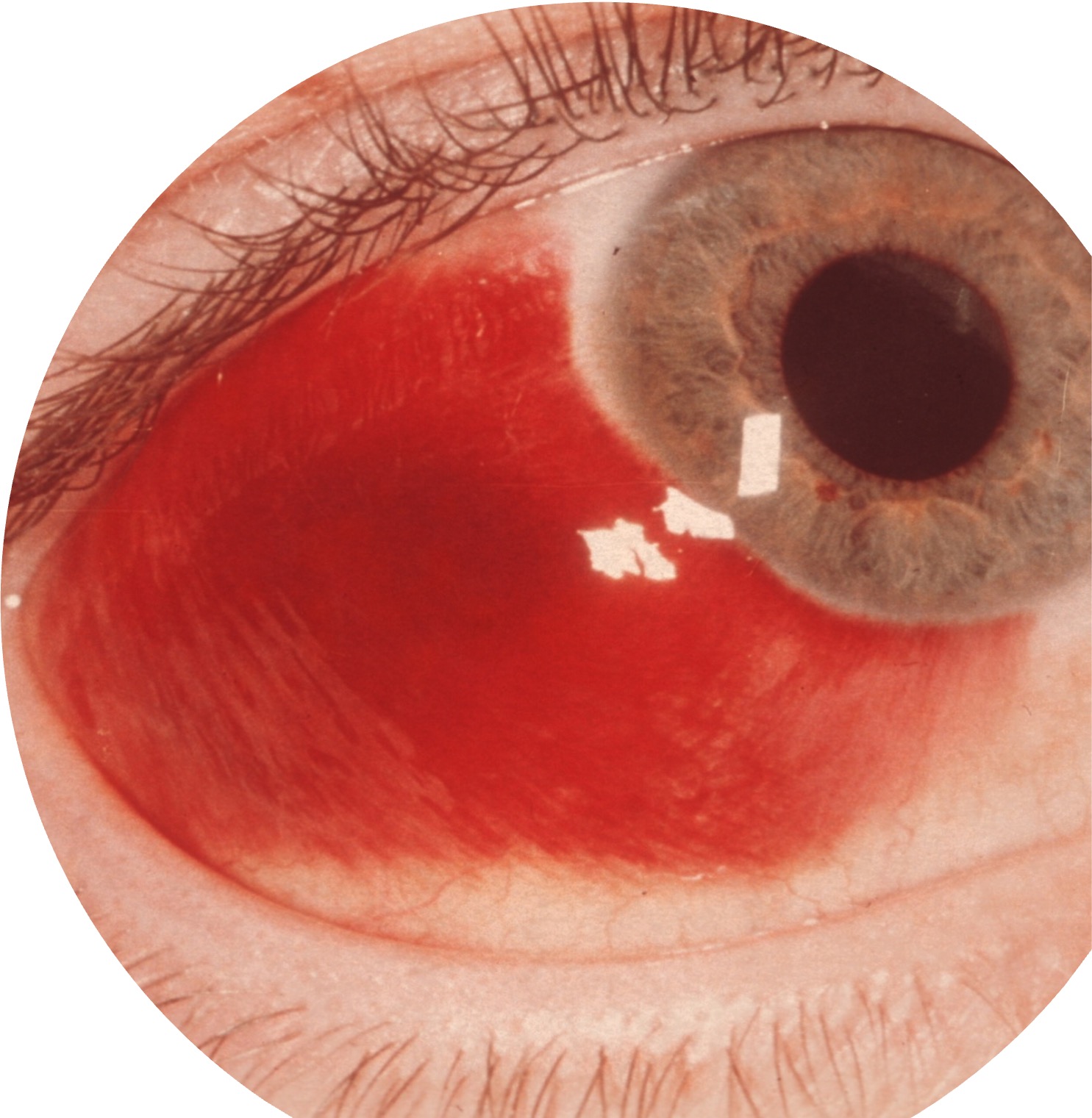
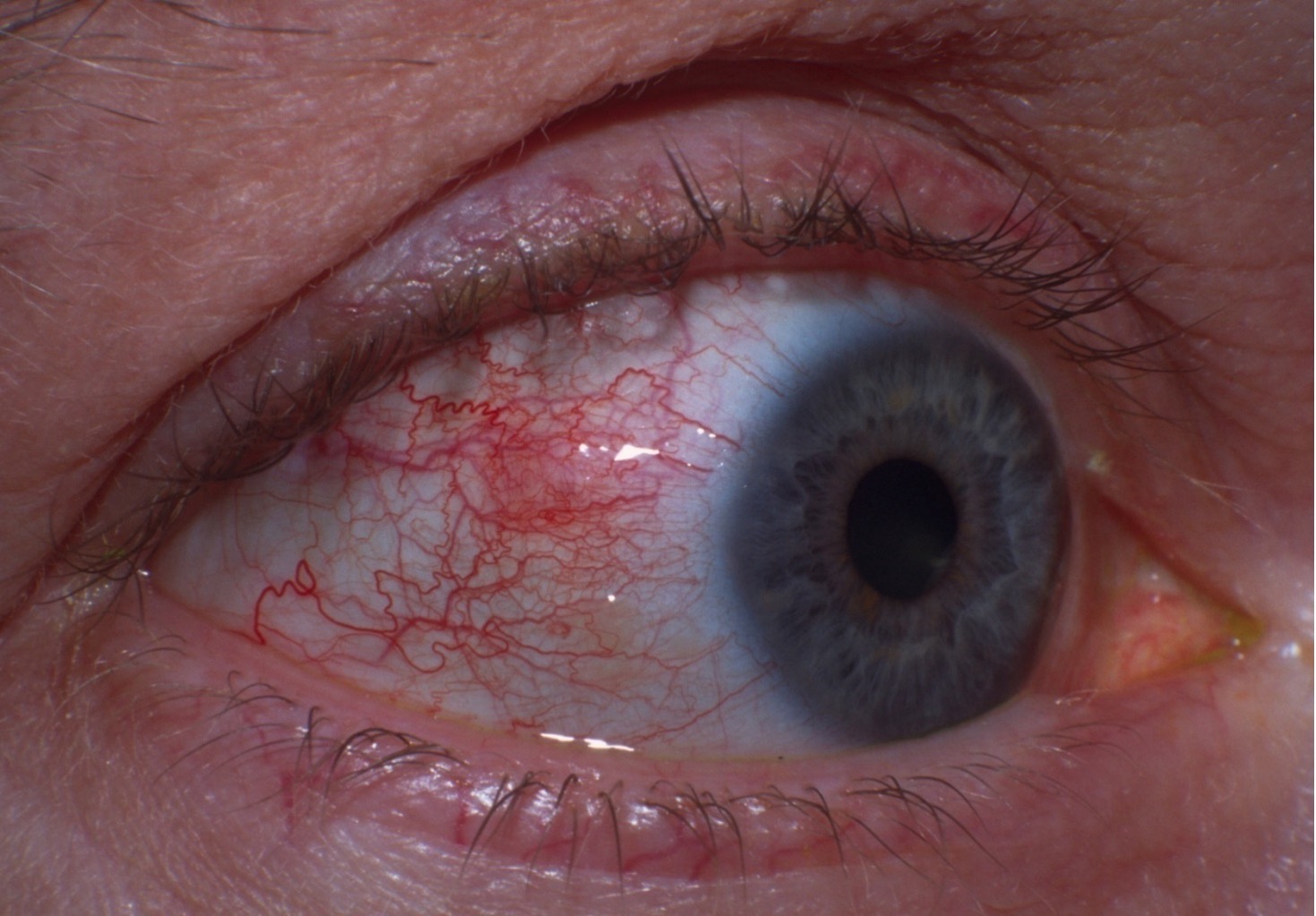
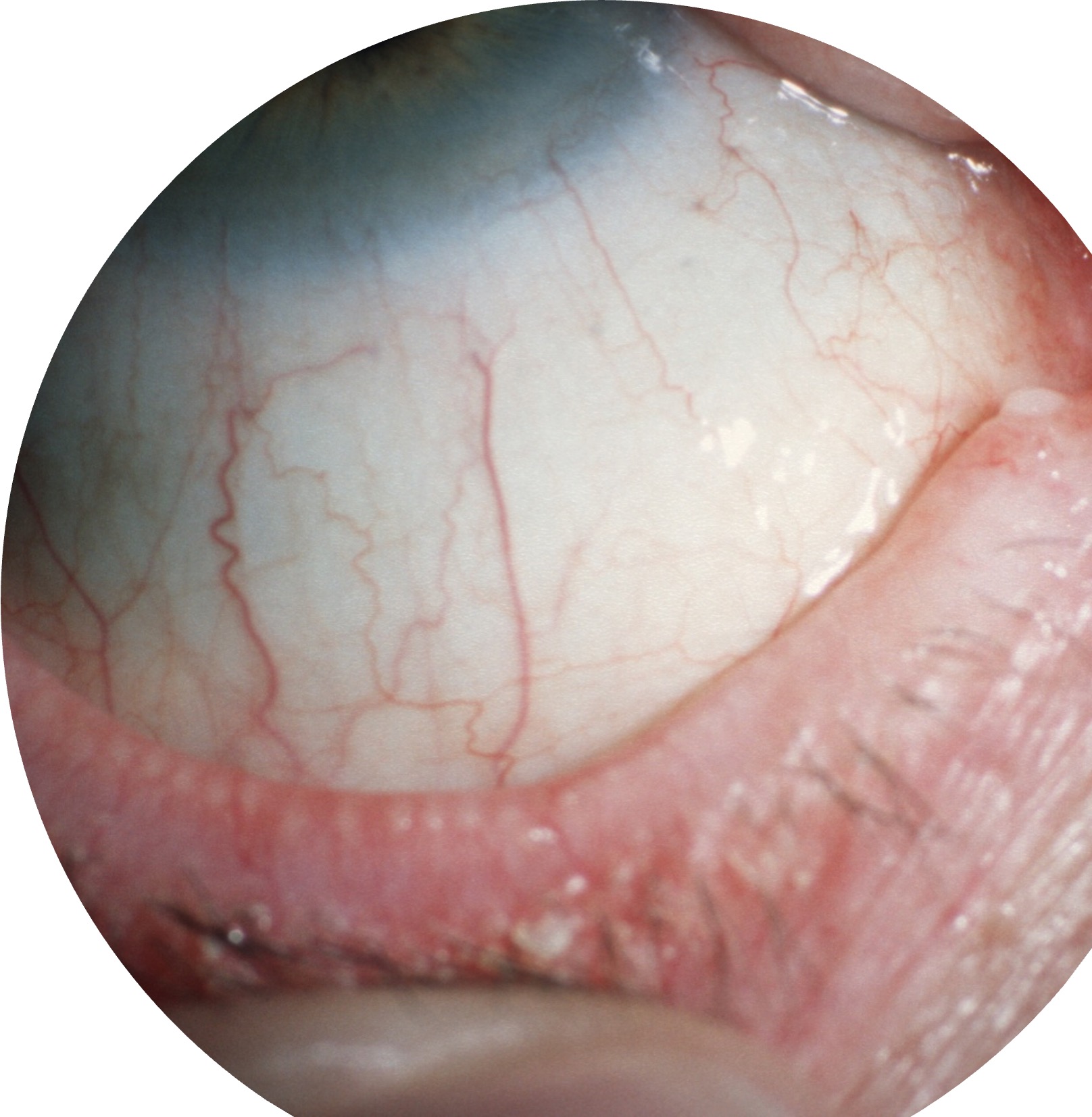
True or false - subconjunctival haemorrhage is an ocular emergency.
False; it is usually benign and self-resolving.

What might the patient be suffering from?
The patient has hypertension and is taking blood thinners
The patient had a recent bout of vomiting sickness
The eyes are not painful and there is no change in vision
The redness is unilateral
The patient is likely suffering a subconjunctival haemorrhage.
What are the types of corneal ulceration?
The types of corneal ulceration are dendritic (HSV), bacterial, acanthamoeba keratitis, and marginal keratitis.
True or false? Dendritic corneal ulceration is caused by the herpes zoster virus.
False; it is caused by the herpes simplex virus (HSV).
True or false? The herpes simplex lies dormant in the trigeminal nerve, travelling along this nerve to cause local infection when reactivated in dendritic ulcer.
True; the herpes simplex virus remains latent in the trigeminal ganglion and can reactivate, leading to dendritic ulcers.
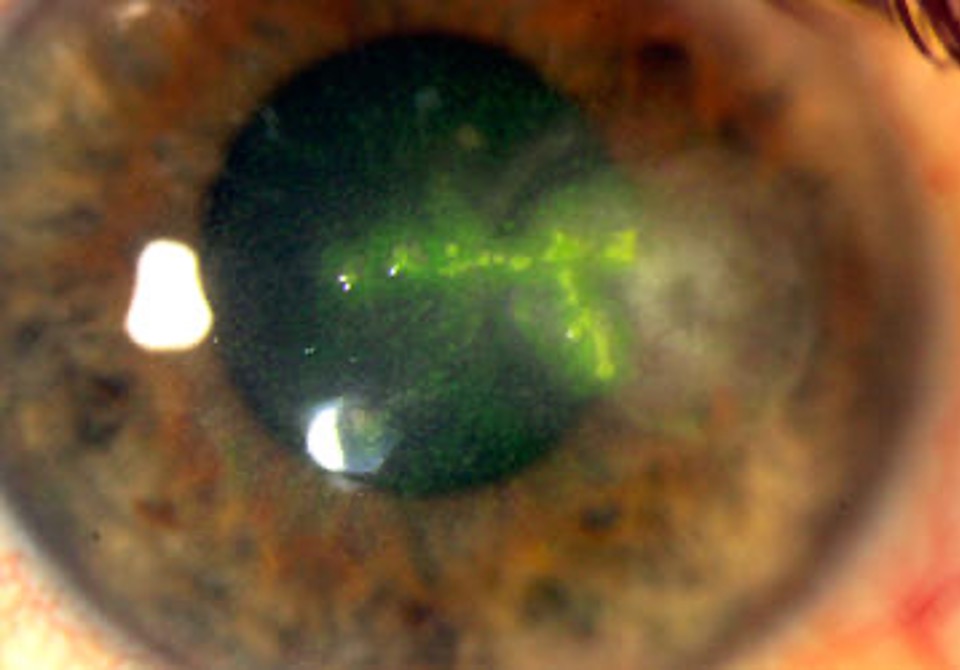
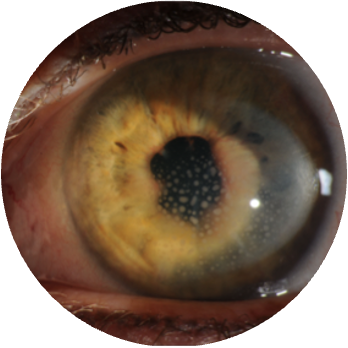
What might the patient be suffering from?
The patient is immunodeficient
The patient has recurrent cold sores
The patient is experiencing pain, photophobia, redness and reduced vision in one eye
Under slit lamp examination with fluorescein, a star-shaped ulcer can be seen in the cornea, as well as infiltrates and inflammation of the stroma
The patient is likely suffering a dendritic ulcer caused by herpes simplex virus infection. This can be identified by the characteristic dendritic shape of the ulcer, as well as the history of cold sores.
What would you advise a patient with a dendritic ulcer?
Anti-viral medication, such as acyclovir, should be prescribed
Steroid treatment may be required if the symptoms are severe
Contact lenses should be avoided until the condition resolves
A biopsy may be taken to check there is no underlying pathology

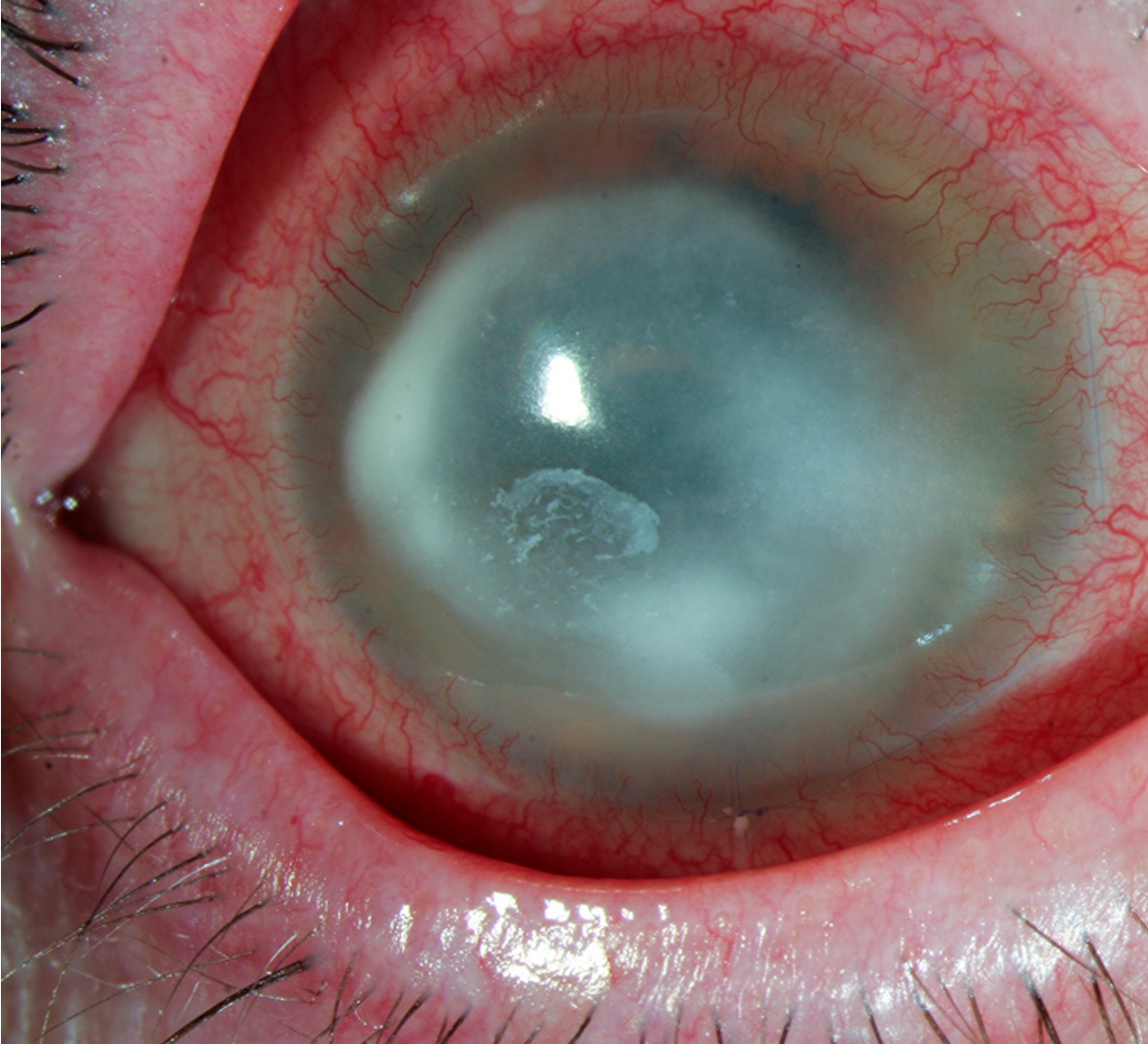
What is the patient likely suffering from?
They are a contact lens wearer
The patient has a history of blepharitis and dry eye
The eye is red, painful and watery
The lids are swollen
The patient is sensitive to light and feels something is getting in the way of their vision
On slit lamp examination, there is a white ulceration on the cornea as well as corneal infiltrates
The patient is likely suffering from a bacterial corneal ulcer, often linked to poor contact lens hygiene or blepharitis and dry eye. It can be distinguished by the white appearance of the ulcer and the watery discharge.
What would you advise a patient with bacterial corneal ulcer?
Strong antibiotics will be prescribed to penetrate the cornea - chloramphenicol is not strong enough in this case
Contact lenses should be avoided until the condition is resolved
Importance of contact lens hygiene
Importance of continued management of blepharitis, as this can overgrow and cause bacterial ulcer
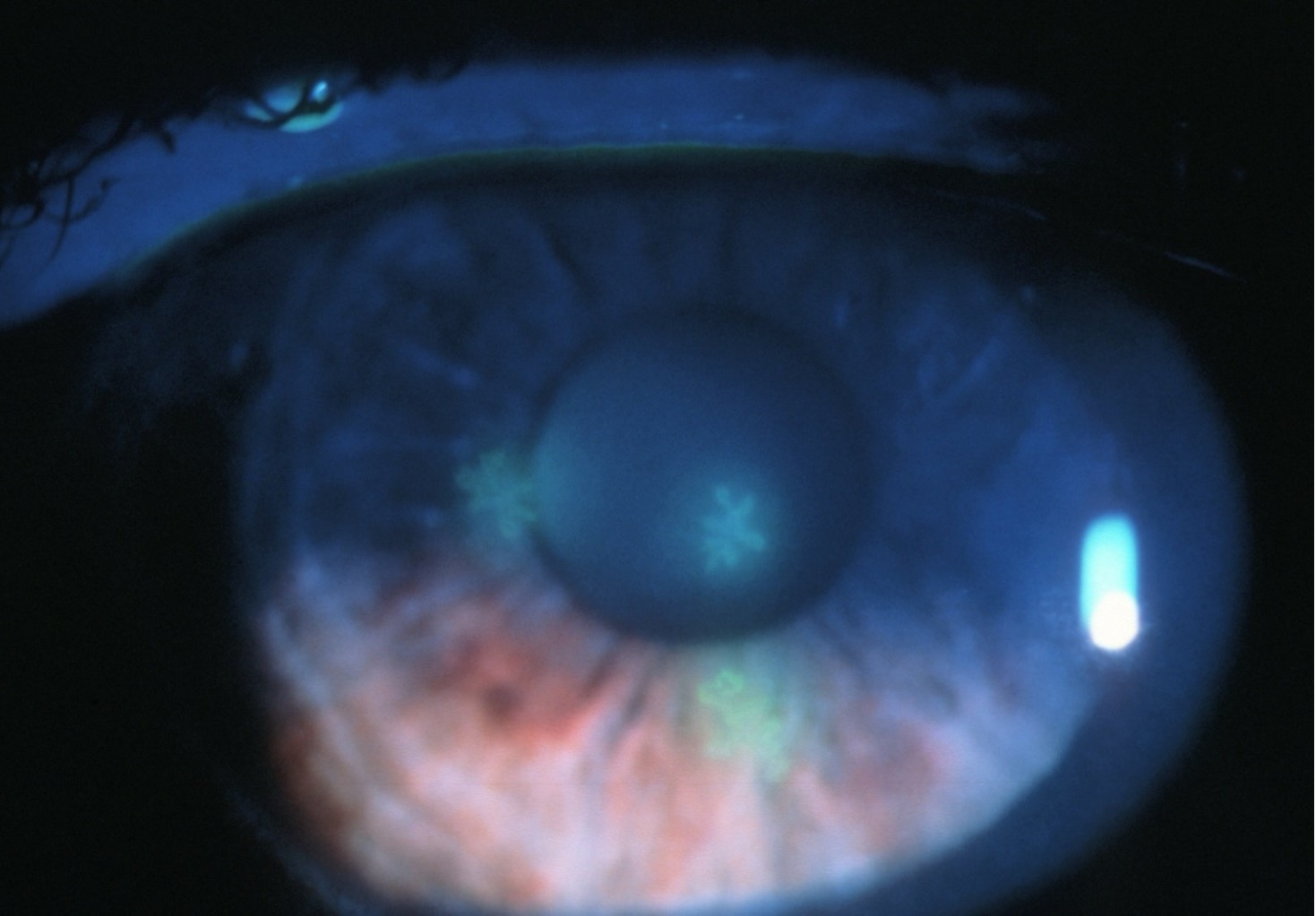
What is the patient likely suffering from?
The patient is a contact lens wearer, and recently went swimming in them as they don’t like to swim in their glasses
The patient recently scratched their eye
The patient is in a significant amount of pain
There are not many outward signs to match their symptoms
On slit lamp examination, there is a faint ring-shaped ulcer and some pus pooling in the cornea (hypopyon)
The patient is likely suffering from acanthamoeba keratitis. This can be identified by their recent corneal scratch plus swimming in their contact lenses, as well as the high level of pain compared to relatively few outward signs.
This is an ocular emergency, and treatment must be initiated rapidly to avoid permanent vision loss.
What would you advise a patient suffering with acanthamoeba keratitis?
Anti-amoebal or antiseptic drops will be prescribed to kill the organism, ideally before it does too much damage to the cornea
Counselling will be required, as the condition can be very serious and may result in permanent vision loss or require corneal graft surgery
Avoid contact lens wear until advised otherwise
Advise that the condition is not contagious and will likely not spread to the other eye unless both were infected at the same time
True or false - acanthamoeba infection proceeds in two stages.
True - in the first stage, the amoeba is actively replicating and breaking down the contents of the cornea; in the second stage, the amoeba forms a hard ulcer and becomes more resistant to treatment.

What is the patient likely suffering from?
History of blepharitis
The eye is uncomfortable, but not painful
On slit lamp examination, there is a peripheral ulcer at the edge of the cornea
The patient is likely suffering from marginal keratitis, which is often caused by an overgrowth of the bacteria associated with blepharitis.
What would you advise a patient suffering with marginal keratitis?
Lid hygiene techniques to manage blepharitis and prevent overgrowth
Hot compress and lubricating drops to alleviate symptoms
Avoid contact lenses until condition resolved
Topical antibiotics or steroids can be prescribed in more serious cases
Episcleritis
Inflammation of the top layer of the sclera
What is the patient likely suffering from?
The patient has previously had chicken pox and suffers from rheumatoid arthritis
The eye is red, tender, and achy, and has watery discharge
On slit lamp examination, there is swelling of the scleral capillaries, but the anterior chamber is clear
The patient is likely suffering from episcleritis, identified by the history of herpes zoster infection and the presence of sceral hyperaemia.
What would you advise a patient suffering with episcleritis?
The condition should self-resolve in one week
Cold compress and lubricating drops can be used to soothe
True or false - blepharitis is a type of uveitis?
False - blepharitis is associated with the eyelids, whereas uveitis is inflammation of the structures that make up the uvea (iris, ciliary body, and choroid).
What is the patient likely suffering from?
The patient is experiencing sudden pain, watering, and redness of the eye
The patient also has lupus
The patient is feeling very light sensitive and has slightly reduced vision in the affected eye
On slit lamp examination, the following can be observed: corneal precipitates, iris nodules, cells and flare inside the aqueous, and synechiae (the iris is stuck to the lens)
The vessels at the limbus are red and inflamed
The patient reports nausea
On tonometry, the IOP is elevated
The patient is likely suffering from iritis. This can be identified by the presence of keratic precipitates and iris nodules, synechiae, and limbal vessel hyperaemia.
What would you advise a patient suffering with iritis?
If they do not have a systemic inflammatory disorder diagnosis, they may need to visit their GP to see if this may be the underlying cause of the inflammation
Topical steroids will be prescribed
Cyclopentolate will be administered to relax the pupil as this may be in spasm
A dilated fundus exam will be needed to check for involvement of the posterior uvea
The patient will need to be monitored for secondary glaucoma
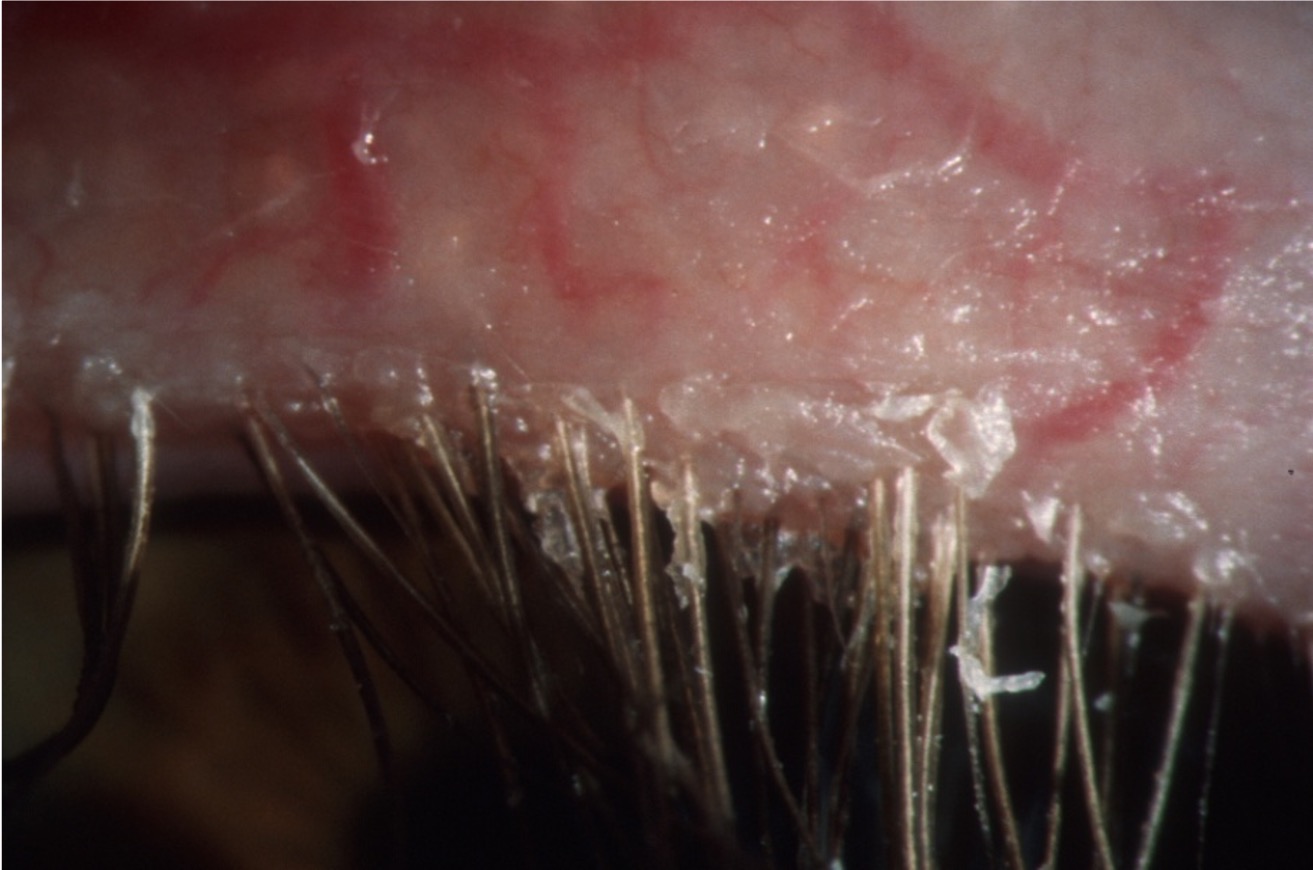
What is the patient likely suffering from?
The patient is experiencing sticky, crusty eyelids bilaterally
The patient has recurrent styes
The eyes are dry and sore
The patient is photophobic
They usually wear their contact lenses, but lately cannot tolerate them
The patient is likely suffering from blepharitis, which is caused by non-infectious bacterial infection and inflammation of the eyelids and lashes, and Meibomian glands.
What are the two types of blepharitis?
Anterior - involves the eyelids and lashes and is usually caused by bacterial overgrowth in this area. This type is associated with crusty lashes and styes.
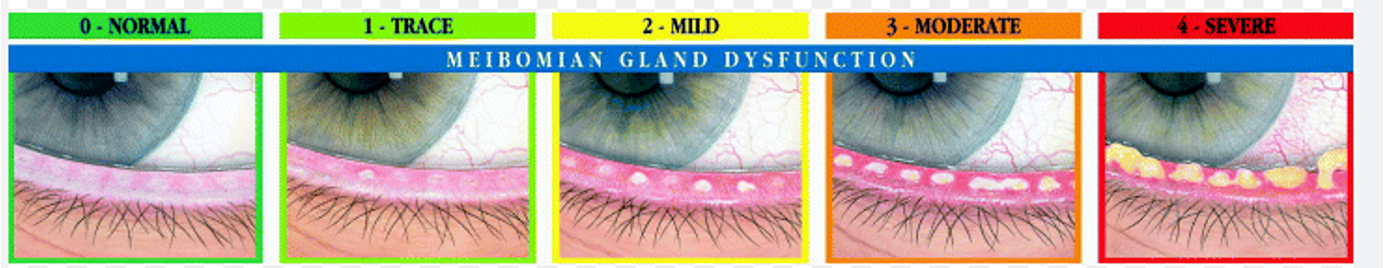
Posterior - aka Meibomian gland dysfunction. This type is associated with a blockage of the Meibomian glands (graded 0-4) preventing formation of a stable tear film and leading to dry eye.
True or false? A person can have both anterior and posterior blepharitis simultaneously.
True, it is possible for a person to have both types concurrently, resulting in a combination of symptoms related to each condition.
What is the patient likely suffering from?
The patient is experiencing red, burning, watery eyes bilaterally
The patient has recurrent styes
The patient is photophobic
They have a history of psoriasis
On slit lamp examination, the Meibomian glands appear to be clogged
The patient is likely suffering from posterior blepharitis. This can be identified by the clogged Meibomian glands, history of inflammatory disorders, and symptoms of dry eye likely caused by an unstable tear film.
What would you advise a patient suffering with blepharitis?
Topical antibiotics may be prescribed if condition is flaring up
Importance of lid hygiene to manage the blepharitis
Hot compress and ocular massage should be used in posterior blepharitis to melt the oil blocking the Meibomian glands
Lubricating eye drops can be used to alleviate the symptoms of dry eye
Steroid drops may be needed if there is corneal involvement and the condition is not responding to lid hygiene
What are the three components of tear production?
Lacrimal sac - watery component
Meibomian glands - oily component
Goblet cells of conjunctiva - mucus layer