Topic 5: Female Reproductive System- 2
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Internal genitalia
ovaries
Accessory organs
Uterine tubes (oviducts), uterus, vagina
External genitalia
vulva
Function of female reproductive system
produce gametes & hormones
prepare to nurture developing embryo
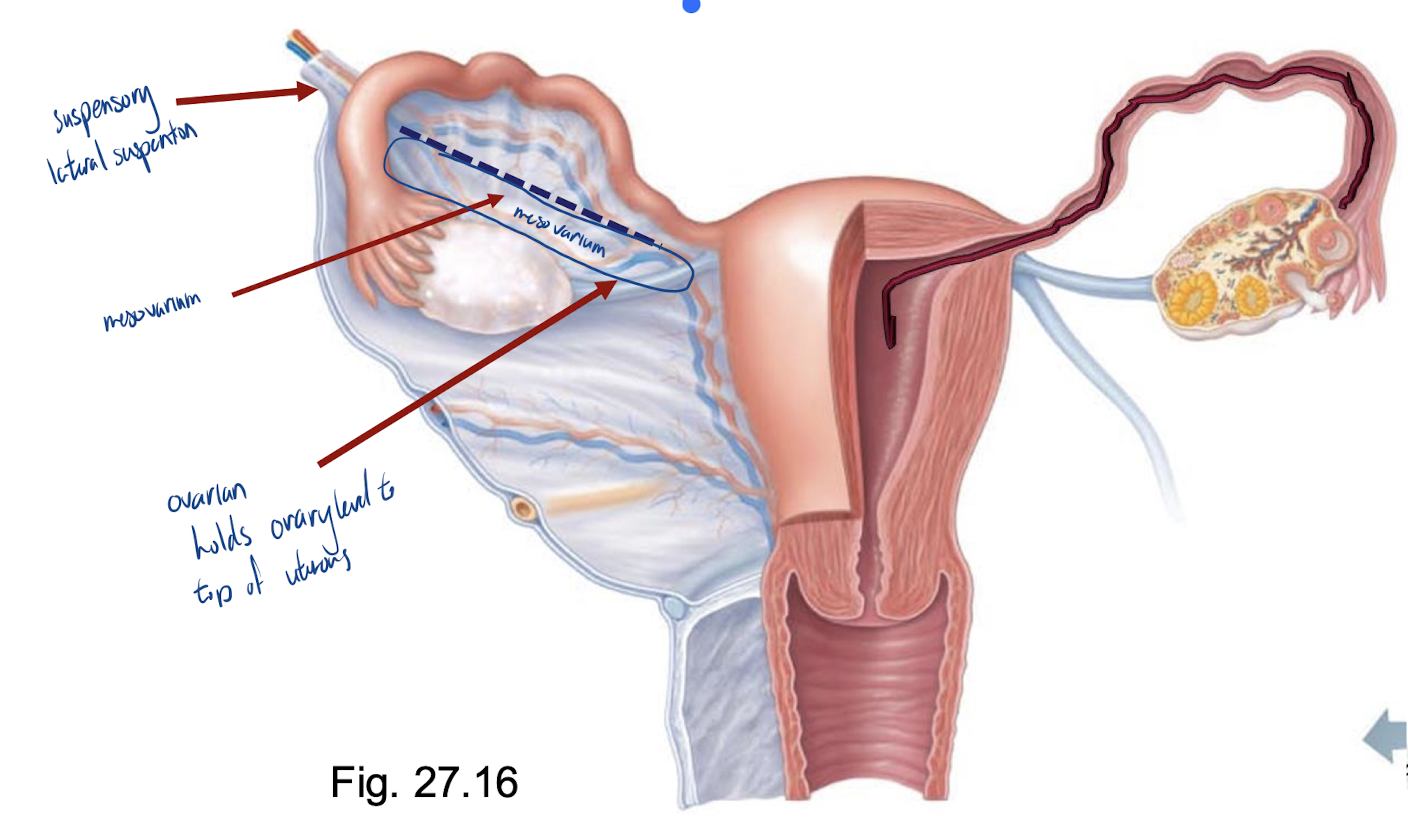
Ovaries
anchored by ligaments
ovarian, suspensory, mesovarium
NB: the mesovarium is part of the broad ligament that supports the ovaries, oviducts and uterus
served by ovarian arteries (branches of the abdominal aorta) plus ovarian branch of uterine arteries
Tunica albuginea
covering external surface of the ovary
Germinal epithelium
final outer covering of ovary
Ovarian cortex
contains follicles at all stages of development
oocyte
granulosa cells
theca cells
Corpus luteum
formed from ovulated follicle each month
prominent at 2nd half of menstrual cycle
no baby- degrades
baby- stays for first 3 months of pregnancy
Oviduct
receive the egg & provide the site for fertilization; ~ 10 cm long
oocyte released into peritoneal cavity → fimbriae direct it into ampulla of oviduct
structure of wall of oviduct also helps oocyte move toward uterus:
1) smooth muscle
2) epithelial cells (lined with cilia)
• external covering = visceral peritoneum; supported by the mesosalpinx
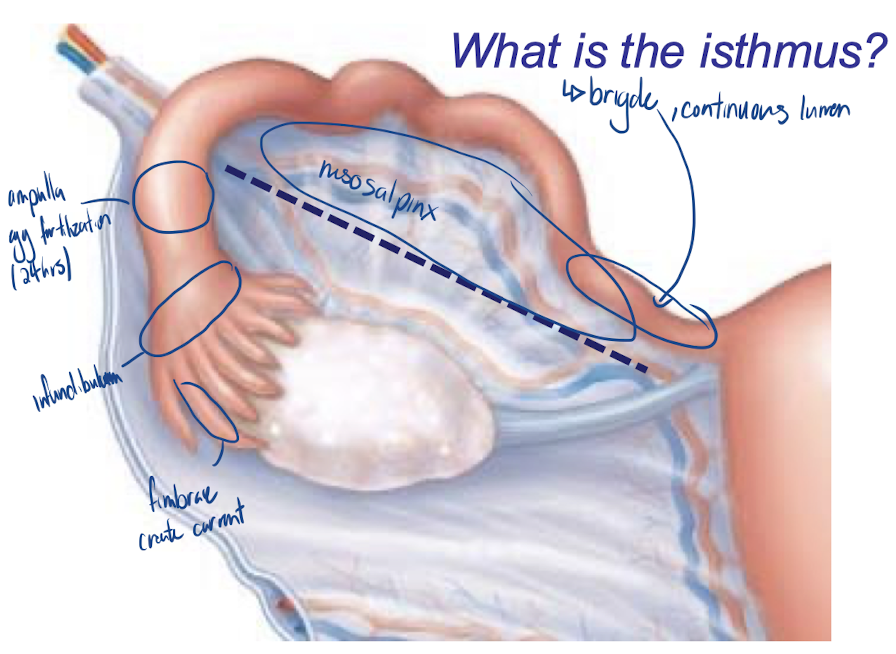
What is the isthmus?
bridge between the oviduct and uterus
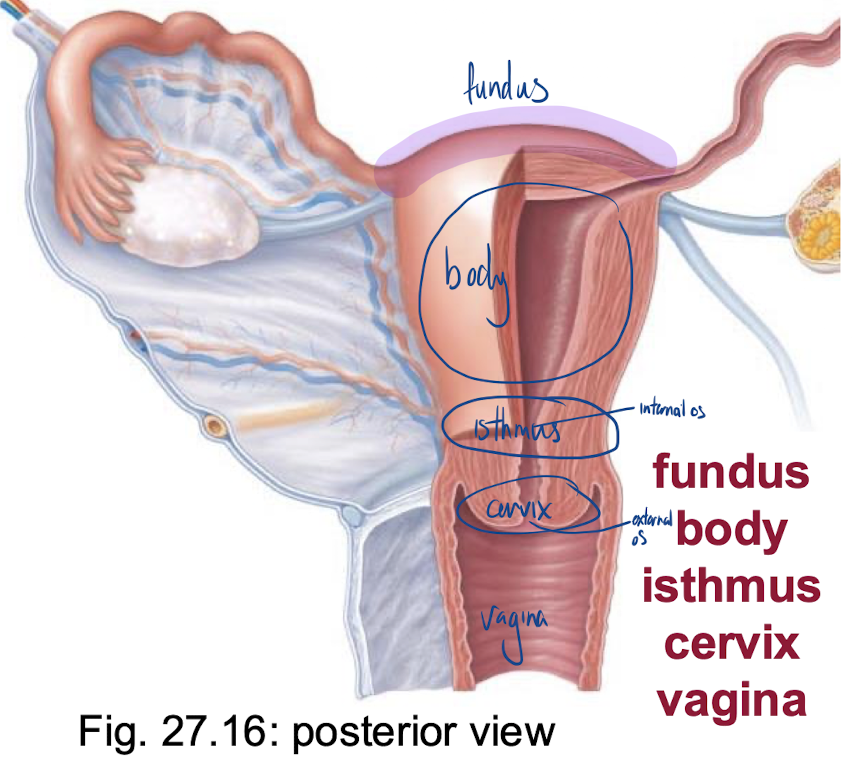
Uterus
anterior to rectum & postero-superior to bladder
receives, retains, nourishes embryo
shape of an inverted pear in nulliparous women
nulliparous women
women never pregnant before
internal os
uterus to cervix
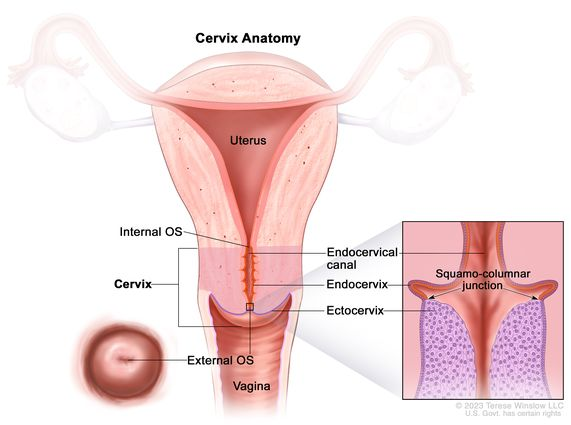
external os
cervix to vagina
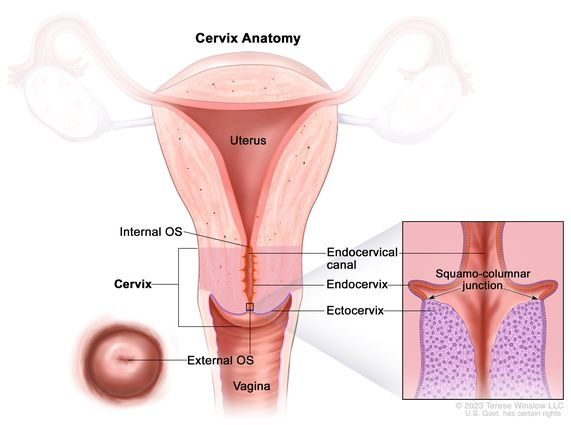
cervical glands
mucus fills cervical canal & covers the external os → prevents infection; less viscous at midcycle to:
regulate by hormones
less of a barrier to get pregnant
promote fertility
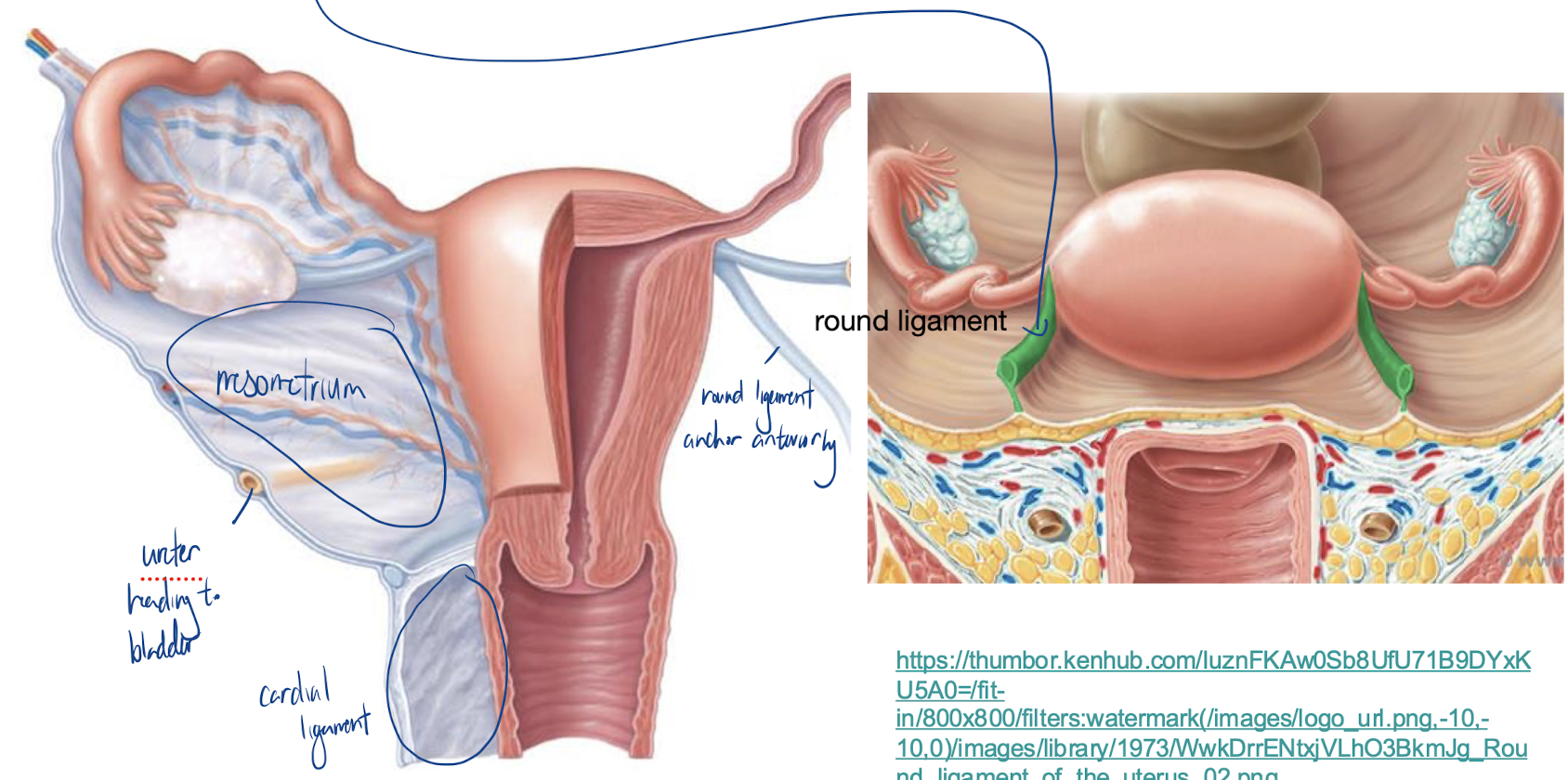
The many supports of the uterus:
mesometrium: laterally (broad ligament)
cardinal (transverse cervical) ligaments: from cervix & upper vagina to lateral walls of pelvis
uterosacral ligaments: to sacrum posteriorly
round ligaments: to anterior body wall
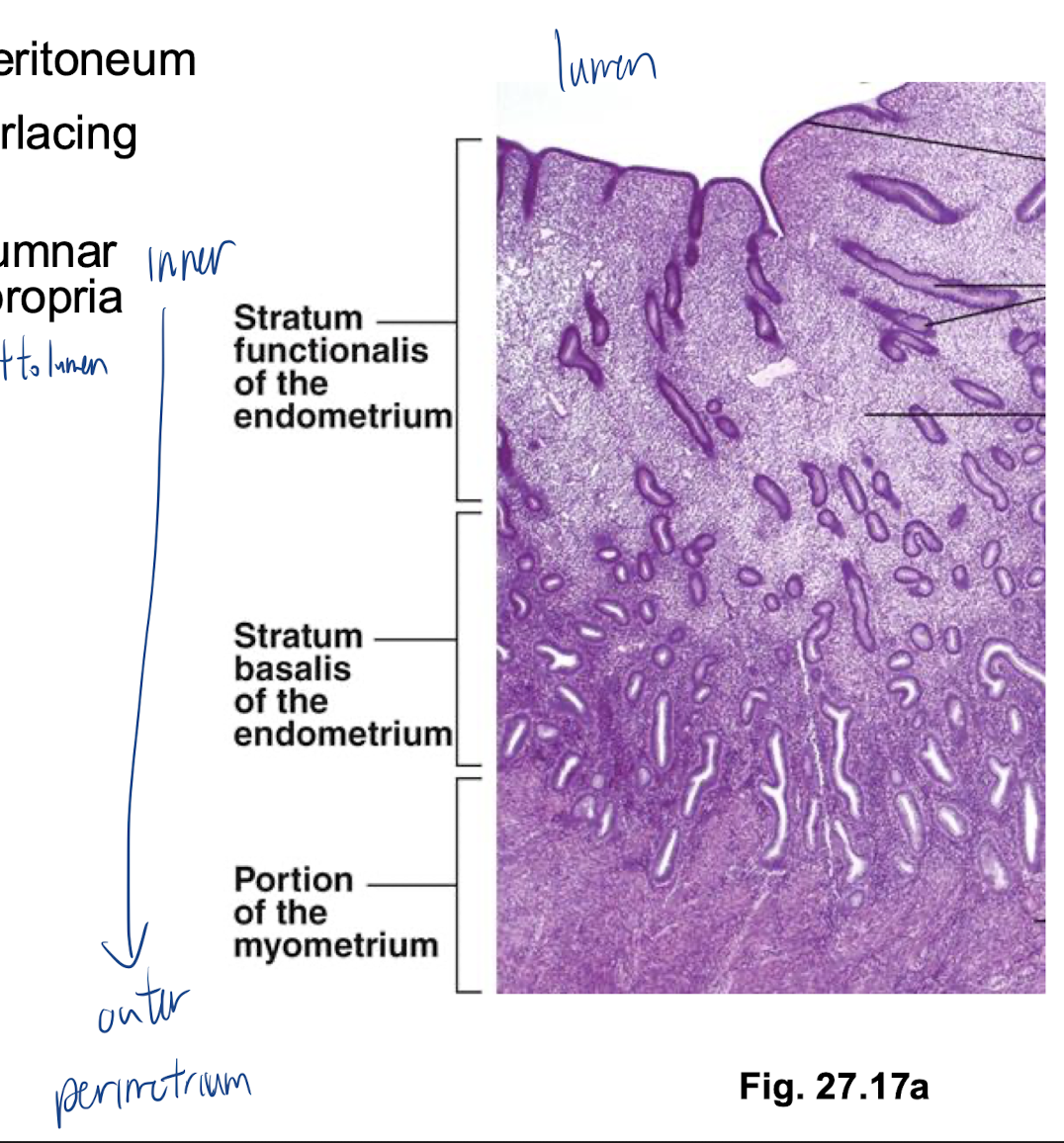
Uterine Wall
3 layers:
perimetrium: = visceral peritoneum
myometrium: middle, interlacing bundles of smooth muscle
endometrium: simple columnar epithelium + thick lamina propria
stratum functionalis: closest to lumen
stratum basalis: deeper
vascular supply of uterus
uterine arteries (from internal iliacs)
to arcuate arteries
radial arteries within myometrium
straight arteries (stratum basalis) or spiral arteries (stratum functionalis)
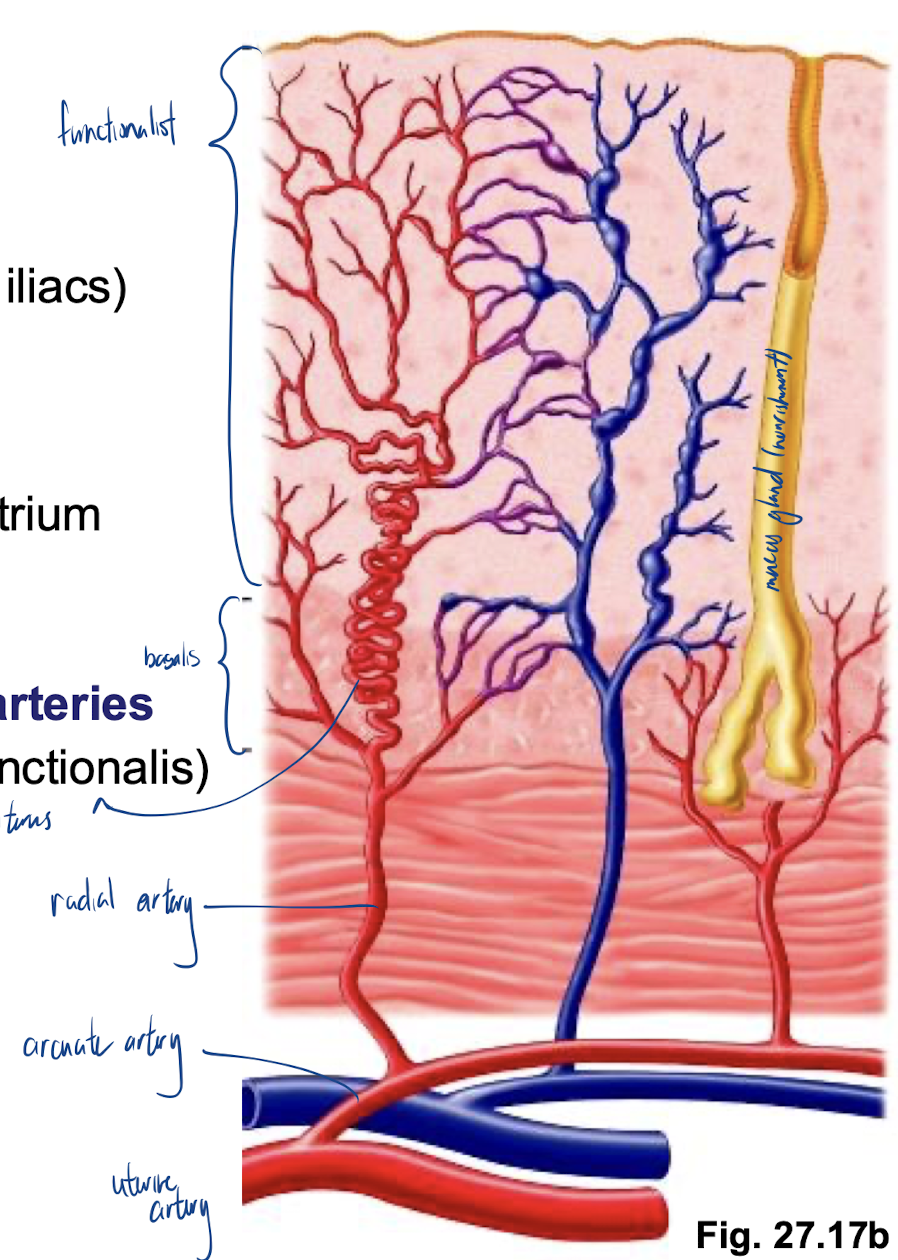
Cause for uterus lining to shed
Spiral artery constriction
Vagina structure
thin-walled tube, 8-10 cm long
urethra is anterior and runs parallel
no glands; lubrication provided by cervical glands
epithelial cells store glycogen and are shed → metabolized to lactic acid by resident bacteria → acidic pH deters infection, but is hostile to sperm
Vagina is a passageway for:
entry of sperm
exit of menstrual flow
delivery of infant
3 layers of the vagina
adventitia: outer, fibroelastic
muscularis: smooth muscle
mucosa: inner, transverse rugae; stratified squamous epithelium
Hymen
Incomplete vascular partition of mucosa near vaginal orifice; of variable durability; can rupture during first sexual intercourse, but also can be ruptured by sports, inserting tampons, even pelvic exams
External Genitalia
vulva: mons pubis, labia, clitoris, structures associated with vestibule
mons pubis: fatty, rounded area overlying pubic symphysis; covered with hair
labia majora: elongated, hair-covered fatty skin folds (homologue of scrotum)
labia minora: thin, hair-free skin folds enclosed by labia majora
vestibule: recess between labia minora - contains openings of urethra, vagina, & greater vestibular glands (homologous to bulbourethral glands)
clitoris: erectile tissue (homologous to penis); hooded by skin fold; richly innervated; corpora cavernosa but no corpus spongiosum
Ovaries have 2 key functions
produce oocytes
produce reproductive hormones (eg: estradiol, progesterone)
Remember:
the hormones a cell produces depends on the enzymes it has
steroids are lipids – can easily traverse PMs
Estradiol synthesis
CHOLESTEROL
progesterone
androstenedione
testosterone
estradiol
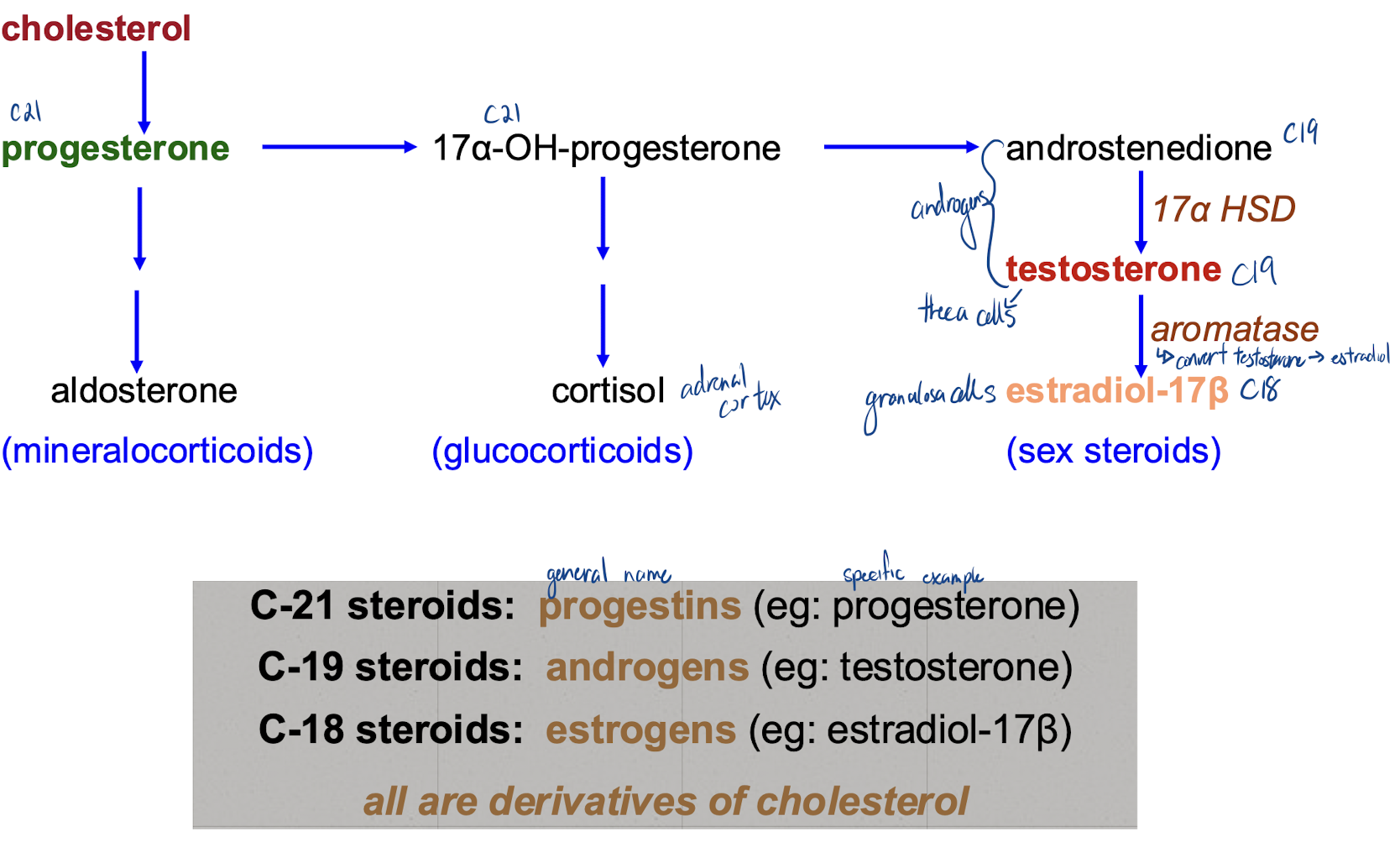
3 types of steroid hormones produced in the ovarian follicle
progestins
androgens
estrogens
Progestins
(eg: progesterone - all have 21 carbons)
produced by all major ovarian cell types: follicular granulosa cells, theca cells, corpus luteum
most important as a product of the corpus luteum - during luteal phase of menstrual cycle & for maintenance of pregnancy
Androgens
(eg: testosterone - all have 19 carbons)
most important as a precursor for synthesis of estradiol
synthesized by follicular theca cells and by corpus luteum
too much testosterone is associated with follicular atresia
Atresia
testosterone buildup causes degeneration of follicle
Estrogens
synthesized by follicular granulosa cells and the corpus luteum
essential for stimulation of follicular development, onset of puberty, etc.
(eg: estradiol - all have 18 carbons)
Anterior Pituitary Hormones
FSH
LH
FSH
Follicle-Stimulating Hormone
stimulates ovarian follicles to grow & produce estradiol
LH
Luteinizing hormone
stimulates testosterone production by theca cells
stimulates ovulation, secretion of steroid hormones by corpus luteum
released from anterior pituitary glands
Hypothalamus hormones
GnRH (gonadotropin-releasing hormone)
GnRH
Gonadotropin-releasing hormone
Stimulates secretion of the secretion of both FSH & LH
granulosa cells, like Sertoli cells, can produce inhibin
Primordial follicle
oocyte + single layer of flattened granulosa cellsstarting point = oocyte surrounded by single layer of flattened follicular cells (will become granulosa cells)
oocyte (primary oocyte) arrested at prophase of meiosis I
by 6 months of age, ovary has full complement of primordial follicles
~2 million at birth; gradual loss (degeneration); ~400,000 remain by puberty
Initiation of development of primordial follicles does NOT require ______ stimulation - some follicles can and do begin developing at ____
gonadotropic; any time
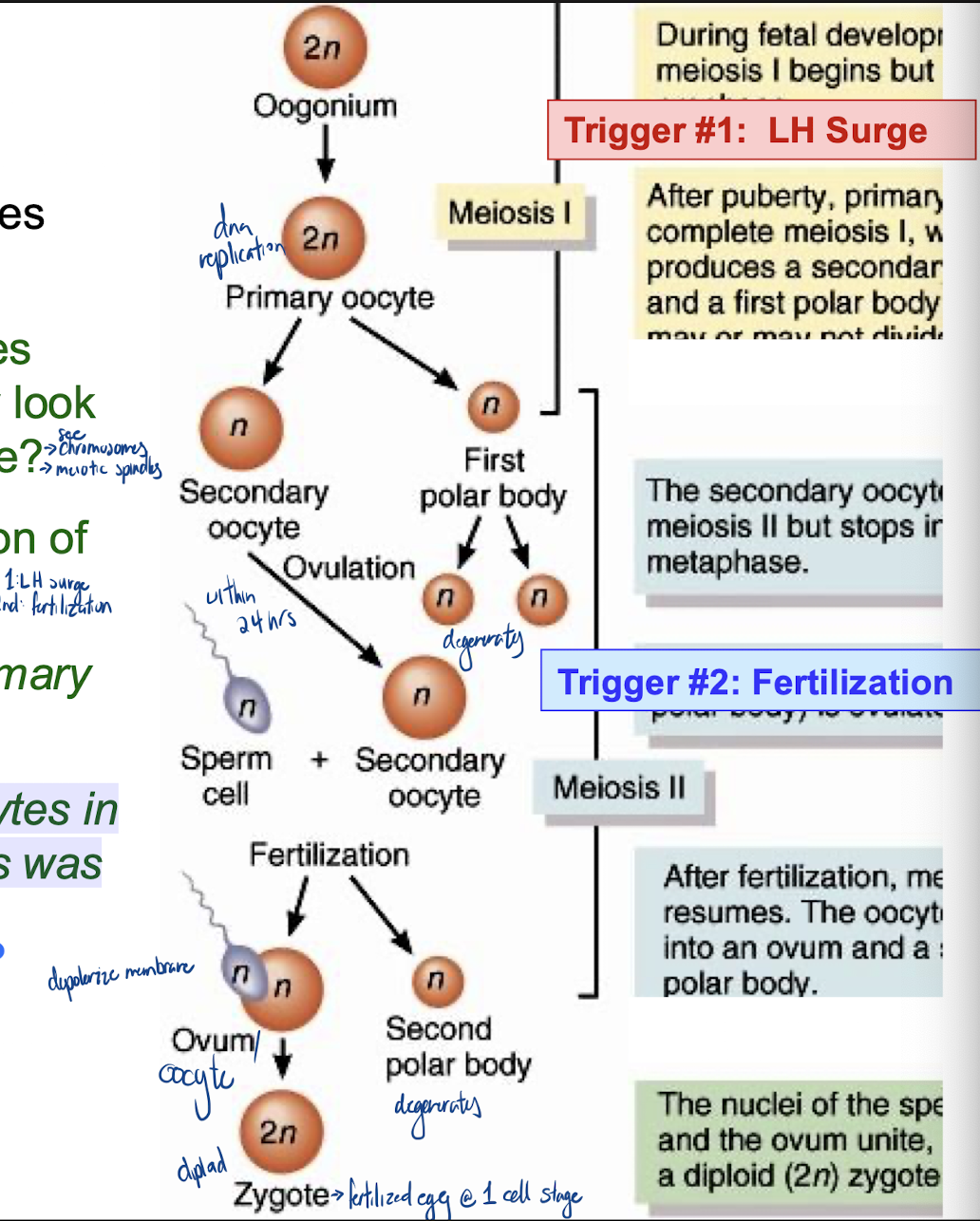
At what stage are oocytes arrested? What would they look like under the microscope?
prophase of meiosis 1
would see chromosomes and mitotic spindles
What triggers the resumption of meiosis the first time?
LH surge
Fertilization
What is the fate of most primary oocytes??
never resume meiosis
What is the fate of most oocytes in which resumption of meiosis was initiated by trigger #1?
most aren’t fertilized (dont complete meiosis)
Ovarian follicular development
Oogonia t primary oocytes accomplished by birth
Primary Follicle: Developmental Events
gonadotropin-independent
oocyte increases in size & acquires a zona pellucida
granulosa cells start to divide & form several layers outside oocyte
outside the basement membrane, ovarian interstitial cells closest to the growing follicle differentiate to form theca cells
throughout these changes called a primary follicle
continued maturation of this follicle requires FSH and LH
What is an antrum? Why is it important to have an antrum in a maturing follicle?
is a fluid-filled cavity that develops within a mature ovarian follicle, also known as a Graafian follicle
make it easier for ovulation to occur
Antral Follicle
a fluid-filled sac on the ovary containing an immature egg
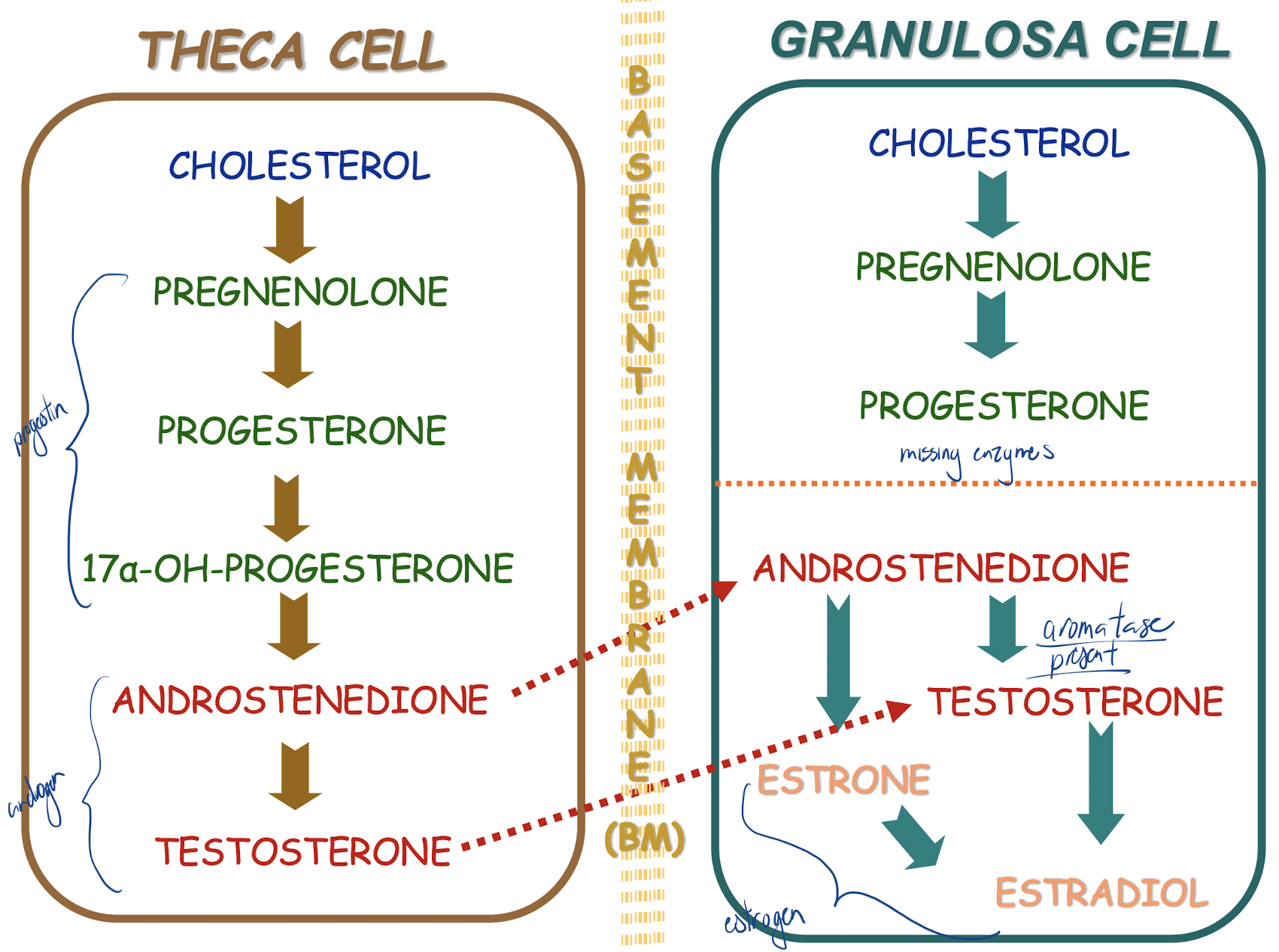
Basement membrane divides follicle into 2 compartments
inner granulosa cell compartment
outer theca cell compartment
Inner granulosa cell compartment
nonvascularized
FSH-responsive:
granulosa cell proliferation (E)
granulosa cell E production
more FSH receptors
Outer theca cell compartment
vascularized
LH-responsive
T production for use by granulosa cells to make E
Theca cell and granulosa cell hormone production diagram
Theca cells dont have the enzyme (aromatase) to convert to estrogen so its needs to be transferred to granulosa cells where the enzyme is present to convert to estrogens
Timing is Everything!
if development coincides with rising FSH levels at beginning of cycle → development will be supported - otherwise: follicular atresia
for one follicle to become dominant, must convert potentially androgenic environment to estrogenic environment - otherwise: atresia!!
Emerging dominant follicle becomes the __________
preovulatory follicle
E levels rise rapidly - FSH switches to inducing receptors for LH on granulosa cells (Why does this make sense? granulosa cells become corpus luteum (LH sensitive only)) → LH stimulates further E & P production stage is now set for LH surge to trigger ovulation
LH surge stimulates
resumption of meiosis - extrusion of polar body #1
P (progesterone) production by granulosa cells
increase in antral fluid volume
release of hydrolytic enzymes
Minor FSH surge
ensures sufficient LH receptors for luteal phase
stimulates synthesis of hyaluronic acid - important in cumulus expansion (let go of tight junctions, help pull oocyte off)
What are cumulus cells?
sub population of grannular cells around oocyte, eventually degenerate
what is a cumulus-oocyte complex (COC)?
oocyte + 2-3 cummulus layers + hyaluraunic acid
Corpus luteum
luteinized granulosa + theca cells + capillaries
yellow body (lots of lipid droplets for steroid production)
a temporary collection of cells that forms on your ovary each menstrual cycle if you're still getting a menstrual period.
appears right after an egg leaves your ovary (ovulation).
job is to make your uterus a healthy place for a fetus to grow.
Unless a pregnancy intervenes, lifespan of CL is
~12 days
Hormone release during different phases of cycle
Proliferative phase: peak estrogen before peak of LH followed by peaking of FSH on edge of to secretory phase.
Secretory phase: Progesterone major peak, smaller estrogen increase
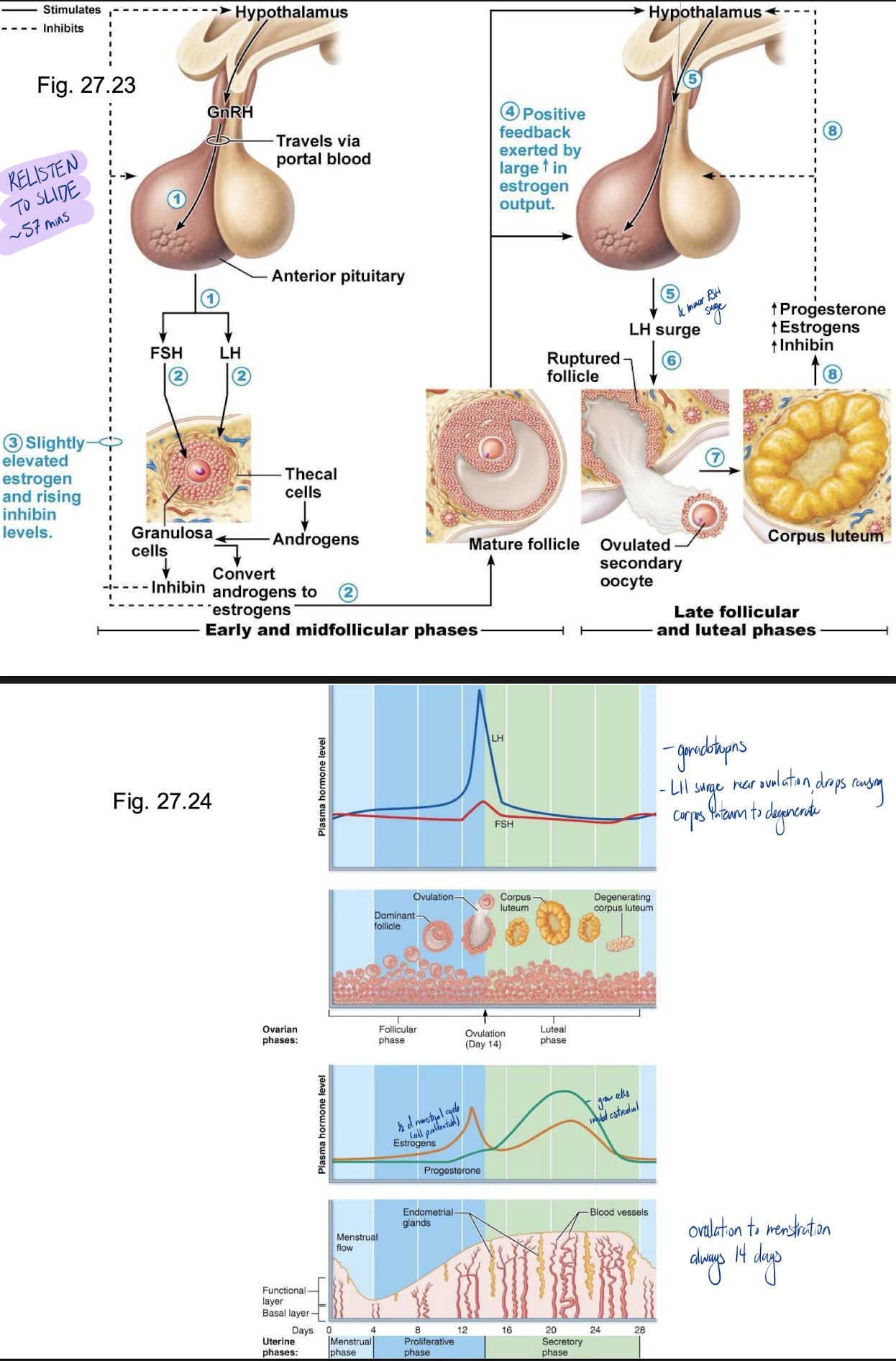
Proliferative phase
resurfacing of epithelium
cell proliferation in response to ovarian E
development of spiral arteries & uterine glands
cervical mucus becomes thin; forms channels that facilitate sperm passage
follicular phase of ovary
Secretory/ovulation Phase
thickening of whole layer due to cell growth & fluid retention
As LH levels decline, CL begins to degenerate (~D24) → in absence of P secretion, uterine endometrium is shed & cycle begins again
When is endometrium maximally receptive to embryo implantation?
Day 21
Why is it called the secretory phase?
glands release glycogen rich secretion in case
What is the cervical plug?
thick and viscous prevent infection
If oocyte is fertilized
hCG is produced in increasing amounts beginning D9-13 after ovulation; hCG rescues the CL until placental progesterone can maintain the pregnancy
hCG
Human chorionic gonadotropin
in early embryo
bind to LH, extend life of corpus luteum
Hormonal regulation of puberty
initial hormonal events are the same in males & females
in females, FSH stimulates E secretion by granulosa cells (LH stimuation provides T precursor from theca cells)
cycles of proliferation & regression until sufficient growth occurs that withdrawal of steroid support (due to atresia of follicles) results in first menstruation (menarche)
first ovulatory cycle often may not occur until a few months later
concept of a critical weight to reach before menarche:
specifically, a critical ratio of fat to lean – Why? (think about aromatase activity in adipose tissue as well as adipose-cell-derived leptin and GnRH release)
adipose tissue for nutrient reserve
adipose tissue has aromatase enzymes, increasing estrodial
Estradiol responsible for what during puberty?
growth & maturation of breasts, reproductive organs
fat redistribution
bone maturation (growth → closure of epiphyseal plates)
(all processes gradually completed over a ~4-year period)
What is menopause?
cessation of menses for at least 12 months
in North America, occurs at mean age of 51.4 years
primary cause is depletion of ovarian follicles
Perimenopause
• extends from early 40s onward - « transitional years »
• ovarian function begins to wane - deprivation of estrogen (and its effects on FSH/LH secretion) can result in: hot flushes, insomnia, irritability, fatigue, headaches, depression/mood changes, loss of libido, poor mental performance/ nervousness, loss of skin elasticity
Menopause occurs at what age
median age of 51.4 years; can live 1/3 of life after ovaries have ceased functioning
Loss of ovarian E affects all tissues that have E receptors
genital tissues: atrophy, vaginal dryness, higher incidence of vaginal infections (lose acid secretions)
urinary tract: linings of bladder & urethra have E receptors; loss of E can lead to increased urinary frequency, urgency, even incontinence
breasts: some atrophy
CV system: atherosclerosis, stroke
estrogen has protective effects (decrease risk before menopause, with menopause causes increased level as men)
skeleton: osteoporosis
Cumulus layer
also known as the cumulus oophorus, refers to a layer of cells surrounding the oocyte (egg cell) in the ovary