Day 17 Muscle Physiology Revised
1/51
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
52 Terms
somatic nervous system is the nervous system that innervates
skeletal muscle fibers
motor unit
- one neuron + all muscle fibers it innervates
neuromuscular junction
Motor neuron releases ACh into the synaptic cleft
Surface of the sarcolemma nearest the synaptic cleft is called the motor end plate; contains ligand-regulated Na+ channels; Schwann cell covers junction
Affected by chemical agents
Organophosphates
- (found in insect repellents)
- (binds and inhibits acetylcholinesterase or Ach E)
- If acetylcholine can’t be broken down, you end up with convulsions, meaning it’ll cause skeletal muscles to continuously contract (can look like seizures)
Black Widow Spider Venom
- Causes explosive release of Ach
- This then causes spastic paralysis (muscles contract and stays contracted because it doesn’t have time to relax)
Curare
- Blocks Ach receptors (Ach can’t bind to their receptors)
- Causes flaccid paralysis (muscle cannot contract)
Botulinum toxin (Clostridium botulinum)
- Blocks Ach release
- Destroys the ends of axons, so no terminals will exist containing neurotransmitters to release Ach
- No Ach released à flaccid paralysis
Four phases of muscle contraction
Muscle excitation
Excitation-contraction coupling
contraction
relaxation
muscle excitation - arrival of motor neuron stimulation (stage)
- stimulate muscle cells so action potential arrives at terminal
- Voltage-gated calcium channels open
- Calcium comes into cell and triggers exocytosis of Ach
- Ach binds to chemically gated sodium channels
- Sodium moves into cell and depolarizes the membrane (-90mv to +75 mv)
excitation-contraction coupling (stage)
· These events link the action potentials on the sarcolemma to the activation of myofilaments
- Depolarizes membrane down through the T-tubule
- Triggers calcium to release from the terminal cisternae
- Calcium binds to troponin molecules
- Active sites now become open by causing triple myosin to move off the active sites
contraction (stage)
- Myosin-heads are bound to ADP + Pi (energized) (meaning it’s ready for action, “cocked position”)
- Cross-bridge formation starts (actin and myosin finally meet up)
- Myosin-head touches and attaches to the active site (cross-bridge formation)
- Power stroke forms (is what makes the actin move towards the M line)
- Releases Myosin and reactivate process by having ATP molecule bind to the myosin-head and breaks cross-bridge formation
relaxation (stage)
- Stop the signal coming from the somatic neuron, stop releasing Ach
- Ach E comes and breaks down Ach, removing it from the synaptic cleft
- Calcium gets reabsorbed back by the sarcoplasmic reticulum because the membrane is no longer depolarized (calcium is removed or released from the troponin)
- Tropomyosin is going to recover from those actin sites (start covering the actin sites again)
sliding filament theory
muscle develops tension and may shorten
(cross-bridge formation)
(power stroke)
(reactivation)
things that help with the relaxation stage
- Gravity
- Elastic forces (titan + tendons)
- Opposing muscles (contracting other muscles)
length of the contraction depends on:
1. Length of the stimulus at neuromuscular junction (NMJ)
2. Ca2+
3. ATP
Rigor Mortis
muscles contract and stay in that position after a person dies
- ATP doesn’t produce anymore so it stays in the excitation-contraction coupling stage
tension production
tension is the pull or tightness exerted by a shortened sarcomere
internal tension
shortens sarcomere - caused by titan
external tension
sarcolemma
- Linked to one of the proteins (dystrophin)
- When actin is pulled in one direction, the linking proteins transmit that action up to the sarcolemma and pull on it to help the entire muscle fiber to contract at the same time
the amount of tension generated by a muscle fiber is dependent on ___
the resting length of the fiber
the frequency of stimulation
calcium levels
type of fibers
amount of ATP available
temperature, pH, and hydration levels
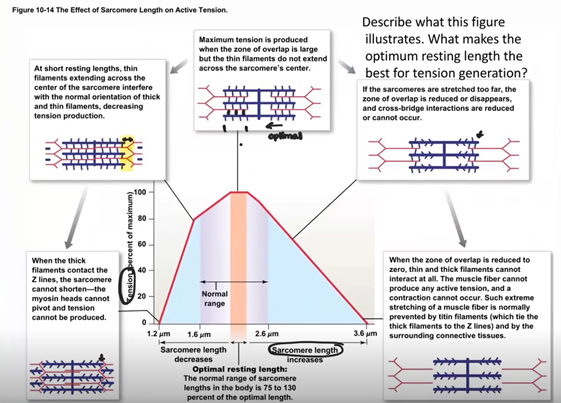
length-tension relationship
Optimal length
Muscle tone
frequency of stimulation
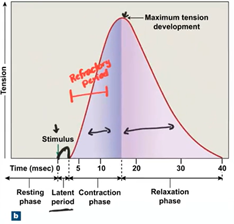
latent period
contraction phase
relaxation phase
refractory period
Like the neurons, muscles require a certain level of stimulation to contract; this is the threshold
At threshold, a single stimulus causes a single quick contraction/relaxation cycle or twitch
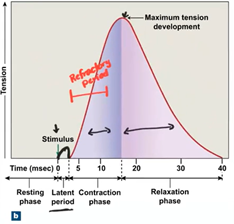
latent period (frequency of stimulation)
a delay of ~2 msec following the stimulus that reflects the time where the action potential sweeps the sarcolemma and T-tubules causing Ca2+ to be released from the SR
contraction phase (frequency of stimulation)
muscle fiber develops tension as cross-bridges form and shortens (~15 msec)
relaxation phase (frequency of stimulation)
Ca2+ quickly reabsorbed into SR; cross-bridges broken and muscle loses tension; returns to resting length (~25 msec)
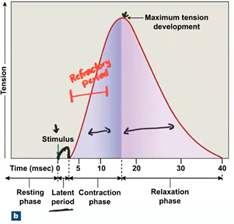
refractory period (frequency of stimulation)
during the first 5 msec of contraction phase, muscle will not respond to a stimulus of any intensity
stimulation frequency
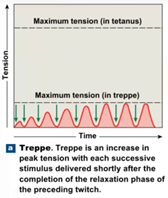
treppe
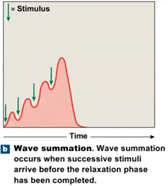
wave summation
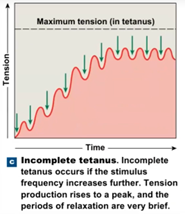
incomplete tetanus
complete tetanus
treppe
muscle fiber still recovers fully between twitches but each builds more tension than the one before
wave summation
Muscle fiber does not completely recover before the next stimulus
incomplete tetanus
muscle fibers relaxes only slightly between stimuli
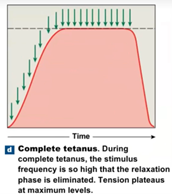
complete tetanus
muscle fibers have no time to relax between stimuli
can lead to muscle damage
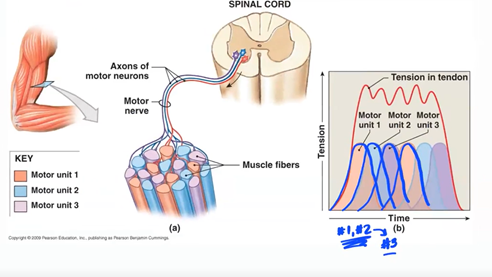
Tension Production in Whole Skeletal Muscles
Fine control (eye) there are 4-6 muscle fibers to each motor neuron
Coarse control (leg muscle) over 1000 muscle fibers to each motor neuron
So how can we generate a stronger and longer muscle contraction?
Increase of frequency of stimulation
Recruitment
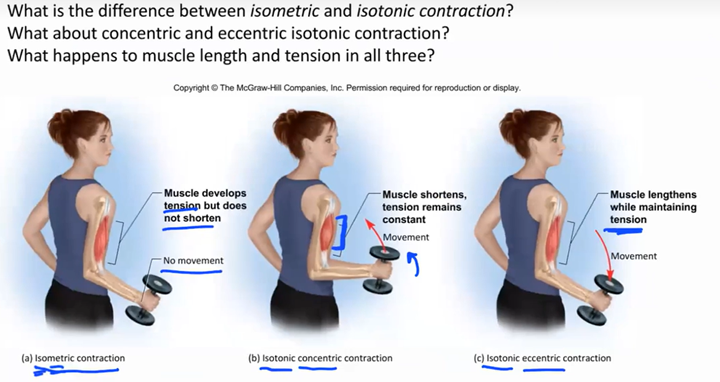
isometric contraction
tension builds (crossbridges formed) but does not overcome resistance so muscle fibers shorten but entire muscle does not
As the internal tension builds to a point where it overcomes the resistance, the muscle now shortens and the box moves
- Same muscle length, no movement
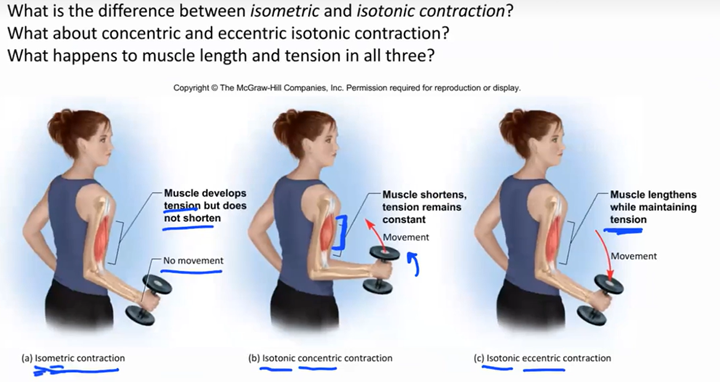
isotonic contraction (movement)
contraction with a change in muscle length but no change in the tension (slightly stronger than resistance)
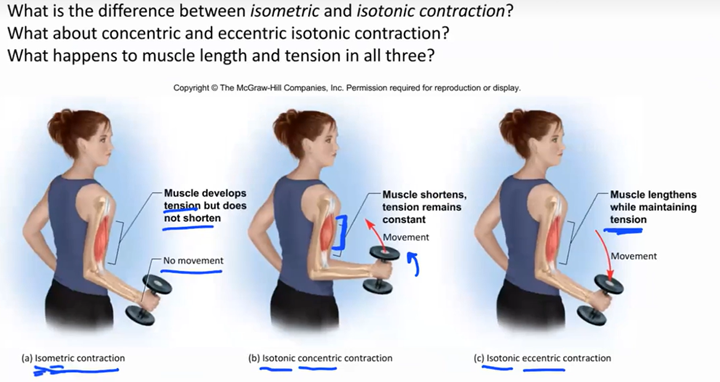
concentric
muscle is shortening with movement
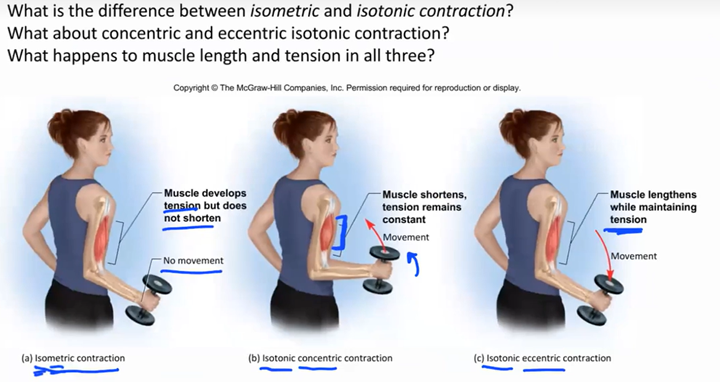
eccentric contraction
muscle is getting longer with movement
Distinguish between acetylcholine, an acetylcholine receptor, and acetylcholinesterase. State where each is found and describe the function it serves.
Acetylcholine (ACh)
Location: Released from the axon terminal of a motor neuron into the synaptic cleft.
Function: A neurotransmitter that binds to receptors on the muscle fiber to trigger muscle contraction.
Acetylcholine Receptor (ACh receptor)
Location: On the motor end plate (sarcolemma of the muscle fiber).
Function: Binds ACh, allowing sodium to enter the muscle cell, initiating an action potential and contraction.
Acetylcholinesterase (AChE)
Location: In the synaptic cleft.
Function: Breaks down ACh after it has bound to the receptor, stopping the signal and ending muscle contraction.
What accounts for the resting membrane potential seen in unstimulated nerve and muscle cells?
The resting membrane potential is due to:
Sodium-Potassium Pump: Actively transports 3 Na+ out and 2 K+ in, creating concentration gradients.
Ion Channels: The membrane is more permeable to K+, so it leaks out, making the inside negative.
Negative Anions: Proteins and anions inside the cell contribute to the negative charge.
This results in a resting membrane potential of around -70 mV.
What is the difference between a resting membrane potential and an action potential?
Resting Membrane Potential: The stable, negative charge across the membrane of an unstimulated cell (typically around -70 mV). It is maintained by ion gradients and the sodium-potassium pump.
Action Potential: A rapid, temporary reversal of the membrane potential (from negative to positive) that occurs when a cell is stimulated. It involves the influx of sodium ions (Na+) and is followed by potassium ions (K+) leaving the cell, leading to electrical signaling.
In short, the resting membrane potential is the cell's "baseline," while the action potential is a rapid change in membrane potential during cell activation.
What change does ACh cause in an ACh receptor? How does this electrically affect the muscle cell?
When acetylcholine (ACh) binds to an ACh receptor on the muscle cell membrane (sarcolemma), it causes the receptor to open ion channels. This allows sodium ions (Na+) to flow into the muscle cell and potassium ions (K+) to flow out, creating a small depolarization of the membrane.
This electrical change generates an action potential in the muscle cell, which then triggers muscle contraction.
How do troponin and tropomyosin regulate the interaction between myosin and actin?
Troponin and tropomyosin regulate the interaction between myosin and actin as follows:
Tropomyosin: At rest, it covers the binding sites on actin where myosin heads attach, preventing contraction.
Troponin: When calcium ions (Ca²⁺) bind to troponin, it causes a conformational change that moves tropomyosin away from the binding sites on actin, allowing myosin to bind to actin and initiate muscle contraction.
Describe the roles played by ATP in the power and recovery strokes of myosin.
Power Stroke:
ATP is hydrolyzed into ADP and Pi (inorganic phosphate) by myosin. This energy release allows myosin to pivot and pull the actin filament toward the center of the sarcomere, generating force and contraction.
Recovery Stroke:
After the power stroke, ATP binds to myosin, causing it to detach from actin. The hydrolysis of ATP into ADP and Pi provides the energy needed for myosin to "reset" to its original position, ready for the next contraction cycle.
What steps are necessary for a contracted muscle to return to its resting length?
For a contracted muscle to return to its resting length, the following steps are necessary:
Cease Nerve Stimulation: The motor neurons stop releasing acetylcholine (ACh), ending the action potential in the muscle.
Calcium Ion Removal: Calcium ions (Ca²⁺) are actively pumped back into the sarcoplasmic reticulum (SR), causing troponin and tropomyosin to cover the actin binding sites again.
Cross-Bridge Detachment: Without calcium, the myosin heads detach from actin, and the muscle stops contracting.
Elastic Recoil: Elastic components of the muscle (like titin and connective tissues) return the muscle to its resting length.
ATP Hydrolysis: ATP binds to myosin, allowing it to reset and prepare for the next contraction cycle.
Why is it important for the transverse tubule to be so closely associated with the terminal cisternae?
The transverse tubules (T-tubules) are closely associated with the terminal cisternae of the sarcoplasmic reticulum to ensure efficient transmission of the action potential into the muscle fiber and rapid release of calcium ions (Ca²⁺).
T-tubules carry the action potential deep into the muscle fiber.
The terminal cisternae store and release Ca²⁺ in response to the action potential.
This close association allows for synchronized muscle contraction, as the rapid calcium release from the terminal cisternae occurs almost simultaneously across the entire muscle fiber.
Without ATP, relaxed muscle cannot contract and a contracted muscle cannot relax. Explain why.
Without ATP, muscles cannot contract or relax due to the following reasons:
Contraction:
ATP is required for myosin to bind to actin and perform the power stroke. Without ATP, myosin heads can't detach from actin after the power stroke, causing a rigor state (as seen in rigor mortis).
Relaxation:
ATP is necessary to pump calcium ions (Ca²⁺) back into the sarcoplasmic reticulum, which stops the contraction signal. Without ATP, calcium stays in the cytoplasm, keeping the muscle contracted.
ATP is also needed for myosin to detach from actin and for the muscle fibers to return to their resting length.
Thus, without ATP, both contraction and relaxation processes are impaired.
What differences would you expect to see between a motor unit where muscular strength is more important than fine control and another motor unit where fine control is more important?
In a motor unit where muscular strength is more important than fine control:
Large motor units: Each motor unit consists of many muscle fibers, leading to stronger contractions.
Fewer motor units: Each motor unit can activate many fibers at once, generating a powerful response.
Example: Leg muscles or back muscles.
In a motor unit where fine control is more important:
Small motor units: Each motor unit consists of only a few muscle fibers, allowing for more precise control.
More motor units: Smaller, more precise control over muscle movement.
Example: Eye muscles or fingers.
Explain why a rising concentration of Ca2+ in the sarcoplasm would enable more myosin0actin cross-bridges to form, and thus result in stronger twitches.
A rising concentration of Ca²⁺ in the sarcoplasm enables more myosin-actin cross-bridges to form because:
Calcium binding to troponin: When Ca²⁺ binds to troponin, it causes a conformational change that moves tropomyosin away from the actin binding sites.
Exposing binding sites: This exposes the myosin-binding sites on the actin filaments, allowing myosin heads to bind to actin and form cross-bridges.
Stronger twitches: More cross-bridges result in more forceful muscle contractions, leading to stronger twitches.
Thus, as Ca²⁺ levels increase, more myosin heads can attach to actin, increasing muscle tension.
State three or more reasons why muscle twitch strength can vary even when stimulus intensity remains constant.
Muscle twitch strength can vary even when stimulus intensity remains constant due to:
Frequency of Stimulation: Higher frequencies of stimulation can lead to temporal summation, where successive twitches build upon each other, resulting in a stronger overall contraction.
Number of Motor Units Activated: The more motor units recruited, the stronger the muscle contraction. Larger motor units with more muscle fibers generate more force.
Muscle Fiber Type: The proportion of fast-twitch (stronger but fatigue quickly) versus slow-twitch fibers (enduring but less forceful) affects the strength of the twitch.
Calcium Ion Availability: If more Ca²⁺ is available in the sarcoplasm, more myosin-actin cross-bridges can form, increasing muscle tension and twitch strength.
Explain the role of tetanus in normal muscle action.
Tetanus in normal muscle action refers to the sustained contraction that results from a high-frequency series of stimuli, preventing the muscle from relaxing between individual twitches. It plays a key role in:
Sustained Force Production: When stimuli are frequent enough, the muscle remains in a continuous contraction, providing steady, powerful force needed for movements like maintaining posture or performing complex actions.
Smooth Movements: Incomplete tetanus (or unfused tetanus) occurs when there’s partial relaxation between stimuli, but the muscle still maintains a smooth and sustained contraction. Complete tetanus occurs when relaxation is entirely prevented, generating maximum tension.
Thus, tetanus allows muscles to generate consistent force, which is essential for most voluntary and involuntary movements.
Describe an everyday activity not involving the arms in which your muscles would switch from isometric to isotonic contraction.
An example of an everyday activity that switches from isometric to isotonic contraction is standing up from a seated position.
Isometric Contraction: Initially, when you prepare to stand, your leg muscles (e.g., quadriceps and glutes) engage in isometric contraction, where they generate force to stabilize your body without changing length.
Isotonic Contraction: As you push yourself up from the seat, your muscles switch to isotonic contraction (specifically concentric contraction), where the muscle fibers shorten, lifting your body into a standing position.
Describe an everyday activity not involving the arms that would involve concentric contraction and one that would involve eccentric contraction.
Here are two examples of everyday activities involving concentric and eccentric contractions:
Concentric Contraction: Climbing stairs
As you lift your body upward to the next step, your quadriceps contract concentrically (muscle shortening) to extend the knee and lift your body.Eccentric Contraction: Descending stairs
When you lower your body to the next step, your quadriceps engage in eccentric contraction (muscle lengthening) to control the descent and prevent you from falling too quickly.