Study guide week 8- heart disease, heart failure, intro to renal
1/115
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
116 Terms
T/F Heart disease and heart failure are the same thing
False! You can have heart disease and not be in heart failure
AV valve and aortic valve regurgitation result in extra _______ work leading to _________ hypertrophy.
-volume
-eccentric
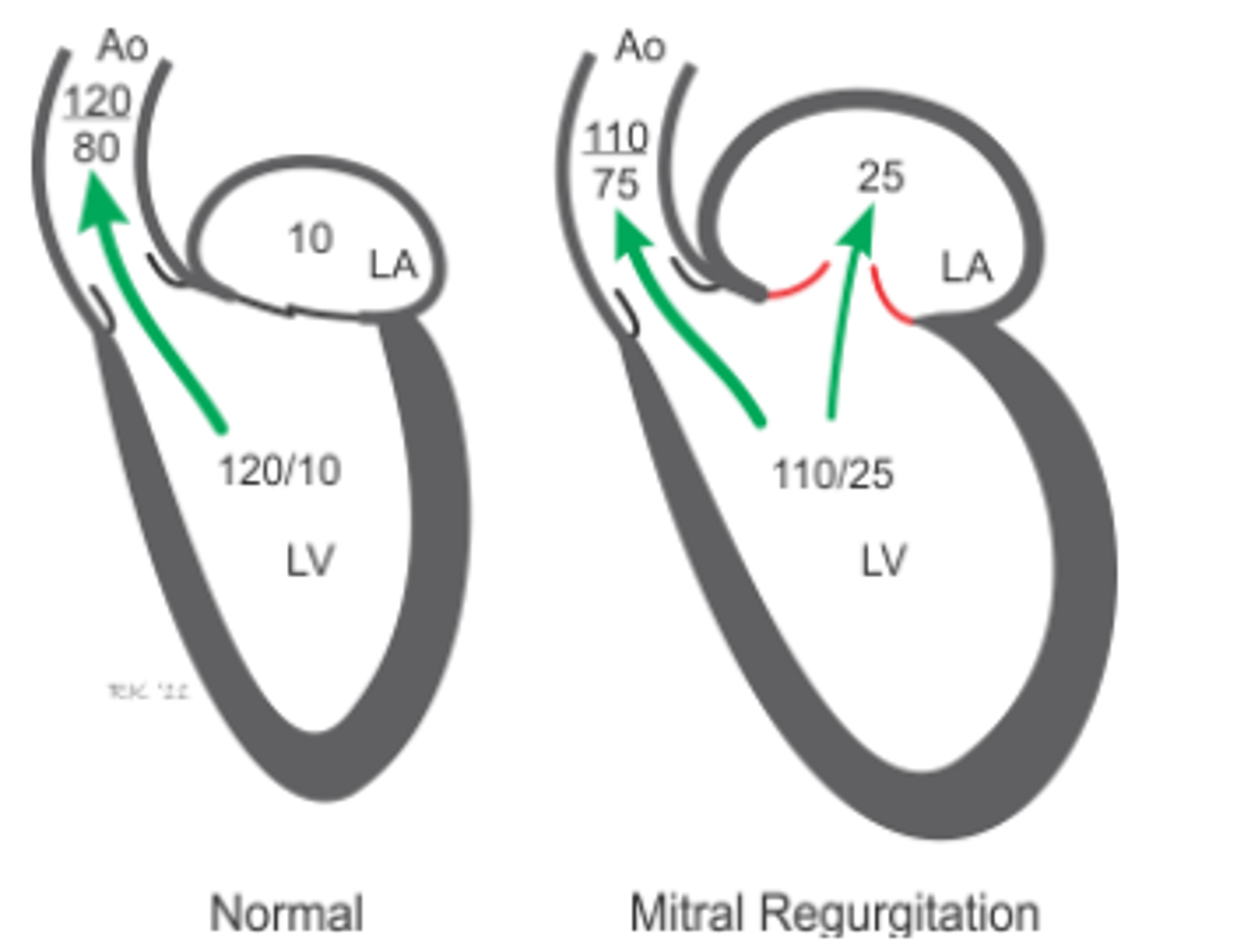
In a mitral regurgitation, what occurs to the pressures within the aorta, Left ventricle, and Left atrium?
Aorta: systolic & diastolic is lower
LV: systolic is lower but diastolic is higher
LA: higher
In aortic regurgitation, what occurs to the pressures within the aorta, Left ventricle, and Left atrium?
Aorta: systolic is higher and diastolic is lower
LV: systolic is higher and diastolic is higher
LA: higher
As a general rule, as the murmur grows louder, what is happening the heart and leak in mitral regurg?
The heart is englarged and the leak is worse.
Is the dog has a respiratory sinus arrhythmia and has a normal sleeping respiration rate, is it likely they are in heart failure?
Much less likely, even with a loud murmure
In a mitral regurgitation, how does the heart compensate for the decreased Forward stroke volume?
Venous return must increase to increase preload which will in turn increase total stroke volume to maintain forward stroke volume. The stressed volume must expand.
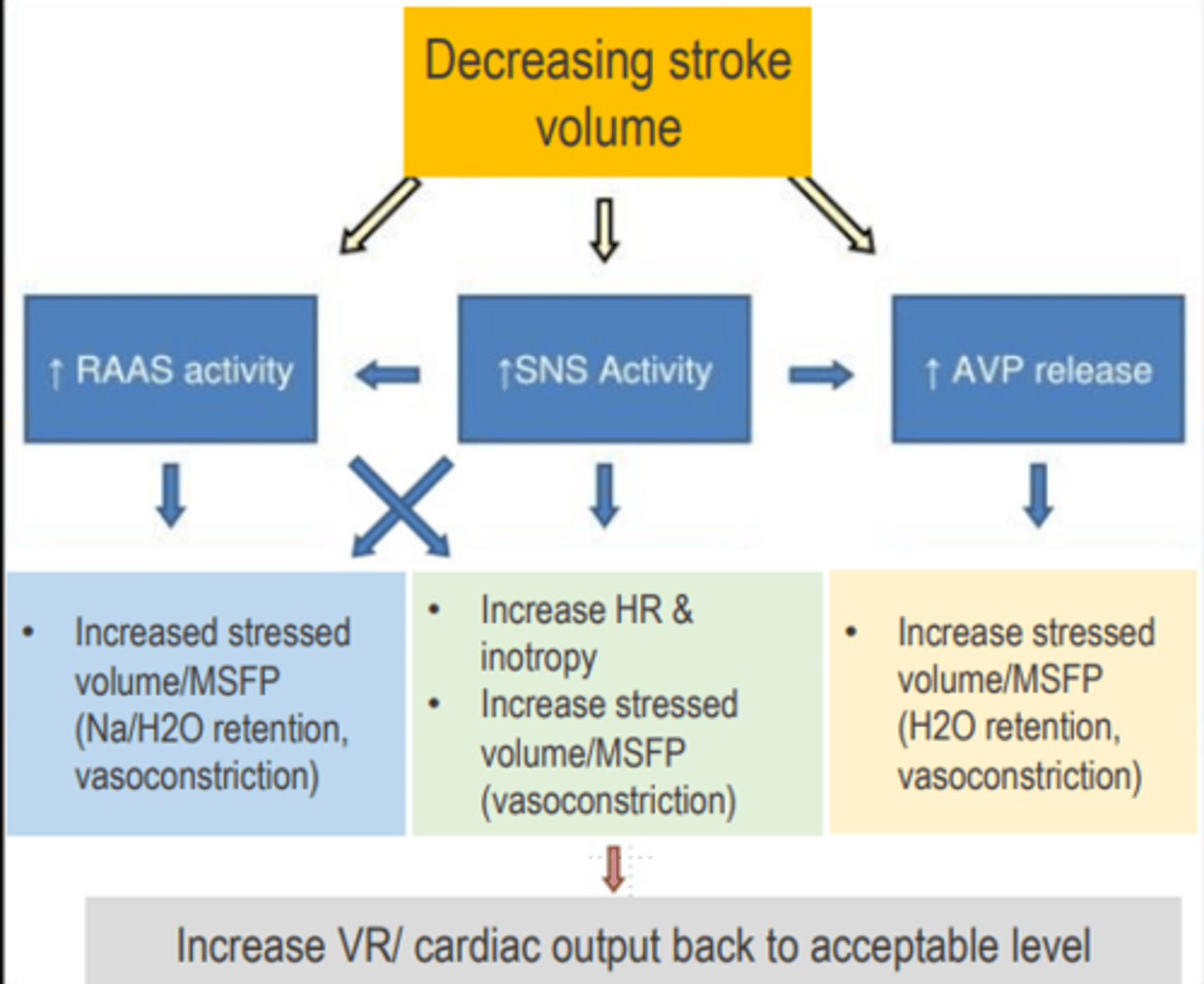
When the body needs to increase its stressed volume, what are 2 ways the body does this?
How do we increase cardiac output?
1.Retain sodium & water (RAAS, ADH)
2.Sympathetic venoconstriction
A. Increase inotropy and chronotropy via sympathetic stimulation. If systolic dysfunction, SVR may also be increased to maintain MAP
In regurgitation, what happens to the atrium feeding the affected ventricle?
The atrium will enlarge to increase Ventricular filling volume (EDV) and to increase TSV. Eventually, end diastolic and atrial pressure increases.
Are acquired cardiomyopathies disease of the muscle or valves?
Disease of the muscle
Do cat cardiomyopathies typically affect diastolic or systolic function? Name an example of a common issue
Diastolic function (impair filling)
Hypertrophic cardiomyopathy (HCM) Unclassified cardiomyopathy (UCM) aka non-specific Restrictive cardiomyopathy (RCM)
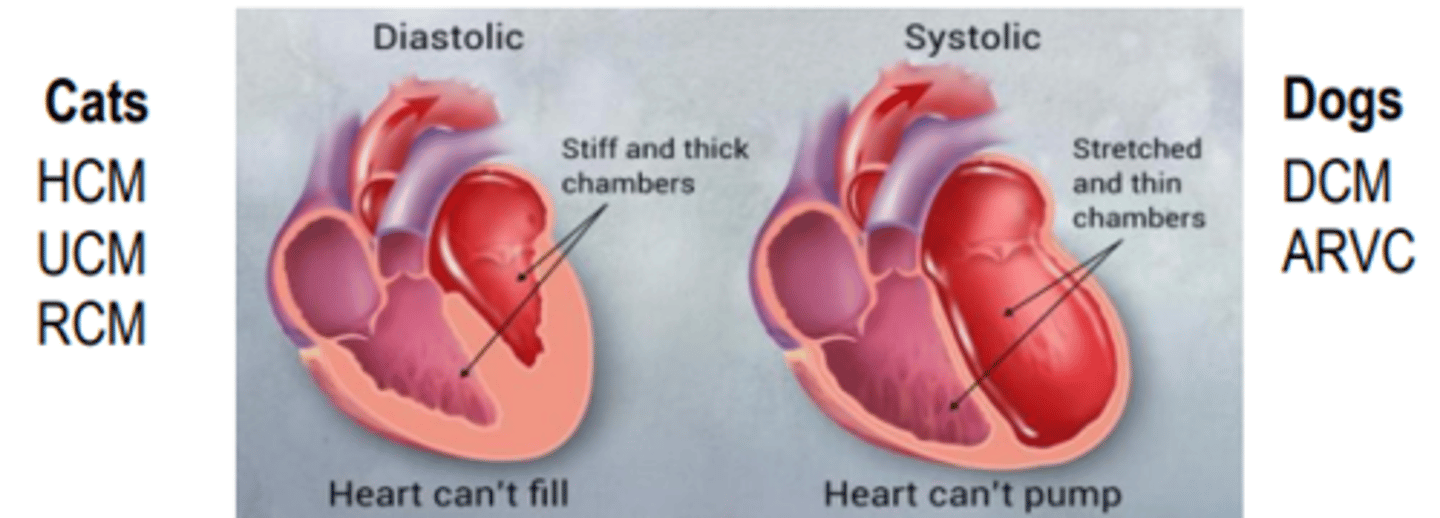
Do dog cardiomyopathies typically affect diastolic or systolic function? Name an example of a common issue
Systolic function (impair pumping)
-Dilated Cardiomyopathy (DCM) and ARVC (the worst form

What happens to forward stroke volume when regurgitation becomes quite severe?
Despite EDV and TSV being quite high, the FSV is lower then a normal heart
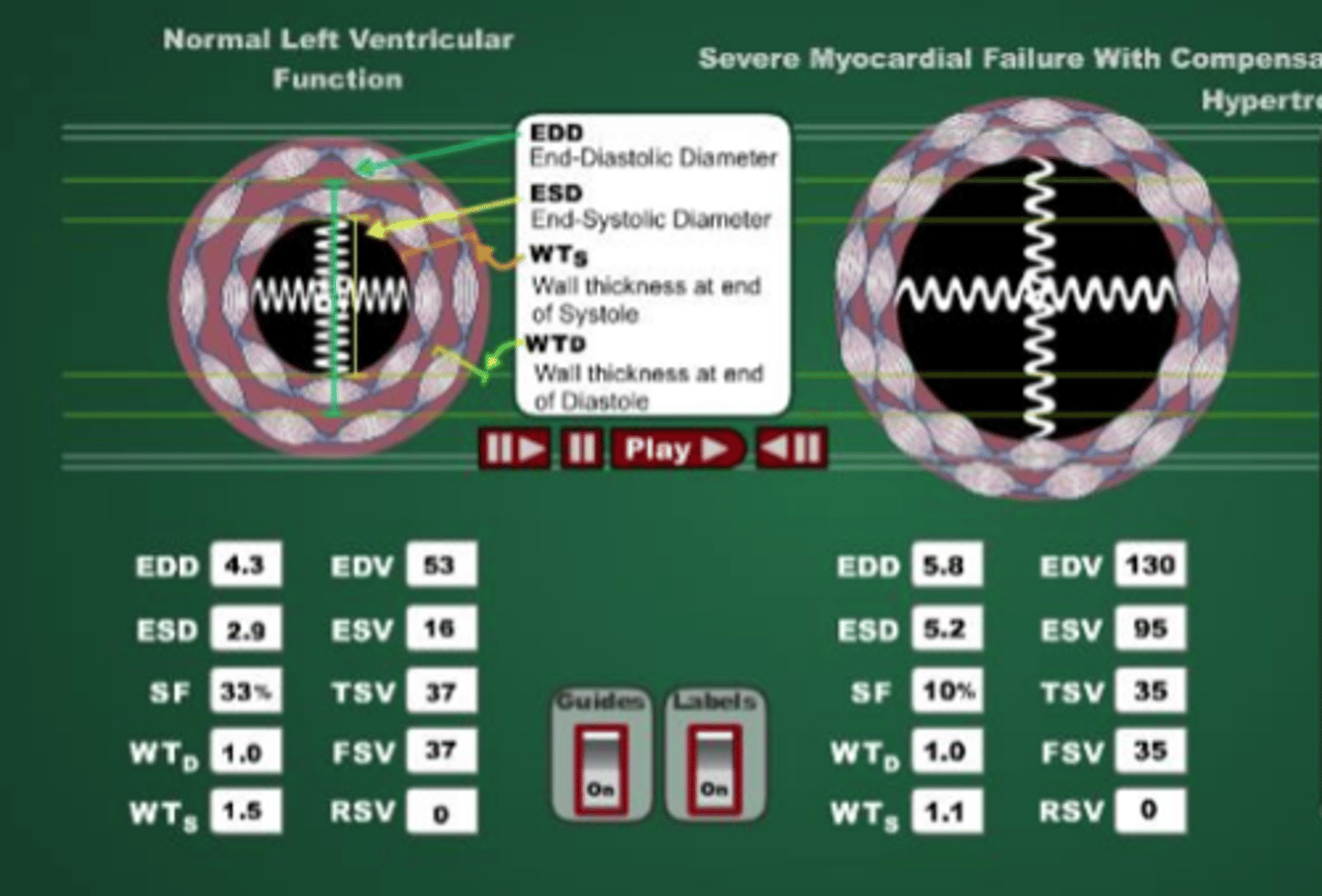
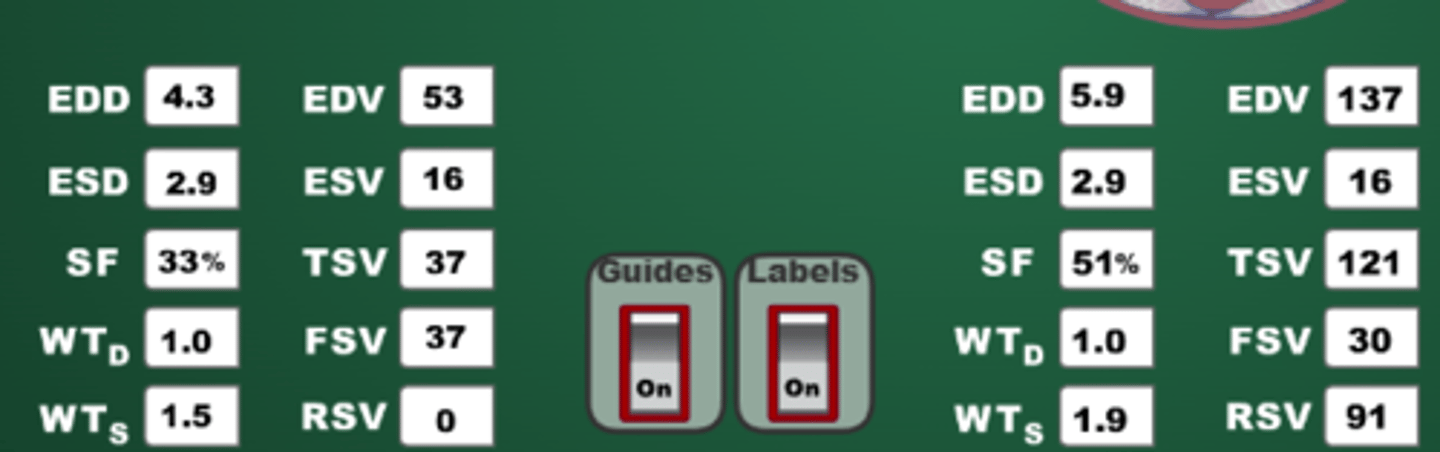
In DCM, what happens to the EDV, ESV, and FSV?
The heart has a harder time contracting, so ESV is higher then in a normal heart, but the EDV also increases in order to maintain FSV.
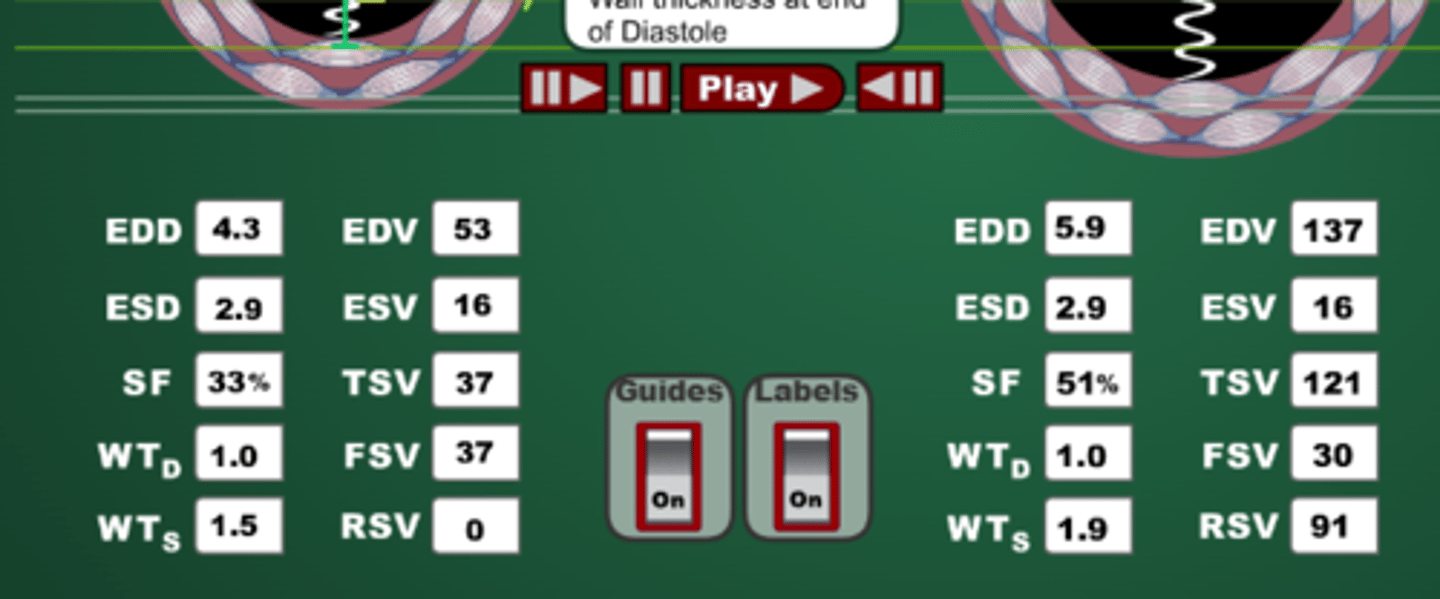
Is there any indication of either systolic or diastolic function based on EDV and shortening fraction in a mitral regurgitation case?
Systolic and diastolic functions still work well, its an issue with the valve. The shortening fraction is 51% which is quite high so its working well.
In moderate myocardial failure, why is stroke volume reduced?
Is dysfunction systolic or diastolic?
Compared to normal, the EDV increases a bit but ESV also increases a lot. So the EDV-ESV is much smaller then normal. Therefore, its a systolic dysfunction.
In Hypertrophic cardiomyopathy such as Feline HCM, what is happening to EDV and shortening fraction? Is this a systolic or diastolic dysfunction?
EDV is decreasing but SF is increasing to 60% (from 33%). It is a diastolic dysfunction
In Feline HCM, is there concentric or eccentric remodeling? Is there a cause?
Concentric remodeling without cause
Is feline HCM a disease or syndrome?
Syndrome which probably represents many disorders
For all types of declining Forward stroke volume, what are the ways we compensate?
If you have a patient without an enlarge atrium, are they more or less likely to be in heart failure?
less
Explain why the oxygen saturation of blood shunted right-to-left cannot be improved by providing a patient with additional supplementary inhaled oxygen.
The blood never goes through the lungs, therefore can never be oxygenated so giving more oxygen is pointless
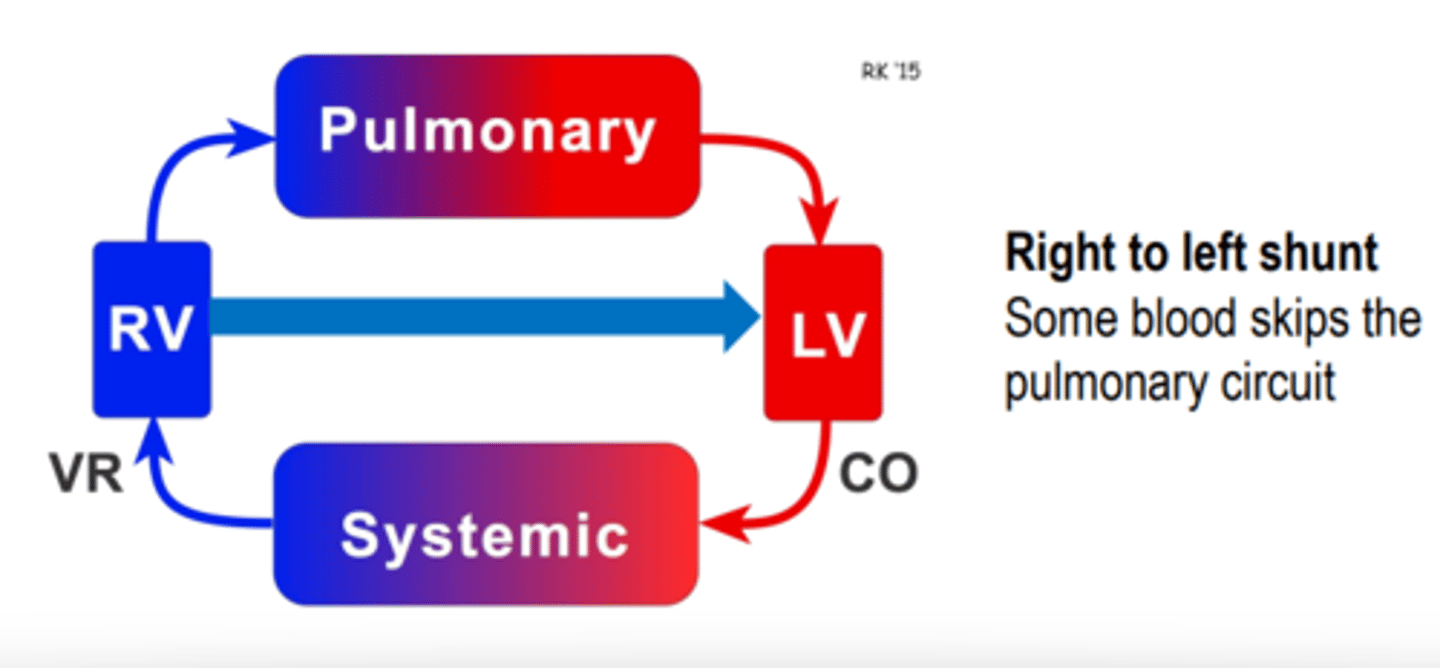
What determines the direction of the shunt? Which way do most shunts start out as?
Pressure gradient
Start left to right since pressure is higher on the left side. The exception is the tetralogy of fallot or a reversal.
Will left to right shunts have normal SpO2?
Yes
What are the consequences of a shunt reversal?
A shunt shifting from left to right means the pressure gradient has switched. The first concern would be the blood is not going to the pulmonary circuit and Sp02 would drop.
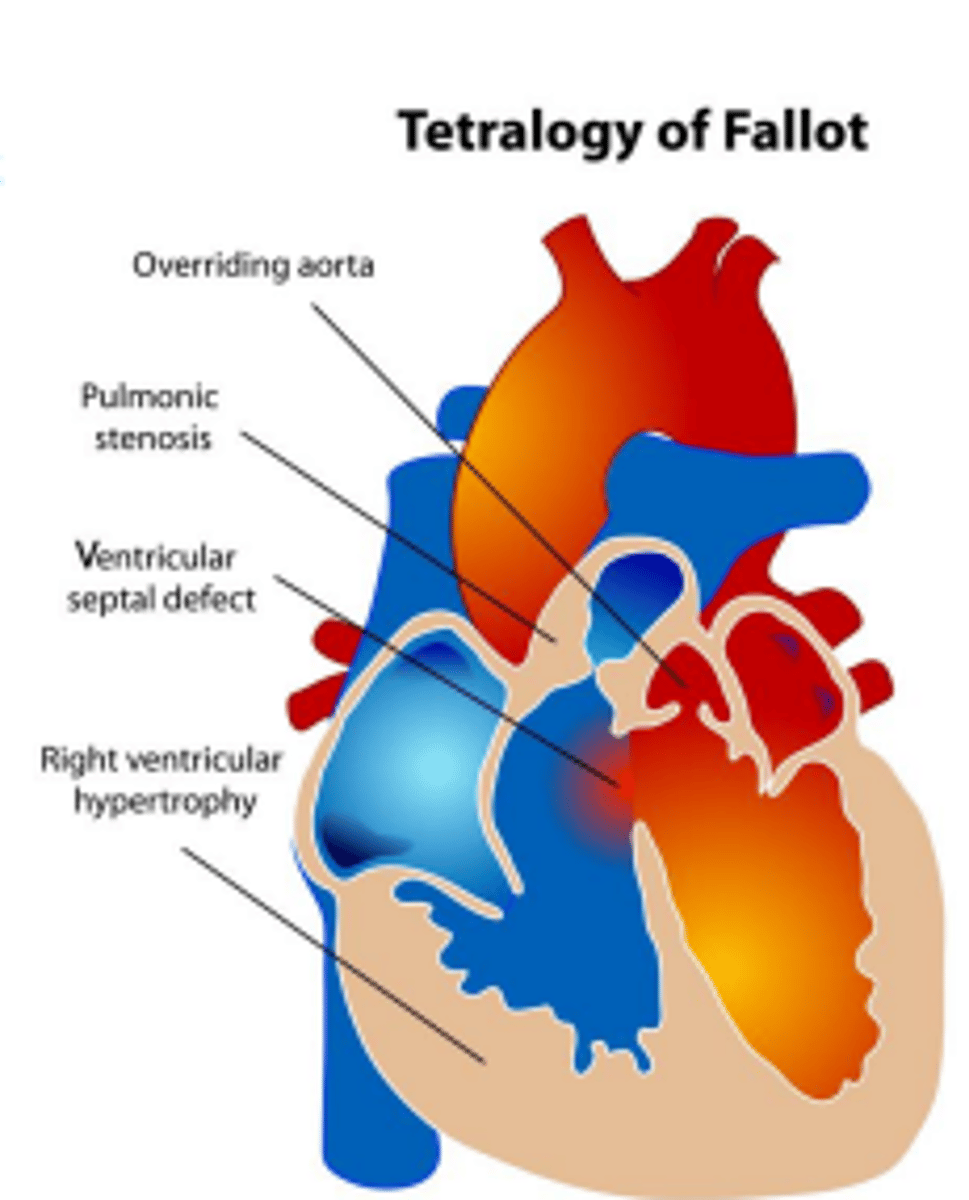
What is a tetralogy of fallot?
Ventricular septal defect with overriding aorta. It starts as a right to left shunt and the pulmonic valve is highly resistant due to stenosis. The aorta provides an escape route to the blood that can't exit thru the pulmonic valve
Heart disease is any ______ of the heart. Heart disease is not heart ______.
abnormality
failure
Heart failure usually results from the progression of heart _______.
disease
Not all heart disease will result in ______ ______
heart failure
What diagnoses heart failure?
YOU! using history, signalment, PE, and ancillary diagnostic findings as well as response to therapy to arrive at the diagnosis.
What are the 2 types of heart failure? Which is most common in our world?
Venous congestion-backward failure(more common)
Poor perfusion- forward failure
Backward heart failure occurs because the body prioritizes maintenance of _____ ______ over maintenance of normal _____ ______
Backward heart failure occurs because the body prioritizes maintenance of cardiac output over maintenance of normal venous pressures
What occurs in cardiogenic pulmonary edema?
Alveoli flood with edema fluid when capillary hydrostatic pressure > 25 mm HG
What does left sided HF lead to?
What about right sided HF?
Left: pulmonary congestion & pressure, pulmonary edema
Right: venous congestion of body organs, ascites,distended jugular vein
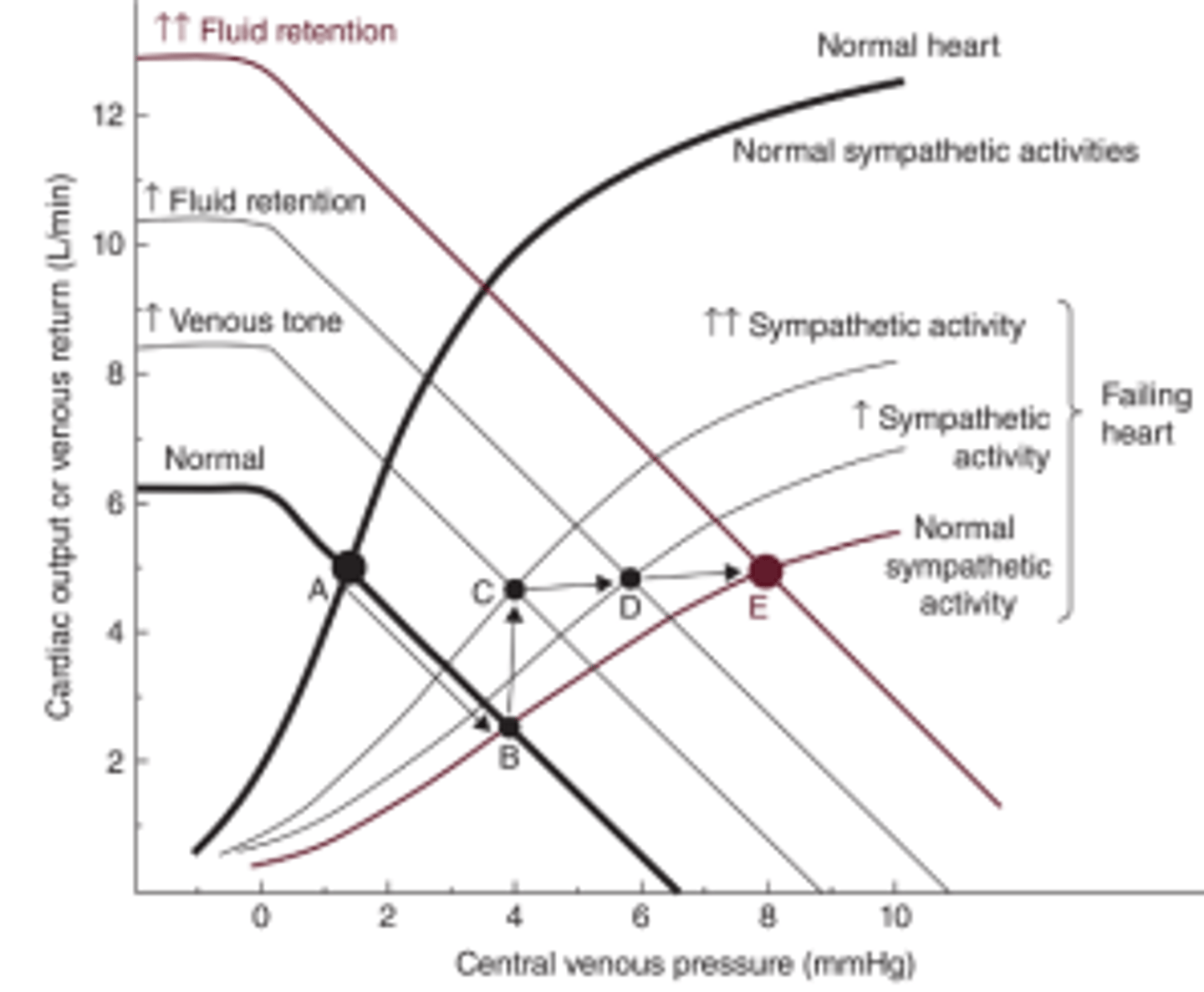
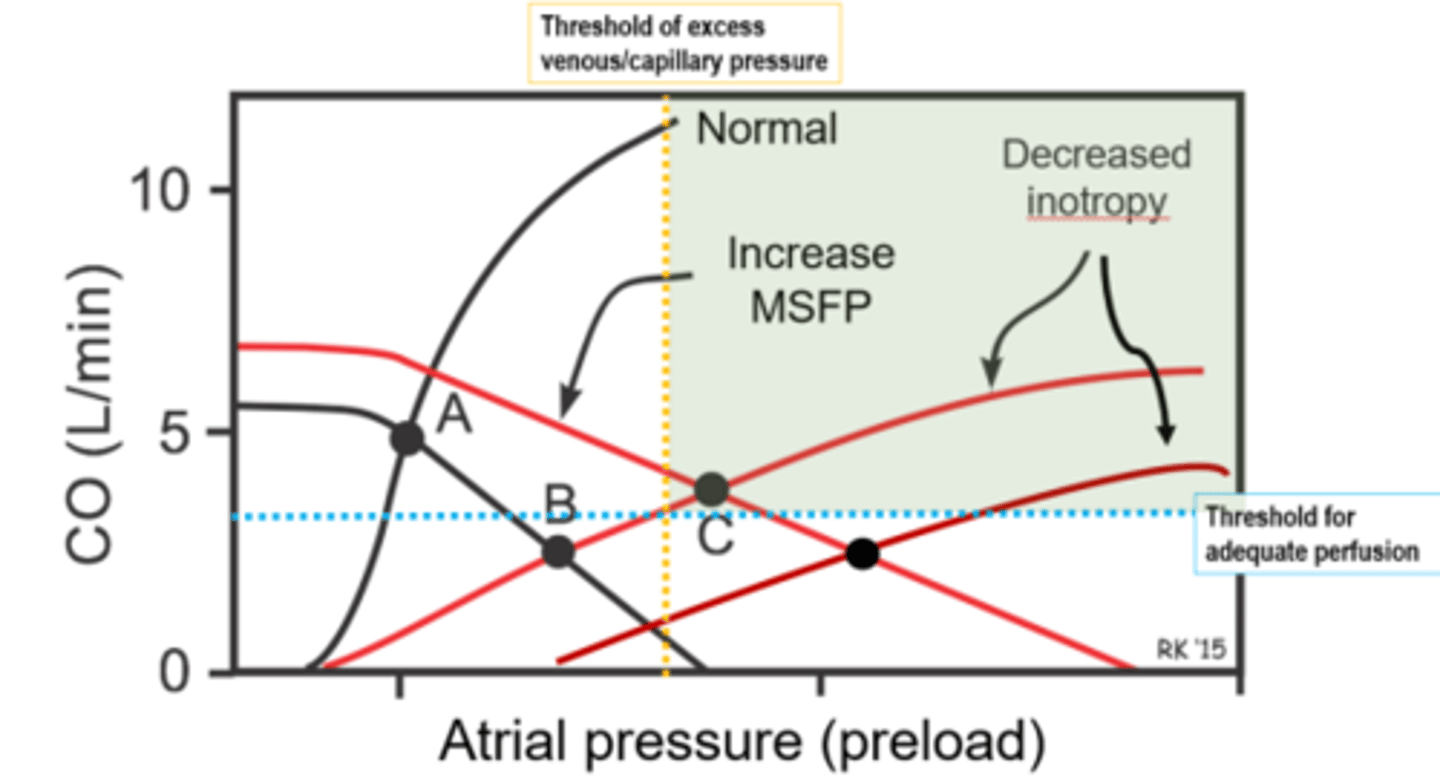
Explain neurohormonal compensation for decreasing cardiac output in terms of vascular function curve/MSFP and the cardiac output curves (aka ventricular function curve).
The vascular function curve/MSFP increases significantly due to increase venous tone and fluid retention.
The Ventricular function increases due to increase symp activity and increasing EDV, inotropy and chronotropy.
Left side CHF results from impaired ________ venous drainage
Right side CHF results from impaired ________ venous drainage
-pulmonary
-venous
As long as cardiac output is above threshold for adequate perfusion, there will be no signs of _____ failure
forward
As long as venous pressures are low enough to keep capillary hydrostati pressure below edema threshold, the patient is _____
dry
What symptoms will we see in our "warm and wet" patients?
Is this forward or backward failure?
-edema and/or effusion without obvious symptoms of low Cardiac output
-backward failure only
What symptoms will we see in our "cold and dry" patients?
Is this forward or backward failure?
-acute drop in caridac output (cold paws & ears) without congestion
-forward failure only
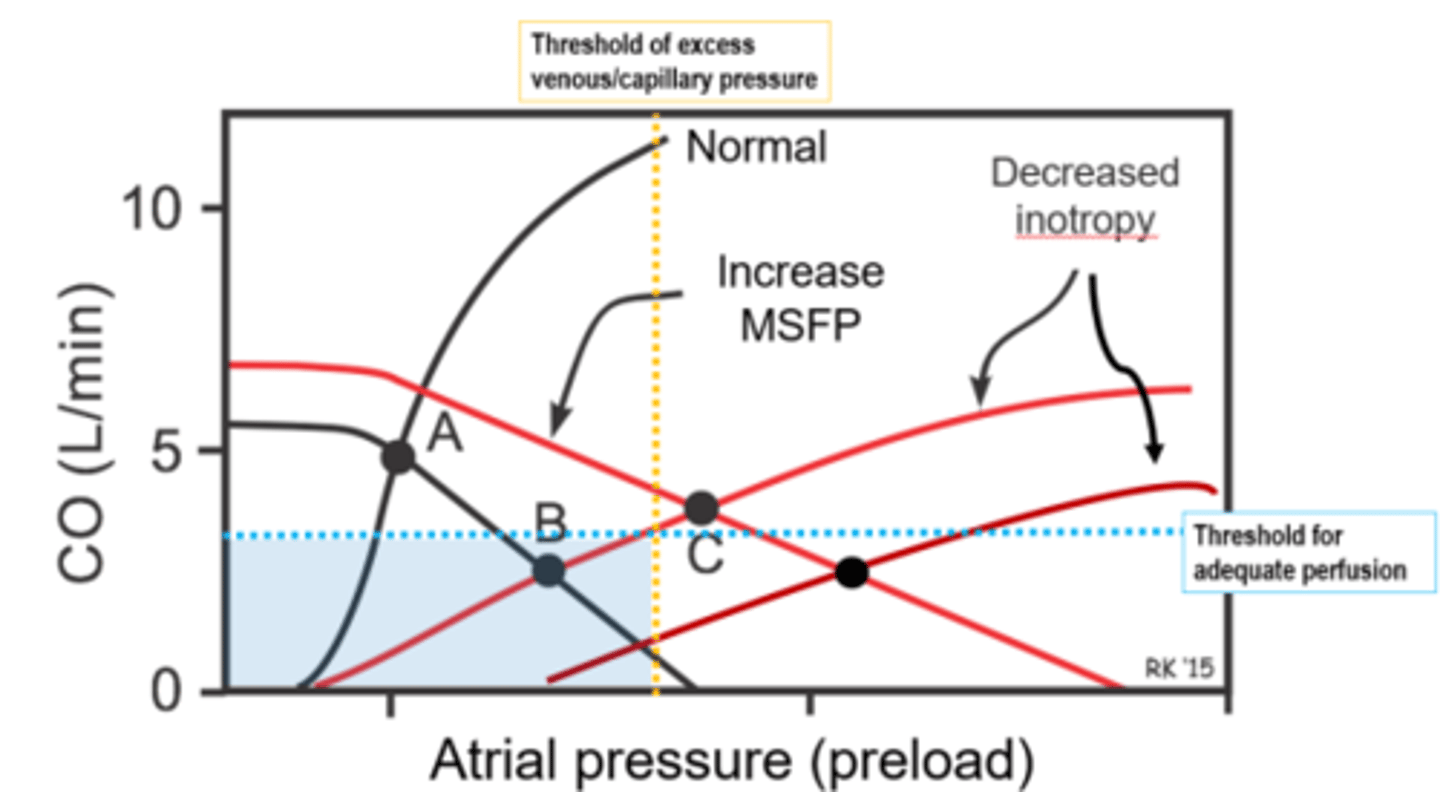
What symptoms will we see in our "cold and wet" patients?
Is this forward or backward failure?
-Congestion (edema and/or effusion) and symptoms of low cardiac output
-both backward and forward failure .
Very bad!
In a warm & wet heart failure case, what would you use to treat?
-Loop Diuretics to help with congestion
-Positive inotrope is helpful (Pimobendan)
-Venodilators may reduce venous congestion (furosemide, pimobendan)
-Arteriolar dilator decreases afterload to increase caridac output (pimobendan)
-Alleviate anxiety to reduce O2 demand
Golden rules for Diagnosis and treatment of CHF:
1.Heart disease must be _________ for CHF. In dogs, murmurs should be ______(usually)
2. You need radiographs to document ______ ________
3. A dog with a slow sleeping ______ ______ or a ______ _____ _______ does not have CHF
4. Many dogs with a murmur cough because of concurrent _______ disease
5. Crackles usually mean ______ disease, not CHF, in _______ animal patients
6. A very enlarged ____ atrium is consistent but not diagnostic of CHF in feline cardiomyopathies, canine DCM, and canine mitral valve disease (ultrasound is your friend)
7. It is really hard to 'overdose' of ______ (furosemide loop diuretic)
Golden rules for Diagnosis and treatment of CHF:
1.Heart disease must be advanced for CHF. In dogs, murmurs should be loud (usually)
2. You need radiographs to document pulmonary edema
3. A dog with a slow sleeping respiratory rate or a respiratory sinus arrhythmia does not have CHF
4. Many dogs with a murmur cough because of concurrent airway disease 5. Crackles usually mean airway disease, not CHF, in small animal patients
6. A very enlarged left atrium is consistent but not diagnostic of CHF in feline cardiomyopathies, canine DCM, and canine mitral valve disease (ultrasound is your friend)
7. It is really hard to 'overdose' of Lasix (furosemide loop diuretic)
Is exercise intolerance a symptom of heart failure in vet medicine?
Not typically
What are the most common signs of HF in vet medicine?
Breathing abnormalities (for left side), Ascites (right side),
Lethargy
Anorexia
Clot (cats)
What drug should you avoid in cardiac patients?
Dexmedetomidine
In a cold & wet heart failure case, what would you use to treat?
-Diuretic to reduce venous congestion:loop like furosemide
-Positive inotrope mandatory—dobutamine in ICU setting with committed owners, pimobendan?
-Vasodilators to reduce afterload IV fluids might be needed but they worsen the congestion
-Survival rate in human medicine ~ 50% from MI, probably lower in veterinary medicine
-QOL/prognosis conversation with owners
In a cold & dry heart failure case, what would you use to treat?
-IV fluids
-Address tachyarrhythmia if present
-Remove pericardial fluid if there is an effusion
What are the 2 holy grails of heart failure treatment? Why aren't they attainable?
1. Stop cardiac remodeling
2. stop vasoconstriction & fluid retention
Nothing found yet to stop remodeling and RAAS inhibition doesn't seem to work
Body fluid are _____ % of animal weight.
They are ___ in extracellular fluid and ____ in intracellular fluid. Of the ECF, _____% is interstitial and ___% is plasma(intravascular).
Body fluid are 60% of animal weight.
They are 1/3 in extracellular fluid and 2/3 in intracellular fluid. Of the ECF, 75% is interstitial and 25% is plasma(intravascular).
What is the equation for total blood volume?
TBV= plasma volume/ (1-hematocrit)
What is the maximum amount of blood that is safe to draw from an animal?
10%
ICF has a ____ potassium, ___ sodium, ___ calcium, and ____ chloride.
ECF has a ____ potassium, ___ sodium, ___ calcium, and ____ chloride.
ICF has a high potassium, low sodium, low calcium, and low chloride.
ECF has a low potassium, high sodium, high calcium, and high chloride.
At a steady state, ECF and ICF has the ____ osmolarity.
same
What is the equation for serum osmolality?
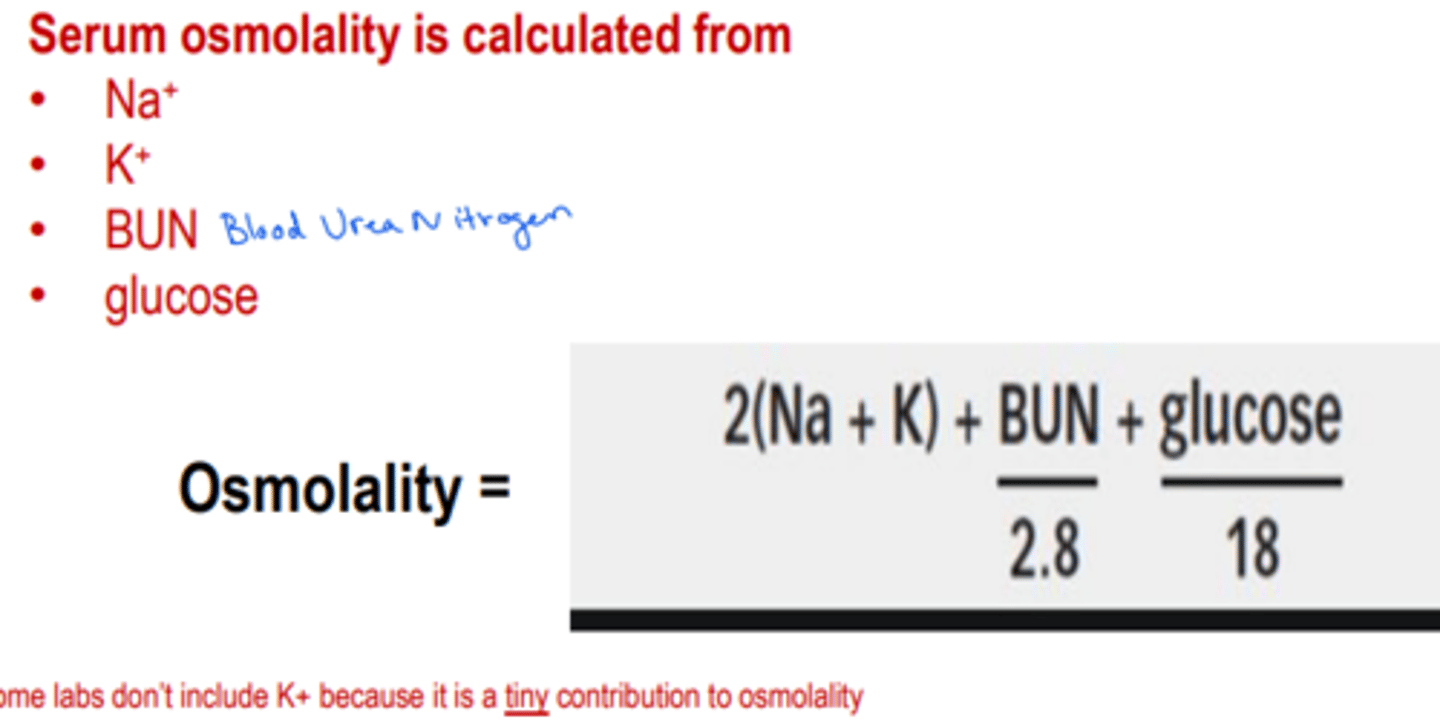
What is the largest component for urine osmolality?
Urea
While we don't typically calculate urine osmolality, we can estimate (very roughly) it based from _____ ______.
Specific Gravity
A. How many osmoles are in 1 mol NaCl?
B. Ca 2+ 1 mMol= how many mEq of charge?
C. How many grams per 100ml are in 0.9% saline?
A. 2 osmoles
B. 2mEq of charge
C. .9 grams per 100 ml
What results in hypernatremia?
hypernatremia= high concentration
-losing more water than sodium
-gaining more sodium than water
What results in hyponatremia?
Hyponatremia=low concentration
-losing more sodium than water
-gaining more water than sodium
Describe what happens to a cat with diabetes mellitus in relation to the serum osmolality and and why
The cat will have high blood glucose and this can increase the serum osmolality making them hyperosmolar
What will happen if an animal ingests too much water with NO electrolytes?
Hypotonic ECF, water will move into cells to equalize ECF and ICF osmolarity
How should you treat an animal with isotonic dehydration?
Is there a shift of fluid between ICF and ECF?
-Needs IV fluids w physiologic osmolarity
-no shift of fluid between ICF and ECF
How should you treat an animal with isotonic hypervolemia?
Is there a shift of fluid between ICF and ECF?
-give a diuretic to get rid of fluid in an isomotic fashion
-no shift of fluid between ICF and ECF
How should you treat an animal with hypertonic hypovolemia?
What is an example of this?
Is there a shift of fluid between ICF and ECF?
-give more H20, less NaCl (such as dextrose)
-left in heat without water
-cells 'shrunk' a bit because ECF is was higher than ICF
How should you treat an animal with hypotonic hypovolemia?
Is there a shift of fluid between ICF and ECF?
- needs IV fluids with a bit more NaCl than normal
-Cells have swelled a bit to balance the hypotonic ECF
Each nephron has 2 capillary beds, what are they and what do they do?
Glomerulus –forms the filtrate (fluid extracted from capillary plasma)
Peritubular – responsible for reabsorbing things from the filtrate and delivering things
that need to be secreted into the filtrate as it transits thru the tubules
What is the job of the proximal tubule?
70% of resorption and secretion
What is the job of the macula densa?
specialized sensor area of tubule
What is the job of the loop of Henle?
sets up interstitial concentration gradient
What is the job of the DCT?
Fine tuning of urine composition
What is the job of the collecting duct?
Adjustment of the urine water content using the interstitial osmotic gradient
What is the difference between short loop nephrons(cortical nephron) and long loop nephrons(juxtamedullary)?
Long loop nephrons have an additional job They establish a corticomedullary gradient of osmotic concentration (using the loop of Henle)
What occurs to the interstitial osmolality as you get deep into the medullary interstitium?
Become more salty (hyperosmotic)
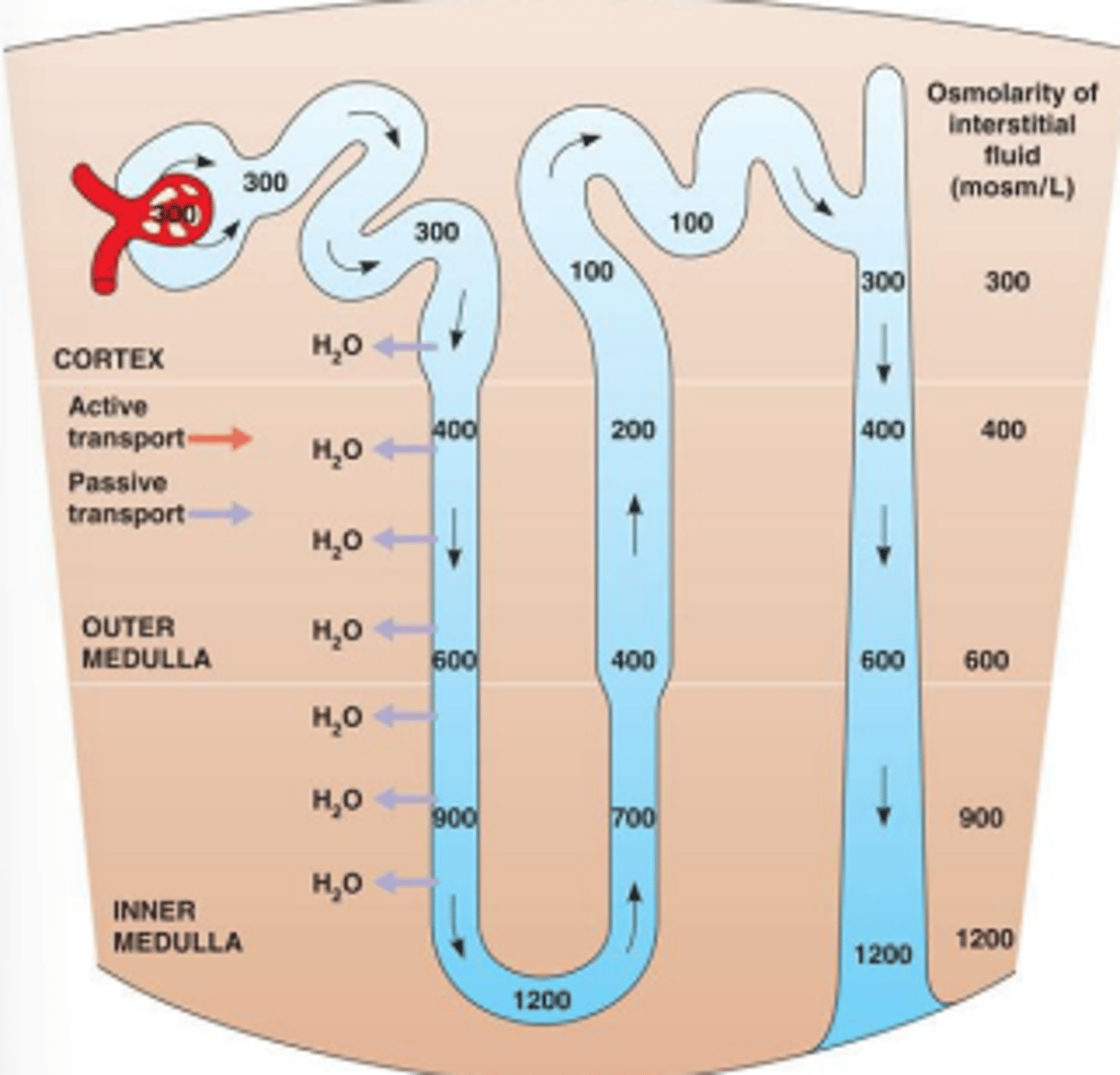
When filtrate passes thru the collecting duct, what occurs when ADH is present?
What occurs when ADH is not present?
If ADH is present water is reabsorbed by the hyperosmotic interstitium and
returned to peritubular capillary blood
If no ADH is present Water is trapped in the filtrate and excreted in urine
Maximum urine concentration is equal to the concentration of the _____ _______; this is controlled by ______ and _____ of long loop nephrons in a kidney
Maximum urine concentration is equal to the concentration of the deep medulla; this is controlled by length and number of long loop nephrons in a kidney
What are the 4 processes that occur in the nephron?
1. Formation of filtrate
2. Tubular reabsorption
3. Tubular secretion
4. Final urine H2O content adjustment & urine excretion
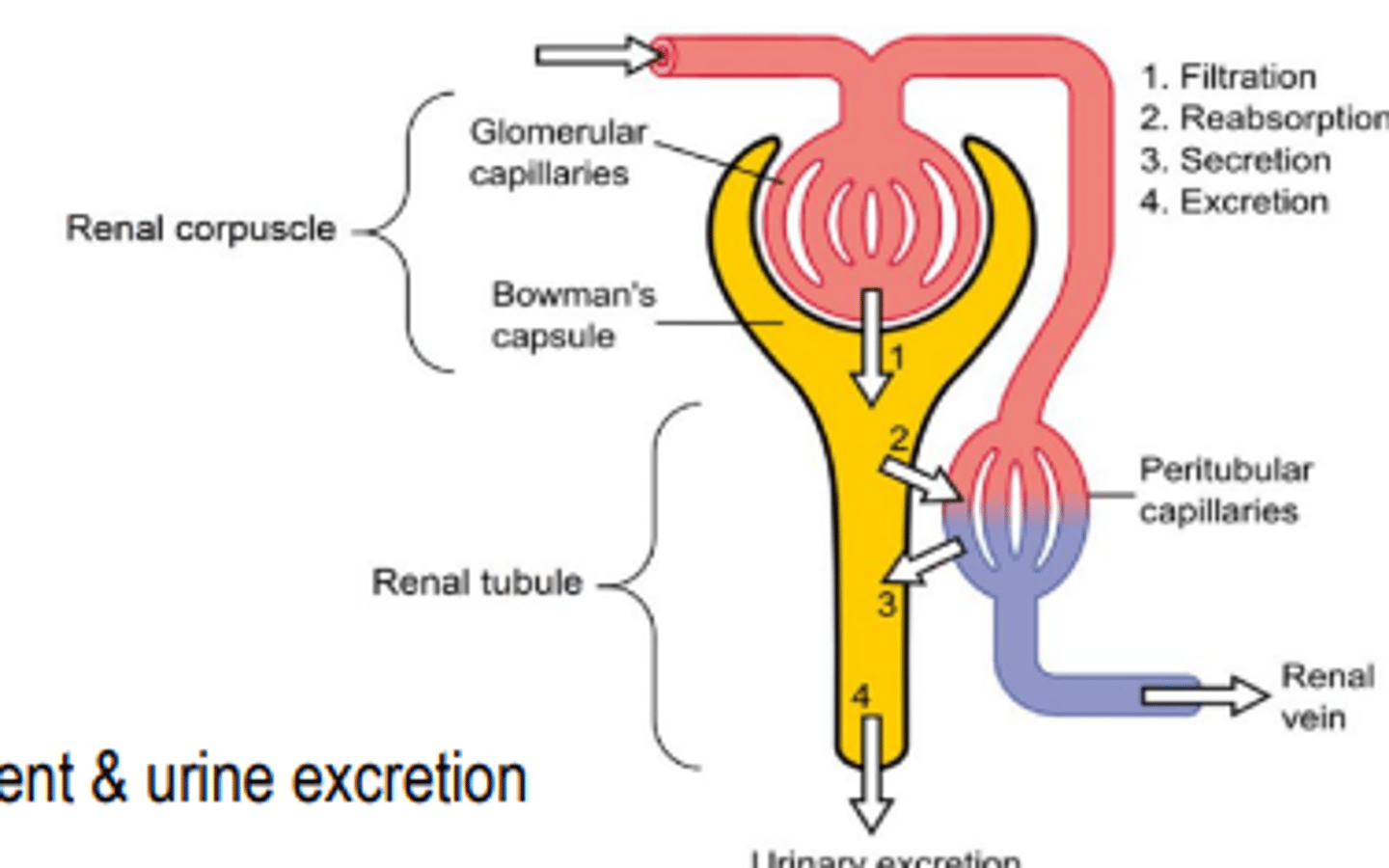
What are the Three layers of the glomerular filtration barrier
1. Larger fenestrations in capillary endothelium
2. Basement membrane (aka basal lamina)
3. Some cells of Bowman's capsule sit on the outside of the basement membrane. These cells have 'fingers' so are called podocyte
The filtrate has basically the same composition as ______ _____
interstitial fluid
For molecules to go through the glomerular filtration barrier, what size and charge should they be?
Small and positively charged
What is occurring in protein-losing nephropathy?
What might lab work and UA show?
There is a defect in one or more layers of the filtration barrier so large molecules (such as albumin) are entering Bowmans space.
You will see a lower serum albumin and protein in the urine
What are the 3 main categories of glomerular disease in dogs?
1. Immune complex mediated glomerulonephritis (ICGN)
2. Focal segmental glomerulosclerosis (FSGS)
3. Amyloidosis
What are the 4 features to diagnose nephrotic syndrome?
1. Hypoproteinemia (Alb <1.6)
2. Proteinuria
3. Edema
4. Lipidemia (↑cholesterol)
What is nephrotic syndrome?
edema from low serum albumin
Define Renal Clearance
Renal clearance is the rate of removal of a substance from the plasma by the kidneys
(removing from plasma and putting it into the urine)
Should plasma glucose be removed by the kidneys? What is the renal clearance?
No plasma glucose should be removed by the kidneys. The renal clearance of glucose should be zero.
Glucose can get into the filtrate but should be 100% reabsorbed
Does penicillin have a high or low renal clearance?
High renal clearance- all of the unbound penicillin gets into the filtrate.
A patient with impaired kidney function will have _____________ clearance of things that should be excreted and/or _________ renal clearance of things that should be reabsorbed.
-Inadequate
-excessive
What is the filtration fraction?
What percentage of plasma fluid passes thru the filtration barrier and became filtrate
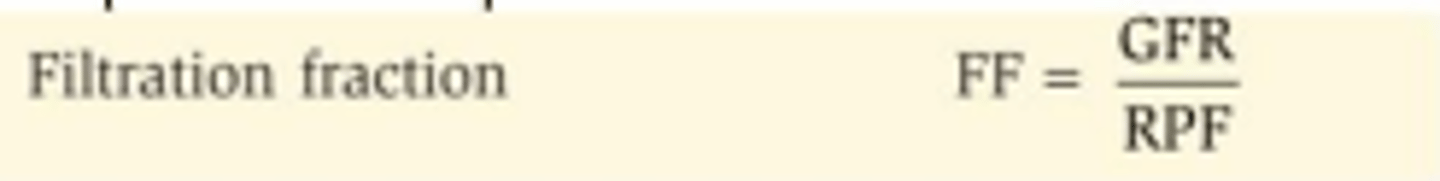
How do we test if enough filtrate is being made?
Use a molecule that is freely filtered, trapped in tubules, and no additional amount is secreted into the filtrate (aka not made in our body). Use Inulin or iohexol in clinical research. The clearance of this molecule is the same as the rate of filtrate formation which is GFR.
How would we test to see if there is enough blood flow to the kidneys (not done in vet med)?
For this test, use a molecule that is
• Freely filtered
• Trapped in the tubules
• Any additional amount that didn't go thru the filtration barrier, is
then secreted into to the filtrate by the peritubular capillaries
Any plasma that runs thru the kidney will have all of this substance removed from it. The clearance of this molecule is the same as the rate of renal plasma flow (RPF)
How do you test if sodium (or another substance is being appropriately reabsorbed by the tubules?
Compare the clearance of sodium (or another substance) to the
clearance of a molecule that is filtered but not reabsorbed or secreted
This calculation tells you the clearance ratio, aka
fractional excretion, which is the percentage of filtered
substance that is not reabsorbed but is left in the urine
FENa > 1% suggests that the tubules are working well
What serum biomarkers do we use to correlate/measure GFR? If this substance is high, is GFR high or low?
Why do we use these?
-Creatinine and SDMA
-if they are high, GFR is low
-easily filtered but not reabsorbed or secreted by the tubules
What is azotemia? What lab values will be higher? What does it indicate?
Azotemia means an accumulation of nitrogenous wastes in the blood. We will see a high creatinine, BUN, and SDMA. This indicates GFR is not adequate.
Pre-renal azotemia- where it occurs? What will be active and will urine be concentrated or dilute?
Reduced perfusion of kidneys .
Urine should be concentrated and RAAS and ADH will be active.
Renal azotemia- where it occurs? Will urine be concentrated?
Intrinsic renal disease
Urine typically not concentrated
Post-renal azotemia- where it occurs?
After the kidneys, Obstruction of urine flow
What are the 4 tubular sodium transporters that AG2 stimulates?
NHE3
NKCC2
NCC
ENaC
How do prostaglandins affect blood flow to the kidneys?
The vasodilate and maintain glomerular blood flow.
What should the oncotic pressure in Bowmans space be?
It should be 0 since there is no protein