Session 9: Invasion & Metastasis and the Effects of Neoplasms
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
82 Terms
Neoplasm
Abnormal growth of cells that persists after the initial stimulus is removed
Malignant neoplasms
An abnormal growth of cells that persists after the intial stimulus is removed and invades surrounding tissue with potential to spread to distant sites
Neoplasia
An irreversible disorder of cell growth, triggered by series of mutations (germline, acquired/somatic) affecting a single cell and its clonal progeny.
The causative mutations give neoplastic cells a survival and growth advantage.
The result is excessive & autonomous proliferation (independent of physiological growth signals).
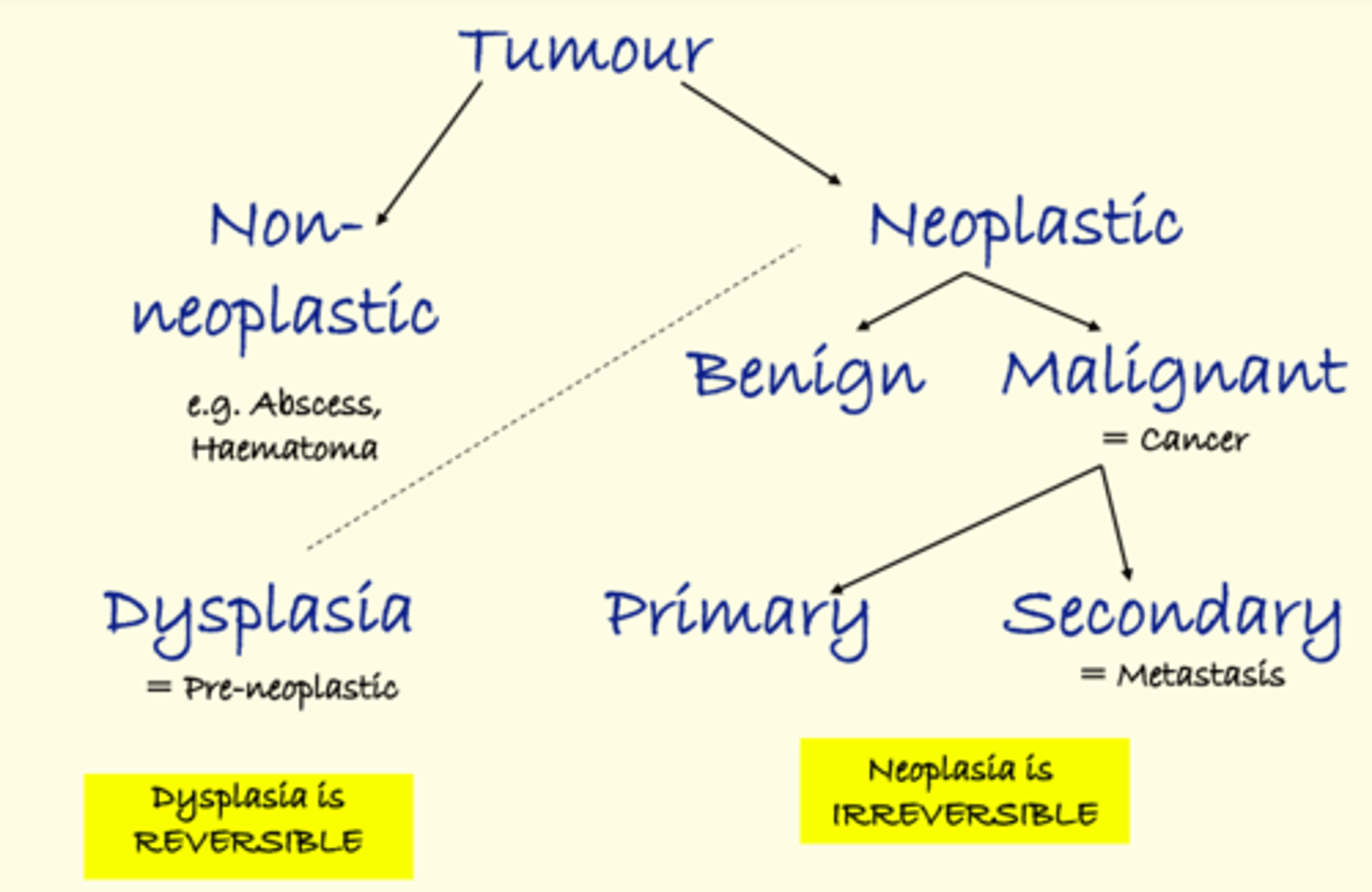
Tumour
Any clinically detectable lump or swelling.
A neoplasm is just ONE type of tumour.
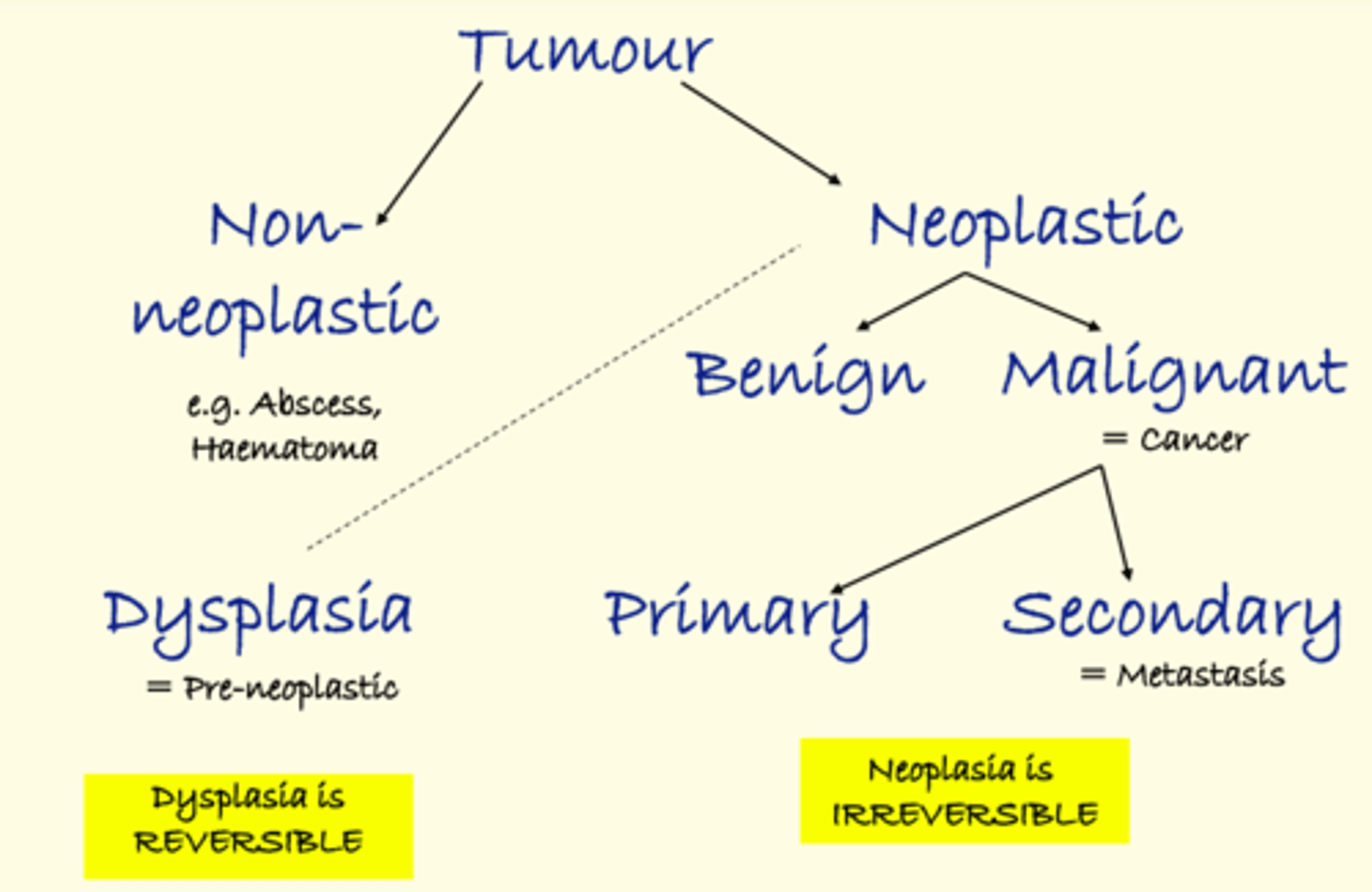
Cancer
Any malignant neoplasm
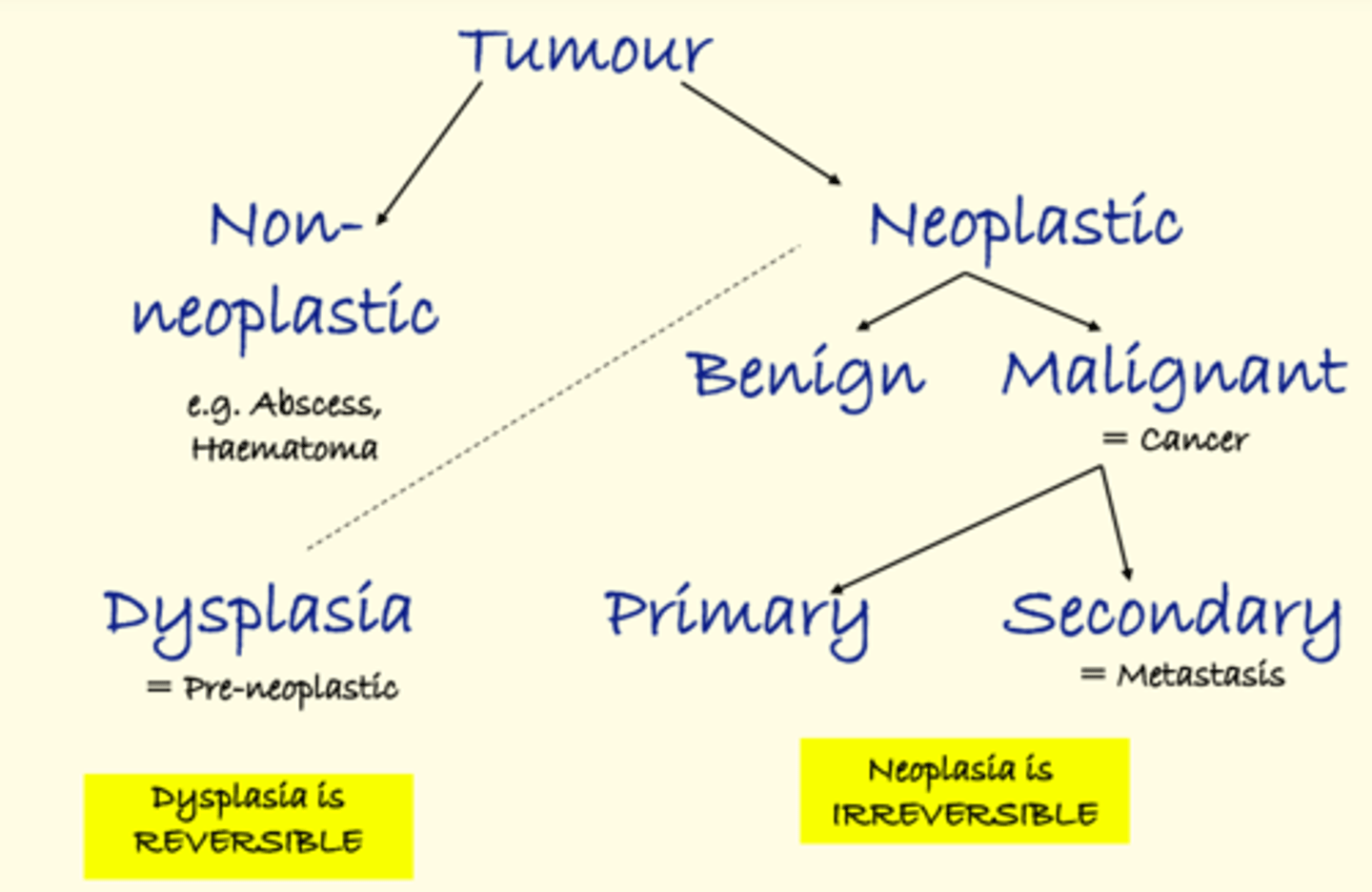
Metastasis
Malignant neoplasm that has spread from its original site to a new non-contiguous site. The original position is the primary site and the place to which it has spread is a secondary site.
Dysplasia
Pre-neoplastic alteration in which cells show disordered tissue organisation. It is not neoplastic because the change is reversible.
Cell maturation and differentiation are delayed
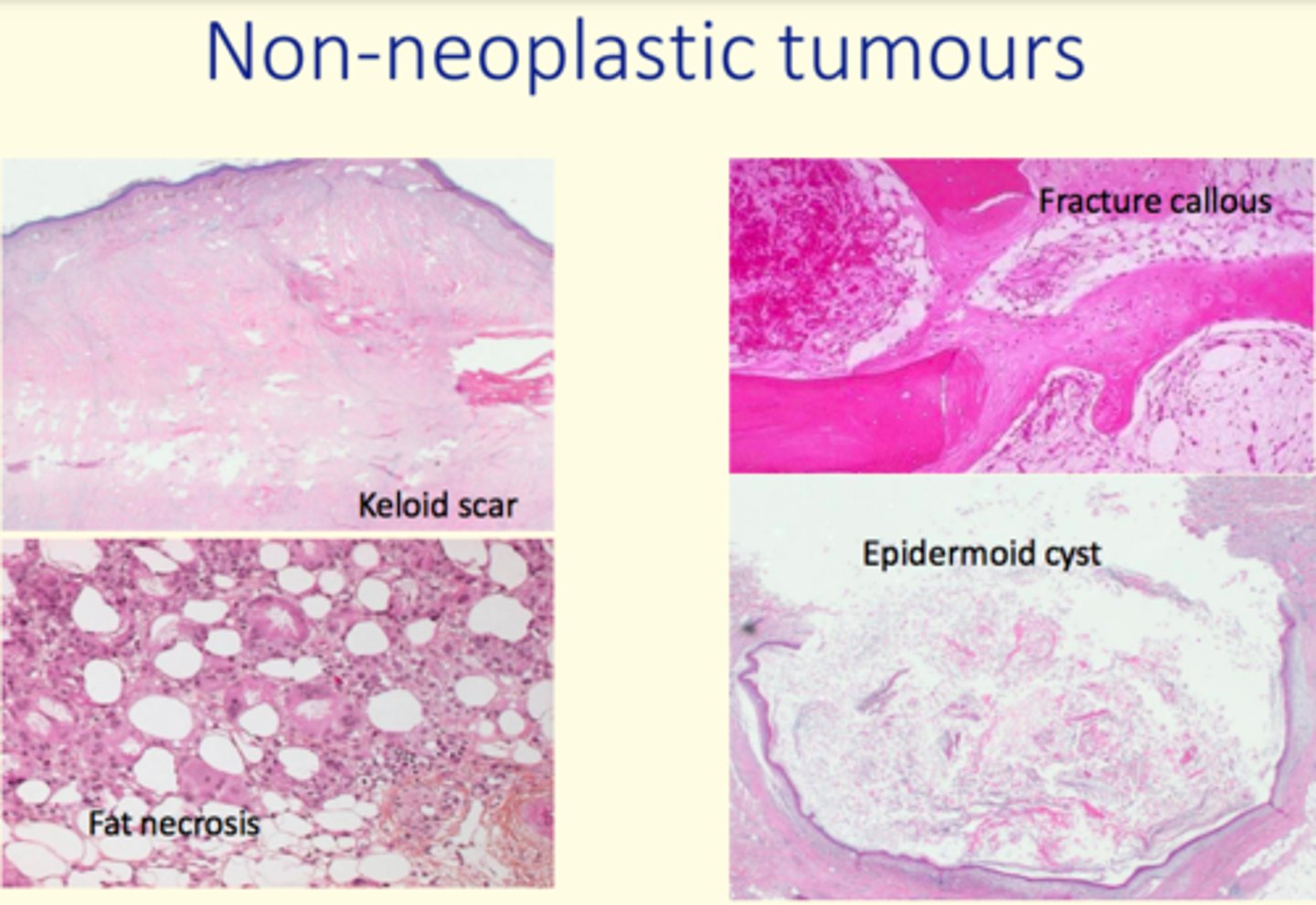
Example of a non-neoplastic tumour
Abscess
Haematoma
Keloid scar
Epidermoid cyst
Benign neoplasms nomenclature
Benign neoplasms end in -oma
Malignant neoplasms nomenclature
Epithelial malignant neoplasm (90%) end in -carcinoma
Stromal malignant neoplasm end in -sarcoma
Carcinomas can be in-situ or invasive. What do these terms mean?
In-situ = no invasion of basement membrane
Invasive = invasion of basement membrane
Give some examples of benign epithelial neoplasms
Stratified squamous = squamous papilloma
Transitional = transititional cell papilloma e.g., bladder mucosa
Glandular = adenoma e.g., adenomatous polyp of colon
Give some examples of (CARCINOMAS) malignant epithelial neoplasms
Stratified squamous epithelium (e.g., skin, mouth, cervix) = squamous cell carcinoma
Glandular epithelium (e.g., stomach, colon, lung, prostate, breast, kidney, pancreas) = adenocarcinoma
Transitional epithelium (e.g., bladder, ureter, renal pelvis) = transitional cell carcinoma or urothelial carcinoma
Others = basal cell carcinoma
Benign neoplasm of connective tissues
Fibrous tissue
Fibroma
Benign neoplasm of connective tissues
Smooth muscle
Leiomyoma
Benign neoplasm of connective tissues
Striated (skeletal) muscle
Rhabdomyoma
Benign neoplasm of connective tissues
Bone
Osteoma
Benign neoplasm of connective tissues
Cartilage
Chondroma
Benign neoplasm of connective tissues
Fat
Lipoma
Benign neoplasm of connective tissues
Nerve/nerve sheath
Neuroma, neurofibroma
Benign neoplasm of connective tissues
Glial cells
Glioma
Sarcomas, malignant neoplasm of connective tissues
Fibrous tissue
Fibrosarcoma
Sarcomas, malignant neoplasm of connective tissues
Smooth muscle
Leiomyosarcoma
Sarcomas, malignant neoplasm of connective tissues
Skeletal muscle
Rhabdomyosarcoma
Sarcomas, malignant neoplasm of connective tissues
Bone
Osteosarcoma
Sarcomas, malignant neoplasm of connective tissues
Cartilage
Chondrosarcoma
Sarcomas, malignant neoplasm of connective tissues
Fat
Liposarcoma
Sarcomas, malignant neoplasm of connective tissues
Nerve sheath
Neurofibrosarcoma
Neoplasms of lymphoid tissue
Lymphoma
Where do lymphomas occur
Occurs in lymphoid tissue, usually in lymph nodes but can also be found in extranodal locations e.g., skin, salivary glands, GI tract
Example of lymphoma
Hodgkin's lymphoma
Germ cell neoplasms
Testis
Teratoma (benign and malignant)
Seminoma
Embryonal cell carcinoma
Ovary
Usually benign
Mature cystic teratoma
Dermoid cyst
Struma ovarii
Neuroendocrine tumours (NET)
Well differentiated = carcinoid tumour
Poorly differentiated = small cell lung carcinoma
Phaeochromocytoma (adrenal, most benign)
-Blastoma tumours
Arise from precursor cells and are composed of cells with immature characteristics seen in developing (embryonic) stages
Melanoma
Malignant tumour of cells derived from neural crest
Mesothelioma
Tumour of mesothelium (malignant)
Benign neoplasm features
- Confined to site of origin
- Do not produce metastases
- Well-defined, rounded pushing outer edge (pushing outer margin)
- With capsule or pseudocapsule
- Microscopically resemble the tissue of origin (they are well differentiated)
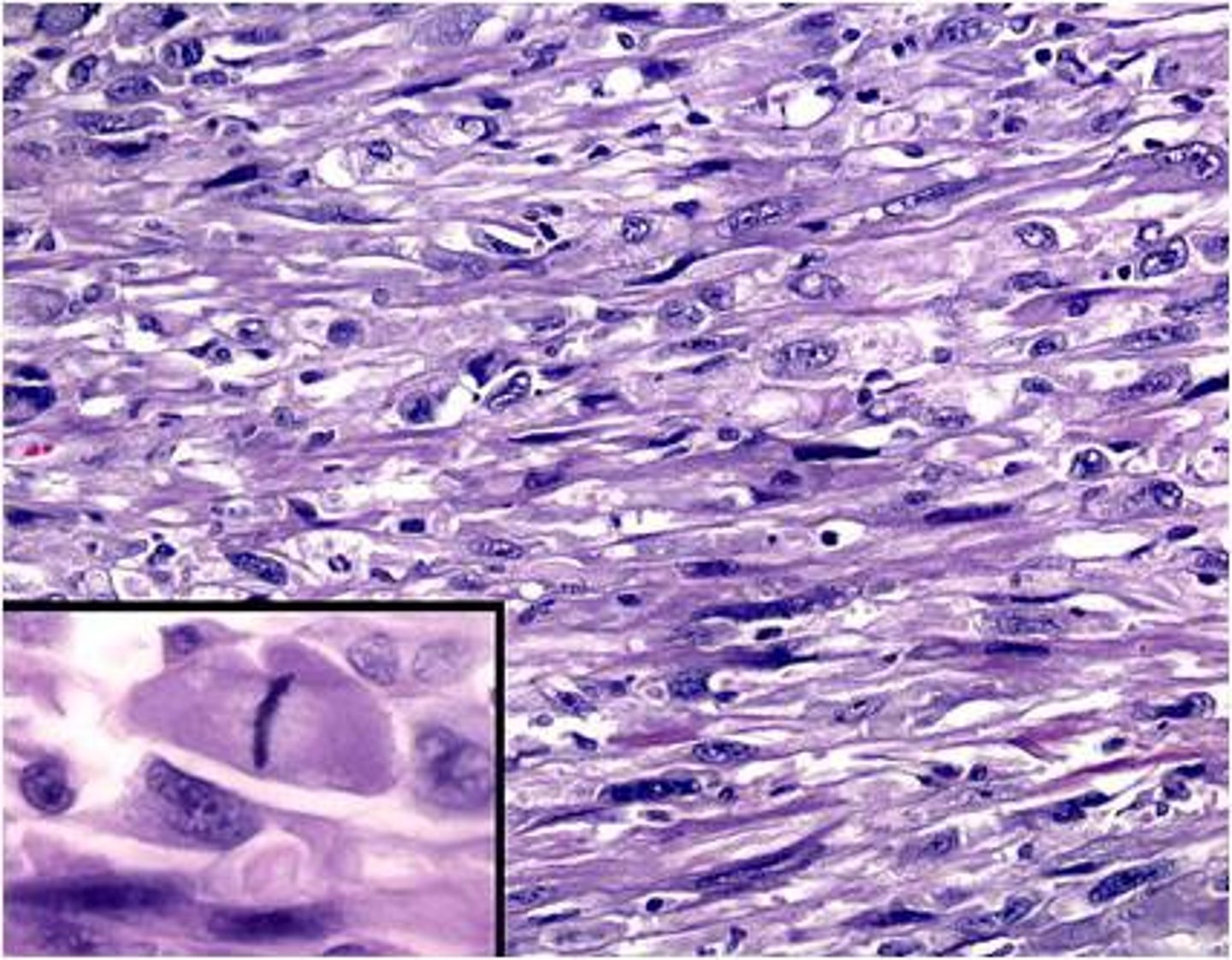
Malignant neoplasm features
- Irregular outer margin & shape
- May show areas of ulceration/necrosis
- Range from well to poorly differentiated
- Microscopically do not resemble the tissue of origin (clinicians use 'grading' to indicate the level of differentiation)
- Potential to metastasise
- Loss of contact inhibition
- Abnormal mitotic figures
High-grade cancer
Grade III/IV
Poorly differentiated, or anaplastic tumor. Very pleomorphic cells, little or no keratin, difficult to identify, enlarge rapidly, metastasizes early
Low-grade cancer
Grade I
Well-differentiated tumor closely resembles tissue of origin, grows slower and metastasizes later
Anaplastic
Undifferentiated cell growth - without form (bizarre)
Cells with NO resemblance to ANY tissue (very poor differentiation)
Dysplastic conditions
Example of oesophageal dysplasia
Barrett's with dysplasia
Dysplastic conditions
Example of epithelial dysplasia
Epithelial dysplasia of the cervix (CIN)
Dysplastic conditions
Example of colon dysplasia
Adenomatous polyps
What is the most lethal ability of malignant cells?
Ability of malignant cells to spread (metastasise) to distant sites leads to a greatly increased tumour burden with local & distant tissue destruction/damage
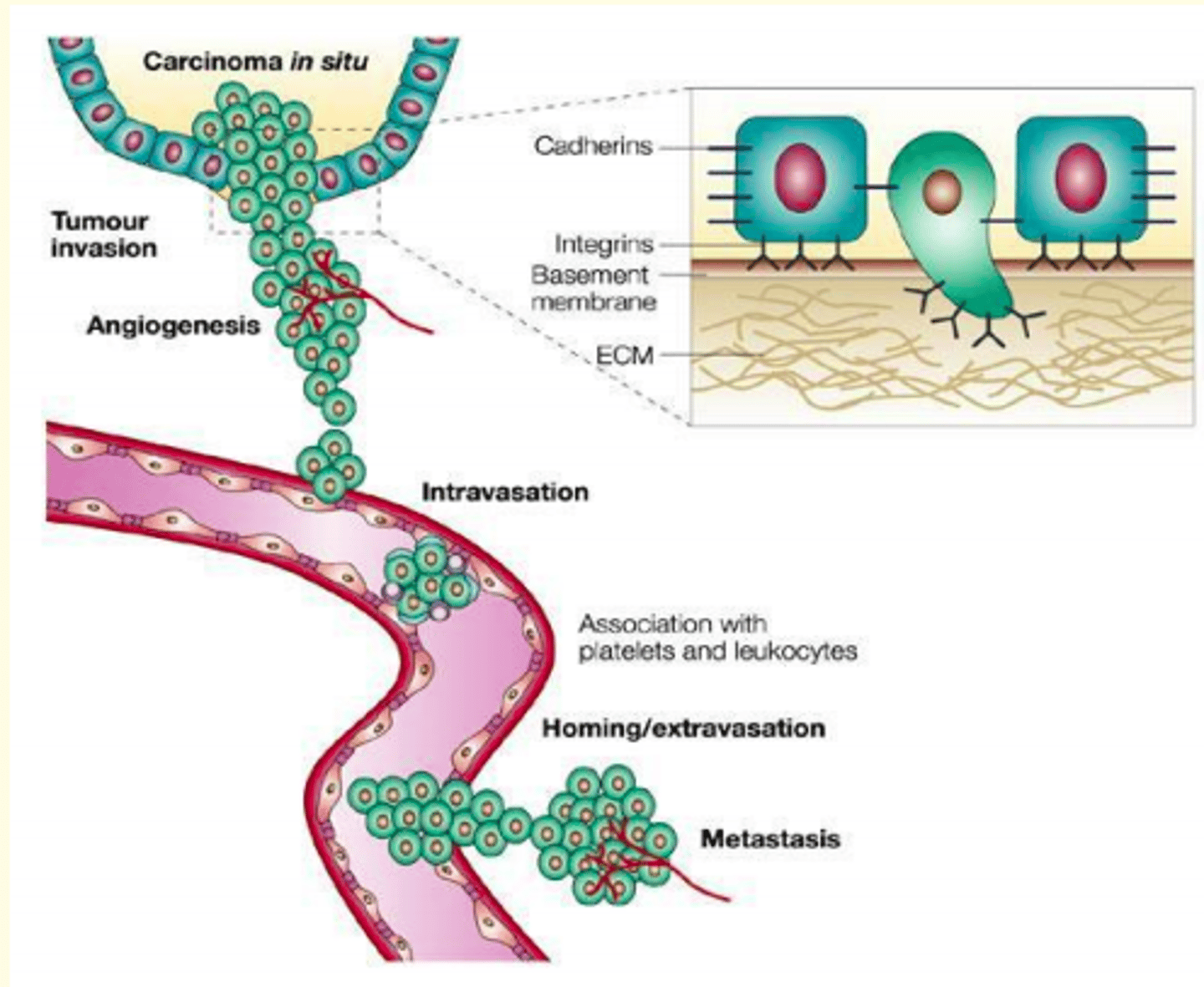
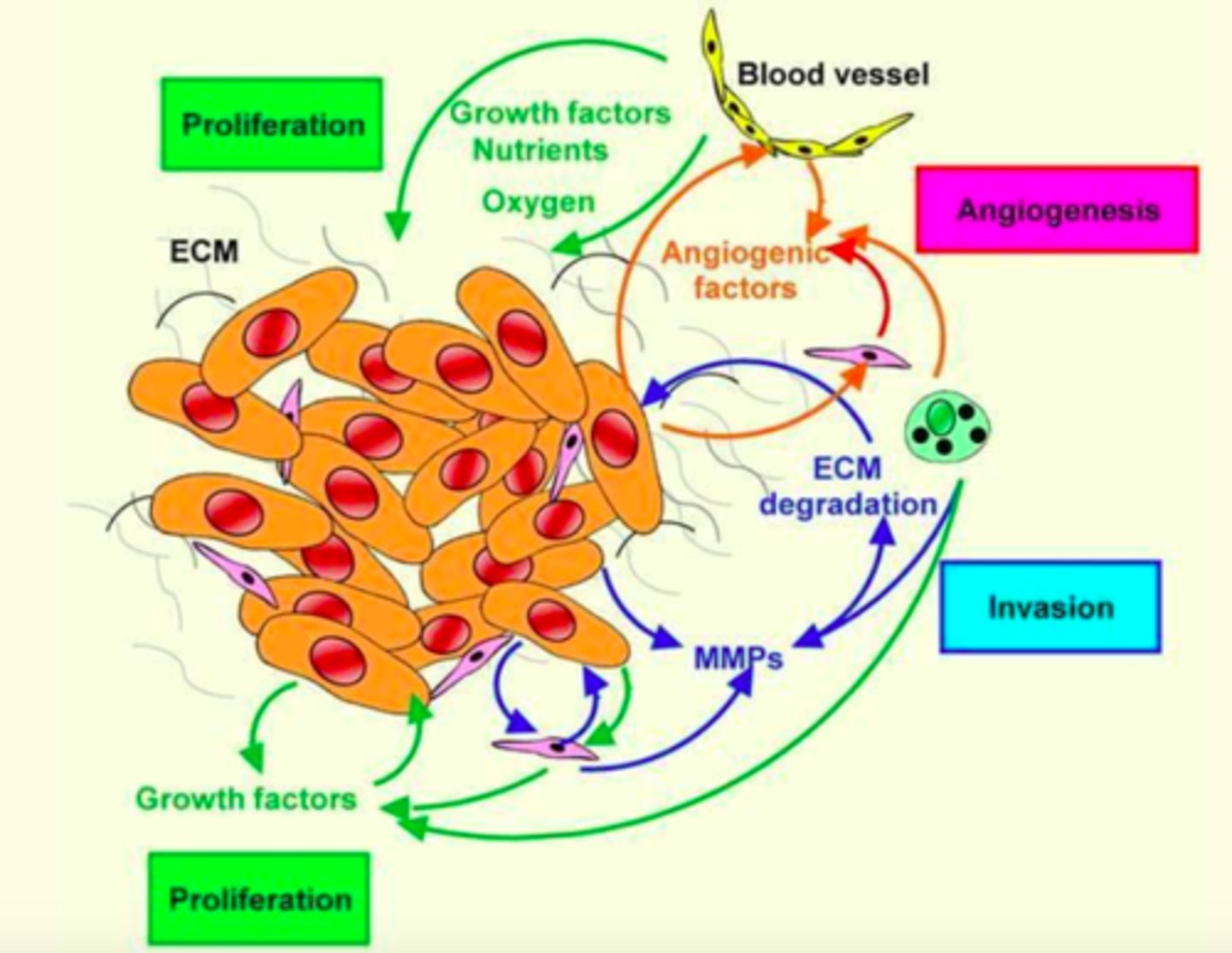
Process of invasion and metastasis of malignant cells
1) Grow and invasion at primary site
2) Enter transport system e.g., lymphatics/blood and lodge at a secondary site
3) Grow at secondary site to form a new tumour. At all points, the cells must evade destruction by immune cells, which depending upon the aggressiveness of the tumour - immune system may or may not be effective
The colorectal polyp to cancer progression model
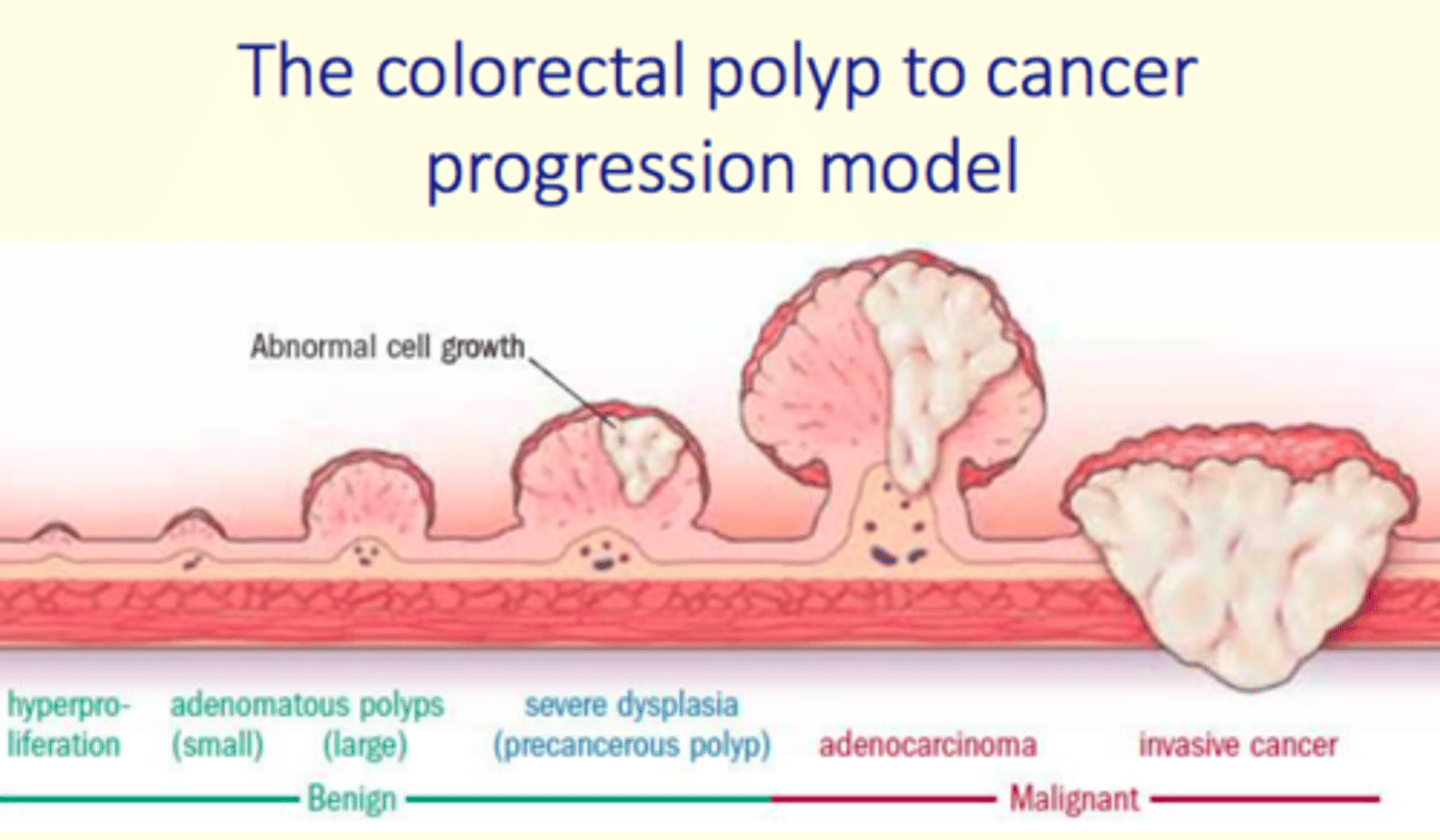
A collection of cells is known as 'monoclonal' if they all originated from a single founding cell.
How do we know that neoplasms are monoclonal?
Evidence that neoplasms are monoclonal came from the study of X-linked gene for the enzyme glucose-6-phosphate dehydrogenase (G6PDH) in tumour tissue from women
The gene has several alleles encoding different isoenzymes.
Early in female embryogenesis, one allele is randomly inactivated in each cell (lyonisation).
in heterozygous women that happen to have one allele encoding a heat stable isoenzyme and one heat labile isoenzyme, normal tissues will be a patchwork of each type.
However, neoplastic tissues only express ONE isoenzyme, indicating a monoclonal group of cells.
Invasion of cancer involves three important alterations which collectively create a carcinoma cell phenotype which appears more like a mesenchymal cell than an epithelial cell (EPITHELIAL TO MESENCHYMAL TRANSITION; EMT)
What are these three alterations?
1) Altered adhesion
Reduction in E-cadherin
Altered adhesion between malignant & stromal proteins involves changes in integrin expression.
2) Stromal proteolysis
Cells must degrade BM & stroma to invade successfully (proteases, matrix metalloproteinases; MMPs)
3) Altered motility
Altered motility involving change in actin cytoskeleton.
Signalling via integrins is important and occurs via small G proteins such as members of the Rho family.
The growth of cancer cells at a secondary site is known as ___
Colonisation
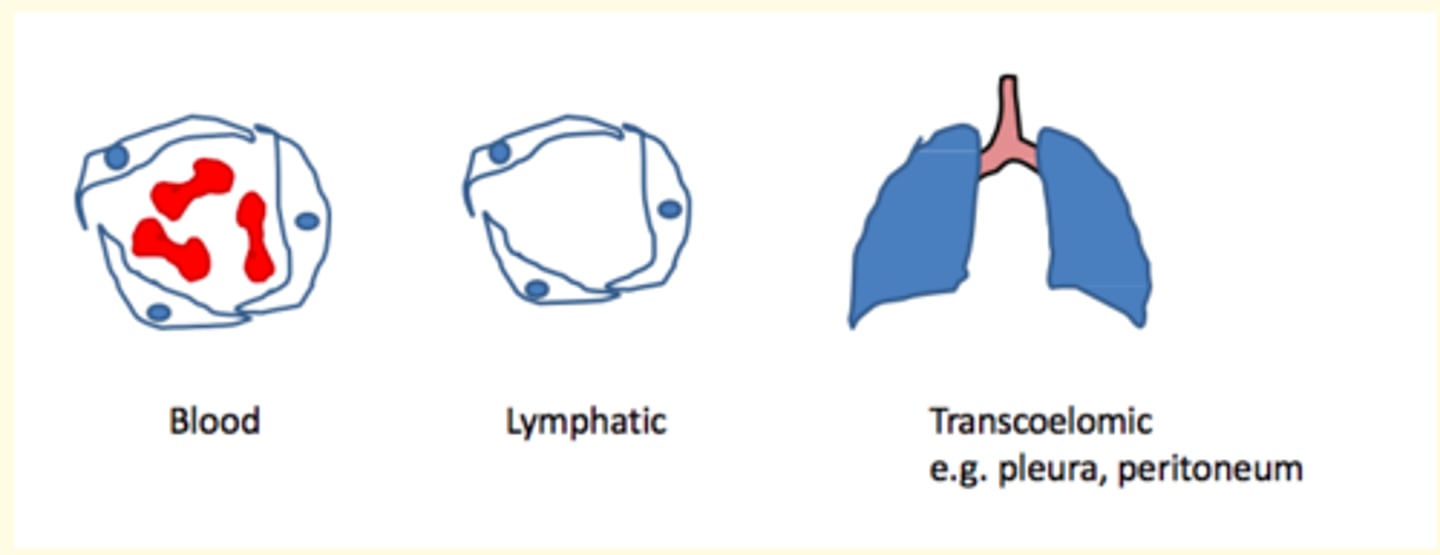
Malignant cells can be transported to distant sites via three routes, what are they?
What are the three routes of metastatic spread?
1) Blood vessels via capillaries/venules
2) Lymphatic vessels
3) Fluid in body cavities (pleura, peritoneal, pericardial, brain ventricles) = transcoelomic spread
Micrometastases
Many malignant cells lodge at secondary sites, but these tiny cell clusters often die or fail to grow into clinically detectable tumours.
Surviving microscopic deposits that do NOT grow are called micrometastases.
Describe the main steps involved in invasion of the ECM by tumour cells
1) Detachment of tumour cells from one another by unzipping of the anchor protein E-cadherin
2) Degradation of the ECM by collagenase which attacks the collagen fibres of the basement membrane
3) Loss of adhesion of cells from integrins
4) Migration of tumour cells through ECM
Stromal invasion involves three important alterations which are...
1) Cells degrade basement membrane & stroma using proteases (matrix metalloproteinase; MMP).
2) Malignant cells take advantage of other nearby non-neoplastic cells = which forms cancer niche. Normal cells provide growth factors/proteases that help cancer thrive.
3) Altered motility involves changes in actin cytoskeleton.
Circulating Tumour Cells (CTCs)
Tumor cells that have passed from tumor into blood; primary; place in research
How can CTCs be detected? What are the main methods of detection?
Flow cytometry
CellSearch system
High-def fluorescence scanning microscopy
Size sorting
Fibre optic/laser scanning techniques
Why is detection of CTCs useful?
May aid an earlier diagnosis, prognosis, prediction, stratification & pharmacodynamics
Tumour dormancy
When a malignant neoplasm relapses years after an apparent cure, it is typically due to one or more micrometastases starting to grow.
At the secondary site, malignant cells must get out of the vessel (___) and then grow to form a clinical metastasis. This is a dynamic process, involving ___, vascular ___ and endothelial ___
At the secondary site, malignant cells must get out of the vessel (extravasation) and then grow to form a clinical metastasis. This is a dynamic process, involving adhesion, vascular migration and endothelial remodelling (Twist gene)
What are the triggers for the development of a metastasis from a micrometastasis?
Complex process - not fully understood.
There must be an alteration in...
1) Microenvironment (soil) becoming more favourable
2) Immune status
3) Angiogenic switch
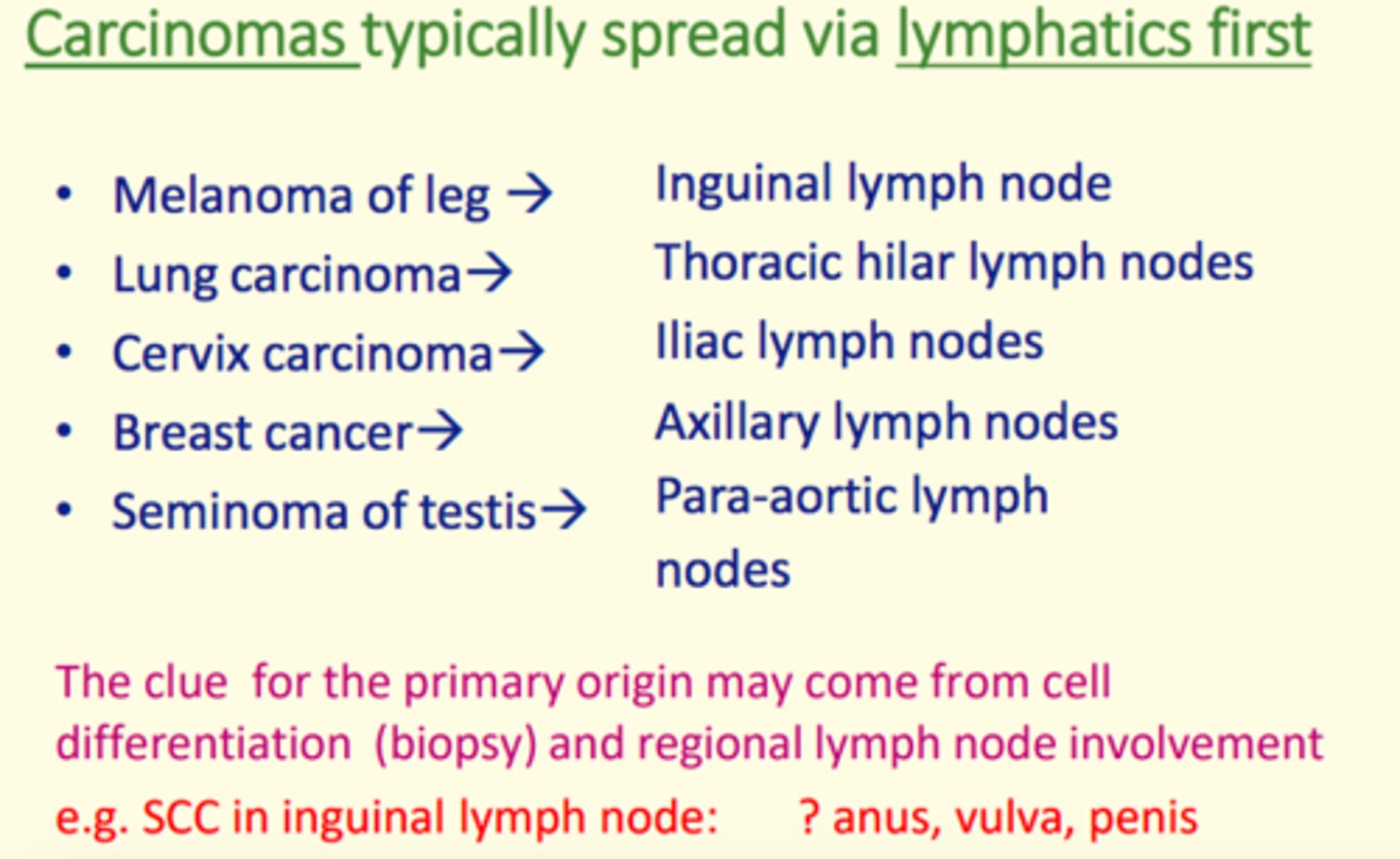
The site of a secondary neoplasm depends on two factors - what are they?
1) Regional drainage
Lymphatic metastasis usually spreads to lymph nodes
Transcoelomic spread usually spreads to other areas in coelomic space or adjacent organs
Bloodborne metastases spread to next capillary bed encountered
2) Seed-and-soil phenomenon
This can explain the unpredictable distribution of blood-borne metastases and is often due to interactions between malignant cells & local tumour environment (the niche) at the secondary site.
Carcinomas typically spread via...
Lymphatics
Sarcomas typically spread via...
Bloodstream
Neoplasms that most frequently spread/metastasise include...
Breast
Bronchus
Kidney
Thyroid
Prostate
Common sites of bloodborne metastasis include...
Lung
Bone
Liver
Brain
GI tract malignancies and melanoma tend to spread to...
Liver
Sarcomas and renal cell carcinoma tend to spread to...
Lung
Malignant neoplasms have personalities
Some malignant neoplasms are more aggressive and metastasise very early e.g., small cell bronchial carcinoma
Others almost never metastasise e.g., basal cell carcinoma (BCC) of the skin
Describe some of the DIRECT and LOCAL effects of neoplasms
1) Direct invasion/destruction of normal tissue
2) Ulceration at surface leading to bleeding
3) Compression of adjacent structures (e.g., in benign tumours)
4) Blocking tubes/orifices
Describe some of the INDIRECT SYSTEMIC effects of neoplasms...
- Paraneoplastic syndrome (release of hormones from tumour)
- Reduced appetite
- Cachexia (weight loss)
- Malaise
- Immunosuppression
- Thrombosis
Malignant tumours can often produce hormones leading to a paraneoplastic syndrome.
Give examples of tumours that can do this.
1) Bronchial squamous cell carcinoma = PTH-like hormone
2) Bronchial small cell carcinoma = ACTH or ADH
Miscellanous systemic effects of neoplasms...
1) Neuropathies affecting brain/peripheral nerves
2) Skin problems e.g., pruritus, abnormal pigmentation
3) Fever
4) Myositis
5) Finger clubbing
Benign neoplasms of endocrine glands are well differentiated and so typically produce hormones.
Give an example of a benign neoplasm that does this
A thyroid adenoma produces thyroxine
Contact inhibition
A process that stops additional cell growth when cells become crowded
Healthy cells stop dividing when it becomes crowded
Features of adenocarcinomas
- May produce mucin
- Can occur in thyroid gland
- Form glandular acini
- Contain intracytoplasmic cytokeratin
Features of dysplasia
- Loss of normal maturation
- Pleomorphism
- Increased mitotic activity
- High nuclear/cytoplasmic ratio
Tumours of soft tissues...
- More often benign (lipomas and leiomyomas)
- Are classified by tissue of origin
- If malignant, are referred to as 'sarcomas'
Some examples of malignant tumours
Multiple myeloma
Osteosarcoma
Lymphoma
Common sites of metastasis
Brain, liver, bone marrow
Cancer cells are posed with challenges in the circulation such as...
- Shear force
- Turbulence of blood flow
- Surveillance & attack from immune cells (NK cells)
- Lack of substratum
- Entrapment in capillary bed
Describe some ways in which cancer cells OVERCOME these challenges
Release of coagulation factors which form an outer platelet shield which eventually forms a tumour platelet microthrombi which protects cancer cells from shearing & turbulence forces
This prevents immune detection using platelet derived MHC class I coating
Differentiation
When cells progress from stem cells to fully mature cells, they differentiate into the fully mature cell of that tissue.
A benign neoplasm has cells that closely resemble the parent tissue = they are well differentiated.
Malignant neoplasms range from well to poorly differentiated.
Cells with NO resemblance to any tissue = anaplastic.
A fully evolved malignant neoplasm exhibits six hallmarks of cancer and two enabling features.
What are they?
Six Hallmarks of Cancer
1) Self-sufficiency in growth signals
2) Resistance to stop signals
3) Cell immortalisation
4) Sustained angiogenesis
5) Resistance to apoptosis
6) Ability to invade and produce metastases
Two Enabling Features
1) Genomic instability
2) Inflammation (local chronic inflammation and angiogenic steal)