Pharmacology I 8/20/25
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
pharmokinetics
body’s affect on the drug over time
5 basic parameters
absorption
distribution
metabolism
excretion
half-life
pharmacodynamics
drugs effect on the body
pharmacotherapeutics
application of drugs for the treatment and management of diseases
bound drugs
the body will try to achieve an equilibrium, it will become unbound → excreted
free drug
can be metabolized → excreted
can have an active metabolite that can also get excreted
goes to the site of action or stored in tissues
drug process
absorption (if taken orally, for ex)
distributed
metabolism
elimination
lag period
where there isn’t enough medication to produce an affect
minimum effective concentration (MEC)
the onset of drug’s effect (when it starts working, and the beginning of the duration of action)
therapeutic window
between the minimum effective concentration (MEC) for desired response and adverse response
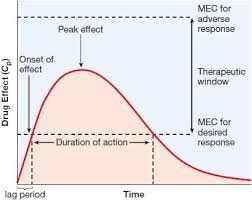
duration of action
length of time the drug produces its therapeutic effect
from the onset of effect → peak effect → the point where it reaches the MEC for desired response again
formulation of drugs
dependent on
barriers drug needs to pass
setting med is administered
urgency of the need for med
stability of the drug
first pass effect
first pass effect
the process where a medication goes through when its taken orally, it’s metabolized typically in liver first before the bloodstream
→ medication can lose potency/effectiveness due to this
routes of drug administeration
po: oral
iv: intravenous
im: intramuscular
sc: subcutanenous
(all except PO are parenteral)
parental administration
any routes of administration that do NOT involve drug absorption via the GI tract (IV, intramuscular, subcutaneous, and transdermal routes)
oral
absorption pattern: variable
advantages: safest and common, convenient, economical
disadvantages: limited absorption of drugs, food can affect, depends on patient compliance, drugs may be metabolized before absorption
intravenous (IV)
absorption not required
advantages: immediate effects, ideal if dose is high volume, good for emergency
disadvantages: inaccessible unless in clinical setting, must be slowly injected
subcutaneous
absorption pattern: depends on drug diluents. aqueous solution is fast, but depot preparation is slow
advantages: good for slow release
disadvantages: drug can be irritation, not good for large volumes
intramuscular
absorption pattern: aqueous solution is fast, depot preparation is slow
advantages: good for moderate amount
disadvantages: can be painful, can cause ___ hemorrhage
DO RECTAL, INHALATION, SUBLINGUAL PG 14
drug absorption
influenced by
route of administration
blood flow
surface area available
solubility
drug-drug interactions
pH
drug concentration (sometimes)
transdermal
absorption pattern: slow and sustained
advantages: bypasses first-pass effect, convenient, good for lipophilic drugs, ideal for drugs quickly eliminated by body
disadvantages: patient allergies, drug must be highly lipophilic, small daily doses
passive diffusion
molecules move down to the concentration gradient
facilitated diffusion
carrier proteins allow drug molecules to piggy-back through the membrane
can become saturated
can be inhibited by competitive compounds
active transport
energy dependent
specific carrier proteins can move drug molecules against concentration gradient
can become saturated
may be competitively inhibited by other cotransported substances
endocytosis
used for large molecules
the membrane engulfs the molecule and then pinches off the drug filled vesicles
passive diffusion
no cellular energy used
drugs move from high → low concentration
stops when concentration is equal
active transport
requires energy from hydrolysis of ATP to move drugs across membrane
drugs move against concentration gradient
drugs are structurally similar to naturally occurring metabolites may need this
slow absorption
oral, IM, subcutaneously
fast absorption
IV, inhalation, sublingual
increased blood flow
increased absorption
decreased surface area
decreased absorption
drug distribution
process where drug leaves the bloodstream and enters the interstitium of tissue’s cells
depends on
ability to permeate capillaries
vascularity of tissues
ability to bind to plasma proteins/tissue protein
fat or water soluble characteristics
drug dissolution
GI tract environment
volume of distribution
amount of drug in the body related to plasma concentration
heart, liver, kidneys
drugs are distributed to _____ ____ ___
skin, muscle, fat
drugs distribute slow to ____ ___ ___
lipid soluble
_____ drugs easily cross through cell membranes including blood brain barrier
water soluble
____ drugs can NOT pass easily through cell membranes
blood-brain barrier
diffusion barrier, which impedes influx of most compounds from blood to brain
ionized molecules can’t enter brain due to structural modifications
non-ionized molecules not bound to plasma proteins can enter brain because they are lipid soluble
liver
enzymes responsible for most oxidative reactions of drugs are in cytochrome p450 system
concentration of blood in bloodstream lowered by first-pass effect and induction/inhibition of drug metabolism
cytochromes p450 (CYPs)
constitute the major enzyme family capable of catalyzing the oxidative biotransformation of most drugs
primary metabolism sites
liver, kidney, biliary tract
prodrug
an inactive/less active drug is “metabolized” into a more active drug
(and an active drug can “metabolize” to less active one)
drug elimination
excretion: removal of waste substances from body fluids
kidney excretion (glomerular filtration, proximal tubular secretion, etc)
clearance: rate of elimination of substances from blood
renal clearance: total amount of drug excreted over time
creatinine clearance (crcl)
indicator for GFR (glomerular filtration rate) and renal function
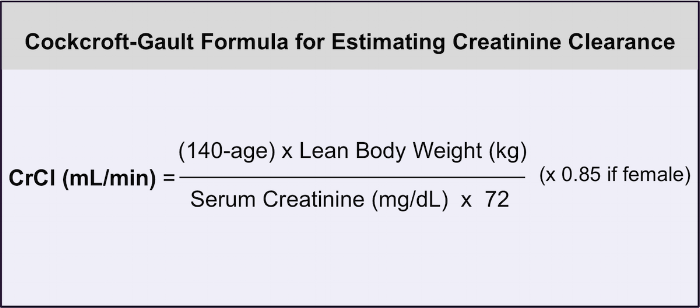
creatinine
comes from skeletal muscle creatine phosphate
most people form same amount everyday
factors influence CrCl
gender
age
weight
height
serum creatinine
half-life
time for a drug CONCENTRATION to fall to one half of its original concentration
measure of how long it takes for half of the drug to disappear from bloodstream
helps determine dosing intervals and “steady state”
six half-life rule
for the concentration of a med to reach a point where it stops causing any effects (basically once it reaches 6 half lives, the med is as good as gone)
onset of action
time interval between time the drug is administered and when the therapeutic effect begins
peak
CONCENTRATION when absorption rate and elimination rate are at equilibrium. not necessarily the peak therapeutic response
drug bioavailability
ability of drug to reach systemic circulation after oral dosage
good indication that amt of med is absorbed
drugs with low oral bioavailability are poorly absorbed in GI tract or partially metabolized by liver