2: Professional nursing practice— Legal and ethical frameworks
Legal aspects of nursing practice
The legal framework around nursing practice is based on the common laws and Acts of the Parliament relevant to healthcare professionals.
Functions of law in nursing
It provides a framework for establishing which nursing actions in the care of individuals are legal.
It differentiates the nurse’s responsibilities from those of other health professionals.
It helps establish the boundaries of independent nursing action.
It assists in maintaining a standard of nursing practice by making nurses accountable under the law.
Nurses have the legal responsibilities common to all members of society particularly in respect of the provision of safe and effective nursing care, the health of the community, and the employer and employee obligations of the nursing profession.
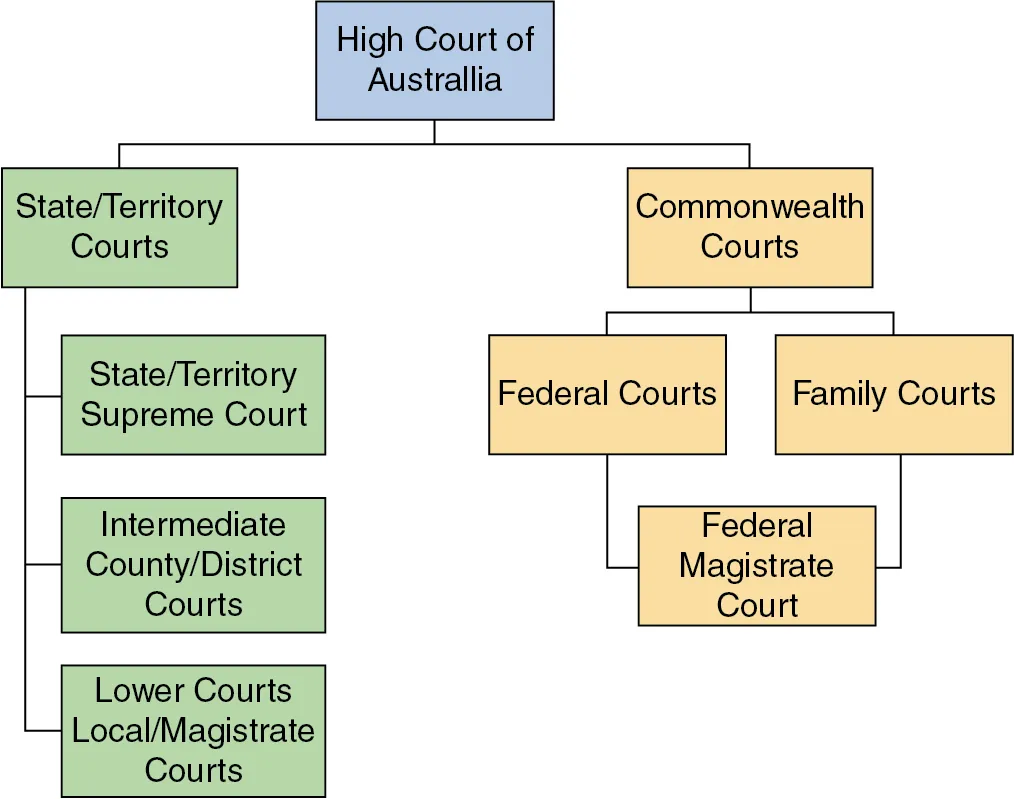
Common Law System
Common Law — the body of law made by judges as a result of decisions in cases that come before the courts; often referred to as case law.
These decisions form precedents (legal principles) and can then be applied in similar cases.
Types of Law
Criminal Laws — concerned with offences against people and their property.
Violation of it is called a “crime,”; and it sanctioned by some form of punishment.
Civil Laws — concerned with the legal disputes between people and/or organisations.
Concerned with differences over personal or property issues that people are unable or unwilling to resolve themselves.
Violation will be required to pay monetary compensation to the person alleging personal or property loss/damage.
Torts — civil wrongs committed by someone against a person or their property, resulting in claims for compensation from the person responsible for causing injury or damage
Acts of Parliament
The parliament has the power to make or unmake laws.
Statutory Laws — laws made by the parliament; also called “legislation.”
Health Practitioner Regulation National Law Act 2009 — aims to create a national registration and accreditation scheme for registered health practitioners.
The regulations accompanying this Act is administered by AHPRA.
Acts may differ from states and territories—nurses are usually bound by the laws of the place they reside.
The Employer
Healthcare institutions as employers are legally responsible for the acts committed by all employees during the course of their employment.
Doctrine of Vicarious Liability — renders an employer vicariously liable for an employee’s actions committed during the course of employment.
Nurses have personal liability for activities carried out in the line of work and must ensure that they work within the scope of employment.
NMBA requires that nurses and midwives only practice when they are covered by an appropriate professional indemnity insurance (PII) policy; and they must declare each year that they have complied with this requirement.
It is the responsibility of healthcare employers to ensure that:
Employees possess the required qualifications, registration and level of competence.
All legal requirements are met, including valid contracts of employment, public liability and indemnity insurance is in place.
Safety standards are observed in relation to standards of care, buildings and equipment.
Discrimination and Human Rights
Workplaces are required by laws to create a workplace free from discrimination , harassment and bullying.
It is essential for healthcare employers and their employees to understand individual and collective rights and responsibilities under human rights and anti-discrimination laws that operate in the jurisdiction.
Laws that operate at federal level | Laws that operate at state and territory level |
• Age Discrimination Act 2004 | • Discrimination Act 1991 (ACT) |
• Australian Human Rights Commission Act 1986 | • Anti-Discrimination Act 1977 (NSW) |
• Disability Discrimination Act 1992 | • Anti-Discrimination Act 1996 (NT) |
• Racial Discrimination Act 1975 | • Anti-Discrimination Act 1991 (QLD) |
• Sex Discrimination Act 1984 | • Equal Opportunity Act 1984 (SA) |
• Anti-Discrimination Act 1998 (TAS) | |
• Equal Opportunity Act 2010 (VIC) | |
• Equal Opportunity Act 1984 (WA) | |
Enforced by the Australian Human Rights Commission | Enforced by state and territory equal opportunity and anti-discrimination agencies |
Unlawful discrimination is said to occur ‘when a person, or a group of people, is treated less favourably than another person or group because of their background or certain personal characteristics’.
Two Forms of Discrimination
Direct discrimination — occurs when someone is treated unfairly because of a personal characteristic; people make unfair assumptions about what people with certain personal characteristics can and cannot do.
Indirect discrimination — occurs when an unreasonable requirement, condition or practice is imposed that disadvantages a person or group because of a personal characteristic.
Universal Declaration of Human Rights — an expression of fundamental values shared by all the members of the international community and has a significant influence on development of the human rights laws of countries.
Human Right
Description
Right to Life
Every individual has the inherent right to life, and no one shall be arbitrarily deprived of their life.
Right to Liberty and Security
Every person has the right to personal freedom and security without the threat of arbitrary arrest or detention.
Freedom from Torture and Inhumane Treatment
No one shall be subjected to torture, cruel, inhumane, or degrading treatment or punishment.
Freedom of Thought, Conscience, and Religion
Everyone has the right to freedom of thought, conscience, and religion, including the freedom to change religion or belief.
Freedom of Expression
Everyone has the right to express their opinions and ideas without fear of interference or repression, including freedom of the press.
Right to a Fair Trial
Everyone has the right to a fair and public hearing by an impartial tribunal in matters of criminal or civil justice.
Right to Privacy
Every individual has the right to privacy in their personal life, home, family, and correspondence, free from arbitrary interference.
Freedom from Discrimination
All individuals are entitled to equal rights and freedoms without distinction based on race, color, sex, language, religion, or other status.
Right to Work
Everyone has the right to work, to choose their employment freely, and to be protected from unemployment or exploitation.
Right to Education
Every individual has the right to free, compulsory elementary education and access to higher education based on merit.
Right to Freedom of Movement
Every person has the right to move freely within their country and to leave any country, including their own, and return.
Right to Asylum
Everyone has the right to seek asylum from persecution in other countries.
Right to Participate in Government
Every individual has the right to take part in the government of their country, directly or through freely chosen representatives.
Right to Social Security
Everyone has the right to social security and the entitlement to necessary social services in the event of unemployment, illness, or old age.
Right to an Adequate Standard of Living
Every person has the right to an adequate standard of living, including adequate food, clothing, housing, and medical care.
Right to Marriage and Family
Adults have the right to marry and to found a family, and such relationships are to be entered into with the free consent of both partners.
Right to Rest and Leisure
Everyone has the right to rest, leisure, and reasonable limitations on working hours, including paid holidays.
Right to Own Property
Every individual has the right to own property alone or in association with others, and no one shall be arbitrarily deprived of their property.
Freedom of Assembly and Association
Everyone has the right to peacefully assemble and to form or join groups, including trade unions, for the protection of their interests.
Additional Human Rights in Australia
Right
Description
Rights of Indigenous People
Indigenous Australians have the right to self-determination, land and cultural preservation, equal access to services, and participation in decision-making processes. Initiatives like "Closing the Gap" aim to address inequalities in health, education, and employment.
Women’s Rights
Women in Australia are entitled to equality under the law, including protection from gender-based discrimination and violence. This encompasses equal pay, reproductive rights, maternity leave, and participation in all sectors of society.
Children’s Rights
Children in Australia are entitled to protection, care, education, and the right to live in a safe environment. Child protection laws ensure the welfare and rights of children, and Australia is a signatory to the UN Convention on the Rights of the Child.
Rights of People with a Disability
People with disabilities are protected under the Disability Discrimination Act 1992 and have the right to full participation in society, including access to education, employment, healthcare, and public services. The National Disability Insurance Scheme (NDIS) supports these rights.
Rights of Older Persons
Older Australians have the right to live with dignity, respect, and autonomy. Age discrimination is prohibited, and older people are entitled to proper care, social services, and protection from elder abuse.
Rights Regarding Sexual Orientation, Gender Identity, and Intersex People
LGBTIQ+ individuals have the right to equality, protection from discrimination, and the right to marry. Laws in Australia ensure protection against discrimination based on sexual orientation and gender identity under the Sex Discrimination Act 1984. Intersex people have rights to bodily autonomy and protection from unnecessary medical procedures.
Health professionals’ own attitudes or personal bias and lack of understanding and knowledge about sexual orientation and gender identification can create barriers to quality care.
This can lead to people delaying seeking medical treatment, experiencing poor levels of care, not openly sharing all their health concerns or withholding vital health information, and even being reluctant to keep up with follow-up care.
Nursing Regulation
Regulation — any government measure enforced to seek control or change the behaviour of individuals or a group of people in society.
Nursing profession in AUS is regulated by AHPRA under the NRAS for health professions.
The primary function of the nursing regulatory authority is to protect the health and safety of members of the public by ensuring that nurses are competent and fit to practise.
Three Nursing Classifications
Nurse Practitioner
Registered Nurse
Enrolled Nurse
It is unlawful for a person to represent themselves as a nurse or use the title ‘nurse’ if they do not meet the requirements for practice.
All courses leafing to registration of EN, RN, or NP, are accredited though the ANMAC and NMBA—and these courses must be taken in an accredited education provider.
Annual practicing certificate or renewal of registration must be obtained from nursing regulatory authority to continue to practice as a nurse.
Ensure registration and enrolment fees are paid each year.
Demonstrate competence fit for practice.
Nursing regulatory authority is empowered to deregister nurse in certain circumstances.
Education providers must ensure relevant details of students are provided to the regulatory authority on commencement of study.
Student register is important to protect the health and safety of members of the public.
Scope of Practice
The scope of practice of a nurse is legally defined, determined by the level to which nurses are educated or their professional qualification, procedures and actions that they are competent to perform and permitted by law.
A nurse must only undertake those clinical duties or tasks if they have completed the necessary educational preparation to be able to do so.
Only ENs who have completed their education in the medication administration unit can administer medicines.
Factors that determine the scope of practice for a nurse are:
The nurse’s level of training and demonstrated competence.
The nurse’s context of practice and level of employment.
State and Commonwealth legislation.
The employer’s policy framework.
Professional Boundaries
Professional boundaries in nursing are the parameters within which nurses practise, to ensure that the limits of professional and therapeutic relationships with individuals in their care are not crossed.
When a nurse crosses professional boundaries then that action is deemed as unprofessional conduct or behaviour and can result in disciplinary action.
It is critical that nurses as healthcare professionals recognise the lines of separation from the person in their care and apply sound judgment in managing issues around professional boundaries.
Common Examples of Professional Boundary Concerns
Sexual misconduct
Dual relationships
Self-disclosure
Gifts and favors
Financial Arrangments
Confidentiality breaches
Boundary violations
Exploitation
Abuse of power
Inappropriate physical contact
Discrimination
Code of Conduct for Nurses — prescribed by the NMBA, these are sets standards for expected practice and behaviour of nurses and it describes what constitutes the limits of professional behaviour in nurse–individual relationships.
Continuing Professional Development
Continuing nursing education is an essential standard for nursing registration.
Nurses as health professionals are expected to have specialist and good general nursing knowledge related to their areas of practice.
Nurses are required to undertake ongoing education. These may include:
Further postgrad studies
Specialist courses or competencies
Through nursing journals
Participating in professional and industrial organisations
Attending conferences and seminars
Contributing to development of policies and procedures
Areas of Legal Liability in Nursing
Legal Liability — a person is subject to certain legal obligations.
Nurses have a responsibility, to themselves and the person in their care, to refuse to perform an activity if:
They are asked to do something that is beyond the legal and professional scope of their role.
They have not been prepared to perform a function safely.
Directions are unclear, unethical, illegal or against the policies of the healthcare agency.
The nurse as a healthcare professional must work within their scope of practice and have a responsibility to be aware of the legal principles and concepts that impact on professional practice.
Contracts
Contract — an agreement between parties that is legally enforceable because of mutuality of agreement and obligation.
It gives rise to rights and obligations that are protected and enforced by the law.
Contracts can be written or implied through actions or agreements.
Individuals implicitly enter contracts with healthcare agencies when admitted for treatment.
Nurses have employment contracts with their employers, outlining rights and obligations.
Industrial awards set wages and conditions for specific groups of employees.
Nurses working through agencies have contracts with the agency and the healthcare facility.
Standards of Care
Standards of Care — the guidelines or criteria for the work performance or level of care that a nurse is expected to deliver.
Nurses must be familiar with standards and understand their scope of practice.
Duty of Care — taking reasonable measures to protect, or at least not cause foreseeable harm, to another person or their property.
Sources of Standards:
Enrolled Nurse Standards for Practice (NMBA)
Healthcare agency policies and procedures
Government policy documents
Professional organization guidelines
Evidence-based practice guidelines
Relevant regulations
Negligence
Negligence — a tort and means a civil wrong that relates to incidents where a person who suffers injury through a negligent act or omission can seek compensation from the person responsible for the negligence.
If a nurse gives care that does not meet accepted standards, the nurse may be held liable for negligence.
It also involves failing to do something that should have been done, or doing something that should not have been done.
In the event of alleged negligence against a nurse, the responsibility or the onus for proving negligence is with the plaintiff or the person alleging negligence. A plaintiff must prove four elements to succeed in an action for negligence:
That the nurse owed the plaintiff a duty of care.
That the nurse breached this duty of care.
That the plaintiff suffered injury or harm as a result of the breach.
The harm was foreseeable.
Types of negligence that result in breach of duty of care and malpractice
Failure to follow standards of care
Failure to use equipment safely
Failure to communicate adequately
Failure to document adequately
Failure to assess and monitor adequately.
Defamation
Defamation of character — any communication, spoken or written, about an individual that injures their reputation.
Libel — defamation when the communication is written.
Slander — defamation when the communication is spoken.
All individuals have a right to privacy and confidentiality in healthcare settings.
Nurses must protect the personal and professional reputations of colleagues.
Avoid discussing or documenting information about individuals or colleagues in a way that could harm their reputation, especially gossiping.
If concerned about standards of care, raise concerns through proper channels and maintain confidentiality.
Ensure that written statements about individuals are objective and avoid defamatory language.
Examples of Defamation in Nursing Practice
Writing a false statement accusing a nurse of providing substandard care.
Making a false or misleading entry in a patient's medical record that could damage their reputation.
Publishing a false article or blog post that defames a nurse's character or professional reputation.
Disclosing confidential information about a colleague or patient in a way that harms their reputation.
Making false accusations of misconduct against a nurse, such as negligence or theft.
Verbally accusing a nurse of incompetence or misconduct.
Spreading false or malicious rumours about a nurse's personal or professional life.
Making negative or offensive comments about a nurse's abilities or character.
False Imprisonment
False imprisonment — the wrongful deprivation of a person’s freedom of movement, such as restraining or detaining a person against their will.
Circumstances where a person may need to be restrained:
to protect them from injury,
protect others from being injured, or
prevent damage of property.
Restraint must only be performed as last resort, if it’s included in their care plan, and authorised by the medical officer.
Written authorisation by a medical officer is generally required for the application of a restraint.
There must be a medical officer’s order for the restraint which states the reason and time period. The order must be reviewed daily.
Examples of False Imprisonment in Nursing
Physically restraining a patient without a valid medical reason or appropriate authorization. This could involve using restraints such as bed rails, belts, or medications.
Restricting a patient's movement or freedom without a legitimate medical reason, such as isolation for infection control.
Obstructing a patient's attempts to leave the hospital or facility, even if they have been discharged.
Withholding a patient's personal belongings or preventing them from accessing their belongings.
Threatening or coercing a patient into staying in the hospital or limiting their freedom.
Assault and Battery
Assault — occurs when a threat to carry out unwanted and unlawful contact on another person is made, thereby causing that person to fear for their safety.
Threatening a patient with physical harm, such as saying, "I'll hurt you if you don't cooperate."
Using intimidation or coercion to make a patient comply with a request, such as threatening to withhold medication or restrict their movement.
Brandishing objects or instruments in a threatening manner, such as shaking a fist or holding a syringe.
Battery — involves the direct, intentional and uninvited application of physical contact to another person’s body that may or may not cause harm.
Touching a patient without their consent, even if the intent is not harmful. This can include unnecessary or excessive physical restraint.
Administering medication to a patient without their informed consent.
Performing medical procedures on a patient without their consent, such as injections or surgery.
Using excessive force when restraining or handling a patient, causing them physical pain or injury.
In nursing practice, a nurse could intentionally or unintentionally commit an act of assault if they did anything in terms of touching someone in their care without consent.
Consent
Consent — an agreement between two parties; usually implied or expressed.
Implied consent — when a person's actions or words indicate that they agree to a procedure or treatment.
If nurse requests a person in their care to hold out their arm so that they can measure their blood pressure, and the person does so, then they have implied their consent to that procedure.
Expressed consent — when a person verbally or in writing agrees to a procedure or treatment.
The patient verbally expressing their agreement to the surgical procedure, then the doctor provides a consent form for the patient to sign, documenting their consent in writing — which serves as a legal evidence of patient’s agreement.
Informed consent — it is given when the person is provided with adequate information about, and understands, the procedure to which they are consenting.
The person consenting understands the risks and benefits involved as well as the actual procedure.
Informed consent for medical and surgical treatment is documented on a consent form, which is a legal record.
Regardless of the form in which consent is given it must be valid. For consent to be valid it must be voluntarily and freely given.
Elements of Valid Consent
That consent is given freely and voluntarily without coercion.
That the person giving consent is fully informed.
That the person giving consent is competent to make decisions.
Legal consent can only be given by a competent adult.
If the person is unable to give consent specific legislation enables others to give consent on the behalf of that person.
Parents and guardians can provide consent for children and minors.
Mental health legislation allows non-consensual treatment of mentally ill persons.
In circumstances when it is difficult to obtain consent, if the person is unconscious, consent can be obtained from someone legally authorised to give consent on behalf of them.
If the situation arises that the person requires emergency treatment and it is impossible to obtain consent from that person, an authorised person may give consent.
In the event of life-threatening situations, the overriding duty of care negates the need for consent and legislation enables medical intervention without consent.
Right to Withhold or Revoke Consent
A person has the right to withhold or revoke their consent at any time provided they are competent to do so.
In this event they must be informed about any detrimental consequences of refusal.
The event must be reported immediately to the nurse in charge and the medical officer, and be documented.
Right to Receive Information
A person receive care has the right to receive information regarding their treatment, care, or any other procedures.
Nurses as healthcare professionals are required to provide appropriate and sufficient information to the person in their care in accordance with the charter of healthcare rights and principles of informed consent.
Nurses must able to answer the person’s questions in an honest and helpful way in relation to their care.
National Safety and Quality Health Service Standards ‘Partnering with consumers’ standard identifies providing required and necessary information as essential to ensuring safe and high-quality care.
It sets out the requirements for information that should be communicated to individuals by the healthcare service or providers to ensure informed consent and assist decision making and care planning.
Confidentiality and Privacy
Confidentiality — restrictions upon private information revealed in confidence, with an understanding that the information will not be disclosed to others.
Privacy — the ownership of one’s own body or information about one’s self.
Nurses have legal and ethical obligation not to disclose confidential information acquired from individuals under their care, unless needed.
Information that are classified as confidential:
Patient Information:
Personal Identifiers: Name, address, date of birth, social security number, medical record number.
Medical History: Diagnosis, symptoms, treatment plans, test results.
Treatment Records: Medications, procedures, surgeries, allergies.
Genetic Information: Family history, genetic testing results.
Mental Health Records: Diagnoses, treatment plans, counselling notes.
Sexual History: Sexual orientation, sexual activity, sexually transmitted infections.
Healthcare Provider Information:
Licensure and Credentials: Professional licenses, certifications, qualifications.
Employment Records: Job titles, salary, performance evaluations.
Disciplinary Actions: Any disciplinary actions taken against the healthcare provider.
Other Information:
Research Data: Data collected for research studies, including patient identifiers.
Billing and Insurance Information: Patient insurance details, billing records, financial information.
Quality Assurance Data: Information used for quality improvement and risk management purposes.
Information concerning a person’s health is protected by law.
Nurses are responsible for protecting records from unauthorised people.
Information provided to other treating healthcare professionals should be kept to a need-to-know basis, and consent from the person must be obtained if a third party requires access to their healthcare records.
A person’s right to privacy must be respected and their affairs must not be discussed with other healthcare patients, non-professional staff or members of the general public.
Appointed guardians or parents can have access to health information.
Nurses should exercise discretion in their off-duty hours and avoid discussing work-related matters publicly.
Nurses must be aware of the social media policies of the NMBA and their employer.
If approached at any time by a representative of an organisation, press, radio or television, a nurse should refrain from giving information but should refer the enquiry to the administrative section or other appropriate department of the healthcare agency.
Be alert to situations where individuals disclose sensitive information and act appropriately.
Mandatory Reporting
Nurses are legally mandated to report suspected cases of child abuse or neglect.
Mandatory reporting aims to protect children and ensure their safety.
Specific requirements for mandatory reporting may differ between states and territories.
Nurses must report suspected cases of physical, emotional, sexual abuse, or neglect.
Two Types of Duties under which nurses are required to report suspected child abuse and neglect:
Duty of Care — This duty arises from the relationship between the nurse and the child. As healthcare professionals, nurses have a responsibility to protect the well-being of children in their care.
Duties of Professional / Industrial Policy — These duties are outlined in professional codes of conduct, workplace policies, or legislation.
Situations that require mandatory reporting
Certain deaths
Injuries involving firearms
Diseases that threaten public health
Medical conditions that may result in harm to public
Professional misconduct
All crimes
Abuse and sexual abuse of children
Abuse of elderly
Domestic violence (in Northern Territory).
Grounds for reporting suspected abuse and neglect
A person tells you that a child has been abused or neglected
A child tells you that they have been abused or neglected
Your own observations give you reason to believe that a child has been abused or neglected.
While there is no specific mandatory reporting law for elder abuse, the Aged Care Amendment (Security and Protection) Act 2007 requires reports to the Office of Aged Care Quality and Compliance.
Mandatory reporting is an AHPRA requirement for all registered health professionals, their employers, and education providers.
Nurses must report suspected cases of elder abuse that involve "notifiable conduct.”
Practised the practitioner’s profession while intoxicated by alcohol or drugs
Engaged in sexual misconduct in connection with the practice of the practitioner’s profession
Placed the public at risk of substantial harm in the practitioner’s practice of the profession because the practitioner has an impairment
Placed the public at risk of harm because the practitioner has practised the profession in a way that constitutes a significant departure from accepted professional standards.
Documentation
A nurse is required to document information about the person on nursing care plans, progress notes, flow charts and any other care-specific documents used in the healthcare facility.
Accurate and concise documentation is essential for communication, legal proceedings, and defending nursing practice.
The NSW Health policy directives principles for creation, management and disposal of healthcare records:
Individual records
Completeness and comprehensiveness
Quality improvement, review, evaluation, and research
Continuity of care
Responsibility for documentation
Durability
Confidentiality
Timeliness of documentation
Storage and Securty
Authenticity
Ownership
Retention
Relevance
Access
Disposal
Reporting of Adverse Events and Clinical Incidents
Nurses have a legal and ethical obligation to report accidents and incidents.
Healthcare agencies use specific forms or electronic systems for incident reporting.
Incident reports help improve quality of care, evaluate practices, and identify safety risks.
Incident reports can be used as evidence in legal proceedings.
Reports must be factual, clear, concise, and objective.
Examples of clinical incidents that must be reported:
Procedures involving the wrong patient or body part resulting in death or major permanent loss of function
Suicide of an inpatient or serious self-harm, suicidal behaviour
Retained instruments/material after surgery requiring re-operation/further surgical procedures
Intravascular gas embolism resulting in death or neurological damage
Haemolytic blood transfusion reaction resulting from ABO incompatibility
Medication error resulting in death of a patient
Maternal death or serious morbidity associated with labour or delivery
Infant discharged to wrong family or infant abduction
Adverse events resulting in serious patient harm or death
Fetal complications associated with healthcare delivery
Delay in recognising or responding to clinical deterioration
Complications of resuscitation or anaesthetic management
Complications of surgery
Complications of an inpatient fall
Infection control breaches
Unexpected death of a mental health patient/consumer
Absconding of any mental health patient/consumer
Therapeutic equipment failure/medical device incident
Hospital-acquired pressure injuries
Clinical deterioration of a mental health patient resulting in harm (physical, verbal or sexual) to staff, other patients or other persons
Inappropriate treatment/s.
Witnessing Wills
While healthcare professionals can assist individuals in making wills, they are generally not allowed to act as witnesses to the document. This is to avoid potential conflicts of interest and to ensure the validity of the will.
Reasons for the Restriction:
Nurses may have a personal relationship with the patient or may be involved in their care, which could potentially influence their judgment or impartiality.
Witnessing a will can blur professional boundaries and create potential ethical dilemmas.
In many jurisdictions, there are specific legal requirements for witnesses to a will, such as being unrelated to the testator and not benefiting from the will.
Alternative Arrangements:
Healthcare facilities often have designated staff members, such as legal or administrative personnel, who can act as witnesses to wills.
Patients can ask family members or friends to witness their wills.
It is generally recommended that individuals obtain witnesses who are unrelated to them and have no personal interest in the will.
Coroner’s Court
Coroners investigate unexpected or violent deaths. Their primary task is to establish the following facts in the event of a coronial investigation:
That death occurred
The identity of the deceased
The date, place, manner and cause of death
The cause of fires or explosives if relevant.
Legislation governing coroners' roles is consistent across Australian states and territories.
Inquests can be conducted years after a death.
Nurses may be called to give evidence in coroners' inquests.
Nurses should seek legal advice before making statements to police or appearing in court.
Nurses are typically represented by their healthcare agency's legal representatives.
Nurses can also choose to be represented by their professional nursing organization.
Examples of reportable deaths
The identity of the person who has died is unknown
The death of the person was violent or unnatural
The death of the person happened in suspicious circumstances
A ‘cause of death’ certificate has not been issued and is not likely to be issued for the person
The death of the person was a healthcare-related death
The death of the person occurred in care, custody or as a result of police operations.
Right to Refuse Treatment
Individuals have the legal right to refuse medical treatment.
Forcing treatment without consent can lead to assault and battery charges.
Examples of Refusal: Refusing medication, procedures, blood transfusions, or organ donations.
Terminally ill patients may choose to refuse life-sustaining treatments.
Respecting an individual's wishes regarding end-of-life care.
Voluntary Assisted Dying: Legal in Victoria, Australia, allowing terminally ill individuals to choose a medically assisted death.
Strict safeguards are in place to ensure voluntary assisted dying is used appropriately.
Conscientious Objection: Healthcare professionals have the right to refuse to participate in voluntary assisted dying.
End-of-Life Care
Key Considerations:
Respect for Wishes: Prioritize the individual's wishes and preferences.
Appropriate Care: Provide care tailored to the person's needs.
Legal Implications: Understand the legal framework for end-of-life care.
Communication: Ensure open communication with all involved parties.
Documentation: Document all aspects of care, discussions, and planning.
Cultural Sensitivity: Respect cultural practices and beliefs.
Focus Areas:
Quality End-of-Life Care: Promote person-centred care and address the unique needs of dying individuals.
Cultural Sensitivity: Recognize and respect diverse cultural practices and beliefs.
Legislation and Standards: Adhere to relevant laws and standards for end-of-life care.
Specific Areas of Legislation:
Substitute Decision Maker — Laws governing the appointment of a person to make decisions on behalf of an incapacitated individual.
Advance Care Directives — Laws related to creating and implementing advance care plans.
National Palliative Standards — provide guidance for managing end-of-life care.
Advance Directives
Advance care directives — documented statements outlining a person's wishes for future medical treatment.
This assist healthcare providers in making decisions when the person is unable to participate.
This is based on patient autonomy and decision-making.
Usually, advance care directives are made by:
The very elderly, who wish to avoid futile, painful and undignified care in the event of cardiac arrest or stroke
Those with a terminal illness who do not wish to prolong their lives
Those undergoing dangerous medical procedures.
Enduring Power of Attorney (EPOA) — Appointing a person to make decisions on behalf of the individual.
The National Framework for Advance Care Directives document identifies policy and best practice guidelines for advance care directives within the context of jurisdictional differences in law and processes in Australia.
Nurses should ensure that advance care directives comply with legislation, reflect the person's wishes, and are up-to-date.
Do not Resuscitate Orders
Do not Resuscitate Order (DNR) / Not for Resuscitation Order (NFR) — order written by the medical practitioners in the person’s medical record following a decision not to attempt to resituate the person if further intervention or treatment is considered futile or unwanted.
These are medical directives that indicate a patient's desire to avoid cardiopulmonary resuscitation (CPR) in the event of a cardiac or respiratory arrest.
The order for NFR must conform to the law of consent, and is based on an expressed decision by the person, their family and medical practitioners.
The reason behind the decision must be documented clearly and reviewed regularly.
Open Disclosure
Open disclosure — the open discussion of adverse incidents that have resulted in harm or potential harm while receiving healthcare with the person, their family and carers.
It involves communicating openly when healthcare does not go to plan and harm has been caused.
Adverse incidents that needed to be disclosed to the person:
medical errors
near miss or no harm
procedural errors
injury during treatment/procedure
Experienced or senior staff should facilitate the process of open disclosure.
Elements of Open Disclosure
An apology or expression of regret, which should include the words ‘I am sorry’ or ‘we are sorry’.
A factual explanation of what happened.
An opportunity for the individual, their family and carers to relate their experience.
A discussion of the potential consequences of the adverse event.
An explanation of the steps being taken to manage the adverse event and prevent recurrence.
The guiding principles of open disclosure framework | Open disclosure process |
1. Open and timely communication | 1. Detecting and assessing incident |
2. Acknowledgement | 2. Signalling the need for open disclosure |
3. Apology or expression of regret | 3. Preparing for open disclosure |
4. Support, and meeting the needs and expectations of individuals, their families and carers | 4. Engaging in open disclosure discussion |
5. Support, and meeting the needs and expectations of those providing healthcare | 5. Providing for follow-up |
6. Integrated clinical risk management and systems improvement | 6. Completing the process |
7. Good governance | 7. Maintaining documentation |
8. Confidentiality |
Legal Responsibilities of nursing Students
Nursing education requires practical or hands-on experience to learn skills and apply knowledge.
Students must be supervised to ensure patient safety and well-being.
Students should be prepared for new skills and have prior practice in nursing labs.
AINs are employed as unqualified staff and should not exceed their scope of practice.
Nursing students are registered with the NMBA during their education.
The NMBA prioritizes public safety and ensures that registered nurses meet high standards.
Nursing students must provide criminal checks and fitness for practice declarations.
Students working in child-related areas must have a working with children clearance or blue card.
Legal Issues in the Nursing Specialties
Medical/surgical nursing
Restraint minimisation in acute settings
Provision of appropriate standards of care by qualified nurses
Ensuring informed consent for medical treatment and care
Competency of nursing staff providing care
Adequate staffing levels for safe and competent care
Working with multidisciplinary healthcare team
Emphasis on care across the lifespan and person-centred care
Critical care nursing
Need for highly specialised skills and ongoing professional competence
Adequate staffing ratios in intensive care areas
Minimising reliance on intensive care setting apparatuses and equipment
Focus on person-centred care and client assessment
Decisions regarding life support or sustaining treatments
Do not resuscitate orders and end-of-life issues
Informed consent issues in critically ill individuals
Perioperative nursing
Anaesthetic and recovery room nursing specialised skills
Ongoing professional competence
Working with different individuals across the lifespan
Legal liability for smooth functioning of operating room procedures
Sterilisation of equipment, instrument and swab counts
Gerontological/aged care nursing
Issues in caring for the elderly related to confusion and dementia
Preventing and minimising use of restraint
Physical layout and design of facilities suitable for the elderly
Ensuring quality of life and choices for the elderly
Protecting the rights of the elderly in residential care facilities
Ensuring safety and accessibility for the elderly in different care environments
Workforce issues and adequate staffing to provide appropriate standard of care
Reporting of abuse
Community health nursing
Working with different individuals across the lifespan (e.g. family health, child health)
Different role expectations in community settings (e.g. more autonomous practitioners)
Working in different settings (e.g. schools, community centres, clinics, general practice settings, homes)
Working collaboratively with other healthcare team members for timely and appropriate care
Awareness of public and community health issues, immunisation, child abuse, workplace safety, personal safety
Hospital in the home
Clinical specialisation
Working with different individuals in their home settings
Need for careful documentation of all aspects of care
Initiating prompt referrals to other services or healthcare team members
Rural and remote area nursing
Lack of healthcare professionals
Problems of remoteness, costs and limited access to healthcare services
Issues of ensuring appropriate standards of care for the remote community
Different role expectations as remote area healthcare professionals (e.g. lack of emergency services, sole practitioners, level of responsibility)
Professional isolation and limited access for continuing professional development
Indigenous health
Ensuring cultural safety and providing culturally appropriate care
Providing right type of care at the right time by the right person in the right place
Lack of trained healthcare professionals
Limited culturally acceptable services, dominant western model of care
Health inequalities
Problems of remoteness, costs and limited access to healthcare services
Different role expectations as healthcare professionals
Lack of emergency services
Sole practitioners, greater level of responsibility, reporting issues
Accident and emergency department
Requirement for highly specialised skills
Level of responsibility and decision making
Dealing with aggressive and violent individuals, high-risk individuals, personal safety
Premature departures by individuals without adequate screening
Need for careful documentation of all emergency staff involved
Reporting incidents to authorities (e.g. road accidents, crime injuries, abuse)
Mental health nursing
Protecting rights of mentally ill individuals
Ensuring appropriate treatment and supervision of mentally ill individuals
Restriction on liberty of mentally ill persons
Participation/involvement in decision making
Voluntary and involuntary patients, community treatment orders, restraint
Controversial treatment modalities for mentally ill persons
Mental health legislation
Child health
Specialist skills in children’s health
Suitability of healthcare facility areas for treating and caring for children
Safety and security issues for children’s wards
Informed consent for treatment from parents or guardians on behalf of children
Screening of healthcare staff working with children
Screening of visitors in children’s wards
Mandatory reporting of child abuse
Ethical Aspects of Nursing
Nurses must adhere to a strict code of professional conduct.
While law sets minimum standards, ethics delineates the highest moral standards.
Ethical practice is crucial in healthcare due to advancements in medicine, resource allocation, quality of life issues, and individual rights protection.
Respecting the abilities and functions of co-workers is essential for providing high-quality care.
Nursing professional groups have specific codes of ethics that members must follow.
Ethics and Morality
Ethics — the moral principles guiding behaviour, unrelated to monetary rewards or prestige.
It involve evaluating people, situations, or actions based on moral values.
Various theories guide ethical behaviour, including deontological, teleological, moral rights, virtue ethics, and ethical principles.
Morality — the principles and standards that guide individual behaviour and decision-making.
Difference of Ethics and Morality
Morality is often seen as a personal or individual code of conduct, shaped by personal beliefs and values.
Ethics is more closely associated with professional or societal standards of behavior. It involves a broader consideration of the impact of one's actions on others and the community.
Ethical principlism — the view that ethical decision making and problem solving is best undertaken by appealing to sound moral principles.
Key Bioethical Principles that Guide Moral Reasoning in Healthcare Practice
Autonomy — the right of individuals to make their own decisions independently.
It imposes on healthcare professionals a moral obligation to respect a client’s choices regarding recommended medical treatment and associated care.
Non-maleficence — moral obligation to do no harm, to avoid causing unnecessary pain or suffering.
It provide justification for condemning any act that unjustly injures a person or causes them to suffer an avoidable harm.
Beneficence — moral obligation to do good, to promote the well-being of others, and to prevent harm.
It requires healthcare professionals to act in the best interests of their patient.
Justice — moral obligation to treat people fairly and equitably.
It requires that healthcare resources are distributed fairly and that all individuals have equal access to quality care.
Nursing Ethics
Bioethics — the study of moral and ethical issues arising from the practice of medicine and related fields.
It provides a framework for analysing and resolving complex ethical dilemmas that healthcare professionals encounter in their daily work.
Common Bioethics Topics:
Abortion: The ethical debate surrounding this centres on the moral status of the foetus, the rights of women, and the role of the state in regulating reproductive decisions.
Euthanasia and Assisted Suicide: These topics involve the ethical considerations surrounding the end of life, including the right to die with dignity and the role of healthcare professionals in assisting with death.
Organ Transplantation: Ethical issues related to this include the allocation of scarce resources, the use of deceased donors, and the potential for exploitation.
Reproductive Technology: The use of these technologies, such as in vitro fertilization (IVF) and genetic testing, raises ethical questions about the creation and manipulation of life.
Person's Right to Privacy and Confidentiality: Protecting patient privacy and maintaining confidentiality is a fundamental ethical principle in healthcare.
Informed Consent: Ensuring that patients are fully informed about the risks, benefits, and alternatives of medical procedures before making decisions.
Economic Rationalization of Healthcare: The ethical implications of cost-cutting measures and resource allocation in healthcare.
Research Ethics: Ensuring that research involving human subjects is conducted ethically, respecting the rights and well-being of participants.
Institutional Ethics Committees: These committees review research proposals to ensure they adhere to ethical standards and protect the rights of participants.
Nursing Ethics — the examination of all kinds of ethical and bioethical issues from the perspective of nursing theory and practice, which in turn rests on the core concepts of nursing.
Accountability
Accountability — In nursing, it means that nurses have the responsibility, legally, ethically and professionally, to provide safe, competence and ethical care.
Nurses are accountable for their actions and decisions, and they must be able to justify their practice to patients, families, and other healthcare professionals.
Nurses are accountable for reporting behaviour that endangers patient safety.
Following policies and guidelines promotes safe and effective care.
Codes of conduct and ethics guide regulatory authorities in assessing misconduct.
Nurses contribute to patient care by implementing treatment plans, providing feedback, and documenting observations.
Values
Values — a belief about the worth of a particular idea or behaviour, or something an individual views as desirable or important.
Values are shaped by family, culture, education, and experiences.
Values guide a person's interactions and decisions.
Everyone has a unique set of values.
Individuals prioritize certain values over others.
Values motivate and guide nurses' professional behaviour.
Ethical behaviour and accountability are core nursing values.
Responsibility, patient safety, and advocacy are also important.
Examples of professional values applied to nursing practice
Caring
Compassion
Courage
Communication
Competence
Commitment
Ethical Issues and Moral Dilemmas
Moral Dilemmas — situations that involve two competing or conflicting moral choices, neither of which is a desirable option in terms of outcomes.
Nurses must apply ethical reasoning and moral decision making process to deal with ethical and moral issues.
Common ethical and bioethical issues
Genetic engineering
Artificial fertilisation
Contraception
Therapeutic abortion
Child abuse
Artificially prolonging life
Voluntary euthanasia
Not for resuscitation orders
Selective non-treatment
Informed consent
Withholding information
Right to refusal of treatment
Quality versus quantity of life
Organ transplantation
End-of-life issues and dying with dignity
Non-therapeutic research
Use of restraints
Confidentiality
Conflict of values and beliefs between members of the health team
Advance care planning
Disclosing and reporting professional practice errors
Veracity, duty and complications in truth telling
Allocation of health resources
Common everyday ethical issues faced by nurses
How to help a person in distress in the present time
How to stop things getting worse for a person
How to best support a family member or carer during times of distress and when the system is not assisting
How to make things less traumatic for someone who is suffering
How to reduce anxiety and vulnerability of people being cared for
Where can nurses get help for own distress
How to make a difference in situations where moral interest of others is not considered
Ethical Decision Making
Ethical decision-making in healthcare requires a rational and systematic approach.
Values, beliefs, and contextual factors influence moral reasoning.
Common themes include patient well-being, accountability, collaboration, and concern for others.
Ethical decision-making model:
Clearly state the problem
Get all the facts
Consider the fundamental ethical principles
Consider how the problem would look from another perspective or using another theory
Identify ethical conflicts
Make the ethical decision and evaluate the decision.
Steps of the nursing process in moral decision making:
Assess the moral/ethical situation
Identify (diagnose) the moral problem/s
Set moral goals and plan a moral course of action
Implement the moral plan of action
Evaluate the moral outcomes of the action.
Revisit the steps from the beginning if the desired moral outcomes do not occur.
When an ethical decision is to be made, the following factors must be considered:
The ethical dilemma must be recognised and defined.
All the facts relevant to the issue and to the individuals involved must be obtained.
The people involved in making a decision must understand the relevant moral rules and principles involved and be able to apply them in an appropriate manner.
Proper evaluation must be made of possible solutions to the problem and of the strategies to be implemented.
Examples of nurses’ obligations in ethical decisions
Maximise the individual’s wellbeing.
Balance the person’s need for autonomy with family members’ responsibilities for the person’s wellbeing.
Support each family member and enhance the family support system.
Carry out hospital policies.
Protect other individuals’ wellbeing.
Protect the nurse’s own standards of care.
Advocacy
Advocacy — In nursing, it means that the nurse acts for and on behalf of the individual in their care.
It is recognised as a professional, moral and ethical obligation of nurses.
The core attributes of nursing advocacy are identified as:
Safeguarding the person’s autonomy
Acting on behalf of the person
Championing social justice in the provision of healthcare.
In nursing, the concept of advocacy is based in nursing ethics, and involves respecting a person’s right to:
Be informed
Make decisions and choices
Confidentiality
Privacy and dignity
Hold their own ethical and religious beliefs.
Forms of Advocacy in Nursing Practice
Informal advocacy — arises naturally from a nurse's interaction with patients and their families. Nurses may advocate for their patient’s rights through everyday interactions.
Advocating for a patient to receive a specific treatment or service
Helping a patient navigate the healthcare system
Supporting a patient's decision-making process
Formal Advocacy — involves organized efforts to influence policy or practice on behalf of patients or the nursing profession. Nurses may participate in advocacy groups or organizations to advocate for specific issues.
Testifying before legislative committees
Writing letters to policymakers
Participating in public campaigns
Clinical Interests
Specific Acts relevant to the nursing profession
Act | Description |
Child Protection Act 1999 (QLD) | Governs the protection of children in Queensland, outlining mandatory reporting obligations for healthcare professionals. |
Coroners Act 2003 (QLD) | Provides the framework for investigating reportable deaths and determining causes of death in Queensland. |
Freedom of Information Act 1982 (Cth) | Allows individuals to access information held by Commonwealth government agencies, impacting health records and patient information in federal agencies. |
Health Practitioner Regulation National Law Amendment Act 2009 (Cth) | Governs the regulation and accreditation of health practitioners, including nurses, across Australia under the National Registration and Accreditation Scheme. |
Mental Health Act 2016 (QLD) | Outlines the rights of patients with mental illnesses and the responsibilities of healthcare professionals regarding the treatment and care of individuals under mental health care. |
Work Health and Safety Act 2011 (QLD) | Ensures the safety of workers, including healthcare professionals, by mandating safe working environments and practices in Queensland workplaces, including hospitals and clinics. |
Drugs, Poisons and Controlled Substances Act 1981 (VIC) | Regulates the control of drugs and poisons, including their manufacture, supply, and use, particularly in healthcare. |
Human Tissue Act 1982 (VIC) | Regulates the donation, use, and transplantation of human tissue, ensuring ethical standards are followed in medical procedures. |
Professional standards for nurses
Practise legally
Legal Compliance
Practise safely, effectively and collaboratively
Person-centred practice
Cultural practice and respectful relationships
Act with professional integrity
Professional behaviour
Teaching, supervising and assessing
Research in health
Promote health and wellbeing
Health and wellbeing
Recognising professional boundaries
Is there a power imbalance in the professional relationship?
Are expectations clear in the professional relationship?
Will performing this activity cause conflict of interest, risks, impair professional judgment?
Is there a dual relationship in the situation?
Is there over-involvement in the professional relationship?
Is there under-involvement, disrespect, omission or indifference, lack of care?
Is there an exploitation of vulnerability that is likely to impact on decision making?
Is the action likely to be seen as assault, unauthorised restraint or unnecessary force?
Is the behaviour within expected legal and ethical conduct?
Steps to observe when witnessing a signature on written consent forms
Ensure that all sections of the consent form are completed. Never ask the person to sign a blank consent form.
If the person wants to alter the consent form the treating medical practitioner must be informed immediately.
If the person asks questions about the nature of the procedure or treatment, the treating medical practitioner must be informed immediately.
On contacting the treating medical practitioner, a relevant entry must be made in the health records including the medical practitioner’s response.
If the person refuses to sign the consent form, the treating medical practitioner and appropriate administrative staff must be notified and the refusal documented in the health records.
Quality documentation
Important considerations for quality documentation:
Reports should be accurate, brief and complete
Reports should be legibly written
Reports should be objectively written
Entries in reports should be made at the time a relevant incident occurs, or as soon as possible after the incident
Abbreviations should not be used in reports unless they are accepted within the healthcare organisation and there is a policy acknowledging this or they are widely acknowledged medical abbreviations
If medical terminology is used in reports, the nurse should be sure of the exact meaning, otherwise it could prove misleading
Any errors made in recording should be dealt with by drawing a line through the incorrect entry and initialing it before continuing
No entry concerning the person’s treatment should be made on behalf of another nurse
All reports need to be dated and signed
To reduce the risk of an incorrect entry being made:
Don’t make an entry in a person’s health record before checking the name on the record
Don’t make an entry in a person’s health record by identifying room or bed number only
Make sure the person’s name and identifying number is on every sheet/page of the document before making an entry
Avoid wherever possible making notes concerning a person on loose paper for rewriting later into the person’s notes.