Microbio lec11 Host-Microbe Interactions and Infectious Disease Transmission
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
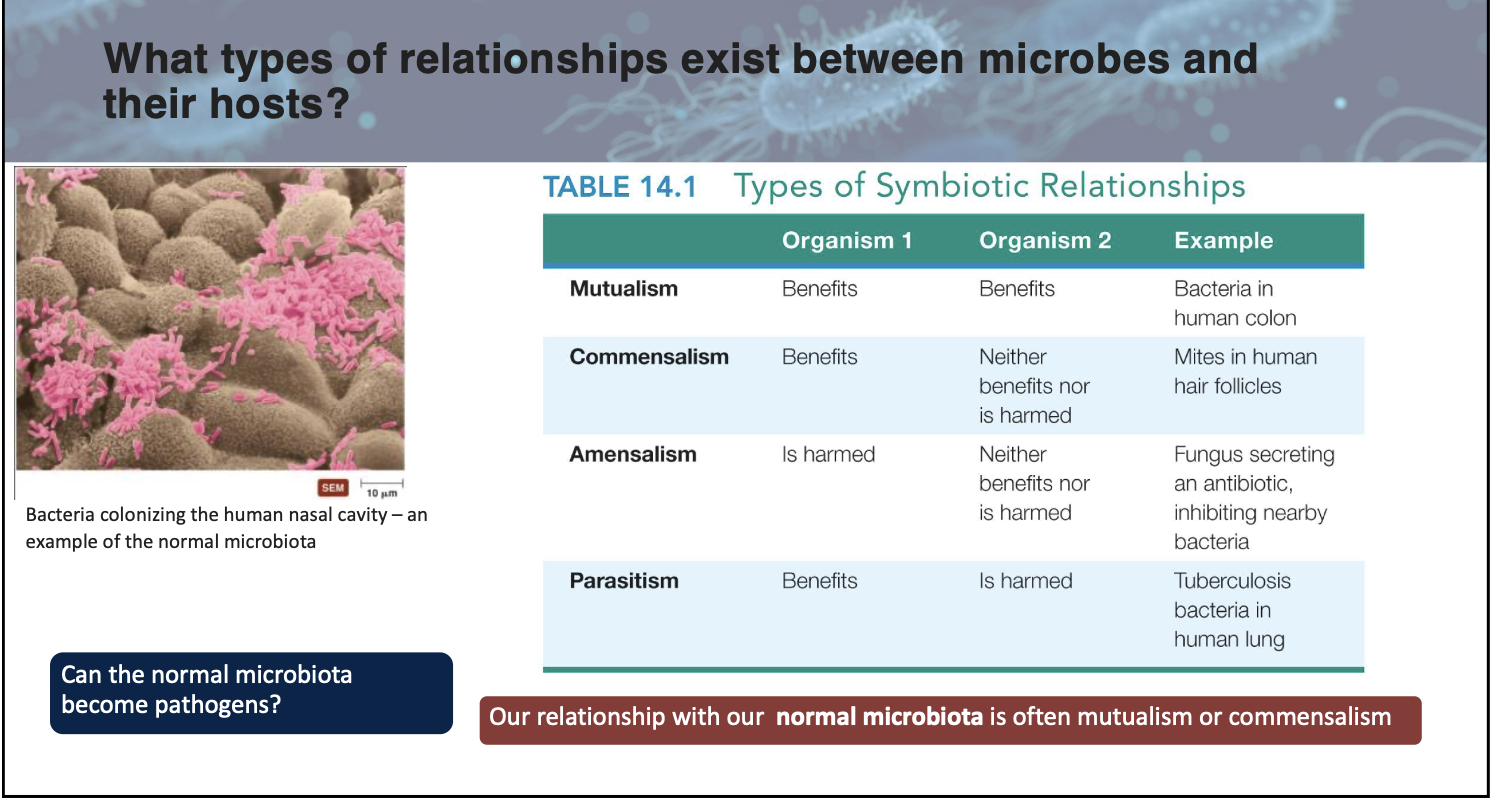
What is;
Mutualism
Commensalism
Parasitism
Amensalism
Mutualism — Interaction where both host and microbe benefit
Commensalism — Situation where one organism benefits without significant effects on the other.
Parasitism — Microbe benefits but the host is harmed
Amensalism — One organism is harmed/inhibited while the other is unaffected (antagonism)
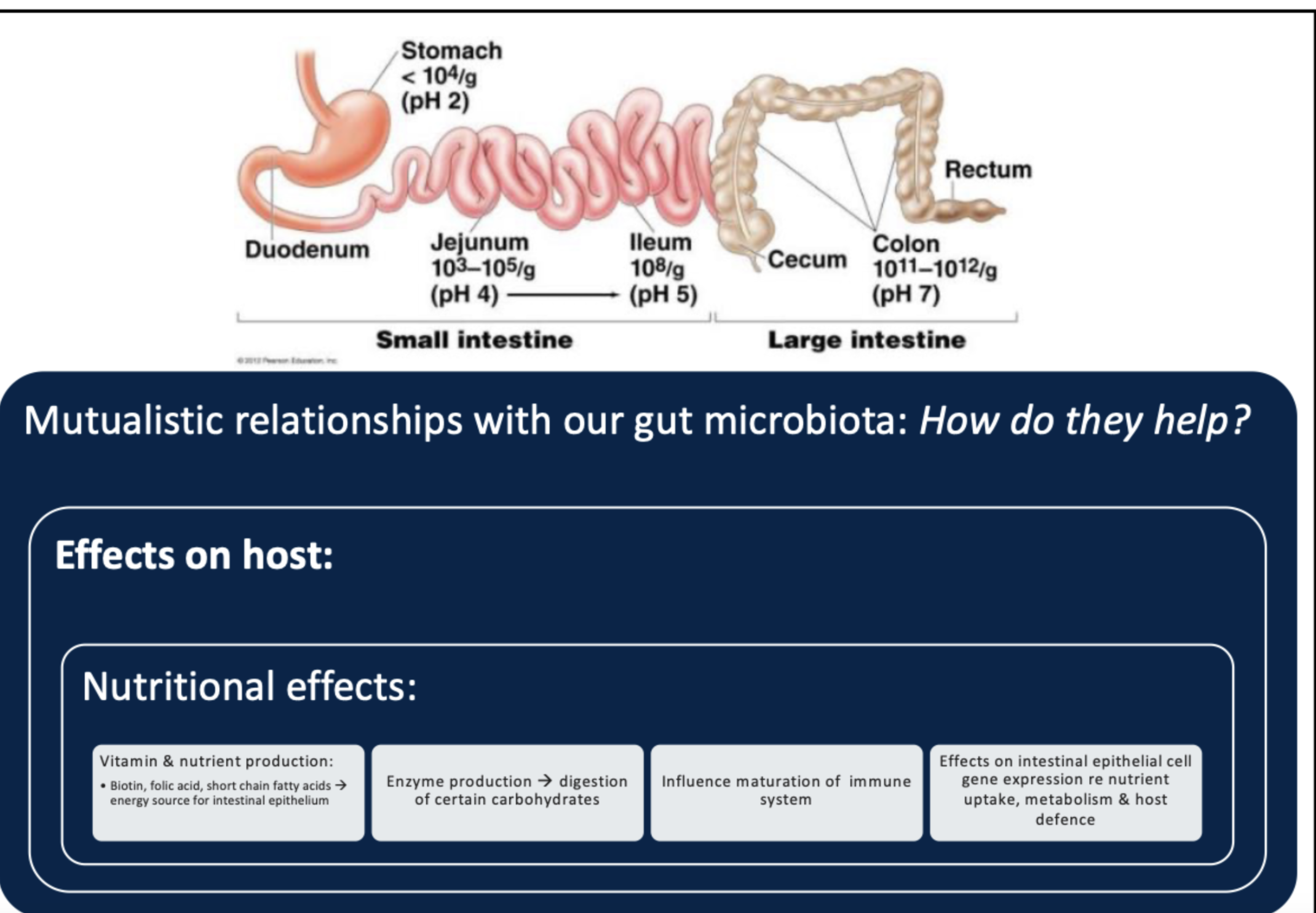
What is the primary function of microbial antagonism in the gut microbiota?
A) Production of vitamins
B) Competition for nutrients and space
C) Production of short-chain fatty acids
D) Suppression of immune responses
B
What term describes the number of microbes needed to infect 50% of exposed animals?
A) Infectious dose
B) Virulence factor
C) Pathogenicity index
D) Microbial load
A (also referred to as the ID50)
Which site in the human body harbors approximately 750 species of aerobic and anaerobic bacteria?
A) Skin
B) Urogenital tract
C) Respiratory tract
D) Mouth
D
attach slide 1 pt6
Highly virulent microbes usually cause disease, while less virulent microbes require larger __________ or weakened hosts.
Infectious doses
attach pt1slide13
__________ is the study of the cause of a disease.
Disease etiology
True/False: The introduction of colonic E. coli into the urethra is an example of an opportunistic infection.
True (it’s an example of “being in the wrong location”)
True/False: The production of biotin and folic acid by gut microbiota contributes to host nutrition.
True (energy source for intestinal epithelium)
True/False: Normal microbiota can never become pathogenic under any circumstances.
False (In certain situations, the normal microbiota can cause infections – and so become opportunistic pathogens)
How does microbial antagonism contribute to host defense mechanisms?
Microbial antagonism prevents pathogen colonization by competing for nutrients and space, lowering pH, and producing bacteriocins that inhibit harmful microbes.
What is the primary role of capsules in bacterial virulence?
A. Nutrient absorption
B. Cell lysis of host epithelium
C. Evasion of host defences
D. Biofilm formation
C
pt2 slide17
What is the primary virulence factor of Giardia intestinalis?
A. Flagella
B. Trophozoite
C. Adhesive disk
D. Cyst wall
C
pt2 slide6
What type of enzymes do bacteria like hyaluronidase and collagenase produce to invade tissues?
A. Membrane-bound enzymes
B. Intracellular enzymes
C. Cytoplasmic enzymes
D. Extracellular enzymes
D
pt2slide11
What is the first step in the process of phagocytosis by immune cells?
A. Ingestion of microbes by phagocytes
B. Fusion of vesicles with the phagosome
C. Chemotaxis of phagocyte to microbes
D. Adherence of phagocyte to microbes
C
pt2 slide15
What happens during the fusion of a phagosome with lysosomes in phagocytes?
A. The phagosome fuses with the nucleus to form a phagolysosome
B. The phagosome fuses with the Golgi body to form a phagolysosome
C. The phagosome fuses with lysosomes to form a phagolysosome
D. The phagosome fuses with the endoplasmic reticulum to form a phagolysosome
C
pt2 slide 15
True/False: Virulence reflects the ease of infection and ability to cause disease.
True
pt2 slide3/4
__________ are short-lived phagocytic cells found in blood and tissues, also known as polymorphonuclear leukocytes (PMNs)
Neutrophils
Note: Monocytes differentiate into Macrophages which are longer lived and differentiate into specialized types in tissues
Bacteria like Listeria monocytogenes escape destruction by phagocytosis using __________, a pore-forming protein that allows escape from the phagosome into the cytosol.
Listeriolysin O
Explain how viruses cause visible changes in infected host cells (cytopathic effects).
Viruses cause cytopathic effects by taking over host cell machinery, leading to visible changes such as syncytia formation, inclusions, cell lysis, or transformation into cancer cells.
Describe two mechanisms by which bacteria evade phagocytosis and survive within host cells.
Bacteria evade phagocytosis by producing capsules that impede capture and prevent digestion through incomplete phagocytosis (e.g., preventing phagosome-lysosome fusion).
Some bacteria produce leukocidins that kill phagocytes.
How do actin tails produced by Listeria facilitate its spread between cells?
The actin tails:
Propel Listeria to cell edges
Extend into neighbouring cells
Facilitate direct spread without extracellular exposure
List three strategies used by pathogens to suppress or evade immune responses, providing specific examples for each strategy (e.g., antigenic variation, protease production).
Strategies include antigenic variation (e.g., Influenza virus), protease production (e.g., Neisseria gonorrhoeae destroys IgA), and immunosuppression (e.g., HIV suppresses immune system function).
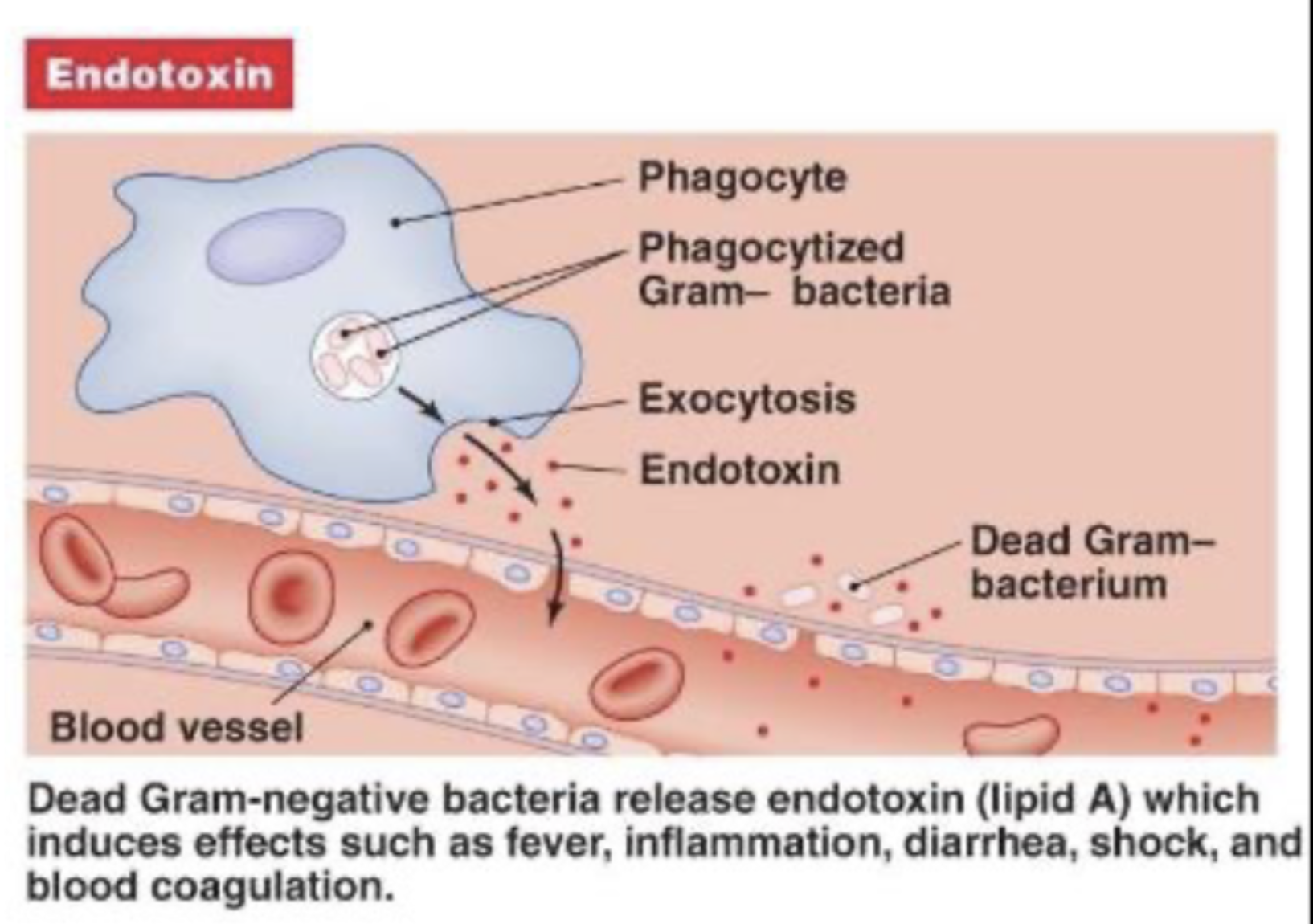
Which of the following is true about endotoxins?
A) Found in Gram-positive bacteria
B) Composed of proteins
C) Secreted by living bacteria
D) In outer membrane of Gram-negative bacteria
D
Note: as for exotoxins, they are found in both G- and G+
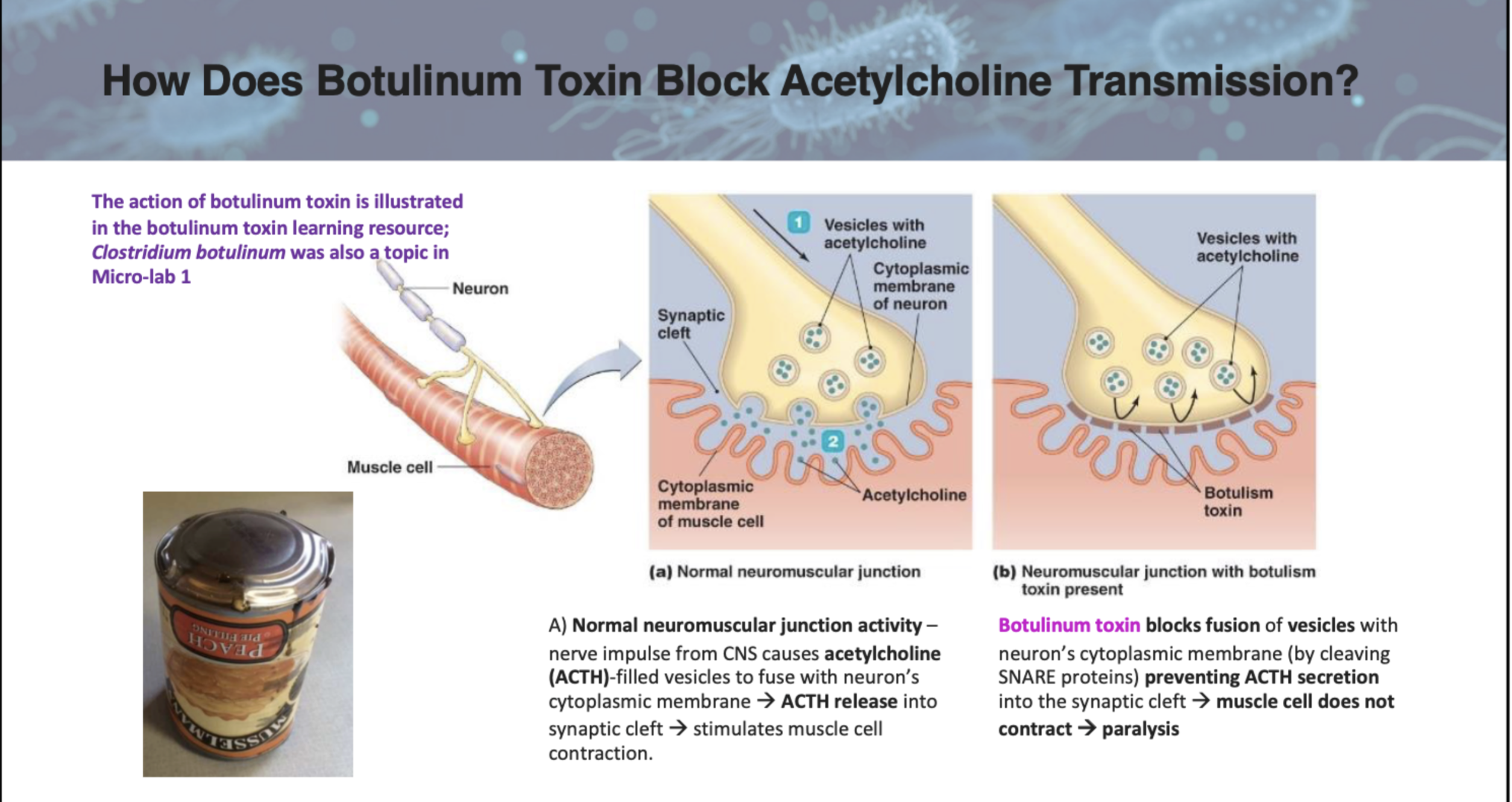
What is the primary effect of botulinum toxin on neuromuscular junctions?
A) Stimulates acetylcholine release
B) Blocks acetylcholine release by cleaving SNARE proteins
C) Prevents muscle relaxation
D) Stimulates cytokine production
B
What is the mechanism of action of cholera toxin?
A) Prevents muscle contraction by blocking acetylcholine secretion through cleaving of SNARE
B) Activates adenylate cyclase, increasing cAMP levels and causing electrolyte loss
C) Induces cytokine release leading to inflammation and shock
D) Directly kills intestinal epithelial cells
B
pt3 slide8
Which bacterial toxin acts as a superantigen?
A) Cholera toxin
B) Botulinum toxin
C) Toxic Shock Syndrome Toxin
D) Tetanus toxin
C
pt3slide12/13
Exotoxins can be classified based on their location of action, such as ________, which act on gut tissues, and ________, which act on nervous system tissues.
Enterotoxins and Neurotoxins
The ________ portion of an A-B type toxin binds to specific receptors on host cells, while the ________ portion exerts toxic effects inside the cell
B and A
The medical application of botulinum toxin includes treating neurological conditions like ________ and its cosmetic use as ________.
Blepharospasm; Botox
Toxoids are altered toxins that retain their ability to stimulate an immune response but lose their ability to cause ________.
Harm
pt3slide15
Explain how cholera toxin leads to severe dehydration and metabolic acidosis in affected individuals
Cholera toxin binds to intestinal epithelial cells, activating adenylate cyclase via its A1 subunit, increasing cAMP levels, which stimulates electrolyte secretion into the intestinal lumen, causing water loss through osmosis, leading to dehydration and metabolic acidosis.
Compare and contrast endotoxins and exotoxins in terms of structure, source, and effects on host cells.
Endotoxins are lipid components (Lipid A) found in the outer membrane of Gram-negative bacteria and induce systemic effects like fever and shock; exotoxins are proteins secreted by both Gram-positive and Gram-negative bacteria that target specific tissues or cellular processes.
How do superantigens like Toxic Shock Syndrome Toxin (TSST) lead to toxic shock syndrome? Include key steps in disease progression in your answer.
Superantigens like TSST link T helper cells to antigen-presenting cells excessively, causing massive T cell activation and cytokine release, leading to fever, hypotension, rash, shock, and multi-organ failure characteristic of toxic shock syndrome.
Which of the following bacteria is more virulent?
A) Staphylococcus aureus
B) Staphylococcus epidermidis
C) Both are equally virulent
D) Neither is virulent
A
What is a common cause of infections in patients with indwelling vascular catheters?
A) Staphylococcus aureus
B) Escherichia coli
C) Staphylococcus epidermidis
D) Salmonella
C
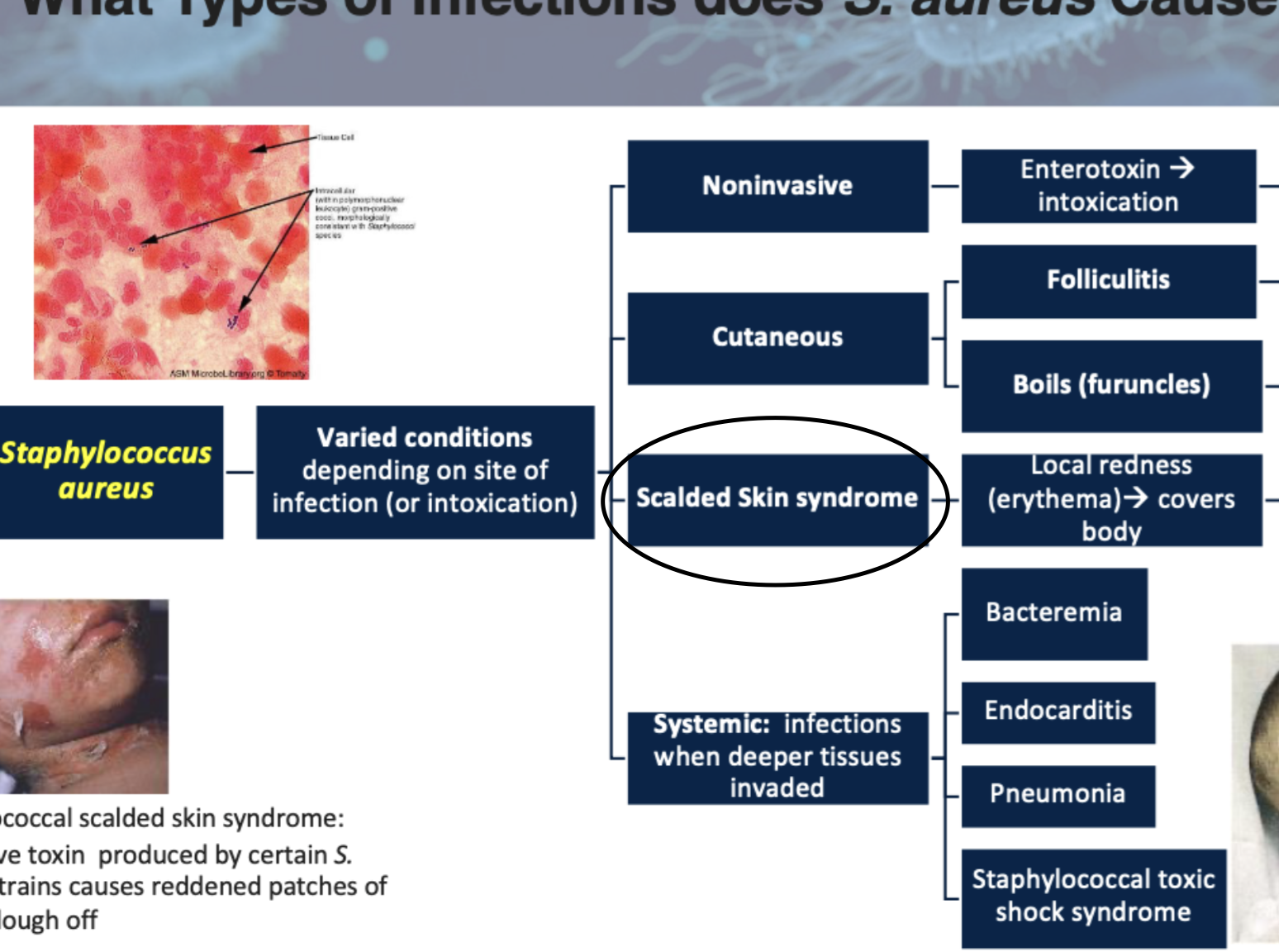
Staphylococcus aureus can cause a condition known as _________________ skin syndrome.
scaled
True/False: Staphylococcus epidermidis is a common cause of skin infections.
False (although it’s usually part of the normal skin microbiota, it rarely causes infection)
Which toxin produced by Staphylococcus aureus causes skin blisters and peeling?
A) Enterotoxin
B) Cytolytic toxin
C) Toxic shock syndrome toxin (TSST)
D) Exfoliative toxin
D
What is the primary mechanism by which Enteropathogenic E. coli (EPEC) causes damage?
A) Using a Type III secretion system
B) Producing Shiga-like toxin
C) Forming biofilms
D) Producing endotoxin
A
Note: producing Shiga-like toxin is a primary mechanism for Enterohemorrhagic
E. coli (EHEC).
Enterohemorrhagic E. coli (EHEC) produces a toxin similar to the Shiga toxin, which can cause _______________________ syndrome
Hemolytic uremic
Note: EHEC is most severe in children and elderly
pt4 slide8
Describe the differences in virulence factor production between Staphylococcus aureus and Staphylococcus epidermidis.
Staphylococcus aureus produces a variety of virulence factors such as coagulase, protein A, and toxins like enterotoxins and TSST, which enable it to cause a wide range of infections. In contrast, Staphylococcus epidermidis is generally less virulent and forms biofilms on medical devices, leading to infections mainly in immunocompromised patients.
attach pt4 slide3
Explain how Staphylococcus aureus causes localized skin infections like boils.
Staphylococcus aureus causes localized skin infections like boils by initiating an infection that involves coagulase leading to formation of fibrin walls. This action would result in the formation of pus-filled abscesses due to leukocydins from the staph killing cells from the immune system that are trying to kill the staph.
What is the primary mode of transmission for Shigella infections?
A) Vector-borne
B) Fecal-oral route
C) Airborne
D) Direct contact with infected animals
B
Which of the following toxins is produced by Shigella and inhibits protein synthesis?
A) Enterotoxin
B) Cytolytic toxin
C) Shiga toxin
D) Hemolysin
C
How does Shigella typically invade host cells?
A) Through a Type II secretion system
B) Using a Type III secretion system
C) By forming biofilms
D) Through endocytosis without a secretion system
B
Note: Type III secretion system Forms a channel between bacterial cell & host cell to inject toxic protein
Compare the virulence factors and disease-causing mechanisms of Enterohemorrhagic E. coli (EHEC) and Shigella.
Both Enterohemorrhagic E. coli (EHEC) and Shigella produce toxins that inhibit protein synthesis and cause cell death. EHEC produces Shiga-like toxin, which damages the large intestine and can lead to hemolytic uremic syndrome. Shigella causes dysentery by attaching to intestinal epithelial cells and spreading through actin polymerization, leading to bloody diarrhea. Both are severe gastrointestinal pathogens but differ in their specific mechanisms of infection.
pt4slide12
Which of the following best describes the typical progression of a Salmonella infection?
A) Immediate bloodstream invasion followed by high-grade fever, epithelial cell death and diarrhea
B) Localized infection of the liver with no gastrointestinal symptoms
C) Attachment to intestinal epithelial cells, endocytosis, intracellular multiplication, and possible spread to bloodstream
D) Direct toxin injection into host cells via Type III secretion system, causing neurological symptoms
C
True/False: Koch's Postulates can be applied to all pathogens without any exceptions.
False (Diseases can be caused by more than one pathogen as well as other cofactors)
pt5slide8
Helicobacter pylori is a Gram-negative, curved rod bacterium that causes _______________________
Gastic (peptic) ulcers
True/False: Helicobacter pylori can survive in the acidic conditions of the stomach by producing urease.
True
What is a major virulence factor of Helicobacter pylori that helps it neutralize stomach acid?
A) Adhesins
B) Flagella
C) Urease
D) Twitching motility
C (to convert urea to ammonia, raises pH (decreases acidity & “neutralizes” stomach acid)
Note: A and B are also virulence factors but I don’t think they’re the most important or major one.
Explain the initial ulcer theories?
Initially, gastric ulcer was thought to be caused by stress/ excess stomach acid consumption of spicy food, alcohol… Therefore at the time it was believed that those conditions would irritate the stomach lining causing ulcer. Also, the stomach was thought to be sterile bcuz of its acidic environment leading to decrease microbes.
Barry Marshall and J. Robin Warren were awarded the ______________ in Physiology or Medicine in for their work on Helicobacter pylori.
Nobel prize
An infectious disease is caused by:
A) non-living agents
B) infectious agents
C) genetics
D) environmental factors
B
True/False: A communicable disease cannot be spread from one host to another.
False (it can be spread meaning its contagious ex. chickenpox)
Note: noncommunicable disease do not spread and are acquired thru alternate routes:
• Ex) Infection resulting from a burst appendix
• Ex) Tooth decay; acne
• Ex) Tetanus – caused by Clostridium tetani
Diseases that occur mainly in animals, but can be transmitted to humans are called __________.
Zoonoses
Which of the following is an example of a sign of a disease?
A) Pain
B) Headache
C) Fever
D) Nausea
C
Note: “signs” are characteristics of a disease that can be observed by examining patient. Pain, headache and nausea are “symptoms,” only felt by patient
A(n) __________ infection is limited to a small area of the body.
Local (ex. boils, bladder infection)
Which of the following is a type of infectious disease?
A) Primary infection
B) Secondary infection
C) Superinfection
D) Subacute
E) All of the above
F) most of the above
E
True/False: The incubation period is the time between recovery and the disappearance of symptoms.
False (it’s the time between infection & first symptoms or signs)
__________ are animate or inanimate sources where microorganisms can survive and multiply.
Reservoirs
True/False: Vectors transmit diseases through direct contact.
False (Involves mechanical/biological transmission of pathogen carried by insects only)
What is a fomite? Give an example.
A fomite is a non-living object involved in the spread of disease. Example: a contaminated doorknob, toothbrush, glasses…
Which of the following is a common portal of entry for microbes?
A) Skin
B) Mucous membranes
C) Placenta
D) All of the above
D