Lecture 31-34 (gastrointestinal system)
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
What is the major function of the digestive system?
to transfer nutrients from the food we eat into our body to be used as fuel and building blocks
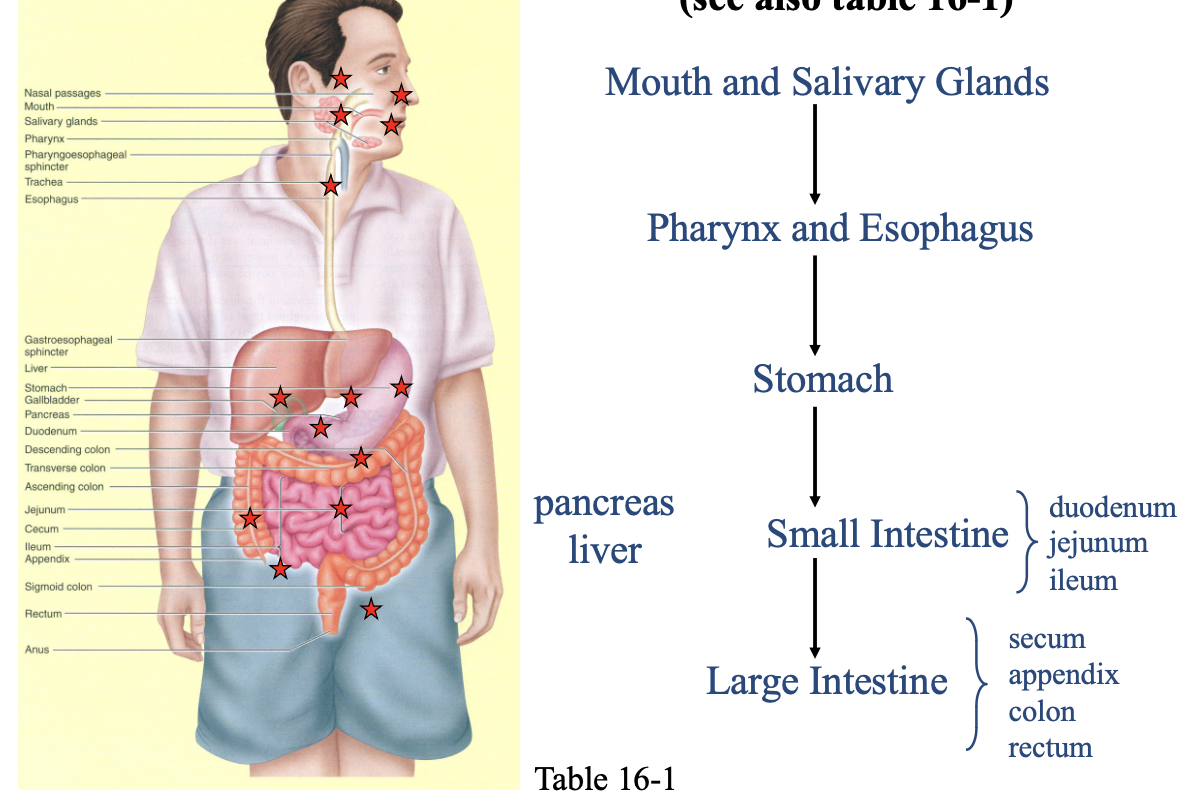
Overview of the Digestive Organs:
mouth and salivary glands
pharynx and esophagus
stomach
small intestine
large intestine
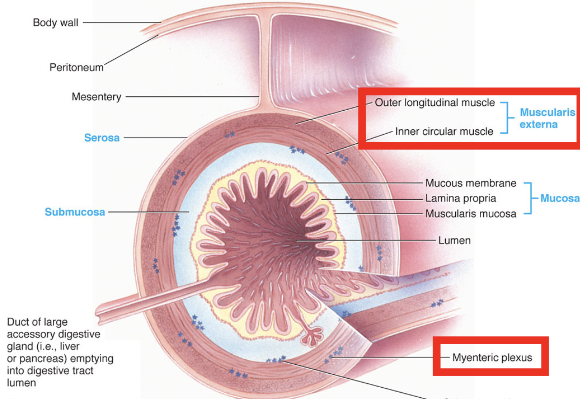
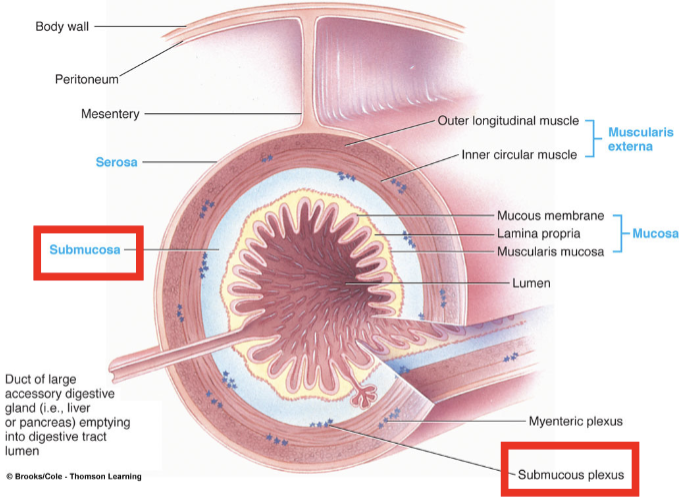
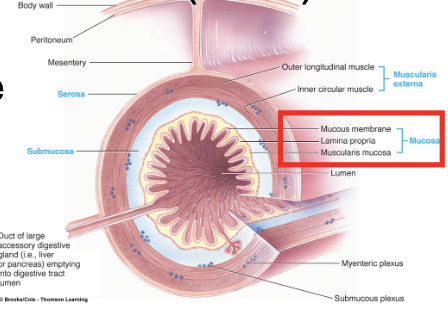
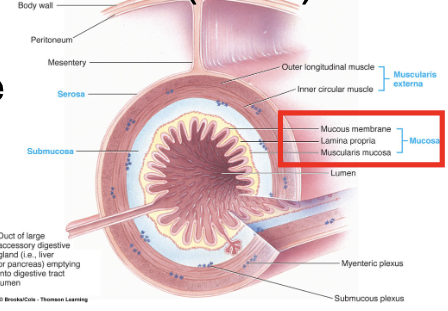
What is the general structure of the digestive tract wall?
made up of four major tissue layer
serosa
muscularis externa
submucosa
mucosa
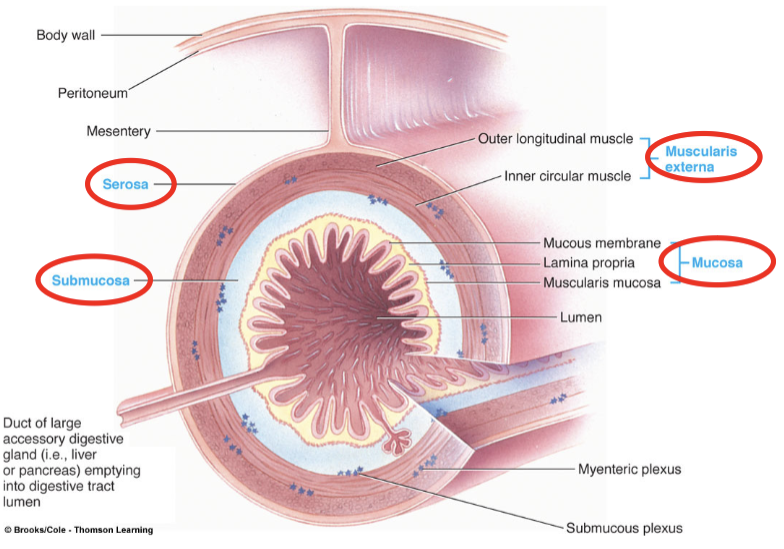
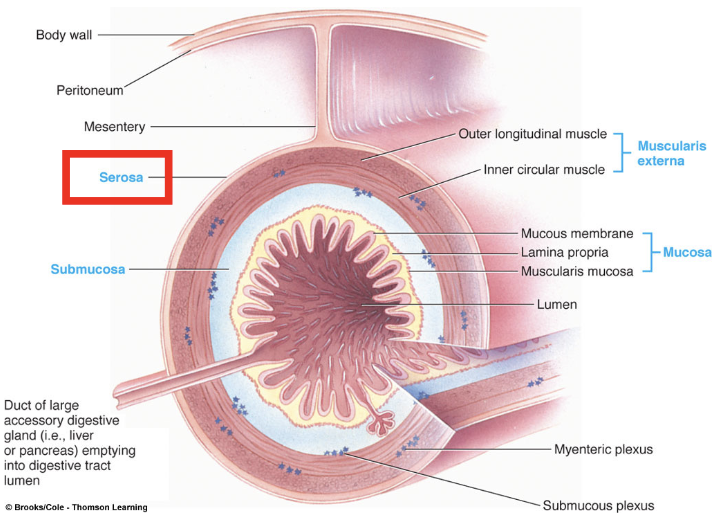
Serosa:
provide a protective outer layer and to secrete serous fluid (lubricates), which reduces friction between digestive organs and surrounding structures
allows freedom for mixing and propulsive movements
continuous with mesentery throughout much of the tract
Muscularis Externa:
major smooth muscle coat of digestive tube where contractile activity produces propulsive and mixing movements
Usually two layers
Inner circular layer → Contraction decreases diameter of lumen
Outer longitudinal layer → Contraction shortens the tube
myenteric plexus
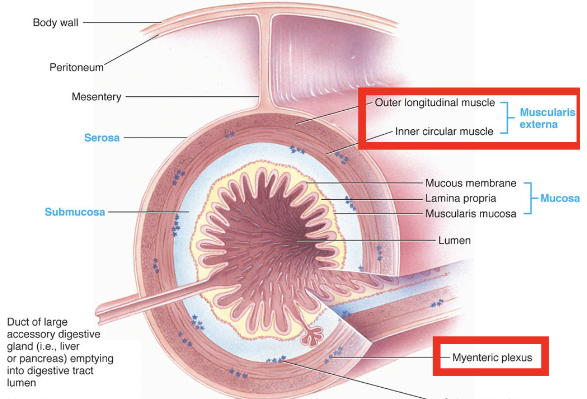
Myenteric plexus:
is part of the enteric nervous system that controls and coordinates muscle contractions (peristalsis) to propel food through the digestive tract
increases overall gut tone and the strength/speed of contractions
provides motor innervation to the muscular layers of the digestive tract
in-between muscle layers
Submucosa:
providing support, elasticity, and nourishment via its blood vessels, lymphatics, and nerves, facilitating nutrient absorption, glandular secretion (mucus, enzymes, electrolytes), and regulating muscle activity (peristalsis) through its nerve network
acts as a structural scaffold, joining the mucosa to the muscle, and plays a key role in sensing stretch and initiating pain signals
contains submucosal plexus nerve network part of the enteric nervous system
Mucosa:
inner lining responsible for protection, secretion, and absorption, acting as a critical barrier against pathogens and toxins while secreting mucus, enzymes, and hormones, and facilitating nutrient uptake through its folded structure that vastly increases surface area
epithelial layer
lamina propia
muscularis mucosa
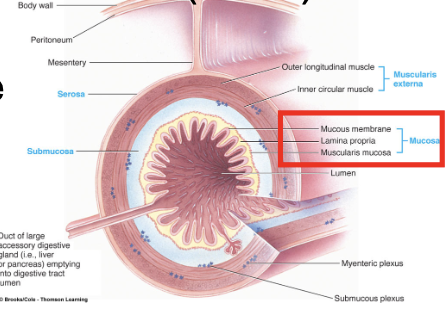
Epithelial layer:
cells modified for secretion and absorption
contains exocrine gland cells → secrete digestive juices, mucus, enzymes into lumen
contains endocrine gland cells → secrete gastrointestinal hormones into capillaries
Lamina propia:
loose connective tissue
small blood vessels, lymphatics, and enteric neurons
contains gut-associated lymphoid tissue (GALT)
True or False: The lumen of the gastrointestinal tract is continuous with the external environment.
True
Why is the lumen being continuous with the external environment important?
pH in the stomach can fall as low as 2 where inside the body the range of pH that is compatible with life = 6.8 - 8.0 (homeostatic range is 7.35 - 7.45)
Harsh Enzymes that hydrolyze food could destroy the body’s own tissues
therefore enzymes are synthesized in an inactive form and are activated when they reach the lumen
Millions of microorganisms inhabit the GI-tract, and these could be lethal if they entered the body proper
What is the process of the digestive system?
ingestion, chewing, swallowing, defecation
secretion
digestion
absorption
What is the purpose of ingestion, chewing, swallowing, defecation?
transfers food into the digestive tract via the mouth
skeletal muscle → voluntary
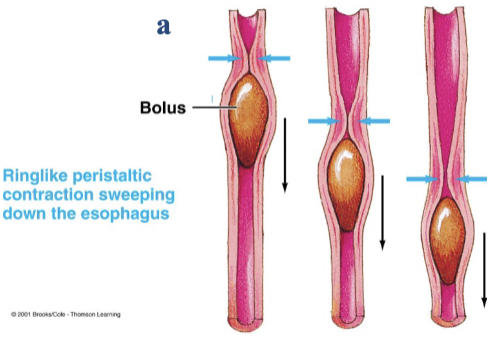
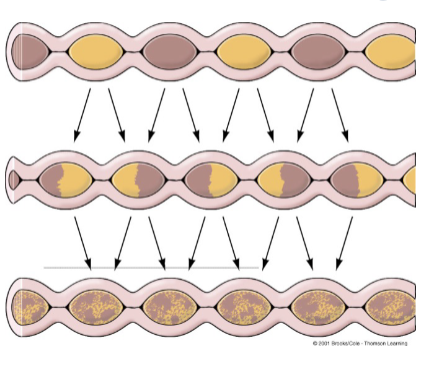
Digestive motility:
muscular contractions that mix and move forward the contents within the tract, facilitating later steps in the digestive process
smooth muscle → involuntary
propulsive movements
mixing movements
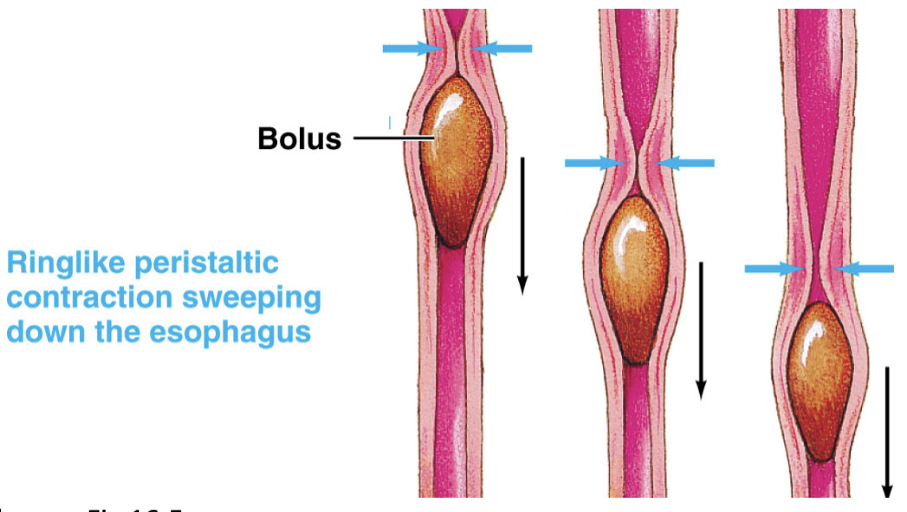
Propulsive movements (peristalsis):
move the contents forward through the digestive tract
happens in the esophagus and when you defecate (large intestine)
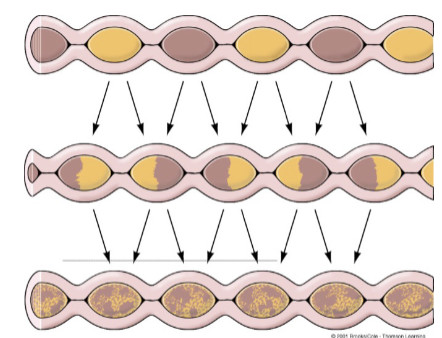
Mixing movements (segmentation):
happens mainly in the stomach + small intestine and serves 3 purposes
aid digestion by mixing food with digestive juices
facilitate absorption by exposing food to absorbing surfaces
forward movement (slow and non-linear)
Exocrine secretion:
digestive juices are secreted into the lumen by exocrine glands upon appropriate neuronal or hormonal stimulation
secretions contain enzymes, acids, buffers, electrolytes, and water that
promote digestion
adjust tonicity
provide lubrication for better movement throughout the tract
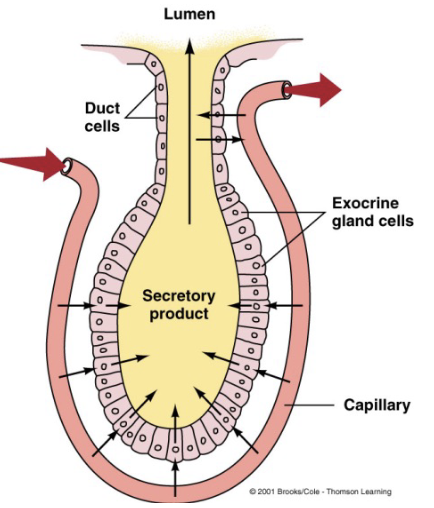
Endocrine secretion:
gut hormones are secreted into the blood by endocrine glands upon appropriate neuronal or nutritional stimulation
gut hormones are chemical messengers released into circulation and act on receptors in distal locations to regulate motility, pancreatic secretions, and other digestive tract (and non-digestive tract) functions
Digestion:
accomplishes the breakdown of structurally complex foodstuffs into smaller, and eventually absorbable units
chemical
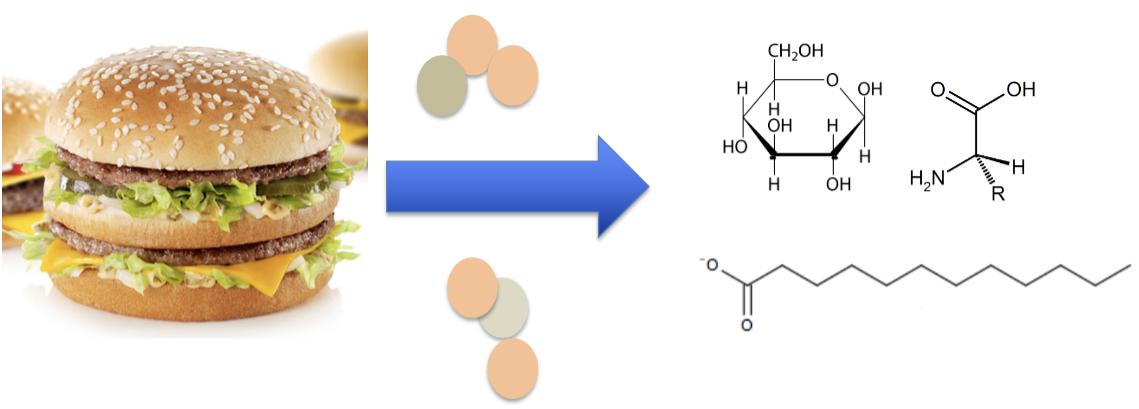
Chemical digestion:
enzymatic hydrolysis of carbohydrates, proteins, and fats into absorbable units
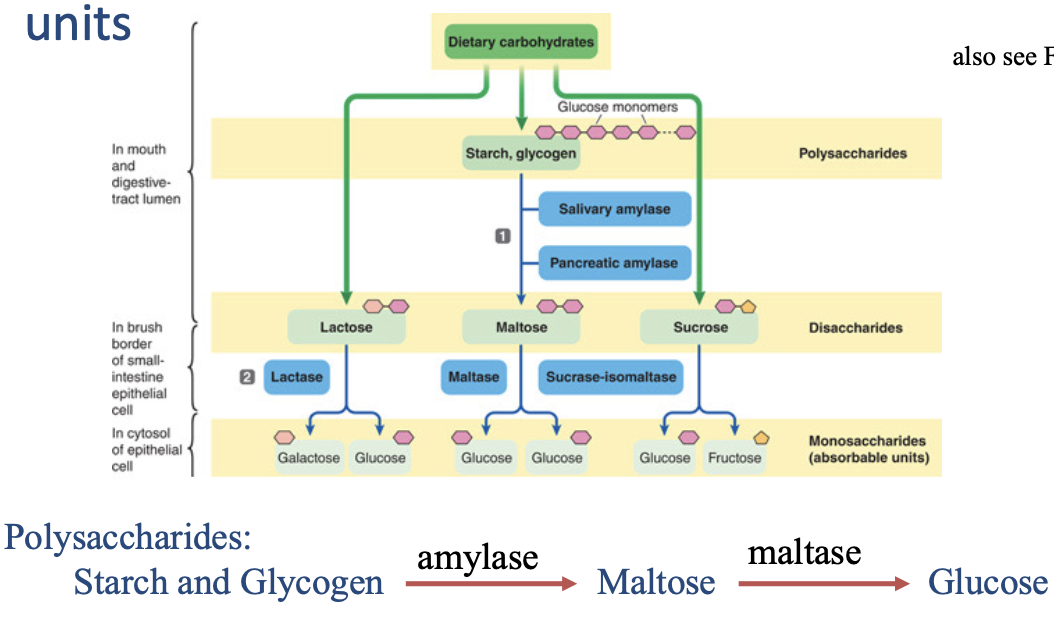
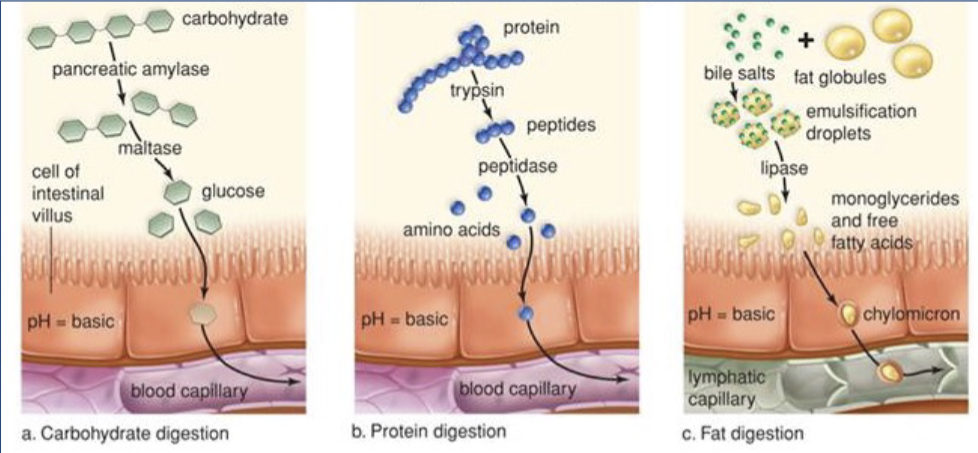
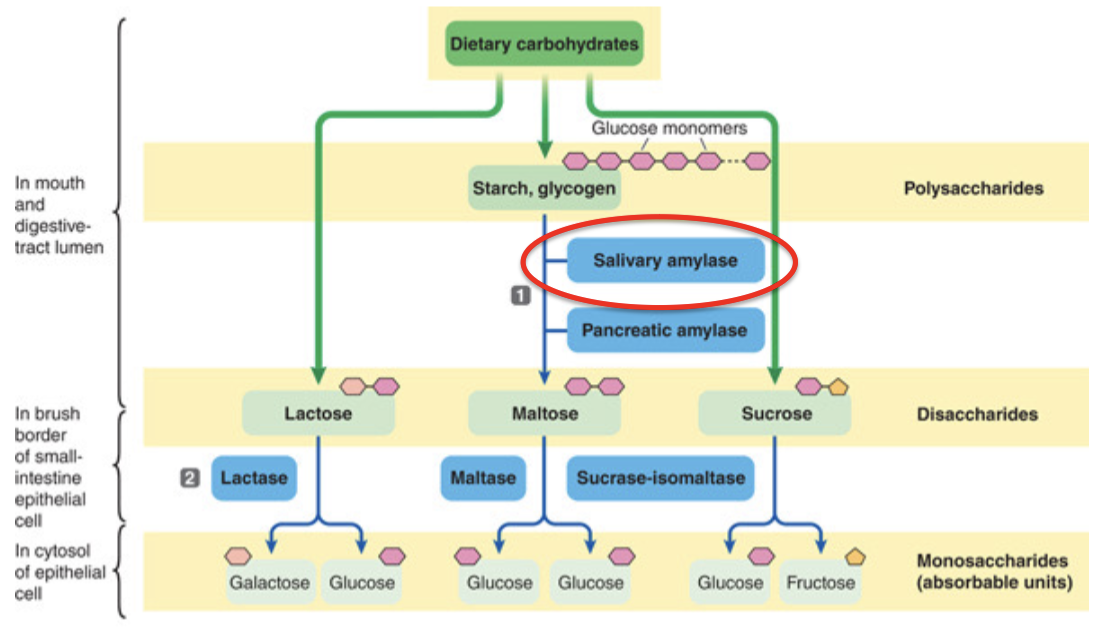
Chemical digestion of carbohydrates:
complex carbohydrates broken down by 1) amylase into disaccharides and then 2) set of enzymes into monosaccharides
only absorb glucose
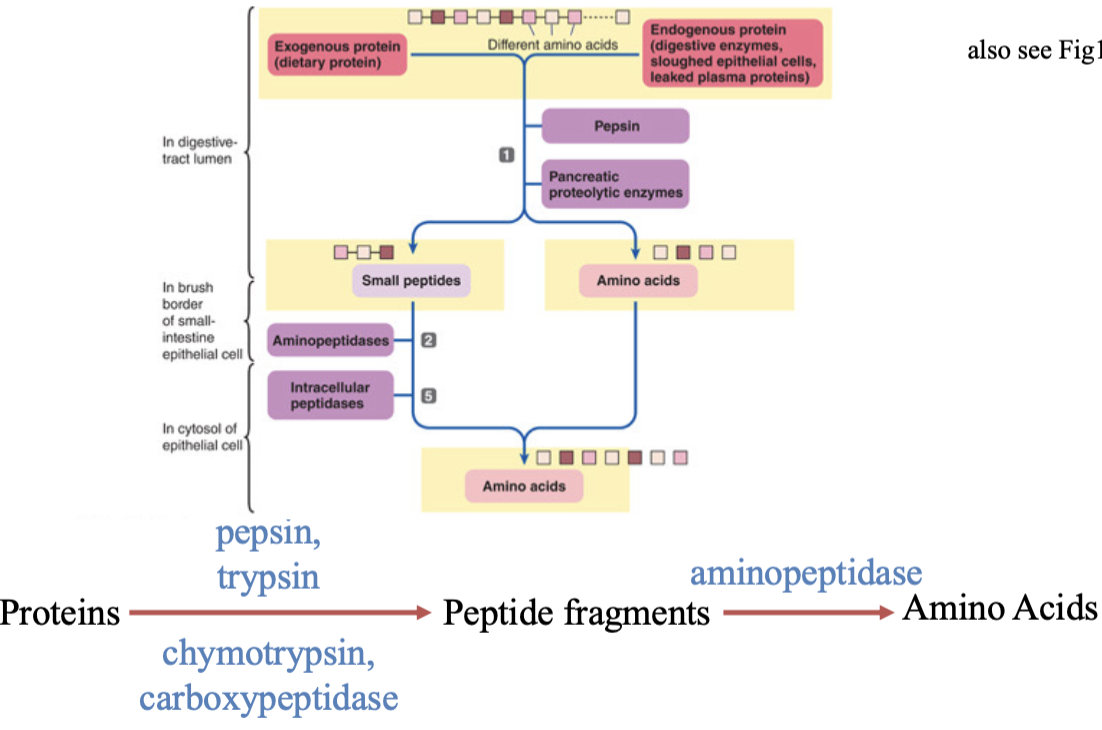
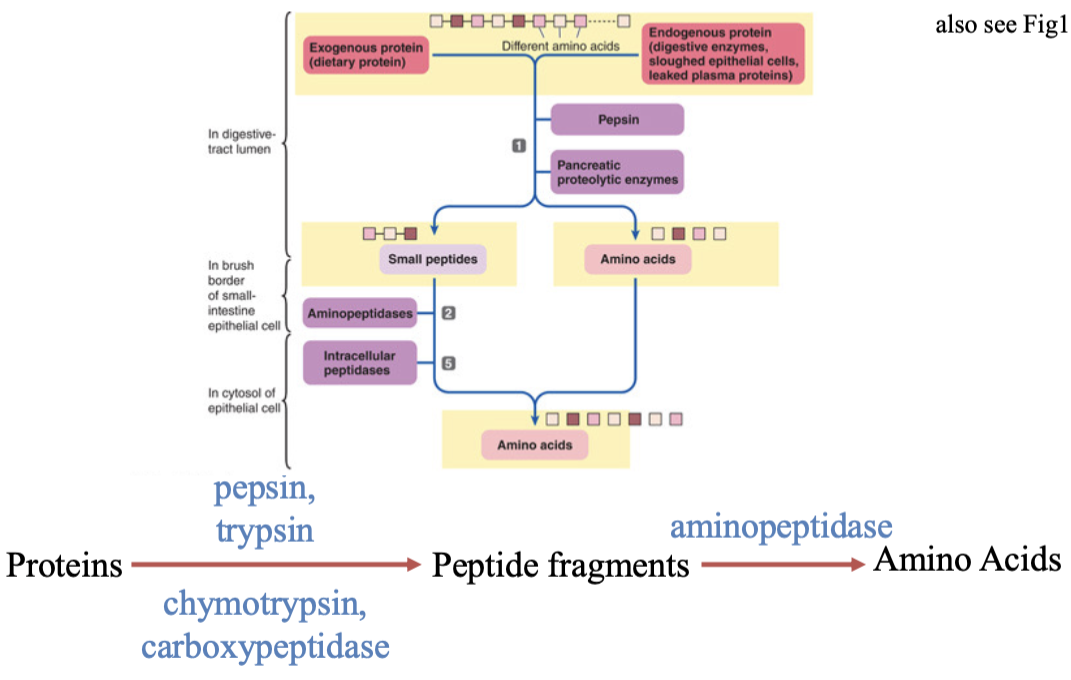
Chemical digestion of proteins:
each enzymes chops bonds between proteins to make smaller fragments of amino acids
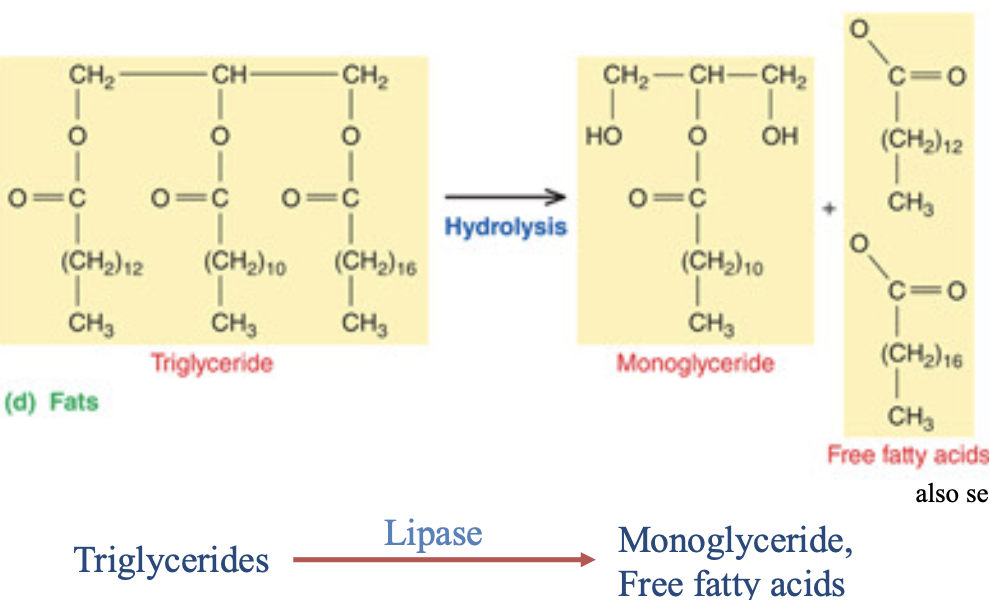
Chemical digestion of fats:
chopping fatty acid tails to form three free fatty acids
Absorption:
the transfer of small absorbable units along with water, vitamins, and electrolytes from the lumen into the blood or lymph
why our blood sugar goes up after a meal
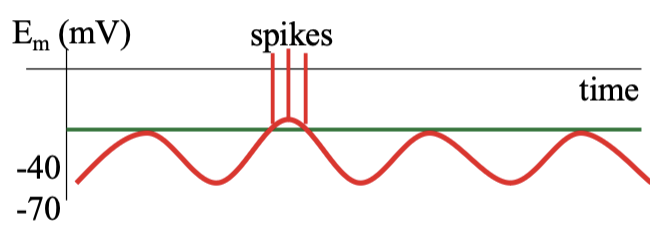
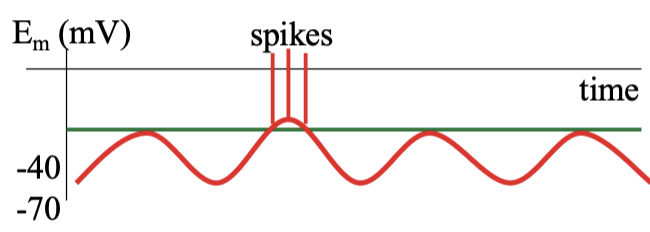
Basic electrical rhythm (BER):
creates a fluctuating potential that allows stronger "spike potentials" to trigger actual muscle spasms, coordinating movements like peristalsis and segmentation, with frequencies varying along the gut
sets the rhythm and frequency for gut contractions, but usually doesn't cause them directly
membrane potential of pacemaker cells in the stomach → interstitial cells of Cajal
What happens when no food is in the lumen of digestive tract?
the membrane potential of pacemaker cells (ICC) oscillate at 3-5 times per sec (3-5 Hz)
ICCs in the small intestine depolarize more frequently (8-11 Hz) → the BER in the small intestine
these depolarizations spread thru gap junctions to smooth muscle cells, then signal propagated through the tract by the enteric nervous system
however, these depolarizations exceed spike threshold only 10-15 times per day → the migrating motility complex
Migrating motility complex:
triggers contractions that are frequent enough to “sweep” residual contents from the stomach & small intestine to the large intestine
triggered by hormone motilin → extrinsic regulation
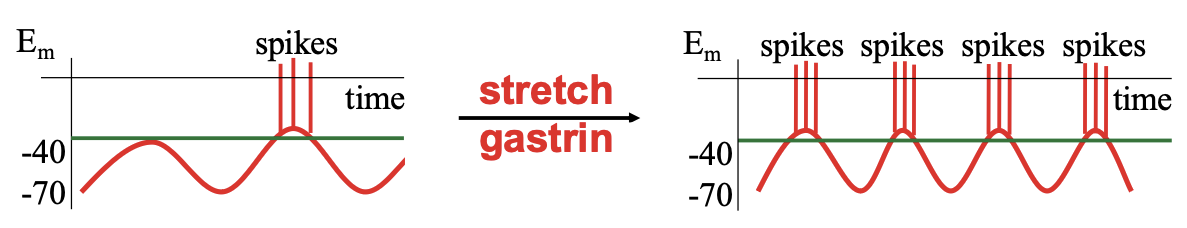
What happens with food in the lumen?
stretch and gastrin (hormone induced by protein in the stomach) activate neural circuits that increase the amplitude & frequency of the basic electrical rhythm (BER) depolarizations
when these depolarizations exceed spike threshold (approx -35 mV), the smooth muscles spike & therefore contract
stretch & gastrin thereby increase digestive tract motility
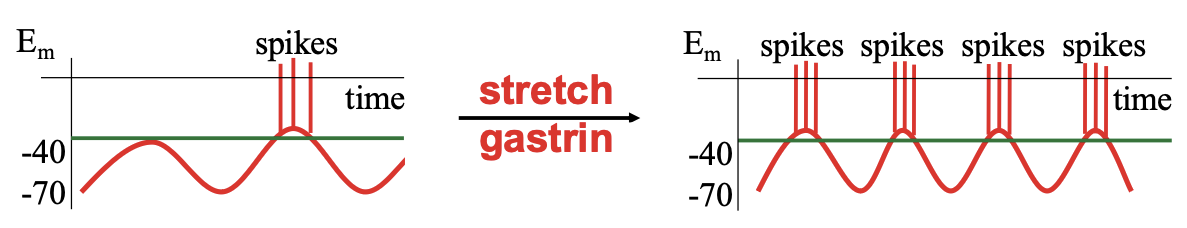
What else can move the ICCs below threshold, inhibit motility signal, or act directly on muscle cells?
certain hormones, intrinsic nerve reflexes, or sympathetic output move ICCs below threshold and inhibit motility signal, or act directly on muscle cells themselves
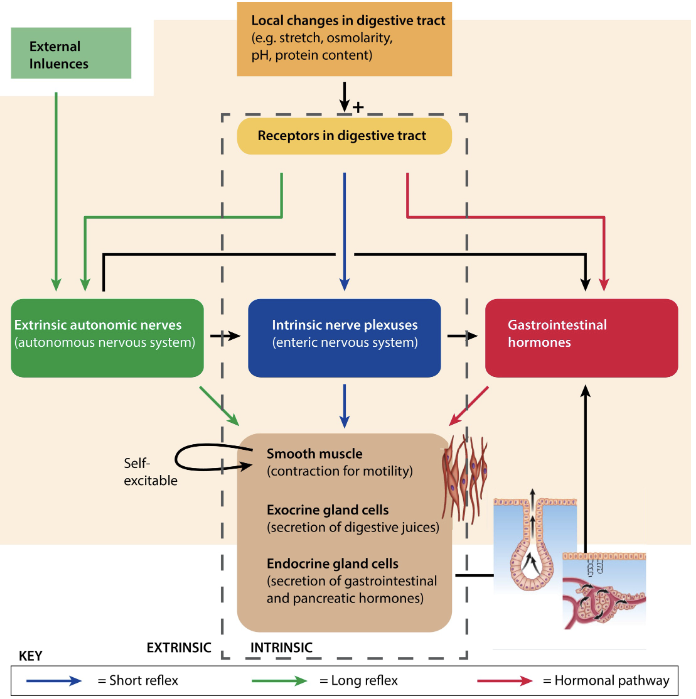
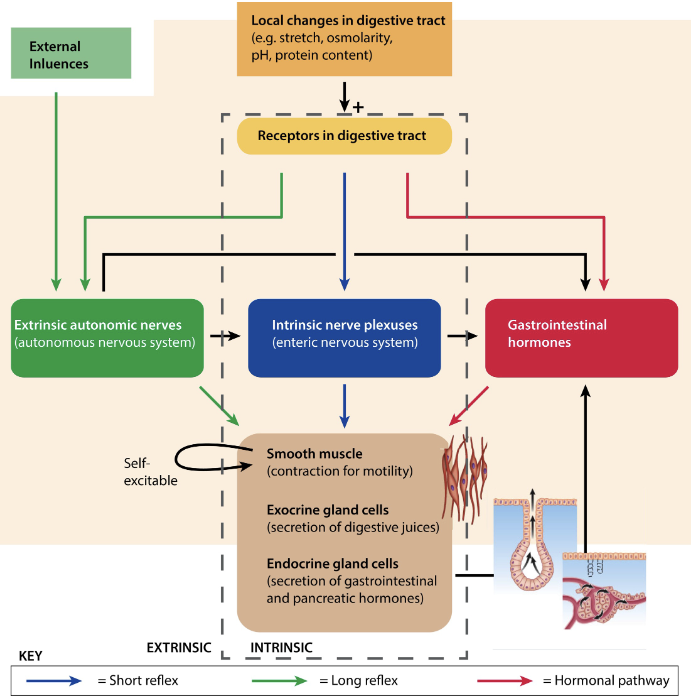
What are intrinsic factors controlling digestive system functions?
autonomous smooth muscle cells
interstitial cells of Cajal (ICC)
enteric nervous system
Autonomous smooth muscle cells:
connected by gap junctions, thereby forming a functional syncytium
single-unit smooth muscle
Interstitial cells of Cajal (ICC):
act as pacesetter cells and generate slow-wave potentials (Basic Electrical Rhythm; BER)
If threshold is reached and action potentials are triggered, then the whole muscle sheet contracts as a unit
Enteric nervous system:
vast network of neurons in the gut wall controlling digestion (motility, secretion, blood flow) autonomously, yet communicating bidirectionally with the central nervous system (CNS) via the gut-brain axis
coordinates local activity within the digestive tract
myenteric + submucosal nerve plexuses
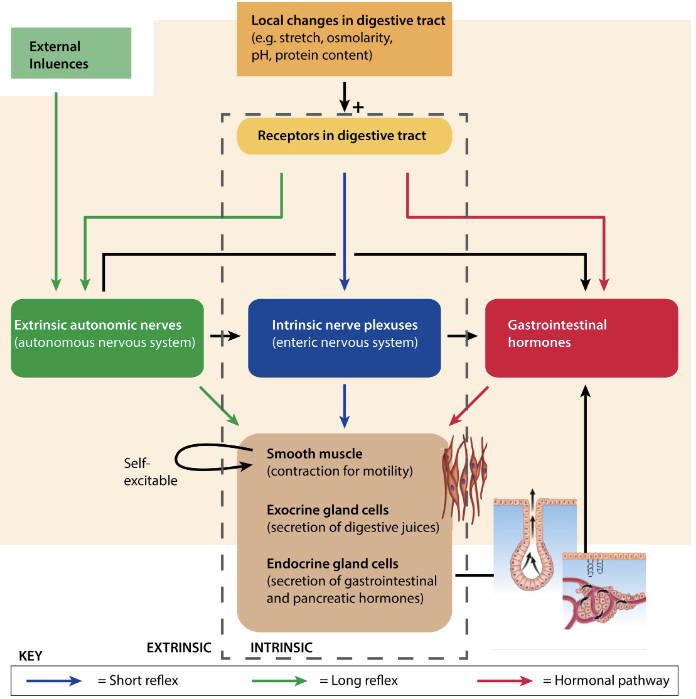
What are the functions of intrinsic factors controlling digestive system?
refers to extrinsic nerves and gastrointestinal hormones
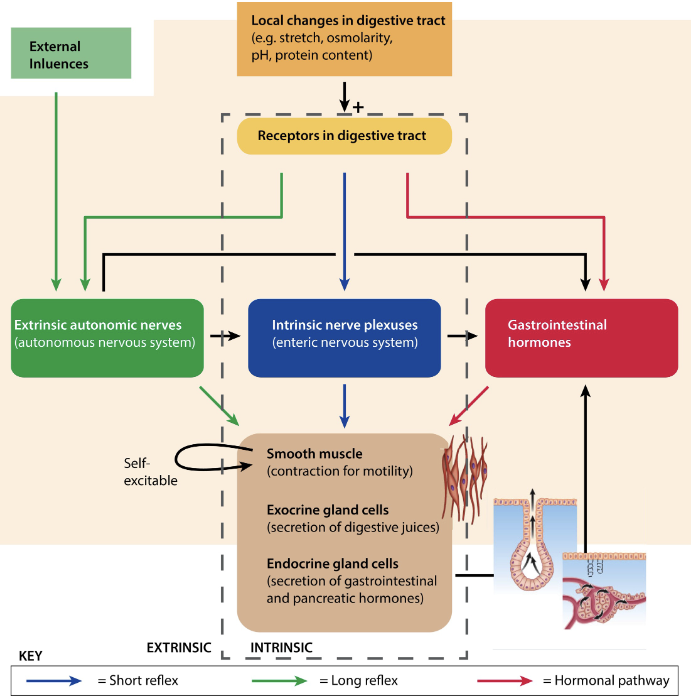
Extrinsic nerves:
originate from outside the digestive system from both the sympathetic and parasympathetic branch where they influence motility and secretion by:
Modifying activity of the enteric nervous system
altering gastric hormone secretion
acting directly on smooth muscle and glands
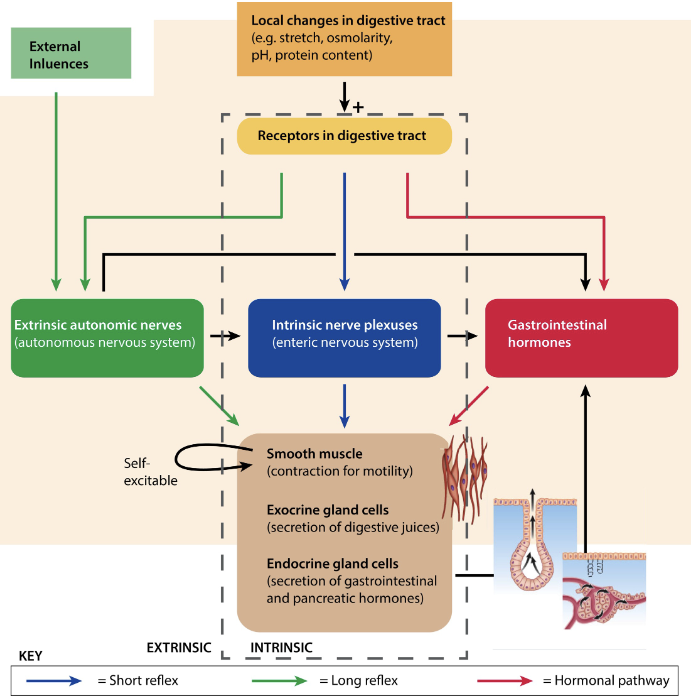
Gastrointestinal hormones:
long-range chemical messengers secreted into blood and act on receptors in distal locations to regulate digestive tract (and non-digestive tract) functions
Lips and Tongue:
contain food in mouth and guide food during chewing and swallowing
Teeth:
begin mechanical breakdown by chewing of food
Palate:
roof of oral cavity from nasal passage
allows chewing and breathing to occur simultaneously
Uvula:
soft tissue that hangs from the rear of the mouth and seals off nasal passage during swallowing
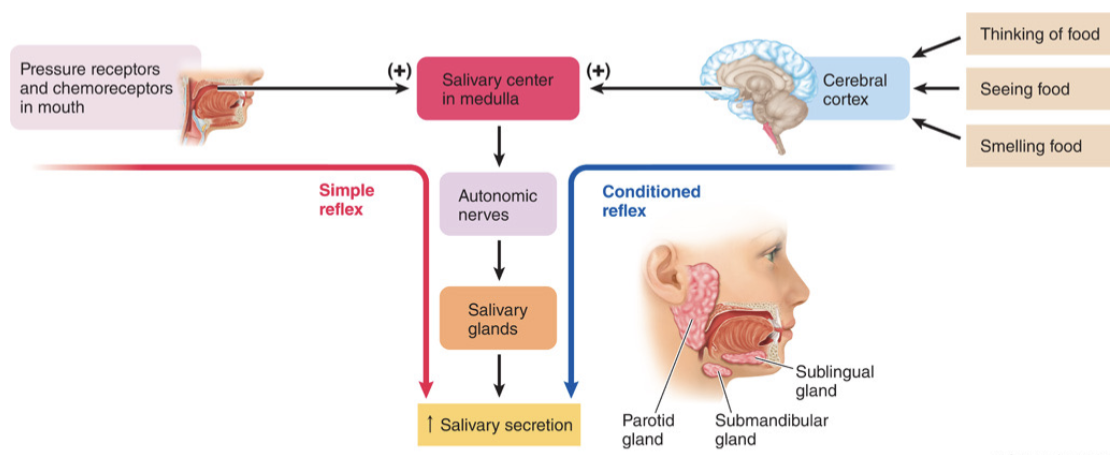
Salivary glands:
made up of 3 gland and secrete saliva in response to autonomic stimulation
sublingual
submandibular
parotid
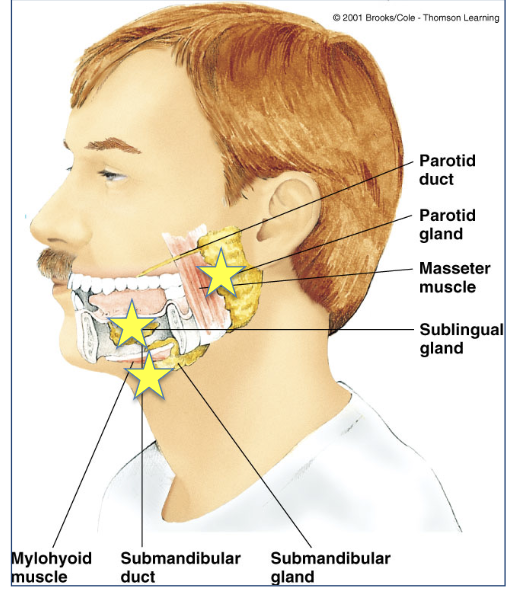
What does saliva contain?
mucus to moisten food and lubricate
lysozyme to lyse bacteria
Bicarbonate buffers which neutralize acids
amylase, which begins chemical digestion of carbohydrates by cleaving polysaccharides into maltose
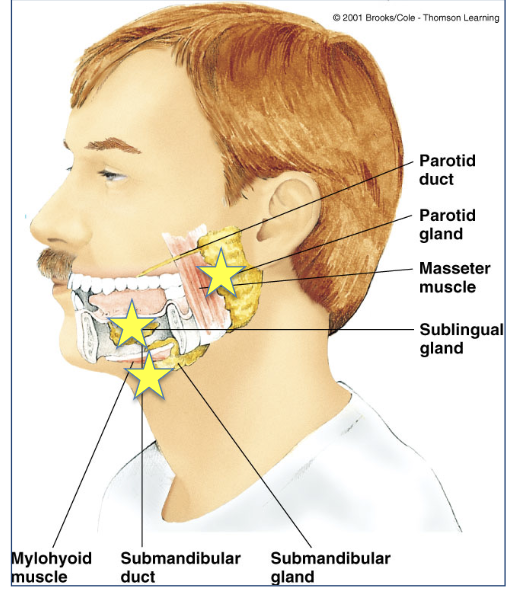
Mouth and Salivary Glands:
describes how salivation works
simple or conditioned reflexes
Where does the digestion of carbohydrates (polysaccharides) start?
starts in the mouth
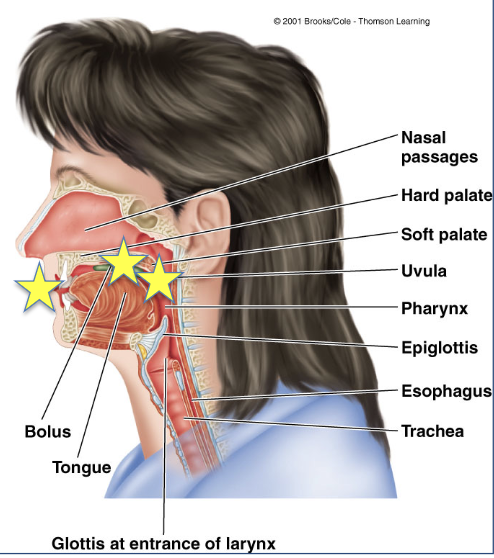
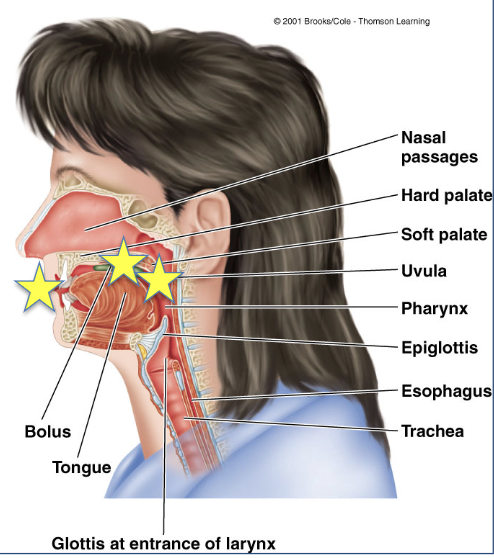
Swallowing:
refers to the entire process of moving food from the mouth, through pharynx
and esophagus, to the stomach in two stages
is a sequentially programmed all-or-none reflex, initiated when bolus is voluntarily forced by tongue to rear of mouth into pharynx
can be initiated voluntarily but cannot be stopped once it has begun
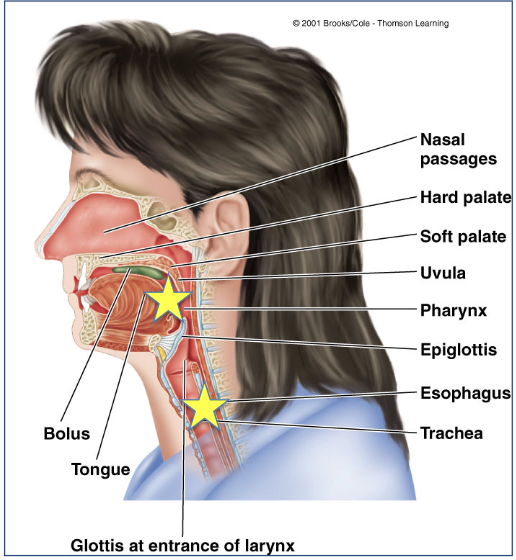
What are the two stages of swallowing?
oropharyngial stage → when the food is still in your mouth entering the pharynx
esophageal stage → when food is in the esophagus
True or False: In the esophageal stage, peristaltic (propulsive) waves move bolus (food) into the stomach.
True, at the end of the oropharyngeal stage, the pharyngoesophageal sphincter closes & breathing resumes
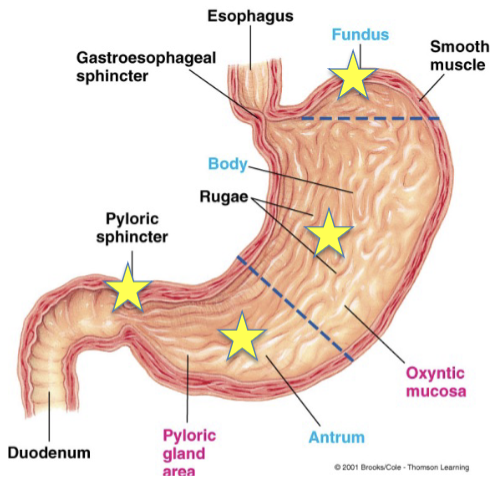
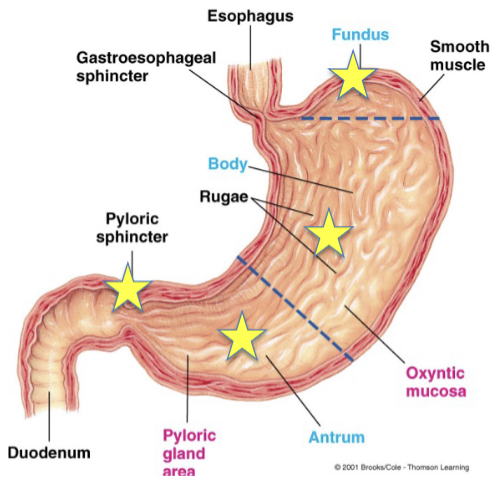
Stomach:
J-shaped chamber located between the esophagus and the small intestine
thick layer of smooth muscle connected to small intestine by pyloric sphincter and is a key regulator of gastric emptying
fundus → located above the gastroesophageal sphincter
body → middle
antrum → bottom
Main functions of the stomach:
store ingested food until it can be emptied into small intestine
occurs in the body of the stomach
create gastric secretions → including HCl and enzymes that begin chemical digestion of protein
gastric motility converts pulverized food to chyme → a thick liquid mixture of pulverized food and gastric secretions
Gastric filling:
gastric volume can expand ~20-fold during a meal, by expansion/ flattening of deep folds
expansion of gastric volume is a vagally-mediated process called receptive relaxation
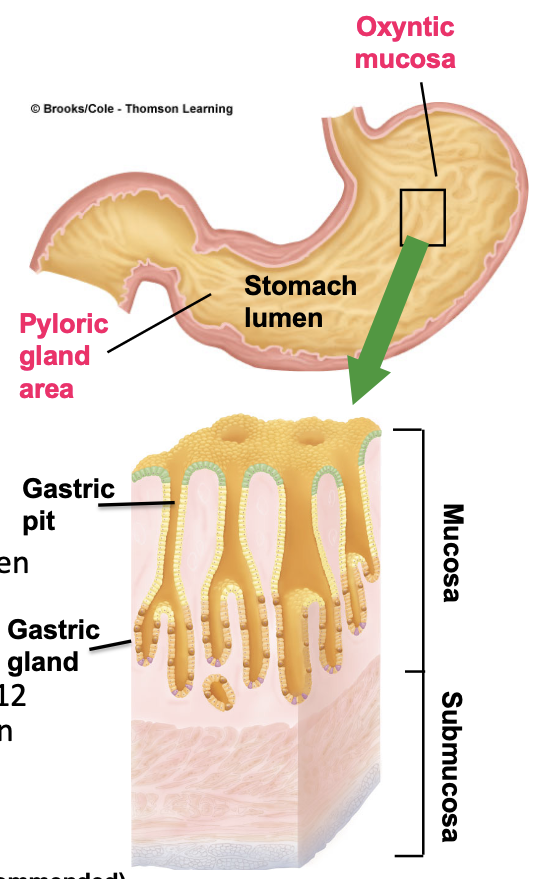
What are the two distinct areas of secretory gastric mucosa?
oxyntic mucosa (body and fundus) and pyloric gland area (antrum)
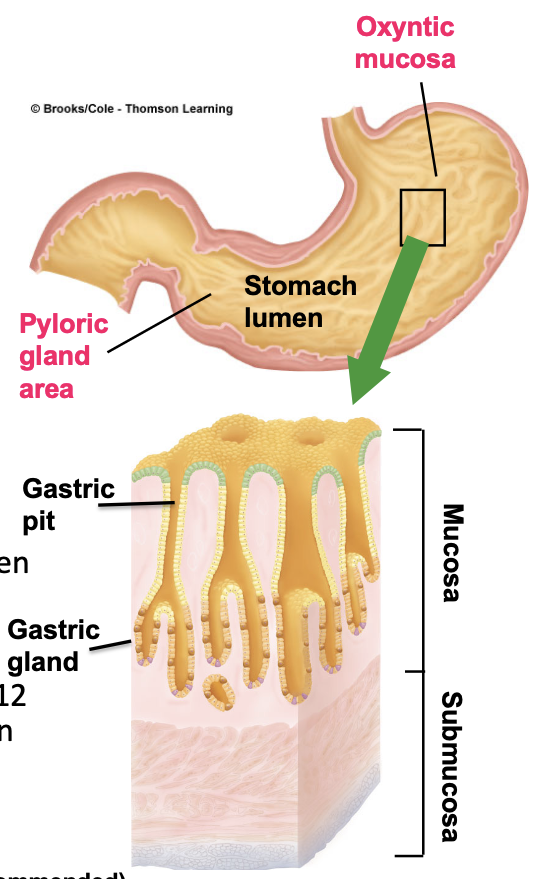
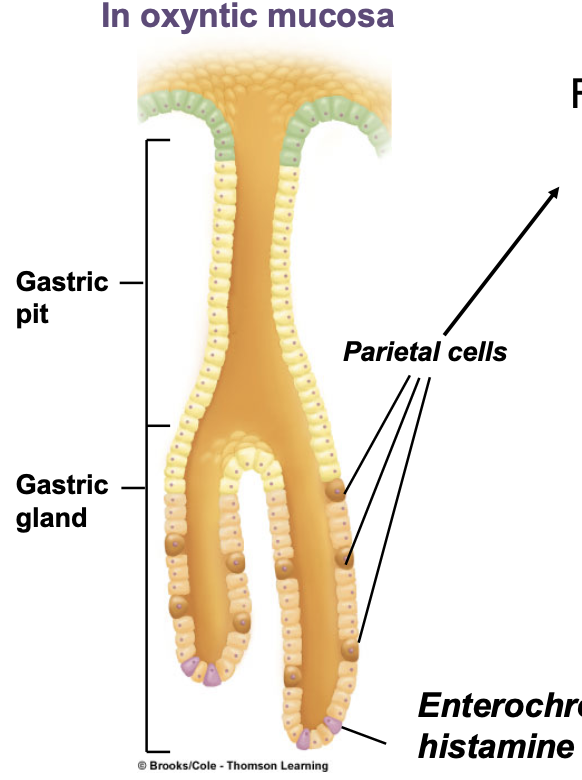
In oxyntic mucosa, what are the 3 types of gastric EXOCRINE secretory cells, associated with gastric pits?
Mucous cells → secrete thin, watery mucus
Chief cells → secrete enzyme precursor, pepsinogen
Parietal (oxyntic) cells secrete HCl and intrinsic factor (essential for normal function of red blood cells)
HCl activates what in the stomach?
activates pepsinogen in the lumen, protecting stomach from itself
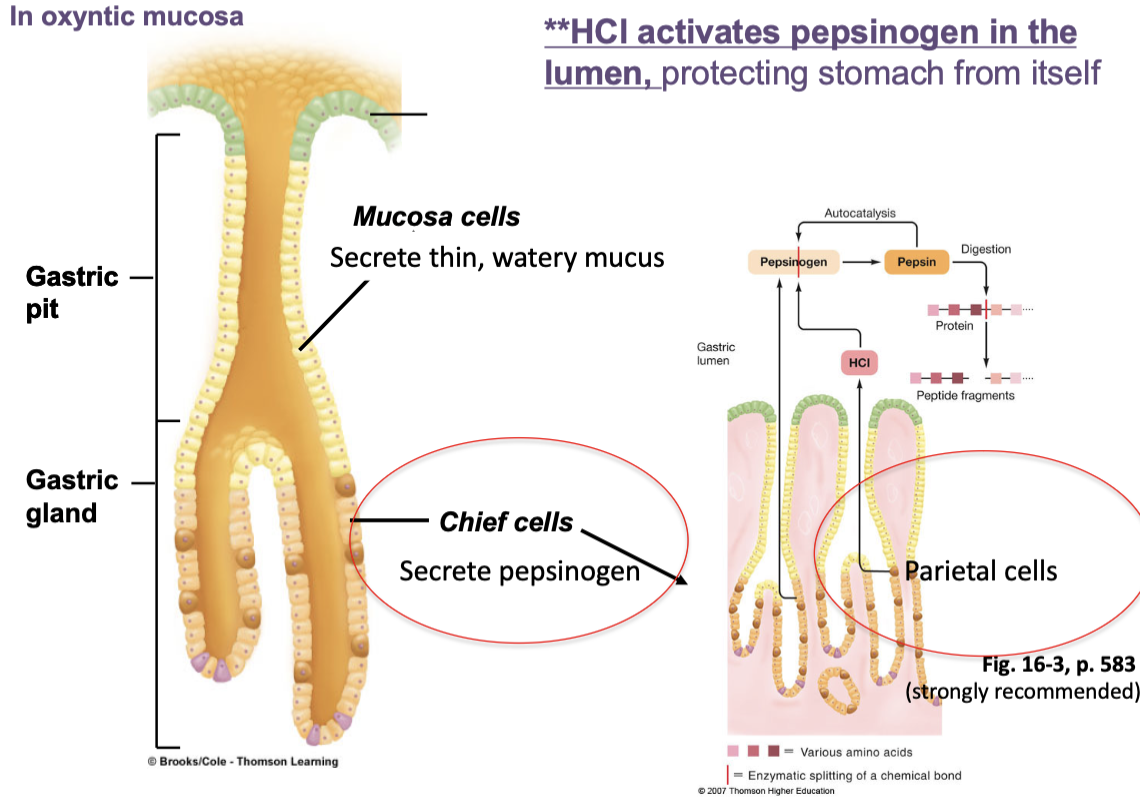
Functions of HCl in the stomach?
activates pepsinogen to active enzyme pepsin and provides acid medium for optimal pepsin activity
denatures protein
along with salivary lysozyme, kills most of the microorganisms ingested with food
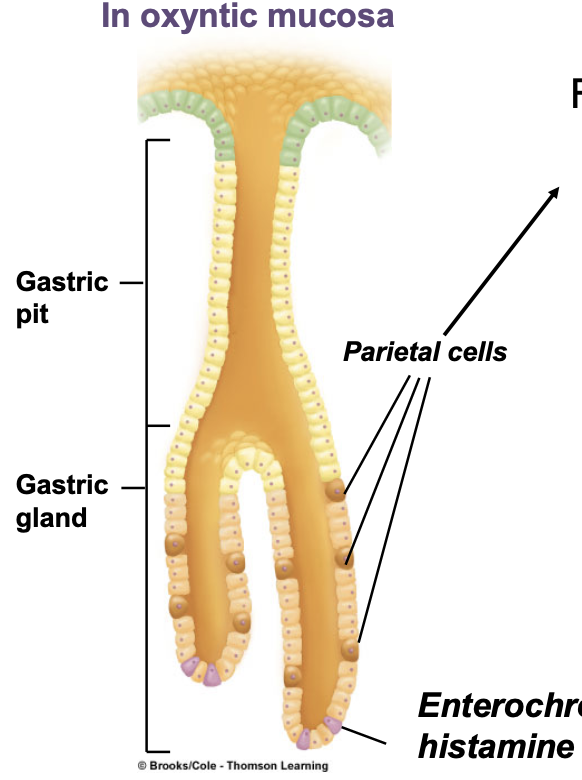
Enterochromaffin- like (ECL) cells:
secrete histamine (activates parietal cells) and is usually a local intermediate in a signaling loop
in this case, activates parietal cells which are the HCl- producing cells
purple spots
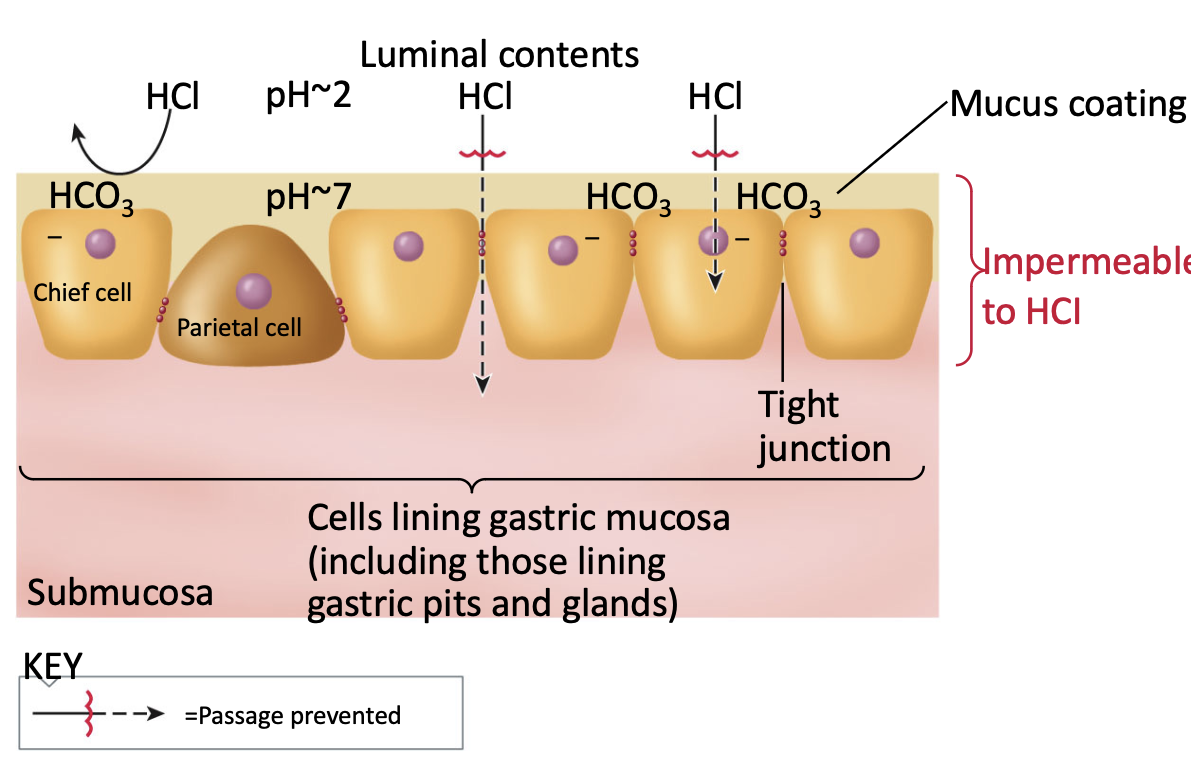
How do stomach cells survive despite the acid?
in between gastric pits, the actual lining of the stomach has mucus producing cells that make a very thick layer of mucus that release bicarbonate
prevents outside of stomach from directly damaging mucosal cells
cells are not meant to last long
Endocrine secretory cells in the pyloric gland area secrete what?
secrete hormone gastrin into bloodstream which stimulates parietal, chief, and ECL cells
G cells
secretes hormone somatostatin into the bloodstream which inhibits parietal and ECL cells
D cells
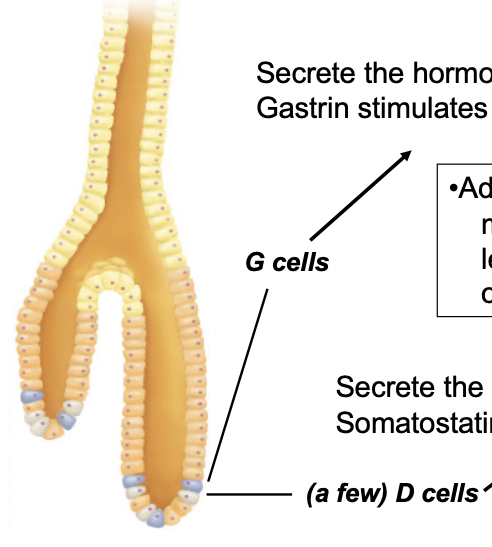
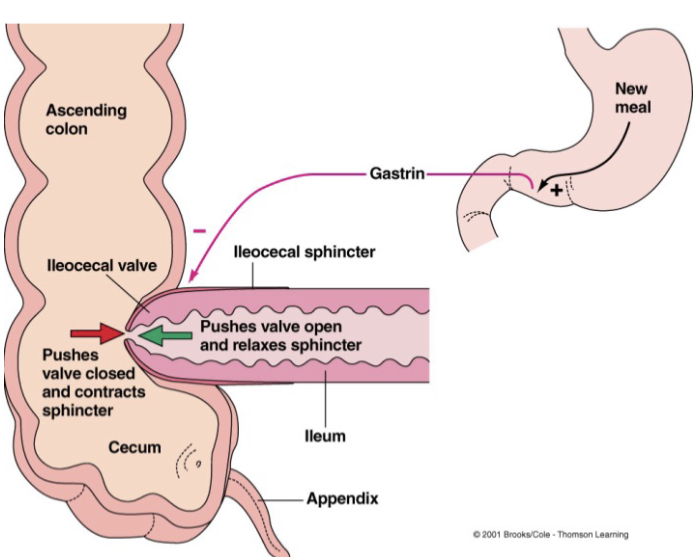
Gastrin increases what?
increases gastric motility and promotes movement of leftover, undigested/unabsorbed material out of ileum into large intestine
Gastric mixing and emptying:
strong peristaltic contractions occur in the antrum that
mix food with gastric secretions to produce chyme
propel chyme towards pyloric sphincter, where a small amount is pushed into the duodenum
in response to chyme, sphincter closes and remaining chyme is tumbled back into the antrum.
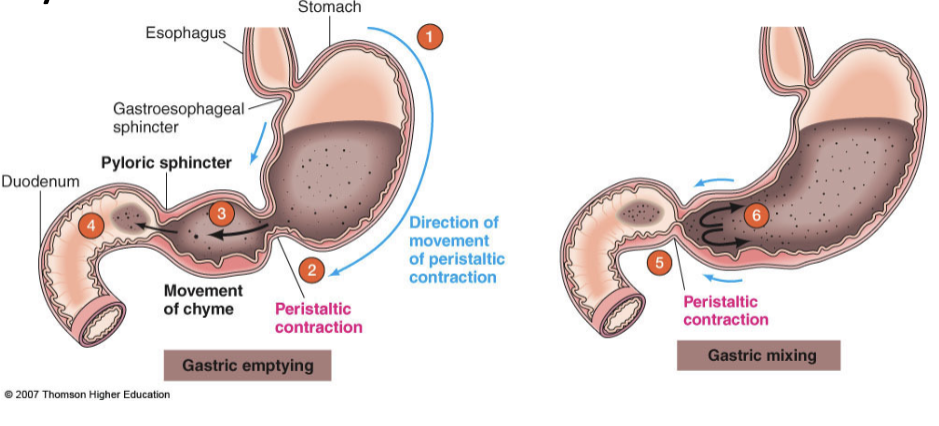
How does the volume of the chyme control gastric mixing and emptying (pyloric function)?
distention directly stimulates stretch receptors on the smooth muscle, stimulates enteric and parasympathetic nervous system as well as the stomach hormone gastrin to increase motility
more volume, more contractions (to an extent)
How does the fluidity of the chyme control gastric mixing and emptying (pyloric function)?
liquids do not require extensive mixing and churning; contents must be rendered fluid before they are evacuated
How does fat control gastric emptying (via neural and hormonal factors)?
fat is only digested and absorbed within the small intestine, so when fat is present in the small intestine further emptying is inhibited
more fat, less movement for absorption
How does acid control gastric emptying (via neural and hormonal factors)?
highly acidic chyme from the stomach is neutralized by sodium bicarbonate (secreted from pancreas) in the duodenum
Un-neutralized acid in the duodenum inhibits gastric emptying
acidic = less emptying
How does hypertonicity control gastric emptying (via neural and hormonal factors)?
increased osmolarity in the duodenum indicates a back-up of nutrients and delays gastric emptying
lots of nutrients = preventing gastric emptying for more absorption
How does distension control gastric emptying (via neural and hormonal factors)?
stomach initiates gastric emptying promoting motility while simultaneous duodenal distension triggers inhibitory hormones
Stomach → has brakes to prevent overfilling of duodenum
Small intestine → too much chyme in the duodenum inhibits gastric emptying
if stretched too much = can’t process efficiently
Factors that regulate gastric motility by triggering neural responses:
neural responses are mediated through both intrinsic nerves (short reflex) and autonomic nerves (long reflex)
collectively this is called the enterogastric reflex
Factors that regulate gastric motility by triggering hormonal responses:
hormonal response involves release of hormones from duodenal mucosa collectively known as “enterogastrones”
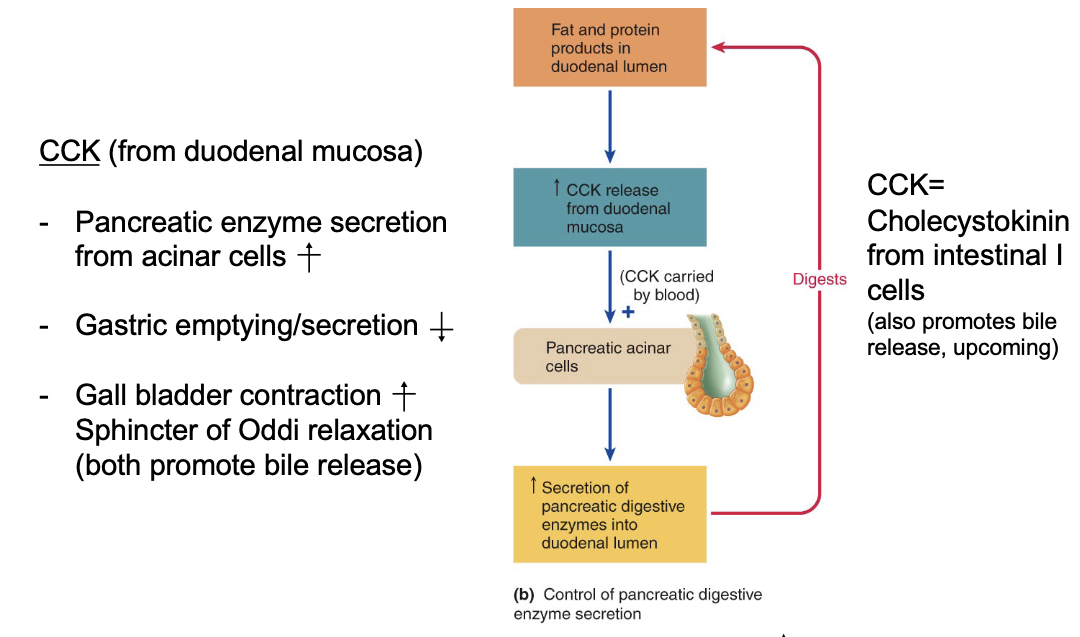
cholecystokinin (CCK) → stimulated by fat in the duodenum
inhibits antral contractions and induces contraction of the pyloric sphincter
secretin → stimulated by unneutralized acid in the duodenum
released by S cells and slows gastric emptying
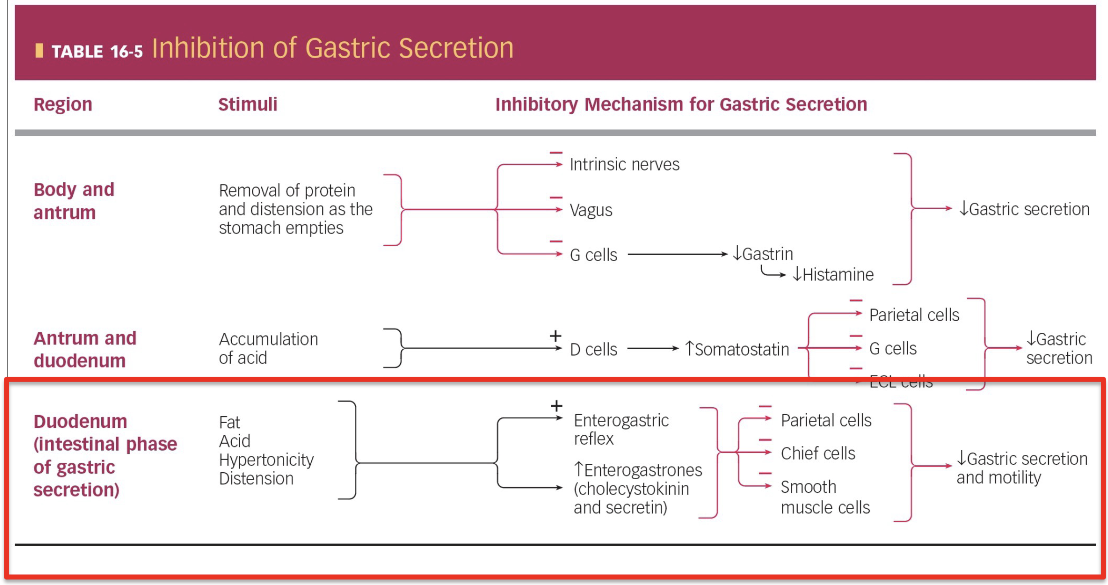
What are the 3 phases in gastric secretion?
cephalic
gastric
intestinal
Cephalic phase:
pre-activation of your stomach by signals that have not yet reached the stomach, that are entirely in the head → seeing, smelling, tasting, chewing, swallowing of food
excitatory → activates the stomach
nervous and endocrine response involved
ACh → Parasympathetic + enteric NS neurotransmitter
intrinsic nerves + G cells activating gastric secretion and motility
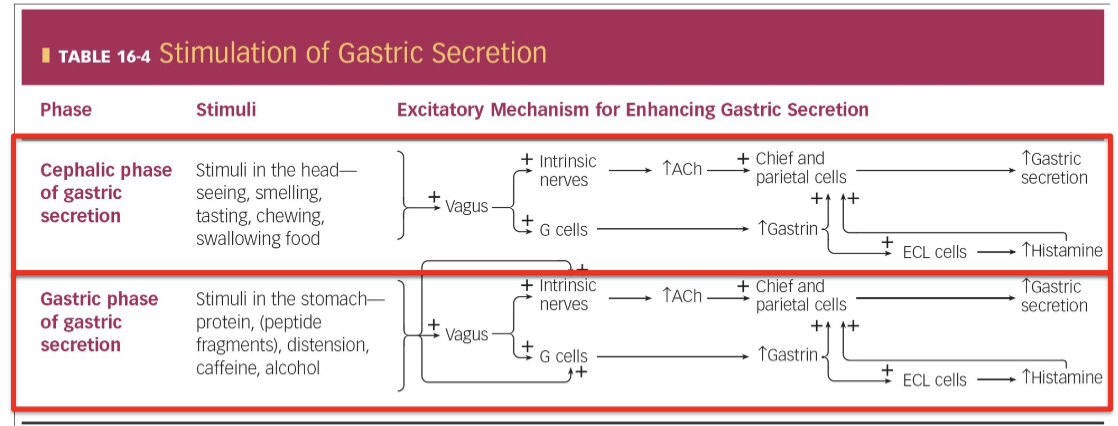
Gastric phase:
once food hits the stomach, gastric emptying will become activated
same as cephalic phase but more potent due to direct signals from within the stomach
excitatory
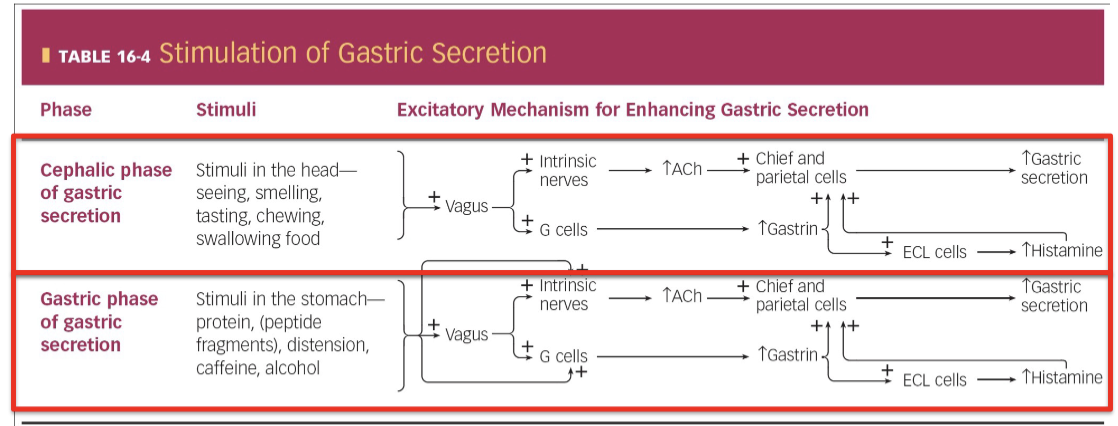
Intestinal phase:
will activate both nerves and hormones (CCK + secretin) that collectively inhibit H+ secretion, pepsinogen, smooth muscle contraction, and overall reduce gastric secretion and motility
inhibitory → slow down stomach
not a lot of acid content
removing protein and extension as stomach empties gradually removes signal that activated stomach
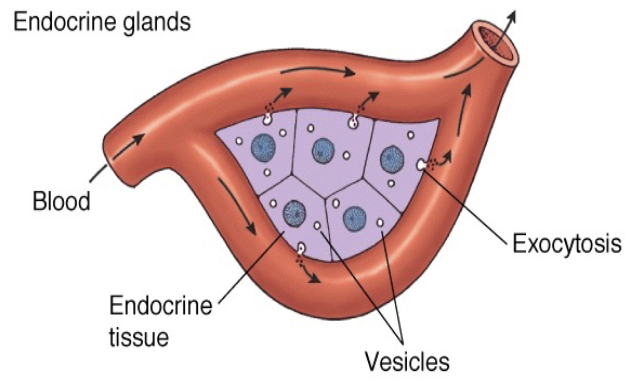
Pancreas:
located dorsal and caudal to the stomach and is a mixed gland that contains both endocrine and exocrine tissue
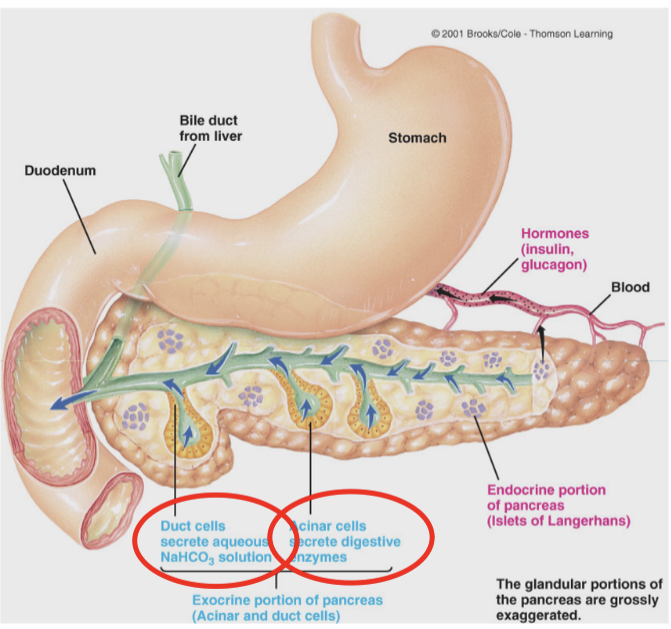
Exocrine pancreas includes what?
duct cells → release sodium bicarbonate (NaHCO3) into duodenum to neutralize acidic chyme
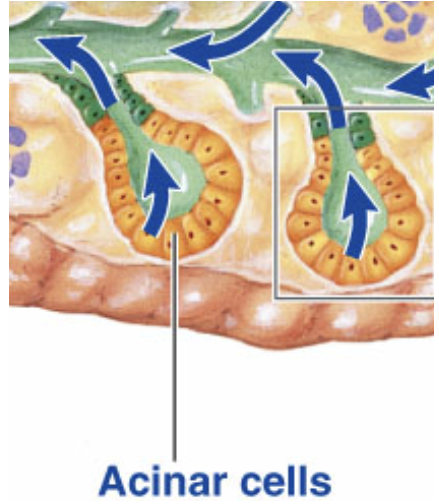
acinar cells
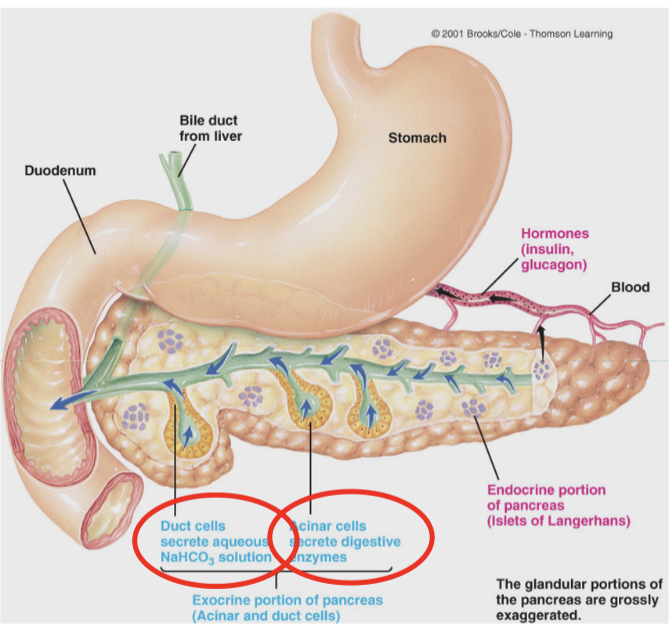
Pancreatic acinar cells:
release digestive enzymes into duodenum and work better at a neutral or alkaline pH
pancreatic amylase → carbohydrate digestion
pancreatic lipase → only enzyme secreted throughout human digestive system that can significantly digest fat
proteolytic enzymes
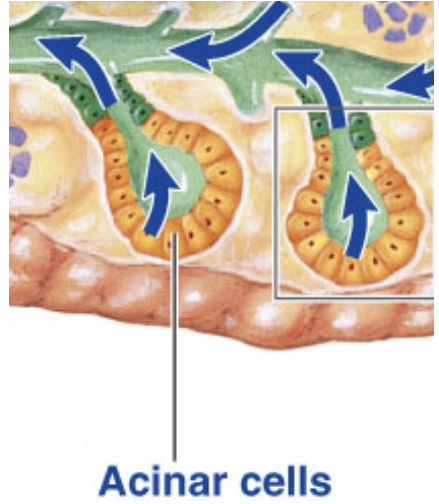
Proteolytic enzymes:
secreted as inactive forms and cleave bonds between amino acids
Trypsinogen → converted to the active form trypsin by enteropeptidase in the luminal (brush border) membrane of small intestine
Chymotrypsinogen → converted to active form chymotrypsin by trypsin
Procarboxypeptidase → converted to active form carboxypeptidase by trypsin
Why are protein-degrading (proteolytic) enzymes (pepsin, trypsin, chymotrypsin and carboxypeptidase) secreted as inactive precursors, while lipid- and carbohydrate-degrading enzymes (amylase, lipase) are secreted as active precursors?
proteins are part of your own body’s structure, so proteases must be tightly controlled; fats and carbs aren’t, so their enzymes can be active right away
ensures they are only activated in the right place and at the right time
How does the pancreas know when to secrete (CCK)?
same CCK that told pancreas to slow down in response to fat is telling to release more lipase and other enzymes (3 proteolytic and amylase) from acinous cells
chyme in the duodenum stimulates pancreatic secretions via intestinal hormones, aka enterogastrones
vagovagal reflex in response to increased volume in duodenum secretin and CCK
weak direct stimulation of duct and acinar cells by vagus (cephalic phase)
CCK feedback loop
How does the pancreas know when to secrete (secretin)?
secretin released in response to acid in duodenum separates endocrine cells called S cells which trigger the release of secretin
goes around in the duct cells which release bicarbonate and neutralize acid → a feedback loop
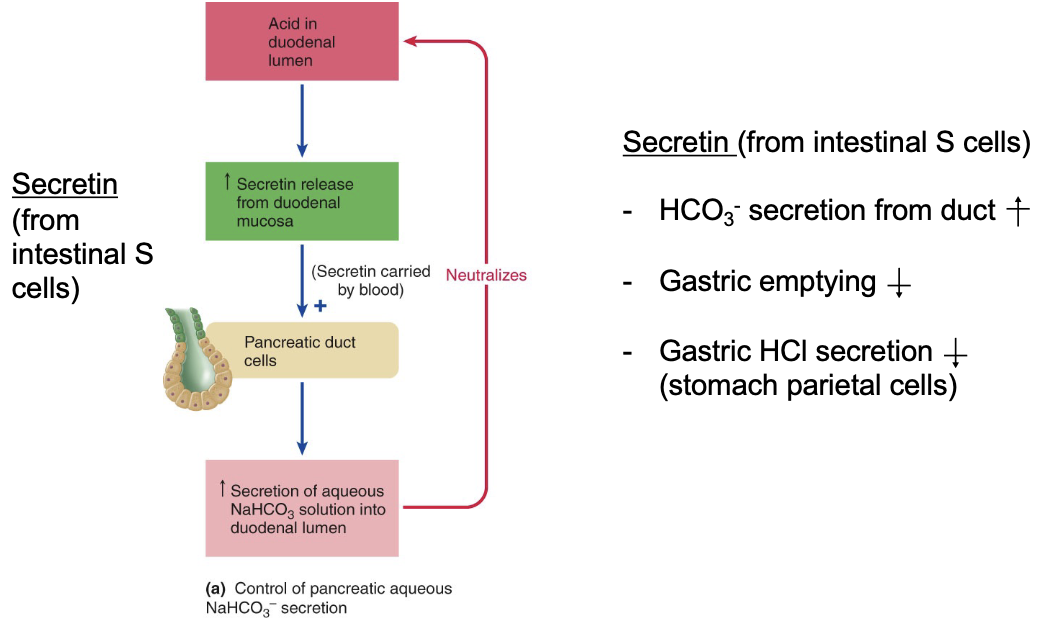
Both the secretin and CCK loops work in parallel as they stimulate and inhibit what?
stimulate the pancreas and inhibit the stomach so as to carefully dose the pace with which we empty our stomach
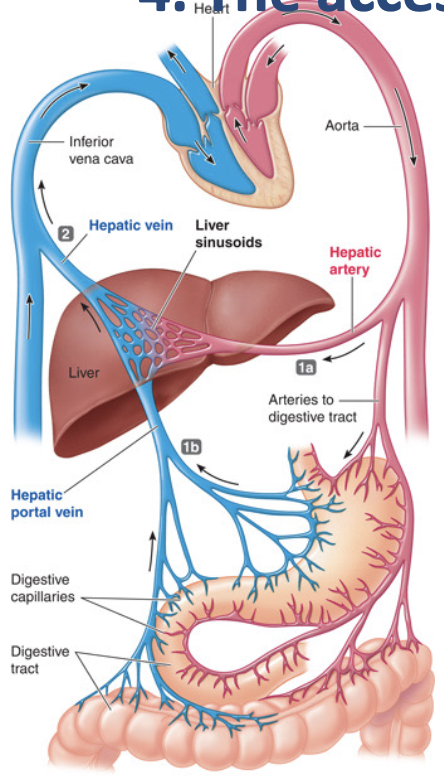
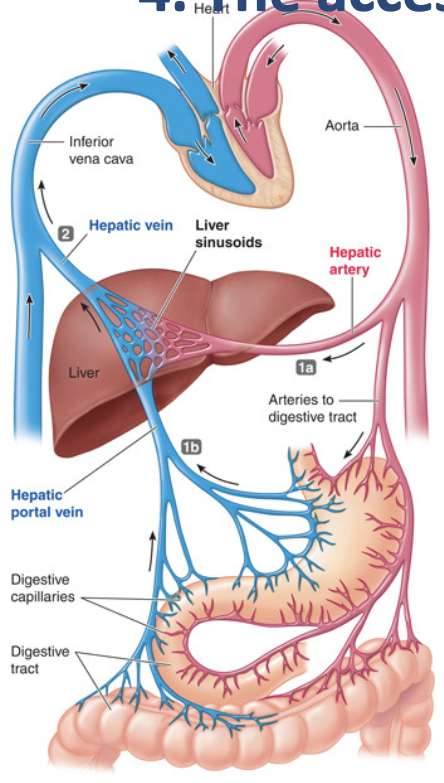
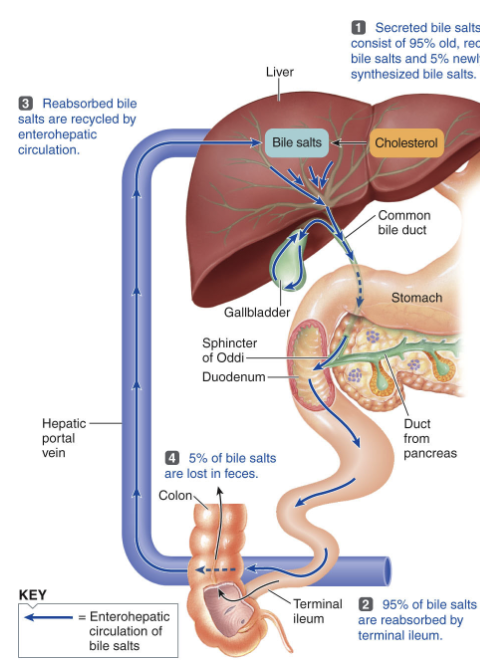
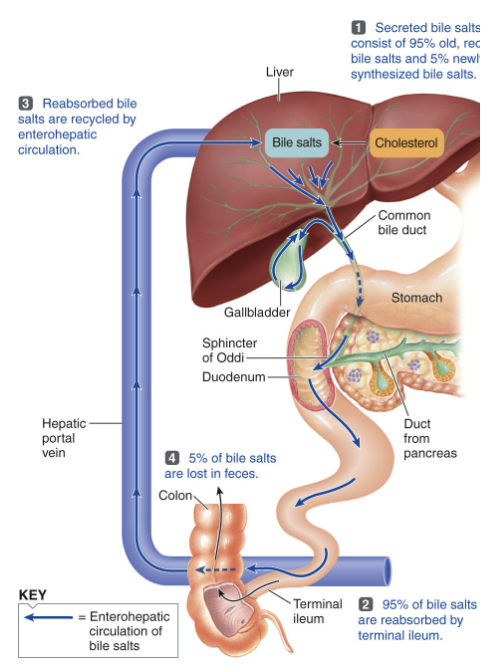
The liver receives its blood from what two sources?
the hepatic artery which provides oxygenated blood and the hepatic portal vein that ensures venous blood from digestive tract is first carried to the liver
blood leaves liver through hepatic vein
Liver functions:
allows for detoxification of absorbed foreign compounds by the liver first, before they access the general circulation
ensures that all absorbed monosaccharides and amino acids are routed to the liver first for processing
The major contribution of the liver to the digestive system is what?
the secretion of bile that is stored in the gall bladder due to CCK
during, between, and after meals
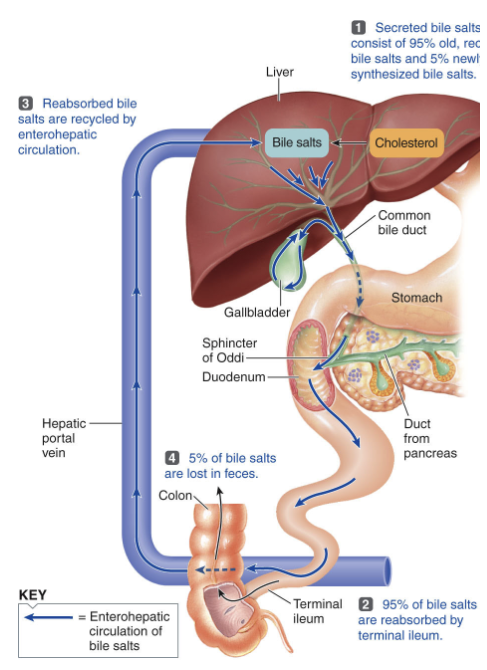
During meals, what happens to bile?
it is secreted from the liver (and/or released from gall bladder) and enters the duodenum
help digest fats by breaking large globules into smaller droplets
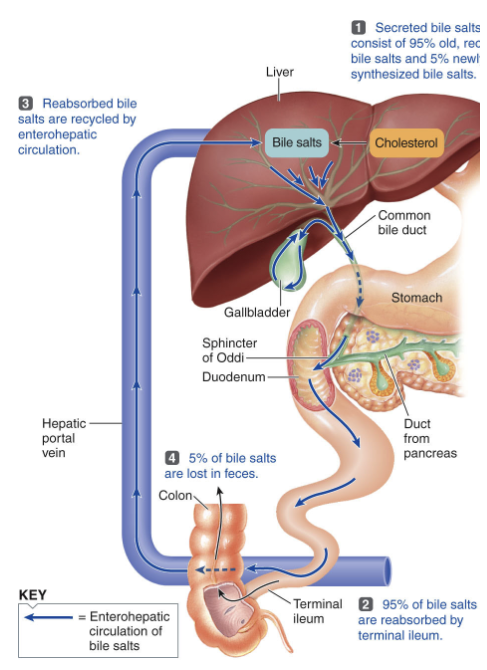
Between meals, what happens to bile?
the sphincter of Oddi closes and bile flows to the gallbladder for storage and concentration, becoming 5-10 times stronger as water is removed
ready to help digest fats when you eat again
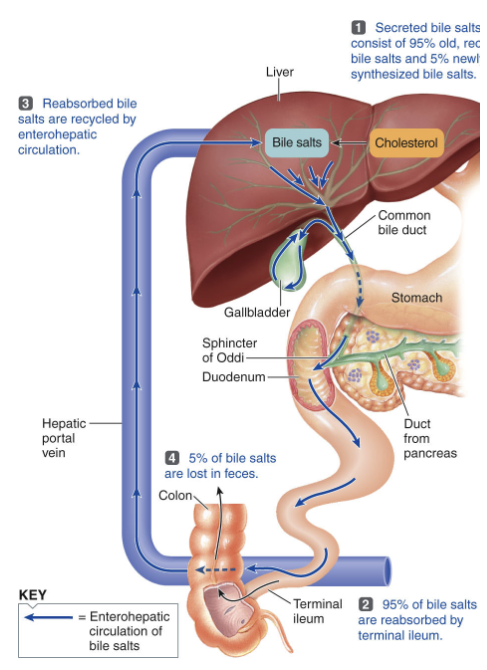
After meals, what happens to bile?
used bile salts get reabsorbed and recycled back to the liver with some ending up in the large intestine and being excreted
~95% of bile salts are reabsorbed in the distal small intestine and carried to the liver
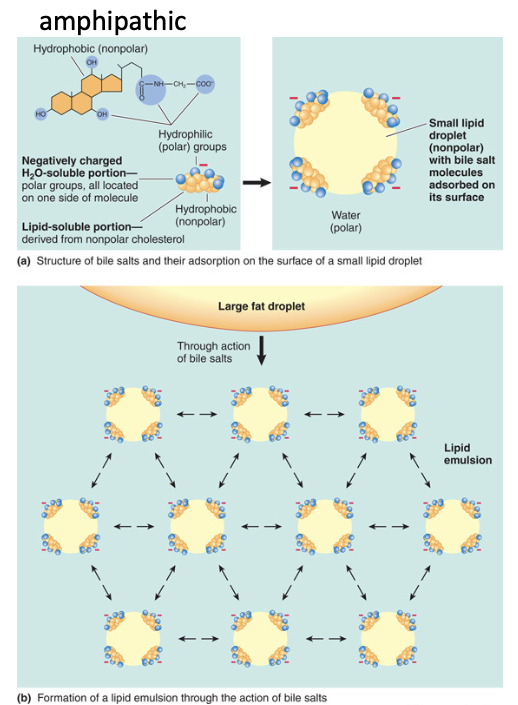
Bile consists of what?
Bile acids/salts
Cholesterol
Phospholipid (Lecithin)
Bilirubin (RBC breakdown product)
Aqueous mixture or bicarbonate, ions, water
Bile plays a role in what?
aids in fat digestion by emulsification → increases surface area for lipase
helps neutralize stomach acid
cholesterol balance
*CCK causes bile to be secreted!
Which of these is NOT a role for cholecystokinin (CCK)?
A) CCK promotes the release of pancreatic digestive enzymes from acinar cells
B) CCK slows down gastric emptying and gastric motility
C) CCK stimulates the release of bile by promoting smooth muscle contractions of the gall bladder and relaxing the sphincter of Oddi
D) CCK promotes the release of gastrin from G cells in the mucosae of the pyloric gland area
D) CCK promotes the release of gastrin from G cells in the mucosae of the pyloric gland area
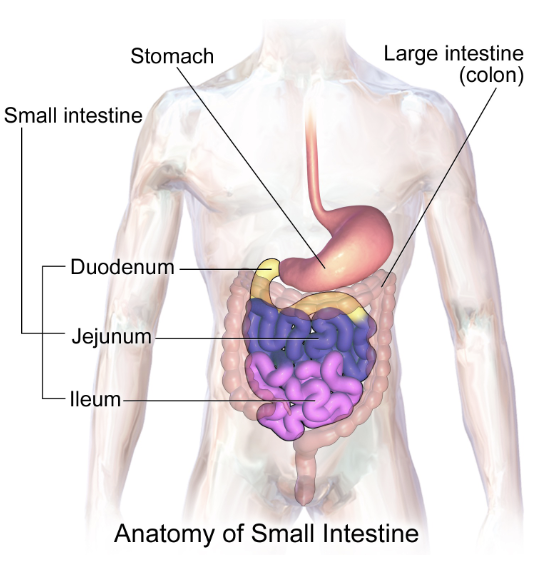
Small intestine:
primary site of digestion and absorption
duodenum → 5%
jejunum → 35-40%
ileum → 55-60%
Motility in the small intestine occurs via what?
occurs via segmentation which both mixes and propels chyme
propulsion occurs because the frequency of local contractions gradually decreases along length of small intestine
mixing food with digestive juices
facilitate absorption
forward movement
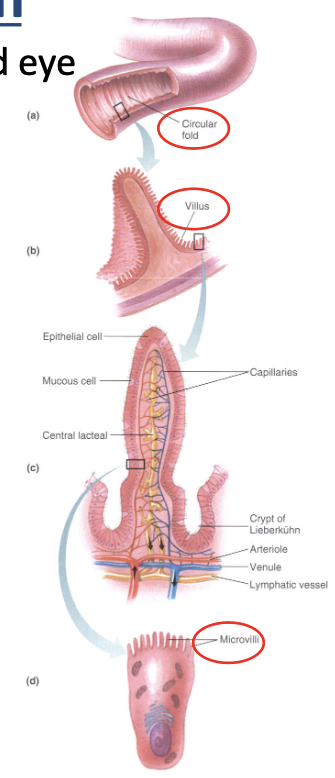
How does the small intestine facilitate absorption?
facilitates absorption by having a large surface area to allow nutrients to be absorbed by diffusion over the mucosal lining
contributes to increase of surface area
circular folds → visible
villi → inside circular folds
microvilli → inside villi
Small intestine digestion:
carbohydrate and protein digestion accomplished by pancreatic enzymes, with fat digestion enhanced by bile secretions all occurring in the intestinal lumen
small intestine produces digestive enzymes but act on surface if cells lining brush border
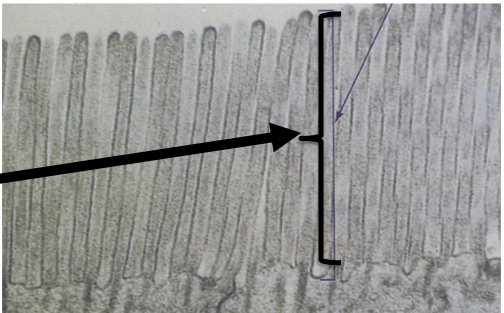
Brush border:
vastly increases surface area for absorption and secretion packed with digestive enzymes for final nutrient breakdown and plays a crucial role in nutrient transport and forming a protective barrier
enteropeptidase
disaccharidases →which complete the digestion of carbohydrates
maltase, sucrase, and lactase
aminopeptidases →which complete the digestion of proteins
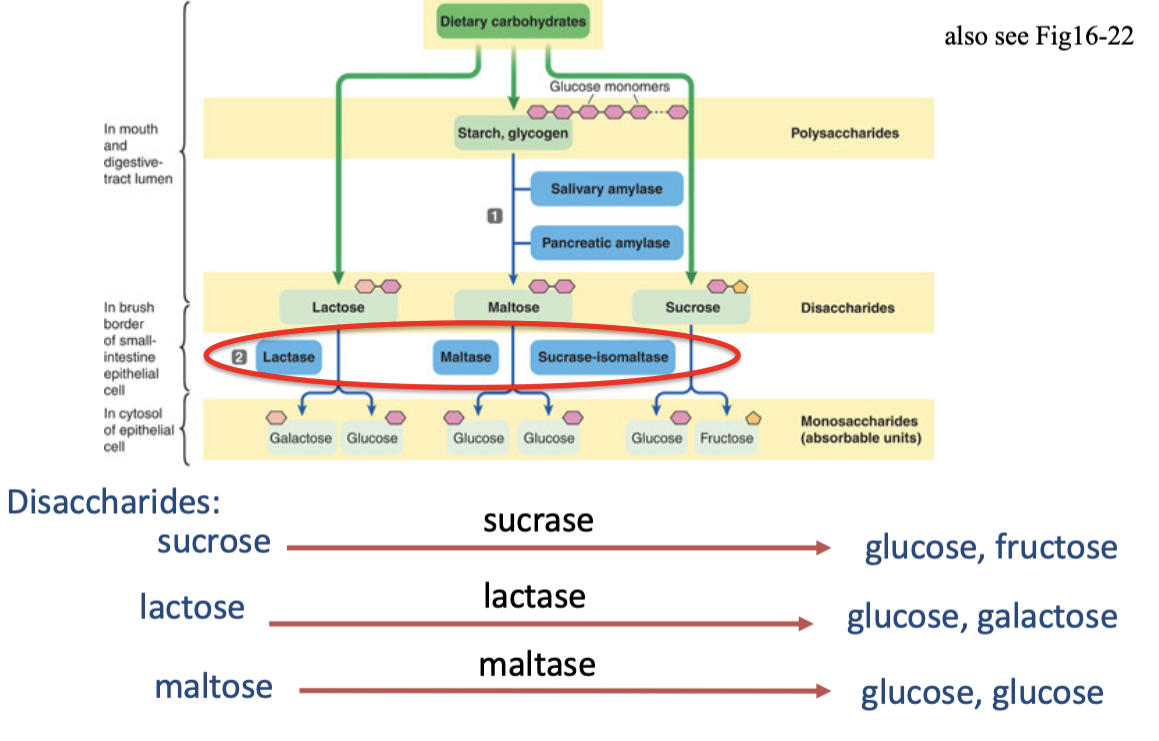
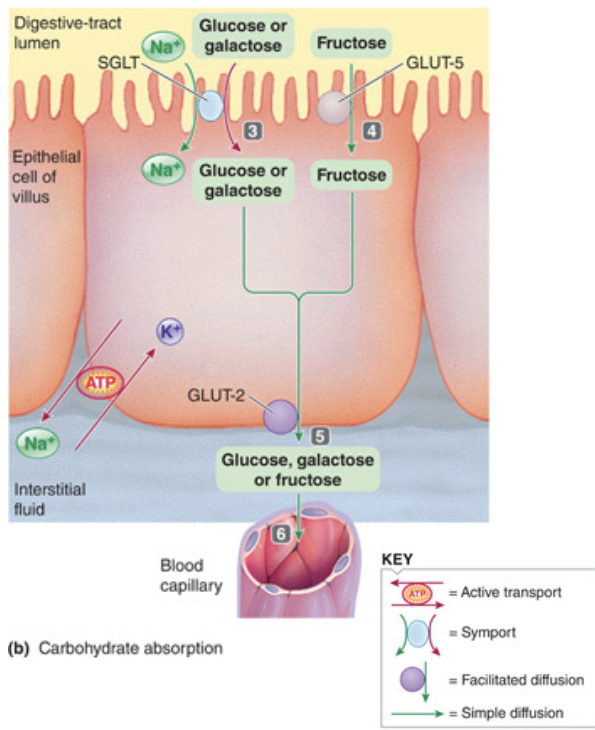
Carbohydrate digestion:
polysaccharides starch and glycogen are converted to the disaccharide maltose by amylase in the mouth and digestive tract lumen
maltose, lactose, and sucrose are converted to monosaccharides (glucose, galactose, and fructose) on the brush border of intestinal epithelial cells by the enzymes lactase, maltase, and sucrase
glucose and galactose are absorbed into the epithelial cells by active transport
fructose enters the epithelial cells by passive facilitated diffusion
glucose, galactose and fructose exit the cell into the blood by passive facilitated diffusion
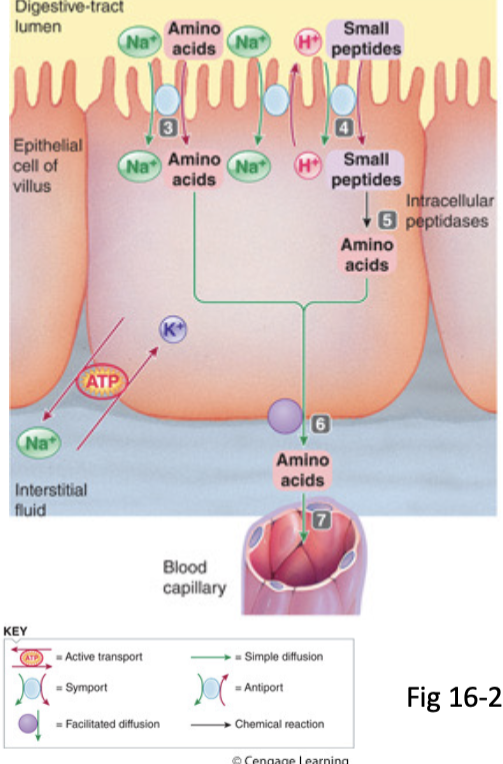
Protein digestion:
proteins hydrolyzed into small peptide fragments and individual amino acids by pepsin and pancreatic proteolytic enzymes
small peptides are broken down into amino acids on the brush
border by peptidases and aminopeptidasesamino acids absorbed into cell via Na+ and energy-dependent active transport and enter blood down their concentration gradients (6/7)
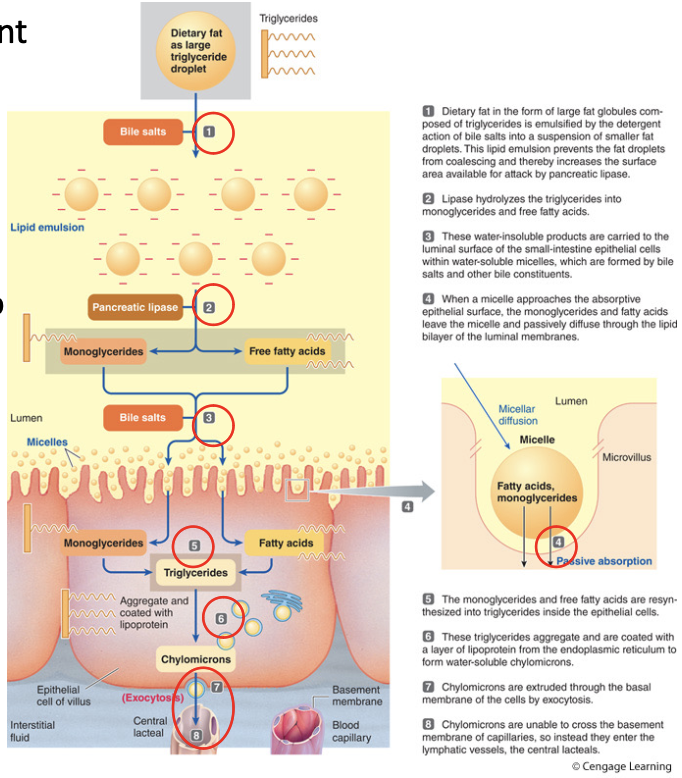
Fat digestion:
fat is emulsified by the detergent action of bile salts
lipases hydrolyze triglycerides into monoglycerides and free fatty acids
water insoluble products move within the interior of micelles to the epithelial cell surface
monoglycerides and free fatty acids diffuse into cell
monoglycerides and free fatty acids resynthesize into triglycerides
triglycerides coated with lipo- protein and form chylomicrons that are exocytosed from cell
chylomicrons enter lymphatic vessels
Small and Large intestine:
separated by the ileocecal valve and sphincter which is a one-way flow
contents from the ileum into cecum (first part of the large intestine)
necessary to keep colonic bacteria from entering the ileum
Large intestine:
primarily for drying and storage, includes
Cecum → blind-ended pouch below ileocecal valve
Appendix → finger-like projection of lymphoid tissue
Colon → ascending, transverse, descending, & sigmoid
Rectum → “straight”, connected to anal canal
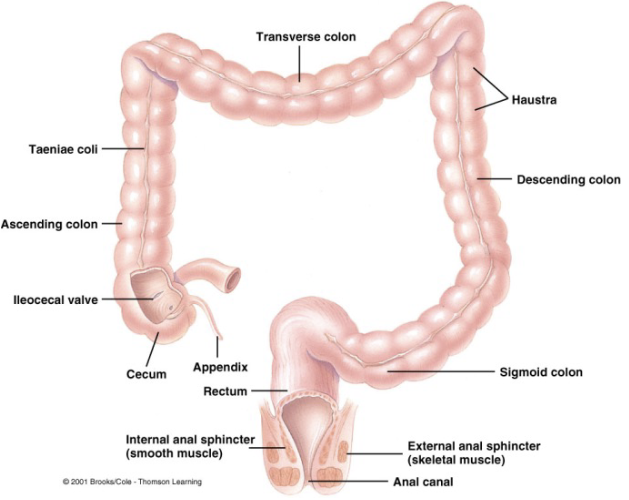
Large intestine motility is influenced through what?
through Haustral contractions, mass movement, and defecation reflex