NSAIDs and Paracetamol
1/147
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
148 Terms
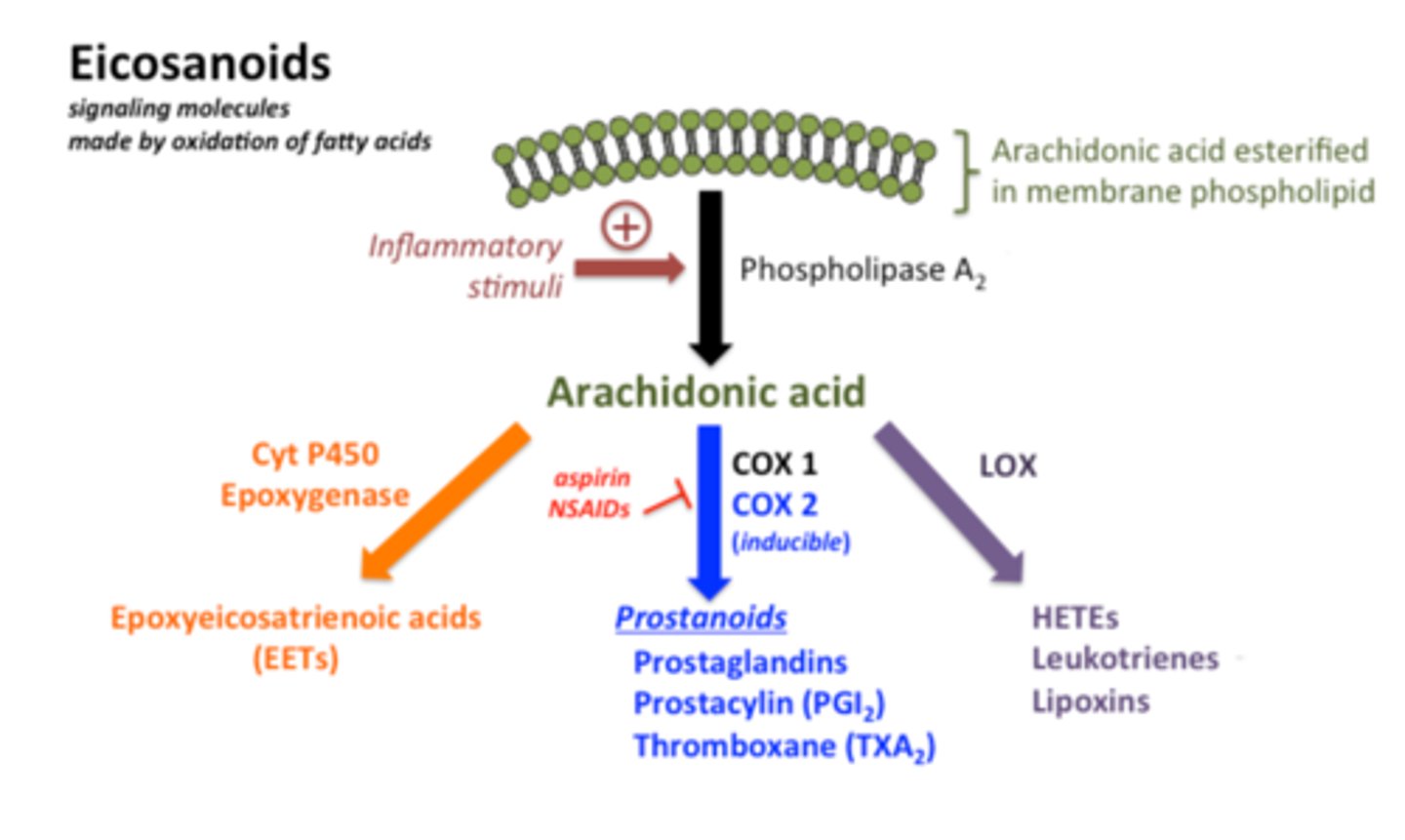
what is the mechanism of action of NSAIDs?
block COX1 or COX2, which are the enzymes that convert arachidonic acid into prostaglandins (inflammatory molecules)
what important NSAID is a salicylate?
Acetylsalicylic acid/Aspirin
Salicylates (Acetylsalicylic acid, Aspirin) have what effects on the animal?
analgesic
antipyretic
anti-inflammatory
antiplatelet aggregation (blood thinning effect)
what adverse effects might a patient present when using Salicylates (Acetylsalicylic acid, Aspirin)?
dogs- mucosal erosion and ulceration
vomiting and melena at high doses
what NSAID is sometimes given chronically at low doses in order to prevent cardiovascular effects due to thrombus?
Acetylsalicylic acid/Aspirin
which biotransformation reaction (I or II) do Salicylates (Acetylsalicylic acid, Aspirin) go through?
both
how are Salicylates (Acetylsalicylic acid, Aspirin) excreted?
urine
which species is more susceptible to the toxic effects of Salicylates (Acetylsalicylic acid, Aspirin)? what adjustment must be made in this case?
cats, because they cannot metabolize it rapidly. therefore, we must increase the dosing interval to 2+ days
clinically, what do we use Salicylates (Acetylsalicylic acid, Aspirin) for?
-minor pain and inflammation in chronic conditions, such as arthritis
-antipyretic in large animals
-antiplatelet effects in thromboembolic disease
what must we be aware of when using Salicylates (Acetylsalicylic acid, Aspirin) as an antiplatelet drug?
there is the possibility of interaction with oral anticoagulants, which can cause bleeding
which NSAIDs can be used as an antipyretic in large animals?
Salicylates (Acetylsalicylic acid, Aspirin)
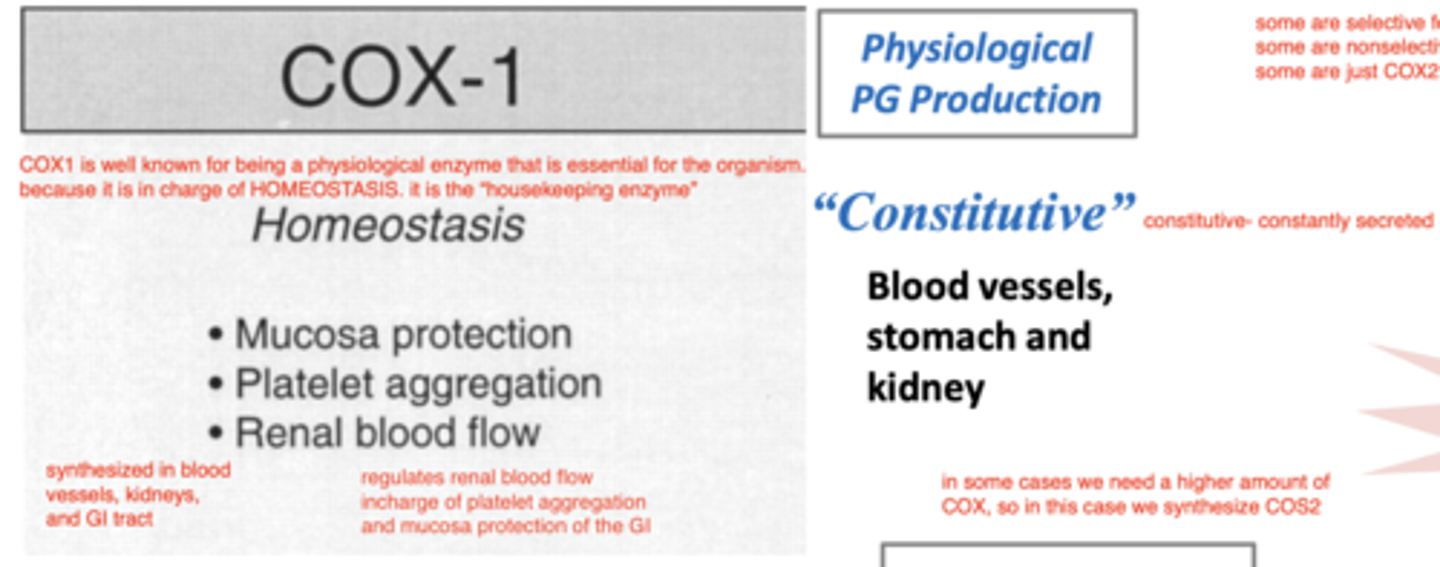
which, COX1 or COX2 is constitutive? what does this mean?
COX1
this means that it is always active (constantly secreted in the body)
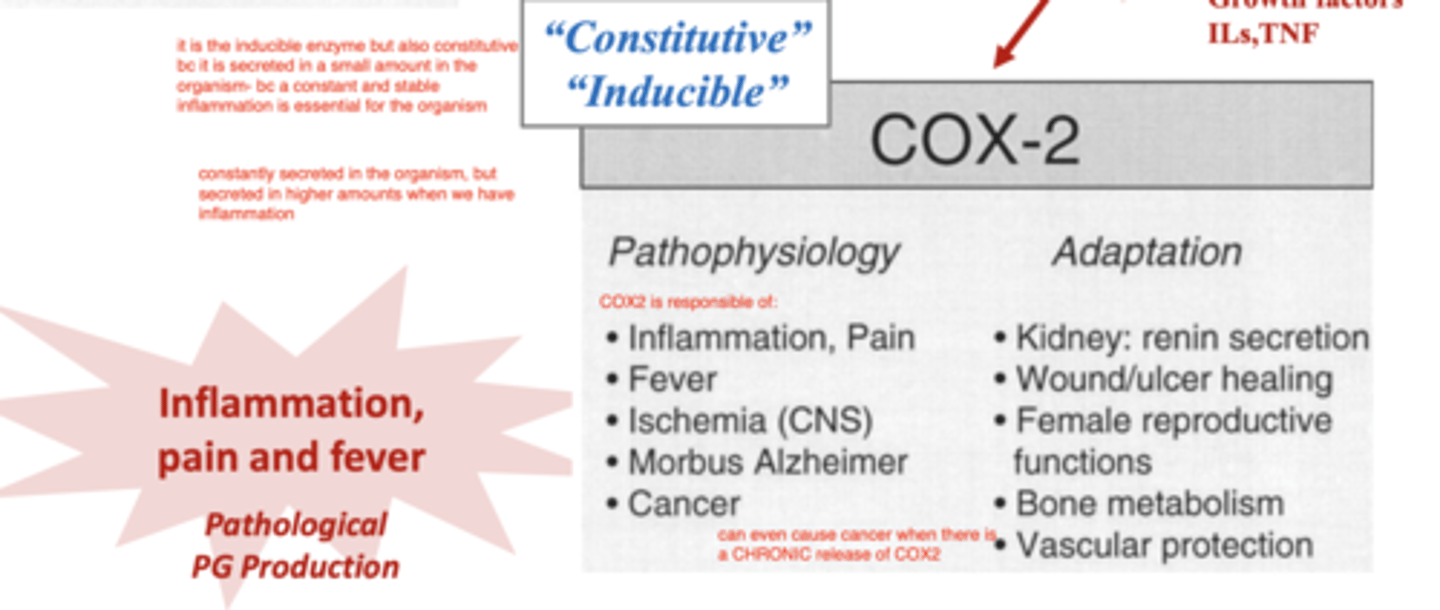
which, COX1 or COX2 is inducive? what does this mean?
COX2
this means that there must be a trigger for its release (it is only released when there is an inflammatory stimulus)
what is COX1?
an constitutive enzyme, constantly released in the blood vessels, stomach, and kidney, as a "housekeeping enzyme"- it is essential for the organism. it regulates renal blood flow, and is
in charge of platelet aggregation and mucosa protection of the GI.
it works by synthesizing prostaglandins.
what is COX2?
an inducible enzyme, that is released in response to inflammatory stimuli into the site of inflammation.
it converts arachidonic acid into prostaglandins, and causes inflammation, pain, fever, ischemia (CNS), Alzheimer Morbus, and even cancer.
where are Salicylates (Acetylsalicylic acid, Aspirin) absorbed in the body?
stomach and duodenum
(they have a marked first-pass effect)
does aspirin have GI side effects?
yes, it can cause mucosal erosion and ulceration in dogs.
which COX do Salicylates (Acetylsalicylic acid, Aspirin) act against?
COX1
is aspirin COX1 or COX2 specific?
COX1
which NSAID is a pyrazolone derivative?
phenylbutazone
what are the effects of phenylbutazone?
anti-inflammatory
antiplatelet
does aspirin have analgesic action?
yes
also has antithrombic, anti-inflammatory, and anti-pyretic effects
does phenylbutazone have antiplatelet action?
yes
also has anti-inflammatory effect
where is phenylbutazone absorbed in the body?
digestive tract
does phenylbutazone have a high or low affinity for plasma proteins?
high (99%)
so is more likely to have reactions with other drugs, especially warfarin
phenylbutazone is used in ______ (species) to relieve pain related with ______
horses; arthritis
which NSAID is contraindicated in food-production species because of its immunosuppressive effects?
phenylbutazone
why is phenylbutazone contraindicated in food producing species?
because it has immunosuppressive effects
how is phenylbutazone excreted?
urine
what are the possible side effects of phenylbutazone?
diarrhea
anorexia
ulcers
colitis
perivascular admin- swelling, necrosis, sloughing at injection site
is it recommended to administer phenylbutazone parenterally?
no, because this can cause necrosis, swelling, and sloughing at the injection site
which is the most commonly used NSAID in horses due to its effectiveness and affordability?
phenylbutazone
what is the main clinical use of phenylbutazone in vet med?
relieve pain related with arthritis in horses
do we use phenylbutazone in dogs?
it is not recommended, because it can cause bone marrow suppression and anemia
which NSAIDs are anthranilic acid derivatives?
tolfenamic acid
flunixin meglumine
what is tolfenamic acid used for in veterinary medicine?
to reduce inflammatory processes related to locomotion and postoperative treatments.
most commonly used in small animals, especially cats.
tolfenamic acid has a higher specificity against _______ (COX1 or COX2)
COX1
which NSAID is good for treating inflammatory processes related to locomotion in small animals?
tolfenamic acid
what adverse reactions can tolfenamic acid produce?
GI irritation- vomiting, diarrhea, decreased appetite
what effects does tolfenamic acid have on the body?
antiinflammatory
antiplatelet
does tolfenamic acid have antiplatelet effects?
yes
+ antiinflammatory
which is more potent- flunixin or phenylbutazone?
flunixin
what is the main effect of flunixin on the body?
analgesic
how can we administer flunixin?
orally or parenterally
flunixin is eliminated from the body by ____
feces
what adverse reactions are possibly produced by flunixin?
mild gastric intolerance
hypoprothrombinemia
what are the clinical applications of flunixin in veterinary medicine?
-treat visceral pain associated with colic in horses
-treat musculoskeletal inflammation
-decrease the inflammatory mediated hemodynamic response to endotoxins
which NSAIDs are the most effective in treating endotoxemia?
flunixin
phenylbutazone
meloxicam
which NSAID is commonly used in horses to treat visceral pain associated with colic?
flunixin
what NSAIDs are belonging to the group of arylpropionic acid derivative?
carprofen
ibuprofen
ketoprofen
noproxen
which arylpropianic acid derivative NSAID is used in animals?
carprofen
carprofen has greater selectivity for _______ (COX1 or COX2)
COX2
carprofen is used in what species?
small animals, especially dogs
what are the effects of carprofen in the organism?
anti-inflammatory
analgesic
how is carprofen administered?
orally
what are the adverse reactions that can be produced by carprofen?
vomiting, diarrhea, anorexia
rare risk of renal or hepatic adverse reactions
what do we use carprofen for in veterinary medicine?
in small animals, especially dogs
long term management of arthritis
acute pain associated with soft tissue and orthopedic surgery
which NSAID is commonly used in dogs to treat acute pain that is associated with soft tissue and orthopedic surgery?
carprofen
what NSAID is commonly used in dogs for the long term management of arthritis?
carprofen
why are ibuprofen, ketoprofen, and naproxen contraindicated in animals?
because they cause severe GI problems- vomiting and possibly death due to GI bleeding from ulcers
which common human NSAIDs are contraindicated in animals due to their severe GI effects (vomiting, death due to GI bleeding by ulceration)?
ibuprofen
ketoprofen
naproxen
does meloxicam target COX 1 or COX2?
COX2
what are the effects of meloxicam?
analgesic
antiinflammatory
which NSAID is considered to be a good analgesic in comparison to other NSAIDs of their class, but occasionally needs analgesia supplementation to achieve desired levels of post surgical analgesia?
meloxicam
why might we sometimes use analgesia supplementation with meloxicam?
to achieve desired levels of postsurgical analgesia
what are the adverse reactions produced by meloxicam?
GI toxicity and perforation (but not much)
NSAIDs that target COX__ (1 or 2) have more GI effects
COX1
how can we administer meloxicam?
oral
SC
IM
IV
what is meloxicam commonly used for?
to treat acute and chronic inflammation associated with musculoskeletal disease and postoperative pain
it can be used in dogs, cats, horses, cattle, pigs
meloxicam is approved for use in what species?
dogs, cats, cattle, pigs, horses
in cats, what NSAID is well tolerated and safe for chronic administration?
meloxicam
which NSAID can be used for its antiexudative action in respiratory conditions, such as pneumonia or endotoxemia?
meloxicam
what are coxibs?
the group of NSAIDs with the highest effect against COX2. this includes firocoxib, deracoxib, and robenacoxib
which NSAIDs have the most effect against COX2?
coxibs- firocoxib, deracoxib, and robenacoxib
which coxib is the most commonly used in vet med?
robenacoxib
(given 1x daily)
is Robenacoxib effective against COX1 or COX2?
VERY effective against COX2
what are the effects of coxibs (firocoxib, deracoxib, and robenacoxib)
analgesic
anti-inflammatory
what are the adverse reactions an animal might have to coxibs (firocoxib, deracoxib, and robenacoxib)?
possible vomiting and anorexia, but rare
NOT gastrolesive
Cardiovascular effects
which, COX1 or COX2 inhibitors are more safe for the GI tract?
COX2 inhibitors
what are the common clinical applications of coxibs (firocoxib, deracoxib, and robenacoxib)?
treatment of postoperative pain and inflammation associated with osteoarthritis, orthopedic and soft-tissue surgery in dogs; musculoskeletal disorders and soft-tissue surgeries in cats
which NSAID is commonly used for the treatment of postoperative pain and inflammation associated with osteoarthritis, orthopedic and soft-tissue surgery in dogs?
coxibs (firocoxib, deracoxib, and robenacoxib)
which NSAID is preferred for the treatment of musculoskeletal disorders and soft-tissue surgeries in cats?
coxibs (firocoxib, deracoxib, and robenacoxib)
what is grapiprant?
not an NSAID, but a new molecule that is a selective antagonist for the EP4 receptor (this is the PGE2 receptor that is responsible for pain and inflammation associated with arthritis)
what is the MOA of grapiprant?
selective antagonist for the EP4 receptor (this is the PGE2 receptor that is responsible for pain and inflammation associated with arthritis)
which drug is a selective antagonist for the EP4 receptor (this is the PGE2 receptor that is responsible for pain and inflammation associated with arthritis)?
grapiprant
what are the effects of grapiprant?
antiinflammatory
how do we administer grapiprant?
orally
what are the possible adverse reactions that can come with grapiprant?
vomiting and inappetance
not gastrolesive
what are the clinical uses for grapiprant?
treatment of osteoarthritis in dogs (they are a good, safer alternative for OA, but are not as effective in treating acute pain)
which is the safest option for the treatment of osteoarthritis in dogs?
grapiprant
which is more effective- traditional NSAIDs or grapiprant?
traditional NSAIDs
which is the new molecule that was approved by the FDA for vet med in 2016, and is used as an osteoarthritis treatment in dogs?
grapiprant
what are Eicosanoids?
signalling molecules made by the oxidation of fatty acids. by action of phospholipase2 (released by inflam. cells), they are converted into arachidonic acid, which is converted by COX 1 and COX 2 into prostaglandins
what are prostanoids?
signalling molecules including prostaglandins, prostacyclin, thromboxane.
synthesized from arachidonic acid by COX1 and COX2.
promote inflammation (pain, fever, and all other inflam. signs)
which- COX1 or COX2- induces the pathological production of prostaglandins?
COX2
which- COX1 or COX2- induces the physiological production of prostaglandins?
COX1
COX2 can be dangerous to the body.. what adaptations have animals acquired for protection?
-renin secretion
-wound/ulcer healing
-female reproductive functions
-bone metabolism
-vascular protection
what triggers the production of COX2?
inflammation (cytokines, growth factors, ILs, TNF)
how are NSAIDs classified into categories?
according to their chemical structure
NSAIDs are ____soluble, so are well absorbed after ______ administration
lipid; oral