Digestive System: Colon, Accessory Organs, and Pathology
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
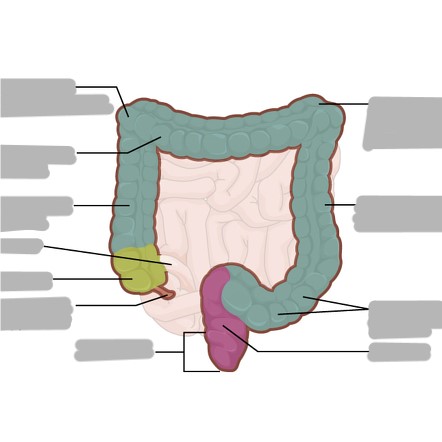
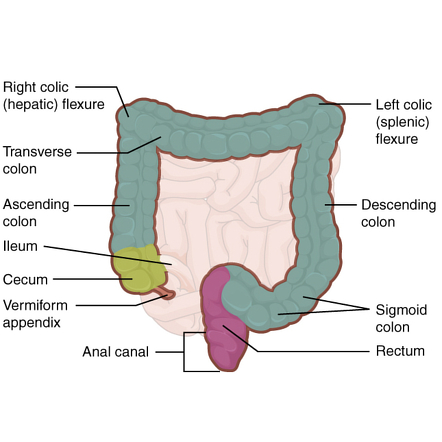
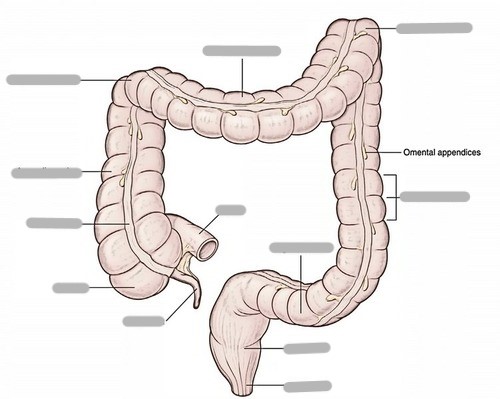
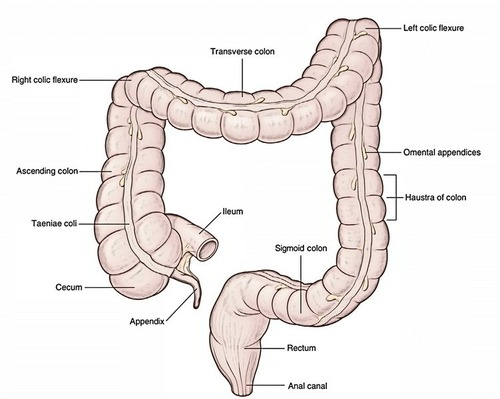
Explain the length and location of the large intestine (colon)
~5 ft long; begins at the ileocecal valve (RLQ) and surrounds the small intestine
What is a by product of the bacterial fermentation in the GI system?
flatulence (CO2 and methane produced)
What % of absorption takes place in the colon?
80% of water absorption
What are taeniae coli?
longitudinal muscles that aid in pushing the waste bolus into the rectum for excretion
What are haustra?
lumps in the large intestine
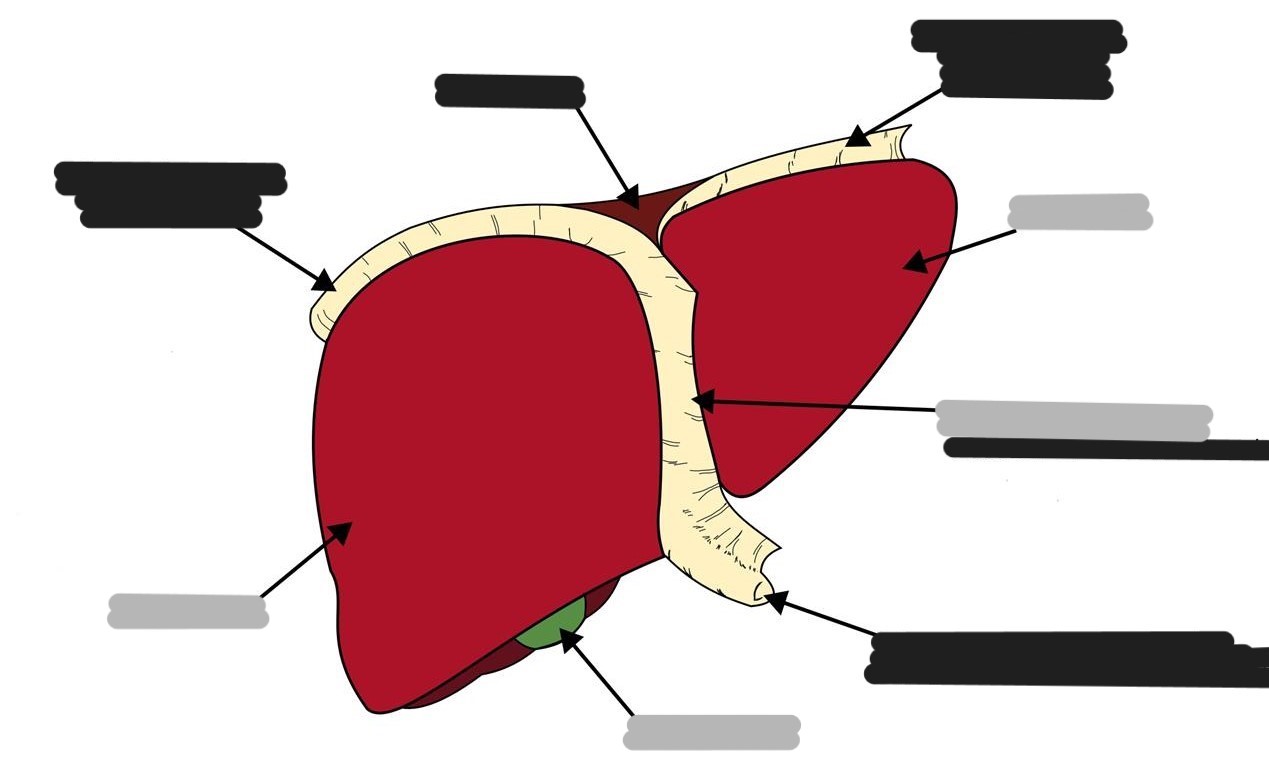
Where is the liver located?
RUQ
What is the part of the liver that separates it into the 2 lobes called?
falciform ligament
What is the main digestive function of the liver?
production of bile
What is the function of bile? What is it made up of?
breaks down fats; made up of water, salts, bilirubin, and cholesterol
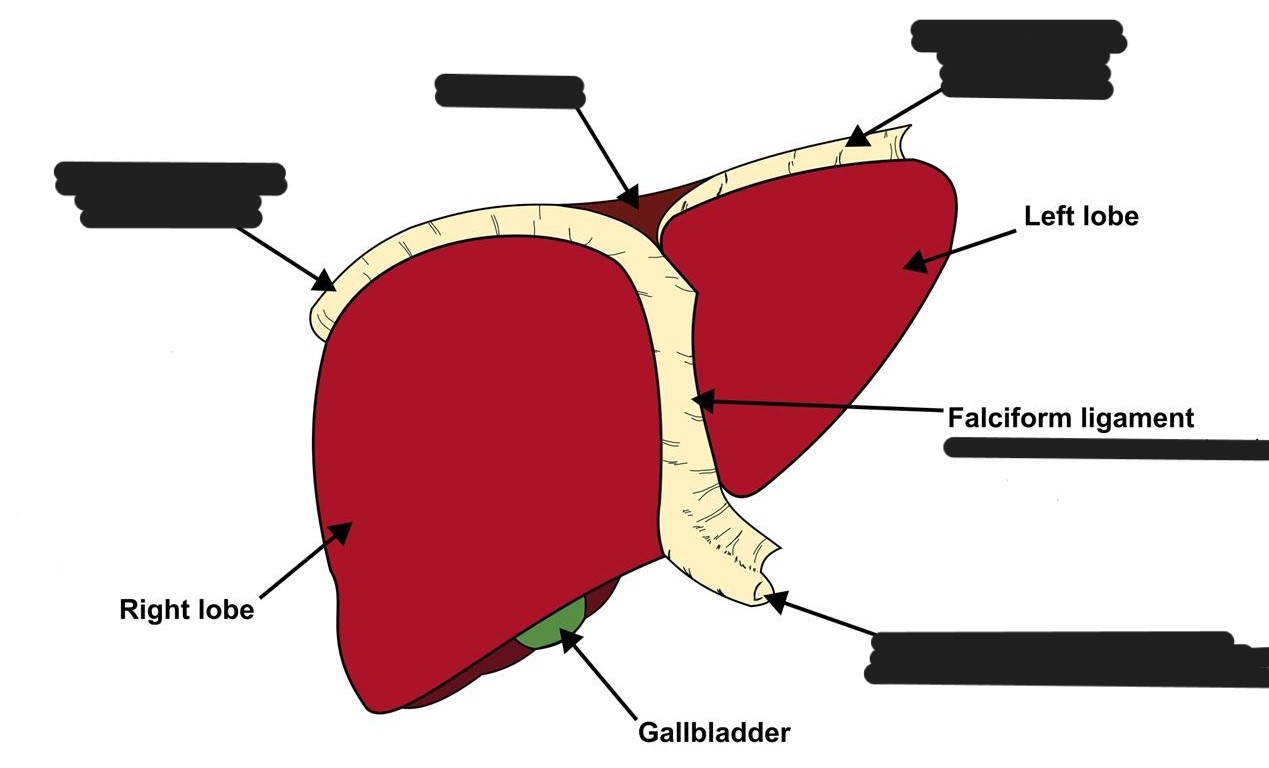
What is the function of the gallbladder?
stores, secretes, and concentrates (absorbs 90% of water) bile
Explain what happens with bile after a fatty meal
cholecystokinin is secreted by cells in the duodenum that stimulates gallbladder to contract
bile is then secreted
What are Kupfer cells?
macrophage cells involved in the destruction of bacteria and other harmful organisms that lie on the lining of the liver (kill pathogens coming from the bowel to the liver)
Explain the endocrine and exocrine functions of the pancreas
endocrine
ductless
secretes insulin directly into the bloodstream to control sugar levels
exocrine (digestive function)
ducts
secretes pancreatic juice/enzymes
contains enzymes that digest food
neutralizes HCl acid from the stomach
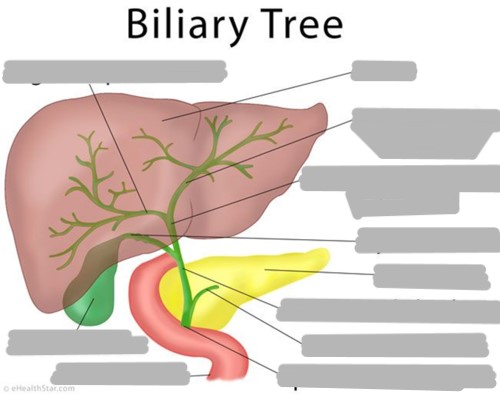
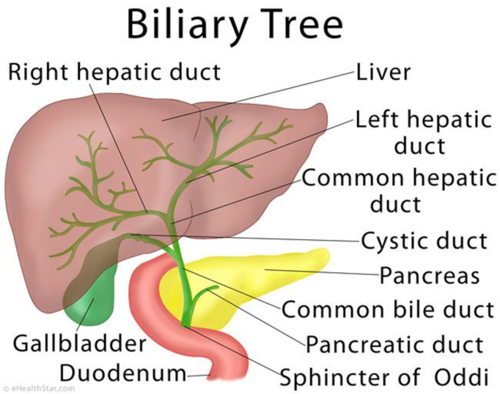
The right and left hepatic ducts join together to form the ___
common hepatic duct
The gallbladder drains into the ___
cystic duct
The cystic duct and the common hepatic join together to form the ___
common bile duct
Before exiting into the duodenum, the common bile duct joins to the ___
pancreatic duct
The common bile duct and pancreatic duct eventually go through the ___ and ___
ampulla of Vater (hepatopancreatic duct) and sphincter of Oddi
Explain Barrett’s esophagus
occurs when the cells in the esophagus begin to change due to chronic exposure to acid
from reflux
precancerous disease
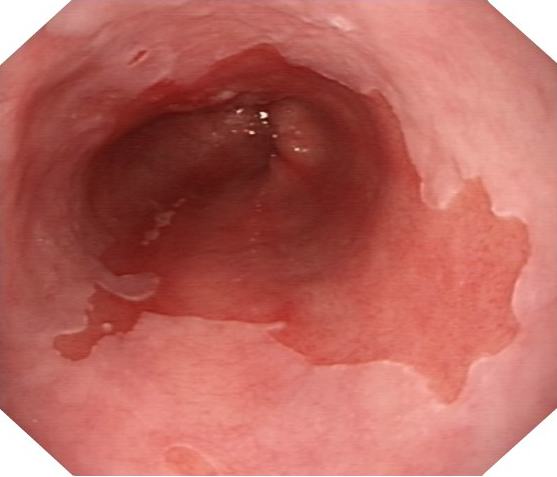
What pathology is shown here?
Barrett’s esophagus
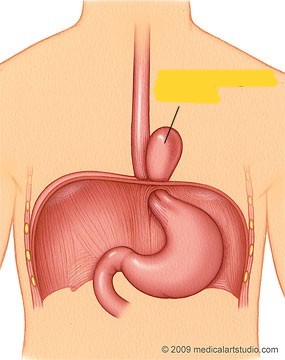
Explain Zenker’s diverticulum
occurs mostly in the elderly
excessive pressure within the lower pharynx, causing the weakest portion of the pharyngeal wall to balloon out, forming a diverticulum
results in dysphagia, cough, halitosis

What pathology is shown here?
Zenker’s diverticulum
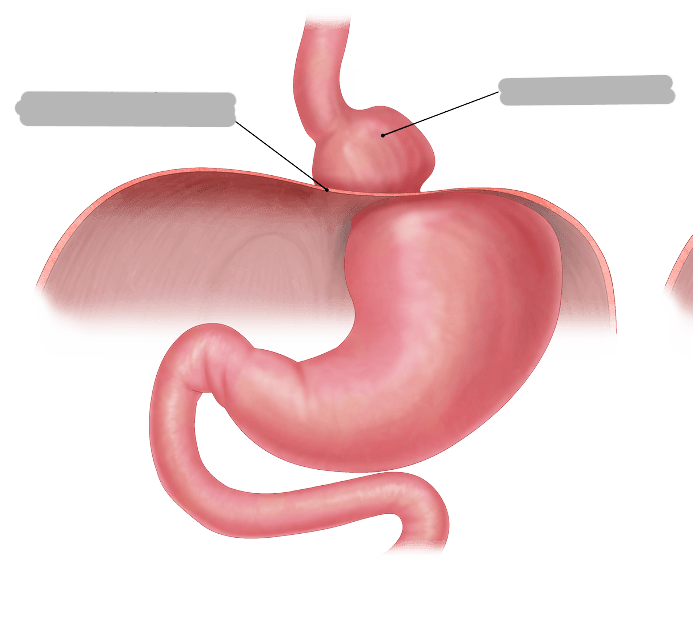
Explain paraesophageal hiatal hernia
hernias in which the GE junction stays where it belongs, but part of the stomach bulges into the chest beside the esophagus
1% of hiatal hernias
causes ischemia (impeded blood supply)
caused by muscle weakness, obesity, pregnancy, trauma
Explain sliding hiatal hernia
stomach and the GE junction slide up into the chest through the hiatus
99% of hiatal hernias
caused by muscle weakness, obesity, pregnancy, trauma
What pathology is shown here?
paraesophageal hiatal hernia
What pathology is shown here?
sliding hiatal hernia
Explain duodenal and gastric ulcers
“peptic ulcers”
open sore of mucosa
caused by infection, inflammation, or substance (tobacco, coffee, aspirin, NSAIDs) which erodes mucosa
Explain duodenal atresia
“closing off” of the duodenum
congenital disease where the duodenum has not developed properly
not open and cannot allow the passage of stomach contents
atresia is usually just distal to ampulla of Vater
about 30% of children with duodenal atresia will have down syndrome
double bubble sign
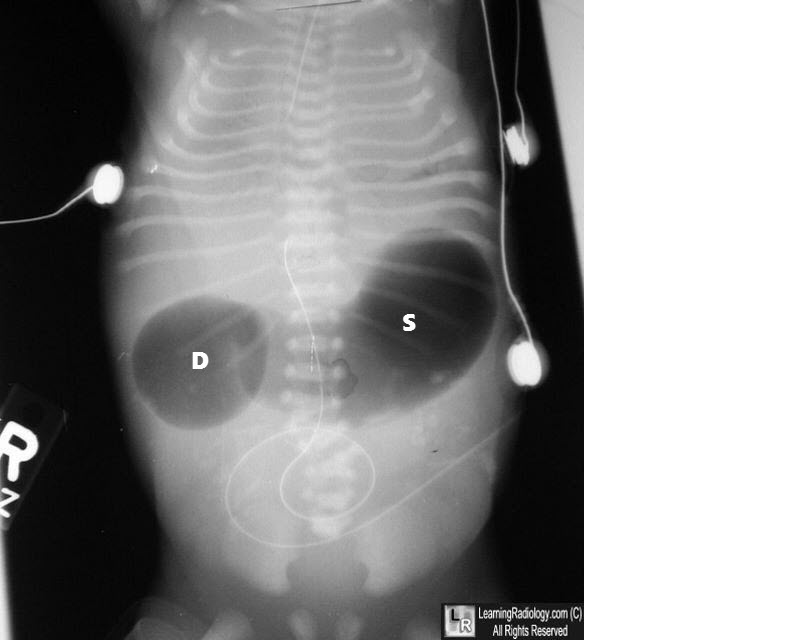
What pathology is shown here?
duodenal atresia
Explain esophageal varices
increased pressure in liver causes varicose veins in esophagus
pressure due to deteriorated function of liver, often from cirrhosis
scar tissue forms, interfering with liver function
radiographic image demonstrates filling defects
wormlike or cobblestone appearance
bleeding is a major complication

What pathology is shown here?
esophageal varices
Explain small bowel obstruction
the most common cause is adhesions secondary to abdominal surgery
radiographically dilated loops of bowel and air fluid levels
paralytic
adynamic bowel obstruction due to paralyzed bowel muscles
mechanical
dynamic bowel obstruction arising from a mechanical cause/foreign body
What are the two types of mechanical ileus?
volvulus: coffee bean sign, twisting upon itself
intussusception: crescent sign, collapsing upon itself

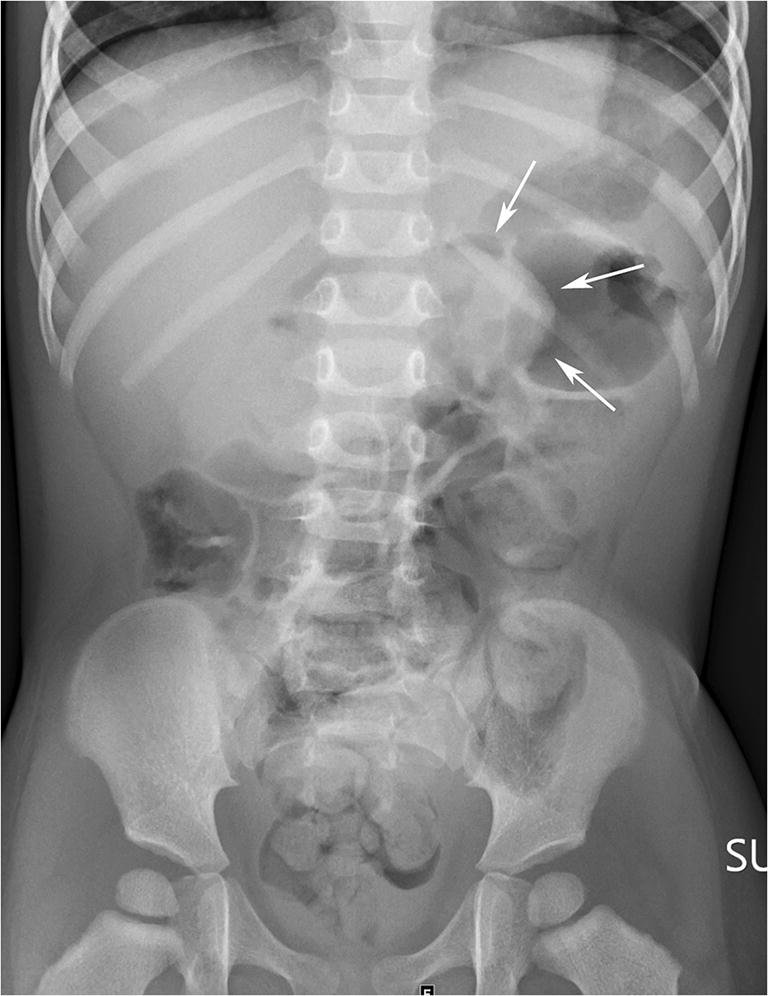
What pathology is shown here?
volvulus
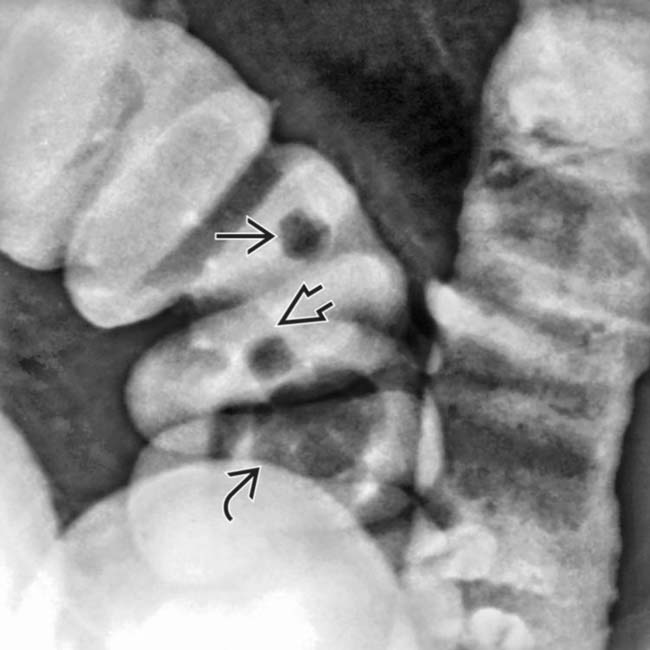
What pathology is shown here?
intussusception
Explain pyloric stenosis
hypertrophy and hyperplasia of muscle in the pyloric canal
most common in newborns
causes projectile vomiting, not tolerating food, continuous crying
“string” sign

What pathology is shown here?
pyloric stenosis
Explain colon polyps
growth on the inside lining
more common as people age
can become cancerous
routine screenings after age 50
Explain colon diverticula
outpouchings on the intestinal wall
most common area is sigmoid colon due to increased pressure
What pathology is shown here?
colon polyps
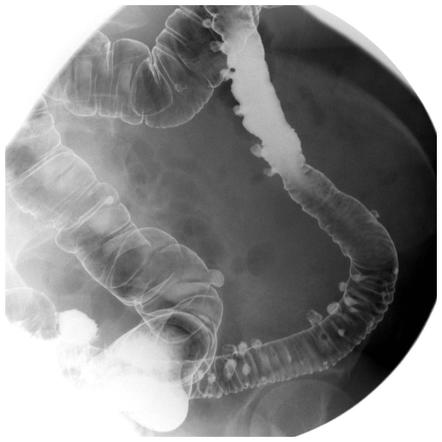
What pathology is shown here?
diverticula
Explain colorectal carcinoma
constriction of the lumen of the colon
most commonly at the rectum
apple core sign

What pathology is shown here?
colorectal carcinoma
Explain cirrhosis
healthy liver tissue is replaced with scar tissue
prevents liver from functioning properly
scar tissue blocks the flow of blood
causes jaundice, increased liver pressure, esophageal varices
caused by alcoholism, hep C, hep B
What pathology is shown here?
cirrhosis (of the liver)
What are the 3 types of gastric bypass surgery?
Roux-en-Y gastric bypass
sleeve gastrectomy
laparoscopic gastric banding
Explain the Roux-en-Y gastric bypass surgery
small stomach pouch
jejunum is cut and attached to new pouch, bypassing the duodenum
the portion of the intestine still attached to the main stomach is reattached farther down (allows digestive juices to flow)
limits amount of food eaten: REDUCES ABSORPTION OF CALORIES AND NUTRIENTS
What is the most invasive of the gastric bypass surgeries?
Roux-en-Y
Explain the sleeve gastrectomy gastric bypass surgery
part of the stomach is separated and removed from the body
the remaining section of the stomach is formed into a tubelike structure
smaller stomach cannot hold as much food, but DOES NOT AFFECT ABSORPTION OF CALORIES AND NUTRIENTS
Explain the laparoscopic banding gastric bypass surgery
a band containing an inflatable balloon is placed around upper stomach
adjustable, non-permanent port is placed under skin
restricts amount of food eaten, but DOES NOT AFFECT ABSORPTION OF CALORIES AND NUTRIENTS
What is the least invasive of the gastric bypass surgeries?
laparoscopic banding
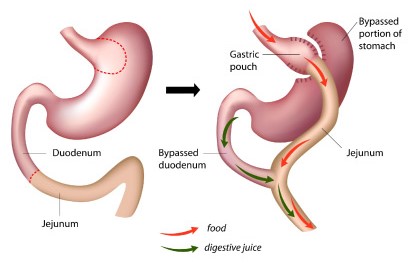
Which type of gastric bypass is shown?
Roux-en-Y
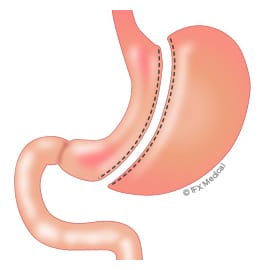
Which type of gastric bypass is shown?
sleeve gastrectomy
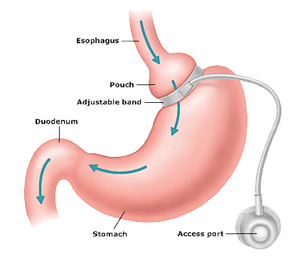
Which type of gastric bypass is shown?
laparoscopic banding