ONTOGENY OF THE DIGESTIVE SYSTEM
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
How does the primitive gut form during embryogenesis?
What structures remain outside the embryo during gut formation?
What embryonic structure gives rise to the peritoneal cavity?
The primitive gut forms when the trilaminar germ disc undergoes cephalocaudal (longitudinal) and lateral (transverse) folding, which incorporates part of the endoderm‑lined yolk sac into the embryo.
The distal yolk sac and allantois remain outside the embryo.
The intraembryonic body cavity is the anlage of the peritoneal cavity.
What tissues form the digestive tract?
• Endoderm → epithelial lining of the gut and glands
• Splanchnic mesoderm → smooth muscle, connective tissue, vasculature
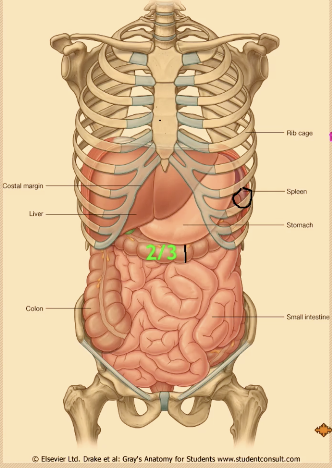
What are the three regions of the primitive gut and their boundaries?
• Foregut: Buccopharyngeal membrane → liver bud(pharyngeal gut to respiratory diverticulum)
• Midgut: Distal to liver bud → junction of right 2/3 & left 1/3 of transverse colon (often left colic flexure)(connected to yolk sac via vitelline duct))
• Hindgut: Distal 1/3 of transverse colon → cloacal membrane
• Foregut → Celiac trunk
• Midgut → Superior mesenteric artery (SMA)
• Hindgut → Inferior mesenteric artery (IMA)
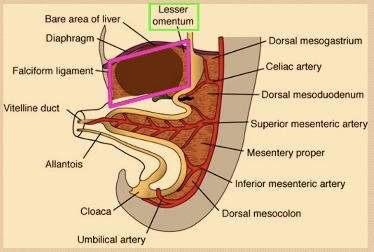
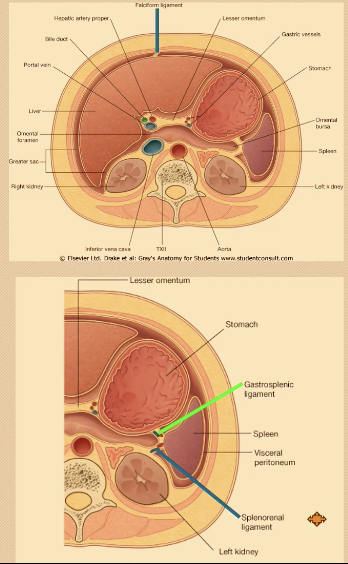
What is the difference between dorsal and ventral mesentery?
•A double layer of peritoneum that suspends viscera from the body wall and contains neurovascular bundles.
Dorsal mesentery: Attaches entire gut to posterior wall; contains celiac, SMA, IMA and associated veins, nerves, lymphatics.
Named : According to attached organ: mesogastrium, mesoduodenum, mesentery, mesocolon.
• Ventral mesentery: Only in caudal foregut; forms lesser omentum (hepatoduodenal ligament) and falciform ligament; liver develops within it. (attaches the liver to the anterior abdominal wall)
(liver found within the ventral mesentery ant to stomach prior to rotation)
Define intraperitoneal organs.
What defines a retroperitoneal organ?
Has a mesentery, covered by visceral peritoneum; not truly “inside” peritoneal cavity (potential space).
Lacks mesentery; located behind posterior parietal peritoneum; may be partial or complete.
HY: Only the transverse colon and the sigmoid colon will retain its part of the mesentery. The ascending colon and descending colon will become cecile or will become retroperitoneal.
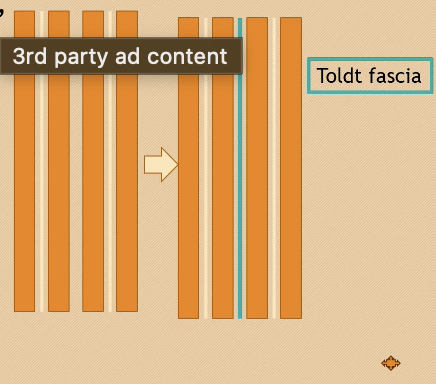
How do secondarily retroperitoneal organs form?
Initially intraperitoneal, then lose mesentery during development and fuse to posterior wall.
Describe what ahppends when you attach two peritoneal membranes together?
HY: if you put two peritoneal membranes together, it's a trilaminar structure. You have epithelium on both sides and connective tissue core in the middle. If you put two together, the epithelium will disappear and the connective tissue will fuse.
What is toldlt fascia
Presence of the tolled fascia can actually lead to a partial separation of the peritoneum whenever you have malignant cells metastasizing between the peritoneal membranes.
Increased ccolic with peristalsis
What is the pressure of the peritoneal cavity?
The peritoneal cavity does not have negative pressure. It has positive pressure to maintain peristalsis.
What are peritoneal ligaments
Double layers of peritoneum connecting organs to organs or body wall; may carry vessels and nerves.(e.g., the falciform ligament or splenorenal ligament); they may carry vessels and nerves
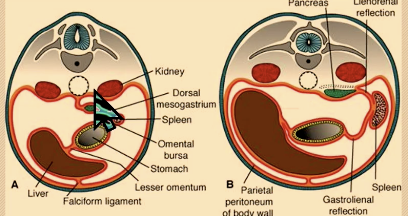
HY: The spleenorhenal ligament was part of the mesogastrium. But when the stomach rotated 90 degrees this way, the posterior mesogastrium actually gets pushed to the left side. And part of it actually fuses to the posterior abdominal wall. The remnant of that between the posterior abdominal wall and the spleen is now called the spleenorhenal ligament. the spleenorhenal ligament is actually a derivative of the primitive mesogastrium.
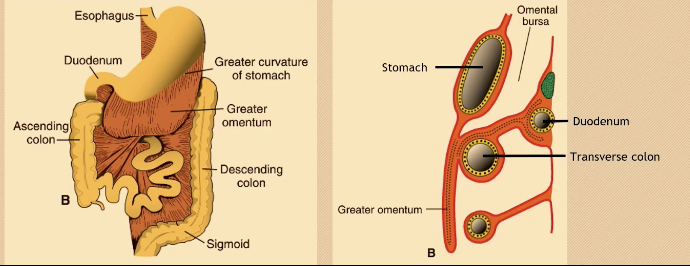
What is the greater omentum?
Large apron-like peritoneal fold from greater curvature of stomach draping over intestines (Over the transverse colon and loops of jejunum and ileum
HY: But look at the diagram. It is now attached not to the posterior abdominal wall, it is attached to the duodenum, which had been earlier pushed into the posterior abdominal wall. So the duodenum is reduced from having a mesentery, becomes retroperitoneal, and on top of that, the transverse mesogon, and with combined greater omentum, is now attached untapped.
How does the stomach rotate?
Fusiform foregut swelling; rotates 90° clockwise so left side faces anteriorly; vagus nerves form trunks.
90° around AP axis; lesser curvature up/right, greater curvature down/left.
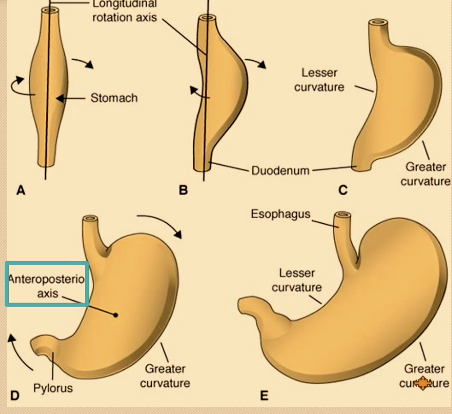
How does the lesser sac form?
Rotation pulls dorsal mesogastrium left, creating the omental bursa.
HY: When the stomach rotates that way, the liver is pushed to the right side. So the space behind the liver and the stomach now is now called the omenthal bursa or called also the lesser sac.
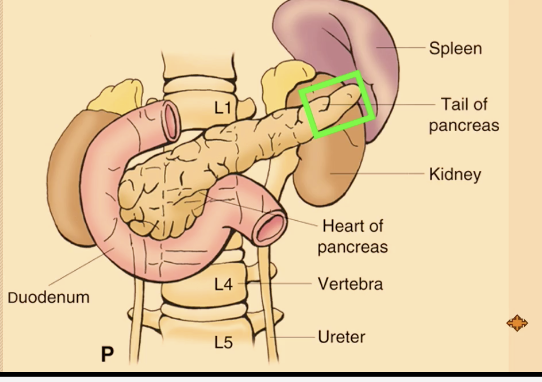
How does the spleen develop and why is it clinically important
From mesoderm in dorsal mesogastrium; intraperitoneal; tail of pancreas in splenorenal ligament.
Hy: So the tail of the pancreas can actually enter the splenorhenal ligament. So we say that the pancreas is retroperitoneal, except for the tail, because it is within the splenorenal ligament.
What are the embryologic origins of the duodenum?
Proximal parts from foregut;
(proximal to the origin of the liver bud) develop from the caudal foregut
distal from midgut; forms C-shape around pancreatic head.
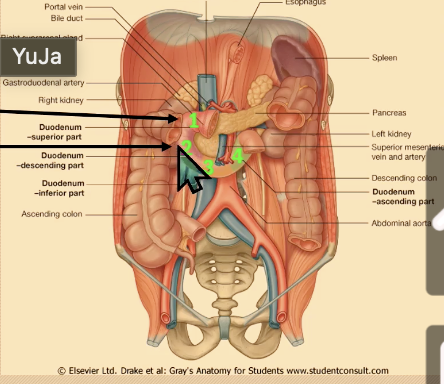
Why is most of the duodenum retroperitoneal?
Dorsal mesoduodenum disappears except at first part. (duodenal cap/ampulla) —> most is thus secondary retroperitoneal
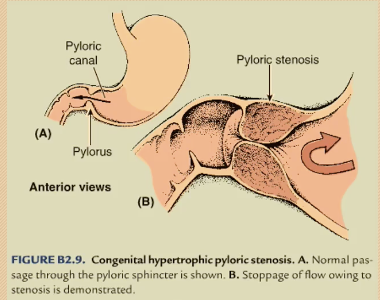
How do pyloric stenosis and duodenal atresia differ?
Pyloric: nonbilious projectile vomiting;
Sphincter hypertrophy, polyhydraminos
Duodenal: bilious vomiting, double bubble sign.
Incomplete recanalization, “double bubble sign”, polyhydraminos
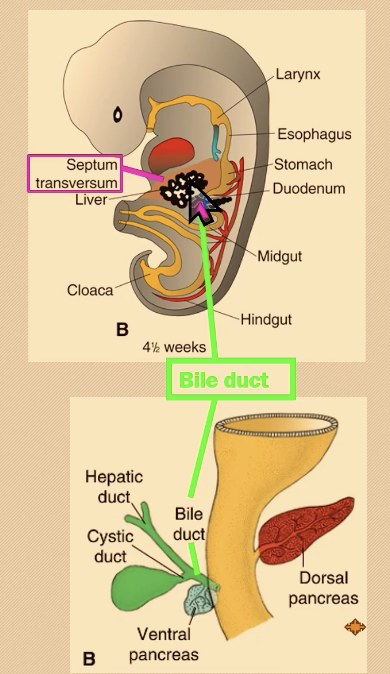
How does the liver develop?
From hepatic diverticulum (endodermal proliferation of hepatic diverticulum ie liver bud) growing into septum transversum; bile duct connects to duodenum.
HY: The two capillary network is, let's say the cilia artery goes to the stomach. There's a capillary network there. That capillary network is drained by the portal vein and goes back into the hepatic sinusoid, which is the second capillary network. So that's why it's called a portal system.
How does liver tissue differentiate?
Endoderm forms hepatocytes; vitelline veins form sinusoids; mesoderm forms stroma.
How does the pancreas form?
Fusion of dorsal and ventral pancreatic buds; ventral forms uncinate + inferior head.
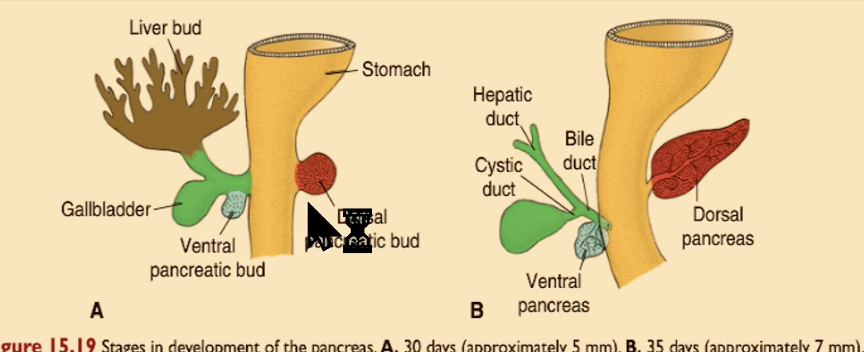
How do pancreatic ducts form?
Main duct (of Wirsung) openng at the major duodenal papilla from ventral + part of dorsal; accessory duct opening at minor duodenal papilla —> from proximal dorsal pancreatic duct.
What anomalies involve pancreas and bile ducts?
Annular pancreas; extrahepatic biliary atresia.
HY: Anomalies associated with deliberate pancreatic development includes extra hepatic atresia, meaning everything outside of the porta hepatis, the hepatic ducts, common bile ducts, they are gone. They did not, let's put it this way, they did not recanalize, they're closed so that the liver cannot drain into the second part of the duodenum. And then you also have an annular pancreas instead of the anterior pancreas rotating posteriorly like this, it would go both ways so that it will now encircle the duodenum and can obstruct the duodenum.
What happens when a pt has a persistent vittiine duct?
Meckel's diverticulum - congenital pouch on the small intestine
What defines the midgut?
What structures form from each limb of the midgut loop?
Communicates with yolk sac; supplied by SMA; bile duct entry to proximal 2/3 transverse colon.
Cephalic: distal duodenum, jejunum, ileum; Caudal: ileum, cecum, appendix, colon.
Why does physiologic herniation occur?
Rapid liver growth reduces abdominal space; intestines herniate into umbilical cord.
How does the midgut rotate?
otal 270° counterclockwise around SMA; returns to abdomen by week 10.
How does the appendix form its position?
Cecal bud descends from RUQ to RLQ, dragging appendix.
Which colons become secondarily retroperitoneal?
Which colons remain intraperitoneal?
Ascending and descending colon.
Transverse (transverse mesocolon) and sigmoid (sigmoid mesocolon).
What causes cecal volvulus?
Failure of ascending colon mesentery fusion.
What structures arise from the hindgut?
What are major hindgut developmental defects
Distal 1/3 transverse colon, descending colon, sigmoid, rectum, upper anal canal.
Imperforate anus; rectourethral/rectovaginal fistula; Hirschsprung disease.
How is the cloaca divided?
Urorectal septum divides into urogenital sinus (anterior) and anorectal canal (posterior).
Why is the pectinate line clinically important?
Separates endodermal (above) from ectodermal (below) anal canal → different innervation, blood, lymph.
Hirschsprung Disease
What causes congenital megacolon?
Absence of enteric ganglion cells → functional obstruction and dilation proximally.