Trauma and ED Organisation (NHS)
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
14 Terms
List some current issues in Emergency Medicine
Waiting times are far too long (significant number of people waiting 4+ hrs)
Staff shortages
Staff burnout and dissatisfaction
Ambulance waiting times
No space in hospitals for the volume of patients
Overloading of other services (eg. General Practice and Social Care) means more patients are presenting straight to the ED
Name a few major changes that have been made to prevent people presenting to the ED in the last few decades.
Seatbelts, safer cars and road design (eg. speed limits)
Gun control
Knife crime units
New vaccines
Prevention
Why was there a major shake up in the organisation and management of EDs in the 2010s?
Trauma Audit & Research Network (TARN) was set up in the 1980s, and started producing reports.
Mortality rates in the UK due to trauma were worse compared to other similar countries (primarily the USA).
There was massive variation in performance between different hospitals.
Different hospitals also had very different specialists and equipment leading to patients being transferred back and forth.
The time between the injury and the patient getting to hospital was increasing steadily through the 90s.
Although TARN reports had led to improved quality of trauma care, it was still deemed insufficient by NCEPOD (National Confidential Enquiry into
Patient Outcome and Death) in 2007 - ‘Trauma - Who Cares?’
This report found that less than half of patients received good care, and many patients were being taken to hospitals that did not have adequate resources.
What major changes were made to trauma organisation in the UK in the 2010s?
Trauma Networks were set up, developed by healthcare staff:
Establishment of major trauma centres (MTC) in regions across the UK.
This centralised resources and staff, allowing 24 hr consultant led care.
Smaller trauma units (eg. minor injuries) were set up in the other hospitals to provide care for minor trauma or emergency care before a patient could be safely transferred to a MTC
Major trauma centre definition
Specialists hospitals responsible for the care of patients with major trauma across a region. They have all the equipment and specialist staff needed in one department.
Scottish Trauma Network
The Scottish Trauma Network (STN) is a bespoke, inclusive and equitable solution, which involves the Scottish Ambulance Service (SAS) and hospitals across Scotland – including 4 major trauma centres – working collaboratively to deliver high quality, integrated, multi-specialty care to severely injured patients. Multiple teams across Scotland (STAG, mountain rescues, health boards etc.) have meetings, develop tools and learning resources etc. Phased in in 2018.
Trauma stats (Scottish Trauma Network)
4th leading cause of death in Western countries
Leading cause of death in people under 40 years old
Each year in Scotland, around 4,000 people are seriously injured, with around 800-1,000 cases being defined as ‘major trauma’.
Major Trauma Triage Tool
Tool designed in Scotland and rolled out in 2021
Used to identify which patients are most likely to benefit from being taken directly to an MTC even if it means bypassing closer hospitals
Adult and paediatric versions
45 min cutoff where patients this far away from a MTC are taken to the nearest TU, even if there are major injuries
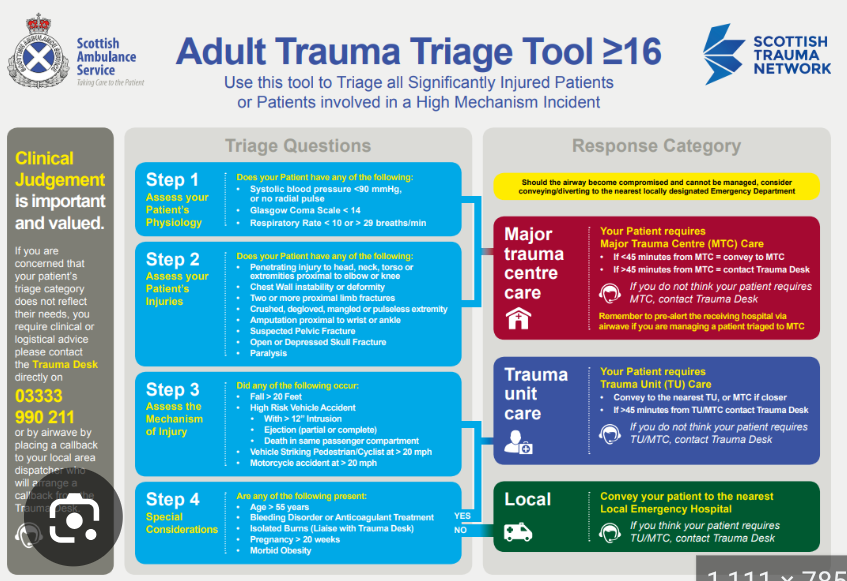
Trauma Desk
Offer peer support to ambulance crews about difficult decisions, and can provide red and yellow assets (specialist resources and teams) or aeromedical transport.
STAG
Scottish Trauma Audit Group
What does STAG do?
Recommenced in 2011 after being active between 1192 and 2002
aims to help severely injured patients to have better:
quality of care
overall experience
long-term outcomes
Collects data from all Scottish hospitals on trauma patients
Example of STAG improving care
University Hospital Wishaw was identified as an outlier for mortality between 2022 and 2023. STAG identified 3 key areas where care needed improvement (rib fractures, frailty and…) and then provided additional training for staff. This significantly reduced mortality in these areas, and the most recent data shows the hospital is no longer an outlier.
SNAP
Scottish National Audit Programme
What does SNAP do?
Part of Public Health Scotland - collects health data and to identify areas for improvement, sharing learning, and promoting development of healthcare.