DDT - Haematology (Peak topic)
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
What is anaemia?
Red blood cells are either: not being produced enough, not have a long enough lifespan (haemolysis), and increased blood cell loss. Can be it’s own disorder, and be caused by another disorder
Symptoms of anaemia
Lethargy, problems breathing, tachycardia (increased heart rate), and there can be no symptoms at all (asymptomatic)
How does the body compensate for anaemia?
Increased heart rate, increased production in immature red blood cells (reticulocytosis)
Causes of anaemia - Failure of productions (Haemoglobin) underlying conditions
Iron deficiency, haemoglobinopathy, anaemia of chronic disease (anaemia caused by an infection, kidney disease or cancer)
Failure of production - RBC underlying conditions
Bone marrow defects, renal failure, vitamin B12 deficiency
Increased RBC loss underlying conditions
Major blood loss could be a factor as well as diseases causing this like bowel disease/cancer where blood would be in faecal matter and stomach ulcers which can cause internal bleeding
Reduced RBC lifespan - structural defects
Sickle cell disease and spherocytosis (where RBC’s are spherical, not biconcave shape)
Reduced red cell lifespan - Caused by the immune system
Autoimmune haemolytic anaemia and incompatible blood transfusion
Reduced RBC lifespan - mechanical
Prosthetic heart valves (where blood leaks into the area between valve and heart tissue, after replacing heart values) hypersplenism (spleen is hyperactive, destroying too many RBC’s) and malaria (destroy’s RBC’s)
Reduced RBC life span - Enzyme defects
Pyruvate kinase and G6PD deficiency cause RBC’s to break down faster than usual
Types of blood cancers
Leukaemia, lymphoma, myeloma, and myelodysplastic syndrome
Ways to develop haematological diseases from the environment
Chemical exposures like benzene
Drugs like alkylating agents
Radiation which can damage cells and tissues, causing cancers
Infections like viruses (HTLV-1) and bacteria (Helicobacter pylori)
Ways to diagnose haematological diseases
Karyotype analysis, FISH and gene sequencing like next generation, as well as flow cytometry
What is leukaemia?
Severe overproduction of WBCs, typically caused by bone marrow failures. Can be either chronic or acute
What is acute leukaemia and chronic leukaemia?
Acute leukaemia causes the aggressive proliferation of lymphocytes which invade organs and result in bone marrow failure. Chronic leukaemia is far more gradual, and affects mature cells
What is flow cytometry and how does it work
Flow cytometry is used to identify cells in homogeneous liquids, useful in cases like blood. Biomarkers are determined by using antibodies connected to fluorochromes for analysis. Also as light passes through the cell, it scatters, giving side and front scatter for additional information, like the size and complexity of the cell
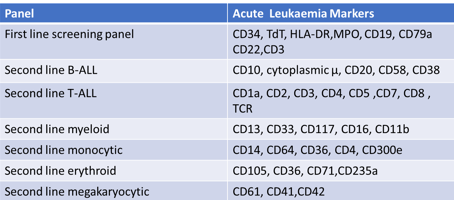
If a patient has biomarkers of CD34, TdT, HLA DR, CD10, CD19, and CD22 presents, which type of leukaemia would they have?
Second-line B-type acute lymphoid leukaemia (B-ALL)
Difference between Lymphoblastic and Myeloblastic
Lymphoblastic affects lymphocytes whilst myeloblastic affects granulocytes or monocytes
Treatment for CML, CLL, AML and ALL (Types of leukaemia)
Common cancer treatments like chemotherapy and stem cell therapy (to treat the abnormal bone marrow). Drugs which target the CNS are common, as leukaemia cells are normally always found in the CNS
What is MRD?
Minimal residual disease are small amounts of cancer left in the body after treatment, even if if seems that there is no disease left
Causes of abnormal haemostasis (coagulation)
Defects of any clotting factors, anticoagulation drugs, as well as low platelet counts (thrombocytopenia)
3 stages of haemostasis
The vascular phase (vasoconstriction to reduce blood loss), platelet phase (plugging the hole using platelets, using von Willebrand factor to bind platelets) and coagulation phase (stabilises plug with fibrin mesh as well as coagulation factors)
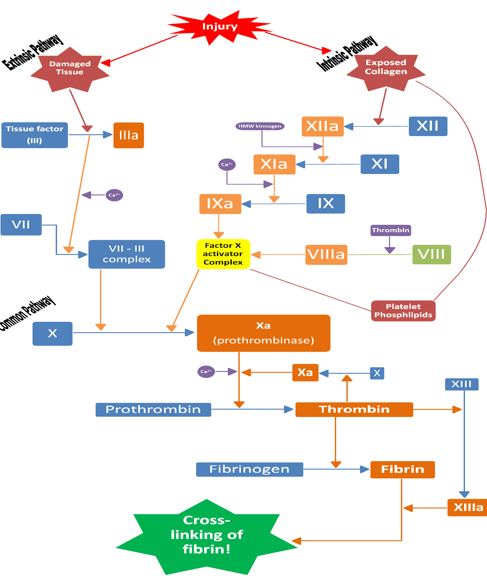
Fibrinogen requires what to convert to fibrin
Thrombin is required
Tests to detect coagulation abnormalities
Prothrombin time to test extrinsic clotting system effectiveness by adding tissue extract and calcium
Thrombin time for clotting after adding extra thrombin
Activated partial thromboplastin time (appt) where phospholipids, surface activators and calcium are added to test intrinsic pathway effectiveness
Fibrinogen to test the amount of fibrinogen in the body
Where are coagulation factors produced?
By the liver
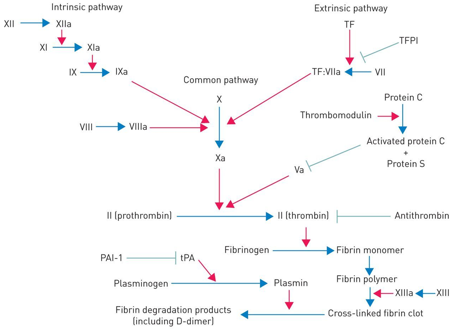
Coagulation factor inhibitors
Tissue factor pathway inhibitor (tfpi) which inhibits factors X, Vii and III tissue factor. Only released locally to prevent unnecessary clots
Antithrombin which inactivates thrombin, with the drug increasing it’s effects significantly
Protein C and S which inhibit cofactor V and VII
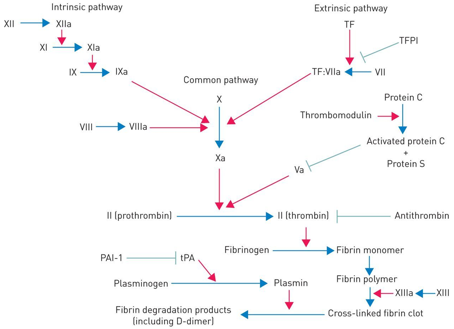
What is fibrinolysis, how does it work and how is it stopped?
Fibrinolysis is the breakdown of blood clots in the body, releasing plasmin, which inhibit fibrinogen, fibrin, factor V and VIII. Stopped by plasminogen activator inhibitor (PAI)
Treatment of abnormal haemostasis (too excessive)
If thrombosis is excessive, using anticoagulation drugs like warfarin or heparin, replacing fibrinogen via cryoprecipitation, and transfusion of platelets alongside fibrinogen side fresh plasma to replace the clotting factors. Also, treating underlying cause is the main objective