Biochemistry Class 9 - Renal and Digestive Systems
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
73 Terms
What are the excretory organs (3)?
Colon, liver, kidney
What does the colon do?
Excretes material that was eaten, but not absorbed
Solid waste
What does the liver do?
Excretes material that was eaten and absorbed, but not dissolved in plasma
Eliminates hydrophobic waste
What does the kidney do?
Eliminates material that was eaten, absorbed, and dissolved in the plasma
Hydrophilic waste
Regulates blood pressure, ion balance, water balance, pH
Secretes erythropoietin to stimulate red blood cell formation
Activates vitmain D
Why are kidneys sensitive to drops in oxygen?
Its functions involve a lot of active transport → thus ATP → thus oxygen
When O2 drops → send out erythropoietin → make more RBCs to carry more O2
What is the anatomy of the renal system?
Kidneys, ureter, bladder, urethra, internal urinary sphincter, external urinary sphincter
All but kidneys are muscular → push urine through
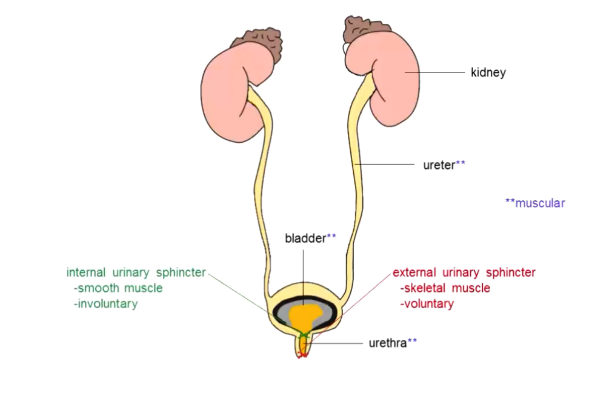
What does the internal urinary sphincter do?
Smooth muscle, involuntary control of urination
What does the external urinary sphincter do?
Skeletal, voluntary muscle
Voluntary control of urination
Below internal urinary sphincter
What is the anatomy of the kidney?
Renal pelvis, ureter, cortex, medulla, nephron
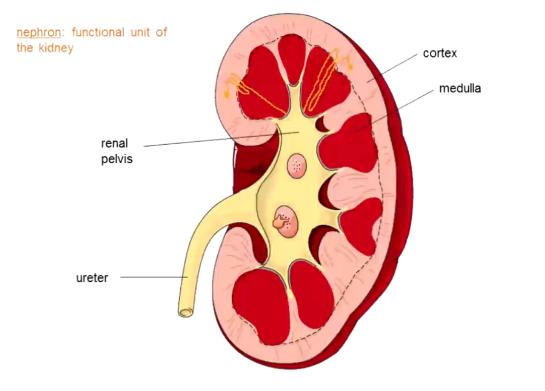
What is a nephron?
Functional unit of the kidney
How does urine go through kidneys?
Nephron begins in cortex → can dip into medulla → filters blood → blood travels through it → drains into renal pelvis → cannot be modified → into ureter
What three processes do nephrons do?
Filtration: moves blood plasma across the capillary wall (single layer of cells) using blood pressure → why kidneys regulate blood pressure
Reabsorption: move a substance from the filtrate back to the blood (glucose, amino acids, water)
Secretion: move a substance from blood and into filtrate (drugs, toxins, creatinine)
Ions are reabsorbed (Na+, HCO3-) and secreted (H+, K+) as necessary
How long can you live without functional kidneys (with no intervention)?
2 days
What is the glomerular filtration rate (GFR)?
125 mL/min
How much blood kidneys filter
Entire blood volume in under an hour
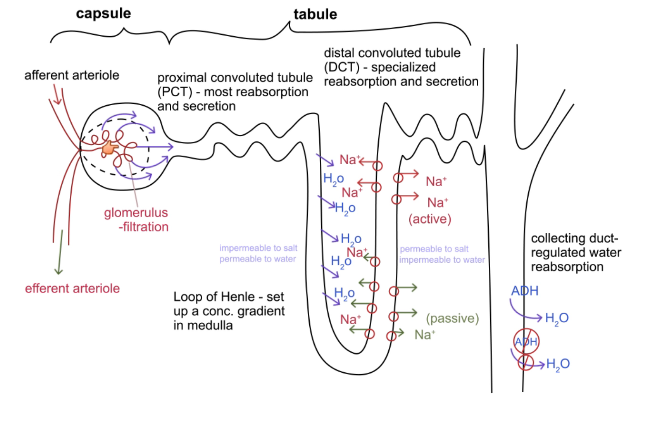
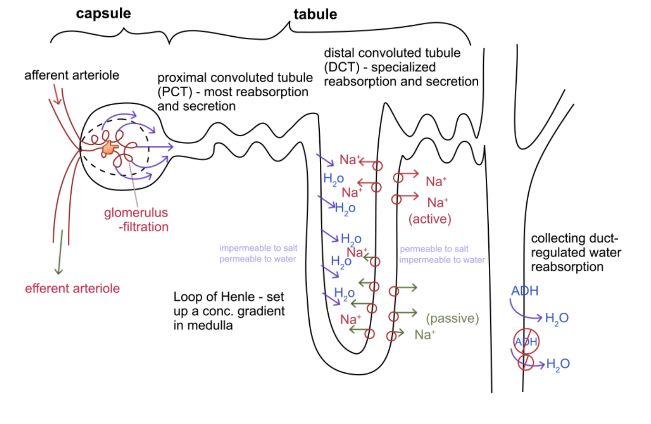
What is the structure of the nephron?
Capsule: glomerulus
Tubule: proximal convoluted tubule, loop of Henle, distal convoluted tubule
Collecting duct

Why are glomeruli important? Why are they unique?
Filter blood: they are porous enough to let small molecules through, but not proteins or cells
Special: supplied with blood an artery and drained by an artery (not a vein)
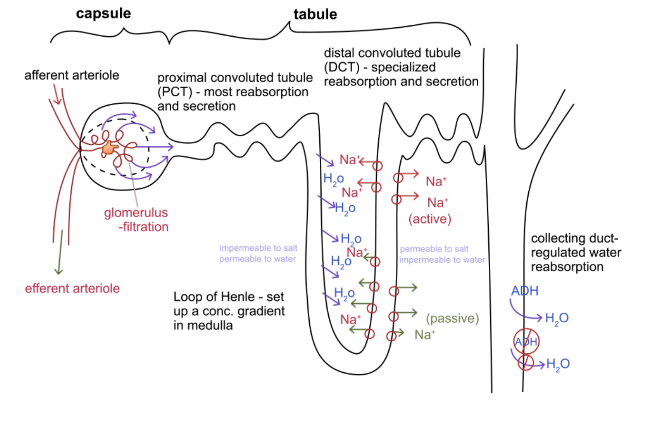
How does the glomerulus recieve and get rid of blood?
Receives through afferent arteriole (approaching)
Gets rid of through efferent arteriole (exit)
Important that both are arteries → they can contract to help control pressure → blood filters at a normal rate
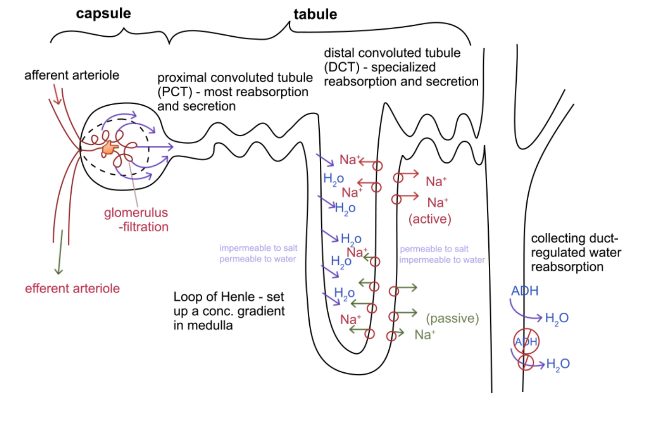
What is the proximal convoluted tubule?
Twisted up part of tubule closest to glomerulus
Most reabsorption and secretion
Relatively unregulated
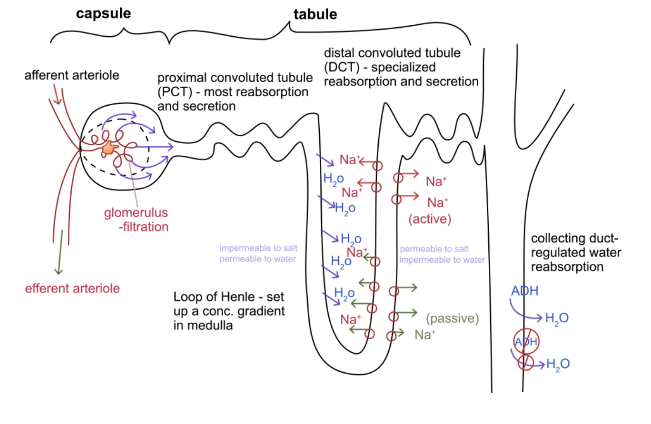
What does the loop of Henle do?
Sets up a gradient in the medulla (saltiness/osmolarity increases as you get further into the medulla)
Each side of the loop has different permeabilities: descending side is only permeable to water, ascending side is permeable to salt and not water (active transport at the top)
No gradient in descending side, but a gradient is set up in the ascending side
Blood in efferent arteriole (does not have much water/super concentrated with proteins and shit) passes by the loop of Henle → water drawn in → this removes the water and sets up a salt gradient in the medulla
How concentrated is urine once it passes through the loop of Henle?
4x more concentrated than normal plasma for short loops
Some animals have lots of long loops, so up to 12x more
In humans, after the loop of Henle, urine is roughly isotonic to plasma
What does the distal convoluted tubule do?
DCT
Specialized reabsorption and secretion
Where aldosterone, parathyroid hormone, and calcitonin affect sodium and calcium reabsorption
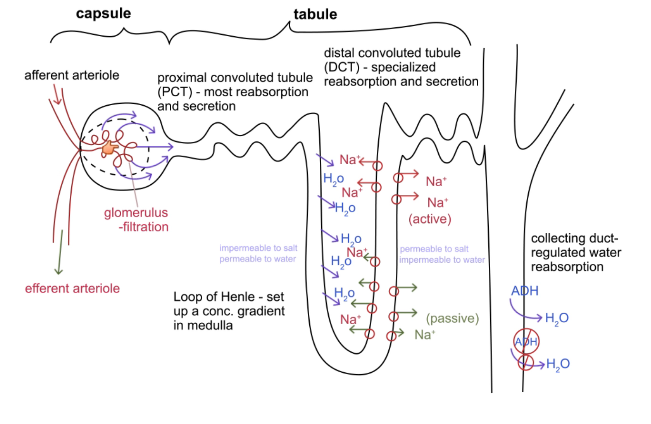
What does the collecting duct do?
Picks up urine from several nephrons
Regulated water reabsorption → retain more if dehydrated
Based on ADH (antidiuretic hormone)
ADH increases how much water is retained by increasing the permeability of the cells to water
How do diuretics work?
Inhibit ADH so you do not retain water when your body needs it
What is the renin-angiotensin system?
Blood pressure falls → kidney secretes renin → angiotensinogen converted to angiotensin I → active → angiotensin converting enzyme (ACE) converts angiotensin I to II → systemic vasoconstriction and increased aldosterone release
How does systemic vasoconstriction affect blood pressure?
All arteries are contracted → increases blood pressure
How does increased aldosterone release affect blood pressure?
Aldosterone released → increased Na + reabsorption → increases blood osmolarity → increased release of ADH → retain more water → increased blood volume → increased blood pressure
Why is blood pressure important?
If too low → cannot drive the flow of blood (organs do not get enough blood)
If kidneys do not get blood → no filtration
What is the juxtaglomerular apparatus?
Contact point between afferent artery and distal convoluted tube (because they are all twisted and shit)
Afferent artery has baroreceptors → detect fall of blood pressure → release renin
Distal tubules have chemoreceptors → detect filtrate osmolarity falling → stimulate afferent artery to release renin and directly dilates the afferent artery
How does ANP regulate blood pressure?
High blood pressure → atria of heart stretch → right atrium releases ANP (atrial natriuretic peptide) → vasodilation and inhibition of renin and aldosterone release
Prevents retention of sodium, thus water
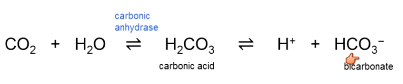
How is pH regulated by the kidney?
Takes several hours/days → respiratory can do this in a couple seconds
All kidney tubule cells have lots of carbonic anhydrase → always have H+ and HCO3-
Generally reabsorb bicarbonate and secrete protons
Blood pH is 74, urine pH is 6.5
When blood pH is too high, stop absorbing bicarbonate
Stop secreting hydrogen when blood pH is high
When pH is low: absorb more bicarbonate, secrete more protons
What are the digestive accessory organs?
Digestive role, but not part of digestive tube
Liver, gallbladder, pancreas, salivary glands
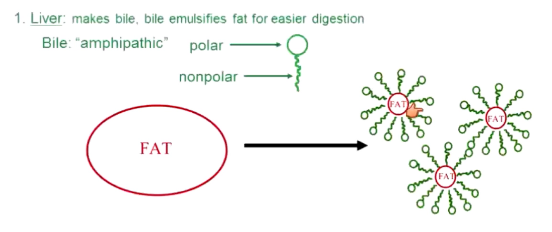
What does the liver do for the digestive system? Is it essential?
Produces bile
Cannot live without it
What does bile do?
Emulsifies fat for easier digestion
Fat wants to clump in fat globs → hard to digest → bile is amphipathic and breaks big fat globs into small ones → easier to digest
Does not actually digest anything
What does the gallbladder do? Is it essential?
Stores and concentrates bile
You can live without it, but cannot eat very high fat diets
What causes gallstones?
Gallbladder stores and concentrates bile too well → bile mixes with cholesterol and such → jam bile duct → gallbladder inflames → impaired
What does the pancreas do? Endocrine role
Excretes insulin and glucagon
What does the pancreas do? Exocrine role.
What if it cannot do this?
Source of digestive enzymes: proteases, lipases, amylases, nucleases
Produces bicarbonate to neutralize stomach acid and bring intestinal pH to a more normal level (6 -7)
If your pancreas is non-functional → malnutrition
How is the alimentary canal wall structured?
From inner to outer: lumen → mucosa → submucosa → circular muscle (runs around) → longitudinal muscle (runs parallel) → serosa (connective tissue)
How do circular and longitudinal muscles function in digestion?
Circular muscles constrict → where they are super thick and contract enough to close the tube, they are called sphincters → act as valves
Longitudinal muscles cause the tube to become shorter → helps with peristalsis
What is peristalsis? Analogy.
Movement through digestive tract
Like threading a drawstring through a sweatpants band
What is the function of the mouth?
Grind food, moisten food, begin starch digestion
What is the structure of the mouth?
Teeth, tongue, salivary glands (technically a digestive accessory organ)
What is the exocrine function of the mouth?
Saliva: mostly water, mucus, and enzymes
Slightly basic
Lysozyme kills bacteria
Amylase digests starch
What are endocrine functions of the mouth?
None
What is the function of the esophagus?
Tube to bring food to stomach
What is the structure of the esophagus?
Stars as skeletal muscle (voluntary) → becomes smooth (involuntary)
Cardiac sphincter: prevents stomach contents from refluxing → failure causes acid reflux
What are exocrine secretions of the esophagus?
Mucus
What are endocrine secretions of the esophagus?
None
What is the function of the stomach?
Very limited digestion and absorption
Storage tank for food
What is the structure of the stomach?
Gastric glands
Pyloric sphincter: regulates entry into small intestine
What is the anatomy of gastric glands?
Mucus cells at top of pit
Parietal cells midway down
Chief cells at the bottom
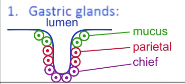
What are exocrine secretions of the stomach?
Mucus cells make mucus
Parietal cells secrete HCl
Chief cells secrete pepsinogen (innate immunity) (inactive form is secreted → travels to lumen → activated by acid)
What does pepsinogen do?
Degrades proteins of bacteria, viruses, and some neurotoxins
What is the endocrine function of the stomach?
G cells scattered throughout the stomach lumen secrete gastrin
What does gastrin do? How is it regulated?
Hormone that increases activity of gastric glands → decreases pH
Regulated via negative feedback of pH: pH falls → release of gastrin stops → gastric glands stop → pH rises)
What is the function of the small intestine?
Almost all digestion and absorption
What is the structure of the small intestine?
Duodenum: first ~5%
Jejunum: mid ~40%
Ileum: last ~55%
Massive increase in surface area for absorption
What causes the increase in surface area in the small intestine?
Mucosa folds up (folds called plicae)
Plicae have villi
Villi have microvilli
All serve to increase surface area
What are exocrine secretions of the small intestine?
Enterokinase (aka enteropeptidase)
Brush border enzymes
What does enterokinase do?
Activates trypsinogen to trypsin (pancreatic protease) to set of a cascade of enzyme activations
What are inactivated enzymes called?
Zymogens
Named “(name of enzyme) ogen”
What do brush border enzymes do?
Disaccharidases and dipeptidases
Last step in digestion of sugars and proteins
What are endocrine secretions of the small intestine?
Enterogastrone
CCK (cholecystokinin)
Secretin
What is enterogastrone?
Hormone of small intestine
Reduces stomach motility triggered by food in the intestine → so you do not put too much in at once
What does CCK (cholecystokinin) do?
Hormone of small intestine
Increases bile release from liver and gallbladder
Triggered by fat and proteins
What does secretin do?
Hormone of small intestine
Increases bicarbonate release from pancreas
Triggered by low pH
What is the function of the large intestine?
Reabsorb water
Stores feces
What is the structure of the large intestine?
Colonic bacteria
Ileocecal valve
Internal/external anal sphincters
What do colonic bacteria do?
Secrete vitamin K
Digest leftover nutrients so pathogenic bacteria cannot grow
What is the role of the ileocecal valve?
Usually closed
Relaxes when there is food in stomach → you have to shit 30 mins after eating ish
What are the internal and external sphincters?
Internal: smooth/involuntary
External: skeletal/voluntary
Allow you to shit (like urinary sphincters do for peeing)
What are the exocrine secretions of the large intestine?
None
What are the endocrine secretions of the large intestine?
None