PSYC 367 Final Exam - UBC
1/294
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
295 Terms
Brain regions involved in processing olfactory info
Olfactory bulb -> olfactory tract (mitral & tufted cell axons) to O1 (piriform)
Other involved regions are; amygdala, entorhinal cortex, hypothalamus, orbitofrontal cortex, hippocampus
Which theory can explain specific anosmia?
In a test, people reported different smell perception of a specific odorant due to genetic differences in odorant receptor expression.
Only consistent with shape theory as vibrational patterns of said odorant are constant.
Which theory can explain stereoisomers?
Consistent with shape theory as molecules of different orientation would activate different receptors
NOT consistent with vibration theory as stereoisomers have similar vibrational frequencies
Olfactory Identification
attaching a verbal label to a smell
Ability peaks around age 20 and declines after 50; may be due to decline in verbal semantic processing
Are hedonic responses learned? - Evolutionary evidence
Innate odour responses are only adaptive and advantageous for specialist species (i.e., california ground squirl)
Disadvantageous for generalist species like rats and humans as we have learned taste aversion, where we avoid substances that have been paired with gastric illness, based on smell.
Evidence of chemosignals?
EEG evidence that body odour carries info about potential partners
Transduction of sourness
Tastants enter through H+ channel or as acid (then dissociated into H+ inside cell)
Evidence for labeled-line theory
Tastes can be "knocked out" in mice but they can still taste the other non-knocked out flavours, proving that some fibres are tuned to specific tastes
How does temperature affect absolute thresholds for taste?
sweet - most sensitive at high temperatures
sour - little effect of temperature
salty or bitter - most sensitive at low temperatures
how does self-adaptation affect absolute thresholds for taste?
detection thresholds for sodium chloride (3 concentrations) increase during continued stimulation of tongue with same tastant
Potential health complications of taster status
supertasters/medium tasters: higher risk of colon cancer
supertasters: lower risk of cardiovascular disease
nontasters: more likely to smoke/consume alcohol
Odorant
Odour-inducing chemical molecule that is small, volatile, hydrophobic, and fat-soluble.
Connections between sensory neurons and the olfactory bulb
Synapses occur in the glomeruli in olfactory bulb
Olfactory nerve synapses with mitral & tufted cells in the olfactory bulb
Axons of olf. sensory neurons form the olfactory nerve (cranial I)
Anosmia
Inability to smell
Mechanism of Anosmia and Covid-19
Not completely understood
- OSNs are not infected by the virus
Believed that instead, support (sustentacular) cells in the olf. epithelium are infected and their inflammatory response blocks odorant receptor expression in OSNs.
Treatment for Covid induced anosmia?
Most successful is olfactory training; active sniffing of same small number of odorants every day
Theories of olfactory neural coding
1. Amoore's lock and key theory
2. Shape theory
3. Vibration theory
Vibration theory
Posits that every odorant has a molecular vibrational frequency, odorants with the same frequency would smell the same.
These frequencies would activate odorant receptors through electron tunneling.
Why test vibration theory?
Odorant with same "shape" can smell different
Olfactory Detection - Factors affecting threshold
Sex, Age, Experience, Attention, Odorant
Olfactory Detection - Attention
Thresholds increase during demanding visual tasks
tip-of-the-nose phenomenon
Inability to name a familiar odor; we have fewer words for smell as opposed to other sensations
Cross-adaptation
Sensitivity for a particular odorant reduced after exposure to different but similar odorant; may occur between odorants that fit into the same receptor
Mechanisms for cognitive habituation? (3)
1. Continuous exposure may cause adaptation/recycling to take longer
2. Odorant molecules may be absorbed into bloodstream causing adaptation to continue
3. Cognitive-emotional factors - e.g. reduced habituation if odorant is believed to be harmful
Are hedonic responses learned? - Developmental evidence
Infants display different preferences from adults
Also some preference from in utero exposure
Pheromones
Chemicals secreted by animals through urine/sweat glands for communication; triggers physiological or behavioural response in another member of the same species.
2 types of pheromones
1. Releasers; trigger an immediate, specific behavioural response (i.e., swarming, attracting mates)
2. Primers; trigger slow physiological change, often hormonal (i.e., new queen production, accelerate puberty)
Neural structures involved in pheromone communication
Amygdala, hippocampus & thalamus
nerves innervating the tongue
Vagus nerve (cranial nerve X)
Glossopharyngeal nerve (cranial nerve IX)
Chorda tympani; a branch of the facial nerve (cranial nerve VII)
5 classes of taste stimuli
4 primaries; sweet, sour, salty, bitter
Umami may be a 5th primary quality
Transduction of sweetness
Tastants activate a pair of G protein-coupled receptors (heterodimer [TAS1R2 & TAS1R3, umami activate a similar heterodimer])
Different types of cells in taste buds and transudction (3)
type 1: housekeeping (also saltiness)
type 2: no synapses, but depolarize then release neurotransmitter (atp) that acts on adjacent receptor cells (sweet, bitter, umami)
Type 3: depolarize then release serotonin at synapse with taste nerve fibre (sour)
Neural code for taste intensity
At higher concentrations, more neurons fire / fire faster
Neural code for taste quality theories (2)
Pattern-coding theory
Labeled-line theory
How does duration affect absolute thresholds for taste?
lower thresholds for longer durations of stimulation (for durations between 200 - 1500 ms)
How does location affect absolute thresholds for taste?
slight variation in absolute threshold for primary taste qualities for different tongue locations (but no areas explicitly for specific tastes)
suprathreshold concentrations can be tasted at any location except middle of tongue (no taste buds)
what makes someone a nontaster versus a taster for
PTC/PROP
No taste for nontasters with high thresholds, bitter for tasters with low thresholds.
nontasters have 2 recessive alleles; tasters have 1 or both dominant alleles (usually) for the gene (TAS2R38) that expresses a specific bitter G protein-coupled receptor
Taste hedonics
pleasure/displeasure evoked by primary taste qualities
- present at birth: evidence from newborn facial expressions for the different tastes smile for sweet, pucker for sour, spitting for bitter
flavour vs taste
Flavour; sensations arising when odorants in the mouth stimulate receptors for smell through the retronasal passage
Taste; refers to the 5 basic tastes
interactions between taste, flavour and/or touch sensations - mislocalization
flavour sensations are perceived to come from the mouth even though transduction occurs in olfactory epithelium
Olfactory Detection - Odorant
Easier to detect odorants with longer carbon chains
Kinesthesis
the system for sensing the position and movement of individual body parts (part of proprioception)
Proprioception
The cumulative sensory input to the central nervous system from all mechanoreceptors that sense body position and limb movement.
Mechanoreceptors
Sensory neuron that responds to mechanical stimulation
Glabrous skin
skin that does not contain hair; found on the palms and soles of the feet
4 Types of mechanoreceptors in glabrous skin
SA I (Merkel) - Closest to surface
FA I (Meissner)
SA II (Ruffini)
FA II (Pacinian)
SA I (Merkel)
Small adaptive field
Slow adaptation rate
MFS; < 5 Hz
Primary function; Coarse texture and pattern
FA I (Meissner)
Small Adaptive field
Fast adaptation rate
MFS; 5 to 50 Hz
Primary function; Low frequency vibration and grip
SA II (ruffini)
Large adaptive field
Slow adaptation rate
MFS; 5 to 50 Hz
Primary function; finger position
FA II (Pacinian)
Large adaptive field
Fast adaptation rate
MFS; 50 to 700 Hz
Primary function; high frequency vibration & fine texture
5th type of fast-adapting tactile mechanoreceptors in hairy skin?
Hair follicle receptor
Kinesthetic Mechanoreceptors
Muscle spindles (for muscle length) and golgi tendon organs (muscle tension & joint position)
Physiological zero
normal skin temperature (30-36 celsius)
No sensation of warmth or cold
The response of warmth and cold thermoreceptors with respect to physiological zero
Warmth fibres increase firing rate to increases in skin temp above 36 celsius
Cold fibres increase firing rate to decreases in skin temperature below 30 celsius
nociceptors (3 types)
Pain receptors stimulated by extreme temperature (thermo nociceptors), severe pressure or excessive stretching (mechano nociceptors), chemicals from injured tissue / spicy food (polymodal nociceptors
4 types of nerve fibres coming from skin
1. Proprioceptors (A-alpha)
2. Mechanoreceptors (A-beta)
3. Pain and Temp (A-delta)
4. Pain, temp, and itch (C)
Proprioceptor (A-alpha fibres)
13-20mm (micrometer) diameter
Very thick myelin
80-120 m/s conduction speed
Mechanoreceptor (A-beta)
6-12mm diameter
thick myelin
35-75 m/s conduction speed
Pain and Temperature (A-delta)
1-5mm diamter
thin myelin
5-30 m/s conduction speed
Pain, temperature and itch (C)
0.2 - 1.5 mm diameter
no myelin
0.5-2 m/s conduction speed
Double pain
Initial sharp pain followed by slower, throbbing pain.
types of chemical membrane receptors on C and A-delta fibres.
A-delta; cold fibres, thermal nociceptors or mechano receptors
C; warmth fibres or polymodal nociceptors
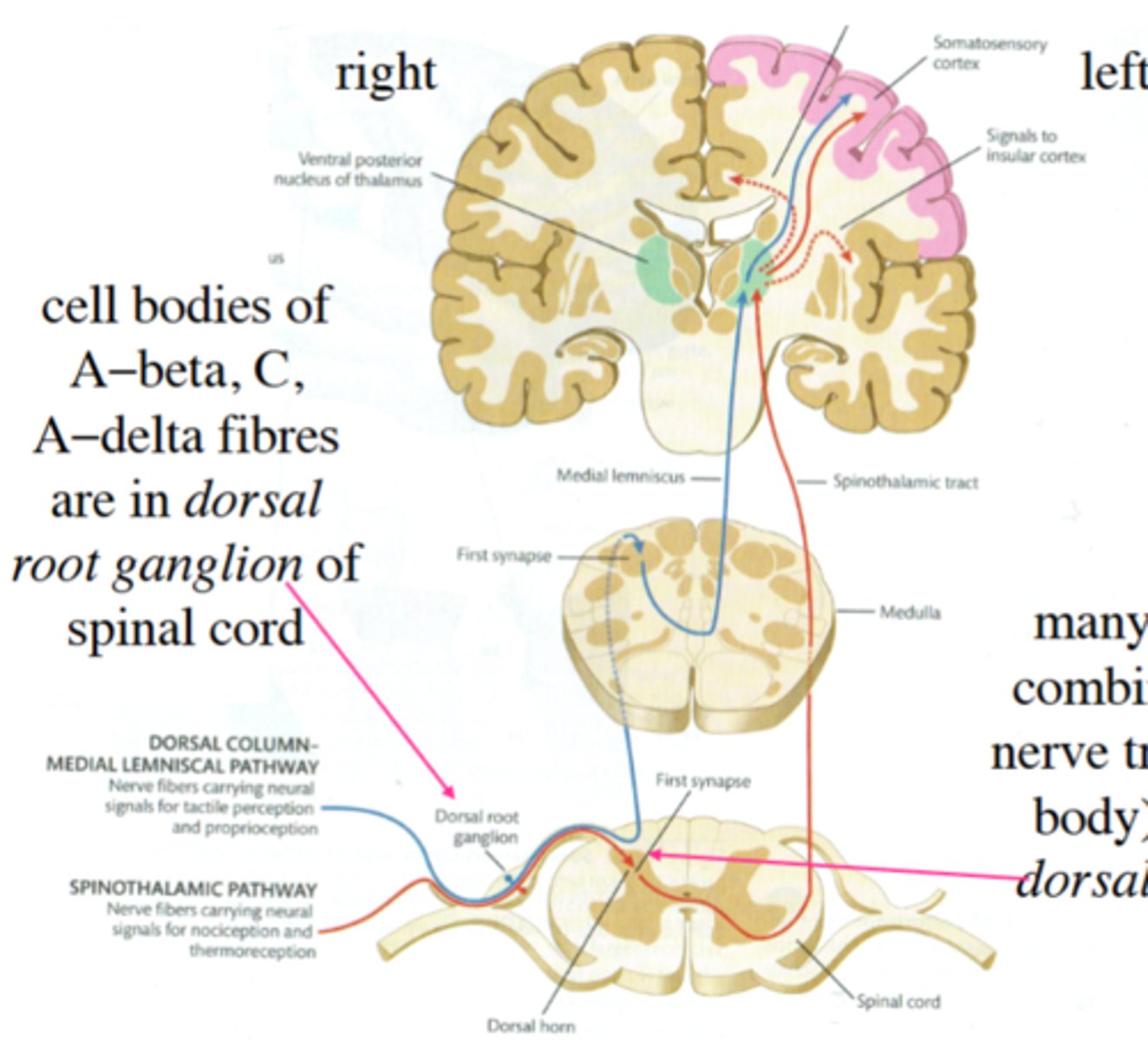
List the main stations where synapses occur, and the connecting pathways, in the dorsal-column-medial-lemniscal pathway and spinothalamic pathway
Dorsal-column-medial-lemniscal pathway; pressure and position
1st synapse for most neurons in the medulla (some synapse in spinal chord)
Then up the dorsal column
2nd synapse at the thalamus in the ventral posterolateral nucleus
3rd synapse in parietal cortex of S1
Spinothalamic pathway; temp & pain
1st synapse in substantia gelatinosa (layer 2) of dorsal horn in spinal cord.
Then through the medulla and up the lateral spinothalamic tract.
2nd synapse at the thalamus in the ventral posterior nucleus (VPL)
3rd synapse in parietal cortex of S1
Somatosensory cortex - 4 sub regions
Broadmann areas
3a, 3b, 1, and 2
Thalamic inputs in S1
Neurons from thalamus synapse in layer 4 of areas 3a (proprioception) and 3b (touch)
Somatotopic maps - Sensory homunculus
Demonstrates that the area of the cortex dedicated to the sensations of various body parts is proportional to how sensitive that part of the body is.
Wilder penfield
Created the somatotopic map (sensory homunculus)
Somatosensory Sensitivity (measure & highest sensitivity)
Sensitivity measured as the inverse of absolute threshold (small threshold = high sensitivity)
Highest sensitivity on face, lowest on foot
Somatosensory discrimination (measure)
Weber's law
Somatosensory acuity (measure and higher sensitivity)
Minimum distance at which two stimuli are just perceptible as 2 seperate (2-point threshold)
Measured by seeing when and where 2 touches are perceptible.
More likely to be detected in areas with larger cortical representation.
the relationship between the sensory homunculus, receptive field size and 2-point thresholds.
areas with smaller receptive fields and larger representation on the sensory homunculus (e.g., hands and face) can detect finer spatial details and have lower 2-point thresholds.
Aristotle's illusion
A touch to fingers crossed or uncrossed can either feel 1 or 2 touches due to differences in cortical representation and location of the areas touched.
Limbic system structures responsible for processing emotion
Anterior cingulate, insula, amygdala
Prefrontal cortex
responsible for modulating pain perception and chronic pain emotional response
modulation of pain
Modulation of pain sensitivity by enkephalins & endorphins (endogenous opiates) released by descending inputs from brain. These opiates block the release of neurotransmitters involved in pain
Neurotransmitters involved in pain
Substance P released by C fibres, picked up by NK-1 receptors on spinal cord. Also glutamate
Gate control theory
Theory that spinal cord contains transmission cells that carry pain signal to the brain to the brain but that there exists fast mechanoreceptor signals that close the pain gate and slow nociceptor signals that open the pain gate.
Transcutaneous Electrical Nerve stimulation (TENS)
Device that delivers electric current through skin near site pain
How does transcutaenous electrical nerve stimulation support gate control theory?
The electric current activates A-beta fibres to close the pain gate and stimulates the release of endogenous opiates.
How do anesthetics work to relieve pain
Produces a total loss of sensation by interrupting signals travelling to brain.
Local anesthetics act at site of injection and block sodium channels
General anesthetics act on brain itself and cause unconsciousness
How do analgesics work to relieve pain?
Non-opiate analgesics like aspirin & ibuprofen block prostaglandin
Opiate analgesics like morphine, codeine & heroin block nociceptor release of neurotransmitter and inhibit spinal cord neurons
How does acupuncture work to relieve pain
Believed to cause a release in endogenous opiates.
Nociceptive pain
pain as a result of stimulation of free nerve endings in skin, muscles & joints.
Inflammatory pain
signal that some type of tissue damage has occurred
Neuropathic pain
pain from damage to neurons of either the peripheral (eg sciatica) or central nervous system (eg MS)
Allodynia
pain due to stimulus that should not be painful, the nociceptors have lower threshold for stimulation
Hyperalgesia
Painful stimuli become more painful, exaggerated sensitivity.
peripheral sensitization
Change in nociceptors
Central sensitization
Increased # of pain receptors, rewiring of connections or loss of inhibitory cells in spinal cord
In terms of sensitization, what happens when pain is not treated?
Hyperalgesia and/or allodynia are exacerbated.
How do anticonvulsants work to relieve pain?
they inhibit a specific type of calcium channel to prevent release of nociceptor neurotransmitter
How does capsaicin work to relieve pain?
Stimulates nociceptors; killing them or using up their supply of neurotransmitter.
How do cannabinoids work to relieve pain?
Block neurotransmitter release from nociceptors and reduce inflammation.
How do NMDA-receptor blockers work to relieve pain?
Prevents glutamate from binding with NMDA receptors on spinal cord neurons
Phantom limb pain (Ramachandran)
Described phantom limb pain through cortical organization of somatosensation. Said phantom limb pain arises due to cortical reorganization, sensory confusion, and a mismatch between the brain's body map and actual physical sensations, which the brain interprets as pain.
Mirror box treatment for phantom limb pain
Placing an injured limb in a box and the uninjured limb in front of a mirror. Move both limbs symmetrically while looking in mirror. This makes it feel like the amputated limb is moving; relieving pain
Electrical stimulation implant treatment for phantom limb pain
Electrical stimulation in spinal cord dorsal column to close pain gate
Visible light wavelength
400-700 nanometers
Properties of light
wavelength, intensity, absorption, diffraction, reflection, transmission, and refraction
Light - Wavelength
the distance between peaks in light waves