1751 Digestive System Exams Upper
1/79
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
80 Terms
How is the Alimentary Canal imaged?
Fluoroscopy or a combination of fluoroscopy and radiography
Fluoroscopy makes it possible to what?
Observe the canal in motion and determine the subsequent procedures for a complete examination
What is the radiographer’s role in fluoro
To assist the patient before and after contrast administration while assisting the radiologist during the procedure. If images are required after fluoroscopy the radiograph will acquire these also
Why is contrast media necessary for visualization of the alimentary canal?
Because it doesn’t have sufficient density to be seen through surrounding structures
Radiolucent - Negative contrast
Air, gas producing tablets crystals or carbon dioxide (soda water)
Anatomic area fill with negative contrast appears dark/black on image
Radiopaque - Positive Contrast
Elements with higher atomic number Ex. Barium
Anatomic area fill with this contrast appears light/white on image
Negative + Positive contrast = double contrast
Common Double Contrast studies
Stomach - Barium sulfate + carbon dioxide (crystals)
Small intestine (SBFT) Barium sulfate + methylcellulose (laxative that produces gas)
Large intestine - Barium sulfate + air
Enteroclysis (small intestine) Barium sulfate + Air
Definition of enteroclysis
An exam of the small intestines that is much more invasive than the SBFT and is reserved for certain pathologies. A tube is placed down the patient’s throat to the end of the duodenum and barium is injected. Air may also be injected for a double contrast exam
What does ROCM stand for
Radiopaque Contrast Media
What is ROCM
High-density pharmacologic agents used to visualize low-contrast tissues in the body
Common tissues visualized with ROCM
Vasculature
Kidneys
Gastrointestinal (GI) Tract
Biliary Tree
2 most commonly prescribed ROCM
Water Insoluble - Non-Iondinated
Water Soluble - Iondinated
Barium atomic #
56
Iodine atomic #
53
Barium Sulfate chemical abbreviation
BaSO4
Barium Sulfate Facts
Water insoluble - salt of the metallic element barium
Most commonly used
Dry powder, paste, or liquid
Powdered barium has different concentrations and is mixed with plain water (Concentration depends on the part to be examined and the radiologist)
Possible Barium Complications
Patient rarely have allergic reactions to barium sulfate. They may react to the preservatives or additives, but not the barium itself
Complications are rare as long as barium sulfate remains in the GI tract
If barium is retained in the large bowel for a prolonged period of time “impaction” may occur
It may form a mass which occludes the lumen of bowel causing constipation or complete obstruction
Patients at risk of impaction are inactive geriatric patients, dehydrated or neonatal patients
Encourage patient to drink plenty of fluids following procedure and doctor may prescribe a laxative
Barium complications 2
Aspiration may be a problem if the patient experiences nausea and vomiting following ingestion of barium
Aspiration of large amounts of barium may lead to pneumonia
Most barium can be cleared by coughing
Safer to aspirate barium than gastrografin/omnipaque
Barium complications 3
Peritonitis (inflammation of the peritoneum) may occur when barium spills into the abdomen from perforations or tears
Most rectal perforations are due to barium tip insertion or over-inflation of the balloon
The body cannot absorb barium outside GI tract
Free barium is mostly inert (chemically inactive) but the dyes, flavoring may cause inflammation
Bacteria and partially digested food matter will also be dumped into the peritoneum with the barium
50% morality rate from peritoneal barium spills
May be surgically removed or aspirated from the cavity
If perforation is suspected radiographer should use water-soluble iodine based contrast media
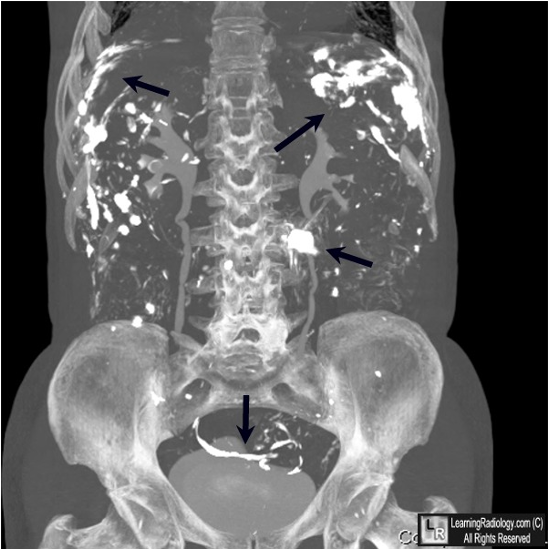
BE Perforation - Free barium in the peritoneal cavity
Speed with which the barium passes through the alimentary canal depends on
Suspending medium
Temperature of the medium
Motility function of the alimentary canal
Normal transit time to reach the ileocecal valve
2-3 hours
Barium reaches the rectum within
24 hours
Contraindication to using barium
Perforated viscus
Obstruction
Surgery following procedure
Water soluble - Iodination contrast media characteristics
Outlines esophagus but doesn’t adhere to mucosa as well as barium
Strong, bitter taste
Satisfactory exam of stomach and duodenum, but not clear detail for small intestine
Moves more quickly than barium suspensions
Easily removed by aspiration either before or during surgery
If escaped into peritoneum through perforation, no ill effects occur
Absorbed from peritoneal cavity and excreted by kidneys
If aspirated gastrografin is hypertonic enough to cause pulmonary edema
Taken orally for rapid large intestine exam if patient cannot receive enema
Contraindication: Pt allergic to iodine

Pulmonary edema due to aspiration of gastrografin
kVp for scout
85
kVp for barium
120
kVp for double contrast
90-100
kVp for water soluble
80-90
Post instructions for barium studies
Alert pt stool may be white for next few days. Barium being evacuated
Resume regular diet following exam, unless otherwise instructed
Drink plenty of fluid to wash out barium (if not may cause constipation)
If constipation occurs, contact dr. may suggest laxative
Fluoro Equipment
Image intensification systems connected to accessory units, such as cine film recorders, television systems, spot-film cameras, digital cameras, and video recorders
Remote control fluoro room can be controlled from adjacent room
Devices used for compression and palpation of abdomen
Compression cone on fluoro unit
Pneumatic compression paddle inflated to put pressure on abdomen
Radiologist hand - with leaded glove
Prep for digestive exams
Check orders (any other exams contrast would interfere with)
Footboard on table
Lead curtain on tower
Bucky tray moved down
Storage for exam
Input pt and dr info
Select data on control panel
Appropriate frames per second
Mix contrast and prepare supplies
Have shield for pt
Devices used for radiation protection
Leaded tower drape
Lead apron
Lead gloves
Bucky slot shield
Protective eyewear
Thyroid shield
Compression paddle
Clinical indications for modified barium swallow study
Oral and pharyngeal dysphagia
food sticking in oropharynx
laryngeal abnormalities
odynophagia (painful swallow)
CVA (Cerebrovascular accident, stroke)
Questionable aspiration
Recent recurrent pneumonia and right lower lobe infiltrates
Progressive neurological diseases
Modified Barium Swallow Study facts
Food tray - Various solid and liquid consistencies inpregnated with barium contrast
Performed by speech pathology and radiology
No prep
Evaluated the oral and pharyngeal stages of swallowing
Clinical indications for esophagram
Food sticking below the collarbone
Hiatal hernia
Zenkers diverticulum
Possible esophageal stricture
Possible esophageal dismotility
Questionable perforation
Possible mass
Reflux/laryngopharyngeal reflux
Screen for esophageal CA
Esophagram facts
Liquid barium
Radiology only
No prep
Evaluates entire esophagus
Are esophagrams performed single or double contrast
Can be single or double
What are carbon dioxide crystals
Effervescent granules, powder or tablets that release carbon dioxide on contact with stomach fluid. Causes gastric distention and smoothing of rugae. Similar to alka seltzer
What is commonly saturated with barium during esophagram
cotton or marshmallows
Is preliminary prep required for esophagram
no
What is valsalva maneuver
Patient takes in breath and is asked to bear down as if trying to move bowels
Why is the valsalva maneuver performed
To rule out hiatal hernia and reflux
What does patient have to remove for esophagram
Clothing from waist up and replace with a gown as well as eyeglasses necklaces and long earrings
What position would you begin an esophagram in
Patient and table erect with barium cup in left hand
What are the routine overhead images for esophagram
AP or PA
RAO or LPO
Right Lateral
AP/PA Esophagus (CR and Positioning)
Patient supine or prone with arms above head
Center the MSP to the grid
Turn head slightly, to assist drinking the barium
Shield Patient
Place IR at the top of the mouth
CR around T5-T6
Instruct patient to take big swallows and expose while esophagus is full of barium
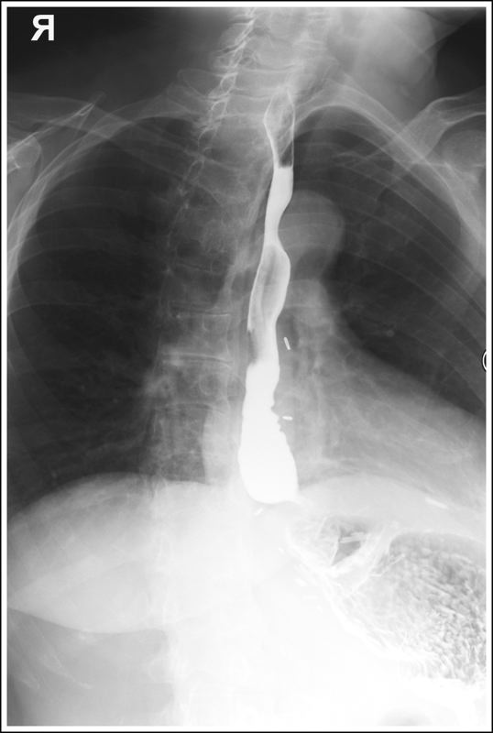
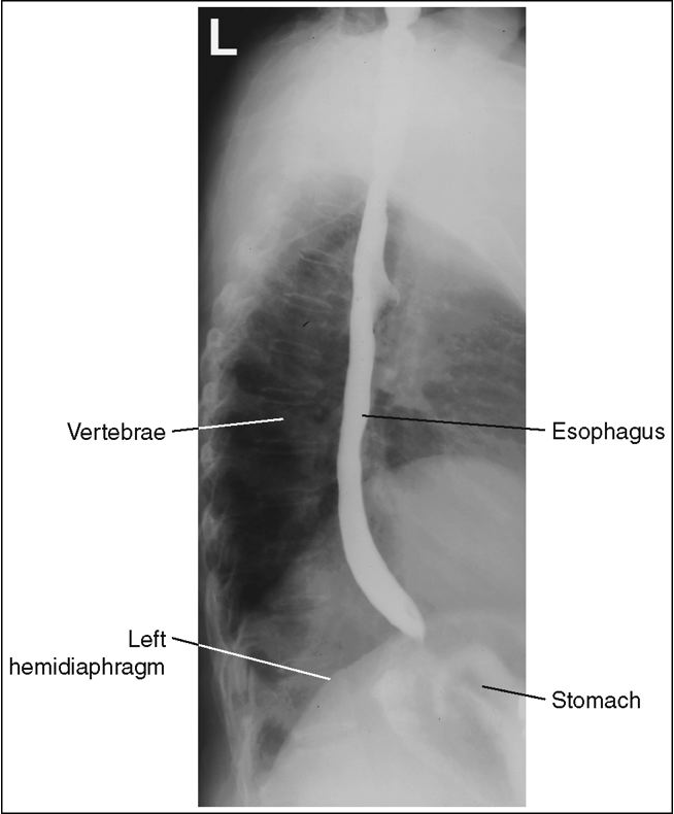
AP/PA Oblique (RAO or LPO) Esophagus (CR and Positioning)
Oblique patient 35 to 40 degrees. This obtains a wider space and unobstructed view of the esophagus between the vertebrae and the heart
RAO - Side down arm at the side and side up arm by the head
Shield patient
Place IR at the top of the mouth
CR - at the level of T5-T6 and 2 inches from the spine to the elevated side
Instruct patient ot take big swallows and expose while esophagus is full of barium
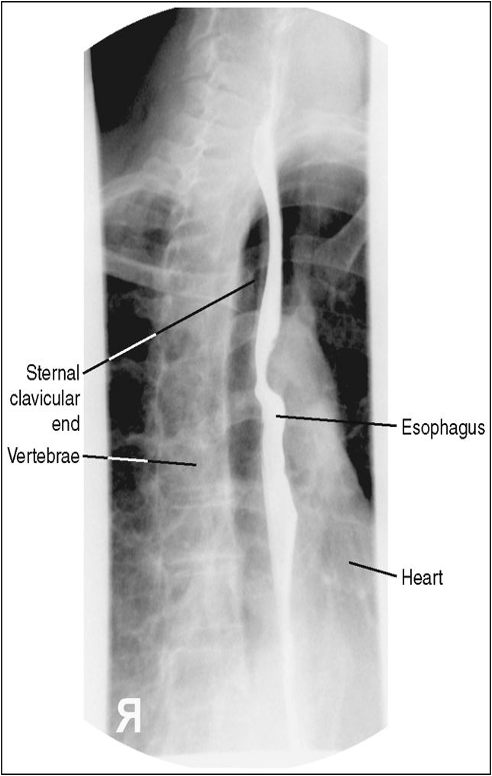
Lateral Esophagus (Right or Left (CR and Positioning)
Recumbent lateral position - preferably right lateral and facing radiographer
Arms forward
MCP centered
Shield patient
Place IR at the top of the mouth
CR at the level of T5-T6
Instruct patient to take big swallows and expose while esophagus is full of barium
Esophagram Eval Criteria (For all 3 positions)
Collimation
Esophagus from lower part of neck to the stomach entrance
Esophagus filled with barium
Penetration of the barium
AP or PA Esophagram Eval Criteria
No rotation of patient
Visualize esophagus through the superimposed thoracic vertabrae
AP or PA Oblique Esophagram Eval Criteria
Esophagus between the vertebrae and the heart
Lateral Esophagram Eval Criteria
Arm not interfering with esophagus
Ribs posterior to the vertebrae superimposed with no rotation
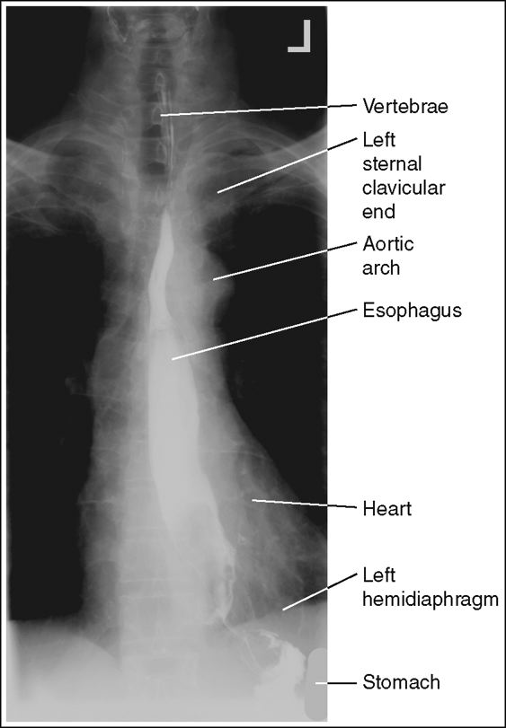
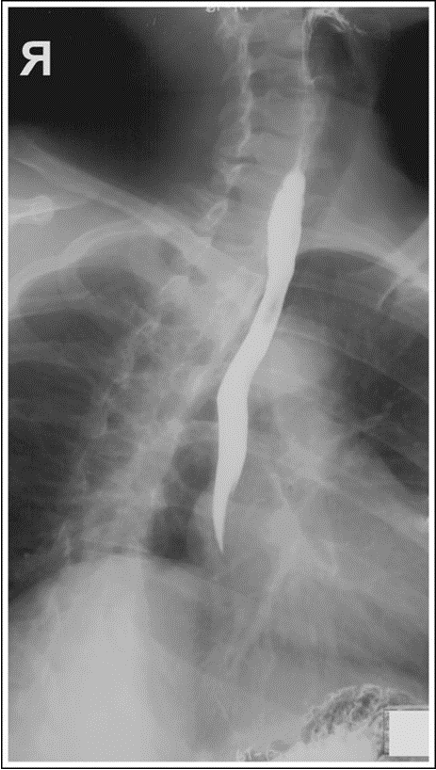
PA Esophagus with Proper positioning
PA Esophagus with Left shoulder rolled up
RAO Esophagus with proper positioning
RAO Esophagus with superior and inferior no barium
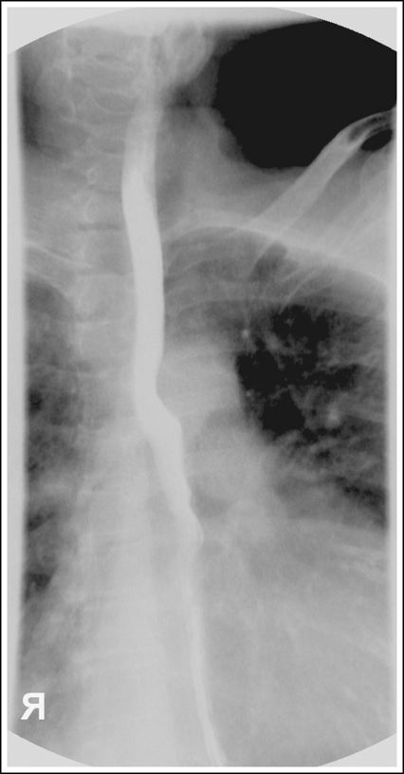
RAO Esophagus with rotation less than 35-40 degrees
Lateral esophagus with proper positioning
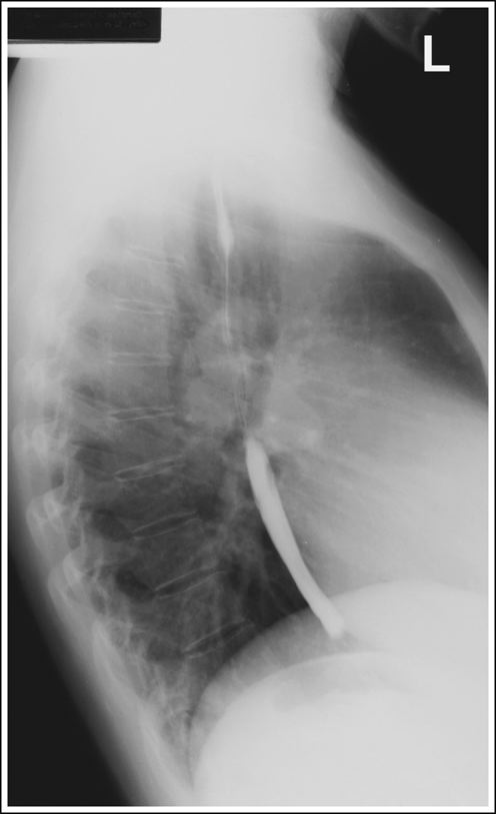
Lateral esophagus with superior and middle no barium
Upper Gastrointestinal Series (UGI) Facts
Try to schedule in AM
Patient should be NPO from midnight until exam (8-9 hours)
No gum chewing or smoking
Brush Teeth but do not swallow water
Mix thick and thin barium if no contraindications and have crystals ready
History of bowel obstruction
Perforation or laceration
Viscus Rupture
Remove clothing from waist up and replace with gown, including glasses necklaces and long earrings
Footboard on table
Lead apron on tower
Control panel ready
UGI Facts 2
May include scout radiograph to rule out contraindications
Patients normally begin with table erect (if unable to stand begin in RAO)
Patient hold barium in left hand
Radiologist has patient drink and fluoro
Have pillow ready for when table is lowered
UGI Routine Projections
AP or PA
RAO or LPO
Right Lateral
Indications for UGI Exam
Bezoar - solid mass of indigestible material that accumulates in the digestive tract that can cause blockage
Phytobezoar - Indigestible plant material such as fibers, skins, and seeds
Trichobezoar - Hair and fingernails usually in patients with mental or anxiety disorders that consume them
Diverticula - small bulging pouches in the digestive system that can become inflamed or infected and lead to blockage of fistula (things connect that shouldn’t connect) (Diverticulosis = disease of having diverticula) (Diverticulitits = inflamed diverticule)
Emesis
Gastritis
Gastric Carcinoma
Ulcers - Sore in the lining of the stomach
Hiatal Hernia - Upper part of stomach pushes through an opening in the diaphragm into the chest cavity
AP Stomach and Duodenum (CR and Positioning)
Supine or trendelenburg for hiatal hernia
14×17 IR
MSP at the level midway between the xiphoid process and the lower rib margin (1-2 inches above lower rib margin L1-L2)
If using 11×14 center between MSP and left lateral abdomen border at the level of L1-L2
Mark left side
Suspend respiration at the end of expiration
Shield gonads
PA Stomach and Duodenum (CR and Positioning)
Recumbent or erect
14×17 IR
CR Recumbent - MSP at the level midway between the xiphoid process and the lower rib margin (1-2 inches above lower rib margin at L1-L2)
CR Erect - Center 3-6 inches lower than recumbent due to visceral movement
Mark left side
Suspend Respiration at the end of expiration
Shield Gonads
PA Oblique Stomach and Duodenum (CR and Positioning)
Recumbent RAO - Visualized the pyloric canal and duodenal bulb. No superimposition of pylorus and duodenal bulb. Gastric peristalsis is more active in this position.
Rotate 40-70 degrees - Hypersthenic patients requires more rotation
11×14 IR
CR - At the level 1-2 inches above lower rib margin (L1-L2) Midway between the vertebrae nd the lateral border of the elevated side
Mark Left Side
Suspend respiration at the end of expiration
Shield Gonads
AP Oblique Stomach and Duodenum (CR and Positioning)
Recumbent LPO - visualized the fundic stomach portion. It does not fill the pyloric canal and duodenal bulb as well as RAO
Rotate 30-60 degrees - Average 45 Hypersthenic requires more rotation
11×14 IR
CR - Midways between the xiphoid process and the lower margin of the ribs
Mark left side
Suspend respiration at the end of expiration
Shield Gonads
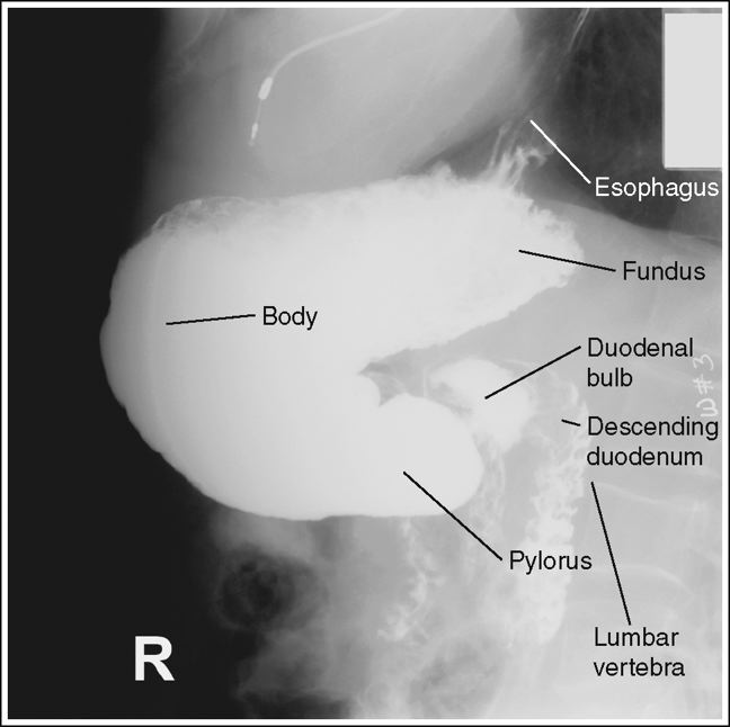
Lateral Stomach and Duodenum (CR and positioning)
Recumbent Right Lateral - Visualized the right retro-gastric space, duodenal loop and the duodenaljejunal junction
Upright left lateral - Visualized the left retro-gastric space
11×14 IR
CR - At the level 1-2 inches above the lower rib margin (L1-L2) Center between the midcoronal plane and the anterior surface of the abdomen
Mark right side down - anterior
Suspend respiration at the end of expiration
Shield gonads
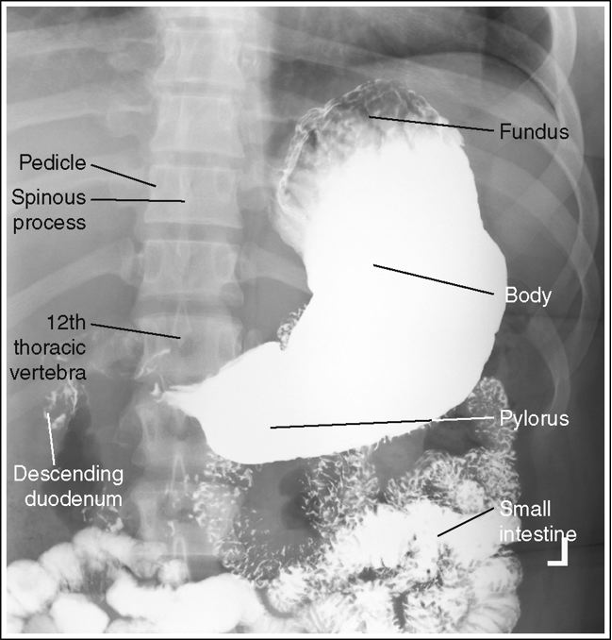
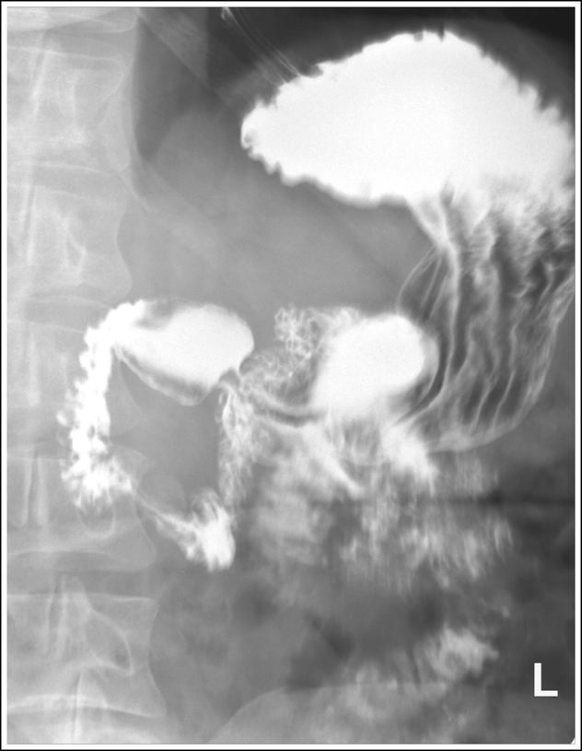
PA Stomach with proper positioning
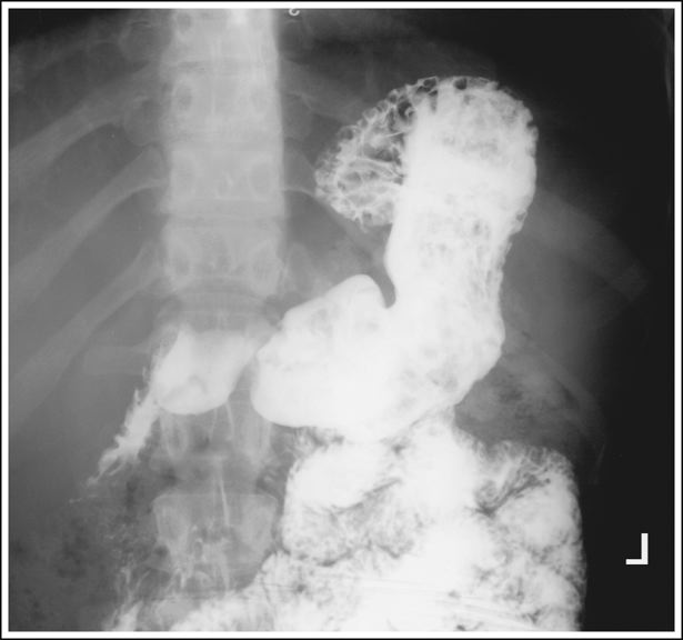
PA Stomach with blotchy appearance within the barium. residual food particles
PA Stomach with fundus overexposed either due to mAs too high or AEC positioned beneath the barium filled body and pylorus

PA Stomach taken on inspiration, compressing and foreshortening the stomach

PA Stomach with proper expiration
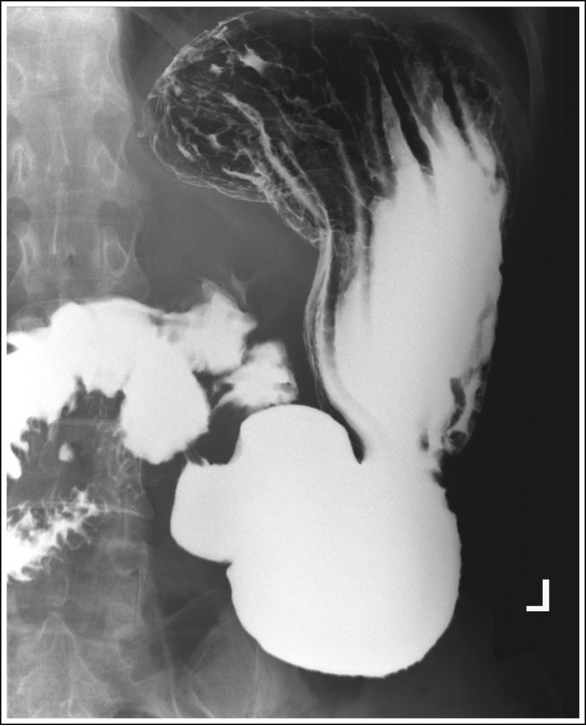
Oblique stomach with proper positioning
Oblique stomach with bony cortices are sharp and the gastric and intestines are blurry. Peristaltic activity of the stomach and small intestines
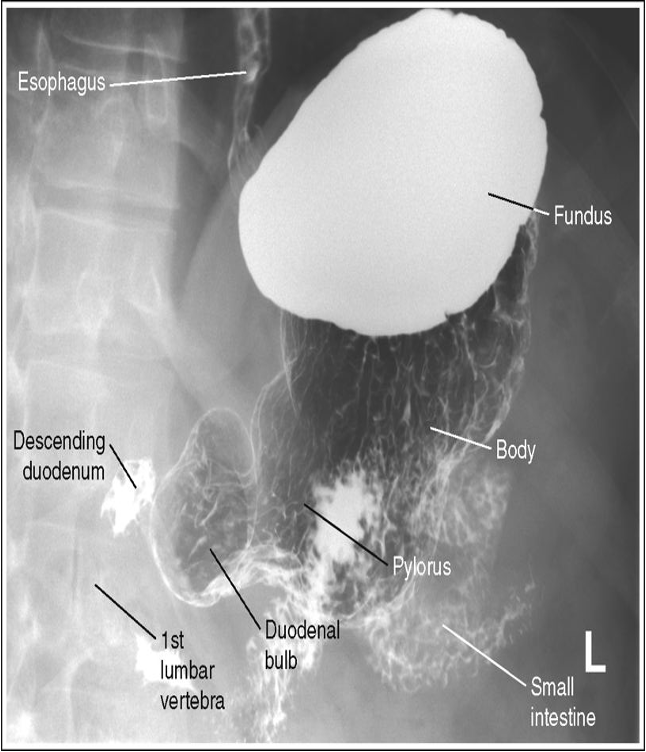
Lateral stomach with proper positioning
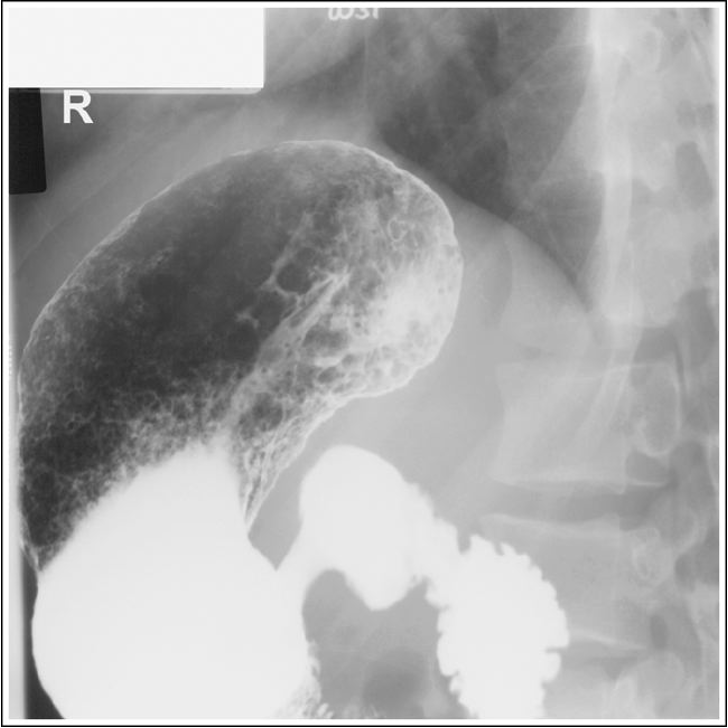
Lateral stomach descending duodenum is partially superimposed over the duodenal bulb and vertebrae, and the posterior surfaces of the thoracic and lumbar vertebrae are not superimposed. Patient was not in a true lateral position