Movement Science - Exam 2
1/144
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
145 Terms
One full gait cycle
starts with heel contact of one foot (0%) and ends with another heel contact of the same/ipsilateral foot (100%)
50% of gait cycle
heel contact of opposite/contralateral foot
Stance phase
60%
foot is on floor (early, middle, late subphases)
Swing phase
40%
leg is swinging forwards
Major determinants of gait result from
minimizing COM movement and minimizing overall energy expenditure
MD of Gait - Stance phase knee flexion
normal = 20 degrees
minimizes vertical movement of COM by keeping body low
MD of Gait - Pelvis list (hip drop)
normal = <1 inch of lateral translation
as foot impacts w/ground - pelvis drops downward on opposite side
minimizes vertical movement of COM
Hip drop and posterior hip rotation are energy efficient movements because they
reduce the movement of COM
MD of Gait - Posterior pelvic rotation
rotation of pelvis posteriorly helps reduce energy expenditure by minimizing the movement of COM
reduces the “braking phase” of gait
MD of Gait - Pronation of the
subtalar joint
MD of Gait - 1st ray dorsiflexion (big toe/1st MTP)
normal = >60 degrees during walking
crucial during toe-off phase of gait
crucial for windlass effect of plantar fascia and subsequent support of foot during weight-bearing activities
MD of Gait - Ankle dorsiflexion
normal = 40 degrees
only need 10-20 degrees during normal gait
What does the talus function as in ankle dorsiflexion during gait
as a frictionless ball bearing (b/c 70% of it is covered with cartilage)
MD of Gait - Gluteal friction
essential for controlling motion at the knee and further down the kinetic chain
upper fibers - lever arm controlling frontal plane motion
lower fibers - control sagittal and transverse plane motions
Gait cycle of running
contact, midstance, propulsion
**Extra phase = double float phase
Most of running injuries are a result of
overload or “chronic overuse”
The 1st thing you should look at when assessing a running injury is
the individual’s training logs and their running experience
People w/low arches
pronate more rapidly through larger ranges of motion
exhibit more SOFT TISSUE injuries
People w/high arches
hit the ground harder and pronate through very small ranges
exhibit more BONY injuries
Who has the 1st highest injury prevalence? 2nd?
1st = people with LOW arches
2nd = people with HIGH arches
Can stretching be generalized as a recommendation to reduce injury risk for running injuries
NO! (choose what pre-exercise warm-up is right for the patient)
What impact does strength training have on load capacity, stress, and strain on joints
increases load capacity
reduces stress and strain on joints
**Runners who strength train exhibit reduced injury rates
Neurodynamics
communication btw different parts of the NS and its relationship to the MSK system
**ability of nerves to move freely and independently of other tissues
Intervention of neurodynamics
mobilization of the NS as an approach of physical treatment
Neurodynamic assessment
evaluates the length and mobility of the NS
How do neurodynamic assessments influence pain physiology
via the mechanical properties of neural tissues and non-neural structures surrounding the NS
Role of the nerve in neurodynamics
helps muscle move (motor), transmits sensory feedback, reflex, autonomic functions
Nerve symptoms and what they may be manifested as
symptoms - numbness, tingling, burning, pain
manifested as - muscle weakness, atrophy, headaches
Clinical neurodynamics
clinical application of mechanics and physiology of the NS as they relate to each other and are integrated with MSK system
Neurodynamic test
series of intentionally sequence body movements that produces mechanical and physiological events in the NS according to the movements of the test
Neurogenic pain
pain that is initiated or caused by a primary lesion or dysfunction in the PNS or CNS
Mechanical functions
tension, compression, movement
Positive neurodynamic test
provocation or reproduction of symptoms
Physiologic functions/key components being tested in neurodynamic testing (interrupt the most!)
intraneural blood flow, impulse conduction, axonal transport, inflammation, mechanosensitivity
Innervated tissues
any tissue innervated by the NS (skin, muscle, tendon…)
Three primary mechanical functions that the NS must successfully execute to move normally
withstand tension
slide in its container
be compressible
Effects of tension on intraneural blood flow
8% elongation - flow of venous BF from nerves starts to diminish
15% elongation - all circulation in/out of nerve is obstructed
Effects of compression on intraneural blood flow
nerves that have been previously compromised by compression may be more sensitive to smaller pressure producing neuropathic symptoms
Neurodynamic sequencing
performance of a set of particular component body movements so as to produce specific mechanical events in the NS
Neurodynamic sequencing - greater strain in nerves occurs where
the force is applied 1st and most strongly
Sequence of movements influences the
location of symptoms
Structural differentiation is performed with
ALL neurodynamic tests
Structural differentiation is achieved by
moving the neural structures in the area in question without movement the MSK tissues in the same region
The NS is emphasized in structural differentiation when the relevant neural structures are moved without
moving the adjacent MSK structures
You use structural differentiation to ______ your diagnosis
confirm
Events occur in the following order during a joint movement
taking up of slack early in the range
rapid neural sliding in the mid-range
tension builds in the NS as nerve movement diminishes at end range
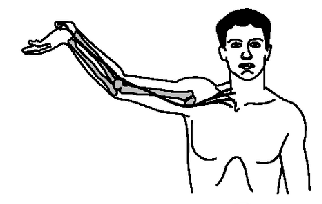
ULNT1 tests what nerve and roots
median N
C5-7
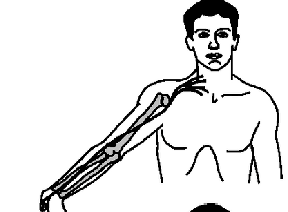
ULNT2 (“supination”) tests what nerve and roots
median N
C5-7
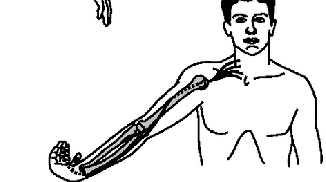
ULNT3 (“pronation”) tests what nerve and roots
radial N
C5-T1
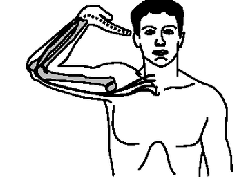
ULNT4 (“goggles on”) tests what nerve and roots
ulnar N
C8-T1
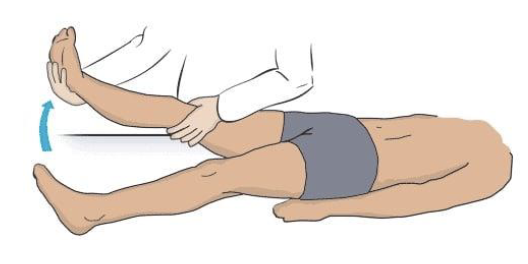
LLNT - Straight leg raise tests what nerve and roots
sciatic N
L4-S2
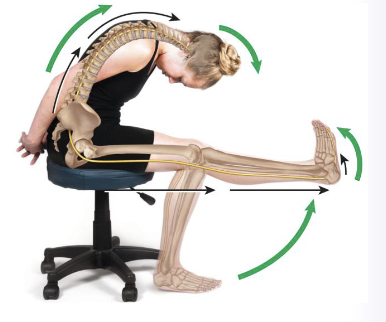
LLNT - Slump test tests what nerve and roots
sciatic N
L4-S3
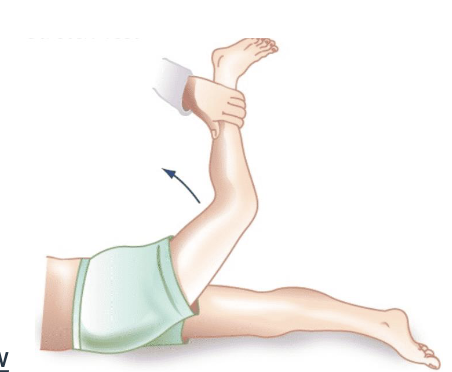
LLNT - Femoral N stretch test (prone knee bend test) tests what nerve and roots
femoral N
L2-4
Which of the lower limb neurodynamic tests is the most sensitive for L5/S1
slump test
Which of the lower limb neurodynamic tests is one of the most reliable tests for mid-lumbar nerve root impingement
femoral N stretch test
Overt signs
observable and explicit responses during clinical assessments related to the NS
Structural differentiation gives what type of result
neural result
Covert signs
refer to subtle findings that may not cause overt symptoms but can still provide valuable diagnostic information
**doesn’t reproduce pt clinical pain
Sliders (nerve flossing)
produces a sliding movement of neural structures relative to their adjacent tissues
**performed by placing tension (elongating) one end of the nerve and reducing tension (shortening) the other end of the nerve in an alternating pattern
Tensioners
produces an increase in tension in neural structures
relies on natural viscoelasticity of the NS but does not pass the elastic limit
**performed by placing tension (elongating) BOTH ends of the nerve
Muscle imbalances lead to
tissue changes that may result in inappropriate patterns of movement
Muscle imbalances are commonly caused by
sedentary lifestyle
What does overuse or underuse of muscles lead to
overuse - shortening/tightening of tonic muscles
underuse - weakening/inhibition of phasic muscles
Global vs local stabilizers
Global - large, long superficial muscles that span two or more joints
Local - small, short deep muscles that span two or more joints
Global and Local stabilizer roles
stabilize and static proprioceptive feedback
**contraction creates tension to introduce stability
Global vs Local movers
Global - large, long superficial muscles that span two or more joints
Local - small, short deep superficial muscles that span two or more joints
Global and Local mover roles
movement and dynamic proprioceptive feedback
**contraction creates movement within a specific pattern
Three types of neuromuscular phenomena that can lead to muscle imbalances
reciprocal inhibition
synergistic dominance
arthrokinetic inhibition
Reciprocal inhibition
occurs when a tight muscle decreases the neural drive to its functional antagonist
**leads to predictable injury patterns
Synergistic dominance
occurs when synergists and stabilizers take over for a weak or inhibited prime mover
Arthrokinetic inhibition
occurs when a muscle is inhibited by joint dysfunction or the capsule that crosses the joint
What things are necessary to ensure proper activity of skeletal muscles
exposure of the human body to gravity forces
routine stability functions
Deficit locomotor system stability triggers
compensatory mechanism - stabilizing function is overtaken by the mobilizing muscles (decreases flexibility)
Upper Crossed Syndrome - Tight/Overactive
upper traps and levator scapulae
pec major/minor
Upper Crossed Syndrome - Weak/Underactive
deep cervical neck flexors
middle and lower traps
Postural imbalances in Upper Crossed Syndrome
forward head posture
increased cervical lordosis and thoracic kyphosis
elevated and protracted (rounded) shoulder
rotation/abduction and winging of scapulae
Lower Crossed Syndrome - Tight/Overactive
thoracolumbar extensors
hip flexors
Lower Crossed Syndrome - Weak/Underactive
abdominals
gluteal muscles (maximus)
Postural imbalances in Lower Crossed Syndrome
thoracic hyperkyphosis
lumbar hyperlordosis
anterior pelvic tilt
slight hip and knee flexion
Key point in MDT
We don’t FIX patients - we ASSIST patients and TEACH them how to self-manage
Primary goal of MDT
identify if pts are appropriate for mechanical therapy or need referral to another provider
Keys to the successful use of MDT
meticulous assessment
emphasis on educating the pt in self-management
appropriate use of progression of forces
Directional preference
direction of loading that reduces or centralizes symptoms and/or improves function
Centralization
PROCESS in which distal symptoms move proximally and remain improved after loading strategies
Centralizing
DURING the application of the loading strategy distal symptoms are being abolished
Centralized
AFTER the application of the loading strategy all distal symptoms are abolished, and only centralized back pain remains
Peripheralization
symptoms move distally or worsen distally with a given direction
End-range and WHY it matters
the final available range with a distinct barrier
often required for meaningful change
Progression of forces (least to most)
pt generated forces
pt overpressure
clinician overpressure
clinician mobilization techniques
manipulation
Average starting point for most patients
10x every 2-3hrs
Postural syndrome
pain only after sustained end-range posture
normal ROM
minimal change with reps
Classification of Postural Syndrome
intermittent local pain
no movement loss
no effect w/repeated movements
pain produced w/sustained static positioning
Treatment of Postural syndrome
micro-break strategies (30-60sec movement breaks every 20-40min)
Dysfunction syndrome (tissue)
local, consistent end-range pain
range loss in that direction
slow remodeling over weeks
Presentation of Dysfunction syndrome
decreased ROM
pain at end ROM
normal load on shortened tissues leads to symptoms
Treatment of Dysfunction syndrome
repeated end-range loading into the limited direction (load/time)
motto is no pain, no gain!
What is the MC syndrome
Derangement syndrome
Derangement syndrome
variable symptoms
possible distal pain, obstructed range
potential for rapid change with the correct direction
What is the “Great imposter” in Derangement syndrome
onset will go from fully functional to total disability
Presentation of Derangement syndrome
typically decreased ROM or obstruction