Embryology - Part 2
1/74
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
75 Terms
Development of the Cornea
What role does the developing anterior epithelium of the lens play in corneal development?
Induction by the developing lens anterior epithelium signals multiple steps in corneal development at the time when the lens vesicle separates from the surface ectoderm
Development of the Cornea
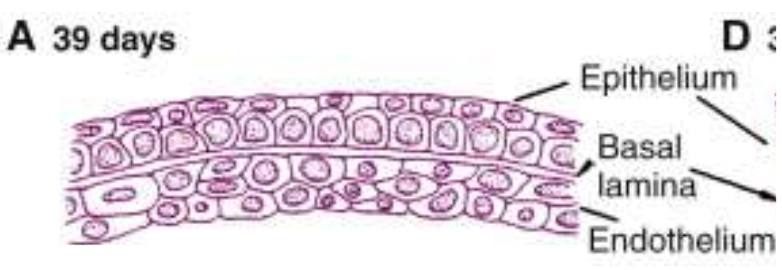
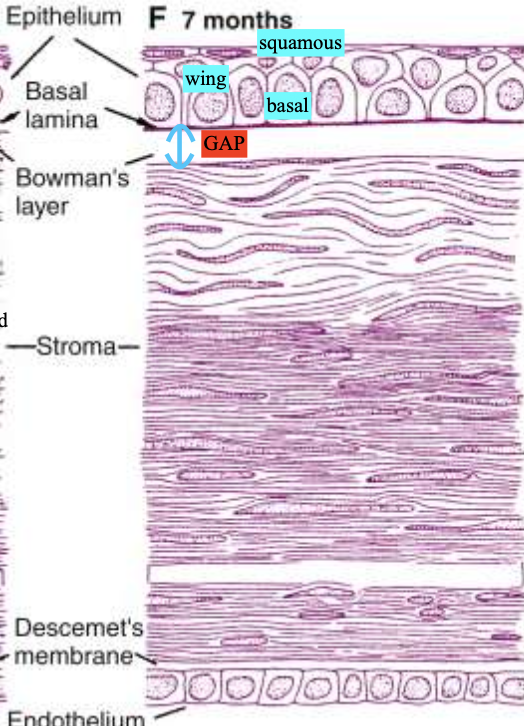
What occurs at 39 days of Corneal Development?
epithelium is a 2-layered structure resting on a basal lamina
endothelium (2-3 layers)
both separated by a narrow cellular space
Development of the Cornea
What occurs at 7 weeks of Corneal Development?
Mesenchyme (fibroblasts) from the periphery migrates between epithelium and endothelium to form the stroma precursor
Fibroblasts → collagen fibers secreted
Stroma is multilayered (5-7 layers thick)

Development of the Cornea
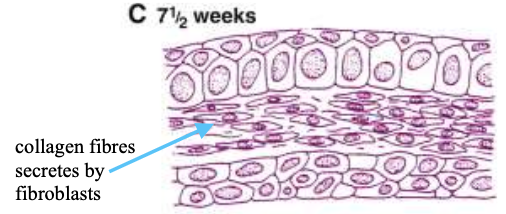
What occurs at 7.5 weeks of Corneal Development?
Mesenchyme (fibroblasts) is arranged in 4-5 incomplete layers
some collagen fibrils begin to appear
Development of the Cornea
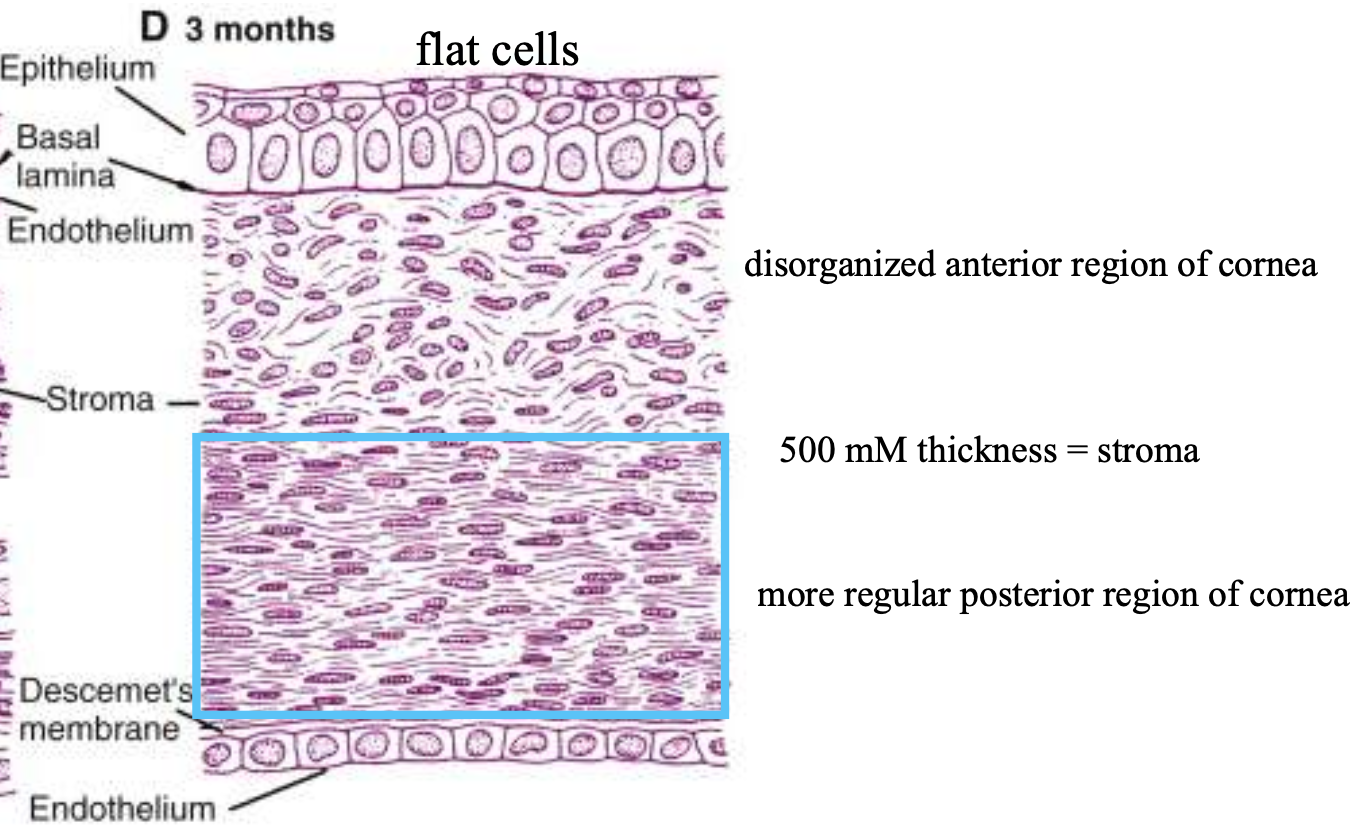
What occurs at 3 months of Corneal Development?
epithelium has 2-3 layers
stroma has 25-30 layers of fibroblasts (keratoblasts), which are more regularly arranged in the posterior half
Descemet's membrane is thin and uneven b/w most posterior keratoblasts & endothelium
Endothelium is 1 layer
Development of the Cornea
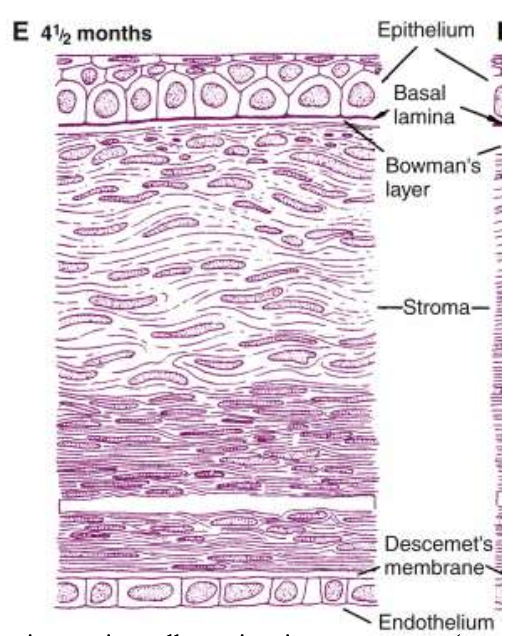
What occurs at 4.5 months of Corneal Development?
Wing cells begin to form above basal epithelial cells.
Bowman's layer begins to emerge under the basal lamina
anterior portion of the stroma stays disorganized, while the posterior stroma becomes more organized
Descemet’s membrane becomes well-developed
Development of the Cornea
What occurs at 7 months of Corneal Development?
Has adult cornea structure
some superficial keratoblasts in stroma stay randomly oriented
Collagenous lamellae in the rest of the stroma are in parallel arrays, with few gaps
gaps get filled by 9 months
Descemet's membrane is fully formed and continuous
Development of the Cornea
What is the role of the First wave of mesenchyme?
- Migrates into the space b/w the corneal epithelium & lens → forms corneal endothelium
By week 8, the mesenchyme proliferates and forms 2 cell thick layers (cuboidal cells) → cells give rise to fibroblasts which produce collagen & ground substance of the stroma
Development of the Cornea
What is the role of the Second wave of mesenchyme?
→ Migrates b/w the developing epithelium & endothelium
this wave helps form the aq humor
Development of the Cornea
What is the role of the Third wave of mesenchyme?
migrates into the area b/w the endothelium and lens → pupillary membrane development
Development of the Cornea
Where do all 3 waves of mesenchyme all originate from?
Neural crest
Development of the Cornea
How does the Corneal Curvature change at birth vs 6 months?
→ Rapid growth of the corneal stroma increases curvature relative to the rest of the globe
At birth: curvature is 55D (circular and steep)
By 6 months: curvature is 44D
Development of the Cornea
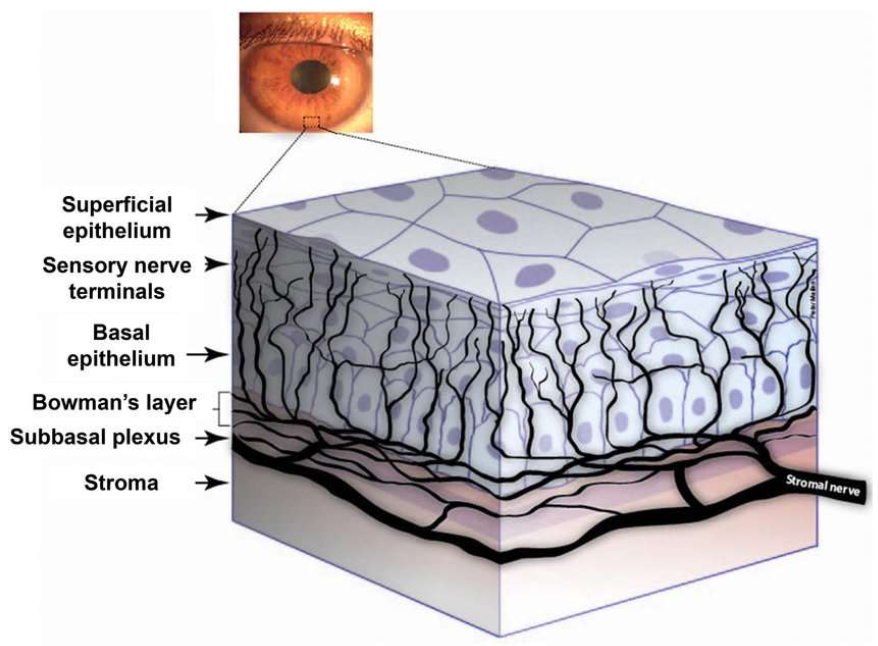
When do corneal nerves enter the developing cornea?
3 months
Development of the Cornea
Describe the development of the Corneal nerves.
Month 3: Corneal nerves enter cornea
Month 5: Nerves grow through the stroma to reach the epithelium
Month 5 to birth: Nerves increase & branch → diffuse whorl network formed in the stroma and subepithelial layers
by the time the eyelids open at 5 months, the cornea is highly innervated
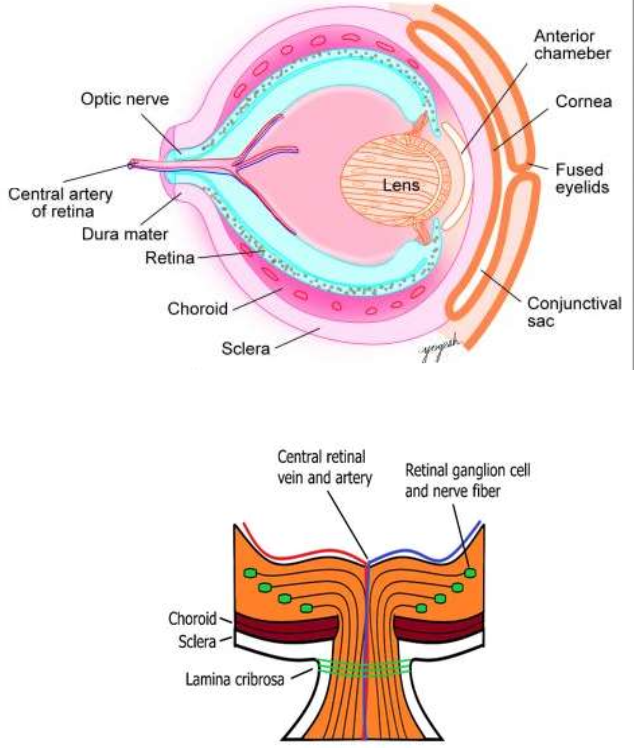
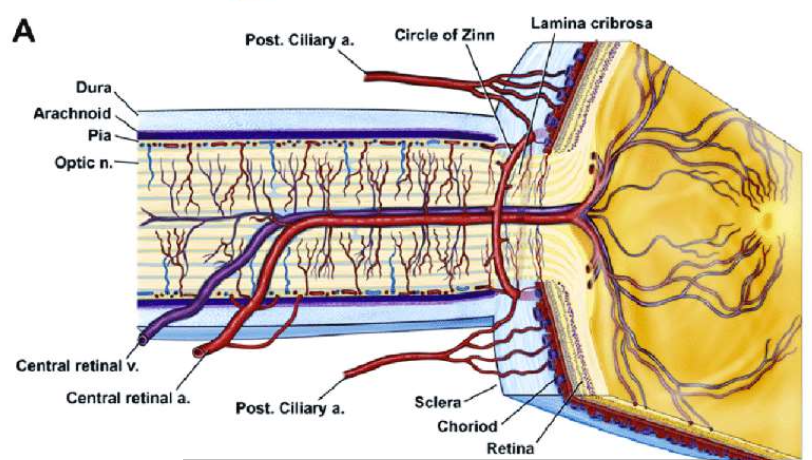
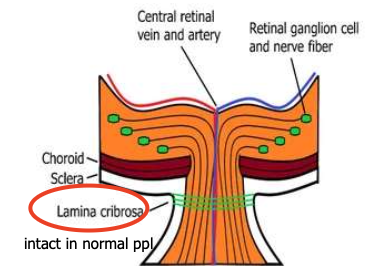
Development of the Sclera
Describe the development of the Sclera.
First develops anteriorly from condensations in the mesenchyme near the limbus
Month 3: Growth continues as it surrounds the optic nerve
Month 4: CT fibers cross the posterior scleral foramen through the optic nerve, producing the 1st CT strands of the lamina cribrosa
Month 5: Sclera (and scleral spur) is well-differentiated
Development of the Sclera
Describe the role of Induction in Scleral development.
RPE cells are needed to initiate scleral development, but not required to complete it
If fetal fissure fails to close, scleral formation continues, but may result in an iris coloboma
Development of the Sclera
What is Scleral development largely controlled by?
IOP
Aq formation
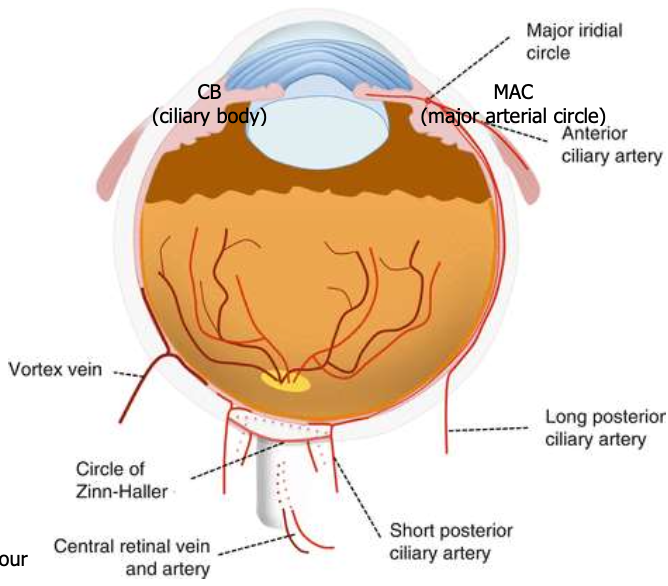
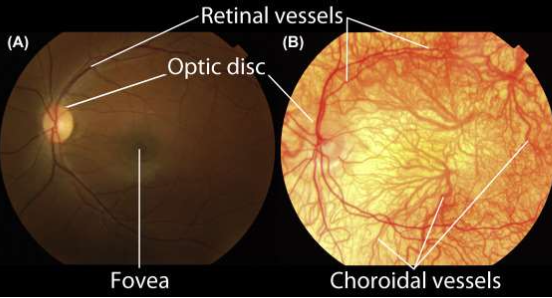
Development of the Choroid
Outline the Choroid Development.
Month 2: Choroid vessels appear
Month 3: Fenestrations in the vessels, covered by a diaphragm (thin membrane) appear
Month 4: Bruch’s membrane develops (prevents choroid vessels from entering the retina)
Month 5: Layers of the large & medium vessels are evident → vortex veins
SPCA are evident + begin to anastomose → Circle of Zinn
Appears last: BM of the choriocapillaris
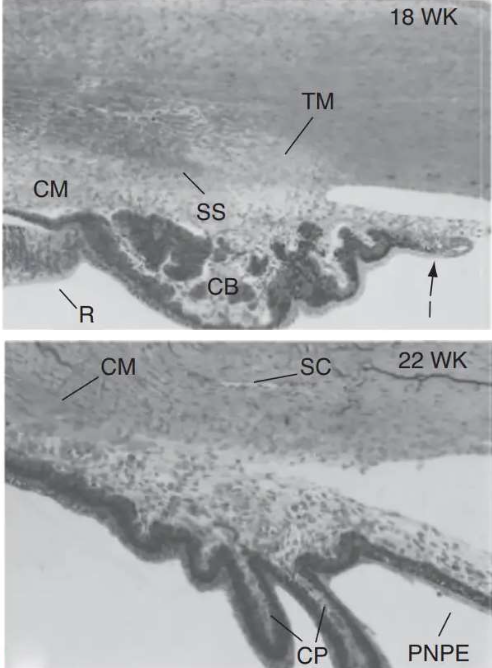
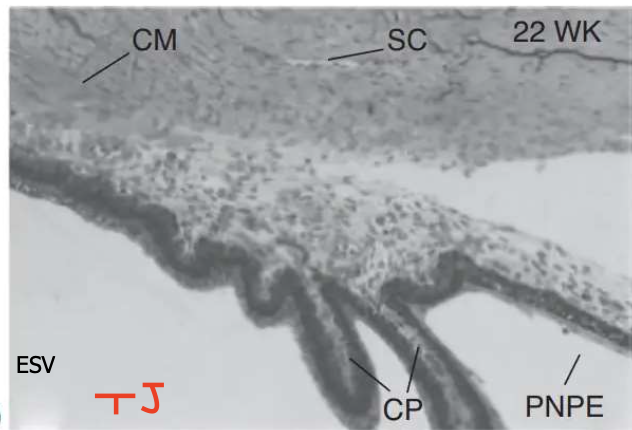
Development of the Ciliary Body
Describe the development of the Ciliary body.
Outer optic cup → outer pigmented epithelium (3rd month)
Inner optic cup → non-pigmented epithelium (NPE) + folds
Folds → ciliary processes
Tight junctions (zonula occludens) appear in NPE (3rd month)
LPCA & ACA anastomosis → Major arterial circle (4th month)
Neural crest → ciliary muscle (5th month)
Development of the Choroid
When does Aq humor production start?
4–6 months
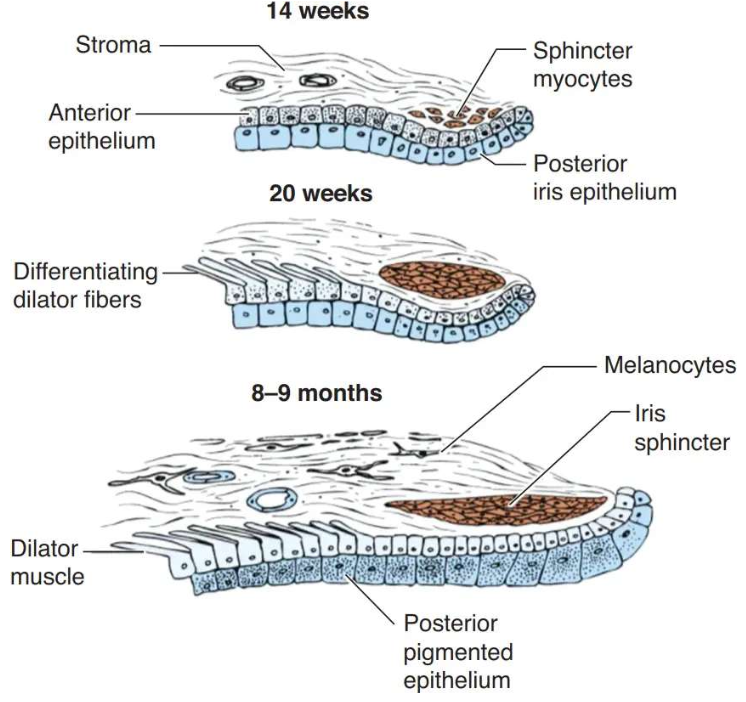
Development of the Iris
How does the Optic Cup contributes to the development of the Iris?
1) Lip of optic cup elongates b/w lens + developing cornea (end of 3rd month)
Outer optic cup layer → anterior iris epithelium
Inner optic cup layer → posterior iris epithelium
2) 2 epithelial layers are joined apex-to-apex (via intercellular junctions)
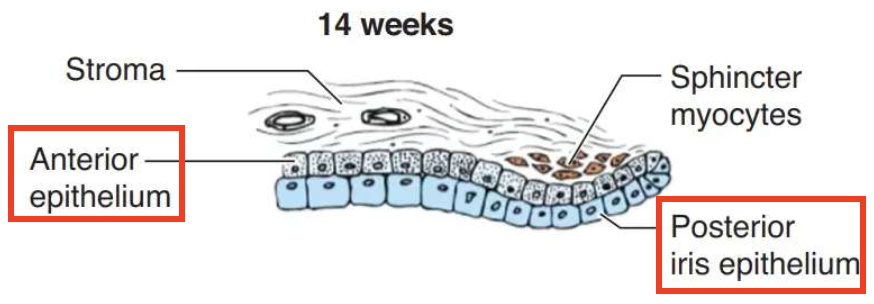
Development of the Iris
How do the spincter & dilator muscle contributes to the development of the Iris? (Mention when this occurs too)
Sphincter muscle (5th month)
Cells from anterior iris epithelium break away into stroma → differentiate into smooth muscle fibers → iris sphincter
Dilator muscle (6th month)
Forms within anterior iris epithelium
Both sphincter & dilator fully developed by birth
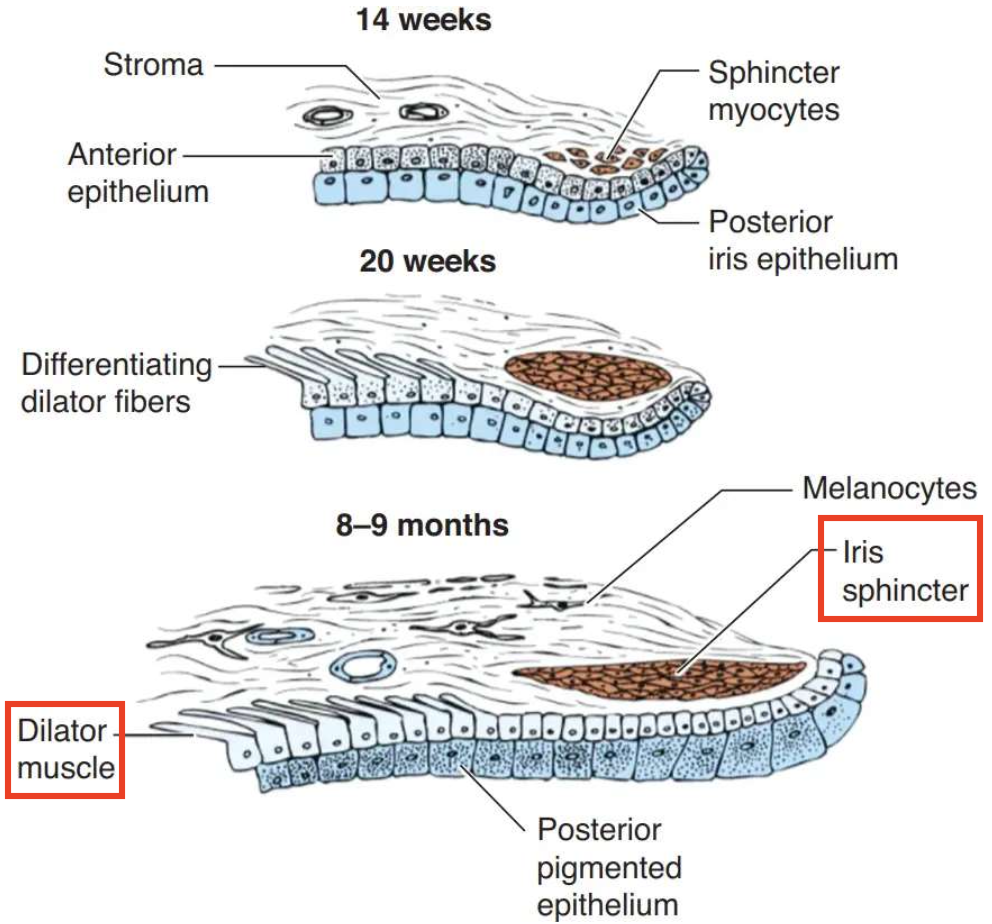
Development of the Iris
What’s the timeline of Iris pigmentation development? (Mention when this occurs too)
Week 10: Pigmentation begins
7 months: Pigmentation complete
Postnatal: Darkening up to ~6 months via stromal melanocytes; stromal maturation until ~7 years
Development of the Iris
How does the ABL & Stroma form?
Mesenchymal cells line up → ABL (with gaps)
Collagen begins to accumulate → iris stroma
More densely packed stromal melanocytes = darker iris color
Development of the Iris
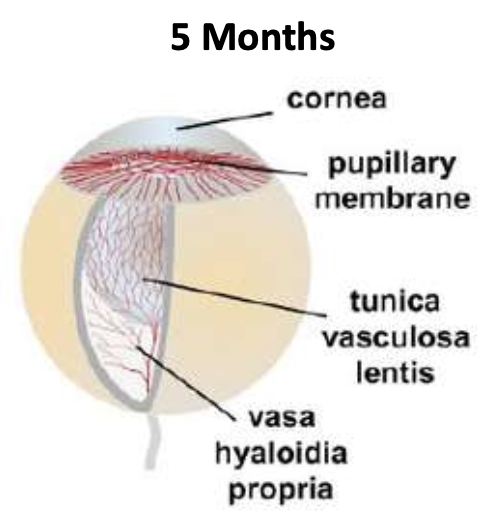
When and where is the Pupillary Membrane formed?
→ Formed during Month 3 from 3rd wave mesenchyme + branches of major circle of iris
forms b/w lens epithelium & corneal endothelium
has 3–4 vascular arcades present by the end of Month 5
Development of the Iris
How does pupillary membrane atrophy occur? (Mention dates)
Month 6: Central vessels become atrophy + become bloodless
By ~8.5 months: Central vessels fragment & disappear
Peripheral vessels contribute to the minor arterial circle of iris
Note: Breakdown of central vessels = key sign pupil is forming shape

Development of the Clilio Iridic Circulation
When does vascular supply of the iris & pupillary membrane begins developing? What supplies it with blood?
8 months via LPCA
Development of the Clilio Iridic Circulation
What’s the role of the LPCA in the vascular supply of the Cilio Iridic circulation?
→ help form the Major Arterial Circle
MAC provides vascular supply to the:
Anterior segment
Pupillary membrane
Iris
ciliary body
Development of the Anterior Chamber.
How is the Anatomical space of the Anterior Chamber created? When does this occur?
During weeks 7 and 8
Undifferentiated mesenchymal tissue b/w corneal endothelium & anterior surface of iris stroma resorb from the centre to the periphery
This creases large gaps → anterior chamber
This entire process is completed by remodeling the tissues
Development of the Anterior Chamber
What growth factors contribute to the growth of the Anterior Chamber?
Every tiny kitty has fuzzy paws
Epidermal (EGF)
Transforming (TGFβ)
Keratinocyte (KGF)
Hepatocyte (HGF)
Fibroblast (FGF)
Platelet-derived (PDGF)
Development of the Anterior Chamber
Where are growth factors presented?
Why is the production of growth factors from corneal cells important?
→ Found in the tear fluid & aq humour
allow for the maintenance and renewal of normal anterior eye tissues
Development of the Anterior Chamber
What are the Major theories in the creation of the Anterior chamber angle?
1) Reorganization Theory: Cellular differentiation and reorganization of the mesenchymal/neural crest cells → mature meshwork of beams & spaces formation
2) Atrophy and Resorption Theory: Cell death/resorption → intertrabecular space formation
Development of the Anterior Chamber
What is the TM? Describe its development.
→ triangular mass of mesenchymal cells
Month 4: becomes more organized
Month 9: trabecular beams and pores are well developed
spaces & pores formed by programmed cell death
Development of the Anterior Chamber
What is Schlemm’s canal derived from? Describe its development.
→ Derived from the deep scleral plexus
4th month: TJ appear in the canal’s endothelial lining
7th month: Canal is fully formed in some quadrants
8th month: Giant vacuoles appear in the endothelium
9th month: Complete circular canal (Schlemm’s canal) is formed
Development of the Anterior Chamber
How does the endothelial lining of the anterior chamber change during development, and what effect does this have on aqueous outflow?
Anterior chamber is lined by a continuous endothelium covering the TM & iridocorneal angle
Month 7: Endothelial membrane is continuous → no aq outflow
Month 9: Endothelial membrane is discontinuous → allows aq outflow
Development of the Vitreous
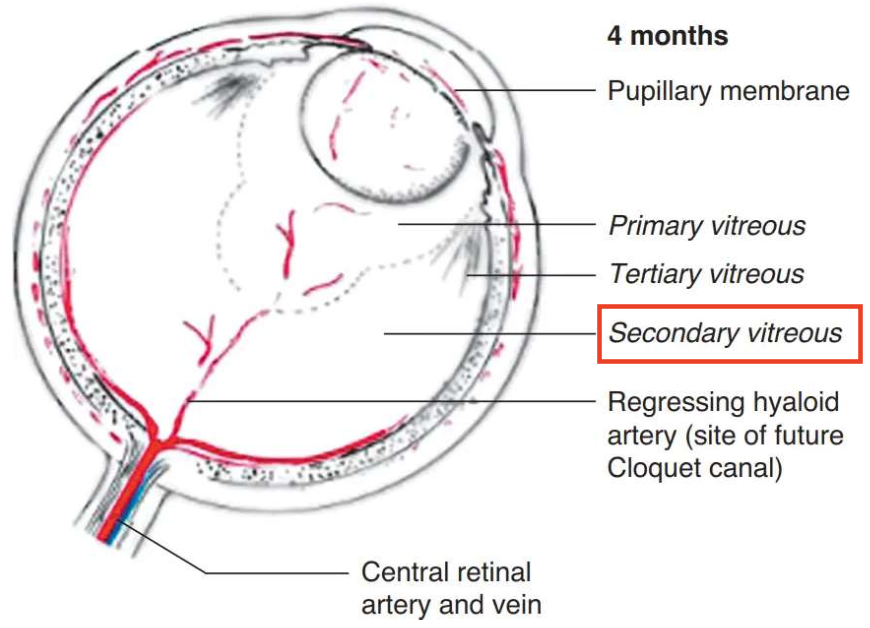
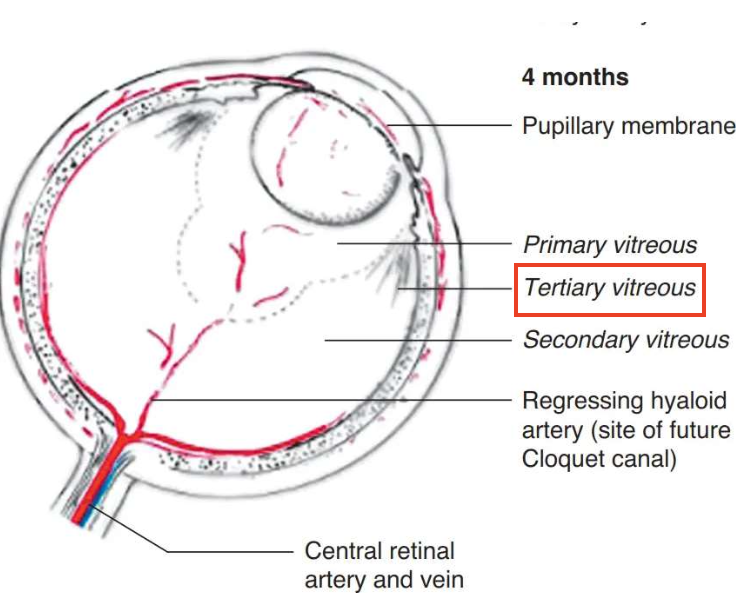
What is the origin and composition of the Primary Vitreous?
Origin: mesenchymal and ectodermal tissue
Composition: Fibrils (from lens and retina) & components from degenerating hyaloid system
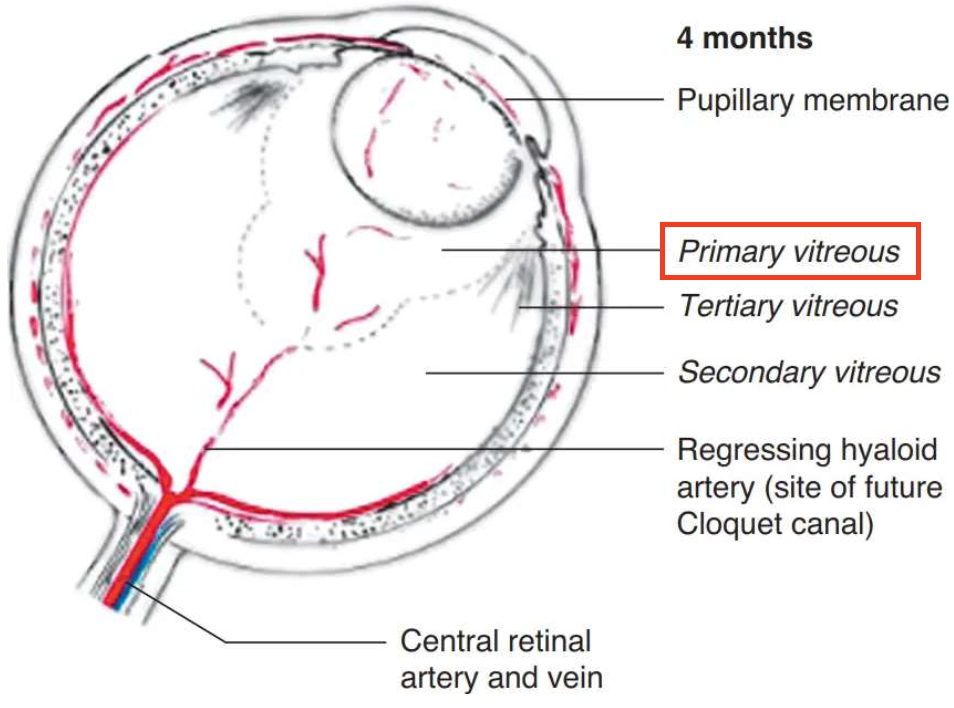
Development of the Vitreous
Describe the Secondary Vitreous.
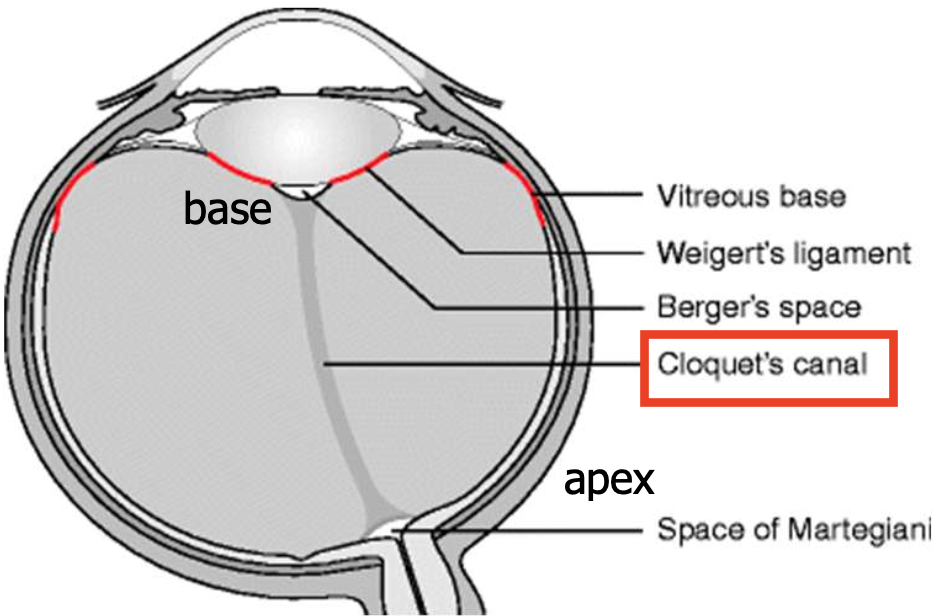
→ made by the neural retina and hyalocytes from the 1er vitreous
has a fibril network and primitive hyalocytes
encloses the 1er vitreous within the atrophying hyaloid vessels → forms the funnel-shaped Cloquet’s canal
Apex - faces optic disc
Base - faces posterior lens
Fully formed by Month 4 and remains in adults
Development of the Vitreous
Describe the Tertiary Vitreous.
Condensed fibrils of the 2er vitreous (anterior to the marginal bundle of Druault) elongate → lens zonules/suspensory ligament of the lens (aka 3er vitreous)
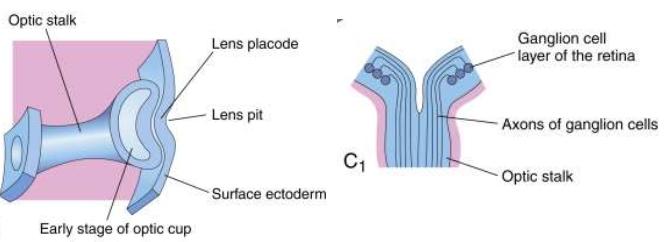
Development of the Optic Nerve
Describe the Optic nerve development.
Optic stalk connects the optic vesicle to the forebrain
Outer stalk layer → forms neuroglial sheath surrounding the nerve
Inner layer → glial cells (oligodendrocytes, astrocytes) & lamina cribrosa components
apoptosis of the cells in inner layer → space for RGC axons to enter the stalk
Development of the Optic Nerve
Describe the further maturation that occurs in Optic nerve development.
Months 2 - 8: Axon ↓50% due to apoptosis
allows glial & CT to enter optic nerve
RGC axons fill the optic nerve lumen and grow toward the LGN
Month 5: Myelination begins
Month 6: Myelination continues to the optic chiasm & reaches the lamina cribrosa 1–3 months after birth
What is Bergmeister’s Papilla?
Glial tissue that remains on the optic nerve head
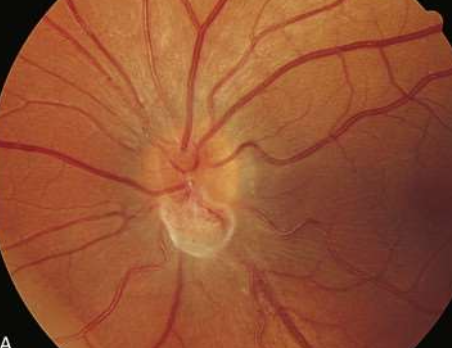
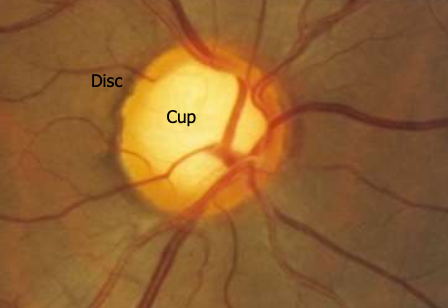
What is Physiological Cupping?
Congenital disorder caused by:
scleral optic canal
glial atrophy of Bergmeister’s papilla
- ↑ cupping = ↑ atrophy
Development of Ocular Adnexa
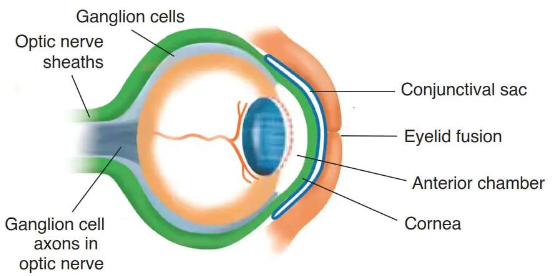
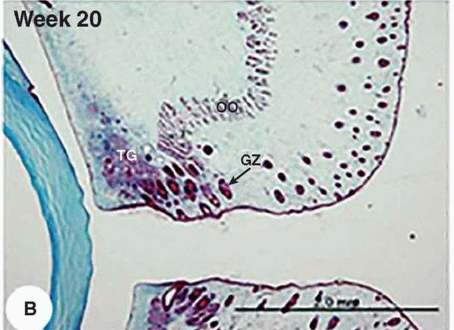
Describe how the Eyelid develops.
Month 2: Folds of surface ectoderm grow towards eachother over the cornea
Month 3: Folds meet & fuse (stay fused)
- Tarsal plates = 1st visible structures
Epithelial buds from the eyelid margins grow into the tarsal plates → form Meibomian glands
Month 4: Zeis and Moll glands develop
- Mesenchyme → Tarsal plates, orbicularis, levator & Müller’s muscle
Development of Ocular Adnexa
Why do the eyes stay fused during development?
Protects eye from amniotic fluid
Prevents keratinization/hardening of cornea & conjunctiva
Development of Ocular Adnexa
What “opens” the fused eyelids?
During 5th-6th month:
Desmosomes at lid margins break down → eyelid separation
Development of Ocular Adnexa
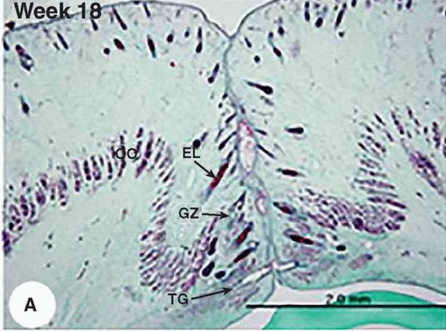
Describe the development of Conjunctiva.
Weeks 9-10: Conjunctiva differentiates within the lid margins after lid fusion
- Nonkeratinized epithelium lines the inner eyelid surface
Palpebral conjunctiva: lines under the lid
Bulbar conjunctiva: joins the corneal epithelium
Weeks 10-11: Unicellular goblet cells appear
Development of Ocular Adnexa
How do Accessory lacrimal glands form?
via inward budding from the palpebral conjunctival epithelium
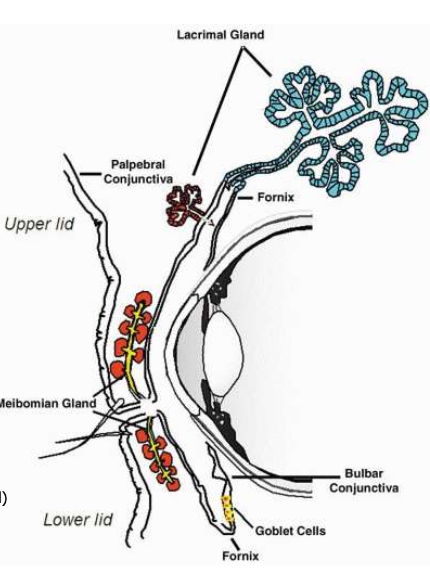
Development of Orbit
Where do Orbital bones originate from?
→ derived from cranial neural crest cells
these cells migrate into the head, surround the developing eye, and form:
Frontonasal process → forms Lacrimal + Ethmoid bones
Maxillary processes → forms Lateral wall and floor
Development of Orbit
What processes allows for the formation of the Orbital bones?
Most orbital bones form via intramembranous ossification
Exception: Sphenoid & Ethmoid bones (endochondral ossification)
Development of Orbit
What is the timeline of the ossification process of Orbital bones?
6th week: Ethmoid is the 1st bone to ossify
3rd month: All bones begin to ossify
6th–7th month: All bones finish ossification
Development of EOMs
Where do EOMs originate from?
Origin: Head mesoderm
Myoblasts migrate around the developing eye → differentiate into striated muscle fibers
Development of EOMs
What is EOM formation influenced by?
→ interactions w/ mesenchymal condensations
3 condensations on each side of head:
1 Pre-mandibular
2 Maxillomandibular
Development of EOMs
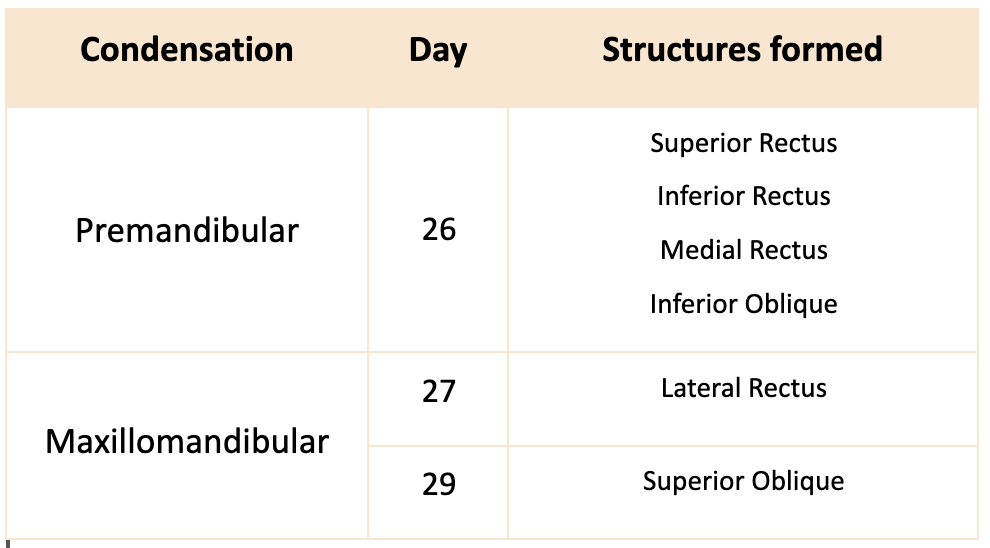
Make a chart on the EOMs derived from the Pre-mandibular & Maxillomandibular condensations.
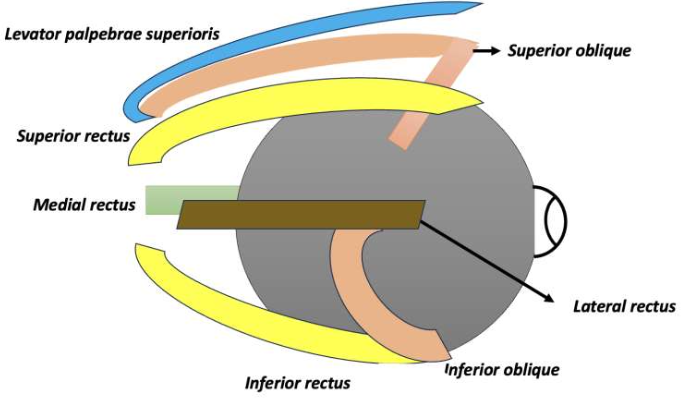
Development of EOMs
When does the EOM tendon attach to the globe?
Mid-3rd month
where they then fuse to sclera near equator
Development of EOMs
How does Tenon's capsule form?
via condensation around eyeball
Development of EOMs
When are Tendinous sheaths formed by?
~18 months
Development of the Nasolacrimal System
Describe the timeline of the Nasolacrimal system formation.
Week 5: Ectoderm invaginates b/w the lateral nasal process & maxillary process
these 2 processes fuse along the nasolacrimal groove
Surface ectoderm folds in and closes off → forming a “cord” that gets buried under the skin
Week 6: Cord extends from medial canthus to nasal cavity → differentiates into nasolacrimal system components
Week 12: Cannalization - Cord proliferates toward:
Medial canthus
Inferior medial nasal cavity
By 7 months: Canalization almost complete
Puncta perforation usually occurs before birth
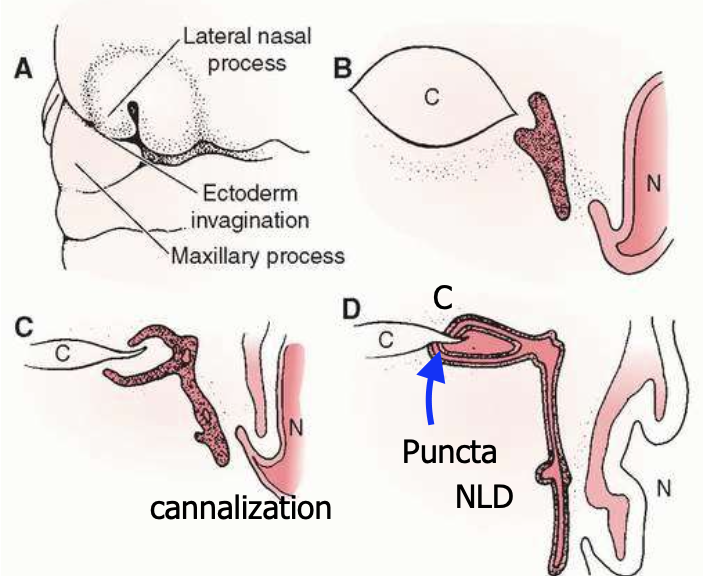
Development of the Nasolacrimal System
During the cord proliferation/cannalization, what structures become recognizable?
Canaliculi
Lacrimal sac
Lumen began to form in lacrimal sac
Nasolacrimal duct
Development of the Nasolacrimal System
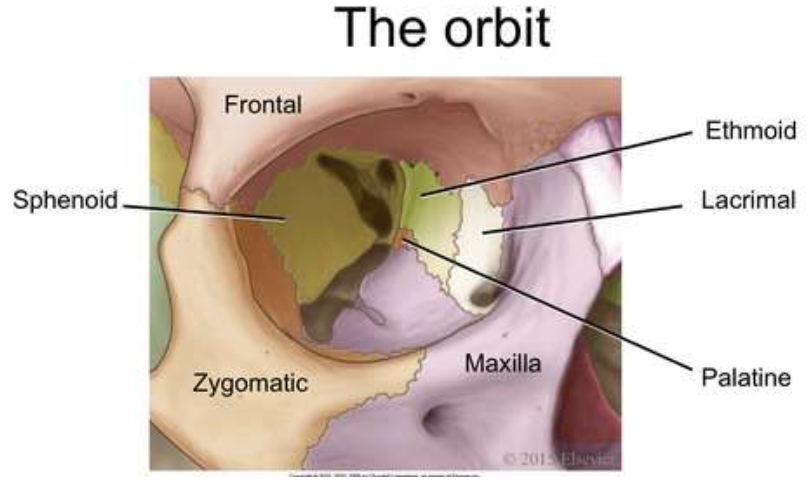
Describe how the Lacrimal gland develops. When is it fully developed?
→ Develops from epithelial buds from conjunctiva of superior fornix
Continues developing after birth
possible origin = neural crest
Full development: ~3–4 years old
What is Dacryostenosis?
blocked tear duct due to incomplete canalization of nasolacrimal duct
Symptoms: epiphora or watery eyes

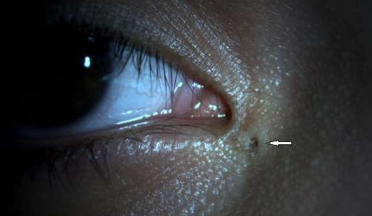
What is Congenital Lacrimal Fistula?
→ Small opening near the inner corner of the eye
caused by an epithelial tract connecting the skin to the canaliculi, lacrimal sac or nasolacrimal duct
instead of canaliculi to tear duct
Symptoms: Asymptomatic or epiphora, watery eyes
What is Punctal Atresia?
→ puncta is closed/absent
caused by genetics
Symptoms: epiphora → tears overflow

Development of Blood Vessel Permeability and Barriers
Where is the Blood-Aqueous Barrier found?
Iris & ciliary body
Development of Blood Vessel Permeability and Barriers
What forms the Inner Blood-Retinal Barrier?
→ formed by retinal capillary endothelial cells with TJ
Supported by Müller cells & pericytes
-Nourishes Inner retina
Development of Blood Vessel Permeability and Barriers
What forms the Outer Blood-Retinal Barrier?
→ Formed by RPE cells
TJ separate retina from choroid
-Nourishes Outer retina
Development of Blood Vessel Permeability and Barriers
Blood-Retinal and Blood-Aqueous Barriers are recognized early in development in the TJ formed in the:
RPE
Non-pigmented ciliary epithelium
Capillaries of the iris and retina
Development of Blood Vessel Permeability and Barriers
What are fenestrations and their role in blood vessel permeability?
Establish vessel permeability in:
Capillaries of ciliary processes
Choriocapillaris
appear early in the gestational period
Function: Allow nutrients to leak through & nourish tissues
What is Iris Coloboma?
→ embryonic fissure fails to close during 5th WG → "keyhole-shaped" pupil
rest of the iris develops normally
can be associated with colobomas of the ciliary body, choroid, retina, or optic nerve

What is Retinal Coloboma?
→ Colobomas affect the retina (sensory & RPE) also involves the choroid b/c its differentiation depends on an intact RPE layer
can result in → vision loss in specific visual fields, low vision
common complications = Retinal detachment & cataract
What causes congenital cataracts during lens development?
1er fiber defect: Failure of proper elongation & alignment → cataract of 1er fibers
2er fiber defect: Interference → sutural cataracts
Viral cause: Maternal rubella infection (4th–7th week) → affects lens
cataract may be present at birth or appear later (virus can persist up to 3 years)

What causes Ocular albinism?
→ occurs due to gene-related defects in melanin production, affecting one or both types of melanocytes
Melanin from the RPE influences normal sensory retina development
without it, many retinal abnormalities occur at birth

What retinal abnormalities are seen in ocular albinism?
Underdeveloped macula
No fovea
↓ rods
Abnormal optic nerve projection LGN (results in binocular issues)
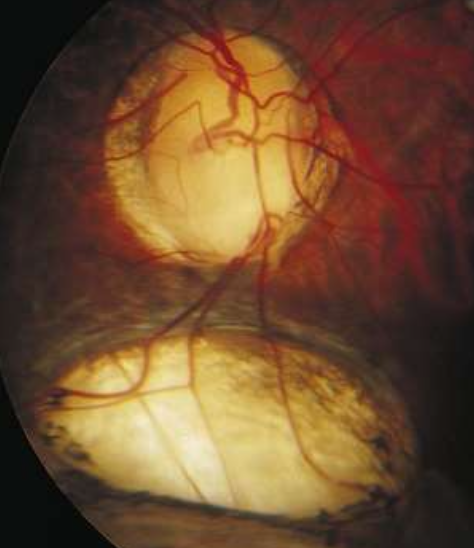
What causes Retinopathy of Prematurity (ROP)?
Premature infants exposed to high O2: develop vasoconstriction of immature retinal vessels → vessels fail to develop
After O2 removal: Vasoproliferation occurs → new vessels form which are leaky with poorly formed endothelial TJ
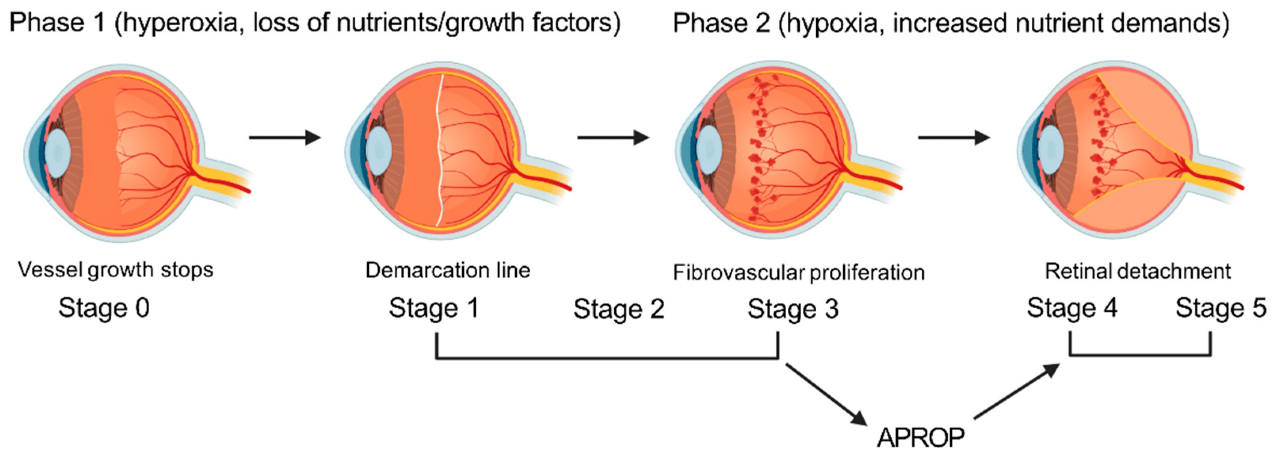
What are the 2 Phases of Retinopathy of Prematurity (ROP)?
Phase 1: Hyperoxia → loss of nutrients/growth factors → vessel growth stops → (Stage 1–2)
Phase 2: Hypoxia → ↑ nutrient demand → fibrovascular proliferation (Stage 3) → retinal detachment (Stages 4–5)
List the serious complications of ROP.
Neovascular invasion of vitreous (vessels grow toward vitreous)
Vitreoretinal adhesions
Vitreoretinal hemorrhage
retinal detachment