xray interpretation
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
106 Terms
criteria for diagnostic quality in interpretation principles
appropriate modality for clinical question
shows full region of interest
criteria of perception in interpretation principles
ability to recognize an abnormality
review entire image
knowledge of normal anatomy and anatomic variation
criteria of cognition in interpretation principles
ability to arrive at appropriate dx
knowledge of disease mechanisms and key features
the four steps to take in overview of the interpretation principles
select appropriate image type
make sure image is of diagnostic quality
identify presence of any abnormalities in the image
determine what the abnormality is → differential dx
what is image selection
selecting the type of image that is suitable for the task to meet diagnostic objectives
the type of image selection that is suited for the diagnostic task should be guided by: (4)
preceived by nature or severity of abnormality (size and accessibility)
efficacy of technique to accurately reveal characteristic radiographic features of abnormality
amount of image detail required for dx
radiation dose; accessibility and cost to pt
what are the 4 main imaging modalities
intraoral
panoramic
CBCT and MDCT
MRI
which imaging modality has highest spatial resolution relative to other modalities in dentistry
intraoral
what is intraoral imagining best used for
evaluating disease involving teeth and supporting structures
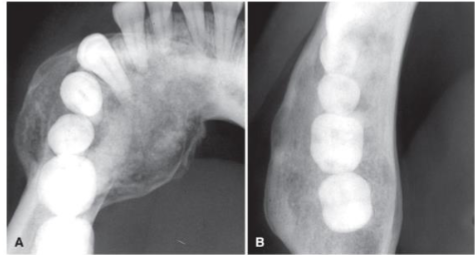
when are PANOs indicated for dx, what is the downside
allows for examination of a larger area; lower image resolution and more artifact (than intraoral)
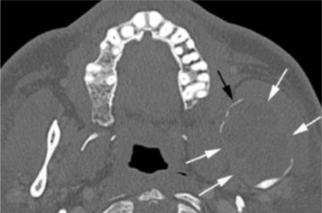
when is CBCT/MDCT indicated
when there is a need to evaluate anatomy in multiple dimensions without anatomical superimposition
when is MRI indicated
soft tissue evaluation
limitations to MRI compared to MDCT
MRI has more info than MDCT, but at lower resolution and hard tissues less well visualized
what are the imaging modality steps
clinical evaluation
check prior imaging
2D images
CBCT/MDCT
MRI
nuclear medicine
when is 3D imaging indicated
if standard 2D imaging is inadequate for diagnostic task
what is a full-mouth radiographic series (FMX)
survey of whole mouth intended to display crowns and roots of all teeth, periapical areas, interproximal areas and alveolar bone including edentulous areas
limitations to periapical images
limitation to geometric distortion
BWXs are optimal for…
revealing interproximal caries
project the crests of the alveolar processes relative to adjacent teeth w minimal distortion
when would you use PAs instead of BWXs to evaluate caries extent and assess periodontal bone loss
when you are evaluating anterior teeth
there are a few disadvantages in PANOs, what are some
susceptibility to pt positioning and movement
unequal magnification and geometric distortion across image
complex pattern of superimposition of anatomic structures challenges interpretation
occasionally overlapping structures can hide lesions
PANO compared to intraoral…
PANO not as useful detecting small carious lesions, fine structure of periodontium, or early periapical disease
PANOs information compared to an FMX
PANO doesn’t provide much additional useful information beyond an FMX for most pts
what does it mean for a radiograph to have image quality
the reliability of an image in its representation of the true state of anatomy examined
what are the parameters of image quality (5)
image sharpness
spatial resolution
contrast resolution
magnification
distortion
what are the 3 points in quality criteria that radiographs should have
record the complete area of interest in the image
have the least possible amount of magnification and distortion
have optimal contrast and spatial resolution to facilitate interpretation for the dx task
what is the point of systematic search strategy
have a list of normal anatomic structures to look at to:
improve detection of abnormalities
helps avoid ‘satisfaction of search’
what is diagnostic reasoning
method of identifying features of the abnormality that will assist in arriving at a plausible interpretation or dx
in diagnostic reasoning, feature memorization is generally less effective than…
understanding basic disease mechanisms for interpretation accuracy (don’t just memorize features of disease, you should understand pathogenesis)
what are the two types of diagnostic reasonings
non-analytical
analytical
what is the non-analytical strategy in dx reasoning
assumes viewing abnormality in its entirety on a global level leads to a more holistic dx hypothesis
deliberate search for deatures that support the hypothesis → “pattern recognition”
success is limited by experince level
what is the analytical strategy in diagnostic reasoning
a step-by-step analysis of features which are used to make interpretation/dx
reduces bias and premature closure of decision making process
it is best to use non-analytical and the analytical strategy together, what should you avoid in diagnostic reasoning
avoid use of non-analytical alone
avoid rote memorization of lesion features
what are the 2 steps in the analytical strategy
describe lesion features
interpret significance of the observed feature
what is the importance of the second step of the analytical strategy: interpret significance of the observed features
use features to determine disease category
narrow down to differential dx
what should your description include in the analytical strategy
L- location
E- edge
S- shape/size
I- internal content
O- other structures
N- number
what are the 5 steps to take in analysis of intraosseous lesions
localize the abnormality
assess periphery and shape of abnormality
analyze the internal structure
assess effects of lesion on adjacent structures
formulate an interpretation
what is an epicenter
geometric center of a lesion of the mesial-distal, superior-inferior, and buccal-lingual extensions
how can an epicenter help identify a lesion
may assist in determining cell or tissue type the lesion is derived from; is less accurate w very large, poorly-defined lesions
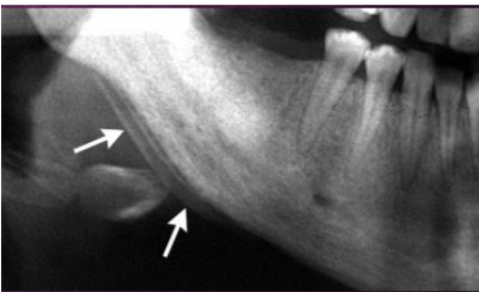
if the epicenter of a lesion is located WITHIN the IAC, what is the more likely origin of the lesion
likely neural or vascular
if there is irregular widening w cortical destruction of the IAC, what is the more likely origin of the lesion
may indicate malignant neoplasm in the canal
if the epicenter of a lesion is located ABOVE the IAC, what is the more likely origin of the lesion
likely odontogenic
if an epicenter of a lesion is located BELOW the IAC, what is the more likely origin of the lesion
likely non-odontogenic
if the epicenter of a lesion is in the ramus, coronoid, or condyle or within the maxilla sinus, what is the more likely origin of the lesion
non-odontogenic
certain lesions tend to be found in certain locations but this does NOT mean…
you should use location alone when formulating a diagnosis
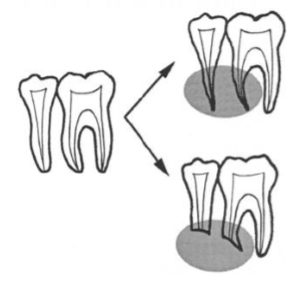
how to describe a lesion extent in multiple dimensions
peri-coronal
peri-apical
inter-radicular

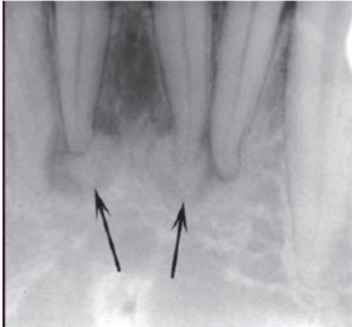
describe the location of this lesion
in the L posterior mandible, pericoronal to #17, involving the IAC and #18
what are the 3 vocabulary words we can use to describe the periphery/border of a lesion
well defined
poorly defined
zone of transition
narrow vs wide
what is the zone of transition
how “quickly” normal bone transitions to abnormal
do well-defined lesions tend to benign or malignant
benign
do poorly-defined lesions tend to malignant or benign
malignant
what are some terms that can be used to further describe a well-defined border
punched out
corticated
sclerotic
radiolucent periphery
what is the term punched out and what is it commonly associated w
sharp, narrow zone of transition, non-corticated
tends to be associated w multiple myeloma
what is the term corticated and what is it commonly associated w
thin, radiopaque line of bone at lesion periphery
associated w benign, slow-growing process
what is sclerotic and what is it commonly associated w
wider, more diffuse zone of transition
reflects ability of lesion to stimulate bone production→ reactive bone formation
what is the term radiolucent periphery and what is it commonly associated w
rim of radiolucency representing soft tissue
associated w benign, slow-growing lesions
generally w outer corticated border and inner/internal radiopacity
how would describe a border that is both well-defined and kind of poorly-defined
whichever is the majority, is how the lesion will be classified
terms that can be used to define a poorly-defined lesions
blending
invasive
what is the term blending
gradual, wide zone of transition
focus on trabeculae rather than marrow spaces
what is the term invasive
wide zone of transition w few or no trabecular between lesion periphery and normal bone→ is more focused in marrow space
associated w rapid growth and aggressive and malignant lesions
invasive can also be called…
permeative: lesion appears to grow through trabeculae producing finger-like extensions

describe the periphery of the lesion
sclerotic, poorly-defined, blending border
what are the terms that can be used to describe size and shape of a lesion
circular or hydraulic shape
unilocular
scalloping
what is circular or hydraulic shape commonly associated w
like a balloon: is a characteristic of a cyst
what is a unilocular shape
means one, corticated, single, well-defined, radiolucency
what is scalloping
series of contagious arcs or semicircles that may develop around roots of teeth or in adjacent bones or cortices
what can scalloping also be called
lobulated or loculated
what is scalloping commonly assoicated w
can be seen in cysts and benign neoplasms; may reflect mechanism of lesion growth
what are the 3 basic categories describing the internal structures of lesions
entirely radiolucent
entirely radiopaque
mixed radiolucent and radiopaque
what does an entire radiolucent lesion represent
normal bone is resorbed
what does an entire radiopaque lesion represent
lesion filled w mineralized matrix
what does a mixed radiolucent and radiopaque lesions represent
clacified material is deposited against a radiolucent background
describe this lesion
lesion is periapical to #24/25, well-defined, mildly sclerotic, w mixed density of radiolucency and radiopacity
what are the types of mixed-density internal structures of lesions:
abnormal trabecular patterns
internal septation
dystrophic calcification
amorphous bone
tooth structure
what are abnormal trabecular patterns
variations in numbers, lengths, thickness and orientations of trabeculae
is internal septation referring to unilocular or multilocular
multilocular- compartments created by septations (striations of bone within lesion)
multilocular lesions can be associated w:
trapped, normal, residual bone
could have been manufactured/created by lesion
appearance of septa can indicate nature and pathogenesis of lesion
what does dystrophic calcification mean
mineralization in damaged soft tissue
what is amorphous bone
dense, often cortical-like bone, but poorly organized
why is it important to look at adjacent structures when describing a lesion
used to infer biologic behavior of a lesion
may aid in dx
understanding disease mechanisms that give rise to changes in required
what are some effects on adjacent structures you can note about a lesion
displacement of teeth
resorption of teeth
widening of PDL
surrounding bone rxn
inferior alveolar canal and mental foramen
cortical boundaries of bone
periosteal rxn
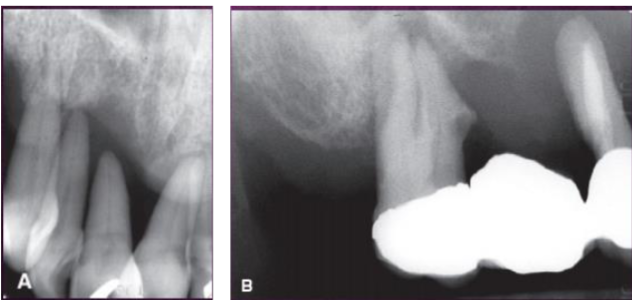
if you see displacement of teeth from a lesion (tipping), what is this commonly associated w
benign, slower-growing, space-occupying lesions
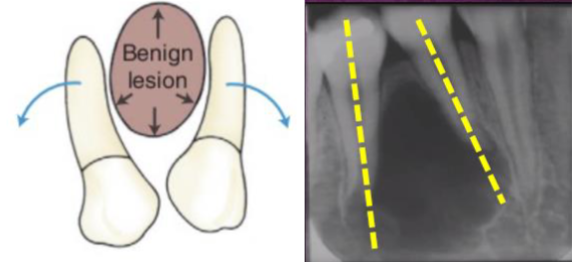
if you see bodily displacement of a tooth/teeth, what type of lesion can this be associated w
most associated w a tumor over a cyst
if you see resorption of teeth from a lesion, what is this commonly associated w
slower-growing, benign process but may result from chronic inflammation
some malignant tumors can occasionally resorb teeth
how can we differentiate malignancies from benign lesions when looking at the resorption of the tooth
malignant: more likely to have thinning or “spiking” root appearance
benign: tend to have smooth borders or resorption continuous w lesion
what should pay attention to when assessing the PDL
observe whether widening is localized or generalized, irregular or uniform, as well as epicenter of widening
adjacent lamina dura should also be assessed
PDL widening w epicenter at apex will imply…
source of inflammation probably from pulp → from pulp necrosis
PDL widening coronal epicenter near crest implies…
source of inflammation is probably periodontal→ periodontal disease
what can the surrounding bone rxn suggest about the lesion
abnormality can stimulate osteoblastic rxn
why is there a corticated border around a cyst
is a bone rxn that develops in response to its enlargement; is NOT part of the cyst
why is it important to evaluate the IAC and mental foramen
changes to IAC can be a characteristic of a specific disease process
why is it important to evaluate cortical boundaries
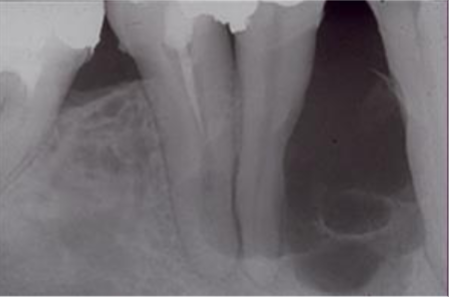
may remodel in response to lesion growth; shape and amount of expansion can provide information about the way the entity is growing and hint at the type of lesion
cortical boundaries of bone may remodel in response to lesion growth, SLOW growth of cortical boundaries allows…
time for new bone formation and expanded surface remains intact; suggests benign lesion
cortical boundaries of bone may remodel in response to lesion growth, RAPID growth of cortical boundaries will outpace…
new formation and cortex lost (eroded); suggests malignancy
if you see more erosion, less expansion, and “floating teeth” this suggests what type of lesion
an agressive, fast-growing malignancy
what are the types of periosteal rxns we can see from a lesion
onion skin pattern
spiculated bone pattern
sunburst pattern
what is the onion skin pattern
layering of new bone mostly seen in inflammatory lesions and more rarely in tumors
what is spiculated bone pattern
formed at right angles to the surface cortex seen w metastatic lesions
what is a sunburst pattern
more exuberant radiating pattern of bone seen in osteosarcoma or hemangioma
what does formulate interpretation means in terms of cognition
elucidate the meaning of observations: determine the significance of observed features and combine clinical info w radiographic description
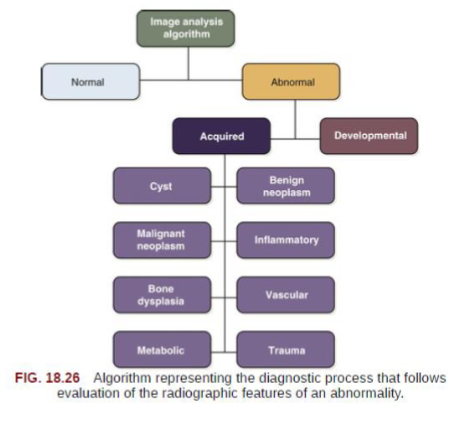
what is the interpretation algorithm (decision tree)
normal or abnormal
developmental or acquired
disease classification/category (if acquired)
ways to proceed