Clinical Skills - Blk 4
1/184
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
185 Terms
For best practice, conduct urinalysis in the first ____ minutes.
30
If urine samples cannot be analyzed quickly enough, what should you do?
Immediately refrigerate in a clean, sealed container
Samples should be warmed to room temperature prior to analysis
Mix thoroughly prior to analysis
Patient-side analysis of urine reduces…
Growth or death of bacteria
Cell and cast degradation, especially with low urine specific gravity
Formation of crystals and amorphous material
Breakdown of bilirubin by sunlight
The urinalysis is only complete with all three parts. What are the three parts?
Physical analysis
Chemical analysis
Sediment analysis
What qualities do we measure when performing physical analysis of urine?
Color, clarity, urine specific gravity
What are the benefits of performing a chemical analysis with the IDEXX VetLab UA Analyzer?
Eliminates subjectivity
Reads pads at the correct time
Compensates for background color of urine
Transfers data automatically to the patient record on the IDEXX VetLab Station and VetConnect PLUS
What are the benefits of performing a sediment analysis with the SediVue Dx Urine Sediment Analyzer?
Accurate, consistent, real-time results in 3 minutes
Small sample volume is required
High-quality images are part of the medical record
Automated microscopy standardizes evaluation of urine sediment
Two-way integration:
Automatically uploads results to the patient record
Charge capture
What volume is used for sediment analysis with the SediVue Dx Urine Sediment Analyzer
165 microliters
If the SediVue Dx Urine Sediment Analyzer is classified as “None detected”, what does that mean?
Element has not been detected. There are not enough recognizable features to classify.
If the SediVue Dx Urine Sediment Analyzer is classified as “<1/HPF”, what does that mean?
Some features are present, although rare and below the clinical reporting threshold
If the SediVue Dx Urine Sediment Analyzer is classified as “Suspect presence”, what does that mean?
There are some recognizable features of an element (cocci, rods, casts) present; however, there are not enough features, or quantity, to report as “present”
If the SediVue Dx Urine Sediment Analyzer is classified as “Present”, what does that mean?
High confidence in the presence of bacteria in the sample
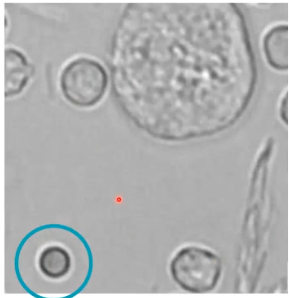
Red Blood Cells (RBC)
Uniform size, round
No nuclear content visible
Area of central pallor
Smallest cell type
Can look similar to lipids but more uniform in size
Potential crenation (not shown here)
High USG
Uniform short projections from cell surface
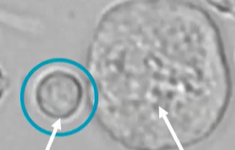
White blood cells (WBC)
Slightly larger than RBCs
Smaller than nonsquamous epithelial cells
Contain internal cellular structures
Nuclei
Granular cytoplasm
Primarily neutrophils but other leukocyte types may be present
What are the two broad categories of epithelial cells?
Squamous
Non-squamous
Transitional cells
Renal tubular epithelial cells
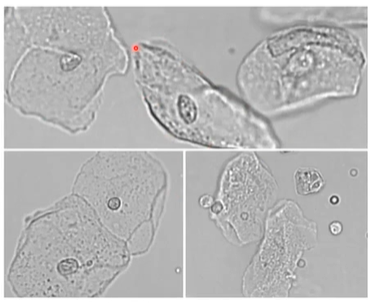
Squamous epithelial cells
Larger than RBCs and WBCs and most nonsquamous epithelial cells
Primarily contamination from the external genitalia
Low numbers can be normal (sloughing of old cells)
High numbers may or may not suggest a significant pathological process
Nonsquamous epithelial cells
Low numbers normal due to cell sloughing and turnover
High numbers possible with hyperplasia
Inflammatory
Noninflammatory
Air-dried, stained cytology preparation recommended if TCC suspected
What are two broad categories of casts?
Hyaline
Nonhyaline
Cellular
Granular
Waxy
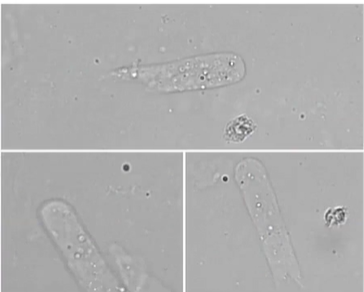
Hyaline casts
Occasional hyaline casts are normal
Low numbers may occur with fever or following strenuous exercise
Dehydration may result in increased numbers
High numbers indicate kidney injury
Often accompanied by proteinuria
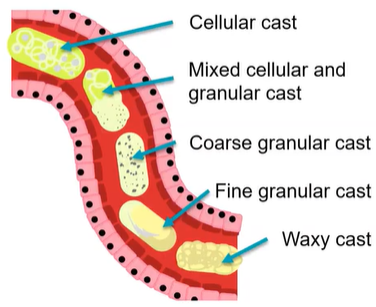
Nonhyaline casts
Cellular casts (rare)
Renal tubular, red blood cells and white blood cells
Granular casts (common)
Coarse to fine
Waxy casts
Well-defined, refractive index
Final stage of cast progression
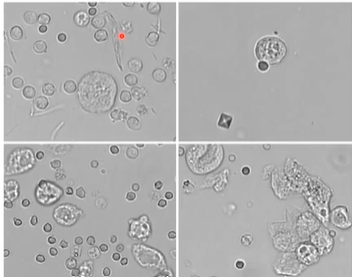
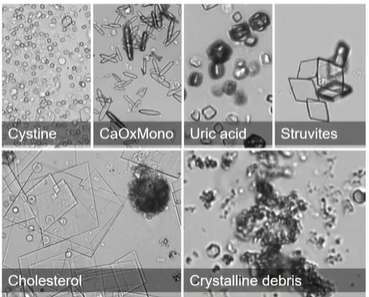
Types of crystals
Calcium oxalate dihydrate
Struvite
Ammonium biurate
Bilirubin
Unclassified crystals
Crystals in urine
Precipitation of various elements
May or may not occur with uroliths
May form or dissolve in aged or altered samples
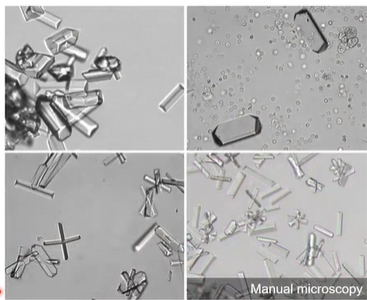
Struvite
Magnesium ammonium phosphate or triple phosphate crystals
Clear, colorless, with coffin-lid shape
Alkaline to slightly acidic urine
Low numbers in healthy dogs
Potential high numbers associated with inflammatory urinary tract disease
Atypical appearance ± variable in number in aged samples
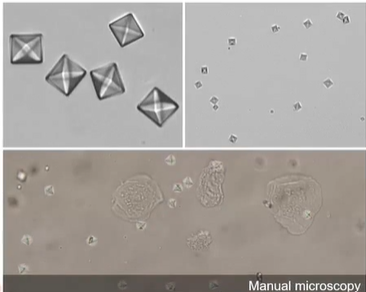
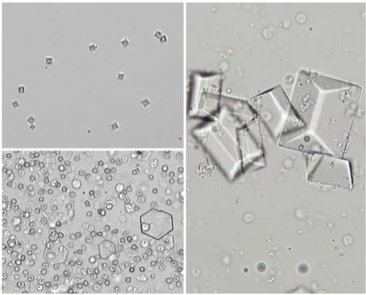
Calcium oxalate dihydrate
Clear, colorless, octahedral, “envelope”
Variable size
Typically found in acidic urine; may see in neutral and alkaline urine
Low numbers in healthy dogs and cats
Commonly a refrigeration artifact
May or may not see with oxalate urolith
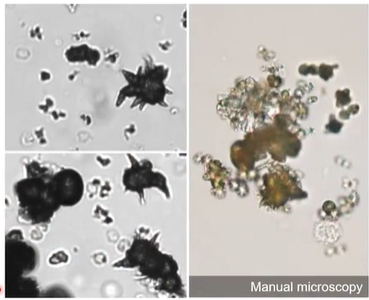
Ammonium biurate
Spherules with or without irregular projections
Brown-orange on manual microscopy
Neutral to acidic urine
Not common in healthy dogs and cats, except in dalmations and bulldogs
Associated with portal vascular shunts (congenital or acquired)
Bilirubin
Needle-like
Yellow to brown on manual microscopy
Low numbers may be normal in dogs, especially in concentrated urine
High numbers in nonconcentrated urine support cholestasis
Any presence in cats is abnormal
What are other crystal types?
Calcium oxalate monohydrate
Cystine
Cholesterol
Uric acid
Drug-related
Atypical presentations of reported crystal types
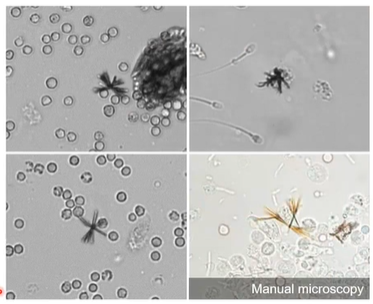
Two broad categories of bacteria
Rods
Cocci
Bacteriuria occurs most commonly due to…
Urinary tract infection
Contamination - during or after collection
What is the gold standard of interpreting bacteriuria?
Urine culture and sensitivity
Negative test does not rule out UTI
Positive test does not confirm UTI
True/False: When testing the accuracy of microscopic detection of bacteriuria in dogs, air-dried and stained bacterial cultures have higher sensitivity and specificity compared to wet mounts.
True
In male goats, cattle, sheep, swine and some camelids, the bulbourethral ducts empty into the urethra at the ischial arch. What forms here that makes retrograde catherization almost impossible?
A urethral recess
The urethral process of the male goat is a site where ________ _________ can block the urethra
Urinary calculi
How to position an animal for cystocentesis
• Position animal in either dorsal recumbency (pad back or use trough for comfort), lateral recumbency, or standing.
• To reduce the possibility of prior urination, have owner carry small dogs from car and have cats in a carrier for several hours prior to arrival at the clinic
• Equipment - 22 gauge 1-1/2” needle with a 5 ml syringe
• Soft massage to relax pet. Localize and stabilize bladder.
True/False: if a sample of urine is not obtained via cystocentesis on the first attempt, redirect the needle
False, change the needle before making another attempt and DO NOT REDIRECT as organs may be lacerated
What are some pros and cons to free catch collection method of urine?
– No trauma
– Frequent contaminants
– Not recommended when suspecting urinary tract infection
– Requires cooperation and timing! (Midstream preferred)
• Good to have device to hold cup
– Preferred when monitoring hematuria or suspect bladder neoplasia
Urinalysis - Physical examination
Color
Influenced by concentration, blood, myoglobin, methemoglobin, medications, bacteria, white blood cells
Clarity
Tubidity-indicates solid particles suspended in urine (e.g., crystals, cells, etc.)
Odors
Ammoniac - urease producing bacteria, cystitis
Putrid-severe bacterial infection
Sulfurous - Proteus infection
Sweet - ketones
Canine USG normal range
1.001 - 1.070
Adequate concentration - 1.025
Feline USG normal range
1.001 - 1.090
Adequate concentration - 1.035
Urinalysis - Glucose
– Glucosuria with hyperglycemia
• e.g. DM, stressed cats, postprandial, Ketamine
– Glucosuria without hyperglycemia-proximal tubular disease
• e.g. Fanconi, hypoxia, toxins, or reagent strip contam w/peroxide,bleach
– False neg. with ascorbic acid, tetracyclines
Urinalysis - Bilirubin
Degrades in presence of UV light
Canine low renal threshold
Feline high renal threshold
Urinalysis - Ketones
Volatile - evaporate quickly
False + in very pigmented or high USG/low pH
May accompany glucosuria
Urinalysis - Urobilinogen
Indicates bile duct is patent
Normal pH of urine
6-7.5
Effect of high protein diet on pH? Effect of plant diet on pH?
High protein diet lowers pH
Plant diet causes higher pH
What values on dipstick may be unreliable in animals?
USG, nitrite, leukocytes, urobilinogen
When do conversations about goals of care typically begin in veterinary medicine?
They often begin when the patient presents with a potentially life-threatening or life-limiting disease.
What role do goals-of-care conversations play throughout a pet’s illness?
They guide diagnostics, treatment, and interventions, and are revisited as needed during the illness.
What are two main barriers to frequent goals-of-care conversations in veterinary and human medicine?
Limited time and insufficient training.
What can be the consequence of not having goals-of-care conversations?
Unwanted interventions and decreased quality of life for the patient.
What communication protocols from human medicine help deliver bad news and guide goals-of-care conversations?
SPIKES, ABCDE, BREAKS, and Serious Illness Conversation Guidelines (SICG).
List the 5 common steps shared across communication protocols adapted for veterinary use.
1) Elicit owner’s understanding
2) Ask how much detail they want
3) Provide tailored information
4) Respond empathetically
5) Review care strategies and decisions.
Who adapted the SICG for veterinary medicine and why is it significant?
Katherine Goldberg; it includes prompts to identify care goals for seriously ill animals and improve client and veterinarian satisfaction.
How do checklists improve end-of-life conversations?
They reduce medical errors and ensure key elements are addressed, improving outcomes and satisfaction.
Why is self-care important for veterinary professionals during end-of-life conversations?
Engaging in serious conversations can be emotionally taxing; preserving mental and physical health supports long-term well-being and effectiveness in care.
What is Critical Incident Stress Management (CISM)?
A structured tool originally from disaster management, adapted to help veterinary professionals cope with traumatic events like euthanasia or treatment failure.
Who are the “first” and “second” victims in CISM terminology?
First victims: clients and their pets; second victims: veterinary professionals traumatized by adverse events.
What is the goal of Critical Incident Stress Management?
To restore mental and emotional health post-trauma and improve team cohesion, retention, and productivity.
What are the three steps of the CISM process?
Stress management, defusing, and debriefing through shared conversations with staff.
What factors influence how end-of-life conversations unfold in veterinary settings?
The veterinarian’s personality, experience, and communication skills.
What percentage of clients are emotionally affected by the death of their pet?
70%
What percentage of clients experience severe grief?
Up to 30%
What percentage of clients report guilt over euthanasia?
Approximately 50%
What contributes to client grief during pet loss?
Perception of professional support provided by the veterinarian.
How often are veterinarians present at a patient’s death compared to other health care professionals?
5 times more often.
What can help reduce stress, compassion fatigue, and burnout among veterinary staff?
Promoting self-care, work-life balance, collegial support, and a respectful practice culture.
What are common sources of discomfort for veterinarians in end-of-life discussions?
Lack of training, time constraints, practice culture, self-blame, feelings of failure, uncertainty, patient QOL concerns, emotional burden.
What are common reasons for client anxiety during end-of-life discussions?
Self-blame, anticipatory grief, impact on bond, uncertainty, emotional response, and pet's QOL
What are the general phases of grief?
Numbness → Searching/yearning → Disorganization/despair → Acceptance and integration
What do alumni surveys identify as the most important skills for veterinary practice success?
Communication skills and dealing with clients
What is a known gap in veterinary education regarding communication?
A skills gap between curriculum content and real-world communication needs.
What are the positive outcomes of skillfully conducted end-of-life discussions?
Validation of decisions, emotional support, improved satisfaction, better client retention.
What are potential negative outcomes of poor end-of-life communication?
Complicated grief, reduced client compliance, lower satisfaction, and increased litigation risk.
What are the core elements of end-of-life communication in veterinary medicine?
Delivering bad news, QOL assessment, euthanasia decision-making, discussing the euthanasia process, and grief support.
What model is used to structure end-of-life conversations in veterinary medicine?
The SPIKES model:
Setting
Perception
Invitation
Knowledge
Empathy
Summary
What is the literal meaning of the word “euthanasia”?
From Greek: “eu” = good, “thanatos” = death
What is a key premise of end-of-life animal care?
End-of-life animal care involves a series of events and discussions, each presenting communication challenges.
What are the key events and discussions involved in euthanasia?
Discuss options, discuss the euthanasia process, support during and after the procedure, and offer grief resources.
What are prominent risk factors associated with severe grief in clients?
Level of attachment, societal attitudes towards pet death, professional support from veterinary staff, and euthanasia.
What are some client expectations during end-of-life care?
Personalized treatment, respect, full medical explanation, kindness and attentive listening, and treating the pet as unique.
What role does the client play as the 'voice' of the animal/pet?
Share observations, concerns, and provide insight on quality-of-life.
What are common communication challenges in end-of-life care?
Discomfort with emotion, time constraints, guiding clients through difficult decision-making, non-medical euthanasia requests, and financial considerations.
What are some aspects of the veterinarian's experience with euthanasia?
Concerns about own emotions, personal level of distress, impact of client presence, unpredictability of client emotions, and repeated demand in practice.
What are the core communication skills needed by a veterinarian?
Non-verbal awareness, open-ended inquiry and reflection, and empathy.
What are nonverbal essentials for veterinarians?
Maximize time and privacy and set the stage.
What are examples of nonverbal cues that can effectively convey support?
Open posture, eye contact, and appropriate touch.
What tasks should a veterinarian perform during end-of-life discussions?
To review information, discuss quality-of-life issues, help clients shift perspective to quality-of-life, and validate difficulty in making the decision.
How can a veterinarian address grief?
Reminisce about the pet, provide grief education/pet loss resources, provide follow-up, and convey messages of validation.
What are some strategies for addressing grief in children?
Avoid euphemisms, include children in decision-making when appropriate, provide healthy modeling, and help children express emotions.
Proestrus
begins with first appearance of blood-tinged vaginal discharge and ends with first acceptance of mating
Estrus
period that bitch allows mating
Diestrus
two months following estrus (reproductive tract under influence P4 from corpora lutea)
P4
Collect plain red top not gel barrier tube
Time to breed and timing of parturition
Rise in P4 > 2.0 ng/mL (and P4 continues to rise), breed on days 3, 4, 5, 6 post surge
Due date predicted as day 65 ± 1 day following the pre-ovulatory serum progesterone rise/LH peak
Value of also running vaginal cytology (cornification)
Neonatal care
Suction, gently swing downward
Mucous trap
Doxapram sublingual
“Not so gentle” rubbing
Tube feeding: red rubber catheter (nose to last rib)
Cats dystocia reported incidence
3.3-5.8%
Dystocia is higher in what types of cats?
Higher in purebred cats
Stage 1 of labor
Onset of uterine contractions
Clinical signs: pant, pace, nesting
Stage 2 of labor
Delivery of fetus
Stage 3 of labor
Delivery of membranes
Clinical signs of dystocia
Female vocalizing
Dam showing signs of pain
Licking at vulva during contraction